Abstract
RATIONALE
Lung cancer (LC) diagnostic pathways are often initiated following suspicious clinical and radiologic findings. We identified delays from first thoracic imaging suspicious for LC to specialist evaluation in a rapid assessment clinic [Lung Diagnostic Assessment Program (LDAP)].
OBJECTIVES
We evaluate the impact of a quality improvement initiative consisting of standardized Computed Tomography (CT) reporting on timeliness of LC diagnostic pathways.
METHODS
Retrospective chart review of LDAP-referred patients established baseline data (January – December 2018). Improvement initiatives included (i) implementation of standardized LDAP referral recommendations at an academic center for patients with suspected LC by thoracic imaging (January 2019), and (ii) spread of standardized reporting to 3 community hospitals (March 2019). Prospective chart review (January - September 2019) evaluated for improvement. Data include dates of CT chest, LDAP referral/assessment and specific phrasing of radiology reports. Continuous data are reported as medians, categorical data as percentages; Mann-Whitney U and chi-squared tests assess for significance.
MEASUREMENTS AND MAIN RESULTS
We reviewed 1,244 LDAP referrals (697 baseline; 547 post-standardization). Patients with a radiologist recommendation for LDAP referral had faster times from CT to referral (median [75th, 90th percentile]) (5[9,15] vs. 6[16,33] days) and specialist assessment (20[27,35] vs. 22[33,50] days). Following standardization, the percentage of LDAP-referred patients with a radiologist recommendation for referral increased (29.2% to 48.3%; P < .001), significant for the academic center (50.2% to 61.8%; P = .006) and community hospitals (12.1% to 35.3%; P < .001).
CONCLUSIONS
Standardized radiologist reporting and specialist referral recommendations for patients with imaging suspicious for LC leads to faster patient referral and assessment.
RÉSUMÉ
JUSTIFICATION
Les voies diagnostiques du cancer du poumon sont souvent initiées à la suite de résultats cliniques et radiologiques suspects. Nous avons repéré des délais entre la première imagerie thoracique suspecte de cancer du poumon et l’évaluation par un spécialiste dans une clinique d’évaluation rapide [Programme d’évaluation diagnostique pulmonaire (PEDP)].
OBJECTIFS
Nous évaluons l’impact d’une initiative d’amélioration de la qualité consistant en des rapports normalisés de tomodensitométrie (TDM) sur la rapidité des voies diagnostiques du cancer du poumon.
MÈTHODES
L’examen rétrospectif des dossiers des patients référés au PEDP a permis d’établir les données de base (janvier - décembre 2018). Les initiatives d’amélioration comprenaient (i) la mise en oeuvre de recommandations de référence a normalisées au PEDP dans un centre universitaire pour les patients suspectés de cancer du poumon par imagerie thoracique (janvier 2019) et (ii) la diffusion de rapports normalisés dans trois hôpitaux communautaires (mars 2019). L’examen prospectif des dossiers (janvier - septembre 2019) évalué en vue d’une amélioration. Les données incluent les dates de TDM thoracique, de la référence/évaluation par le PEDP et la formulation précise des rapports de radiologie. Les données continues sont rapportées sous forme de médianes, les données catégorielles sous forme de pourcentages; les tests Mann-Whitney U et chi-carré évaluent la significativité.
MESURES ET PRINCIPAUX RÈSULTATS
Nous avons examiné 1244 références au PEDP (697 références; 547 après normalisation). Les patients avec une recommandation du radiologue pour une référence au PEDP avaient des délais plus rapides entre la TDM et la référence (médiane [75e, 90e centile]) (5[9,15] comparativement à 6[16,33] jours) et évaluation spécialisée (20[27,35] comparativement à 22[33,50] jours). Suite à la normalisation, le pourcentage de patients référés au PEDP avec une recommandation d’un radiologue a augmenté (29,2 % à 48,3 %; P < 0.001), et était significatif pour le centre académique (50,2% à 61,8%; P = 0,006) et les hôpitaux communautaires (12,1 % à 35,3 %; P < 0,001).
