 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Program performance monitoring provides evidence of the quality and value of the services that tuberculosis (TB) programs provide.
All TB programs in Canada are encouraged to monitor the same core indicators of performance using the definitions and suggested targets provided.
This framework should be considered a minimum standard for monitoring Canadian TB programs; jurisdictions are encouraged to monitor additional indicators relevant to the populations served.
Assessment against targets produces quantitative measures of performance, which are useful to reallocate efforts and resources.
Program performance monitoring should be annual, with summaries made available to TB programs and other relevant stakeholders, as well as the public.
Program performance monitoring requires adequate human resources dedicated to data collection, validation and analyses processes.
Interpretation of monitoring results should be performed in close collaboration with the physician/nursing leads to ensure clinically relevant judgments are properly considered.
Solutions to programmatic underperformance should be collaborative, involving members of TB-affected communities, select population groups, and relevant stakeholders.
TB programs should monitor their capacity to provide patient-centered care and favorably influence long-term outcomes, which, among other program staff, is dependent on having dedicated support of a social worker.
KEY POINTS
1. Introduction
This new chapter of the Canadian TB Standards (the Standards) is focused on the role of program performance monitoring in the era of TB elimination. This chapter describes a program performance monitoring framework as part of the Standards to measure the value, quality and impact of services provided by TB programs across Canada.Citation1,Citation2 In addition to frontline staff of TB programs, the intended audience for this chapter includes TB program managers, health policy leaders and physician/nursing leads.
2. Background
In 2014, after the full endorsement of its member states through a World Health Assembly resolution, the World Health Organization (WHO) began promoting the new End TB Strategy as the global approach to eliminating TB.Citation3 This strategy outlines three major pillars: the provision of high-quality, patient-centered prevention and care (Pillar 1); increased political will, and sustained resources for bold action (Pillar 2); and research and innovation (Pillar 3).Citation4 Implementation of these pillars is meant to help achieve three targets by the year 2035: 1) reduce the number of new TB cases by 90% and 2) the number of TB-attributable deaths by 95%, both as compared to 2015; and 3) have no TB-affected families incurring catastrophic costs due to TB.Citation4
To evaluate national progress toward achieving these targets, systematic program performance monitoring is recommended as part of the End TB strategy and has been widely adopted internationally.Citation5–9 Canada is a signatory to the End TB Strategy and thus has an obligation to implement this recommendation. The purpose of such evaluations is to distinguish programs that promote health and prevent disease from those that do not.Citation10 In turn, monitoring generates information that can be used to judge the quality and value of public health programs, like TB services.Citation11 An appropriately designed program performance monitoring framework should document progress toward goals, identify areas for improvement and demonstrate the impact of resource investments.Citation12
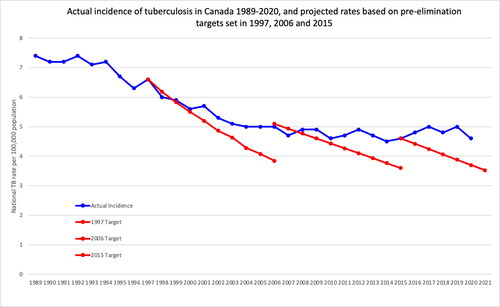
Although the importance of TB program performance monitoring in Canada has been discussed for more than 20 years, notably by Health Canada, the pan-Canadian Public Health Network and Inuit Tapiriit Kanatami, a national framework does not yet exist.Citation13–17 In the same period, a substantial reduction in cases has not been achieved, with the overall annual incidence of TB in Canada remaining flat for 16 years, as in (see Chapter 1: Epidemiology of Tuberculosis in Canada).
Figure 1. Actual incidence of TB in Canada.
Actual incidence: Reported cases from the Notifiable diseases on-line (PHAC)Citation20 1924 to 2019 in Canada
1997 target: 5% annual reduction in casesCitation21
2006 target: Reach a target incidence of 3.6 by 2015. A linear relationship was plotted and extended beyond the 2015 goal.Citation22
2015 target: Reduce new incident cases by 90% in 2035 as compared to 2015.Citation4 Note that these case numbers are for Canada overall and differ for select populations within Canada.
Meanwhile, performance indicators have been adopted in other settings to assess regional and national TB prevention and care services. For example, 1 study from the United States showed marked improvements in outcomes within local health regions that actively monitored and evaluated performance relative to those that passively collected data.Citation18 In England, where a national standard of performance indicators exists, research has contributed to recommendations for new indicators to improve the overall quality and value of TB services within the context of elimination.Citation19 In sum, program performance monitoring has been successful elsewhere, and this chapter provides recommendations for use by TB programs in Canada.
