ABSTRACT
Background
Persistent pain is a prevalent condition that negatively influences physical, emotional, social and family functioning in adolescents. Pain science education is a promising therapy for adults, yet to be thoroughly investigated for persistent pain in adolescents. There is a need to develop suitable curricula for adolescent pain science education.
Methods
An interdisciplinary meeting of 12 clinicians and researchers was held during March 2018 in Adelaide, South Australia. An a priori objective of the meeting was to identify and gain consensus on key learning objectives for adolescent pain science education using a modified-Delphi process.
Results and Conclusion
Consensus was reached via a modified Delphi process for seven learning objectives to form the foundation of a curriculum: 1) Pain is a protector; 2) The pain system can become overprotective; 3) Pain is a brain output; 4) Pain is not an accurate marker of tissue state; 5) There are many potential contributors to anyone’s pain; 6) We are all bioplastic and; 7) Pain education is treatment. Recommendations are made for promising areas for future research in adolescent pain science education.
RÉSUMÉ
Contexte: La douleur persistante est une pathologie répandue qui influence négativement le fonctionnement physique, émotionnel, social et familial chez les adolescents. L'éducation à la science de la douleur est une thérapie prometteuse pour les adultes, mais doit encore faire l'objet d’études plus approfondies en ce qui concerne la douleur persistante chez les adolescents. Il est nécessaire d'élaborer des programmes d'études appropriés pour l'éducation aux sciences de la douleur chez les adolescents.
Méthodes: Une réunion interdisciplinaire de 12 cliniciens et chercheurs s'est tenue en mars 2018 à Adélaïde, en Australie du Sud. L'un des objectifs de la réunion fixé a priori était de déterminer par consensus les principaux objectifs d'apprentissage de l'éducation à la science de la douleur chez les adolescents à l'aide d'un processus Delphi modifié.
Résultats et conclusion: Un processus Delphi modifié a permis d’atteindre un consensus sur les sept objectifs d'apprentissage qui devraient constituer la base d'un programme d'études : 1) La douleur est un protecteur ; 2) Le système de la douleur peut devenir surprotecteur ; 3) La douleur est un produit du cerveau; 4) La douleur n'est pas un marqueur précis de l'état des tissus ; 5) Il y a beaucoup de acteurs contributifs potentiels à la douleur de chaque personne; 6) Nous sommes biologiquement plastiques et; 7) L'éducation à la douleur est un traitement. Des recommandations sont formulées en ce qui concerne les domaines les plus prometteurs sur lesquels devraient porter les futures études en matière d’éducation des adolescents à la science de la douleur.
Introduction
Pain is common in adolescents.Citation1,Citation2 For a significant minority, pain persistsCitation3 and negatively impacts physical, emotional, social and family functioning.Citation4–Citation9 Understanding why pain persists and how to respond effectively to it can be challenging for those who experience persistent pain. Guidelines recommend healthcare providers assist adolescents with persistent pain to understand their pain experience.Citation10 An established form of education – pain science education – aims to provide a framework to understand one’s pain condition, by exploring what pain is, what function it serves, and how it works.Citation11 Research suggests that when pain science education is delivered in conjunction with other treatments within a biopsychosocial framework, adults with persistent pain experience clinically meaningful improvements in pain and disability.Citation11–Citation13 However, little is known about the application or effectiveness of pain science education for adolescents with persistent pain.
Broadly, pain education can be divided into two components: pain science education (i.e. how and why is pain produced?), and pain management education (i.e. what should you do about your pain?). Pain science education aims to align a clinician and patient’s understanding of pain with modern pain science, whereby pain represents a need to protect, rather than a perceived reflection of tissue damage.Citation14,Citation15 Commonly pain science education involves changing one’s concept of pain from a biomedical paradigm toward a biopsychosocial model that considers the experience of pain to be influenced by biological (e.g. nociception, genetics), psychological (e.g. cognitions, beliefs), and social/contextual (e.g. family, school) factors.
