ABSTRACT
AIM: Sleep disorders can affect behaviours and social skills through various different mechanisms. The purpose of this study was to determine whether or not sleep habits can be used as a marker for social competence and behaviour in early childhood in the context of neurodevelopmental disorders.
METHODS: Three hundred seventeen children aged 4–6 years were enrolled. Our case group consisted of 166 children with neurodevelopmental disorder and our control group of 151 healthy children. Participants were administered Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5)-based psychiatric evaluation, a data form, the Social Competence and Behavior Evaluation scale (SCBE-30), the Denver Developmental Screening Test II (DDST-II), and the Children’s Sleep Habits Questionnaire (CSHQ). Data obtained from scale scores and psychiatric examination results were subjected to statistical analysis.
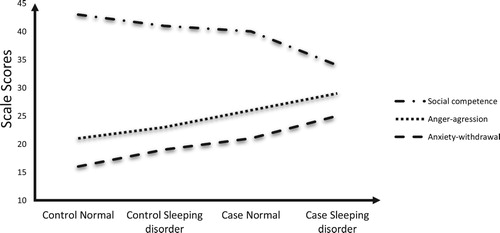
RESULTS: The mean CSHQ score in the case group was significantly higher than in the control group (p < 0.001). The case group social competence score was significantly lower and anxiety-withdrawal and anger-aggression scores were significantly higher than in the control group (p < 0.001). Male subjects attained lower social competence scale scores. Social competence was higher in the group receiving pre-school education, while anger-aggression and anxiety-withdrawal were lower. Correlation analysis revealed that social competence decreased in line with sleep habits scores, while anger-aggression and anxiety-withdrawal increased.
CONCLUSIONS: Social competence scores decreased in line with sleep habits scores, while anger-aggression and anxiety-withdrawal scores increased. It may be beneficial to approach sleep habits as a potential marker of social competence, aggressive, and anxious behaviours and neurodevelopmental disorders in pre-school children, and to intervene early.
Introduction
Infants and young children spend the majority of their time asleep. In addition to processes such as normal growth and development, tissue renewal, and immune system functions, sleep is also important for memory, central nervous system repair, and cognitive, behavioural, and emotional functions [Citation1]. Sleep problems are reported in 25% of pre-school children. Previous population-based studies have shown a significant association between sleep problems in childhood and emotional or behavioural problems [Citation2]. Sleep disorders are frequently determined in young children presenting to paediatric psychiatric polyclinics. Sleep problems have been observed to be associated with the intensity of psychiatric symptoms, and also to increase the risk of such symptoms [Citation3]. Psychiatric disorders and sleep disorders are frequently comorbid, and this relationship is probably a two-way one [Citation4]. The individual’s sleep physiology is also thought to be linked to the risk of long-term psychopathology [Citation5]. Children with sleep problems experience more difficulties with emotional and attentional regulation and adjustment to school than those without such problems [Citation6]. Sleep problems are another condition shown to have an adverse impact on mental and verbal skills, daily living skills, socialization skills, and motor development, particularly in children with neurodevelopmental disorder [Citation7].
Social competence in children is defined as the ability to establish effective social relations with peers, family members, and people in their environment, such as other adults, and to use social skills in an adaptive manner [Citation8]. Pre-school socially competent behaviours are shaped around positive participation and self-regulation skills during interaction with peers [Citation9]. More than 40% of pre-school children have exhibited some sensitivities in early social-emotional health. Disorders that commence during this period are known to be capable of persisting for the child’s lifetime [Citation10]. Socially competent kindergarten children are more successful than less competent peers in developing positive attitudes to school, and in achieving good grades and success [Citation9]. Important links have been determined between a child’s emotional regulation skills and increasing social competence, and anger-aggression and difficulties with emotional regulation impair social competence [Citation9,Citation11]. Low social competence in early childhood can have adverse impacts on exclusion and interiorization in late childhood and early adolescence [Citation12]. Socially competent children are successful at school and have high self-esteem, thus laying a strong long-term foundation. The risks of behavioural problems, substance dependence, poor school adaptation, violence, juvenile criminality, and antisocial behaviour increase in children with deficiencies in social competence unable to achieve these [Citation11].
