ABSTRACT
Background: Binge eating disorder (BED) and obesity in adolescents is associated with variations in social cognition and emotion regulation. The current study aimed to evaluate the Theory of Mind (ToM) abilities in adolescents with obesity with and without BED and to examine how they related to emotional and psychopathologic evaluations.
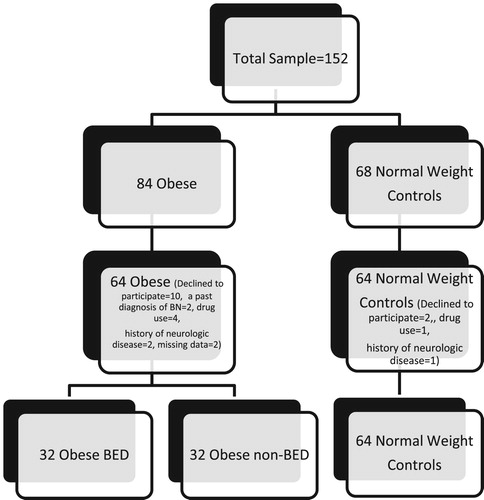
Methods: One hundred twenty-eight adolescents comprising 32 non-BED adolescents with obesity, 32 adolescents with BED and obesity, and 64 healthy controls (HC) completed a battery of tests to analyze their social cognition and clinical psychopathologic profile.
Results: Patients with BED and non-BED patients with obesity showed poorer performance in emotional regulation and social cognition tasks compared with normal-weight adolescents without BED. Various correlations were evident between depression, emotional regulation problems, and eating attitudes and patterns.
Conclusions: Patients with BED and non-BED adolescents with obesity showed a decline in ToM tasks, independent of their clinical psychopathological profile. Consistent with other studies, this is the first study to assess both social cognition and emotion regulation skills in adolescents with BED and obesity.
Introduction
Binge eating disorder (BED) is a pyschiatric disorder that mainly describes as repetitive binge eating episodes, but with no appropriate balancing behaviours and habits to compensate for the weight-gaining effect of excessive intake of food such as in bulimia nervosa (BN) [Citation1]. Some studies reported that patients with BED, less likely to had general psychopathology and greater eating-disordered cognitions to compared with other eating disorders [Citation2–4].
Ranzenhofer et al. [Citation5] reported that girls with BED had poorer quality of life in domains of self-esteem, and social/interpersonal functioning than boys. Also, increasing evidence suggests that a deficit in recognizing own and other’s emotions, the feeling of loss of control over eating, and the correlation between binging and depressive symptoms is a noticeable marker of eating disorder psychopathology in BED [Citation6].
Theory of mind (ToM) is one of the sub-components of social cognition that embraces all the skills necessary to manage social communication and relationships. It raises the consciousness that someone has a mind with various mental states such as belief, intuition, plan, emotion, knowledge, desire and intentions, and that this may be different from one’s own [Citation7,Citation8]. ToM is essential to comprehend the deficiencies in the social functioning of the individual in eating disorders. Because individuals with eating disorders have serious difficulties in understanding and acquiring the opinions of others about body appearance disorders, physical health conditions, treatment needs, and the behavioural consequences of their condition [Citation9].
In recent times, the literature has focused to the field of social cognitive abilities in participiants with eating disorders, mostly focused on anorexia nervosa (AN) and bulimia nervosa (BN), so the results of these studies are controversial [Citation10,Citation11]. ToM has not been evaluated in detail in adolescents with BED. Patients with BED have emotion regulation problems (e.g. [Citation12]) and manifest difficulties in emotion classification (e.g. [Citation13,Citation14]), in addition to undermined levels of interoceptive awareness [Citation6]. The literature suggests that patients with obesity are deprived of the right strategies to manage emotions and binge eating could form a strategy to combat untreated negative emotions [Citation15]. Furthermore, emotional eating, which has continual variable eating attitudes among patients with BED, has been associated with higher levels of alexithymia among binge attacks. Therefore, it has been stated that binge eating could be a pathologic behaviour as a result of a combination of failure to identify and communicate the emotional state of the individual or other individuals, and planning of response prevention strategies or a combination of these two aspects [Citation16].
