ABSTRACT
Background
National strategies from North America call for substantive improvements in entry-level pain management education to help reduce the burden of chronic pain. Past work has generated a valuable set of interprofessional pain management competencies to guide the education of future health professionals. However, there has been very limited work that has explored the development of such competencies for individual professions in different regions. Developing profession-specific competencies tailored to the local context is a necessary first step to integrate them within local regulatory systems. Our group is working toward this goal within the context of entry-level physiotherapy (PT) programs across Canada.
Aims
This study aimed to create a consensus-based competency profile for pain management, specific to the Canadian PT context.
Methods
A modified Delphi design was used to achieve consensus across Canadian university-based and clinical pain educators.
Results
Representatives from 14 entry-level PT programs (93% of Canadian programs) and six clinical educators were recruited. After two rounds, a total of 15 competencies reached the predetermined endorsement threshold (75%). Most participants (85%) reported being “very satisfied” with the process.
Conclusions
This process achieved consensus on a novel pain management competency profile specific to the Canadian PT context. The resulting profile delineates the necessary abilities required by physiotherapists to manage pain upon entry to practice. Participants were very satisfied with the process. This study also contributes to the emerging literature on integrated research in pain management by profiling research methodology that can be used to inform related work in other health professions and regions.
RÉSUMÉ
Contexte: Contexte: Les stratégies nationales nord-américaines préconisent des améliorations sensibles à la formation de base en matiére de prise en charge de la douleur afin de contribuer à la réduction du fardeau de la douleur chronique. Des travaux antérieurs ont généré un ensemble de compétences interprofessionnelles utile en matiére de prise en charge de la douleur afin de guider la formation des futurs professionnels de la santé. Cependant, trés peu de travaux ont porté sur l'acquisition de telles compétences pour des professions individuelles dans différentes régions. L’uisition de compétences spécifiques à une profession adaptées au contexte local est une première étape nécessaire pour leur intégration dans les systèmes réglementaires locaux. Notre groupe travaille à cet objectif dans le cadre de programmes de formation de base en physiothèrapie partout au Canada.
Objectifs: Cette étude visait à créer un profil de compétences consensuel pour la prise en charge de la douleur, propre au contexte canadien de la physiothérapie.
Méthodes: Un devis Delphi modifié a étè utilisé pour parvenir à un consensus parmi des formateurs en milieu universitaire et clinique en matière de douleur en milieu universitaire et clinique.
Résultats: Des représentants de 14 programmes de formation de base en physiothérapie (93 % des programmes canadiens) et de six formateurs en milieu clinique ont été recrutés. Après deux tours, 15 compétences ont atteint le seuil d’approbation prédéterminé (75 %). La plupart des participants (85 %) ont déclaré être « très satisfaits »du processus.
Conclusions: Ce processus a permis de dégager un consensus sur un nouveau profil de compétences en matiére de prise en charge de la douleur propre au contexte canadien de la physiothérapie. Ce profil délimite les habiletés requises des physiothérapeutes pour prendre en charge la douleur en début de pratique. Les participants ont été très satisfaits du processus. Cette étude contribue également à la littérature émergente sur la recherche intégrée en matière de prise en charge de la douleur en définissant une méthodologie de recherche qui peut être utilisée pour éclairer des travaux similaires dans d’autres professions de la santé et dans d’autres régions.
Introduction
Chronic pain is a major health care issue associated with significant burden in terms of personal suffering and low quality of life for millions of North Americans.Citation1,Citation2 The lack of comprehensive pain management education across entry-level health care programs has been recognized as a major barrier to alleviating the burden of chronic pain.Citation2 Previous work has shown that there are widespread discrepancies in how health care providers are trained to manage pain, both within and across health care professions.Citation3–5 These inconsistencies likely contribute to health care providers feeling ill-prepared in caring for their patients suffering from pain,Citation6–8 as well as people living with pain feeling misunderstood by their health care providers.Citation8–11
National strategies from the United States and Canada emphasize the central importance of entry-level education to address the identified inconsistencies in pain management education.Citation1,Citation2 These national strategies call for the development of pain management competencies to guide the education of future health care professionals.Citation1,Citation2 The integration of key stakeholders in this process, such as people living with pain, health care students, and pain management educators, is essential to develop tailored tools that are relevant to the people who will be using them.Citation12–15 To date, there has been limited work on entry-level health care education about pain management that focuses on developing resources tailored to specific contexts (e.g., across different regions and/or professions) and that uses robust participatory research methods. For example, seminal work from Fishman and colleaguesCitation16 generated a valuable set of interprofessional pain management competencies; however, research is yet to explore the development of corresponding competencies for individual health care professions and include end users (e.g., people living with pain, educators, or students) in the creation process. Past work has highlighted the need for profession-specific competencies to match the unique attributes of each profession,Citation17,Citation18 as well as the importance of including stakeholders in the research process to increase relevance of the output and facilitate its uptake by end users.Citation13 In Canada, many health care professions are governed at the provincial level, with their own regulatory systems and priorities. Developing profession-specific competencies that are tailored to the local context is a necessary first step in further integrating pain management competencies within local regulatory systems.
