ABSTRACT
Background: Coronary artery disease (CAD) is common in aortic stenosis patients, but its proper management in the setting of transcatheter aortic valve replacement (TAVR) is not established. We sought to explore whether the extent of revascularization by percutaneous coronary intervention (PCI) has an impact on clinical outcomes after TAVR.
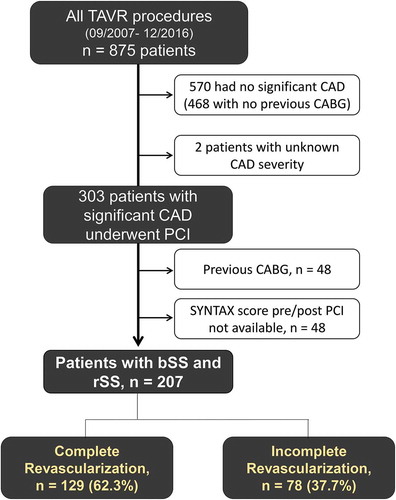
Methods: Out of 875 consecutive patients, 303 underwent PCI prior to TAVR. Baseline (pre-PCI) and residual (post-PCI) SYNTAX score (bSS and rSS), as well as their ratio (SYNTAX revascularization index, SRI) were calculated for 207 patients who underwent PCI for native CAD at a median of four days before TAVR. The endpoints were the 30-day safety endpoint (VARC-2 definition) and 1-year mortality.
Results: In patients undergoing PCI prior to TAVR, bSS was 11.0 ± 7.2, rSS was 2.8 ± 5.3, and SRI was 81.7 ± 27.9%. Complete revascularization (rSS = 0 and SRI = 100%) was achieved in 129 patients (62.3%). The rate of the 30-day safety endpoint was influenced by the STS score and the bSS, but not by the completeness of coronary revascularization. At one year post-TAVR, complete revascularization was associated with a lower mortality (adjusted HR, 0.450 [0.218–0.926], p = 0.030). This mortality advantage was more evident in patients with multivessel CAD (n = 130; HR, 0.304 [0.120–0.772]) than in patients with single-vessel CAD (n = 77; HR, 0.752 [0.207–2.731]).
Conclusions: In patients with CAD undergoing TAVR, complete percutaneous coronary revascularization is safe and associated with lower one-year mortality, especially in patients with multivessel CAD.
Introduction
Sharing similar pathophysiology and risk factors, coronary artery disease (CAD) and aortic stenosis (AS) commonly coexist in patients referred for surgical or transcatheter aortic valve replacement (TAVR).Citation1–Citation3 Non-revascularized CAD is associated with increased earlyCitation4 and lateCitation5,Citation6 mortality after aortic valve replacement, while coronary artery bypass grafting (CABG) reduces this risk if performed concomitantly with valve replacement.Citation7,Citation8 CABG is, therefore, recommended in patients undergoing aortic valve replacement who have ≥50–70% reduction in luminal diameter of one or more of the major coronary arteries.Citation8,Citation9 On the other hand, previous studies did not show a similar advantage of percutaneous coronary intervention (PCI) performed in the setting of TAVR.Citation10 Unlike CABG, which typically and most commonly leads to complete revascularization of all obstructive coronary lesions, PCI may lead to variable degrees of revascularization. Indeed, previous studies have shown that complete revascularization is seldom achieved in patients undergoing PCI prior to TAVR.Citation11,Citation12
Additionally, the inconsistency of data on the prognostic value of CAD in patients undergoing TAVRCitation3,Citation13 is in part ascribed to the way the severity and completeness of treatment of CAD are defined in previous studies. The Synergy between PCI with Taxus and Cardiac Surgery (SYNTAX) score serves to objectively quantify the burden of CAD, while its derivatives (the residual SYNTAX score and the SYNTAX revascularization index) are established measures of the extent of coronary revascularization.Citation14
The primary objective of the present study was to compare the outcomes of patients undergoing PCI prior to TAVR stratified according to the extent of revascularization as quantified by the residual SYNTAX score.
Materials and methods
This is a retrospective analysis of 875 consecutive patients enrolled in our prospective TAVR registry (NCT03192774) in the period from September 2007 to December 2016. The registry was approved by the local ethics committee, and each patient has provided a written informed consent for analysis of anonymized data. Eligibility for TAVR was determined by the local heart team, taking into account the patient’s age, operative risk (based on established operative risk scores as well as other comorbidities not included in the scores), anatomical considerations, life expectancy, and the likelihood that TAVR would lead to a significant clinical improvement.