Sleep is not static. It undergoes a constant change from the foetal period to adult life, with the most rapid change occurring in the first 6 months of life. These changes are associated with appropriate maturation of the relevant neural pathways, and normal sleep development will not occur in the absence of normal brain development [Citation13]. Neurodevelopmental disorders are a disease group whose findings are characterized by impaired acquisition of cognitive, behavioural, and social skills during the developmental period [Citation14]. Sleep disorders are generally more common in children with neurodevelopmental disorder than in healthy children [Citation15]. Optimal brain development is thought to be related to the individual’s circadian rhythm [Citation16].
Sleep is described as linked to social competence, behaviour, and neurodevelopment in the previous literature. The purpose of our study was to investigate whether sleep habits can be used as a marker of social competence and behaviour in early childhood.
Methods
The research was planned as a prospective case-control study. Ethical committee approval was granted on 29 May 2017 (no. 2017-04-06). Three hundred fifty subjects were enrolled between June 2017 and February 2018. When those dropping out of their own volition and failing to complete the study were excluded, the research was finally conducted with 317 subjects. Following approval from the local ethical committee, participants were enrolled from among children presenting to the hospital. One hundred sixty-six children aged 4–6 with psychiatric disease and 151 healthy children with no disease were enrolled on a voluntary basis. The control consisted of patients with no active psychiatric symptoms presenting to the Healthy Child Clinic. Patients, control group subjects, and parents were read the consent form and provided written informed consent. A data form consisting of structured multiple-choice questions to be answered in written and prepared by specialist psychiatrists was used to determine cases’ sociodemographic and clinical characteristics. These forms were completed by physicians. Subjects with chronic disease other than known psychiatric disease and with parents lacing a sufficient level of education to permit healthy reading and completion of the inventories were excluded. The case group consisted of patients diagnosed by a psychiatrist at DSM-5-based psychiatric evaluation. Absence of any diagnosis in the control group was also confirmed through a psychiatric evaluation.
Psychometric instruments
The SCBE-30 was applied to all subjects. This scale consists of three subscales containing 10 questions each assessing children’s problem symptoms and social skills in the pre-school period. The social competence subscale examines positive characteristics such as cooperation in the company of peers seeking means of resolving disagreements. The anger-aggression subscale examines problem symptoms such as defiance of adults and externalizing such as inappropriate and aggressive behaviour in relations with peers. The anxiety-withdrawal subscale examines internalizing problem symptoms such as sadness and depression and timidity within a group [Citation17]. The validity and reliability of the Turkish-language version have been confirmed [Citation18].
The Children’s Sleep Habits Questionnaire (CSHQ) investigating children’s sleep habits and sleep-related problems was administered to all subjects. Developed by Owens et al., the CSHQ is regarded as a sleep screening tool useful for determining behavioural and medically based sleep problems [Citation19]. It consists of 33 questions and assesses bedtime resistance, sleep onset delay, sleep duration, sleep anxiety, night wakings, parasomnias, sleep disordered breathing and daytime wakefulness. The inventory is completed retrospectively by the mother and father. A total score of 41 is regarded as a cut-off point, and values above these are considered “clinically significant.” The validity and reliability of the Turkish-language version were studied by Perdahlı Fiş et al. [Citation20].
The Denver Developmental Screening Test II (DDST-II) was applied to the case group. Denver II is the 1992 revision of the Denver Developmental Screening Test [Citation21]. The test has been adapted and standardized to Turkish society and is used to determine developmental problems that may be encountered in children. The test can be applied to children up to the age of 6 and evaluates fine motor skills, gross motor skills, language skills, and social skills [Citation22].
Statistical analysis
Descriptive statistics (mean, standard deviation, minimum, median, and maximum) were used to describe continuous variables. The Mann–Whitney U test was used to compare two independent and non-normally distributed continuous variables. Presence of correlation between scores representing continuous variables was assessed using Spearman’s Rho correlation coefficient. The Kruskal–Wallis H test was used to compare continuous variables in more than two groups. Two-way evaluations of groups with statistical significance were performed using Dunn’s multiple comparisons test with Bonferroni correction. The chi-square test was used to assess relations between categorical variables. Statistical significance was set at 0.05. Analyses were performed on MedCalc Statistical Software version 12.7.7 (MedCalc Software BVBA, Ostend, Belgium; http://www.medcalc.org; 2013).