CONCLUSIONS:
Les rapports de radiologues normalisés et les recommandations de référence vers un spécialiste normalisées pour les patients dont l’imagerie est suspecte de cancer du poumon permettent une référence et une évaluation plus rapides des patients.
Introduction
Lung cancer (LC) is the leading cause of cancer-related mortality in North America with most patients diagnosed at an advanced stage.Citation1 Delays in LC care can exist at all points between onset of symptoms to initiation of treatment and are associated with disease progression.Citation2–10 Diagnostic pathways are often initiated following suspicious imaging findings, though coordination of care in this phase is prone to delays due to transitions of care.Citation11,Citation12 Minimizing delays in LC diagnostic pathways may lead to initiation of treatment at an earlier stage, thereby improving outcomes. Timely LC care is important independent of effects on survival, as diagnostic and treatment delays are associated with increased patient distress.Citation13 Radiology has an important role to play in LC diagnostic pathways and significant benefits can be achieved by standardizing communications between radiologists and referring physicians.Citation14–17
In Southeastern (SE) Ontario, we identified delays from first thoracic imaging suspicious for LC to specialist referral in a rapid assessment clinic (Lung Diagnostic Assessment Program [LDAP]). We also identified marked heterogeneity in radiologist recommendations for evaluation of patients with suspicious imaging, which contribute to potential confusion and delays in diagnostic pathways and referrals. In fact, local baseline data demonstrated that patients with suspicious imaging for LC whose radiology report recommended referral to the LDAP were referred faster than those patients without a specific recommendation for LDAP-referral (6.9 vs. 12.9 days).Citation18 We chose this strategy because of growing evidence that templated reporting and recommendations improves the uniformity of dictated reports.Citation16 We sought to improve timeliness of local diagnostic pathways through the implementation and regional spread of a standardized radiology reporting recommendation for patients with imaging suspicious for LC.
Methods
Context
The LDAP of Southeastern Ontario is a rapid assessment clinic at an academic tertiary care hospital that provides patients with suspected LC access to specialists who coordinate care from diagnosis until transition to treatment. This predominantly rural region has a population of >500,000 patients, and every year almost 500 patients with a new LC diagnosis are seen in the regional cancer center, of which more than 60% are diagnosed with their management expedited through the LDAP. As there is no formal LC screening program in this region, patients are referred to the LDAP based on imaging findings suspicious for LC that are either discovered incidentally or during evaluation of clinical symptoms. Historically, our region has had the lowest relative 5-year LC survival in the province (15%) compared with the provincial average of 20.8%.Citation19 While the reasons for this discrepancy are multifactorial, delays in the LC diagnostic pathway may contribute.
At our center, there are dedicated cardiothoracic radiologists and several non-thoracic subspecialty radiologists who also report thoracic imaging in outpatients and when on-call. There are also several regional community hospitals staffed with radiologists; in some cases, locum radiologists. Of these community hospitals, 3 contribute the vast majority (∼90%) of regional referrals to the LDAP and were therefore selected for the intervention.
Interventions
We performed a stakeholder analysis with the cardiothoracic radiologists and radiology department head at the academic center, as well as the LDAP respirologists, manager, and quality improvement (QI) leader to review local data showing that patients with a radiology recommendation for LDAP referral experienced more timely care and discussed improvement strategies. This led to the development of standardized radiographic criteria on the CT that should prompt a recommendation for LDAP referral, which are in line with the LDAP entry criteria. These criteria were shared with all radiologists reporting thoracic CTs and accessible at the time of reporting, and included: a solitary pulmonary nodule or mass, multiple pulmonary nodules, mediastinal or hilar adenopathy, pleural effusion with suspicion of malignancy, non-resolving pneumonia or other imaging findings concerning for intrathoracic malignancy. At the academic center, this led to the development of the standardized macro embedded within PowerScribe 360 (Nuance Communication, Burlington, Massachusetts), “Referral to the [name of academic center] Lung Diagnostic Assessment Program is recommended,” with the macro called upon at the time of CT chest reporting. Meanwhile, to prompt this recommendation, the standardized radiology recommendation for LDAP referral and imaging criteria were then spread among 3 community hospitals by meeting with key stakeholders from each site. Local radiology leaders then met with frontline radiologists at each site to implement utilizing their respective reporting templates. Plan-Do-Study-Act (PDSA) cycles are summarized in .