Pre-TAVR assessment routinely included coronary angiography. All angiograms were reviewed by the Heart Team, which made the decision of whether coronary intervention was required before/with TAVR or not. In general, patients with significant stenosis of a major epicardial coronary artery were considered for PCI staged (before) or concomitant (in the same session) with TAVR. The choice between staged vs. concomitant PCI was based on the size of the perfused myocardium and the expected complexity of the intervention, as well as the clinical status.
Coronary angiography analysis
In all patients with obstructive CAD (defined as ≥50% stenosis of at least one epicardial coronary artery measuring ≥1.5 mm), the SYNTAX score (SS) was calculated. In brief, each significant lesion was defined based on the modified American Heart Association coronary tree segment classification and separately scored considering bifurcation/trifurcation, aortic ostial location, chronic occlusion, vessel tortuosity, lesion length and calcification, as well as thrombus formation. Finally, the scores of all lesions were added to obtain the patient’s raw SYNTAX score.Citation15 For patients who underwent PCI staged (within three months) before or concomitant with TAVR, the SS was calculated before (baseline SYNTAX score, bSS) and after PCI (residual SYNTAX score, rSS).Citation16 In addition to the rSS (postulated to represent the burden of residual obstructive CAD post revascularizationCitation16), the SYNTAX revascularization index (SRI = [ΔSS/bSS] × 100) was calculated to represent the proportion of CAD burden successfully eliminated by revascularization.Citation17 Complete revascularization was defined as an rSS of 0 (corresponding to an SRI of 100%) while incomplete revascularization was defined as rSS >0. In 20 randomly-selected patients, SS was measured by two observers blinded to each other’s assessment. The intraclass correlation coefficient of both measurements was 0.95 (95% confidence interval: 0.87–0.98).
The following subgroups were considered as having “no significant CAD”: 1) no angiographic evidence of CAD; 2) CAD without obstructive lesions; 3) patients with obstructive CAD, yet considered not significantly contributing to patient’s symptoms (n = 99; SS = 3.0 [0.0–7.0]). Patients with no significant CAD served as a control group, and patients who underwent PCI were compared to that group. Patients with prior CABG, as well as those whose angiograms were not available (i.e. only report is available), were excluded from this analysis (). Adverse events were assessed in hospital, and regular clinical follow-up was performed at 30 days, 6 and 12 months, and yearly thereafter.
Study endpoints
The primary endpoint of the present study was all-cause mortality at one year. Secondary endpoints were 1) the Valve Academic Research Consortium (VARC) early safety endpoint; a composite of all-cause mortality, all stroke, life-threatening bleeding, acute kidney injury, coronary artery obstruction requiring intervention, major vascular complication, and valve-related dysfunction requiring repeat procedure,Citation18 2) the individual VARC safety endpoints, and 3) spontaneous and periprocedural myocardial infarction (MI) occurring within 72 hours post-TAVR applying the VARC definitions.Citation18
Statistical analysis
Qualitative variables are summarized as frequencies and percentages, while quantitative variables are summarized as mean±SD or median [25th – 75th quartiles], depending on variable distribution. Inter-group comparisons were conducted using Student’s t-test for continuous variables. For categorical variables, inter-group comparison was conducted using chi-square test and trends were tested using linear-by-linear association. Survival curves were created using the Kaplan–Meier method, and compared using log-rank and Cox proportional hazard regression analyses. For the latter, the hazard ratio (HR) and the 95% confidence interval (CI) are presented. Multivariable binary logistic regression analysis was performed using entry criteria of p < 0.05 in univariable analysis and backward elimination, and the odds ratio (OR) and the 95% CI are presented. Data analysis was performed using SPSS V.24.0 (IBM Corp., New York, USA).
Results
The study included 875 consecutive patients undergoing TAVR; predominantly through a transfemoral approach (n = 856, 97.8%). The Medtronic CoreValve and Evolut R devices were implanted in 343 patients, the Edwards Sapien XT and Sapien 3 devices in 414, the Boston Scientific Lotus valve in 89, and other devices in the rest.