Interdisciplinary care is recommended as the optimal model for treating adolescent persistent pain,Citation10 however, many therapies offered in interdisciplinary care may appear counterintuitive to one’s understanding of the cause of their pain. For example, if someone with persistent pain believes their pain is an indicator of tissue damage, they may consider psychological therapies irrelevant, and limit movement or immobilize the painful body part to prevent further damage. One potential method to reverse this situation is to give people with pain a clear explanation of why psychological therapies and movement-based therapies are key strategies for persistent pain. As such, pain science education acts as a prelude to pain management education; it is not intended to replace active rehabilitation interventions, but rather to enhance and facilitate their acceptance. Additionally, improving one’s understanding of pain may influence the perception of pain itself, as demonstrated in studies with adults.Citation11,Citation12 This is predicted on the basis of contemporary theories of brain and neurological function (see Wallwork et al.Citation16), which emphasize the capacity of cortical processing to integrate cognitive and contextual variables.Citation17,Citation18
There is limited evidence investigating pain science education in adolescents. To date, three school-based studies have demonstrated that adolescents have the capacity to learn pain science topics via a 30-minute lecture,Citation19 an 11-minute video,Citation20 and a four-week classroom-style intervention.Citation21 The classroom intervention study is the only randomized controlled trial, investigating the effects of adolescent pain science education, by combining education with neck exercises for chronic neck pain.Citation21 However, this study was too small to detect clinically-meaningful effects, and included a short follow-up (i.e. 4 weeks).
Curricula-building is an important part of health education, yet no curricula exist to educate adolescents about pain. We set out to begin the process of developing an adolescent pain science education curriculum, starting with establishing key learning objectives. An interdisciplinary meeting was held in March 2018 in Adelaide, South Australia. The a priori objective of the meeting was to identify and gain consensus on key learning objectives for adolescent pain science education using a modified-Delphi process.
Methods
Design
We conducted a three-round modified Delphi process during an interdisciplinary meeting on 20-21st March 2018 in Adelaide, Australia. The Delphi approach is a consensus method to determine the extent to which a group of individuals agree on given topics, using iterative rounds, interspersed with controlled feedback.Citation22 A modification involved the fact that respondents were not anonymous during the discussion process.
Panel
A convenience sample of participants were invited to attend the meeting if they were available to attend a workshop in Adelaide on 20-21st March 2018 following the Pain Adelaide Scientific Meeting on 19th March 2018, and satisfied one or more of the following criteria: previously published in the field of pain science education, pediatric pain or pain perception, working clinically in pediatric pain medicine, expertise in pain curriculum development or consumer-targeted pain education resources or pursing graduate studies in pediatric pain. There is no consensus regarding the optimal number of panelists in the Delphi-process; the experience and expertise of the panelists is considered more important than the number.Citation23 G.L.M. invited panelists, coordinated the meeting and served as moderator.
Procedures
On the first day, panelists attended a series of presentations to review the state of the field of pediatric pain science education (see for meeting agenda). On day two, a modified Delphi study was conducted to identify and gain consensus on pain science education learning objectives for adolescents. The number of rounds was predetermined at 3. Panelists were instructed to focus on the content of the learning objective, not on developing age-appropriate language for that learning objective.
Table 1. Meeting agenda surrounding modified-Delphi.
Round 1
In round 1, panelists were divided into two groups by the moderator aiming to achieve an even split of expertise. Both groups were asked to list potential learning objectives for adolescent pain science education. As stimulus, both groups were provided a reference list of pain science learning objectives previously developed for adultsCitation24,Citation25 and children (aged 8–12).Citation26 The moderator compiled all suggested learning objectives into one list.
Round 2
In round 2, the compiled list of proposed learning objectives was supplied to the two groups. The groups were asked to remove similar or duplicate learning objectives and those they deemed unnecessary. The moderator retrieved the two lists and noted discrepancies. A discussion around discrepancies was facilitated by the moderator, until consensus was achieved.
Round 3
In round 3, the list of potential learning objectives derived from round 2 were presented to all panelists. They were asked to anonymously select the top five learning objectives for relevance to adolescents using anonymous, electronic survey software (SurveyMonkey™). After each round the anonymous results were reported to the panelists, and they were given the opportunity to “rescue” the bottom two ranked objectives. If a rescue was attempted, it would trigger a group discussion and a revote. If no rescue was attempted, the bottom two ranked objectives were discarded until seven remained. We chose seven objectives on the basis of a large literature, particularly the work of Miller.Citation27 We concede that that work was based on short-term memory experiments, and that keeping to “the magical number seven” when it comes to learning objectives also reflects the collective opinion of panelists on a balance between coverage of the content and manageability of the curriculum.
