ABSTRACT
OBJECTIVE: The purpose of this study was to evaluate the relationship between childhood traumas (CTs) and severity and symptom dimensions of Obsessive Compulsive Disorder (OCD).
METHOD: One hundred and sixty (160) patients diagnosed with OCD were included. The Yale-Brown Obsessive-Compulsive Scale (YBOCS), the Childhood Trauma Questionnaire (CTQ), the Beck Depression Inventory (BDI), and the Beck Anxiety Inventory (BAI) were applied to the participants.
RESULTS: According to a cut-off score of > 35 for CTQ total score, 71 (44.4%) OCD patients had no CT history and 89 (55.6%) OCD patients had CTs history. There were no significant difference between the two groups with regard to YBOCS total score or to obsessions and compulsions except aggressive obsessions. The associations between aggressive obsessions, BDI total score, BAI total score and emotional abuse were statistically significant, but the correlation between aggressive obsessions and emotional abuse was no longer significant after controlling for BDI and BAI total scores. In the parallel multiple mediator model analysis, there were not statistically significant mediator effects of depression and anxiety variables in the relationship between emotional abuse and aggressive obsessions. Mobility in childhood was significantly correlated with physical abuse, and this correlation was still significant after controlling for BDI and BAI total scores. BDI total score was significantly associated with sexual abuse.
CONCLUSION: The relationship between CTs and OCD should be reconsidered in light of other contributing factors such as comorbidity.
Introduction
Obsessive Compulsive Disorder (OCD) is diagnosed according to the presence of obsessions and compulsions. It has an estimated lifetime prevalence of 2.3%, and it tends to co-occur with a significant social and occupational impairment, poor quality of life and chronic course [Citation1,Citation2]. As we know from the genetic studies of OCD, approximately 50% of the OCD symptom variance has been explained by non-genetic environmental factors; thus, it is important to determine these factors to understand the aetiology of the disease [Citation3].
Traumatic experiences during childhood, including abuse and neglect, can cause or exacerbate psychiatric disorders in adulthood [Citation4]. Childhood traumas (CTs) can affect neurobiological and neuroendocrine systems and lead to vulnerability to developing psychiatric disorders in later life [Citation5]. There are many studies on the relationship between CTs and adult psychopathology, and it has been shown that CTs are significantly associated with psychosis, affective disorders, anxiety disorders, substance use disorders and borderline personality disorder [Citation6–12].
There are also studies claiming that CTs are observed more frequently in patients with OCD when compared to healthy controls [Citation13–15]. Multiple CTs are shown to increase adult OCD nearly five times [Citation16]. When we look at the relationship between CTs and OCD severity and chronicity, there are inconsistent results in the literature. Some studies found a significant relationship with CTs and OCD severity [Citation17–19], while others did not [Citation20–22]. In a recent meta-analysis, it has been found that exposure to trauma is related to the severity of compulsions, but not to the severity of obsessions [Citation23]. In a clinical study, CTs were found to be related to treatment resistance [Citation24]. In another study, CTs found to be related only to the comorbidity of OCD, not to the severity or chronicity thereof [Citation20]. Aggression, sexual and religious obsessions and ritualistic compulsions were found to be related to higher CT scores in an OCD patient group [Citation25]. In a prospective study seeking risk factors for developing OCD, childhood sexual abuse was related to all OCD symptom dimensions except contamination/washing, and physical abuse was linked to shameful thoughts dimension [Citation26]. There have also been studies linking suicidality and CTs in OCD [Citation25].
Although the above-mentioned studies revealed significant results about the relationship between CTs and OCD, there are also inconsistent results and limited studies, particularly about the type of CTs and symptom dimensions of OCD. In this study, we aim to investigate if exposure to CTs in a large sample of OCD patient group make any difference according to sociodemographic and clinical features. Our hypothesis is; CTs are linked to severity and symptom dimensions of OCD.