Table 1. Plan-Do-Study-Act (PDSA) cycles.
Study of the interventions
We conducted a retrospective chart review of all LDAP-referred patients (January 2018 – December 2018) to establish baseline data and to prospectively assess for improvement (January - September 2019 for the academic center, March – September 2019 for community hospitals). We collected data including dates of CT chest, LDAP referral and assessment. We also collected data regarding the site at which imaging was performed, radiologist recommendations, including the language used in radiology reports for suspected LC, and appropriateness of referral as assessed by LDAP internal triage processes. Patients were excluded from the outcome measure if they were not assessed in the LDAP, because they declined referral or did not meet LDAP entry criteria (ie, deemed to have low suspicion of malignant disease, had a known cancer diagnosis, or were under the care of a treating oncologist and/or respirologist), but were included in process measures. Patients were also excluded from the analysis if their CT chest was performed outside of LDAP catchment area (ie, not at the sites targeted with the intervention).
Measures
The outcome measure was timeliness of LC care for LDAP patients as measured by the median time from CT chest to LDAP assessment. This measure was chosen as the literature suggests that delays in care negatively affect clinical outcomes.Citation20,Citation21
Process measures were (i) the proportion of LDAP-referred patients with a radiology recommendation for LDAP referral, (ii) the overall number of LDAP referrals, (iii) the proportion of referrals with a radiology report recommending LDAP referral that met standardized entry criteria and (iv) the median time from CT chest to LDAP referral. These measures were selected because it was hypothesized that increasing the proportion of patients with a recommendation for LDAP referral would improve the timeliness of referral for a greater number of patients and also increase the number of patients appropriately referred to the LDAP.
Balancing measures were (i) the median time from LDAP referral to assessment, ensuring that the increase in referrals did not negatively impact timeliness of care in other phases of the diagnostic process; and (ii) number of inappropriate referrals to the LDAP per month (ie, not meeting standardized LDAP entry criteria), to ensure that the anticipated increase in referrals did not lead to an unnecessary increase in workload.
Analysis
Descriptive data are reported as n (%). Continuous data are reported as medians (75th, 90th percentile). The Mann-Whitney U test was used to compared differences in referral and assessment intervals. Chi-square tests were used to compare differences in proportion of patients with recommendations for LDAP referrals. Run charts were used to assess for nonrandom variation resulting from the improvement process. We used SQUIRE 2.0 guidelines in the reporting of our initiative.Citation22
Ethical considerations
The local research ethics board granted study permission.
Results
Data were collected from 1,244 consecutive LDAP patient referrals, including 697 patients at baseline and 547 patients after standardization. There were 70 LDAP referrals with radiology reports from peripheral hospitals other than the 3 participating community hospitals (43 baseline, 27 post-standardization); these were excluded from analysis.
Process measures
Following standardization of radiology reporting, there was an increase in LDAP-referred patients with a radiologist recommendation for referral from 29.2% (191/654) to 48.3% (251/520) (P < .001) (), significant for the academic center (50.2% [147/293] to 61.8% [157/254]; P = .006) and community hospitals (12.1% [44/361] to 35.3% [94/266]; P < .001). Uptake in standardized radiology reporting varied across community hospitals; Sites A and C had an increase in LDAP-referred patients with a radiologist recommendation for referral (6.5% to 42.5%, P < .001; 2.0% to 12.9%, P = .04), while Site B experienced no significant change (30.5% to 22.4%; P = .31). Run charts demonstrate a nonrandomized increase in the number and proportion of LDAP referrals with radiologist recommendation for referral, demonstrating that the change was in keeping with the improvement intervention (). Following standardization of radiology reporting, the average number of monthly LDAP referrals increased non-significantly for the academic center (24.4 to 28.2; P = .10) and significantly for community hospitals (25.8 to 38.0; P = .006) (). The proportion of patient referrals that met standardized entry criteria increased from 83.3% to 88.1% (P = .02), significant for the academic center (78.8% to 89.8%; P < .001), but unchanged for community hospitals (Site A, 88.4% to 87.1%, P = .70; Site B, 86.3% to 83.7%, P = .67; Site C, 82.4% to 87.1%, P = .57) (). Lastly, the median (75th, 90th percentile) time from CT to LDAP referral was 5 days (9, 15) for patients with a radiologist recommendation for LDAP-referral compared with 6 days (16, 33) for patients without this recommendation (P < .001) ().