Results
The rate of diagnoses of sleep disorders in our study (CSHQ cut-off point: 41) was significantly higher than that in the control group (p < 0.001). The incidence of sleep disorders was 2,89-fold (1/0,345) higher in our case group. Mean CSHQ score, and anxiety-withdrawal and anger-aggression aggression scores were also significantly higher in the case group, while social competence scores were significantly lower (p < 0.001). Males also comprised more of the case group, which also had a lower level of receipt of pre-school education (p < 0.001) ().
Table 1. Comparison of the Children’s Sleep Habits Questionnaire (CSHQ), Social Competence and Behavior Evaluation (SCBE-30) scale scores, age, duration of sleep, sex, and pre-school education in the case and control groups.
Intelligence level distributions in the group diagnosed with intellectual Disabilities (ID) were evaluated with the help of clinical assessment and DDST-II. Borderline mental capacity was present in 15 cases (35%), mild mental retardation in 19 (44%), moderate mental retardation in 8 (19%), and severe mental retardation in 1 (2%). Mean CSHQ scores were 44, 68 – 48, 33 – 54, and 62 – 59, respectively. Subjects in the group diagnosed with ID frequently had nervous and mild cognitive problems, and CSHQ scores increased in line with the severity of mental retardation.
Male subjects among the entire study group achieved significantly lower social competence scale scores (p < 0.001), and higher anxiety-withdrawal scale scores (p = 0.006) than girls. Social competence increased in the group receiving pre-school education, while significant decreases were observed in anger-aggression, and anxiety-withdrawal (p < 0.001) ().
Table 2. Assessment of scale scores in terms of sex and pre-school education.
Analysis of disease subgroups in the patient group paid particular attention to gender. Significant variation was determined among CSHQ scores in male gender (p = 0.004). Two-way comparisons revealed that the median value of the communication disorder (CD) group was lower than those of the attention-deficit hyperactivity disorder (ADHD) (p = 0.046) and ID (p = 0.024) groups. Significant variation was also observed in social competence scores in male gender (p = 0.001). Two-way comparisons revealed that the median value of the CD group was significantly higher than those of the ADHD (p = 0.006), ID (p = 0.0001), and autism spectrum disorder (ASD) (p = 0.001) groups. Although significant variation was observed in anxiety-withdrawal scores in males in this group, no significant difference was determined at two-way comparison. To summarize, boys with neurodevelopmental disorder were more affected by sleep and social competence diagnoses than girls ().
Table 3. Comparison of scale scores after gender distribution in the case group.
Distributions of sleep disorder diagnoses determined using the CSHQ in the case subgroups are shown in (). Analysis revealed a significant difference between CSHQ and social competence scale scores in the case group irrespective of gender distribution (p = 0.028 and p < 0.001). Neurodevelopmental disorders were also affected by sleep and social competence disorders (). The difference determined between CSHQ scores was not statistically significant at two-way comparisons. Children diagnosed with ADHD, ID, and ASD achieved significantly lower social competence scores than the CD group (p = 0.014, p < 0.001, p < 0.001) (). Social competence scores decreased in the CD, ADHD, ID, and ASD groups, in descending order. The best social competence scores were in the CD group.
Table 4. Comparison of scale scores by diagnosis groups in the case group.
Table 5. Two-way comparisons between disease groups.
CSHQ score was negatively correlated with social competence (0.278, 27.8%) and positively correlated with anger-aggression (0.290, 29%), and anxiety and withdrawal (0.317, 31.7%) scores ().
Table 6. Correlation analysis of Children’s Sleep Habits Questionnaire (CSHQ) and Social Competence and Behavior Evaluation (SCBE-30) scores.
Mean social competence scores in the control and case groups were higher among subjects without sleep problems than in those with such problems, while mean anger-aggression and anxiety-withdrawal (). Possession of sleep problem appears to reduce social incompetence, while increasing anger-aggression and anxiety-withdrawal.