Methods
Participants
One hundred and eighty-three patients, all of whom were diagnosed with OCD according to Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (SCID-I), and all of whom were admitted to the Bakırköy Mazhar Osman Mental Health and Neurological Diseases Education and Research Hospital OCD outpatient clinic between March and September 2018, participated in the study. Of the participants, only those between 18 and 65 years of age and of sufficient cognitive ability to answer the scales were included in the study, and those with a psychotic disorder, mental retardation, lack of education, severe neurological disorder or cognitive deficits were excluded. Ultimately the study consisted of one hundred and sixty patients. The study protocol was approved by the local ethics committee (February 6 2018 date and 127 number) and the written informed consent form was given to all participants.
Measures
For determining the sociodemographic characteristics of the participants, a sociodemographic data form, which included questions about early separation from parents, childhood mobility, the divorce of parents and ethnic differences was applied.
Yale-Brown Obsessive-Compulsive Scale (YBOCS) is an interviewer-rated scale developed to measure the type and severity of OCD. YBOCS total severity score is the sum of the first 10 items, ranging from 0 to 40. For the symptom dimensions of OCD, the YBOCS Symptom Checklist was used. The Turkish validity and reliability study of theYBOCS has been conducted by Karamustafalıoglu et al. [Citation27].
Childhood Trauma Questionnaire (CTQ) is a self-report scale that consists of 28 items and 5 subscales (emotional abuse, emotional neglect, physical abuse, physical neglect and sexual abuse). It is a five-points Likert-type scale ranging from 1 to 5. In the reliability and validity study of the Turkish version of the CTQ, the following cut-off scores were suggested: for total CTQ score > 35 points; for emotional abuse and physical neglect subscales > 7 points; for emotional neglect subscale > 12 points; and for physical and sexual abuse subscales > 5 points [Citation28].
The Beck Depression Inventory (BDI) was used to assess the severity of depression, and the Beck Anxiety Inventory (BAI) was used to assess anxiety severity. Both scales are four-point Likert-type self-report scales, and the validity and reliability of the Turkish versions of both scales have been confirmed [Citation29,Citation30].
Statistical analysis
All statistical analyses were performed using the “Statistical Program for Social Sciences version 22.0.” Comparisons of sociodemographic and clinical data were made with Mann–Whitney U test and chi-square analysis. Spearman rho correlations were performed to determine the relationships between CTQ subscales and obsessions, compulsions and total scores on the YBOCS, BDI and BAI. Partial correlation analysis was performed for the relationships of aggressive obsessions-emotional abuse, and mobility in childhood-physical abuse to control for BDI and BAI scores. The parallel multiple mediator model analysis was performed by using the PROCESS macro, for the mediator effects of depression and anxiety variables in the relationship of emotional abuse and aggressive obsessions. P < 0.05 was considered to be the statistically significant level in all analyses.
Results
According to a cut-off score > 35 for CTQ total score, 71 (44.4%) OCD patients had no CT history and 89 (55.6%) OCD patients had CT history. Sixty-eight (42.5%) patients had experienced emotional abuse (EA), 156 (97.5%) patients had experienced physical neglect (PN), 72 (45%) patients had experienced emotional neglect (EN), 41 (25.6%) patients had experienced physical abuse (PA) and 39 (24.4%) patients had experienced sexual abuse (SA).
The sociodemographic characteristics of the OCD groups according to the existence of CT history are presented in . The only statistical difference between the two groups was childhood mobility (P = 0.003).
Table 1. Sociodemographic characteristics of the OCD groups.
Comorbidities in the OCD group without CT history and the OCD group with CT history are presented in . There were no statistically significant difference according to comorbidities between the two groups. The number of the comorbidities in the OCD without CT group was 1.35 ± 0.57 and the number of comorbidities in the OCD with CT group was 1.33 ± 0.6 (P = 0.795).
Table 2. Comorbidity characteristics of the OCD groups.
As given in , there were no significant difference between the two groups with regard to obsessions and compulsions except aggressive obsessions (P = 0.011). The mean YBOCS total score for the OCD group with no CT history was 20.39 ± 6.81 and for the OCD group with CT history was 21.31 ± 7.72 (P = 0.371). The mean BDI total score for the OCD group with no CT history was 17.59 ± 10.44 and for the OCD group with CT history was 21.75 ± 11.21 (P = 0.018). The mean BAI total score for the OCD group with no CT history was 15.85 ± 11.68 and for the OCD group with CT history was 20.37 ± 13.36 (P = 0.03).