Over the study period (2007–2016), we observed a relatively higher prevalence of CAD, previous MI, and previous PCI in the earlier than the later patient quartiles. While the rate of peri-TAVR PCI performance was highest in the first quartile, there was a trend toward more complete percutaneous revascularization in the latest patient quartile (Figure S1).
In 303 patients with significant CAD, PCI was performed either staged (within three months) before or concomitant with TAVR (). Table S1 compares the baseline and periprocedural characteristics and Table S2 summarizes early safety outcomes of patients who underwent PCI vs. those who did not. Patients who underwent PCI did not have an increased risk of the composite safety endpoint at 30 days post-TAVR. Importantly, the rates of acute kidney injury and life-threatening bleeding were not increased. Patients who underwent PCI had a higher prevalence of peripheral arterial disease (20.8% vs. 14.2%, p = 0.016) and more frequently had major vascular complications after TAVR (7.6% vs. 3.3%, p = 0.007).
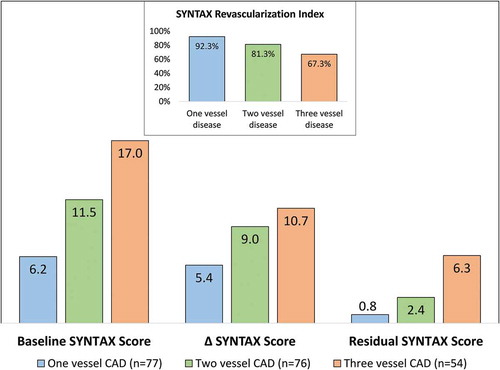
Out of those who underwent PCI, bSS and rSS were calculated in 207 patients (age, 81.6 ± 6.1 years; STS score, 6.6 ± 5.6, follow up time 731 [364–1214] days after TAVR) (). In these patients, PCI was performed concomitant with TAVR in 29.1% of cases and staged (at a median of 4 [IQR: 0–8] days before TAVR) in the rest; with no difference in early safety outcomes between concomitant vs. staged PCI. The bSS was 11.0 ± 7.2, while the rSS was 2.8 ± 5.3. The ∆ SYNTAX Score (∆SS) was 8.1 ± 5.6 corresponding to an SRI of 81.7 ± 27.9%.
The impact of the extent of revascularization on clinical outcomes
Complete revascularization (i.e. rSS = 0 and SRI = 100%) was achieved in 129 patients (62.3%), while the rSS and the SRI were 7.5 ± 6.2 and 51.6 ± 24.4% in those with incomplete revascularization. compares the baseline and periprocedural characteristics of patients with complete vs. incomplete revascularization. Patients with incomplete revascularization had a more severe CAD (more multivessel disease, 82.0% vs. 51.2%; and a higher bSS, 15.6 ± 7.5 vs. 8.1 ± 5.3; p < 0.001) and a lower left ventricular ejection fraction (LVEF: 49.6 ± 14.4 vs. 55.0 ± 12.7%, p = 0.009). The frequency of left main or left main-equivalent as well as of proximal left anterior descending CAD was not different between the two groups. Although ∆SS was similar in both groups (8.1 ± 5.9 vs. 8.1 ± 5.3), this corresponded to a smaller SRI in the incomplete (51.6 ± 24.4%) than in the complete revascularization group (100%). summarizes early safety outcomes of the two groups. Patients in whom complete revascularization was achieved had a lower risk of the composite early safety endpoint as compared to those with incomplete revascularization (24.8% vs. 39.7%, p = 0.029; OR: 0.50 [0.273–0.915]). On multivariable analysis, the correlation between complete revascularization and early safety endpoint was no more significant (OR: 0.705 [0.341–1.457], p = 0.345), while STS score (OR: 1.088 [1.025–1.155], p = 0.005) and bSS (OR: 1.048 [1.004–1.095], p = 0.031) emerged as independent determinants of the risk of the early safety endpoint.