Figure 1. Percentage of Lung Diagnostic Assessment Program (LDAP)-referred patients with radiologist recommendation for referral to the LDAP by site, before and after standardization (process measure).
* statistically significant difference.
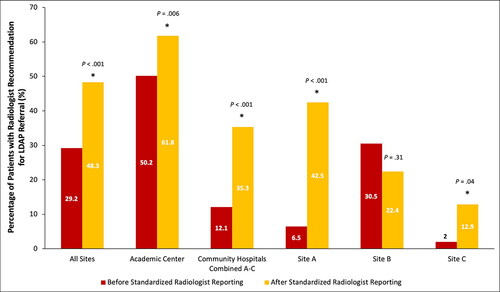
Figure 2. Run chart demonstrating the number (A) and proportion (B) of Lung Diagnostic Assessment Program (LDAP) referrals with radiologist recommendation for referral over time.
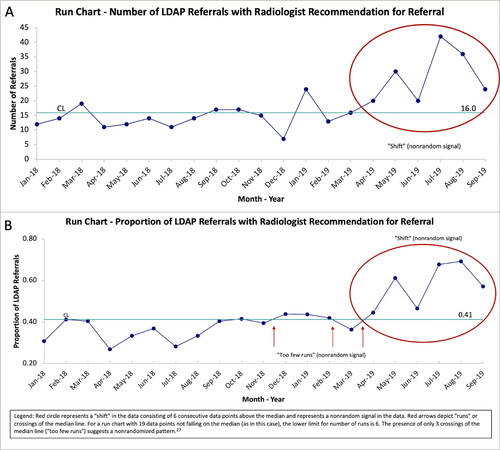
Figure 3. Impact of radiologist recommendation for referral to the Lung Diagnostic Assessment Program (LDAP) on time from computerized tomography (CT) chest to LDAP referral and assessment. Panel A: Time from CT chest to LDAP referral (process measure); Panel B: Time from CT chest to LDAP assessment (outcome measure); Panel C: Time from LDAP referral to assessment (balancing measure).
Box and whisker plot showing the median, interquartile and minimum and maximum days of the time interval between dates of CT to LDAP referral and assessment. X, mean; white font, median; * statistically significant difference (Mann-Whitney U-test).
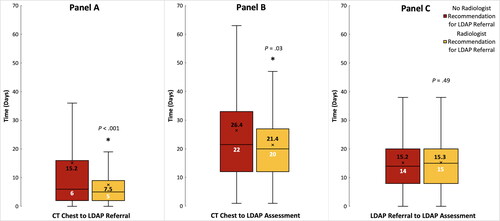
Table 2. Impact of standardized radiology reporting on pattern of LDAP referrals (process measure).
Outcome measure
The median (75th, 90th percentile) time from CT to specialist assessment was 20 days (27, 35) for patients with a radiologist recommendation for referral versus 22 days (33, 50) for patients without a recommendation for referral (P = .03) ().
Balancing measure
For patients with a radiologist recommendation for LDAP referral, the median (75th, 90th percentile) time from referral to assessment was 15 days (20, 27) compared with 14 days (20, 27) for patients without this radiologist recommendation (P = .49) (). While the overall proportion of referrals meeting LDAP entry criteria increased (process measure), the number of referrals per month increased as well, resulting in a non-significant increase in the number of inappropriate referrals from community hospitals (3.4 per month to 5.3 per month, P = 0.09), though unchanged for the academic center (4.1 per month to 4.4 per month, P = 0.72). We identified instances where patients were redundantly referred to the LDAP (ie, the patient already had an oncologist/respirologist [N = 8], were admitted to hospital [N = 5], or already known to the LDAP [N = 1]).