Discussion
A higher quantity or quality of sleep in childhood is associated with better behavioural and cognitive outcomes. The results of previous studies indicate a link between pre-school sleep and behaviour and cognition [Citation23]. In addition, sleep parameters have been documented as a basic foundation for social functions in schoolchildren, adolescents, and adults [Citation24]. Optimal sleep supports pre-school children’s adaptive functioning. Sleep in this period is associated with a series of social, sensory, and cognitive adaptation mechanisms [Citation25]. Social skills deficiency in children is known to result in adverse outcomes in the long term, and social competence affects life in a multifaceted manner. Social skills in early childhood are also an indicator of social competence at later ages. Insufficient or poor-quality sleep in early childhood can compromise social-emotional functions through its effect on the developing brain [Citation26]. One recent study determined that length of sleep is positively correlated with social competence [Citation25]. Correlation analysis in our study showed that participants’ social competence decreased as CSHQ scores, severity of sleep problems in other words, increased, in both the case and control groups. We observed that participants’ anger-aggression and anxiety-withdrawal scores increased in line with sleep problems. Recent studies have suggested that a shorter duration of night sleep exacerbates behavioural problems. Hyperactivity, decreased academic performance, externalizing symptoms, anger, aggression, and impulsivity have been linked to sleep disorder [Citation27].
Social development becomes particularly pronounced when children start school. They evolve with their peers and learn to live in a community. Development of social skills with pre-school education is thought to be useful for children’s social development and to be effective in preventing emotional disturbances [Citation28,Citation29]. In our study, and in agreement with the previous literature, social competence scores were higher and anger-aggression and anxiety-withdrawal scores were lower in the group receiving pre-school education. The realization of the effect of sleep on emotional functioning in children is also important. Childhood is a critical time when children develop the ability to regulate their emotions. Poor sleep has been proved to be linked to anxiety, emotional problems, and depressive symptoms. Additionally, decreased sleep durations have been revealed to adversely affect emotional functioning, especially in developing children [Citation30]. Previous studies have determined links between individuals’ sleep problems and several psychiatric and neurological disorders [Citation31–33].
Variations have been observed in the regulation of gene expression during wakefulness and sleep. Genes regulated during seep are thought to contribute to brain plasticity and memory consolidation [Citation34]. Sleep is a critical brain function for learning and development. The newborn sleep cycle has been shown to be linked to executive functioning and verbal IQ scores at subsequent ages. Neonatal studies have reported that sleep problems adversely impact on neurodevelopmental outcome scores [Citation35]. Intelligence levels decreased in the ID group in our study, while CSHQ scores and sleep problems increased.
The proportion of boys in the case group was greater than that in the control group. We attributed this to ASD, CD, ADHD, and ID being predominantly male neurodevelopmental disorders. Previous studies have also demonstrated a greater preponderance of males in these disorders [Citation36–39]. Sleep disorders in children with neurodevelopmental disorders may be more resistant to treatment, and more severe and permanent than those in healthy children [Citation40]. Weak sleep has been determined to have an adverse impact on the concept of Theory of Mind, defined as the ability to determine the mental states of others, by affecting executive functioning. It has also been determined to adversely affect emotional information processing and to be associated with neurodevelopmental disorders [Citation41,Citation42]. The failure of autonomic nervous system homeostasis in the sleep-wake cycle affecting subsequent emotional, cognitive and social development represents one of the models of the developmental foundations of ASD [Citation43]. The estimated prevalence of sleep disorders in ASD ranges between 40% and 80% [Citation15]. In our study, sleep disorder was determined in 48% of the ASD group and in 66% of the entire neurodevelopmental group. Rates of sleep disorder diagnosis were higher in children with neurodevelopmental disorder compared to the healthy children. Social competence scores decreased as sleep problems increased among all participants, and this was more pronounced in the group with neurodevelopmental disorder.
Sleep problems in the pre-school problem have been shown to have an adverse impact on cognitive abilities in the elementary school period. Sleep problems were negatively associated with performance on tasks assessing working memory [Citation44]. Sleep disorders have a particularly adverse effect on objective-focused behaviours when the aims are abstract or complex impact [Citation45]. Sleep disorders are common in ADHD [Citation46]. Learning and attention problems have been reported in 57% of parents of children with sleep disorder [Citation47]. ADHD group CSHQ scores in our study were higher than those in the ASD and CD groups. Approximately 25–50% of children and adolescents with ADHD are known to experience sleep problems. Appropriate intervention in these problems can increase the quality of life and reduce the severity of ADHD and the disturbance it causes [Citation48]. Sleep disorders were observed at as high a rate as 78% of the ADHD group in our study.