Our group has recently started working toward the goal of establishing nationally accepted competencies for pain assessment and management within the context of entry-level physiotherapy (PT) programs across Canada.Citation18,Citation19 Physiotherapists (PTs) play an essential role in in the management of pain, through the use of biopsychosocial interventions to increase patient knowledge and self-management skills, to reduce pain and disability, as well as to empower individuals to manage and live well with pain.Citation20,Citation21 Work from our group has clearly highlighted the need for tailored competencies to guide the improvement of entry-level pain education for PTs across Canada.Citation18 The current lack of a national pain competency profile for PTs likely contributes to the major discrepancies observed in how pain management competencies are integrated across Canadian PT education programs.Citation19
The primary aim of this study was to achieve consensus across stakeholders on a new competency profile for pain management education, specific to the entry-level Canadian PT context.
Methods
Design
A modified Delphi design was used to achieve consensus across relevant stakeholders on a competency profile for pain management education in Canadian PT programs. The modified Delphi is an iterative process that uses a systematic progression of repeated rounds of voting to achieve agreement.Citation22–24 This approach strategically uses existing literature, perspectives of stakeholders and the judgment of experts within a field to reach consensus.Citation22,Citation25 Ethics approval for this study was granted by the McGill University Institutional Review Board.
Scope of the Competency Profile and Conceptual Framework
Throughout the generation and the consensus-building process, the scope of the profile was anchored by the definition of a competency as “an observable ability of a health professional, integrating multiple components such as knowledge, skills, and attitudes.”Citation26(p641) This profile aimed to offer a profile of PT-specific core competencies that delineate the necessary abilities required to manage pain upon entry to practice.Citation18 In addition to distinct competencies, key concepts (e.g., therapeutic alliance) were defined and included in the profile to facilitate their interpretation and application. The framing of these distinct competencies was explicitly intended to align with the highest level of Miller’s four-level pyramid of competency assessment (i.e., does). Miller’s pyramid is a framework for teaching and assessing clinical reasoning or competencies among health profession learners.Citation27,Citation28 It provides a four-level, hierarchical depiction of competencies and their assessment, moving from the lowest level of knows (acquisition of knowledge), to knows how (application of knowledge), to shows how (demonstration of competency), and, finally, to the highest level of does (performing the competency within a clinical setting).Citation28 The does level requires adequate mastery of the three lower levels (i.e., knows, knows how, and shows), making it an attractive level of competency for this profile.Citation27 Though all levels of the pyramid are important, we assumed that the lower levels can be subsequently detailed within more granular educational profiles or curriculum guidelines to facilitate curriculum development, once there is consensus on these higher-level competencies.
Creation of a Steering Group
The steering group supervised the entire Delphi process. This group was formed by integrating members of different stakeholder groups, which included two people living with pain (LC, LS), one recent PT graduate (NM), and six university-based pain educators from Canadian institutions (AH, DW, GB, JM, TW, YTL). In addition, two methodological experts (AB, AT) provided input on the Delphi and implementation processes of this study. Individuals were invited to join the steering group based on their relevant knowledge, expertise, and past engagement. All members of the steering group had equal involvement in the planning and decision making related to all aspects of this project.
Delphi Participants
Throughout this article, we used the term Delphi participants to refer to people who voted in the Delphi, which includes both university-based pain educators and clinical pain educators. Aligned with existing methodological recommendations, Delphi participants were recruited purposively.Citation29
Each of the 15 university PT programs in Canada has designated one or two representatives who lead the entry-level pain education at their local program; this national network of university-based pain educators is named the Pain Education in Physiotherapy Curriculum Initiative (PEPCI). Building on previous work,Citation18 we invited PEPCI members to participate in the study via e-mail. PEPCI members from the same university were asked to consult one another in order to submit one vote per institution.
Clinical educators were also recruited to acknowledge the role that clinical placements play in shaping pain management skills for PT students. A recruitment e-mail was circulated to members of the Canadian Physiotherapy Association Pain Science Division, recent graduates from McGill University (Montreal, Quebec), University of Alberta (Edmonton, Alberta), and Université de Sherbrooke (Sherbrooke, Quebec) certificate in chronic pain management programs, as well as clinical specialists in pain from the Canadian Physiotherapy Association. Clinical educators were eligible if they had a minimum of five years of clinical practice experience focused on pain management as well as completing one of the following: (1) a postlicensure certificate program in pain management offered by a Canadian university or equivalent continuing education training in pain management and/or (2) certified as a pain science clinical specialist by the Physiotherapy Specialty Certification Board of Canada. In addition, clinical educators had to be actively involved in clinical supervision of PT students.