Results
Panel
A total of 14 invitations were sent to potential participants. Twelve participants formed the panel, and all 12 participated in the entirety of the three-round modified-Delphi process. The characteristics of the participants are presented in . The mean age of the panelists was 38.3 years (± 12.4 years). Seven participants (58.3%) were female. Nine participants (75%) worked in Australia, two (16.7%) in the United States of America and one (8.3%) in Canada. The panel was constituted of experts from various health-related professions, including; physical therapists (50%), psychologists (25%), a medical doctor (8.3%), a nurse (8.3%) and an exercise physiologist (8.3%).
Table 2. Characteristics of the panel.
Results of Round 1
A flow chart outlining the modified-Delphi process is provided in . In round 1, two groups of six panelists were formed. Group 1 and Group 2 proposed 15 and 16 learning objectives respectively, resulting in a total of 31 candidate learning objectives for adolescent pain science education.
Results of Round 2
The same two groups of six panelists were retained for round 2. Following group discussions, Group 1 and Group 2 retained 7 and 10 learning objectives respectively. The moderator then facilitated a discussion with all panelists to reach consensus on discrepancies. The discrepancies included: (1) Group 2 split “pain is a protective output” into two learning objectives: “pain is a protector” and “the pain system can become overprotective”. Consensus was reached that these would remain 2 separate learning objectives. (2) Group 2 included “it is possible to live a normal life again” as an independent learning objective, whereas Group 1 removed this objective entirely. Agreement was reached to include this objective, but re-worded to “it is possible to improve/get better/you can do it”. (3) Group 2 had included “no-one else can decide whether or not you are in pain” as an independent learning objective, whereas Group 1 clustered this in a group titled “your pain is unique and real”. Agreement was reached to amalgamate the two objectives into one, reworded to “your pain is unique and real (valid) and no-one else can decide if you have it”. (4) The following objectives did not fall under another category and both groups agreed on removing these entirely: “your brain is not broken” and “pain is common”. At the conclusion of round 2, consensus was reached that 9 of the 31 original learning objectives were retained.
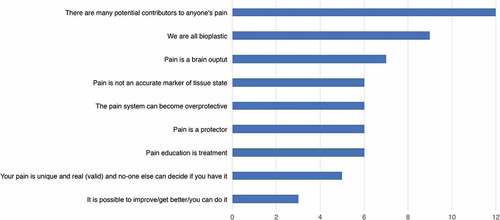
Results of Round 3
Panelists indicated the top five most relevant learning objectives for adolescents, from the nine identified in round 2 (see ). The highest ranked learning objective was “there are many potential contributors to anyone’s pain” indicated in the top 5 by all 12 participants (100%). The two lowest ranked objectives were “pain is unique and real (valid) and no-one can decide if you have it” (5 of 12; 42%) and “it is possible to improve/get better/you can do it” (3 of 12; 25%). A re-vote and discussion were triggered, resulting in the same two learning objectives being ranked lowest, and consequently discarded. At the conclusion of round 3 the following seven learning objectives were proposed: 1) Pain is a protector; 2) The pain system can become overprotective; 3) Pain is a brain output; 4) Pain is not an accurate marker of tissue state; 5) There are many potential contributors to anyone’s pain; 6) We are all bioplastic and; 7) Pain education is treatment. Further explanations of adolescent learning objectives are presented in . A comparison of adult and adolescent pain science learning objectives is presented in .
Table 3. Key learning objectives for adolescent pain science education resulting from a modified-Delphi style consensus.
Table 4. A comparison of adolescent and adult learning objectives for pain science education.
Discussion
Following a modified-Delphi process 12 panelists reached consensus on seven key learning objectives for adolescent pain science education: 1) Pain is a protector; 2) The pain system can become overprotective; 3) Pain is a brain output; 4) Pain is not an accurate marker of tissue state; 5) There are many potential contributors to anyone’s pain; 6) We are all bioplastic and; 7) Pain education is treatment. These learning objectives have the potential to form the basis of an education curriculum to improve an adolescent’s knowledge of pain.