One of the limitations of this study is the greater preponderance of boys in the case group compared to the control group. This derived from a greater predominance of male gender in patients with neurodevelopmental disorders. In order to determine the effect of this, we also analysed the study data in terms of gender differences. Another limitation of our study is the difficulty of diagnosing in ID in this age group and the limited usefulness of the DDST-II employed. In addition, although subjects were enrolled from a similar income level, no date is available for external conditions that might affect sleep hygiene. Our study involved a large number of subjects in an age group that included pre-school children, an age group that has been little studied to date. We used reliable and valid tools updated in the light of the latest developments and needs. We obtained data in an area in which only limited data have been available from previous studies. We think that these represent the powerful aspects of our study.
Conclusion
On the basis of our research findings, we determined an association between sleep habits in the pre-school period and aggressive and anxious behaviours. We think that sleep habits may represent a marker in these areas in pre-school children. We also determined significant relations between sleep habits and neurodevelopmental disorders. We think that based on our results, sleep habits in early childhood can also be a risk indicator for neurodevelopmental disorders. We determined that social competence and behaviour can be as much affected in this group as in healthy children. We think that sleep in children in this age group should be treated as a potential indicator or neurodevelopmental disorders, social competence and behaviour, and that early interventions are required.
Acknowledgements
The authors are grateful to the patients and controls for their participation. They alone are responsible for the content and writing of the paper. They declare that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria, educational grants, participation in speakers’ bureaus, membership, employment, consultancies, stock ownership, or other equity interest).
Disclosure statement
No potential conflict of interest was reported by the authors.
ORCID
Tayfun Kara http://orcid.org/0000-0002-2156-3457
Ömer Alpgan http://orcid.org/0000-0002-2208-0617
Semra Yılmaz http://orcid.org/0000-0002-6527-2432
Ismail Akaltun http://orcid.org/0000-0002-9938-9276
References
- Davis KF, Parker KP, Montgomery GL. Sleep in infants and young children: part one: normal sleep. J Pediatr Health Care. 2004;18:65–71. doi: 10.1016/S0891-5245(03)00149-4
- Calhoun SL, Fernandez-Mendoza J, Vgontzas AN, et al. Prevalence of insomnia symptoms in a general population sample of young children and preadolescents: gender effects. Sleep Med. 2014;15:91–95. doi: 10.1016/j.sleep.2013.08.787
- Huhdanpää H, Klenberg L, Westerinen H, et al. Sleep and psychiatric symptoms in young child psychiatric outpatients. Clin Child Psychol Psychiatry. 2018;23:77–95. doi: 10.1177/1359104517718366
- Licis A. Sleep disorders: assessment and treatment in preschool-aged children. Child Adolesc Psychiatr Clin N Am. 2017;26:587–595. doi: 10.1016/j.chc.2017.02.009
- Meltzer LJ. Sleep and developmental psychopathology: introduction to the special issue. J Clin Child Adolesc Psychol. 2017;46:171–174. doi: 10.1080/15374416.2016.1220316
- Williams KE, Nicholson JM, Walker S, et al. Early childhood profiles of sleep problems and self-regulation predict later school adjustment. Br J Educ Psychol. 2016;86:331–350. doi: 10.1111/bjep.12109
- Taylor MA, Schreck KA, Mulick JA. Sleep disruption as a correlate to cognitive and adaptive behavior problems in autism spectrum disorders. Res Dev Disabil. 2012;33:1408–1417. doi: 10.1016/j.ridd.2012.03.013
- Hoffman MF, Quittner AL, Cejas I. Comparisons of social competence in young children with and without hearing loss: a dynamic systems framework. J Deaf Stud Deaf Educ. 2015;20:115–124. doi: 10.1093/deafed/enu040
- Denham SA, Blair KA, DeMulder E, et al. Preschool emotional competence: pathway to social competence? Child Dev. 2003;74:238–256. doi: 10.1111/1467-8624.00533
- Thomson KC, Guhn M, Richardson CG, et al. Profiles of children’s social-emotional health at school entry and associated income, gender and language inequalities: a cross-sectional population-based study in British Columbia. Canada. BMJ Open. 2017;7(7):e015353. doi:10.1136/bmjopen-2016-015353.