3. Design and limitations of a performance monitoring framework
In 2018, the National Collaborating Center for Infectious Diseases conducted a scoping review, compiling reports and TB program performance indicators from 25 distinct programs in other low-incidence countries and regions as well as for 3 TB-affected population groups in Canada: First Nations, Inuit and foreign-born populations. Analysis of these documents led to a list of 105 program performance indicators with potential applicability to Canada. That same year, those indicators were discussed at a national meeting and ranked using a modified Delphi technique.Citation23,Citation24 The meeting concluded with expert consensus achieved on 8 core indicators of TB program performance relevant to the aforementioned priority populations.Citation17,Citation24
These eight core indicators were reviewed by all of the authors of this chapter with additions made during facilitated discussion to produce a more generalizable tool. The end result is a framework of twelve indicators (see ) that can be used to evaluate TB services across Canada.
Table 1. Indicators and related targets.
The resulting framework comprises program performance indicators (actions) that are largely pragmatic and judged to adhere to the following criteria: relevant, well-defined, reliable, technically feasible, practical and have a history of use elsewhere.Citation25 It is, however, not without limitation. For example, TB programs in provinces and territories that have a high proportion of foreign-born persons may ultimately perform well across most or all program performance indicators, but see limited reduction of incidence.Citation26,Citation27 This is because replenishment of the reservoir of TB infections may continually occur among those from high-TB-incidence nations.Citation28–31 (see Chapter 13: Tuberculosis Surveillance and Tuberculosis Testing and Treatment in Migrants). Implementing this framework will require dedicated human resources with requisite qualifications to properly compile and report these data. This investment is justified, as program performance monitoring produces valuable information for programmatic improvement, strengthens program management activities, improves accountability and generates evidence of the value of TB services.Citation11,Citation18,Citation32
4. Core program performance indicators
This program performance monitoring framework includes 12 indicators, with accompanying targets. In the absence of preexisting national data, targets were set to strike a balance between being achievable and motivational based on expert guidance. Future iterations of this nationally applicable framework should adjust these targets based on actual performance.
Overall, this initial performance monitoring framework focuses on the management of patients with smear-positive pulmonary TB and their contacts, as these groups are considered the highest priorities for optimal program performance. Indicators are grouped according to the following goals/objectives.
4.1. Elimination
The goals for pre-elimination and elimination are set in Canada’s international commitments and programs should be monitoring their own year-on-year progress toward meeting them. The pre-elimination target for low-incidence settings is an active case rate of 10/1,000,000 population by 2035, while the elimination target is 1/1,000,000 population by 2050 at the national level. Progress toward elimination depends on achieving a rate of decline that aligns with those targets, but will be influenced by the local epidemiology of TB in the populations served by the program. As a result, the rate of decline will vary by the reporting program.
4.2. Objectives for examination of immigrants and refugees
Foreign-born persons contribute the highest absolute number and proportion (>70%) of TB cases in Canada, which creates pressure on the pace of decline that can be achieved domestically. Therefore, programs should give priority to managing Immigration Medical Exam referrals (see Chapter 13: Tuberculosis Surveillance and Tuberculosis Testing and Treatment in Migrants).Citation26,Citation33
4.3. Objectives for case management and treatment
Timely diagnosis of, and effective treatment initiation in, people with pulmonary TB is paramount in preventing the transmission of TB, and to prevent further morbidity and mortality for these individuals. Maximizing successful treatment (cure or treatment completed) while minimizing unsuccessful treatment outcomes (TB-related death, treatment non-completion loss to follow-up) are key outcomes. In addition, the psycho-social and behavioral needs of people affected by TB may influence local epidemiology and individual outcomes. Addressing these issues is central to the program’s ability to provide patient-centered care (see Chapter 5: Treatment of Tuberculosis Disease).
4.4. Objectives for contact management
Preventing the reactivation of latent TB infections is an equally crucial component of TB elimination, particularly for priority contacts — that is, close contacts of persons with smear-positive, pulmonary TB (see Chapter 11: Tuberculosis Contact Investigation and Outbreak Management).
The calculations for each indicator tabulate the number of times the action was completed out of the number of times it was applicable, displayed as a proportion.Citation34 These proportions are then compared quantitatively to defined targets. Definitions of these actions and targets are provided in , while methods for analysis and reporting are provided in .