In the literature, studies have been conducted on obesity and impulsivity, emotional factors, social cohesion and social relations, self-esteem, and accompanying psychopathologies; however, few studies have evaluated social cognitive abilities using appropriate tests for adolescents with exogenous obesity [Citation17].
Binge eating disorder patients have a comparable ability to understand one’s own or others’ emotions but a more impaired capacity to understand and code their own emotions compared with non-BED obese patients [Citation6]. Therefore, binging could be a critical behaviour because of poor problem solving strategies or role in the communication process. Thus, the goal of this study was to evaluate differences in social cognition abilities and emotional regulation difficulties in a sample of adolescents with BED and obesity, adolescents with obesity only, and normal-weight controls to explore the negative or positive correlation with the clinical presentation (i.e. anxiety symptoms, depressive symptoms and eating behaviours). In this context, we hypothesized that (1) an obesity group with BED would show poorer performance than a non-BED obese group and healthy controls, particularly in terms of social cognitive abilities and emotion regulation difficulties; (2) and that binge eating was associated with clinical profile, especially the severity of anxiety and depressive symptoms.
Methods
Participants and procedures
Our study was conducted between April 2017 and April 2018 at Dokuz Eylul University and Katip Çelebi University. Priori power analysis demonstrated that a sample size of 60 participants per group was required based on an 80% power to detect the alpha = 0.05 and a medium effect size (f = 0.25) making use of a MANOVA with two levels and three dependent variables with a 0.05 two-tailed significance level. Diagnostic interviews were conducted with a total 64 participiants with consideration to the 2000 Centers for Disease Control and Prevention (CDC) data; patients with a 95th percentile or more body mass index (BMI) and 64 normal weight adolescents of similar age, biological sex, and pubertal stage with a BMI between the 3rd and 85th percentile were enrolled for the normal weight control (NWC) group.
The obesity group was divided into two equal groups, with and without BED (32 per group) (). All patients were independently examined by two child psychiatrists for BED using an exhaustive evaluation composed of a diagnostic assessment with the adolescent and parents based on the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition [Citation18] criterias, and also determined using the Schedule for Affective Disorders and Schizophrenia for School-Age Children-Lifetime Version (K-SADS-PL) [Citation19]. The exclusion criteria for patients with obesity with or without BED were as follows: a past diagnosis of AN or BN, current or past comorbid diagnosis of any history of trauma with accompanying neurologic disease or prolonged loss of consciousness, current severe medical conditions and use of drugs that may cause obesity, endocrine pathology (e.g. Cushing syndrome, hypothyroidism) syndromic origin obesity, active infection, and unwillingness to contribute (). All participants gave written informed consent before their attendance in the study. The Dokuz Eylul University Ethics Committee approved the study (Date: January 13th, 2017, Number: 1162).
Measures
Emotional and social cognition assessment
To determine particular characteristics in social cognition of the participants, we used four different tasks, the Reading the Mind in the Eyes Test (RMET), the Faces test, the Faux Pas Test (FPT), and the Unexpected Outcomes Test (UOT). The Faces test was established by Ekman in 1987 [Citation20] to identify emotion from faces. In our study, the short form by Baron-Cohen [Citation21] was used, in which 20 photographs reflecting emotional expressions are shown. The RMET was first described by Baron-Cohen et al. in 1997 [Citation21] and modified in [Citation22]. It aims to assess the capability of recognizing the mental state, going beyond simple emotions, by looking at a person's eye expression [Citation22]. The version of the test for children by Girli et al. has been translated into Turkish [Citation23]. The UOT, developed by Dyck et al. in 2001 [Citation24], aims to determine the ability to relate to the causes of emotions and apply reasoning skills in order to explain the apparent conflict between the feelings and the feelings that were revealed during the situations. It was found that the UOT was internally consistent, combined with other emotion recognition and comprehension tests and general cognitive ability, and had good interrater reliability (r = 0.91), and at the same time the validity was shown [Citation25]. Baron-Cohen et al. [Citation26] used tasks of the FPT to evaluate high mental references in addition to other social cognition tests. FPT tasks are considered as a good measurement tool of second-stage ToM impairments; in these tests it is stated that the skill of the person indicates the severity of the mental disorder. Good interrater reliability was demonstrated in a thesis study conducted in Turkey [Citation25].