To ensure diversity in the recruitment of participants, the steering group also agreed on the following minimum diversity inclusion criteria for composition of the voting group: (1) at least one participant who identified as a woman and at least one participant who identified as a man, (2) at least one native English speaker and one native French speaker (to represent Canada’s bilingual population), (3) at least one clinician from public practice and one clinician from private practice, and (4) at least one person who self-identifies as a person of color or as a member of Indigenous or First Nations community.
Modified Delphi Procedures
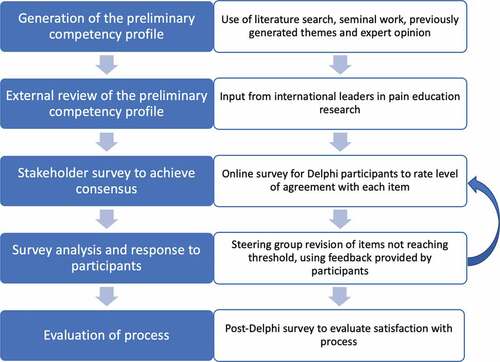
Anchored in the methodological recommendations for modified Delphi studies,Citation23,Citation25 the following steps were completed: (1) generation of the preliminary competency profile, (2) external review of the preliminary competency profile, (3) stakeholder survey to achieve consensus, (4) survey analysis and response to participants, and (5) evaluation of process. An overview of the entire process is presented in .
Figure 1. Overview of modified Delphi process. This figure provides an overview of the different steps involved in our modified Delphi process.
Step 1: Generation of the Preliminary Competency Profile
The steering group developed the preliminary version of the competency profile, based on themes from a recent national workshop that used a nominal group technique to ask key Canadian stakeholders in pain management what PTs should be able to do upon completing entry-level education. These stakeholders included pain educators, people living with pain, and recent PT graduates. In addition, a literature search and seminal work in the field were used to generate this preliminary version.Citation16,Citation30,Citation31 Throughout this initial process, the steering group ensured that all competencies were aligned with the scope of the profile, while maintaining clarity and limiting redundancy.
Step 2: External Review of the Preliminary Competency Profile
A group of international leaders in research on pain education (n = 5) reviewed the preliminary version of the competency profile to ensure that the content and scope of the items were consistent with existing international recommendations and the broader literature on competencies.Citation16,Citation30,Citation31 This expert consulting group included members of the task force that developed the International Association for the Study of Pain (IASP) Inter-professional Core Competencies in Pain Management, the task force that developed the IASP PT Pain Education Curriculum Guidelines, and a PT faculty that systematically implemented the IASP PT Pain Education Curriculum Guidelines within their entry-level education program.
Step 3: Stakeholder Survey to Achieve Consensus
Interested Delphi participants were invited to attend an online orientation meeting detailing the processes involved in the Delphi, such as the voting scheme and the expected timeline. They were provided with background information regarding the rationale and the research supporting the development of the competency profile prior to completing the Delphi survey. Any questions were answered at that time and participants were encouraged to seek clarification via e-mail if needed. At the start of each round, participants were e-mailed a link to the online Delphi survey and provided consent before voting. Data were collected between July and September 2020 using SurveyMonkey (San Mateo, CA).
Voting Process
Delphi participants were asked to anonymously rate their level of agreement with each competency according to the following scale: (1) favorable to its inclusion in the competency profile (green light), (2) favorable to the inclusion of a revised version (yellow light), or (3) favorable to removing it from the competency profile (red light). In addition, participants were asked to rate their level of agreement with the definition of key concepts related to the competencies (e.g., social justice or therapeutic alliance) using the same scale. They were also invited to provide a rationale for their response and suggest potential improvements for each item (i.e., competencies or definitions) using an open-text box. Aligned with Delphi methodology best practices, the threshold for consensus was defined a priori at ≥75% agreement across all participants to retain or exclude an item.Citation29,Citation32 We expected this study to require two to four rounds to reach consensus on all competencies.
Step 4: Survey Analysis and Response to Participants
Following each round, the level of participant agreement for each item was summarized using frequency counts. Participants’ open-text responses for items not reaching consensus were summarized and used to inform the revision of the competency profile within each round. The steering group had access to the summary of feedback, as well as the anonymized comments, to enhance rigor and credibility. The steering group updated the competencies that did not reach consensus, based on the feedback provided. Participants were provided with an overview of the votes (i.e., the frequency of green light, yellow light, and red light votes for each item), as well as a summary of the feedback received alongside the new version (revised iteration) of the items not reaching consensus. Modification of an item was clearly highlighted within the survey and both versions of the item were included to allow for comparison. Steps 3 and 4 were repeated iteratively until all items reached consensus for inclusion or exclusion, following which a summary of the changes was circulated alongside the finalized competency profile.
Step 5: Evaluation of Process
Participants were asked to complete an anonymous post-Delphi survey to evaluate satisfaction with the overall process using a seven-point scale (ranging from very unsatisfied to very satisfied). In addition, the survey assessed participants’ interest in using a similar Delphi process when making future consensus decisions related to this topic. Feedback from participants regarding potential improvements was sought using open-text comments.