Table 1. Baseline and periprocedural characteristics of patients with complete vs. incomplete coronary revascularization
Table 2. Thirty-day safety endpoints after TAVR in patients with complete vs. incomplete coronary revascularization*
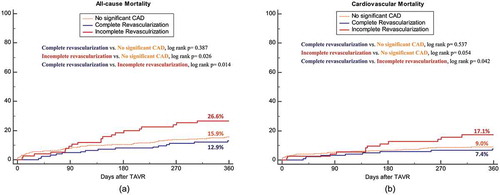
At one year post-TAVR, complete revascularization was associated with a lower all-cause mortality (12.9% vs. 26.6%, log rank p = 0.014; HR: 0.45 [0.23–0.86]) and cardiovascular mortality (7.4% vs. 17.1%, log rank p = 0.042; HR: 0.42[0.18–0.998]) ( and ). Those with complete revascularization had a comparable one year survival to patients with no significant CAD, while those with incomplete revascularization had an increased mortality ( and ). On multivariable analysis, complete revascularization was associated with reduced mortality (HR: 0.450 [0.218–0.926], p = 0.030) after accounting for baseline differences in clinical characteristics (reduced left ventricular ejection fraction, HR: 1.436 [0.673–3.063]; low gradient severe aortic stenosis, HR: 1.616 [0.768–3.401]; and bSS, HR: 0.996 [0.941–1.055]) as well as the quartile of year of the procedure (p = 0.864). As continuous variables, rSS and SRI were associated with one-year mortality while bSS and ∆SS were not ().
Table 3. Coronary artery disease characteristics associated with one year mortality among patients undergoing PCI peri-TAVR
Single vs. multivessel CAD
shows the burden of CAD at baseline (bSS), the extent of revascularization (as an absolute [∆SS] and relative [SRI] SS reduction), as well as the residual CAD burden (rSS) in patients with one, two, and three vessel CAD undergoing PCI. Although patients with multivessel CAD had a higher ∆SS, this was relatively lower in relation to the higher bSS in that group (i.e. corresponding to a lower SRI). Accordingly, patients with multivessel CAD had a higher rSS than patients with single vessel CAD. Complete revascularization was achieved in 81.8%, 60.5%, and 37.0% of patients with single, two, and three vessel disease, respectively. In the subgroup of patients with single vessel disease (n = 77), completeness of revascularization did not have a significant impact on one year mortality (16.4% vs. 21.4% in complete vs. incomplete revascularization, p = 0.663; HR: 0.752[0.207–2.731]). On the other hand in patients with multivessel disease (n = 130), complete revascularization was associated with a significantly lower one year mortality (9.7% vs. 27.8%, p = 0.008; HR: 0.304 [0.120–0.772]) (Figure S2).
Discussion
The main finding of the present study is that revascularization of significant coronary artery stenoses in patients undergoing TAVR is: 1) safe (posing no increased peri-procedural risks); and 2) associated with a survival benefit in the mid-term, especially in patients with multivessel CAD.
The clinical advantage of coronary revascularization prior to TAVR, if established, has to be weighed against the potential increase in the risks of kidney injury, vascular complications, stent thrombosis, and bleeding complications. Early safety endpoints were actually less frequent in patients with complete revascularization. However, multivariable analysis revealed that complete revascularization per se is not the reason for this observation, but rather the lower STS score and bSS in this group. Complete revascularization had a positive impact on mid-term survival, independent of bSS and LV function. Survival of patients with complete revascularization was comparable to patients with no significant CAD. Patients with multivessel CAD achieved the most remarkable benefit, suggesting that a strategy of complete peri-TAVR revascularization should be considered in this group of patients.
While bSS impacted early safety outcomes, we found no impact of bSS or ∆SS on one-year mortality. On the other hand, both SRI and rSS had a significant prognostic value in the mid-term. This implies that regardless of the complexity of CAD at baseline and the absolute extent of revascularization, the mid-term prognosis is rather influenced by the ratio of treated to untreated burden of CAD.
In our cohort, patients with reduced LVEF were less likely offered complete revascularization (49% vs. 68% in patients with preserved LVEF), reflecting the tendency of the operator to be more conservative/to accept suboptimal results in this patient subset. This appears, however, to be a suboptimal strategy as those patients have been shown in a large meta-analysis to get a survival benefit from interventional (as compared to conservative) treatment and especially from CABG (which typically provides complete revascularization).Citation19
PCI and the extent of revascularization in patients undergoing TAVR, what the evidence shows
PCI in patients undergoing TAVR
In a meta-analysis by Kotronias et al., patients who underwent PCI prior to TAVR were compared to patients who underwent TAVR without PCI.Citation10 Major vascular complications and 30-day mortality were more common in patients who underwent pre-TAVR PCI, while other 30-day outcomes, as well as one-year mortality were not different between the two groups. Although the analysis included nine studies, the association between pre-TAVR PCI and higher 30-day mortality was driven by a single studyCitation20 in which patients who had PCI more commonly presented with cardiogenic shock and cardiac arrest. Sensitivity analysis excluding this study turned out similar outcomes between patients with vs. without PCI pre-TAVR.