The Difficulties in Emotion Regulation Scale (DERS) was established by Gratz and Roemer in 2004 [Citation27]. The 5-point Likert scale, which consists of six subscales, evaluates mood regulation in six dimensions. The internal consistency coefficient of the Turkish pyschometric evaluation was found to be 0.93 and test-retest reliability was 0.83 (p < .01, n = 59), similar to the original scale [Citation28].
Clinical assessment
Eating disorder psychopathology: the Eating Disorder Examination Questionnaire (EDE-Q) and Eating Attitudes Test Questionnaire (EAT-40) were used to determine the asperity of eating disorder pyschopathology. The EDE-Q is the self-report version of the Eating Disorder Assessment Interview [Citation29]. In the Turkish psychometric evaluations, the internal consistency coefficient was 0.93 and the test-retest reliability was 0.91 [Citation30]. EAT-40 was created by Garner and Garfinkel in 1979 to determine the attitudes and behaviours of patients with AN and eating problems. Savaşır and Erol found that the Cronbach's alpha internal consistency coefficient of the scale was 0.70, the test-retest reliability of the scale was r = .65 [Citation31].
Depressive symptomatology was evaluated using the Children Depression Inventory (CDI), which was developed by Kovacs in 1992 [Citation32]. The cut-off point is 19 and the highest score is 54. No special training is required to apply the scale. Öy in 1991 [Citation33] found that the Cronbach's alpha internal consistency coefficient of the scale was 0.80, and the test-retest reliability of the scale was r = 0.70.
Anxiety symptomatology was assessed using the State Trait Anxiety Inventory (STAI 1–2), which was established by Spielberger, Gorsuch, and Lushene in 1970 [Citation34]. The reliability and validity study of the Turkish version were conducted by Öner and Le Compte in 1985 [Citation35]. They found the alpha reliability coefficient for the Trait Anxiety Scale was between 0.83 and 0.87 and the alpha reliability coefficient for the State Anxiety Scale was found between 0.94 and 0.96.
Statistical analysis
The differences in all study variables were analyzed using the Statistical Package for the Social Sciences (IBM, NY), version 22 for Windows. Before the statistical analysis was performed, it was checked as to whether the data met the assumptions of the parametric tests, normal distribution, and homogeneity of variance by using the Kolmogorov–Smirnov test. Variables (STAI-TX1, STAI-TX2, EDE-Q, DERS) that did not show normal distribution were evaluated using the a multivariate analysis of variance (MANOVA) test. In the event of multivariate significance, analysis of variance (MANOVA) per test score was performed with subsequent post-hoc Bonferroni tests if distribution assumptions were met. Post hoc comparisons were performed for measures that showed statistically significant differences at the .05 level.
Chi-square analysis was used to compare categorical variables between the groups. Pearson’s correlation test was used to determine the direction and level of correlation between the variables, and the results are indicated using the correlation coefficient (r) and significance level values (p). P < .05 was considered statistically significant. Analyses of covariance were conducted for significant results considering confounding factors.
Results
Result of Sociodemographic Data and Clinical Assesment
summarizes the main features of the participants and the identification of the clinical characteristics between the groups. There were no differences between groups in terms of age, sex, and parental education level (all groups) (). As predicted, BMI scores were lower in the NWC group compared with the other two groups, which did not differ from each other (p** = .071). The obese non-BED group had higher EAT-40 scores when compared with the obese BED group, but there was no statistically significant difference. However, there was a statistically significant difference when compared with the NWC group (p < .05) according to all scores of the EDE-Q except shape concern scores. Additionally, the non-BED obese group showed more anxiety symptom levels than the BED obese and NWC groups, the BED obese group showed more depressive symptom levels than the non-BED obese and NWC groups according to the CDI and STAI 1–2, but there was no statistically significant difference between the BED obese and non-BED obese group.
