Abstract
Optic neuritis is an autoimmune condition where demyelination of the optic nerve leads to visual impairment. It is typically associated with autoimmune disorders but can also be triggered by certain drugs known for causing axonal demyelination and nerve fiber degradation. Metronidazole, a common antibiotic, has been identified as one such drug. We describe the acute onset of optic neuritis after a single intravenous dose of metronidazole. Initially presenting with symptoms suggestive of acute gastroenteritis, her condition rapidly progressed to severe visual loss in her right eye following metronidazole administration. She was treated with intravenous steroids and showed good recovery in a follow-up visit. Optic neuritis is an uncommon adverse reaction associated with metronidazole therapy. While the precise cause is under debate, various studies suggest that neuronal damage could be due to free radicals, thiamine analogues, oxidative stress, or the inhibition of protein synthesis. The management of optic neuritis, regardless of the cause, typically involves high-dose corticosteroids.
Keywords:
Introduction
Metronidazole, a widely used antibiotic and antiprotozoal medication, is generally very safe [Citation1]. A rare side effect of metronidazole is optic neuritis [Citation2–7]. We present, in accordance with the CARE Guidelines (https://www.care-statement.org), a case of sudden vision loss and reversible optic neuritis after treatment with intravenous metronidazole.
Case report
A 35-year-old lady with no significant past medical history presented to the emergency department (ED) with a five-day history of fever and abdominal pain, associated with multiple episodes of vomiting and watery diarrhea. Her vital signs were within normal limits, other than mild tachycardia (114 beats/min) and hypotension (108/73 mmHg). Systemic examinations revealed no abnormalities other than dry mucus membranes indicating dehydration. She received 1000 mL of intravenous 0.9% Sodium Chloride, 4 mg of intravenous ondansetron, and 500 mg of intravenous metronidazole for presumed acute gastroenteritis. Blood investigations revealed hyperchloremic metabolic alkalosis with hypokalemia (2.9 mEq/L) (), and she received 30 mg oral potassium chloride.
Table 1. Important lab investigations.
The patient was discharged with advice on maintaining good hydration and a prescription for oral metoclopramide. She returned to the ED the next day with a complete loss of vision in her right eye and a mild diffuse headache, and reported that her visual disturbance began shortly after receiving IV medications in the previous visit and worsened in the ensuing day. The patient reported no relevant family history and denied taking any supplements or chronic medication prior to the episode.
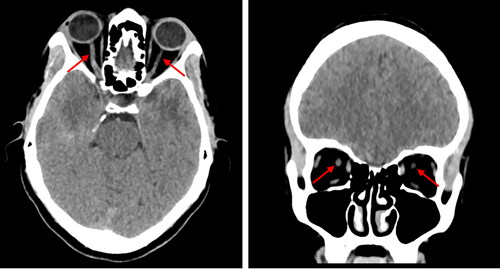
On her second visit, her vital signs were again normal. However, the visual acuity in her right eye was significantly decreased to merely light perception compared to the left. Additionally, her pupils were equally reactive bilaterally with normal, painless eye movements. Neither of the eyes showed any discharge or conjunctival injection. A slit lamp examination revealed optic disc edema with normal macula and normal intra-ocular pressure in the right eye. Non-contrast computed tomography (CT) showed an increased right optic nerve sheath diameter (). Neurological assessments, including cerebellar examination, showed no abnormalities.
Figure 1. Axial and coronal reconstruction of non-contrast CT head showing the right optic nerve sheath diameter greater than left (red arrows).
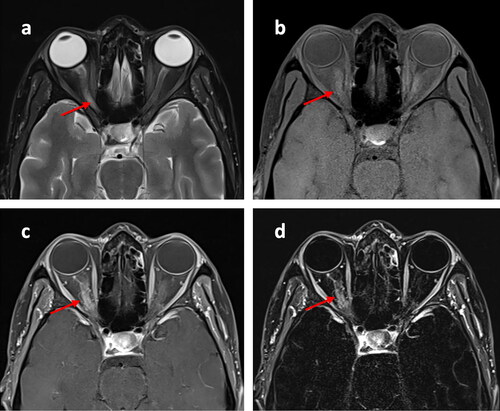
Magnetic resonance imaging (MRI) scan of the head and orbits revealed swelling and abnormal T2WI hyperintensity in the right optic nerve, confirming the presence of optic neuritis with a normal appearing left optic nerve (). Blood investigations, including autoimmune screening, were normal. Lumbar puncture showed clear cerebrospinal fluid (CSF) and raised white blood cells (WBCs) with lymphocytic predominance. However, there was no evidence of bacterial, mycobacterial, fungal, or viral infection, or malignancy ().