It is noteworthy to consider that a large proportion of panelists (43%) ranked the learning objective “pain is unique and real (valid) and no-one else can decide if you have it” in their list of top five objectives. However, due to our a-priori aim of retaining only seven learning objectives, this item was not included in the final outcome. Some may consider this eighth learning objective clinically useful and we include it here for consideration of future endeavors in adolescent pain science education.
Comparison between Adult and Adolescent Learning Objectives
There are similarities between extant adult and new adolescent pain science learning objectives (see ). Both sets of objectives emphasize the involvement of the brain in pain perception, differentiate pain from tissue damage or injury, and outline that the pain system can adapt. However, there are also clear differences. The adult version outlines neurophysiological processes of pain persistence (e.g. descending modulation), for adolescents, the concept that “pain can become overprotective” is introduced instead. The adolescent concepts are also simplified compared to adult educational objectives. For example, while adult objectives refer to distributed brain activity, the adolescent objectives describe pain as a brain output, and state that “pain is a protector”. Instead of describing the influence of environmental or contextual factors as for adults, the adolescent objectives state “there are many potential contributors to anyone’s pain”. Finally, the adolescent objectives do not include language that refers to “pain messages” versus “danger messages”, such is seen in adult objectives.
It is important to keep in mind that the aim of the Delphi process was to identify the broad concepts, not precisely define the optimal wording. The language used to present these concepts to adolescents will likely need to be simplified and embedded in examples and contextual information. The differences between adult and adolescent learning objectives for pain science likely reflects the panelists views on what constitutes developmentally appropriate content for adolescence. Achieving language appropriate for adolescent development was outside the scope of the aim of this meeting, however addressing this will be a necessary next step.
Limitations
This study has limitations. First, the panel did not include adolescents with persistent pain or their families, because we were concerned about developing the curriculum and key scientific concepts. We consider it imperative that adolescents and their families be involved in progressing from this stage to the development of resources, clarification of messages, and identification of concepts they value and believe are important. As a next step, young people and their parents should be involved in the co-creation and testing of pain science education resources. Second, the panel included institutional representation from three countries, Australia, the United States and Canada. As such, the panelist’s reflections on learning objectives are likely to be influenced by the culture, ethnicity, and health care systems of these countries (although we note that some of the panelists had previously lived and grown up in other countries). It is possible that adolescents living in developing countries may require a different set of learning objectives. Third, this study did not differentiate developmental stages across adolescence. There may be benefit in tailoring pain science learning objectives to the different developmental stages (e.g. early, middle, late adolescence), rather than the entire period. Tailoring may be required according to an adolescent’s educational and literacy level. Future testing of these objectives could explore whether this is necessary.
Future Directions
Several pain science learning objectives have been recommended, but a curriculum is required to extend this work. Future research may consider developing the content of these learning objectives, exploring the necessity of education tailored to pain conditions, testing delivery methods, and evaluating credibility of information. It is possible that adolescents with persistent pain may benefit from increasing pain science literacy within their wider community, including parents, caregivers, siblings, healthcare providers, school personnel and peers. There is an outstanding need for a validated tool to measure pain science knowledge of adolescents, such as those that exist for adults,Citation15,Citation24 and are being developed for children (8– 12 years).Citation26 Finally, to determine what effect pain science education actually has on patient-relevant outcomes, trials should follow. Considering the difficulties undertaking randomized controlled trials in pediatric populations,Citation33 alternate designs may be considered such as single case experimental designs and multiple-baseline designs.
Conclusion
The interdisciplinary meeting on adolescent pain science education, held in Adelaide, Australia, gathered clinical and research professionals across pain education and pediatric pain to identify learning objectives for clinical application of pain science education to adolescents. We reached consensus on seven learning objectives to form the foundations of a pain science education curriculum: 1) Pain is a protector; 2) The pain system can become overprotective; 3) Pain is a brain output; 4) Pain is not an accurate marker of tissue state; 5) There are many potential contributors to anyone’s pain; 6) We are all bioplastic and; 7) Pain education is treatment.
Supplemental Material
Download MS Excel (10.6 KB)Acknowledgments
We acknowledge the help of Tracy Jones for organising the logistics of the meeting.