(2) Comparison of Emotional and Social Cognition Assessment
Table 1. Sociodemographic and clinical characteristics of adolescents with obese BED, non-obese BED and normal weight control groups.
shows the comparison of data of the emotional and social cognition assessments of the participants. The NWC group had significantly higher social cognition total scores than the other two groups. The performance of the obese BED group was also better than in the obese non-BED group in the RMET, Faces test, and UOT scores but there was no statistically significant difference.
Table 2. Results of Emotional and Social Cognition Assessment: means (M), standard deviations (SD), and group differences in obese BED, non-obese BED and normal weight control groups
There was no statistically significant difference between the obese BED and obese non-BED groups in goal, strategy, impulsivity, non-acceptance, and clarity subscales of the DERS scores. When we evaluated the total score of the DERS, there was no statistically significant difference between the three groups (p > .05); however, there was a statistically significant difference between the obese BED group and the other two groups in the awareness subscale of DERS. The obese BED group had higher scores than the other two groups in the awareness subscale of DERS.
Analysis of covariance demonstrated that differences remained significant after adjusting for depression (CDI) and anxiety (STAI 1–2) in all EDE-Q subscales; total score: F(1,54) = 23.265, p < .001, η2 = 0.271; restraint eating: F(1,54) = 18.870, p < .001, η2 = 0.232; eating concern: F(1,54) = 11.451, p < .001, η2 = 0.155; weight concern: F(1,54) = 43.867, p < .001, η2 = 0.505; shape concern: F(1,54) = 34.535, p < .001, η2 = 0.356, EAT-40: F(1,54) = 15.322, p < .001, η2 = 0.432, and all ToM Tasks; Faces test: F(1,54) = 20.085, p < .001, η2 = 0.243; RMET, F(1,54) = 22.538, p < .001, η2 = 0.265; UOT: F(1,54) = 22.006, p < .001, η2 = 0.260; FPT: F(1,54) = 8.342, p = .032, η2 = 0.218; Comprehension test: F(1,54) = 18.240, p < .01, η2 = 0.118.
presents all findings of correlations. In the obese BED group, the EDE-Q eating concern correlated with Faces test scores (rs = −0.355, p < .05); FPT correlated negatively with CDI, the EDE-Q shape concern, and the strategy subscale of DERS scores (rs = −0.399, p < .05; rs = −0.407, p < .05; rs = −0.368, p < .05); BMI and the EDE-Q shape concern correlated with UOT scores (rs = −0.436, p < .05; rs = −0.361, p < .05), and the EDE-Q eating concern correlated with comprehension test scores (rs = −0.387, p < .05). Other clinical factors were not connected with performance in tasks of ToM.
Table 3. Results of the correlation model between social cognitive measures and other clinical variables in the obese BED group.
Discussion
The findings of the current study propose that obesity is a condition that causes individuals to experience physical and spiritual difficulties, resulting in many psychopathologies. The evaluation of social cognitive abilities in children and adolescents with exogenous obesity who have similar psychosocial characteristics to eating disorders along with BED is thought to be critical in terms of both the etiology and clinical course of these diseases. The primary goal of the current study was to investigate emotional and social cognition deficits in subjects with BED and obesity in contrast with normal weight healthy adolescents. In line with this goal, different prospects of emotion regulation were evaluated using the DERS scale and ToM tasks. The second aim was to explore the connection between accomplishments in these tasks with the clinical profile, which was broadly examined. This is the first study to use clinical data and ToM tasks to assess social cognition in adolescents with obesity and BED. We hypothesized that patients with obesity with BED would represent lesser ToM abilities and that this would be independent of their clinical status. The results partially supported the first hypothesis that adolescents with BED and obesity would show poorer performance than normal-weight adolescents without BED in ToM tasks. On the other hand, adolescents with BED did not differ from those in the non-BED-obese group.