Results
Delphi Participation
A total of 20 participants were recruited, including representatives from 14 Canadian PT universities (14/15; 93% of all Canadian entry-level PT programs) and six clinical educators; predefined diversity criteria were met (). One university representative was unable to participate in this study, being on leave during the period of data collection. Nonetheless, the number of participants was within the typical range for Delphi studies.Citation23,Citation29 All participants completed the two rounds for item evaluation and answered the evaluation survey to provide feedback on the process (response rate: 100%).
Table 1. Summary of recruited clinical educators
Competency Profile
The Delphi process resulted in the generation and stakeholder endorsement of the Pain Education in Physiotherapy (PEP) competency profile, which consists of 15 competencies that delineate the necessary abilities required to manage pain upon entry to practice (). The steering group initially generated a preliminary version of the competency profile, which consisted of 15 competencies and 17 key concept definitions. Throughout the external review and the Delphi evaluation process, 5 new key concept definitions were added to the profile and existing items were revised to enhance clarity, ensure the use of adequate terminology (e.g., developing a diagnosis), and update item phrasing to better align it with the profile values (e.g., using “assessment with the person” rather than “assessment of the person” to further demonstrate person-centeredness). By the end of the second round of the Delphi process, all 15 competencies and 23 key concept definitions reached the required consensus threshold (75%). Most competencies (12/15, 80%) reached a high level of endorsement (85% and above). A breakdown of the final agreement rate for each competency and the number of rounds required for reaching consensus is provided in .
Table 2. Final version of the PEP competency profile (bolded words are defined in the glossary)
Table 3. Summary of final agreement rate (green light vote) for each competency
The competencies can be divided into two different domains (), which emerged iteratively during the generation of the preliminary profile. The first domain is composed of eight competencies that address specific aspects of pain management, such as performing a comprehensive assessment, using appropriate tools and strategies to monitor progress, or collaborating with relevant professionals. The second domain consists of seven competencies that permeate all aspects of pain management, such as promoting autonomy, using an ethical approach to care, or demonstrating active listening and empathy.
Post-Delphi Evaluation
All 20 participants completed the post-Delphi questionnaire. The findings suggest a high level of satisfaction with the Delphi process, with nearly all respondents feeling very satisfied (n = 17, 85%) or satisfied (n = 2, 10%) with it. Only one respondent reported being partially satisfied with the process. All respondents (n = 20) mentioned they would be interested in using a similar Delphi process when making future consensus decisions related to this project. Responses to the open-ended questions were consistent with this high level of satisfaction and endorsement. Several participants stated that the Delphi process was clearly outlined and easy to follow. Potential improvements suggested by participants include discussing some of the modifications with other participants through focus groups. The clarity of the results and the justification provided when adapting an item led participants to report feeling included throughout the process. Comments regarding the final competency profile were encouraging, although it was highlighted that some competencies lacked the sufficient granularity to inform specific teaching and learning strategies, due to the high-level scope of the profile.
Discussion
This study provides a novel contribution to the literature on pain management education. The purpose of this study was to generate and gain stakeholder consensus on a pain management competency profile that is specific to the Canadian PT context. By doing so, this work aimed to address the identified need to develop core competencies in pain management that are specific to a region (i.e., Canada) and a profession (i.e., PT) and that could be used to inform entry-level curriculum design and assessment.
One of the novel aspects of the PEP competency profile lies in the use of robust and transparent consensus-building methods to guide the development of this competency profile. The concept of integrated knowledge translation research also informed some of the methodological choices, such as the inclusion of key stakeholders in the research process.Citation47 Integrated knowledge translation research calls for involvement of end users in the creation of new knowledge and provides a strong foundation to support the resulting competency profile.Citation47,Citation48 More specifically, collaborating with people living with pain as active members of the steering group is likely to have contributed to the person-centeredness of the PEP competency profile by building on their lived experiences of pain and key aspects of care that often remain unaddressed.Citation9–11,Citation49 In addition, engaging clinical pain educators in the voting process helped ensure that the competencies were directly relevant to real-life settings in addition to their academic pertinence. The contribution of key stakeholders actively involved in the topic through their lived experiences of pain and their practical experience in providing pain management may have led to the emergence of competencies dedicated to interpersonal skills (e.g., using adequate communication strategies or promoting autonomy) that related to all aspects of pain management. Including people living with pain in the steering group is an important and novel improvement on previous work. However, including a sample of people living with pain as part of the external review process would have permitted the integration of a broader range of perspectives (e.g., via national advocacy groups) and enabled members of this stakeholder group to serve as external evaluators. Future work related to consensus-building processes in pain should consider this additional level of involvement of people living with pain.