Table 3. Comparisons of the OCD groups according to obsessions.
As presented in and , the correlations of CTQ subscales with obsessions, compulsions, YBOCS total score, BDI total score and BAI total score revealed that the associations between aggressive obsessions, BDI total score, BAI total score and emotional abuse were statistically significant (r = 0.234, r = 0.386, r = 0.288, respectively). The correlation between aggressive obsessions and emotional abuse was not significant after controlling for BDI and BAI total scores (r = −0.150, P = 0.29; r = −0.175, P = 0.14, respectively). For the mediation effects of depression and anxiety, we used the parallel multiple mediator model because both variables could have a causal relationship with each other and the relationship between them was statistically significant (r = 0.599, P < 0.001). In these analyses, there were not statistically significant mediator effects of depression and anxiety variables in the relationship of emotional abuse and aggressive obsessions (P > 0.05) ( and ).
Figure 1. The mediator roles of depression and anxiety in the relationship of emotional abuse and aggressive obsessions.
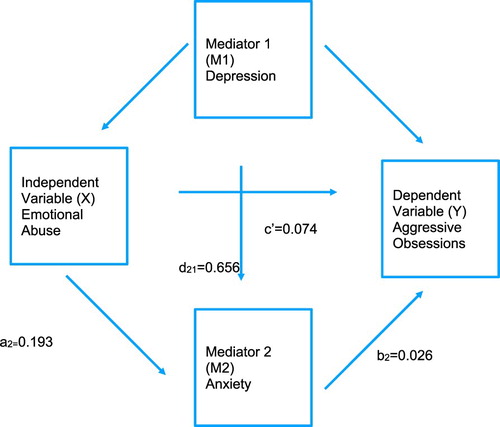
Table 4. Comparisons of the OCD groups according to compulsions.
Table 5. Correlations of the CTQ total and subscales scores with obsessions, compulsions and total scores of the YBOCS, BDI, BAI.
Table 6. The mediator roles of depression and anxiety in the relationship of emotional abuse and aggressive obsessions.
Mobility in childhood was significantly correlated with physical abuse (r = −0.203, P = 0.005) and, after controlling for BDI and BAI total scores, the correlation was still significant (r = −0.204, P = 0.005; r = −0.211, P = 0.004, respectively). BDI total score was significantly associated with sexual abuse (r = 0.310).
Discussion
Exposure to trauma in early life has been associated with a complex interaction with emotional, physiological, behavioural, social/interpersonal and cognitive outcomes [Citation31]. In this study, we aimed to investigate the impact of childhood trauma exposure to OCD symptoms and severity by comparing two groups of OCD patients, those with and those without CT. Among our sample, 55.6% of the patients (n = 89) scored above cut-off for CTQ and those were classified as OCD with the childhood trauma group. OCD symptom severity, obsession and compulsion scores did not differ significantly across groups except aggressive obsessions being significantly more common among the OCD with CT group. Aggressive obsessions correlated with BDI, BAI and childhood emotional abuse scores. When BDI and BAI scores were controlled, the relationship with childhood emotional abuse and aggressive obsessions lost significance and there were not statistically significant mediator effects of depression and anxiety variables on this relationship. Mobility in childhood correlated with physical abuse in childhood. This relationship was not affected by controlling for BDI and BAI. Finally, BDI scores correlated with childhood sexual abuse.
Childhood traumatic experiences have been reported in 60% of adults and in clinical samples rates are higher up to 80% to 90% [Citation32]. Consistent with these results, in our study 55.6% of the OCD patient population reported CT. 97.5% of our population reported physical neglect, which is higher than the previous reports. The literature on the relationships between CT types and OCD indicates that all CT types are associated with OCD and that their effect sizes are very close in magnitude [Citation23]. Participants in this study were recruited from a local government hospital and their socioeconomic levels may be lower than that of the previous studies' populations. It is also important to consider the possible impact of cultural differences on these results.
Childhood mobility and physical abuse were significantly correlated in this study. Childhood mobility has been shown to increase the risk of suicide, violence and psychopathology [Citation33]. It has been suggested that frequent childhood mobility is more common among individuals with low socioeconomic status and may be a sign of family malfunction [Citation34]. Because mobility in childhood can be easily overlooked as a factor in the adult population, its relationship with physical abuse is important to keep in mind.