In the accumulating scientific literature, studies evaluating emotion recognition and the emotion regulation difficulties of patients with BED are limited compared with other eating disorders. Systematic reviews and meta-analyses based on emotion regulation in BED are restricted to the findings of studies with normal weight healthy groups or focus on obesity rather than BED [Citation36,Citation37]. One study used ToM tasks to examine social cognition deficits in adults with obesity and BED. Aloi et al. [Citation6] observed a comparable capability to recognize others’ emotions but impaired ability in defining and analyzing their self emotions when compared with non-BED patients with obesity. Percinel et al. [Citation25] found that children with obesity had lower scores for all kinds of social cognition task compared with healthy controls. Our findings are partly consistent with the outcomes of other study results. In the Faces test and RMET used to evaluate emotion detection and recognition abilities, the obese group with BED and non-obese group with BED were found to have significantly lower scores than in the NWC group. Therefore, future studies should further explore the role of social cognitive abilities as risk factors in childhood obesity. These findings suggest that patients with obesity have some difficulties in recognition of self emotions and others’ emotions, despite the presence of BED. Our results are coherent with the findings of a study in an adult sample, but they need to be confirmed in studies with larger samples [Citation6].
In a study published in 2019, adolescent emotion regulation difficulties were found more likely to be particularly salient in pathways towards obesity risk [Citation38]. On the other hand, Ruscitti et al. [Citation39] showed that participiants with BED (similar to BN and AN binge/purge subtypes) seemed less prone to reconsider their emotions than women with restrictive subtypes of AN. Furthermore, it has been found that this strategy is used less even when the disease is worse. The results of our study suggest that binge eating episodes can be used to cope with emotional difficulties. Robinson [Citation40] suggested that psychotherapy was beneficial in treatment because it decreased the sensitivity to implicit emotional conflict. In addition, individuals with BED considered the capability to recognize own emotional situations better than patients with other eating disorder subgroups (AN, BN and otherwise not mentioned eating disorders). In contrast, some studies reported difficulty in emotion regulation in BED compared with other eating disorder subgroups [Citation41]. In this respect, considering the emotional difficulties of the participants of our study is considered an important issue in the treatment modalities like Preventing Emotional Eating Routines programme (PEER) [Citation42]. In a systematic review investigating the emotional regulation model in BED and obesity sampling, Leehr et al. found evidence that negative emotions triggered binge eating episodes in the BED group, as distinct from the obese group [Citation43]. Patients with BED tend to suppress their feelings more, and feel their emotions less often when compared with NWCs [Citation44]. Many studies found a positive correlation between anger indeterminity, depression, and binge eating attacks [Citation45].
In our study, when the DERS sub-scales were evaluated, the obese BED group had higher scores in the goal, strategy, awareness, non-acceptance, and total subscales than the other groups, whereas the non-obese BED group had poorer scores than the other groups in the impulsivity and clarity subscales. However, there was no statistically significant difference when compared with the other two groups. In five of the seven subscales, it was found that obese patients with BED received the poorest scores of all subjects, which gives an opinion about why this group performed poorly in their emotional regulation capabilities. Our findings seem to be consistent with research showing that there are difficulties with emotion regulation in patients with BED. In addition, the fact that non-obese patients with BED scored poorer than the other groups in terms of impulsivity subscale scores is consistent with the literature, but the role of BED in this respect should be evaluated in further studies [Citation46,Citation47]. Future studies should investigate the bidirectional interaction role played by emotion regulation strategies in the relationship between BED and obesity.
The “total scale score” (difficulty score in total mood regulation) was obtained by collecting scores from all other subtests. The distinctive feature on this scale is that it assesses the overall difficulty alongside the emotion regulation challenges in six different ways. In our study, when we evaluated all the test scores of all participants, it was determined that the patients with obesity with BED and non-obese patients with BED scored more than the control sample as seen in the subtest scores. Our findings are in agreement with studies reporting that emotion regulation and emotion management skills are impaired in patients with BED [Citation48,Citation41].