An interesting characteristic of the PEP competency profile was the emergence of two competency domains during the generation of the preliminary profile (). The first domain delineates competencies that address specific aspects of pain management, such as performing a comprehensive pain assessment or facilitating appropriate transitions in care for the person living with pain. The second domain includes competencies relevant to more global aspects of pain management, such as using a person-centered approach and tailored communication strategies. Each competency in the second domain is intended to be relevant to the demonstration of competencies in the first domain (e.g., using a person-centered approach and tailored communication strategies while completing a comprehensive pain assessment). The second domain may be broad, but we believe it brings in a novel piece that our stakeholders felt was not addressed in previous work. Though the ideas captured by this domain are likely applicable to all approaches of care and may overlap with the existing Canadian physiotherapy competency profile,Citation30 they are of particular importance in the context of pain management. Having a domain dedicated to competencies relevant to all aspects of pain management is valuable to facilitate the in-depth development of these skills, while limiting redundancy by not repeating each of the interpersonal aspects of care that are vital to each of the specific aspects of pain management. It is also useful to facilitate both teaching and evaluation strategies by emphasizing what common aspects of care can be taught and assessed in relation to specific aspects of pain management.
The final version of the PEP competency profile bears some resemblance with previous work in the field, such as the IASP curriculum guidelinesCitation31 and the European Pain Federation core curriculum.Citation50 These guidelines describe curriculum content related to pain management but do not answer the identified need for high-level competencies that delineate the required abilities to apply such content successfully and provide adequate pain management upon entry to practice. Our work is also similar to the competency profile generated by Fishman and colleagues, which has a strong interprofessional focus.Citation16 Both competency profiles advocate for using a multidimensional and person-centered approach to pain management, while considering the various contextual factors likely to influence access to and provision of care. In addition, they emphasize the importance of using adequate tools and strategies in pain management, as well as including communication competencies such as expressing compassion and empathy. However, the PEP competency profile further extends the work from Fishman and colleaguesCitation16 as a discipline-specific resource but also by expanding the breadth and depth of the competencies included. For example, Fishman’s competency related to empathic and compassionate communication is anchored in the assessment of pain (domain 2, competency 4), whereas the PEP competency profile frames these elements in relation to all aspects of care (competencies 11 and 15). Similarly, the notion of advocacy is anchored in the treatment process in Fishman’s profile (domain 4, competency 5), whereas we included different contexts for advocacy, such as at the level of the family, care providers, or institution (competency 8), without anchoring them in a specific aspect of care. Though it could be argued that these differences are the results of having a different focus (i.e., interprofessional versus PT specific), the unique structure of the PEP competency profile plays an important role in this increased depth. More specifically, it differentiates between competencies addressing specific aspects of pain management (first domain) and competencies relevant to all aspects of pain management (second domain). This allows competencies such as promoting autonomy to be explicitly linked to all specific aspects of pain management without excessive repetitions. To our knowledge, this is the first time that a competency profile in pain management includes a stand-alone domain focused on overarching competencies. This is particularly relevant because the lack of these competencies (e.g., adequate communication, demonstrating empathy, or using a person-centered approach to care) has been linked with impaired therapeutic alliance and increased stigma for people living with pain.Citation9,Citation11,Citation49 Having these competencies clearly identified in the PEP competency profile holds the potential to help address them better and improve their application to clinical practice.
Another strength of the PEP competency profile is its alignment with how the broader literature defines competencies.Citation26,Citation27 This is the result of the input from educational experts, because they helped to ensure that the preliminary version of the PEP competency profile was consistent with the existing literature on competencies. In addition, the scope of the competency profile was made explicit to Delphi participants from the beginning, because the orientation session provided them with the definition of a competency as “an observable ability of a health professional, integrating multiple components such as knowledge, skills, and attitudes”Citation26(p641) and clarified how the competencies would be anchored in this definition. Throughout the Delphi process, the steering group ensured that framing of the competencies was explicitly aligned with the highest level of Miller’s four-level pyramid of competency assessment (i.e., does). As a result, the final competencies are all located at the does level of Miller’s pyramid, which describes the situation where the learner has acquired the desired skill and performs it appropriately in clinical practice.Citation28 We expect that the PEP competency profile could be used to inform curriculum guidelines and detail the competencies located at lower levels. This choice allowed us to omit competencies from these lower levels of Miller’s pyramid, as compared to the work from Fishman and colleagues,Citation16 which included content located on different levels. For example, the competencies of the first domain from Fishman and colleagues’ profile detail what the learner should know rather than the practical application of the desired knowledge, skills, and attitudes in clinical settings.