Figure 2. Axial T2 MRI of the orbits showing a swollen hyperintense right optic nerve (a). Axial T1 FS pre-contrast (b), post-contrast (c), and subtraction (d) MRI of the orbits, showing right optic nerve post-contrast enhancement. Right optic nerve is highlighted with arrows.
She received 1 gram of intravenous methylprednisolone for five days and was discharged after a week’s hospital stay, with scheduled outpatient follow-up appointments. A follow-up examination revealed a complete resolution of optic disc edema and improvement in the patient’s vision to close finger counting, ten days after the discharge.
Discussion
Metronidazole, a synthetic nitroimidazole compound, offers broad-spectrum antibiotic and antiprotozoal coverage, primarily targeting anaerobic bacteria [Citation8]. Metronidazole diffuses into the organism, inhibits protein synthesis by interacting with ribonucleic acid (RNA), and causes a loss of helical deoxyribonucleic acid (DNA) structure and strand breakage [Citation9]. Despite its safety record, rare cases of serious neurotoxic effects like encephalopathy, peripheral neuropathy, and optic neuritis have been reported [Citation10].
Optic neuritis, primarily autoimmune, leads to optic nerve demyelination and vision loss; the exact impact of metronidazole remains unclear. Rao et al. connected neuronal damage to free radicals, Alston et al. identified neuropathy from metronidazole’s conversion into thiamine analogs, and Hassan et al. demonstrated its neurotoxicity via thiamine deficiency and oxidative stress in a study with 60 albino Wistar rats [Citation11–13]. Other researchers hypothesize that metronidazole’s binding to RNA molecules may inhibit protein synthesis, subsequently triggering axonal degeneration [Citation14]. Since the early 1990s, increasing reports have linked metronidazole with optic neuropathy [Citation7]. Among twelve published cases (five case reports and one case series), most patients received longer courses and higher doses (1000-1500 mg/day) before visual symptoms appeared, but our patient received a single dose of 500 mg metronidazole (). All but one case had complete resolution after discontinuing metronidazole and treatment with corticosteroids [Citation2–7]. All other cases besides the present case had bilateral optic neuritis. Also, while others had additional central nervous system issues, our patient experienced solely optic neuritis.
Table 2. Previously published case reports and series on metronidazole induced optic neuropathy.
Treatment of optic neuritis of any cause includes high-dose corticosteroids. Some speculate that IV corticosteroids might be better than oral steroids in promoting faster visual recovery and possibly delaying the onset of multiple sclerosis [Citation15–17]. Immunomodulatory therapies like intravenous immunoglobulin or plasma exchange have not been proven beneficial in optic neuritis [Citation18–20]. However, in case of metronidazole induced optic neuritis, immediate discontinuation of metronidazole should also be considered.
This case report contributes valuable information to the existing body of scientific literature. To our knowledge, it presents the first instance of optic neuritis induced by a single dose of metronidazole. It’s important to note a limitation in our conclusion: we did not re-administer the drug to confirm its causative role. Nevertheless, considering that our thorough assessments uncovered no other potential causes, and in line with the Naranjo adverse drug reaction (ADR) probability scale, metronidazole was identified as the "probable" culprit behind the patient’s optic neuritis (ADR probability score of 6) [Citation21].
Conclusion
Optic neuritis is a rare complication of metronidazole therapy. Immediate discontinuation of metronidazole and treatment with high-dose corticosteroids appear to bring complete recovery in most cases.
Consent statement
An informed written consent was obtained from the patient to publish this report after anonymizing all the personal details, in accordance with the journal’s patient consent policy.
CRediT author statement
Kaleem Basharat: involved in data curation and wrote original draft. Muhammad Abd Ur Rehman: validated, wrote, reviewed, and edited the manuscript. Nada Saeed Amr Elharabi: conceptualized the study and did literature review. Waleed Awad Salem: reviewed and edited the manuscript, also supervised the study.
CARE Checklist.pdf
Download PDF (777.8 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Data sharing is not applicable to this article as no new data were created or analyzed in this study.
Additional information
Funding
References
- Löfmark S, Edlund C, Nord CE. Metronidazole is still the drug of choice for treatment of anaerobic infections. Clin Infect Dis. 2010;50 Suppl 1:1–6. doi:10.1086/647939.