In our cohort, PCI was not associated with increased incidence of the composite early safety endpoint. However, the incidence of major vascular complications was higher in patients who underwent PCI. Although the higher incidence of vascular complications can be explained by the significantly higher prevalence of peripheral arterial disease in patients who underwent PCI, careful management of the puncture sites is warranted in these patients, aiming at prevention and early detection of vascular complications. It should also be noted that most PCIs in this cohort were conducted through a transfemoral access, and whether a transradial approach strategy would have decreased the risk of post-TAVR vascular complications is unknown.
Overall, the comparison of patients undergoing PCI prior to TAVR vs. TAVR without PCI has a limited clinical relevance when run in a non-randomized setting, as PCI is usually performed in patients with more severe CAD and larger myocardial ischemia. Moreover, pooling all patients who underwent PCI together is rather inappropriate, as the severity of CAD and the extent of revascularization achieved are quite different between patients. On the other hand, determining the extent of revascularization to be targeted when PCI is to be performed in the setting of TAVR is of a significant clinical value.
Complete revascularization in patients undergoing TAVR
In a meta-analysis by Witberg et al, the impact of completeness of revascularization on the outcomes of patients undergoing PCI prior to TAVR was investigated (6 studies, 3107 patients).Citation21 The included studies used different cut-points of rSS (zero,Citation11 three,Citation12 eight,Citation22,Citation23 nine,Citation24 or fourteenCitation25) to classify the extent of revascularization. Patients with more complete revascularization (indicated by a lower rSS) had a lower mortality in the mid-term (0.7 to 3 years) after TAVR. In line with those results, we found a positive impact of complete revascularization—especially of multivessel CAD- on mid-term outcomes, without increasing the periprocedural risk.
Previous studies have demonstrated the overall advantage of complete revascularization in patients with CAD especially those with multivessel disease, being associated with lower long-term mortality, myocardial infarction, and repeat revascularization.Citation26 The nuclear substudy of the COURAGE (Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation) trial demonstrated that the risk of death or myocardial infarction is lowered when ischemia burden is reduced, particularly if baseline ischemia was moderate to severe, and that the risk is eliminated in those with no residual ischemia.Citation27 In a pooled analysis from randomized trials of left main or multivessel CAD revascularization, PCI resulting in complete revascularization was associated with a similar long-term survival to CABG resulting in complete revascularization, while the risk was elevated after PCI with incomplete revascularization.Citation28 The authors suggested that the ability to achieve complete revascularization should be considered in the choice of revascularization strategy, and this has been recently adopted by the European coronary revascularization guidelines, recommending that completeness of revascularization is to be prioritized when considering the decision between CABG and PCI.Citation29
Limitations
Data are derived from a retrospective analysis of prospectively collected data, rather than from a randomized study. Allocation of a given patient into the complete vs. incomplete revascularization group is influenced by the clinical status and the operator’s preference and experience, and this might have introduced some bias into the results. Only prospective randomized trials can eliminate such a potential bias. Additionally, functional assessment of coronary lesions was not performed and the anatomical SS was not core-lab adjudicated. Although our study is one of the largest studies of patients undergoing PCI peri-TAVR, it remains relatively small, especially the single vessel CAD subgroup. This calls for careful interpretation of the results of this group, as well as for conducting larger prospective studies in this field. The study represents a broad period of the TAVR experience which included significant evolution of TAVR techniques and technology as well as potential change in revascularization thresholds over the years of the analysis. Future prospective large scale studies confined to a specific time frame would better avoid these biases. Finally, post-CABG patients were excluded from the study and extrapolating our conclusions to this population should be avoided.
Conclusion
Revascularization of significant native coronary artery stenoses in patients undergoing TAVR is safe may confer a survival benefit in the mid-term, especially in patients with multivessel CAD.
Supplemental Material
Download Zip (1.9 MB)Disclosure statement
Drs. Richardt and Abdel-Wahab have received institutional research grants from St. Jude Medical, Biotronik and Medtronic. Dr. Abdel-Wahab is a proctor for Boston Scientific. The other authors have no conflicts of interest to declare.