Limitations
When considering the results of the current study, some limitations need to be taken into account. Participants with no clinically diagnosed intellectual disability were selected for the study sample, but there may have been differences between the intelligence levels of the participants, which may affect the understanding of the test and giving appropriate responses. Another possible limitation is the higher psychopathology scores of the obese BED group, which would have an effect on the findings if the group differences in ToM and emotion regulation were due to severity of illness. There are also studies evaluating the deterioration of social cognitive functions independent of neurocognitive impairments. The inclusion of neurocognitive tests evaluating brain regions in which social cognitive functions are associated and controlling the impact on social cognition may lead to more reliable findings. Moreover, we did not consider comorbid features such as mood disorders, other neurodevelopmental disorders or eating disorders which can be associated with deteriotaion in ToM variables. Additionally, the cross-sectional pattern of the current study prevents any continuous explications considering the intercourse between social cognition and BED psychopathology. Prospective and longitudinal studies would allow for a deeper understanding of whether and how complexities in social cognition subscribe to the improvement and preservation of the disorder.
Conclusion
The current study examined whether social cognition and emotional regulation add to our understanding of the psychopathology of BED and being overweight. The results of this study may have clinical intimations in the recruitment of social abilities in patients with BED. Thus, proposing individual designs to rehabilitate social abilities, a kind of exercise in social apprehension and grasping the mental situations of others, may be advantageous in this community. It was thought that the findings obtained at the end of the study might be helpful in assessing the biologic factors that may facilitate the effective features of the diseases, and in the improvement of more efficient and permanent treatment approaches, and the adherance of patients to treatment.
Disclosure statement
No potential conflict of interest was reported by the authors.
ORCID
Serkan Turan http://orcid.org/0000-0002-6548-0629
Gonca Özyurt http://orcid.org/0000-0002-0508-0594
Gönül Çatlı http://orcid.org/0000-0002-0488-6377
Ayhan Abacı http://orcid.org/0000-0002-1812-0321
Yeşim Öztürk http://orcid.org/0000-0001-9167-7815
Aynur Pekcanlar Akay http://orcid.org/0000-0001-7535-1735
References
- Grucza RA, Przybeck TR, Cloninger CR. Prevalence and correlates of binge eating disorder in a community sample. Compr Psychiatry. 2007;48(2):124–131.
- Wilfley DE, Schwartz MB, Spurrell EB, et al. Using the eating disorder examination to identify the specific psychopathology of binge eating disorder. Int J Eating Disord. 2000;27:259–269.
- Glasofer DR, Tanofsky-Kraff M, Eddy KT, et al. Binge eating in overweight treatment-seeking adolescents. J Pediatr Psychol. 2007;32(1):95–105.
- Crow SJ, Agras WS, Halmi K, et al. Full syndromal versus sub-threshold anorexia nervosa, bulimia nervosa, and binge eating disorder: a multicenter study. Int J Eating Disord. 2002;32:309–318.
- Ranzenhofer LM, Columbo KM, Tanofsky-Kraff M, et al. Binge eating and weight-related quality of life in obese adolescents. Nutrients. 2012;4(3):167–180.
- Aloi M, Rania M, Caroleo M, et al. Social cognition and emotional functioning in patients with binge eating disorder. Eur Eat Disord Rev. 2017;25:172–178.
- Baron-Cohen S. The theory of mind deficit in autism: how specific is it? British Journal of Developmental Psychology. 1991;9:301–314.
- Martino DJ, Strejilevich SA, Fassi G, et al. Theory of mind and facial emotion recognition in euthymic bipolar I and bipolar II disorders. Psychiatry Res. 2011;189:379–384.
- Tapajoz P de Sampaio F, Soneira S, Aulicino A, et al. Theory of mind and central coherence in eating disorders: two sides of the same coin? Psychiatry Res. 2013;210:1116–1122.
- Adenzato M, Todisco P, Ardito RB. Social cognition in anorexia nervosa: evidence of preserved theory of mind and impaired emotional functioning. PloS One. 2012;7(8):e44414.
- Dejong H, Van den Eynde F, Broadbent H, et al. Social cognition in bulimia nervosa: a systematic review. Eur Psychiatry. 2013;28(1):1–6.
- Zeeck A, Stelzer N, Linster HW, et al. Emotion and eating in binge eating disorder and obesity. Eur Eat Disord Rev. 2011;19(5):426–437.
- Pinaquy S, Chabro H, Simon C, et al. Emotional eating, alexithymia, and binge-eating disorder in obese-women. Obes Res. 2003;11:195–201.