Disclosure statement
In the last 5 years, G. Lorimer Moseley has received support from: ConnectHealth UK, Seqirus, Kaiser Permanente, Workers’ Compensation Boards in Australia, Europe and North America, AIA Australia, the International Olympic Committee, Port Adelaide Football Club and Arsenal Football Club. Professional and scientific bodies have reimbursed him for travel costs related to presentation of research on pain at scientific conferences/symposia. He has received speaker fees for lectures on pain and rehabilitation. He receives book royalties from Noigroup publications, Dancing Giraffe Press & OPTP. David Moen receives royalties for a book on pain education and rehabilitation. No other authors report conflicts of interest.
Supplementary material
Supplemental data for this article can be accessed here.
Additional information
Funding
References
- Swain MS, Henschke N, Kamper SJ, Gobina I, Ottová-Jordan V, Maher CG. An international survey of pain in adolescents. BMC Public Health. 2014;14(1):447. doi:10.1186/1471-2458-14-447.
- Dissing KB, Hestbæk L, Hartvigsen J, Williams C, Kamper S, Boyle E, Wedderkopp N. Spinal pain in Danish school children–how often and how long? The CHAMPS study-DK. BMC Musculoskelet Disord. 2017;18(1):67. doi:10.1186/s12891-017-1424-5.
- King S, Chambers CT, Huguet A, MacNevin RC, McGrath PJ, Parker L, MacDonald AJ. The epidemiology of chronic pain in children and adolescents revisited: a systematic review. Pain. 2011;152(12):2729–38. doi:10.1016/j.pain.2011.07.016.
- Forgeron PA, King S, Stinson JN, McGrath PJ, MacDonald AJ, Chambers CT. Social functioning and peer relationships in children and adolescents with chronic pain: A systematic review. Pain Res Manag. 2010;15(1):27–41. doi:10.1155/2010/820407.
- Tham SW, Holley AL, Zhou C, Clarke GN, Palermo TM. Longitudinal course and risk factors for fatigue in adolescents: the mediating role of sleep disturbances. J Pediatr Psychol. 2013;38(10):1070–80. doi:10.1093/jpepsy/jst051.
- Rousseau-Salvador C, Amouroux R, Annequin D, Salvador A, Tourniaire B, Rusinek S. Anxiety, depression and school absenteeism in youth with chronic or episodic headache. Pain Res Manag. 2014;19(5):235–40. doi:10.1155/2014/541618.
- Eccleston C, Crombez G, Scotford A, Clinch J, Connell H. Adolescent chronic pain: patterns and predictors of emotional distress in adolescents with chronic pain and their parents. Pain. 2004;108(3):221–29. doi:10.1016/j.pain.2003.11.008.
- Mackner LM, Bickmeier RM, Crandall WV. Academic achievement, attendance, and school-related quality of life in pediatric inflammatory bowel disease. J Dev Behav Pediatr. 2012;33(2):106–11. doi:10.1097/DBP.0b013e318240cf68.
- Logan DE, Simons LE, Stein MJ, Chastain L. School impairment in adolescents with chronic pain. J Pain. 2008;9(5):407–16. doi:10.1016/j.jpain.2007.12.003.
- Palermo T, Eccleston C, Goldschneider K, Larkin MK, Sethan N, Turner H Assessment and management of children with chronic pain: A position statement from the American pain society. 2012 [ Accessed 2019 July 2]. http://americanpainsociety.org/uploads/get-involved/pediatric-chronic-pain-statement.pdf.
- Moseley GL, Butler DS. Fifteen years of explaining pain: the past, present, and future. J Pain. 2015;16(9):807–13. doi:10.1016/j.jpain.2015.05.005.
- Louw A, Zimney K, Puentedura EJ, Diener I. The efficacy of pain neuroscience education on musculoskeletal pain: a systematic review of the literature. Physiother Theory Pract. 2016;32(5):332–55. doi:10.1080/09593985.2016.1194646.
- Wood L, Hendrick PA. A systematic review and meta‐analysis of pain neuroscience education for chronic low back pain: short‐and long‐term outcomes of pain and disability. Eur J Pain. 2019;23(2):234–49. doi:10.1002/ejp.1314.
- Moseley GL. Combined physiotherapy and education is efficacious for chronic low back pain. Aust J Physiother. 2002;48(4):297–302. doi:10.1016/S0004-9514(14)60169-0.
- Moseley GL. Unravelling the barriers to reconceptualisation of the problem in chronic pain: the actual and perceived ability of patients and health professionals to understand the neurophysiology. J Pain. 2003;4(4):184–89. doi:10.1016/S1526-5900(03)00488-7.