Barriers to standardized reporting
Some radiologist reports included non-standardized language to recommended specialist referral for suspected LC; 31 LDAP referred patients (2.6%) had a CT report with such non-standardized language, most from Site B (23 [74.2%]). When reports with non-standardized language were included in the analysis, there was a non-statistically significant increase in the proportion of LDAP-referred patients from Site B (41.1% to 49.0%; P = .36).
Discussion
Summary
The implementation and regional spread of standardized radiology reporting that recommends LDAP referral for patients with suspected LC led to faster patient referral and assessment. We used QI methodology to implement standardized radiology reporting at a local academic center and spread this initiative to 3 community hospitals. This led to an increase in both the number and proportion of patients with standardized radiology reporting. Patients with a standardized radiologist recommendation for LDAP referral experienced faster time from CT chest to LDAP referral and assessment even as the number of LDAP referrals with standardized recommendation increased. While the median improvement in time to LDAP referral and specialist assessment was 1 and 2 days, respectively, there was a significant reduction in the distribution of data for both process and outcome measures as demonstrated in . In fact, the 75th and 90th percentile values for time to LDAP referral were reduced by 7 days and 18 days, respectively, while the 75th and 90th percentile values for time to specialist assessment were reduced by 6 and 15 days, respectively. As such, 25% of patients experienced a 7-day faster LDAP referral and 10% of patients experienced a 15-day improvement in time to specialist assessment, which is a clinically meaningful difference for patients that experience the longest delays and demonstrates improved equity of care. By spreading the initiative to regional community hospitals, and observing similar improvements, we enhanced regional equity in care.
Our initiative was associated with an unanticipated increase in the proportion of LDAP-referred patients that met standardized entry criteria with the introduction of standardized reporting, driven primarily by an increase in appropriate referrals from the academic center. This suggests that standardized reporting led to improved compliance with LDAP entry criteria, likely due to clear, standardized indications for LDAP referral. However, the proportion of LDAP-referred patients from the community hospitals that met standardized LDAP entry criteria was unchanged, despite an overall increase in referrals from these sites, leading to an increase in both appropriate and inappropriate referrals from the community sites. There was no change in timeliness of LDAP assessment observed despite this increased volume, suggesting that inappropriate referrals were effectively identified and diverted through the LDAP internal triage process and that improved efficiencies in the diagnostic pathways were able to accommodate the larger referral volume of appropriate referrals. Furthermore, there was no difference in time from LDAP referral to assessment between patients with a radiology recommendation for referral compared to those without, which supports that the impact of our intervention was a result of improving time from abnormal imaging to LDAP referral.
Interpretation
Timeliness in LC care is critical as delays have been associated with disease progression and patient distress.Citation8–10,Citation13 While a survival benefit has not been demonstrated, interventions that lead to timely diagnosis and staging may improve patient outcomes.Citation2–4,Citation7 Radiologic imaging is often the starting point for LC diagnostic pathways, yet these pathways can be prone to delays.Citation11,Citation12 Significant benefits can be achieved by standardizing communications between radiologists and referring physicians. For example, addition of the Fleischner Society guidelines to chest CT reports increased the likelihood of receiving recommended follow-up care for incidental pulmonary nodules.Citation14 Meanwhile, the use of Lung-RADS as a structured reporting system provides clear and concise communication of LC screening results, which is central to guiding providers toward the appropriate management pathway.Citation17,Citation23 Therefore, radiology has an important role in improvement initiatives that aim to streamline LC diagnostic pathways, which may enable faster access to specialist care and improve patient outcomes.