5. Analytic and action strategies
describes how to measure and analyze performance of TB programs based on the indicators in this framework. This analytic strategy is separate from the clinical care of patients, which is covered in other chapters of these standards.
5.1. Reporting schedule
Performance monitoring will be achieved by completing reports on the indicators presented here, according to the formulas provided in . Program performance indicators for the immediate past calendar year should be reported in February or March of the current year, except for treatment outcomes of all patients diagnosed with TB disease in the previous calendar year, which can be reported only a full year after. Annual program performance reports should be discussed with appropriate local public health representatives and community partners to ensure accountability, determine whether and how actions should be changed to improve outcomes and contextualize the information in a culturally-safe manner.Citation35 Program managers (leads) are best positioned to implement change. This makes it crucial that program managers oversee the process and develop a mechanism to properly engage stakeholder groups.Citation36 Annual summary reports should be published online to promote transparency and contribute to benchmarking efforts across the country.
Implementation of this program performance monitoring framework includes the completion of annual reports (to assess local performance over time) that are consistent across jurisdictions (to assess relative performance). Timely completion and sharing of these reports will help minimize delays in making program improvements. TB programs should allocate adequate human resources for data collection and validation to monitor these indicators. Validation should be performed in close collaboration with the physician/nursing leads and relevant community partners.
5.2. Recommended demographic, clinical and social variables
It is recommended that data be analyzed by age, sex/gender and population group to maintain a focus on where there is greatest need for TB services and care and where inequities can be mitigated. These levels of disaggregation align with international and Canadian standards for sex- and gender-based analysis of health data.Citation37–41 Depending on local decisions for programs to collect or link with other data, analyses can also include other significant social strata of risk, including human immunodeficiency virus (HIV) status, persons experiencing homelessness, persons with limited labor participation and/or high-risk occupations and persons currently or recently incarcerated.
5.3. Role of social work in addressing patient and client needs
Responses to TB-associated social risk factors should be addressed by a dedicated TB-program social worker; the ability of programs to do this should be monitored. Among communicable infectious diseases, TB in particular illustrates how structural barriers imposed by racism, classism and colonialism in Canada require political commitment to make health systems available and accessible to all (see Chapter 12: An Introductory Guide to Tuberculosis Care Serving Indigenous Peoples and Chapter 13: Tuberculosis Surveillance and Tuberculosis Testing and Treatment in Migrants).Citation42,Citation43 At the same time, psycho-social, behavioral and biological considerations complicate TB disease and its management (eg, substance use disorders, contact network structures, HIV/AIDS (acquired immunodeficiency syndrome), diabetes, undernutrition).Citation44–55 Because the specific tasks of the dedicated TB-program social worker may vary, programs can assess the impact of this support in various ways, including: 1) reporting the proportion of patients connected to a primary care provider by the end of TB care; 2) reporting the proportion of patients experiencing homelessness who are adequately housed by the end of TB care; and 3) assessing housing conditions among patients with infectious TB.
6. Summary
In a federation, meeting the challenge of TB elimination is made more difficult by inherent differences in the delivery of health services across the country. Accordingly, each province and territory contributes parts of what, in sum, constitutes the national response. Every person with active TB in Canada matters, and by committing to the aspirational End TB targets, there is a recognition that every prevented case counts more than ever. The purpose of this chapter is to encourage TB program leads and staff to provide evidence to communities, the public at large, health authorities and governments of progress toward desired outcomes. The core program performance indicators described in this chapter are considered the minimum standard for all programs.
Disclosure statement
The CTS TB Standards editors and authors declared potential conflicts of interest at the time of appointment and these were updated throughout the process in accordance with the CTS Conflict of Interest Disclosure Policy. Individual member conflict of interest statements are posted on the CTS website.
Funding
The 8th edition Canadian Tuberculosis Standards are jointly funded by the Canadian Thoracic Society (CTS) and the Public Health Agency of Canada, edited by the CTS and published by the CTS in collaboration with AMMI Canada. However, it is important to note that the clinical recommendations in the Standards are those of the CTS. The CTS TB Standards editors and authors are accountable to the CTS CRGC and the CTS Board of Directors. The CTS TB Standards editors and authors are functionally and editorially independent from any funding sources and did not receive any direct funding from external sources.
The CTS receives unrestricted grants which are combined into a central operating account to facilitate the knowledge translation activities of the CTS Assemblies and its guideline and standards panels. No corporate funders played any role in the collection, review, analysis or interpretation of the scientific literature or in any decisions regarding the recommendations presented in this document
References
- World Health Organization. Strategy for the control and elimination of tuberculosis. In: Implementing the WHO Stop TB Strategy: A Handbook for National Tuberculosis Control Programmes. Geneva: WHO Press; 2008.