Contrary to our hypothesis, we could not find any relationship between OCD symptom severity and CT severity/types of CT. Our finding is in line with previous clinical studies that found no significant relationship between CT and OCD severity [Citation20–22]. In a meta-analysis suggesting that CTs are related to severity of compulsions but not the severity of obsessions, not only OCD but all Obsessive Compulsive Spectrum Disorders were included, which might explain the difference between our results and the results of the meta-analysis [Citation23]. It has been suggested that in the studies that found a significant relationship between CT and OCD severity, comorbidity (depression and anxiety levels) might be a mediator [Citation20]. The link between childhood traumatic experiences and the occurrence of OCD has been found to be stronger if the children had tended to be more anxious and/or depressed before the trauma [Citation17]. Consistent with these findings, we found higher depression and anxiety levels in the OCD-with-CT group than in the OCD-without-CT group.
Aggression, sexual and religious obsessions and ritualistic compulsions were found to be more common in an OCD patient group with CTs, and traumatic life events were associated with obsessions/checking and symmetry/ordering symptom dimensions in another OCD patient sample after controlling for comorbidity [Citation19,Citation25]. We found a mild correlation between aggressive obsessions and emotional abuse but the correlation was no longer significant after controlling for depression and anxiety levels and there were not statistically significant mediator effects of depression and anxiety variables on this relationship. Studies on symptom dimensions in major depressive disorder (MDD) and OCD comorbidity revealed inconsistent results. There have been studies that found no significant differences with regard to symptom dimensions and comorbidity in OCD [Citation35–37]. Contrary to this finding, taboo thoughts (aggressive, sexual, religious obsessions) have been reported to be related to comorbid MDD and anxiety disorders in OCD [Citation38,Citation39]. This relation may be an explanation for the association between aggressive obsessions and depression and anxiety levels in our study.
CT also have been linked to the development of MDD [Citation10]. CTs have been reported to increase the severity, chronicity and treatment resistance of MDD [Citation40–42]. In this study, we found depression severity and sexual abuse are correlated. Although in the literature, emotional abuse/neglect and physical abuse were found to be the most common CTs in MDD, sexual abuse was found to increase the risk of depression 1.8 times [Citation43–45]. It has been suggested that the severity and the duration of the childhood trauma, and not the type of trauma, are associated with adult psychiatric disorders, but sexual abuse has been proved to be the most damaging type, which might have a greater impact on comorbidity development [Citation23].
Our first limitation was the cross-sectional study design, which did not allow us to make causal relations across our results. The second limitation of our study was the use of self-report measures, especially for CTs, which may have led to potential recall bias. Lack of evaluations for personality disorders, life-time tic comorbidity and meta-cognitive variables are also limitations of our study.
In this study, which included a large sample of OCD patients, we could not find a relationship between the existence of CTs and OCD severity. There were significant correlations between childhood mobility and physical abuse, and between depression and sexual abuse history. Depression and anxiety levels were higher in the CT-exposed OCD group. The association between childhood traumas and their psychological sequelae in adulthood have been well known for a long time, but the underlying mechanisms remain unknown. CTs may have a mediator effect on the development of different psychopathologies and may increase the comorbidity rates in vulnerable individuals. To clarify the effects of CTs on OCD, comparisons with other psychiatric disorders might be helpful.
Disclosure statement
No potential conflict of interest was reported by the authors.
ORCID
Ayşegül Kart http://orcid.org/0000-0003-1248-835X
Hakan Türkçapar http://orcid.org/0000-0001-5298-8039
References
- Ruscio AM, Stein DJ, Chiu WT, et al. The epidemiology of obsessive-compulsive disorder in the National Comorbidity Survey Replication. Mol Psychiatry. 2010;15:53.
- Van Oudheusden LJB, Eikelenboom M, Van Megen HJGM, et al. Chronic obsessive-compulsive disorder: prognostic factors. Psychol Med. 2018;48(13):2213–2222.
- Lervolino AC, Rijsdijk FV, Cherkas L, et al. A Multivariate Twin study of obsessive-compulsive symptom dimensions. Arch Gen Psychiatry. 2011;68(6):637–644.