Supplementary data
Supplemental data for this article can be accessed here.
Additional information
Funding
References
- Vandeplas A, Willems JL, Piessens J, De Geest H. Frequency of angina pectoris and coronary artery disease in severe isolated valvular aortic stenosis. Am J Cardiol. July 1, 1988;62:117–400.
- Stewart BF, Siscovick D, Lind BK, et al. Clinical factors associated with calcific aortic valve disease. Cardiovascular health study. J Am Coll Cardiol. 1997 March 1;29:630–634.
- D’Ascenzo F, Conrotto F, Giordana F, et al. Mid-term prognostic value of coronary artery disease in patients undergoing transcatheter aortic valve implantation: a meta-analysis of adjusted observational results. Int J Cardiol. October 3 2013;168:2528–2532. doi:10.1016/j.ijcard.2013.03.062.
- Tjang YS, van Hees Y, Korfer R, Grobbee DE, van der Heijden GJ. Predictors of mortality after aortic valve replacement. Eur J Cardiothorac Surg. September 2007;32:469–474. doi:10.1016/j.ejcts.2007.06.012.
- Lund O, Nielsen TT, Pilegaard HK, Magnussen K, Knudsen MA. The influence of coronary artery disease and bypass grafting on early and late survival after valve replacement for aortic stenosis. J Thorac Cardiovasc Surg. September 1990;100:327–337.
- Mullany CJ, Elveback LR, Frye RL, et al. Coronary artery disease and its management: influence on survival in patients undergoing aortic valve replacement. J Am Coll Cardiol. July 1987;10:66–72.
- Thalji NM, Suri RM, Daly RC, et al. The prognostic impact of concomitant coronary artery bypass grafting during aortic valve surgery: implications for revascularization in the transcatheter era. J Thorac Cardiovasc Surg. February 2015;149:451–460. doi:10.1016/j.jtcvs.2014.08.073.
- Nishimura RA, Otto CM, Bonow RO, et al. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: executive summary: a report of the American college of cardiology/American heart association task force on practice guidelines. Circulation. June 10 2014;129:2440–2492. doi:10.1161/CIR.0000000000000029.
- Bonow RO, Carabello BA, Kanu C, et al. ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American college of cardiology/American Heart association task force on practice guidelines (writing committee to revise the 1998 guidelines for the management of patients with valvular heart disease): developed in collaboration with the society of cardiovascular anesthesiologists: endorsed by the society for cardiovascular angiography and interventions and the society of thoracic surgeons. Circulation. August 1 2006;114:e84–231. doi:10.1161/CIRCULATIONAHA.106.176857.
- Kotronias RA, Kwok CS, George S, et al. Transcatheter aortic valve implantation with or without percutaneous coronary artery revascularization strategy: a systematic review and meta-analysis. J Am Heart Assoc. 2017 June 27;6. doi:10.1161/JAHA.117.005960.
- Van Mieghem NM, van der Boon RM, Faqiri E, et al. Complete revascularization is not a prerequisite for success in current transcatheter aortic valve implantation practice. JACC Cardiovasc Interv. August 2013;6:867–875. doi:10.1016/j.jcin.2013.04.015.
- Shamekhi J, Stundl A, Weber M, et al. Impact of coronary artery disease in patients undergoing transfemoral transcatheter aortic valve implantation. Int J Cardiol. October 15 2017;245:215–221. doi:10.1016/j.ijcard.2017.07.082.
- Sankaramangalam K, Banerjee K, Kandregula K, et al. Impact of coronary artery disease on 30-day and 1-year mortality in patients undergoing transcatheter aortic valve replacement: a meta-analysis. J Am Heart Assoc. 2017 October 11;6. doi:10.1161/JAHA.117.006092.
- Farooq V, Head SJ, Kappetein AP, Serruys PW. Widening clinical applications of the SYNTAX score. Heart. February 2014;100:276–287. doi:10.1136/heartjnl-2013-304273.
- Serruys PW, Morice MC, Kappetein AP, et al. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med. March 5 2009;360:961–972. doi:10.1056/NEJMoa0804626.