- Joy JM. Evaluating positive social competence in preschool populations. Sch Community J. 2016;26:263–290.
- Bornstein MH, Hahn CS, Haynes OM. Social competence, externalizing, and internalizing behavioral adjustment from early childhood through early adolescence: developmental cascades. Dev Psychopathol. 2010;22:717–735. doi: 10.1017/S0954579410000416
- MacLean JE, Fitzgerald DA, Waters KA. Developmental changes in sleep and breathing across infancy and childhood. Paediatr Respir Rev. 2015;16:276–284.
- Harris JC. New classification for neurodevelopmental disorders in DSM-5. Curr Opin Psychiatry. 2014;27:95–97. doi: 10.1097/YCO.0000000000000042
- Robinson-Shelton A, Malow BA. Sleep disturbances in neurodevelopmental disorders. Curr Psychiatry Rep. 2016;18(1):6. doi:10.1007/s11920-015-0638-1.
- Powell WT, LaSalle JM. Epigenetic mechanisms in diurnal cycles of metabolism and neurodevelopment. Hum Mol Genet. 2015;24(R1):R1–R9. doi:10.1093/hmg/ddv234.
- LaFreniere PJ, Dumas JE. Social competence and behavior evaluation in children ages 3 to 6 years: The short form (SCBE-30). Psychol Assess. 1996;8:369–377. doi: 10.1037/1040-3590.8.4.369
- Çorapçı F, Aksan N, Arslan-Yalçın D, et al. Emotional, behavioral and social adjustment screening at school entry: social competence and behavior evaluation-30 scale. Turk J Child Adolesc Mental Health. 2010;17:63–74.
- Owens JA, Spirito A, McGuinn M. The Children’s Sleep Habits Questionnaire (CSHQ): psychometric properties of a survey instrument for school-aged children. Sleep. 2000;23:1043–1051. doi: 10.1093/sleep/23.8.1d
- Fiş NP, Arman A, Ay P, et al. Çocuk Uyku Alışkanlıkları Anketinin Türkçe geçerliliği ve güvenilirliği. Anadolu Psikiyatri Derg. 2010;11:151–160. Turkish.
- Frankenburg WK, Dodds J, Archer P, et al. The Denver II: a major revision and restandardization of the Denver developmental screening test. Pediatrics. 1992;89:91–97.
- Anlar B, Yalaz K. Denver II developmental screening test, adaptation and standardization in Turkish children. Ankara: Hacettepe University Press; 1995; Turkish.
- Reynaud E, Vecchierini MF, Heude B, et al. Sleep and its relation to cognition and behaviour in preschool-aged children of the general population: a systematic review. J Sleep Res. 2017. doi:10.1111/jsr.12636.
- Walker MP. The role of sleep in cognition and emotion. Ann N Y Acad Sci. 2009;1156:168–197. doi: 10.1111/j.1749-6632.2009.04416.x
- Vaughn BE, Elmore-Staton L, Shin N, et al. Sleep as a support for social competence, peer relations, and cognitive functioning in preschool children. Behav Sleep Med. 2015;13:92–106. doi: 10.1080/15402002.2013.845778
- Bonuck KA, Blank A, True-Felt B, et al. Promoting sleep health among families of young children in head start: protocol for a social-ecological approach. Prev Chronic Dis. 2016;13:E121. doi:10.5888/pcd13.160144.