- Copeland WE, Shanahan L, Hinesley J, et al. Association of childhood trauma exposure with adult psychiatric disorders and functional outcomes. JAMA Netw Open. 2018;1(7):e184493. doi: 10.1001/jamanetworkopen.2018.4493
- Cross D, Fani N, Powers A, et al. Neurobiological development in the context of childhood trauma. Clin Psychol (New York). 2017;24(2):111–124.
- Salokangas, RKR., Schultze-Lutter, F, Schmidt, SJ, et al. Childhood physical abuse and emotional neglect are specifically associated with adult mental disorders. J Ment Health. 2019:1–9. doi: 10.1080/09638237.2018.1521940
- Lewis SJ, Arseneault L, Caspi A, et al. The epidemiology of trauma and post-traumatic stress disorder in a representative cohort of young people in England and Wales. Lancet Psychiatry. 2019;6(3):247–256.
- Cecil CAM, Viding E, Fearon P, et al. Disentangling the mental health impact of childhood abuse and neglect. Child Abuse Negl. 2017;63:106–119.
- Jaffee SR. Child maltreatment and risk for psychopathology in childhood and adulthood. Annu Rev Clin Psychol. 2017;13:525–551.
- Lindert J, von Ehrenstein OS, Grashow R, et al. Sexual and physical abuse in childhood is associated with depression and anxiety over the life course: systematic review and meta-analysis. Int J Public Health. 2014;59:359–372.
- Martín-Blanco A, Soler J, Villalta L, et al. Exploring the interaction between childhood maltreatment and temperamental traits on the severity of borderline personality disorder. Compr Psychiatry. 2014;55(2):311–318.
- O’Leary P, Coohey C, Easton SD. The effect of severe child sexual abuse and disclosure on mental health during adulthood. J Child Sex Abuse. 2010;19:275–289.
- Adams TG, Kelmendi B, Brake CA, et al. The role of stress in the pathogenesis and maintenance of obsessive-compulsive disorder. Chronic Stress (Thousand Oaks). 2018;2. doi: 10.1177/2470547018758043
- Lafleur DL, Petty C, Mancuso E, et al. Traumatic events and obsessive compulsive disorder in children and adolescents: is there a link? J Anxiety Disord. 2011;25:513–519.
- Carpenter L, Chung MC. Childhood trauma in obsessive compulsive disorder: The roles of alexithymia and attachment. Psychol Psychother Theory Res Pract. 2011;84:367–388.
- Park S, Hong JP, Bae JN, et al. Impact of childhood exposure to psychological trauma on the risk of psychiatric disorders and somatic discomfort: Single vs. multiple types of psychological trauma. Psychiatry Res. 2014;219:443–449.
- Briggs ES, Price IR. The relationship between adverse childhood experience and obsessive-compulsive symptoms and beliefs: The role of anxiety, depression, and experiential avoidance. J Anxiety Disord. 2009;23:1037–1046.
- Mathews CA, Kaur N, Stein MB. Childhood trauma and obsessive-compulsive symptoms. Depress Anxiety. 2008;25(9):742–751.
- Cromer KR, Schmidt NB, Murphy DL. An investigation of traumatic life events and obsessive-compulsive disorder. Behav Res Ther. 2007;45(7):1683–1691.
- Visser HA, van Minnen A, van Megen H, et al. The relationship between adverse childhood experiences and symptom severity, chronicity, and comorbidity in patients with obsessive-compulsive disorder. J Clin Psychiatry. 2014;75(10):1034–1039.
- Bey K, Lennertz L, Riesel A, et al. Harm avoidance and childhood adversities in patients with obsessive-compulsive disorder and their unaffected first-degree relatives. Acta Psychiatr Scand. 2017;135(4):328–338.
- Selvi Y, Besiroglu L, Aydin A, et al. Relations between childhood traumatic experiences, dissociation, and cognitive models in obsessive compulsive disorder. Int J Psychiatry Clin Pract. 2012;16(1):53–59.
- Miller ML, Brock RL. The effect of trauma on the severity of obsessive-compulsive spectrum symptoms: a meta-analysis. J Anxiety Disord. 2017;47:29–44.