It should be acknowledged that due to our focus on the does level, some stakeholders have reported wanting more granularity to inform the practical applications of the PEP competency profile, such as detailing content (e.g., best practice recommendations), as well as teaching and learning strategies. This feedback is important and highlights the need for subsequent work around the practical implementation of the PEP competency profile. An important next step would therefore be to expand the PEP competency profile through developing curriculum guidelines, entrustable professional activities, and assessment strategies. We also acknowledge that important barriers to implementing these competencies are still possible, both at a local program level and at a national regulatory level, which might impede uptake of the PEP competency profile. Future work with relevant stakeholders (e.g., PT program directors, university-based pain educators, or national regulators) is needed to unpack the barriers and facilitators related to uptake of our competency profile. It is also important to point out that the protocol for this study was not registered prior to its implementation. Though this is not standard practice for Delphi methodology, or for other consensus-building methods that are unrelated to hypothesis testing,Citation22–25 preregistration would help further improve transparency.
Conclusion
A national Delphi process that delineates the necessary competencies required to manage pain upon entry to practice was used to achieve consensus on a novel competency profile specific to the Canadian PT context. The steering group members and the review provided by the international leaders in research on pain education helped create a preliminary version of the profile, which was subsequently refined and endorsed by Delphi participants, which consisted of university-based (n = 14) and clinical (n = 6) pain educators. The final version of the PEP competency profile includes 15 competencies, which can be divided into two interdependent domains. The first domain focuses on specific aspects of pain management, whereas the second domain details competencies relevant to all aspects of pain management. Building on this profile, future research will need to detail the content relevant to each competency, develop curriculum guidelines for pain education in Canada, and understand potential barriers to implementation. The consensus-building and participatory research methods used in this study provide a practical example of the processes involved in the creation and approval of a competency profile and may be useful to inform future interventions to improve pain education across health care professions and geographic regions.
Informed Consent Statement
This study was approved by the IRB of the Faculty of Medicine and Health Sciences at McGill University (approval number: A11-E78-19A). All participants provided informed written consent to participate in this project prior to the start of this study.
Disclosure Statement
The nature of participatory research is that stakeholders are participants and are expected to have investments in the area researched; this investment is part of the research process. Consistent with this approach to research, the majority of the authors are university lecturers or professors focusing on pain education and receive a salary for this work. In addition, the following authors report financial compensation and/or royalties related to their work in pain education outside of their academic positions: DW, YTL, LS, MHB, RF, NP, and TW.
Additional information
Funding
References
- Canadian Pain Task Force. Chronic pain in Canada: laying a foundation for action. Government of Canada; 2019. https://www.canada.ca/en/health-canada/corporate/about-health-canada/public-engagement/external-advisory-bodies/canadian-pain-task-force/report-2019.html.
- The National Institutes of Health. National pain strategy - a comprehensive population health-level strategy for pain. The National Institutes of Health; 2016.
- National Academies of Sciences. The national academies collection: reports funded by national institutes of health. In: Stroud C, Posey Norris SM, Bain L, editors. The role of nonpharmacological approaches to pain management: proceedings of a workshop. Washington (DC): National Academies Press (US).
- Watt-Watson J, McGillion M, Hunter J, Choiniere M, Clark AJ, Dewar A, Johnston C, Lynch M, Morley-Forster P, Moulin D, et al. A survey of prelicensure pain curricula in health science faculties in Canadian universities. Pain Res Manage. 2009;14(6):439–44. doi:10.1155/2009/307932.
- Thompson K, Johnson MI, Milligan J, Briggs M. Twenty-five years of pain education research-what have we learned? Findings from a comprehensive scoping review of research into pre-registration pain education for health professionals. Pain. 2018;159(11):2146–58. doi:10.1097/j.pain.0000000000001352.
- Synnott A, O’Keeffe M, Bunzli S, Dankaerts W, O’Sullivan P, O’Sullivan K. Physiotherapists may stigmatise or feel unprepared to treat people with low back pain and psychosocial factors that influence recovery: a systematic review. J Physiother. 2015;61(2):68–76. doi:10.1016/j.jphys.2015.02.016.
- Alexanders J, Anderson A, Henderson S. Musculoskeletal physiotherapists’ use of psychological interventions: a systematic review of therapists’ perceptions and practice. Physiotherapy. 2015;101(2):95–102. doi:10.1016/j.physio.2014.03.008.
- Toye F, Seers K, Hannink E, Barker K. A mega-ethnography of eleven qualitative evidence syntheses exploring the experience of living with chronic non-malignant pain. BMC Med Res Methodol. 2017;17(1):116. doi:10.1186/s12874-017-0392-7.
- De Ruddere L, Craig KD. Understanding stigma and chronic pain: a-state-of-the-art review. Pain. 2016;157(8):1607–10. doi:10.1097/j.pain.0000000000000512.
- Wideman TH, Edwards RR, Walton DM, Martel MO, Hudon A, Seminowicz DA. The multimodal assessment model of pain: a novel framework for further integrating the subjective pain experience within research and practice. Clin J Pain. 2019;35(3):212–21. doi:10.1097/AJP.0000000000000670.
- Cohen M, Quintner J, Buchanan D, Nielsen M, Guy L. Stigmatization of patients with chronic pain: the extinction of empathy. Pain Med. 2011;12(11):1637–43. doi:10.1111/j.1526-4637.2011.01264.x.