- Scharf RJ, Demmer RT, Silver EJ, et al. Nighttime sleep duration and externalizing behaviors of preschool children. J Dev Behav Pediatr. 2013;34:384–391. doi: 10.1097/DBP.0b013e31829a7a0d
- Hubert B, Guimard P, Florin A. Cognitive self-regulation and social functioning among French children: a longitudinal study from kindergarten to first grade. Psych J. 2017;6:57–75. doi: 10.1002/pchj.160
- Lau EX, Rapee RM, Coplan RJ. Combining child social skills training with a parent early intervention program for inhibited preschool children. J Anxiety Disord. 2017;51:32–38. doi: 10.1016/j.janxdis.2017.08.007
- Vriend J, Davidson F, Rusak B, et al. Emotional and cognitive impact of sleep restriction in children. Sleep Med Clin. 2015;10:107–115. doi: 10.1016/j.jsmc.2015.02.009
- Pucci SH, Pereira Mda G. The mediator role of psychological morbidity on sleep and health behaviors in adolescents. J Pediatr (Rio J). 2016;92:53–57. doi: 10.1016/j.jped.2015.03.008
- Schneider HE, Lam JC, Mahone EM. Sleep disturbance and neuropsychological function in young children with ADHD. Child Neuropsychol. 2016;22:493–506. doi: 10.1080/09297049.2015.1018153
- Tolaymat A, Liu Z. Sleep disorders in childhood neurological diseases. Children. 2017;4:84. doi:10.3390/children4100084.
- Stickgold R. Sleep-dependent memory consolidation. Nature. 2005;437:1272–1278. doi: 10.1038/nature04286
- Shellhaas RA, Burns JW, Hassan F, et al. Neonatal sleep-wake analyses predict 18-month neurodevelopmental outcomes. Sleep. 2017;40(11). doi:10.1093/sleep/zsx144.
- Ormond S, Brownlow C, Garnett MS, et al. Profiling autism symptomatology: an exploration of the Q-ASC parental report scale in capturing sex differences in autism. J Autism Dev Disord. 2018;48:389–403. doi: 10.1007/s10803-017-3324-9
- Becker SP, Cusick CN, Sidol CA, et al. The impact of comorbid mental health symptoms and sex on sleep functioning in children with ADHD. Eur Child Adolesc Psychiatry. 2018;27:353–365. doi: 10.1007/s00787-017-1055-2
- Longo IA, Tupinelli GG, Hermógenes C, et al. Prevalence of speech and language disorders in children in the western region of São Paulo. Codas. 2017;29(6):e20160036. doi:10.1590/2317-1782/20172016036.
- Lin JD. Population with intellectual disability based on 2000–2007 national registers in Taiwan: age and gender. Res Dev Disabil. 2009;30:294–300. doi: 10.1016/j.ridd.2008.05.001
- Stores G. Multifactorial influences, including comorbidities, contributing to sleep disturbance in children with a neurodevelopmental disorder. CNS Neurosci Ther. 2016;22:875–879. doi: 10.1111/cns.12574
- Tesfaye R, Gruber R. The association between sleep and theory of mind in school aged children with ADHD. Med Sci. 2017;5:18. doi:10.3390/medsci5030018. doi: 10.29387/ms.2017.5.1.18-20
- Baron-Cohen S. Theory of mind and autism: a review. Int Rev Res Ment Retard. 2000;23:169–184. doi: 10.1016/S0074-7750(00)80010-5
- Inui T, Kumagaya S, Myowa-Yamakoshi M. Neurodevelopmental hypothesis about the etiology of autism spectrum disorders. Front Hum Neurosci. 2017;11:354 eCollection 2017. doi:10.3389/fnhum.2017.00354.
- Nelson TD, Nelson JM, Kidwell KM, et al. Preschool sleep problems and differential associations with specific aspects of executive control in early elementary school. Dev Neuropsychol. 2015;40:167–180. doi: 10.1080/87565641.2015.1020946
- Dahl RE. The impact of inadequate sleep on children’s daytime cognitive function. Semin Pediatr Neurol. 1996;3:44–50. doi: 10.1016/S1071-9091(96)80028-3
- Durmuş FB, Arman AR, Ayaz AB. Chronotype and its relationship with sleep disorders in children with attention deficit hyperactivity disorder. Chronobiol Int. 2017;34:886–894. doi: 10.1080/07420528.2017.1329207
- Calhoun SL, Fernandez-Mendoza J, Vgontzas AN, et al. Learning, attention/hyperactivity, and conduct problems as sequelae of excessive daytime sleepiness in general population study of young children. Sleep. 2012;35:627–632.
- Miano S, Parisi P, Villa MP. The sleep phenotypes of attention deficit hyperactivity disorder: the role of arousal during sleep and implications for treatment. Med Hypotheses. 2012;79:147–153. doi: 10.1016/j.mehy.2012.04.020