- Farooq V, Serruys PW, Bourantas CV, et al. Quantification of incomplete revascularization and its association with five-year mortality in the synergy between percutaneous coronary intervention with taxus and cardiac surgery (SYNTAX) trial validation of the residual SYNTAX score. Circulation. July 9 2013;128:141–151. doi:10.1161/CIRCULATIONAHA.113.001803.
- Genereux P, Campos CM, Yadav M, et al. Reasonable incomplete revascularisation after percutaneous coronary intervention: the SYNTAX revascularisation index. EuroIntervention. October 2015;11:634–642. doi:10.4244/EIJY14M10_05.
- Kappetein AP, Head SJ, Genereux P, et al. Updated standardized endpoint definitions for transcatheter aortic valve implantation: the valve academic research consortium-2 consensus document (VARC-2). Eur J Cardiothorac Surg. November 2012;42:S45–60. doi:10.1093/ejcts/ezs533.
- Wolff G, Dimitroulis D, Andreotti F, et al. Survival benefits of invasive versus conservative strategies in heart failure in patients with reduced ejection fraction and coronary artery disease: a meta-analysis. Circ Heart Fail. 2017 January;10. doi:10.1161/CIRCHEARTFAILURE.116.003255.
- Singh V, Rodriguez AP, Thakkar B, et al. Comparison of outcomes of transcatheter aortic valve replacement plus percutaneous coronary intervention versus transcatheter aortic valve replacement alone in the United States. Am J Cardiol. December 1 2016;118:1698–1704. doi:10.1016/j.amjcard.2016.08.048.
- Witberg G, Zusman O, Codner P, Assali A, Kornowski R. Impact of coronary artery revascularization completeness on outcomes of patients with coronary artery disease undergoing transcatheter aortic valve replacement: a meta-analysis of studies using the residual SYNTAX score (Synergy Between PCI With Taxus and Cardiac Surgery). Circ Cardiovasc Interv. March 2018;11:e006000. doi:10.1161/CIRCINTERVENTIONS.118.006388.
- Witberg G, Regev E, Chen S, et al. The prognostic effects of coronary disease severity and completeness of revascularization on mortality in patients undergoing transcatheter aortic valve replacement. JACC Cardiovasc Interv. July 24 2017;10:1428–1435. doi:10.1016/j.jcin.2017.04.035.
- Paradis JM, White JM, Genereux P, et al. Impact of coronary artery disease severity assessed with the SYNTAX score on outcomes following transcatheter aortic valve replacement. J Am Heart Assoc. 2017 February 20;6. doi:10.1161/JAHA.116.005070.
- Khawaja MZ, Asrress KN, Haran H, et al. The effect of coronary artery disease defined by quantitative coronary angiography and SYNTAX score upon outcome after transcatheter aortic valve implantation (TAVI) using the edwards bioprosthesis. EuroIntervention. August 2015;11:450–455. doi:10.4244/EIJY14M05_09.
- Stefanini GG, Stortecky S, Cao D, et al. Coronary artery disease severity and aortic stenosis: clinical outcomes according to SYNTAX score in patients undergoing transcatheter aortic valve implantation. Eur Heart J. October 1 2014;35:2530–2540. doi:10.1093/eurheartj/ehu074.
- Garcia S, Sandoval Y, Roukoz H, et al. Outcomes after complete versus incomplete revascularization of patients with multivessel coronary artery disease: a meta-analysis of 89,883 patients enrolled in randomized clinical trials and observational studies. J Am Coll Cardiol. October 15 2013;62:1421–1431. doi:10.1016/j.jacc.2013.05.033.
- Shaw LJ, Berman DS, Maron DJ, et al. Optimal medical therapy with or without percutaneous coronary intervention to reduce ischemic burden: results from the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial nuclear substudy. Circulation. March 11 2008;117:1283–1291. doi:10.1161/CIRCULATIONAHA.107.743963.
- Ahn JM, Park DW, Lee CW, et al. Comparison of stenting versus bypass surgery according to the completeness of revascularization in severe coronary artery disease: patient-level pooled analysis of the SYNTAX, PRECOMBAT, and BEST trials. JACC Cardiovasc Interv. July 24 2017;10:1415–1424. doi:10.1016/j.jcin.2017.04.037.
- Neumann FJ, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS guidelines on myocardial revascularization. Eur Heart J. 2018 August 25. doi:10.1093/eurheartj/ehy658.