ABSTRACT
We hereby report a case of a patient with Wilson’s disease, presenting only with psychiatric symptoms without significant hepatic or neurological symptoms. A 27-year-old woman was admitted to the psychiatric ward with symptoms of somatic preoccupation, auditory hallucinations, suicidal behaviour, regressed behaviour, and severe anxiety. She suffered from paralyzing sensation in both big toes, without any abnormal findings in nerve conduction tests or any neurological signs and symptoms. Also, no significant hepatic impairment was presented. Psychiatric symptoms improved with antipsychotics, mood stabilizers, and other psychotropic agents, but dysphagia and general weakness developed later. She had a family history of Wilson’s disease. High signal intensities in the basal ganglia, midbrain, and pons were observed with fluid-attenuated inversion-recovery (FLAIR) imaging. Based on abnormal findings in the urine copper and serum ceruloplasmin tests, as well as the presence of the ATP7B mutation, a diagnosis of Wilson’s disease was made. Therefore, our case report suggests that future studies should consider the evaluation of psychiatric symptoms in the diagnostic conceptualization of Wilson’s disease.
Introduction
Wilson’s disease is an inherited autosomal recessive disorder that leads to copper metabolism impairment and the accumulation of copper in several organs, especially in the liver, brain, and cornea [Citation1]. In the pathogenesis of Wilson’s disease, the reduced excretion of copper into the bile is caused by the ATP7B mutation and, eventually, results in the accumulation of copper in the organs. The main clinical manifestations are hepatic, neurological, and psychiatric symptoms. Among these manifestations, liver disease is regarded as the main problem in Wilson’s disease [Citation2,Citation3]. In the context of presenting symptoms and natural courses of Wilson’s disease, the observed hepatic and neurological abnormalities are relatively well-known. Hepatic injury in Wilson’s disease can present in a wide range, from asymptomatic to liver cirrhosis. Also, dysarthria, dystonia, tremor, and parkinsonian symptoms can present as neurological symptoms in Wilson’s disease. A diagnosis of Wilson’s disease is mostly made at the ages between 5 and 35, with a mean age of diagnosis at 13 years old [Citation4]. With regards to Wilson’s disease, hepatic injuries firstly manifest at the ages between 9 and 13 [Citation3,Citation5], whereas neurological signs and symptoms firstly present at the ages between 15 and 21 [Citation6]. However, the presenting ages of the first psychiatric manifestations of Wilson’s disease are not yet clear. The average age of psychiatric symptom onset is reported at 22.6 years [Citation7]. Nevertheless, the prevalence of psychiatric symptoms in patients with Wilson’s disease ranges from 10 to 100 percent [Citation8]. Moreover, the early appearance of psychiatric symptoms during the onset of Wilson’s disease is uncommon. Thus, the diagnosis of Wilson’s disease might be hindered in cases with preponderance of psychiatric symptoms and manifestations [Citation8].
We hereby report a Wilson’s disease case presenting exclusively with psychiatric symptoms, including somatic preoccupation, suicidal behaviour, and auditory hallucinations, without significant liver injuries or neurological symptoms. The patient gave informed consent for publication. This case report is approved by the institutional review board (IRB) of Inje University Haeundae Paik Hospital, Busan, Korea (IRB number: 2018-08-011).
Case presentation
A 27-year-old woman presented with somatic preoccupation (erratic sensations in both toes), auditory hallucinations, suicidal and regressed behaviour, as well as severe anxiety, was admitted to the psychiatric ward of a university-affiliated general hospital located at Busan, South Korea. Despite the onset of the paralyzing sensation in both toes occurring 3 weeks before the patient’s admission to the hospital, no significant neurological symptoms in accordance with erratic sensation were detected. In addition, she presented with auditory hallucinations in the form of her dead brother’s voice telling her that she should die, together with the delusion that she was the devil. The patient presented with suicidal behaviour and acted with impulsivity. According to her past psychiatric history, a gradual decrease in interpersonal and social activities was observed 6 months prior to her hospitalization, and leaving her job was frequently reported in her early 20s. The medical family history revealed that her brother died from Wilson’s disease. With respect to laboratory findings, except for a mild elevation in aspartate aminotransferase (44 U/L [7–38 U/L]), lactic acid dehydrogenase (272 U/L [130–270 U/L]), and prothrombin time (16.0 s [10.0–13.0 s]), no hepatic abnormalities were detected. There were no abnormal findings during the nerve conduction tests for the following nerves: bilateral sural, superficial peroneal, bilateral common peroneal and posterior tibial. Similarly, no abnormalities were observed during the electromyographical tests for the tibialis anterior muscle, peroneus longus muscle, and gastrocnemius muscle.