Other centers have studied the impact of radiologist-initiated referral systems on timeliness of LC care. In the UK, a radiologist-initiated fast-track CT pathway for patients with a chest x-ray suspicious for LC led to earlier diagnosis and treatment decisions.Citation24 Meanwhile, a Canadian academic hospital implemented a radiologist-initiated referral system to LC specialists, that reduced time between CT imaging suspicious for LC to specialist referral and consultation.Citation12 Unlike our study, they did not address the larger-scale regional spread of the referral process. Our study is the first to spread a radiology-directed QI initiative for CT scans suspicious for LC to community hospitals by engaging with community radiologists. Our study is unique in its use of QI methodology to implement standardized radiologist reporting. By clearly defining entry criteria for the LDAP, standardizing CT reporting language, and spreading to community hospitals, we addressed system barriers, optimized timeliness of care and improved regional equity of care.
The uptake of standardized radiology reporting varied across community hospitals, with significant uptake in 2 out of 3 community hospitals. The site without an increase in standardized radiology reporting also accounted for the highest percentage of radiologist reports using non-standardized language to recommend specialist referral, which may explain the lack of observed improvement. Harvey et al.Citation25 found that conditional phrasing of CT chest recommendations resulted in a 32% lower rate of recommendation adherence compared with absolute phrasing, demonstrating the importance of absolute phrasing and standardized CT recommendations. Future improvement cycles will attempt to improve uptake and consistency of standardized radiology reporting, which would ultimately lead to an even more robust effect on timeliness of care.
Limitations
While standardized radiology reporting increased the overall proportion of appropriate referrals to the LDAP, there was also an overall increase in the number of referrals, which resulted in an overall increase in “inappropriate” referrals. Given that there was no change in timeliness of LDAP assessment observed despite this increased volume of referrals, we suspect that inappropriate referrals were effectively identified and diverted through the LDAP internal triage process, though with a possible, unmeasured impact on workload associated with triage. Further improvement efforts to increase the appropriateness of referrals through optimization of incorporation of the LDAP entry criteria into standardized radiology reporting may alleviate this.
Another limitation to our initiative is that, currently, referral to the LDAP must be initiated by another physician, usually the practitioner receiving the abnormal imaging report. This depends on the timely transmission of the report to the physician who ordered the study and is influenced by the individual workflow patterns of referring physicians. Future improvement cycles will employ a radiology-initiated referral process to eliminate this delay, similar to other groups.Citation12,Citation26 Another limitation to our study is lack of universal implementation of standardized radiology reporting across all referral sites. While most LDAP patients are referred from the academic center and 3 community hospitals, the LDAP still received 70 referrals during the study period (5.6% of all referrals) from other peripheral sites that were not targeted for the improvement initiative. While it may not be possible to reach all peripheral sites, future initiatives will attempt to reach the greatest number of patients possible.
While our intervention focused on standardized radiology reporting of CT chest, we recognize potential value in broadening this approach to other imaging modalities (eg, chest x-ray). While incorporating this strategy may increase referrals to the LDAP, there is the risk of increased inappropriate referrals and subsequent diagnostic delays due to high clinic volumes. Our intervention may benefit from the introduction of new standardized radiology reporting templates that embed the standardized macro within the report so as to prompt radiologists to consider referral to the LDAP if appropriate. A system that further incorporates the LDAP entry criteria as a point-of-care reference may further help with appropriateness of LDAP referrals and will be explored with the radiology team.
Finally, many community hospitals utilized locum radiologists to report imaging. Locum physicians would likely be less familiar with local referral and management pathways. As such, to maximize the impact of our program, a secondary mechanism of identifying imaging suspicious for LC may be of value, which could include an automated process that identifies worrisome language in the radiology report and generates an LDAP referral.
Conclusion
The implementation and regional spread of standardized radiology reporting that recommends LDAP referral for patients with suspected LC led to significant uptake in standardized reporting and a faster time to specialist referral and patient assessment. Our intervention had the greatest impact on those patients that experienced the longest delays in care, thereby improving equitability of care. Not only was timeliness of care improved with standardized radiology reporting, but standardization also improved regional equity in LC diagnostic pathways and access to care through an increase in appropriate LDAP referrals. Variations on a standardized reporting pathway may be applied at other institutions to improve patient care. Future improvement cycles include ongoing standardization of radiology templates, feedback to community sites regarding appropriateness of referrals, spread of standardized radiology reporting to other imaging modalities and facilitation of direct specialist referral, which have potential to further improve timeliness of care.