- Wallwork SB, Bellan V, Catley MJ, Moseley GL. Neural representations and the cortical body matrix: implications for sports medicine and future directions. Br J Sports Med. 2015;50(16):990–96. doi:10.1136/bjsports-2015-095356.
- Apkarian AV. Nociception, pain, consciousness, and society: A plea for constrained use of pain-related terminologies. J Pain. 2018;19(11):1253–55. doi:10.1016/j.jpain.2018.05.010.
- Moseley GL, Vlaeyen JW. Beyond nociception: the imprecision hypothesis of chronic pain. Pain. 2015;156(1):35–38. doi:10.1016/j.pain.0000000000000014.
- Louw A, Podalak J, Zimney K, Schmidt S, Puentedura EJ. Can pain beliefs change in middle school students? A study of the effectiveness of pain neuroscience education. Physiother Theory Pract. 2018;34(7):542–50. doi:10.1080/09593985.2017.1423142.
- Wager J, Stahlschmidt L, Heuer F, Troche S, Zernikow B. The impact of a short educational movie on promoting chronic pain health literacy in school: A feasibility study. Eur J Pain. 2018;22(6):1142–50. doi:10.1002/ejp.1202.
- Andias R, Neto M, Silva AG. The effects of pain neuroscience education and exercise on pain, muscle endurance, catastrophizing and anxiety in adolescents with chronic idiopathic neck pain: a school-based pilot, randomized and controlled study. Physiother Theory Pract. 2018;34(9):682–91. doi:10.1080/09593985.2018.1423590.
- Jones J, Hunter D. Qualitative research: consensus methods for medical and health services research. BMJ. 1995;311(7001):376. doi:10.1136/bmj.311.7001.376.
- Hsu -C-C, Sandford BA. The Delphi technique: making sense of consensus. Pract. Assess., Res. Eval. 2007;12:1–8.
- Catley MJ, O’Connell NE, Moseley GL. How good is the neurophysiology of pain questionnaire? A rasch analysis of psychometric properties. J Pain. 2013;14(8):818–27. doi:10.1016/j.jpain.2013.02.008.
- Moseley GL, Butler DS. Explain pain supercharged. Adelaide (South Australia): Noigroup Publications; 2017.
- Pate JW, Hush JM, Hancock MJ, Moseley GL, Butler DS, Simons LE, Pacey V. A child’s concept of pain: an international survey of pediatric pain experts. Children (Basel). 2018;5(1):1–12.
- Miller GA. The magical number seven, plus or minus two: some limits on our capacity for processing information. Psychol Rev. 1956;63(2):81. doi:10.1037/h0043158.
- Neziri AY, Haesler S, Petersen-Felix S, Muller M, Arendt-Nielsen L, Manresa JB, Andersen OK, Curatolo M. Generalized expansion of nociceptive reflex receptive fields in chronic pain patients. Pain. 2010;151(3):798–805. doi:10.1016/j.pain.2010.09.017.
- Wall PD, McMahon SB. The relationship of perceived pain to afferent nerve impulses. Trends Neurosci. 1986;9:254–55. doi:10.1016/0166-2236(86)90070-6.
- Ringkamp M, Raja SN, Campbell JN, Meyer RA Peripheral mechanisms of cutaneous nociception. In: McMahon SB, Koltzenburg M, Tracey I, Turk D, editors. Wall and Melzack’s Textbook of Pain. Vol 6. Philadelphia, PA: Elselvier/Saunders; 2013.
- Wand BM, Tulloch VM, George PJ, Smith AJ, Goucke R, O’connell NE, Moseley GL. Seeing it helps: movement-related back pain is reduced by visualization of the back during movement. Clin J Pain. 2012;28(7):602–08. doi:10.1097/AJP.0b013e31823d480c.
- Moseley GL. Graded motor imagery is effective for long-standing complex regional pain syndrome: a randomised controlled trial. Pain. 2004;108(1–2):192–98. doi:10.1016/j.pain.2004.01.006.
- Caldwell PH, Murphy SB, Butow PN, Craig JC. Clinical trials in children. Lancet. 2004;364(9436):803–11. doi:10.1016/S0140-6736(04)16942-0.