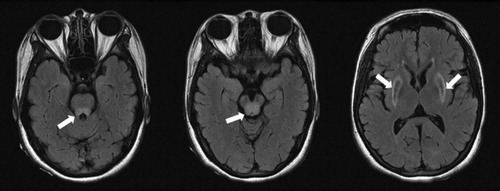
Under the initial diagnosis of brief psychotic disorder, based on the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) [Citation9], the patient was medicated with olanzapine 20 mg, valproate 600 mg, and clonazepam 0.5 mg per day. The avoidance of valoproate was usually recommended in hepatic dysfunction [Citation10]. However, since the level of her hepatic injury was minimal and her suicidal behaviours and impulsivity were prominent, valproate was used. There was a mild improvement in the occurrence of auditory hallucinations, suicidal behaviour, and impulsivity, while the regressed behaviour and somatic concerns were sustained under the psychiatric treatment. Due to the high signal intensities detected in the basal ganglia, midbrain, and pons during fluid-attenuated inversion-recovery (FLAIR) imaging (), encephalopathy, because of metabolic or autoimmune abnormalities, was presumed as putative diagnosis. Despite the absence of Kayser-Fleischer rings, abnormal results from the 24 h urine copper test (80.6 μg/day [16.0–60.0 μg/day]) and the serum ceruloplasmin test (< 4.0 mg/dL [17.9–53.3 mg/dL]) were identified, along with the existence of the ATP7B mutation that leads to impaired copper excretion into the bile. Hence, the patient’s diagnosis of Wilson’s disease was confirmed by a hepatologist.
Discussion
Wilson’s disease presents with a wide range of psychiatric manifestations. It has been reported that the most commonly associated psychiatric symptoms are depression, personality changes, incongruent behaviour, and irritability. In addition, suicidal behaviour, impulsiveness, labile mood, bipolar affective symptoms, dysthymia, cognitive impairment, psychosis, anxiety, and sexual preoccupation have also been reported in patients with Wilson’s disease. Because of this broad spectrum of symptoms, there are no specific psychiatric symptoms that could be associated with Wilson’s disease [Citation8,Citation9,Citation11]. In addition, although psychiatric symptoms are frequently presented along with Wilson’s disease, they are not considered in the scoring system for Wilson’s disease diagnosis, as reported by the European Association for the Study of the Liver [Citation2]. The main symptomatology considered for Wilson’s disease diagnosis includes, the presence of Kayser-Fleischer rings, neurological signs, serum ceruloplasmin levels, coombs-negative hemolytic anemia, liver and urinary copper values, and chromosomal mutations. During the initial scoring system adaptation, in the “neuropsychiatric symptom suggestive of Wilson’s disease” item, the patient scored 2, which corresponded to “probable.” However, as mentioned earlier, neuropsychiatric symptoms associated with Wilson’s disease are too broad and have no specific symptomatology. Therefore, a limitation exists when evaluating the existence of Wilson’s disease by this score alone, when only psychiatric symptoms occur. Following specific laboratory testing to evaluate copper metabolism, the patient scored 6, a value corresponding to a “highly likely Wilson disease” diagnosis.
Psychiatric symptoms are not rare in Wilson’s disease but are not considered as diagnostic. On the contrary, psychiatric symptoms are considered as comorbid symptomatology that appears with liver or neurological impairment. Thus, without any hepatic or neurological manifestations, a case of Wilson’s disease presenting only with psychiatric symptoms might require a more sophisticated diagnostic algorithm.
Disclosure statement
No potential conflict of interest was reported by the authors.
ORCID
Jung An Lee https://orcid.org/0000-0001-9106-3805
Nae-Yun Heo http://orcid.org/0000-0001-6571-8935
Bong Ju Lee http://orcid.org/0000-0002-4194-6842
Gyung-Mee Kim https://orcid.org/0000-0002-8010-1607
Jung Goo Lee http://orcid.org/0000-0003-3393-2667
Seon-Cheol Park http://orcid.org/0000-0003-3691-4624
References
- Ferenci P. Pathophysiology and clinical features of Wilson disease. Metab Brain Dis. 2004;19:229–239. doi: 10.1023/B:MEBR.0000043973.10494.85
- European Association for Study of Liver. EASL clinical practice guidelines: Wilson’s disease. J Hepatol. 2012;56:671–685. doi: 10.1016/j.jhep.2011.11.007
- Saito T. Presenting symptoms and natural history of Wilson disease. Eur J Pediatr. 1987;146:261–265. doi: 10.1007/BF00716470
- Lin LJ, Wang DX, Ding NN, et al. Comprehensive analysis on clinical features of Wilson’s disease: an experience over 28 years with 133 cases. Neurol Res. 2014;36:157–163. doi: 10.1179/1743132813Y.0000000262
- Walshe JM. Wilson’s disease presenting with features of hepatic dysfunction: a clinical analysis of eighty-seven patients. Q J MEd. 1989;70:253–263.
- Lorincz MT. Neurologic Wilson’s disease. Ann N Y Acad Sci. 2010;1184:173–184. doi: 10.1111/j.1749-6632.2009.05109.x
- Zimbrean PC. Psychiatric aspects of Wilson disease: a review. Gen Hosp Psychiatry. 2014;36:53–62. doi: 10.1016/j.genhosppsych.2013.08.007
- Akil M, Brewer GJ. Psychiatric and behavioral abnormalities in Wilson’s disease. Adv Neurol. 1995;65:171–178.
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington (DC): American Psychiatric Association; 2013.
- Lacerda G, Krummel T, Sabourdy C, et al. Optimizing therapy of seizures in patients with renal or hepatic dysfunction. Neurology. 2006;67:S28–S33. doi: 10.1212/WNL.67.12_suppl_4.S28
- Shanmugiah A, Sinha S, Taly AB, et al. Psychiatric manifestations in Wilson’s disease: a cross-sectional analysis. J Neuropsychiatry Clin Neurosci. 2008;20:81–85. doi: 10.1176/jnp.2008.20.1.81