- Cole B, Nilsen DM, Will L, Etkind SC, Burgos M, Chorba T. Essential Components of a Public Health Tuberculosis Prevention, Control, and Elimination Program: Recommendations of the Advisory Council for the Elimination of Tuberculosis and the National Tuberculosis Controllers Association. MMWR Recomm Rep. 2020;69(7):1–27. doi:10.15585/mmwr.rr6907a1.
- Uplekar M, Weil D, Lonnroth K, et al. WHO’s new End TB Strategy. The Lancet. 2015;385(9979):1799–1801. doi:10.1016/S0140-6736(15)60570-0.
- World Health Organization. The End TB Strategy. https://www.who.int/tb/strategy/End_TB_Strategy.pdf. Published 2015. Accessed July 5, 2021.
- Australian Government Department of Health and Ageing. The strategic plan for control of tuberculosis in Australia: 2011–2015. Australian Government Department of Health and Ageing. www1.health.gov.au. Accessed June 30, 2021.
- Degeling C, Carroll J, Denholm J, Marais B, Dawson A. Ending TB in Australia: Organizational challenges for regional tuberculosis programs. Health Policy. 2020;124(1):106–112. doi:10.1016/j.healthpol.2019.11.009.
- Public Health England. Collaborative TB Strategy for England, 2015 to 2020: end of programme report. 2015. GW-1954.
- Pan American Health Organization. The End TB Strategy: Main Indicators in the Americas. 2020.
- Kritski A, Barreira D, Junqueira-Kipnis AP, et al. Brazilian Response to Global End TB Strategy: The National Tuberculosis Research Agenda. Revista da Sociedade Brasileira de Medicina Tropical. 2016;49:135–145. doi:10.1590/0037-8682-0330-2015.
- Davidson EJ. Evaluative Reasoning. Methodological Briefs: Impact Evaluation. 2014;4:1–14.
- Coelho AA, Martiniano CS, Brito EWG, et al. Tuberculosis care: an evaluability study. Revista Latino-Americana de Enfermagem. 2014;22(5):792–800. doi:10.1590/0104-1169.3294.2482.
- Centers for Disease Control. Framework for Program Evaluation in Public Health. MMWR. 1999;48(RR-11):1–40.
- Health Canada. Health Canada’s Strategy against Tuberculosis for First Nations on-Reserve. Ottawa, Ont.: Health Canada; 2012.
- Health Canada. Health Canada’s Monitoring and Performance Framework for Tuberculosis Programs for First Nations on-Reserve. Feb 12 2016.
- Pan-Canadian Public Health Network. Guidance for Tuberculosis Prevention and Control Programs in Canada. 2013.
- Inuit Tapiriit Kanatami. Inuit Tuberculosis Elimination Framework. 2018.
- Haworth-Brockman M, Balakumar S, Head B, Keynan Y. Towards TB Elimination: Shared Priorities for TB Program Performance Measurement in Canada, a Proposal for Discussion. Winnipeg, Manitoba: National Collaborating Centre for Infectious Diseases; June 2019. 453.
- Cass A, Shaw T, Ehman M, Young J, Flood J, Royce S. Improved Outcomes Found After Implementing a Systematic Evaluation and Program Improvement Process for Tuberculosis. Public Health Reports. 1974-). 2013;128(5):367–376. doi:10.1177/003335491312800507.
- Cavany SM, Sumner T, Vynnycky E, et al. An evaluation of tuberculosis contact investigations against national standards. Thorax. 2017;72(8):736–745. doi:10.1136/thoraxjnl-2016-209677.
- Government of Canada, Public Health Agency of Canada. Reported cases from 1924 to 2019 in Canada - Notifiable diseases on-line. https://diseases.canada.ca/notifiable/charts?c=pl. Published 2000. Updated Accessed January 1, 2000.
- Proceedings of the National Consensus Conference on Tuberculosis. December 3-5, 1997. 1998;24(Supplement 2):1-24.
- The global plan to stop TB 2006-2015: actions for life: towards a world free of tuberculosis. Geneva: Stop TB Partnership; 2006.
- Stewart TR. The Delphi technique and judgmental forecasting. Clim Change. 1987;11(1-2):97–113. doi:10.1007/BF00138797.
- Niederberger M, Spranger J. Delphi Technique in Health Sciences: A Map. Front Public Health. 2020;8:457. doi:10.3389/fpubh.2020.00457.