Acknowledgments
The authors are thankful for the KHSC cardiothoracic radiologists (Justin Flood and Giang Nguyen) for involvement in the change initiatives and the LDAP Team, including Nicole O’Callaghan.
Disclosure statement
The authors report no conflict of interest.
Funding
This work was supported by the Queen’s University Department of Medicine Quality Improvement and Patient Safety Research Award.
Data availability statement
Due to the nature of this research, participants of this study did not agree for their data to be shared publicly and, therefore, supporting data is not available.
References
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA A Cancer J Clin. 2020;70(1):7–30. doi:https://doi.org/10.3322/caac.21590.
- Kanarek NF, Hooker CM, Mathieu L, et al. Survival after community diagnosis of early-stage non-small cell lung cancer. Am J Med. 2014;127(5):443–449. doi:https://doi.org/10.1016/j.amjmed.2013.12.023.
- Gould MK, Ghaus SJ, Olsson JK, et al. Timeliness of care in veterans with non-small cell lung cancer. Chest. 2008;133(5):1167–1173. doi:https://doi.org/10.1378/chest.07-2654.
- Olsson JK, Schultz EM, Gould MK. Timeliness of care in patients with lung cancer: a systematic review. Thorax. 2009;64(9):749–756. doi:https://doi.org/10.1136/thx.2008.109330.
- Kim JOA, Davis F, Butts C, et al. Waiting time intervals for non-small cell lung cancer diagnosis and treatment in Alberta: quantification of intervals and identification of risk factors associated with delays. Clin Oncol (R Coll Radiol)). 2016;28(12):750–759. doi:https://doi.org/10.1016/j.clon.2016.06.010.
- Lo DS, Zeldin RA, Skrastins R, et al. Time to treat: a system redesign focusing on decreasing the time from suspicion of lung cancer to diagnosis. J Thorac Oncol. 2007;2(11):1001–1006. doi:https://doi.org/10.1097/JTO.0b013e318158d4b6.
- Samson P, Patel A, Garrett T, et al. Effects of delayed surgical resection on short-term and long-term outcomes in clinical stage I non-small cell lung cancer. Ann Thorac Surg. 2015;99(6):1906–1913. doi:https://doi.org/10.1016/j.athoracsur.2015.02.022.
- Yilmaz A, Damadoglu E, Salturk C, et al. Delays in the diagnosis and treatment of primary lung cancer: are longer delays associated with advanced pathological stage?Ups J Med Sci. 2008;113(3):287–296. doi:https://doi.org/10.3109/2000-1967-236.
- Geiger GA, Kim MB, Xanthopoulos EP, et al. Stage migration in planning PET/CT scans in patients due to receive radiotherapy for non-small-cell lung cancer. Clin Lung Cancer. 2014;15(1):79–85. doi:https://doi.org/10.1016/j.cllc.2013.08.004.
- Mohammed N, Kestin LL, Grills IS, et al. Rapid disease progression with delay in treatment of non–small-cell lung cancer. Int J Radiat Oncol. 2011;79(2):466–472. doi:https://doi.org/10.1016/j.ijrobp.2009.11.029.
- Percac-Lima S, Ashburner JM, Shepard JA, et al. Timeliness of recommended follow-up After an Abnormal Finding on Diagnostic Chest CT in Smokers at High Risk of Developing Lung Cancer. J Am Coll Radiol. 2016;13(5):497–504. doi:https://doi.org/10.1016/j.jacr.2016.01.007.
- Tremblay A, Strilchuk N, Taghizadeh N, et al. Radiologist initiated specialty referral for patients suspected of having a thoracic malignancy. Canadian Journal of Respiratory, Critical Care, and Sleep Medicine. 2017;1(4):180–185. doi:https://doi.org/10.1080/24745332.2017.1377055.
