Abstract
Hydrogen peroxide, at 35% concentration, is a potent surface cleaner not intended for ingestion. We present a case of unintentional ingestion of 35% hydrogen peroxide by a 3-year-old male that resulted in portal venous gas. In particular, we illustrate the correlation of ultrasound with computed tomography with the prospect of pediatric patients avoiding unnecessary ionizing radiation and barriers to care.
Introduction
Hydrogen peroxide is an oxidizing agent used as a disinfectant [Citation1]. Household hydrogen peroxide is 3% concentration and unlikely to cause significant harm if ingested unintentionally. However, at 35% concentration, 30 mL can produce over 3000 mL of oxygen [Citation2]. Gas emboli, gastrointestinal bleeding, and death are reported complications from hydrogen peroxide ingestion [Citation3]. Hyperbaric oxygen (HBO) therapy is a treatment option. However, there are no guidelines to identify high-risk patients to treat with HBO [Citation3, Citation4]. Here, we present a case of a patient not treated with HBO and the decision-making involved regarding his treatment plan.
Case presentation
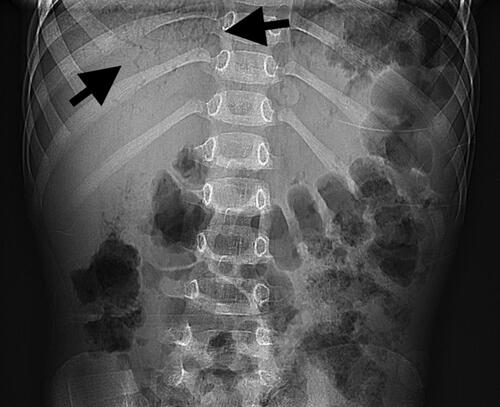
An unvaccinated 3-year-old boy presented to a community emergency department after unintentionally ingesting a couple of sips of 35% hydrogen peroxide. According to the report on presentation, he mistook hydrogen peroxide for water. There were no co-ingestions. The patient had multiple episodes of vomiting and hematemesis en route to the hospital. At the community hospital, his vital signs were temperature (T): 98 °F, heart rate (HR): 106 beats per minute, respiratory rate (RR): 24 breaths per minute, oxygen saturation (SpO2): 98% on room air, and weight: 12.7 kilograms (kg). The community hospital contacted their state poison center, which recommended an oral challenge. The patient vomited again, prompting further laboratory and radiographic workup. An abdominal radiograph () revealed portal venous gas. A complete blood count and comprehensive metabolic panel were normal. The community hospital again conferred with their poison center for further recommendations. The patient received a normal saline bolus and intravenous (IV) ondansetron. A nasogastric tube placed to low intermittent wall suction allowed for gastric decompression. An ambulance transferred the patient across state lines to the nearest pediatric tertiary care facility.
Figure 1. Abdominal radiograph. Upright radiograph demonstrates branching lucencies (arrows) in the right upper quadrant, compatible with portal venous gas.
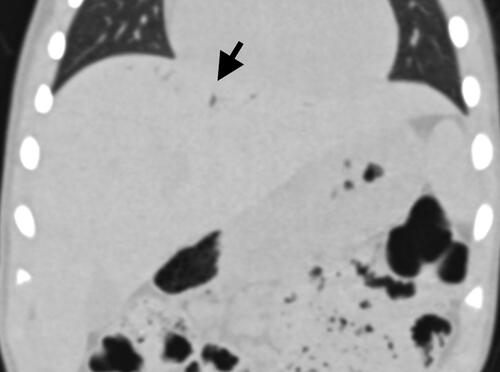
His parents felt he was not acting normally at the community hospital but reported that his mental status had improved when he arrived at the pediatric tertiary care facility. The toxicology service was consulted by the emergency department and recommended computed tomography (CT) scans of the head, chest, abdomen, and pelvis without contrast to detect the presence and volume of gas emboli and subsequent need for HBO therapy. The abdominal CT ( and ) demonstrated small to moderate portal venous gas. CT imaging was otherwise negative for any abnormalities.
Figures 2. Abdominal computed tomography (CT) without contrast. Representative axial image confirms linear gas densities (arrow) within the hepatic dome.

Figures 3. Abdominal computed tomography (CT) without contrast. Representative coronal lung window image confirms linear gas densities (arrow) within the hepatic dome.
The pediatric tertiary care center did not have emergent HBO therapy, but used a pediatric echocardiogram to assess risk of cerebral gas embolism requiring transfer to an HBO-capable facility. The echocardiogram demonstrated a normal heart with no atrial or ventricular septal defect, so the patient remained at the pediatric tertiary care center. Furthermore, after a discussion with the attending radiologist, an abdominal ultrasound (US) was performed to determine if gas could be visualized on US to use serial US to assess the resolution of portal venous gas instead of imaging that required radiation. Abdominal US ( and ) showed gas shadows in the liver.
Figures 4. Abdominal sonography. Representative sagittal image of the liver demonstrates echogenic foci with posterior acoustic shadowing in the peripheral hepatic dome, compatible with portal venous gas. On follow up the next day, this finding had resolved.

Figure 5. Abdominal sonography. Representative sagittal image of the liver demonstrates echogenic foci with posterior acoustic shadowing in the peripheral hepatic dome, compatible with portal venous gas. On follow up the next day, this finding had resolved.