- von Schirnding Y. Health in Sustainable Development Planning: The Role of Indicators. Geneva: World Health Organization; 2002. WHO/HDE/HID/02.11.
- Langlois-Klassen D, Wooldrage KM, Manfreda J, et al. Piecing the puzzle together: foreign-born tuberculosis in an immigrant-receiving country. European Respiratory Journal. 2011;38(4):895–902. doi:10.1183/09031936.00196610.
- World Health Organization. Global Tuberculosis Control: surveillance, Planning, Financing. Geneva: WHO Press; 2005.
- Asadi L, Heffernan C, Menzies D, Long R. Effectiveness of Canada’s tuberculosis surveillance strategy in identifying immigrants at risk of developing and transmitting tuberculosis: a population-based retrospective cohort study. The Lancet Public Health. 2017;2(10):e450–e457. doi:10.1016/S2468-2667(17)30161-5.
- Greenaway C, Pareek M, Chakra C-NA, et al. The effectiveness and cost-effectiveness of screening for latent tuberculosis among migrants in the EU/EEA: a systematic review. Eurosurveillance. 2018;23(14):17. doi:10.2807/1560-7917.ES.2018.23.14.17-00543.
- Berrocal-Almanza LC, Harris R, Lalor MK, et al. Effectiveness of pre-entry active tuberculosis and post-entry latent tuberculosis screening in new entrants to the UK: a retrospective, population-based cohort study. The Lancet Infectious Diseases. 2019;19(11):1191–1201. doi:10.1016/S1473-3099(19)30260-9.
- Kruijshaar ME, Abubakar I, Stagg HR, Pedrazzoli D, Lipman M. Migration and tuberculosis in the UK: targeting screening for latent infection to those at greatest risk of disease. Thorax. 2013;68(12):1172–1174. doi:10.1136/thoraxjnl-2013-203254.
- Ehman M, Shaw T, Cass A, et al. Developing and Using Performance Measures Based on Surveillance Data for Program Improvement in Tuberculosis Control. Journal of Public Health Management and Practice. 2013;19(5):E29–E37. doi:10.1097/PHH.0b013e3182751d6f.
- Stop TB Partnership, World Health Organization. The Global Plan to Stob TB 2011-2015: transforming the Fight towards Elimination of Tuberculosis. Geneva: World Health Organization; 2011.
- Horsburgh CR, Feldman S, Ridzon R. Practice Guidelines for the Treatment of Tuberculosis. Clinical Infectious Diseases. 2000;31(3):633–639. doi:10.1086/314007.
- Curtis E, Jones R, Tipene-Leach D, et al. Why cultural safety rather than cultural competency is required to achieve health equity: a literature review and recommended definition. International Journal for Equity in Health. 2019;18(1):174. doi:10.1186/s12939-019-1082-3.
- Canadian Health Services Research Foundation. Performance Reporting to Help Organizations Promote Quality Improvement. Healthcare Policy | Politiques de Santé. 2008;4(2):70–74.
- Health Canada. Health Portfolio Sex and Gender-Based Analysis Policy. https://www.canada.ca/en/health-canada/corporate/transparency/corporate-management-reporting/heath-portfolio-sex-gender-based-analysis-policy.html. Published 2017. Accessed July 27, 2021.
- World Health Organization. Closing data gaps in gender. https://www.who.int/activities/improving-treatment-for-snakebite-patients. Published 2019. Accessed July 27, 2021.
- Global Health Data Exchange | GHDx. http://ghdx.healthdata.org/. Accessed July 27, 2021.
- Gigli KH. Data Disaggregation: A Research Tool to Identify Health Inequities. Journal of Pediatric Health Care. 2021;35(3):332–336. doi:10.1016/j.pedhc.2020.12.002.
- Gomes MGM, Barreto ML, Glaziou P, et al. End TB strategy: the need to reduce risk inequalities. BMC Infectious Diseases. 2016;16(1):132. doi:10.1186/s12879-016-1464-8.
- Smith A, Herington E, Loshak H. Tuberculosis Stigma and Racism, Colonialism, and Migration: A Rapid Qualitative Review. Ottawa (ON): Canadian Agency for Drugs and Technologies in Health; 2021.
- Mathema B, Andrews JR, Cohen T, et al. Drivers of Tuberculosis Transmission. J Infect Dis. 2017;216(suppl_6):S644–S653. doi:10.1093/infdis/jix354.