- Birnie KA, Dib K, Ouellette C, Dib MA, Nelson K, Pahtayken D, Baerg K, Chorney J, Forgeron P, Lamontagne C, et al. Partnering for pain: a priority setting partnership to identify patient-oriented research priorities for pediatric chronic pain in Canada. CMAJ Open. 2019;7(4):E654–e64. doi:10.9778/cmajo.20190060.
- Forsythe LP, Carman KL, Szydlowski V, Fayish L, Davidson L, Hickam DH, Hall C, Bhat G, Neu D, Stewart L, et al. Patient engagement in research: early findings from the patient-centered outcomes research institute. Health Aff (Millwood). 2019;38(3):359–67. doi:10.1377/hlthaff.2018.05067.
- Fitzcharles M-A, Brachaniec M, Cooper L, Dubin R, Flynn T, Gerhold K, Häuser W, Cowan K, Laupacis A, Marleau R, et al. A paradigm change to inform fibromyalgia research priorities by engaging patients and health care professionals. Can J Pain. 2017;1(1):137–47. doi:10.1080/24740527.2017.1374820.
- Poulin P, Shergill Y, Romanow H, Busse JW, Chambers CT, Cooper L, Forgeron PA, Olsen Harper A, Hudspith M, Iorio A, et al. Researching what matters to improve chronic pain care in Canada: a priority-setting partnership process to support patient-oriented research. Can J Pain. 2018;2(1):191–204. doi:10.1080/24740527.2018.1433959.
- Fishman SM, Young HM, Arwood LE, Chou R, Herr K, Murinson BB, Watt-Watson J, Carr DB, Gordon DB, Stevens BJ, et al. Core competencies for pain management: results of an interprofessional consensus summit. Pain Med. 2013;14(7):971–81. doi:10.1111/pme.12107.
- van Lankveld W, Afram B, Staal JB, van der Sande R. The IASP pain curriculum for undergraduate allied health professionals: educators defining competence level using Dublin descriptors. BMC Med Educ. 2020;20(1):60. doi:10.1186/s12909-020-1978-z.
- Wideman TH, Miller J, Bostick G, Thomas A, Bussières A. Advancing pain education in Canadian physiotherapy programmes: results of a consensus-generating workshop. Physiother Canada Physiothérapie Canada. 2018;70(1):24–33. doi:10.3138/ptc.2016-57.
- Wideman TH, Miller J, Bostick G, Thomas A, Bussieres A, Wickens RH. The current state of pain education within Canadian physiotherapy programs: a national survey of pain educators. Disabil Rehabil. 2019;42(9):1–7.
- Moseley GL, Butler DS. Fifteen years of explaining pain: the past, present, and future. J Pain. 2015;16(9):807–13. doi:10.1016/j.jpain.2015.05.005.
- Thacker L, Walsh RM, Song SG, Khan HA, Parmar P, Vance KT, Grant G, Mesaroli G, Hunter J, Vader K, et al. Exploring physiotherapy practice within hospital-based interprofessional chronic pain clinics in Ontario. Can J Pain. 2021;5(1):96–106. doi:10.1080/24740527.2021.1905508.
- Hasson F, Keeney S, McKenna H. Research guidelines for the Delphi survey technique. J Adv Nurs. 2000;32:1008–15.
- Boulkedid R, Abdoul H, Loustau M, Sibony O, Alberti C. Using and reporting the Delphi method for selecting healthcare quality indicators: a systematic review. PLoS One. 2011;6(6):e20476. doi:10.1371/journal.pone.0020476.
- Hauer KE, Cate OT, Boscardin CK, Iobst W, Holmboe ES, Chesluk B, Baron RB, O’Sullivan PS. Ensuring resident competence: a narrative review of the literature on group decision making to inform the work of clinical competency committees. J Grad Med Educ. 2016;8(2):156–64. doi:10.4300/JGME-D-15-00144.1.
- Humphrey-Murto S, Varpio L, Wood TJ, Gonsalves C, Ufholz L-A, Mascioli K, Wang C, Foth T. The use of the delphi and other consensus group methods in medical education research: a review. Acad Med. 2017;92(10):1491–98. doi:10.1097/ACM.0000000000001812.
- Frank JR, Snell LS, Cate OT, Holmboe ES, Carraccio C, Swing SR, Harris P, Glasgow NJ, Campbell C, Dath D, et al. Competency-based medical education: theory to practice. Med Teach. 2010;32(8):638–45. doi:10.3109/0142159X.2010.501190.
- Ten CO, Carraccio C, Damodaran A, Gofton W, Hamstra SJ, Hart DE, Richardson D, Ross S, Schultz K, Warm EJ, et al. Entrustment decision making: extending Miller’s pyramid. Acad Med. 2021;96(2):199–204. doi:10.1097/ACM.0000000000003800.