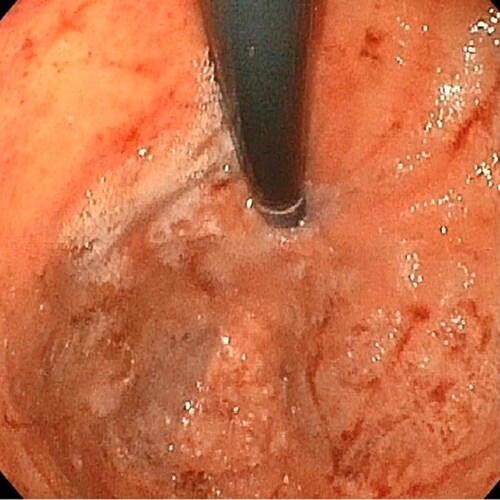
Figure 6. Endoscopy demonstrated superficial erosions, erythema, and edema of the gastric body after ingestion of ∼30ml of 35% hydrogen peroxide.

Figure 7. Endoscopy demonstrated superficial erosions, erythema, and edema of the cardia/fundus after ingestion of ∼30ml of 35% hydrogen peroxide.
The patient was admitted to the pediatric intensive care unit (PICU). His hourly neurological checks remained normal overnight. A repeat abdominal US showed resolution of gas. The patient was doing well and was transferred to the pediatric gastroenterology service.
Pediatric gastroenterology was consulted due to the caustic nature of 35% hydrogen peroxide. They recommended keeping the patient nil per os (NPO) with maintenance IV fluids and planned an endoscopy around 48 h post-ingestion. Esophagogastroduodenoscopy (EGD) performed on hospital day 3 demonstrated erythema and edema (Zargar grade 1) in the stomach without ulcers ( and ). The esophagus and proximal duodenum were normal. His diet was advanced as tolerated, and he was discharged on hospital day 3 on sucralfate and omeprazole for 2 weeks.
Discussion
This case illustrates the use of abdominal ultrasound to detect portal venous gas and cardiac ultrasound to assess risk of right-to-left shunt following ingestion of high concentration hydrogen peroxide.
Given the report of abnormal mental status and findings of portal venous gas on abdominal radiograph, head and abdominal CT scans with effective radiation dose of 3.16 millisieverts (mSv) were first performed to rule out cerebral or systemic gas emboli. After the head CT scan was normal, an echocardiogram was used to determine if the child had an atrial or ventricular septal defect to consider right-to-left shunting of gas emboli into arterial circulation. If the child had a septal defect, transfer to a center with emergency hyperbarics would have been considered instead of observing at a referral center due to an increased risk of acute decompensation. Serial abdominal US was used to evaluate portal venous gas to reduce radiation exposure to this toddler instead of additional CT scans. A previous case illustrated the use of ultrasound to identify portal venous gas in an adult [Citation4].
“Our patient also underwent EGD, which found only mild erythema and edema (Zargar grade 1). There are no specific endoscopy guidelines for pediatric ingestions of high concentration hydrogen peroxide. A retrospective ten-year study through the Illinois Poison Center found that EGD results were consistently benign with mild (Zargar 1) or normal findings [Citation5]. The authors advocated against routine EGD in patients with high-concentration hydrogen peroxide ingestions [Citation5]. Hatten et al. studied 294 cases over ten years from National Poison Database System (NPDS) [Citation6]. Among the 118 patients undergoing EGD, five had severe injuries (Zargar grade 3: deep ulcerations; or Zargar grade 4: necrosis), predominately characterized by vomiting, hematemesis, and unintentional ingestion of high-concentration hydrogen peroxide. They found that all significant mucosal injury (Zargar 3 or 4) would have been found by only performing EGD in patients “with evidence of embolic event, significant gastrointestinal bleeding (melena or more than scant hematemesis), pneumomediastinum on radiography, or history of gastric bypass” [Citation6].
Aeromedical transport might increase further oxygen bubble formation or bubble size. If inter-hospital transfer is necessary for a patient with cerebral or systemic gas embolism, we suggest ground transport or low-altitude air transport. We recommend contacting your poison control center or local toxicologist for advice regarding these patients.
Conclusion
This case highlights the use of ultrasound in a pediatric ingestion of high-concentration hydrogen peroxide. Abdominal ultrasound demonstrated portal venous gas and avoided further radiation exposure to a young child. Exclusion of cardiac septal defects with echocardiogram made cerebral gas embolism less likely. A child with a normal neurological exam and no cardiac septal defects may be observed clinically without CT. A child without hematemesis may not need endoscopy.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Manning EP, Laskowski LK, Nelson LS, et al. Images in emergency medicine. Young woman with epigastric pain and vomiting. Ingestion of 35% hydrogen peroxide. Ann Emerg Med. 2014;64(3):1–4.
- Mullins ME, Beltran JT. Acute cerebral gas embolism from hydrogen peroxide ingestion successfully treated with hyperbaric oxygen. J Toxicol Clin Toxicol. 1998;36(3):253–256.
- French LK, Horowitz BZ, McKeown NJ. Hydrogen peroxide ingestion associated with portal venous gas and treatment with hyperbaric oxygen: a case series and review of the literature. Clin Toxicol (Phila). 2010;48(6):533–538.
- Hendriksen SM, Menth NL, Westgard BC, et al. Hyperbaric oxygen therapy for the prevention of arterial gas embolism in food grade hydrogen peroxide ingestion. Am J Emerg Med. 2017;35(5):809.e5-809–e8.
- Karydes H, Bryant SM. Hydrogen peroxide ingestions: the scope of the injury. Clin Toxicol (Phila). 2012;50(4):271–272.
- Hatten BW, French LK, Horowitz BZ, et al. Outcomes after high-concentration peroxide ingestions. Ann Emerg Med. 2017;69(6):726–736.e2.