- Kwan CK, Ernst JD. HIV and Tuberculosis: a Deadly Human Syndemic. Clinical Microbiology Reviews. 2011;24(2):351–376. doi:10.1128/CMR.00042-10.
- Gupta KB, Gupta R, Atreja A, Verma M, Vishvkarma S. Tuberculosis and nutrition. Lung India: Official Organ of Indian Chest Society. 2009;26(1):9–16. doi:10.4103/0970-2113.45198.
- Sylla L, Bruce RD, Kamarulzaman A, Altice FL. Integration and co-location of HIV/AIDS, tuberculosis and drug treatment services. International Journal of Drug Policy. 2007;18(4):306–312. doi:10.1016/j.drugpo.2007.03.001.
- Zumla A, Malon P, Henderson J, Grange J. Impact of HIV infection on tuberculosis. Postgraduate Medical Journal. 2000;76(895):259–268. doi:10.1136/pmj.76.895.259.
- Marais BJ, Lönnroth K, Lawn SD, et al. Tuberculosis comorbidity with communicable and non-communicable diseases: integrating health services and control efforts. The Lancet Infectious Diseases. 2013;13(5):436–448. doi:10.1016/S1473-3099(13)70015-X.
- Cormier M, Schwartzman K, N’Diaye DS, et al. Proximate determinants of tuberculosis in Indigenous peoples worldwide: a systematic review. The Lancet Global Health. 2019;7(1):e68–e80. doi:10.1016/S2214-109X(18)30435-2.
- Ali M. Treating tuberculosis as a social disease. The Lancet. 2014;383(9936):2195. doi:10.1016/S0140-6736(14)61063-1.
- Khan K, Rea E, McDermaid C, et al. Active Tuberculosis among Homeless Persons, Toronto, Ontario, Canada, 1998–2007. Emerging Infectious Diseases. 2011;17(3):357–365. doi:10.3201/eid1703.100833.
- Marks SM, Taylor Z, Burrows NR, Qayad MG, Miller B. Hospitalization of homeless persons with tuberculosis in the United States. Am. J. Public Health. 2000;90(3):435–438. doi:10.2105/ajph.90.3.435.
- Parriott A, Malekinejad M, Miller AP, Marks SM, Horvath H, Kahn JG. Care Cascade for targeted tuberculosis testing and linkage to Care in Homeless Populations in the United States: a meta-analysis. BMC Public Health. 2018;18:485. doi:10.1186/s12889-018-5393-x.
- Baker MA, Harries AD, Jeon CY, et al. The impact of diabetes on tuberculosis treatment outcomes: A systematic review. BMC Medicine. 2011;9(1):81. doi:10.1186/1741-7015-9-81.
- Stevenson CR, Forouhi NG, Roglic G, et al. Diabetes and tuberculosis: the impact of the diabetes epidemic on tuberculosis incidence. BMC Public Health. 2007;7(1):234. doi:10.1186/1471-2458-7-234.
- World Health Organization. Compendium of Indicators for Monitoring and Evaluating National Tuberculosis Programs. Geneva: World Health Organization; 2004.
- Henderson DA. The challenge of eradication: lessons from past eradication campaigns. Int J Tuberc Lung Dis. 1998;2(9 Suppl 1): S4–S8.
- World Health Organization. International Health Regulations. Geneva: WHO Press; 2005.
- Center for Disease Control. TB - National TB Program Objectives and Performance Targets for 2025. Centers for Disease Control and Prevention Web site. https://www.cdc.gov/tb/programs/evaluation/indicators/default.htm. Published 2019. Accessed September 18, 2019.
- Bareja C, Waring J, Stapledon R, Toms C, Douglas P. Tuberculosis notifications in Australia. Commun Dis Intell. 2011;38(4):E356–E368. 2014;
- Alaska Departement of Health and Social Services. Alaska Tuberculosis Program Manual. 2017.
- Minnesota Department of Health. Published 2021. https://www.health.state.mn.us/diseases/tb/stats/index.html. Accessed Jul 6, 2021.
- California Department of Public Health. TB Performance Trends for National and California Objectives. 2016.
- Heffernan C, Long R. Would program performance indicators and a nationally coordinated response accelerate the elimination of tuberculosis in Canada? Can J Public Health. 2019;110(1):31–35. doi:10.17269/s41997-018-0106-x.
- Chan IHY, Kaushik N, Dobler CC. Post-migration follow-up of migrants identified to be at increased risk of developing tuberculosis at pre-migration screening: a systematic review and meta-analysis. The Lancet Infectious Diseases. 2017;17(7):770–779. doi:10.1016/S1473-3099(17)30194-9.