- Semiz UB, Inanc L, Bezgin CH. Are trauma and dissociation related to treatment resistance in patients with obsessive-compulsive disorder? Soc Psychiatry Psychiatr Epidemiol. 2014;49(8):1287–1296.
- Ay R, Erbay LG. Relationship between childhood trauma and suicide probability in obsessive-compulsive disorder. Psychiatry Res. 2018;261:132–136.
- Grisham JR, Fullana MA, Mataix-Cols D, et al. Risk factors prospectively associated with adult obsessive-compulsive symptom dimensions and obsessive-compulsive disorder. Psychol Med. 2011;41:2495–2506.
- Karamustafalıoglu OK, Ucısık AM, Ulusoy M, et al. Reliability and validity of the Yale-Brown Obsessive-Compulsive Scale 29. National congress of psychiatry summary book, Bursa, Savas Ofset, s; 1993. p. 86.
- Sar V, Ozturk E, İkikardeş E. Validity and reliability of the Turkish version of childhood trauma questionnaire. Turk Klin J Med Sci. 2012;32(4):1054–1063.
- Hisli, N., 1989. Validity and reliability of the Beck depression scale for university student. Psikol Derg. 7, 3–13.
- Ulusoy M. (1993). Validity and reability of Beck Anxiety Scale [unpublished master thesis]. İstanbul, Bakirkoy Training and Research Hospital for PsychiatryNeurology and Neurosurgery.
- Rockville MD. (2014). Substance abuse and mental health services administration. trauma-informed care in behavioral health services. Treatment Improvement Protocol (TIP) Series 57. HHS Publication No. (SMA) 13-4801.
- Saunders BE, Adams ZW. Epidemiology of traumatic experiences in childhood. Child Adolesc Psychiatr Clin N Am. 2014;23(2):167–184. vii.
- Webb RT, Pedersen CB, Mok PL. Adverse outcomes to early middle age linked with childhood residential mobility. Am J Prev Med. 2016;51(3):291–300.
- Mok PL, Webb RT, Appleby L, et al. Full spectrum of mental disorders linked with childhood residential mobility. J Psychiatr Res. 2016;78:57–64.
- Tükel R, Polat A, Ozdemir O, et al. Co morbid conditions in obsessive-compulsive disorder. Compr Psychiatry. 2002;43:204–209.
- Quarantini LC, Torres AR, Sampaio AS, et al. Comorbid major depression in obsessive-compulsive disorder patients. Compr Psychiatry. 2011;52:386–393.
- Kalra H, Trivedi JK, Dalal PK, et al. Uncomplicated and complicated obsessive-compulsive disorder: an exploratory study from India. Compr Psychiatry. 2008;49:51–54.
- Nestadt G, Di CZ, Riddle MA, et al. Obsessive-compulsive disorder: subclassification based on co-morbidity. Psychol Med. 2008;39(9):1491–1501.
- Hasler G, LaSalle-Ricci VH, Ronquillo JG, et al. Obsessive-compulsive disorder symptom dimensions show specific relationships to psychiatric comorbidity. Psychiatry Res. 2005;135:121–132.
- Korkeila J, Vahtera J, Nabi H, et al. Childhood adversities, adulthood life events and depression. J Affect Disord. 2010;127:130–138.
- Bernet CZ, Stein MB. Relationship of childhood maltreatment to the onset and course of major depression in adulthood. Depress Anxiety. 1999;9:169–174.
- Johnstone JM, Luty SE, Carter JD, et al. Childhood neglect and abuse as predictors of antidepressant response in adult depression. Depress Anxiety. 2009;26:711–717.
- Chapman DP, Whitfield CL, Felitti VJ, et al. Adverse childhood experiences and the risk of depressive disorders in adulthood. J Affect Disord. 2004;82(2):217–225.
- Gibb BE, Chelminski I, Zimmerman M. Childhood emotional, physical, and sexual abuse, and diagnoses of depressive and anxiety disorders in adult psychiatric outpatients. Depress Anxiety. 2007;24(4):256–263.
- Negele A, Kaufhold J, Kallenbach L, et al. Childhood trauma and Its relation to chronic depression in adulthood. Depress Res Treat. 2015;2015:650804.