- de Bleecker JL, Leroy BP, Meire VI. Reversible visual deficit and corpus callosum lesions due to metronidazole toxicity. Eur Neurol. 2005;53(2):93–95. doi:10.1159/000085506.
- McGrath NM, Kent-Smith B, Sharp DM. Reversible optic neuropathy due to metronidazole. Clin Exp Ophthalmol. 2007;35(6):585–586. doi:10.1111/j.1442-9071.2007.01537.x.
- Anwyll N, Gerry P, Gormley J. Reversible optic neuropathy secondary to metronidazole. BMJ Case Rep. 2020;13(12):e237141. doi:10.1136/bcr-2020-237141.
- Peng PH, Wu TE, Lin TY. Metronidazole-Induced irreversible optic neuropathy. Case Rep Ophthalmol. 2021;12(2):392–395. doi:10.1159/000512625.
- Nuro E, Bursztyn LL, Mendonça DA, et al. Neuroimaging evidence of optic tract involvement in metronidazole-induced optic neuropathy. Can J Neurol Sci. 2023;50(2):290–291.
- Putnam D, Fraunfelder FT, Dreis M. Metronidazole and optic neuritis. Am J Ophthalmol. 1991;112(6):737. doi:10.1016/s0002-9394(14)77290-3.
- Rosenblatt JE, Edson RS. Metronidazole. Mayo Clin Proc. 1983;58(3):154–157.
- Edwards DI. Nitroimidazole drugs–action and resistance mechanisms. I. Mechanisms of action. J Antimicrob Chemother. 1993;31(1):9–20. doi:10.1093/jac/31.1.9.
- Hernández Ceruelos A, Romero-Quezada LC, Ruvalcaba Ledezma JC, et al. Therapeutic uses of metronidazole and its side effects: an update. Eur Rev Med Pharmacol Sci. 2019;23(1):397–401.
- Rao DN, Mason RP. Generation of nitro radical anions of some 5-nitrofurans, 2- and 5-nitroimidazoles by norepinephrine, dopamine, and serotonin. A possible mechanism for neurotoxicity caused by nitroheterocyclic drugs. J Biol Chem. 1987;262(24):11731–11736.
- Alston TA, Abeles RH. Enzymatic conversion of the antibiotic metronidazole to an analog of thiamine. Arch Biochem Biophys. 1987;257(2):357–362.
- Hassan MH, Awadalla EA, Ali RA, et al. Thiamine deficiency and oxidative stress induced by prolonged metronidazole therapy can explain its side effects of neurotoxicity and infertility in experimental animals: effect of grapefruit co-therapy. Hum Exp Toxicol. 2020;39(6):834–847. doi:10.1177/0960327119867755.
- Bradley WG, Karlsson IJ, Rassol CG. Metronidazole neuropathy. Br Med J. 1977;2(6087):610–611.
- Gal RL, Vedula SS, Beck R. Corticosteroids for treating optic neuritis. Cochrane Database Syst Rev. 2015;2015(8):Cd001430.
- Beck RW, Cleary PA, Anderson MM, Jr., et al. A randomized, controlled trial of corticosteroids in the treatment of acute optic neuritis. The optic neuritis study group. N Engl J Med. 1992;326(9):581–588. doi:10.1056/NEJM199202273260901.
- Beck RW, Cleary PA, Trobe JD, et al. The effect of corticosteroids for acute optic neuritis on the subsequent development of multiple sclerosis. The optic neuritis study group. N Engl J Med. 1993;329(24):1764–1769. doi:10.1056/NEJM199312093292403.
- Noseworthy JH, O’Brien PC, Petterson TM, et al. A randomized trial of intravenous immunoglobulin in inflammatory demyelinating optic neuritis. Neurology. 2001;56(11):1514–1522. doi:10.1212/wnl.56.11.1514.
- Roed HG, Langkilde A, Sellebjerg F, et al. A double-blind, randomized trial of IV immunoglobulin treatment in acute optic neuritis. Neurology. 2005;64(5):804–810. doi:10.1212/01.WNL.0000152873.82631.B3.
- Ruprecht K, Klinker E, Dintelmann T, et al. Plasma exchange for severe optic neuritis: treatment of 10 patients. Neurology. 2004;63(6):1081–1083. doi:10.1212/01.wnl.0000138437.99046.6b.
- Naranjo CA, Busto U, Sellers EM, et al. A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther. 1981;30(2):239–245. doi:10.1038/clpt.1981.154.