- Miller G. The assessment of clinical skills/competence/performance. Acad Med. 1990;65(9):A63–S7. doi:10.1097/00001888-199009000-00045.
- Taylor E. We agree, don’t we? The Delphi method for health environments research. Herd. 2020;13(1):11–23. doi:10.1177/1937586719887709.
- NPAG. National Physiotherapy Advisory Group. Competency profile for physiotherapists in Canada. Physiotherapy Education Accreditation Canada; 2017. https://www.peac-aepc.ca/pdfs/Resources/Competency%20Profiles/Competency%20Profile%20for%20PTs%202017%20EN.pdf.
- International Association for the Study of Pain. Curriculum outline on pain for physical therapy. 2018. [ accessed 2018 Mar 29]. https://www.iasp-pain.org/Education/CurriculaList.aspx.
- Diamond IR, Grant RC, Feldman BM, Pencharz PB, Ling SC, Moore AM, Wales PW. Defining consensus: a systematic review recommends methodologic criteria for reporting of Delphi studies. J Clin Epidemiol. 2014;67(4):401–09. doi:10.1016/j.jclinepi.2013.12.002.
- Knights S. Reflection and learning: the importance of a listener. In: Boud D, Keogh R, Walker D, editors. Reflection: turning experience into learning. New York, NY: Nichols Publishing Company. 1985;85–90.
- Beauchamp T. Principlism in bioethics. In: editors, Bermúdez P, Seoane J. Bioethical decision making and argumentation. 1st ed. Springer International Publishing . 2016;1–16.
- Foster NE, Hill JC, O’Sullivan P, Hancock M. Stratified models of care. Best Pract Res Clin Rheumatol. 2013;27(5):649–61. doi:10.1016/j.berh.2013.10.005.
- Setchell J, Dalziel B. Using critical reflexivity to enhance clinical care: a clinician perspective. J Humanities in Rehabil. 2019. https://www.jhrehab.org/2019/04/15/using-critical-reflexivity-to-enhance-clinical-care-a-clinician-perspective/.
- First Nation Health Authority. Cultural humility. 2020. https://www.fnha.ca/wellness/cultural-humility.
- Mercer SW, Reynolds WJ. Empathy and quality of care. The British Journal of General Practice: The Journal of the Royal College of General Practitioners. 2002;52 Suppl:S9–12.
- World Health Organization. Health equity: world health organization. 2020. https://www.who.int/topics/health_equity/en/.
- Canadian Physiotherapy Association. Code of ethical conduct. 2020. https://physiotherapy.ca/sites/default/files/code-of-conduct-en.pdf.
- Maclachlan M, Khasnabis C, Mannan H. Inclusive health. Trop Med Int Health. 2012;17(1):139–41. doi:10.1111/j.1365-3156.2011.02876.x.
- Oxford Reference. Lived experience. 2020. https://www.oxfordreference.com/view/10.1093/oi/authority.20110803100109997.
- Okun S, Schoenbaum S, Andrews D, Chiambaran P, Chollette V, Grumman J, Leal S, Lown B, Mitchell P, Parry C, et al. Patients and health care teams forging effective partnerships. NAM Perspect. 2014;4(12). doi:10.31478/201412f.
- Dukhanin V, Searle A, Zwerling A, Dowdy DW, Taylor HA, Merritt MW. Integrating social justice concerns into economic evaluation for healthcare and public health: a systematic review. Soc Sci Med. 2018;198:27–35. doi:10.1016/j.socscimed.2017.12.012.
- Kinney M, Seider J, Beaty AF, Coughlin K, Dyal M, Clewley D. The impact of therapeutic alliance in physical therapy for chronic musculoskeletal pain: a systematic review of the literature. Physiother Theory Pract. 2020;36(8):886–98. doi:10.1080/09593985.2018.1516015.
- Barlow J, Wright C, Sheasby J, Turner A, Hainsworth J. Self-management approaches for people with chronic conditions: a review. Patient Educ Couns. 2002;48(2):177–87. doi:10.1016/S0738-3991(02)00032-0.
- Jull J, Giles A, Graham ID. Community-based participatory research and integrated knowledge translation: advancing the co-creation of knowledge. Implementation Sci. 2017;12(1):150. doi:10.1186/s13012-017-0696-3.
- Gagliardi AR, Berta W, Kothari A, Boyko J, Urquhart R. Integrated knowledge translation (IKT) in health care: a scoping review. Implementation Sci. 2016;11(1):38. doi:10.1186/s13012-016-0399-1.
- Slade SC, Molloy E, Keating JL. Stigma experienced by people with nonspecific chronic low back pain: a qualitative study. Pain Med. 2009;10(1):143–54. doi:10.1111/j.1526-4637.2008.00540.x.
- European Pain Federation. Core curriculum for European diploma in pain physiotherapy. 2017. https://europeanpainfederation.org/wp-content/uploads/2018/10/EFIC-Pain-Physiotherapy-Curriculum1.pdf.