- Long R, Asadi L, Heffernan C, et al. Is there a fundamental flaw in Canada’s post-arrival immigrant surveillance system for tuberculosis? PLOS One. 2019;14(3):e0212706. doi:10.1371/journal.pone.0212706.
- Ronald LA, Campbell JR, Rose C, et al. Estimated impact of World Health Organization latent tuberculosis screening guidelines in a region with a low tuberculosis incidence: retrospective cohort study. Clin Infect Dis. 2019;69(12):2101–2108. doi:10.1093/cid/ciz188.
- Long R, Ellis E. Public Health Agency of Canada, Canadian Lung Association, Canadian Thoracic Society. Canadian Tuberculosis Standards. 2007.
- Rutstein SE, Ananworanich J, Fidler S, et al. Clinical and public health implications of acute and early HIV detection and treatment: a scoping review. J Int AIDS Soc. 2017;20(1):21579. doi:10.7448/IAS.20.1.21579.
- Long R, Niruban S, Heffernan C, et al. A 10-year population based study of ‘opt-out’ HIV testing of tuberculosis patients in Alberta, Canada: national implications. PLoS One. 2014;9(6):e98993. doi:10.1371/journal.pone.0098993.
- Bogers SJ, Hulstein SH, Schim van der Loeff MF, et al. Current evidence on the adoption of indicator condition guided testing for HIV in western countries: A systematic review and meta-analysis. EClinicalMedicine. 2021;35:100877. doi:10.1016/j.eclinm.2021.100877.
- World Health Organization, UNAIDS, The Global Fund, PEPFAR. A Guide to Monitoring and Evaluation for Collaborative TB/HIV Activities-2015 Revisions. Geneva: WHO Press; 2015.
- Canadian Medical Association. Guidelines for the identification, investigation and treatment of individuals with concomitant tuberculosis and HIV infection. Bureau of Communicable Disease Epidemiology, Canada Department of National Health and Welfare. CMAJ. 1993;148(11):1963–1970.
- Long R, Houston S, Hershfield E. Canadian Tuberculosis Committee of the Centre for Infectious Disease P, Control P, Public Health Branch HC. Recommendations for screening and prevention of tuberculosis in patients with HIV and for screening for HIV in patients with tuberculosis and their contacts. CMAJ. 2003;169(8):789–791.
- Haworth-Brockman MJ, Keynan Y. Strengthening tuberculosis surveillance in Canada. CMAJ. 2019;191(26):E743–E744. doi:10.1503/cmaj.72225.
- Migliori GB, Nardell E, Yedilbayev A, et al. Reducing tuberculosis transmission: a consensus document from the World Health Organization Regional Office for Europe. Eur Respir J. 2019;53(6):1900391. doi:10.1183/13993003.00391-2019.
- Golub JE, Bur S, Cronin WA, et al. Delayed tuberculosis diagnosis and tuberculosis transmission. The International Journal of Tuberculosis and Lung Disease. 2006;10(1):24–30.
- Mitchison DA. Infectivity of patients with pulmonary tuberculosis during chemotherapy. Eur Respir J. 1990;3(4):385–386.
- LaFreniere M, Dam D, Strudwick L, McDermott S. Tuberculosis drug resistance in Canada: 2018. Can Commun Dis Rep. 2020;46(1):9–15. doi:10.14745/ccdr.v46i01a02.
- Benator D, Bhattacharya M, Bozeman L, et al. Rifapentine and isoniazid once a week versus rifampicin and isoniazid twice a week for treatment of drug-susceptible pulmonary tuberculosis in HIV-negative patients: a randomised clinical trial. Lancet (London, England). 2002;360(9332):528–534.
- Calderwood CJ, Wilson JP, Fielding KL, et al. Dynamics of sputum conversion during effective tuberculosis treatment: A systematic review and meta-analysis. PLOS Med. 2021;18(4):e1003566. doi:10.1371/journal.pmed.1003566.
- World Health Organization. WHA44.8 TUBERCULOSIS CONTROL PROGRAMME. 1991.
- Hargreaves JR, Boccia D, Evans CA, Adato M, Petticrew M, Porter JDH. The Social Determinants of Tuberculosis: From Evidence to Action. Am. J. Public Health. 2011;101(4):654–662. doi:10.2105/AJPH.2010.199505.
- Veen J. Microepidemics of tuberculosis: the stone-in-the-pond principle. Tuber Lung Dis. 1992;73(2):73–76. doi:10.1016/0962-8479(92)90058-R.