- Brocken P, Prins JB, Dekhuijzen PR, et al. The faster the better?—A systematic review on distress in the diagnostic phase of suspected cancer, and the influence of rapid diagnostic pathways. Psychooncology. 2012;21(1):1–10. doi:https://doi.org/10.1002/pon.1929.
- McDonald JS, Koo CW, White D, et al. Addition of the Fleischner Society Guidelines to chest CT examination interpretive reports improves adherence to recommended follow-up care for incidental pulmonary nodules. Acad Radiol. 2017;24(3):337–344. doi:https://doi.org/10.1016/j.acra.2016.08.026.
- Kang SK, Doshi AM, Recht MP, et al. Process improvement for communication and follow-up of incidental lung nodules. J Am Coll Radiol. 2020;17(2):224–230. doi:https://doi.org/10.1016/j.jacr.2019.11.023.
- Aase A, Fabbrini AE, White KM, et al. Implementation of a standardized template for reporting of incidental pulmonary nodules: feasibility, acceptability, and outcomes. J Am Coll Radiol. 2020;17(2):216–223. doi:https://doi.org/10.1016/j.jacr.2019.11.013.
- Fintelmann FJ, Bernheim A, Digumarthy SR, et al. The 10 pillars of lung cancer screening: rationale and logistics of a lung cancer screening program. Radiographics. 2015;35(7):1893–1908. doi:https://doi.org/10.1148/rg.2015150079.
- Mullin M, Howard T, Dhillon G, et al. Impact of radiologist recommendations on timeliness of lung cancer referral: baseline data to guide a quality improvement initiative. J Thorac Oncol. 2019;14(10):S348–S349. doi:https://doi.org/10.1016/j.jtho.2019.08.705.
- Cancer System Quality Index. https://www.csqi.on.ca/search?navsearch=LHIN10SouthEast&sort_by=search_api_relevance. Jun 2018., Accessed 30 Mar 2020.
- Gomez DR, Liao K-P, Swisher SG, et al. Treatment delay in lung cancer time to treatment as a quality metric in lung cancer: staging studies, time to treatment, and patient survival. Radiother Oncol. 2015;115(2):257–263. doi:https://doi.org/10.1016/j.radonc.2015.04.010.
- Kasymjanova G, Small D, Cohen V, et al. Lung cancer care trajectory at a Canadian centre: an evaluation of how wait times affect clinical outcomes. Curr Oncol. 2017;24(5):302–309. doi:https://doi.org/10.3747/co.24.3611.
- Ogrinc G, Davies L, Goodman D, et al. SQUIRE 2.0 (Standards for QUality Improvement Reporting Excellence): Revised publication guidelines from a detailed consensus process. BMJ Qual Saf. 2016;25(12):986–992. doi:https://doi.org/10.1136/bmjqs-2015-004411.
- American College of Radiology. Lung-RADSTM version 1.1 assessment categories release date: 2019. https://www.acr.org/-/media/ACR/Files/RADS/Lung-RADS/LungRADSAssessmentCategoriesv1-1.pdf. Accessed 30 March 2020.
- Lal A, Phillips S, Russell C, et al. The novel use of fast track CT to select patients for lung cancer clinics: effect on clinic efficiency, waiting times, and patient satisfaction. Postgrad Med J. 2011;87(1026):264–268. doi:https://doi.org/10.1136/pgmj.2010.109330.
- Harvey HB, Wu CC, Gilman MD, et al. Correlation of the strength of recommendations for additional imaging to adherence rate and diagnostic yield. J Am Coll Radiol. 2015;12:1216–1222. doi:https://doi.org/10.1016/j.jacr.2015.03.038.
- Leiro-Fernández V, Botana-Rial M, Tilve-Gómez A, et al. Effectiveness of a protocolized system to alert pulmonologists of lung cancer radiological suspicion. Clin Transl Oncol. 2014;16(1):64–68. doi:https://doi.org/10.1007/s12094-013-1042-0.
- Provost LP, Murray S. The Health Care Data Guide: Learning from Data for Improvement. San Francisco, CA: Jossey-Bass; 2011.