- Fox GJ, Dobler CC, Marks GB. Active case finding in contacts of people with tuberculosis. The Cochrane Database of Systematic Reviews. 2011;(9):CD008477. doi:10.1002/14651858.CD008477.pub2.
- National Tuberculosis Controllers A, Centers for Disease C, Prevention. Guidelines for the investigation of contacts of persons with infectious tuberculosis. Recommendations from the National Tuberculosis Controllers Association and CDC. MMWR Recomm Rep. 2005;54(RR-15):1–47.
- Luzzati R, Migliori GB, Zignol M, et al. Children under 5 years are at risk for tuberculosis after occasional contact with highly contagious patients: outbreak from a smear-positive healthcare worker. Eur Respir J. 2017;50(5):1701414. doi:10.1183/13993003.01414-2017.
- Daley CL, Small PM, Schecter GF, et al. An outbreak of tuberculosis with accelerated progression among persons infected with the human immunodeficiency virus. An analysis using restriction-fragment-length polymorphisms. The New England Journal of Medicine. 1992;326(4):231–235. doi:10.1056/NEJM199201233260404.
- Canada PHAo. Chapter 12: Canadian Tuberculosis Standards 7th Edition: 2014 – Contact follow-up and outbreak management in Tuberculosis control. Published 2014. https://www.canada.ca/en/public-health/services/infectious-diseases/canadian-tuberculosis-standards-7th-edition/edition-8.html. Accessed February 17, 2014.
- Ai J-W, Ruan Q-L, Liu Q-H, Zhang W-H. Updates on the risk factors for latent tuberculosis reactivation and their managements. Emerging Microbes Infect. 2016;5(2):e10. doi:10.1038/emi.2016.10.
- Fox GJ, Dobler CC, Marais BJ, Denholm JT. Preventive therapy for latent tuberculosis infection—the promise and the challenges. International Journal of Infectious Diseases. 2017;56:68–76. doi:10.1016/j.ijid.2016.11.006.
- Rangaka MX, Cavalcante SC, Marais BJ, et al. Controlling the seedbeds of tuberculosis: diagnosis and treatment of tuberculosis infection. Lancet. 2015;386(10010):2344–2353. doi:10.1016/S0140-6736(15)00323-2.
- Dobler CC, Martin A, Marks GB. Benefit of treatment of latent tuberculosis infection in individual patients. European Respiratory Journal. 2015;46(5):1397–1406. doi:10.1183/13993003.00577-2015.
- Kim HW, Kim JS. Treatment of Latent Tuberculosis Infection and Its Clinical Efficacy. Tuberculosis and Respiratory Diseases. 2018;81(1):6–12. doi:10.4046/trd.2017.0052.
- Comstock GW, Edwards PQ. The competing risks of tuberculosis and hepatitis for adult tuberculin reactors. Am Rev Respir Dis. 1975;111(5):573–577. doi:10.1164/arrd.1975.111.5.573.
- Menzies D, Adjobimey M, Ruslami R, et al. Four months of rifampin or nine months of isoniazid for latent tuberculosis in adults. N Engl J Med. 2018;379(5):440–453. doi:10.1056/NEJMoa1714283.
- Macaraig MM, Jalees M, Lam C, Burzynski J. Improved treatment completion with shorter treatment regimens for latent tuberculous infection. Int j Tuberc Lung Dis. 2018;22(11):1344–1349. doi:10.5588/ijtld.18.0035.
- Ferebee SH, Mount FW. Tuberculosis Morbidity in a Controlled Trial of the Prophylactic Use of Isoniazid among Household Contacts. American Review of Respiratory Disease. 1962;85(4):490–510.
- Molhave M, Wejse C. Historical review of studies on the effect of treating latent tuberculosis. Int J Infect Dis. 2020;92S:S31–S36. doi:10.1016/j.ijid.2020.03.011.
Appendix 1:
Monitoring tuberculosis program performance
The framework for monitoring tuberculosis program performance outlined in Chapter 15 consists of 12 program performance indicators; a rationale for each is provided below along with international and national history of use or recommendation precedents. As in the text, in 2018, the National Collaborating Center for Infectious Diseases performed a scoping review of TB program performance indicators in epidemiologically similar settings (high-income, low-TB incidence) coupled with general global recommendations. Indicators were selected from this review. As shown in the following data, more recent recommendations and strategies have been reviewed in preparation of this chapter for a history of use. This list of prior use/recommendation is representative, and not exhaustive.
Table 2. Calculating and presenting TB program performance indicators.