- Villarejo C, Jiménez-Murcia S, Álvarez-Moya E, et al. Loss of control over eating: a description of the eating disorder/obesity spectrum in women. Eur Eat Disord Rev. 2014;22:25–31.
- Dingemans A, Danner U, Parks M. Emotion regulation in binge eating disorder: a review. Nutrients. 2017;9(11):1274.
- Aldao A, Nolen-Hoeksema S, Schweizer S. Emotion-regulation strategies across psychopathology: a meta-analytic review. Clin Psychol Rev. 2010;30(2):217–237.
- Koch A, Pollatos O Reduced facial emotion recognition in overweight and obese children. J Psychosom Res. 2015;pii:S0022-3999(15)00468-7. doi:10.1016/j.jpsychores.2015.06.005.
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed Washington (DC): Author; 2013.
- Kaufman J, Birmaher B, Brent D, et al. Schedule for affective disorders and schizophrenia for school- age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. Journal of the American Academy of Child &Adolescen Psychiatry. 1997;36(7):980–988.
- Ekman P, Friesen WV, O’Sullivan M. Universal and cultural differences in the judgments of facial expressions of emotion. J Pers Soc Psychol. 1987;53(4):712–717.
- Baron-Cohen S, Jolliffe T, Mortimore C, et al. Another advanced test of theory of mind: evidence from very high functioning adults with autism or Asperger syndrome. Journal of Child Psychology and Psychiatry. 1997;38(7):813–822.
- Baron-Cohen S, Wheelwright S, Hill J, et al. The ‘reading the mind in the eyes’ test revised version: A study with normal adults, and adults with Asperger syndrome or high-functioning autism. Journal of Child Psychology and Psychiatry. 2001;42(2):241–251.
- Girli A. Psychometric properties of the Turkish child and adult form of “reading the mind in the eyes test”. Psychology. 2014;05(11):1321–1337.
- Dyck MJ, Ferguson K, Shochet IM. Do autism spectrum disorders differ from each other and from non-spectrum disorders on emotion recognition tests? Eur Child Adolesc Psychiatry. 2001;10:105–116.
- Percinel I, Ozbaran B, Kose S, et al. Increased deficits in emotion recognition and regulation in children and adolescents with exogenous obesity. World J Biol Psychiatry. 2018;19(2):112–118.
- Baron-Cohen S, O'Riordan M, Stone V, et al. Recognition of faux pas by normally developing children and children with Asperger syndrome or high-functioning autism. J Autism Dev Disord. 1999;29(5):407–418.
- Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: development, factor structure, and initial validation of the difficulties in emotion regulation scale. J Psychopathol Behav Assess. 2004;26(1):41–54.
- Saritas D, Gençöz T. Psychometric properties of the difficulties in emotion regulation scale (DERS) in a Turkish adolescent sample. 12th European congress of psychology; Istanbul; 2011.
- Fairburn CG, Cooper Z, O’Connor M. Eating disorder examination (16.0D). In: Fairburn CG, editor. Cognitive behavior therapy and eating disorders. New York, NY: Guilford Press; 2008. p. 309–313.
- Yucel B, Polat A, Ikiz T, et al. The Turkish version of the eating disorder examination questionnaire: reliability and validity in adolescents. Eur Eat Disord Rev. 2011;19:509–511.
- Savaşır I, Erol N. Eating attitude test: anorexia nervosa symptoms index. Journal of Psychology. 1989;7:19–25.
- Kovacs M. Rating scale to depression in school-aged children. Acta Paedopsychiatr. 1980/1981;46:305–315.
- Öy B. Depression scale for children: validity and reliability study. Turkish Journal of Psychiatry. 1991;2(2):132–136.
- Spielberger CD, Gorsuch RL, Lushene RE. Manual for state-trait anxiety inventory. Palo Alto: California Consulting Psychologists Press; 1970.
- Öner N, LeCompte A. State-trait anxiety inventory handbook. 2nd ed İstanbul: Boğaziçi University Press; 1985.
- Kittel R, Brauhardt A, Hilbert A. Cognitive and emotional functioning in binge-eating disorder: a systematic review. Int J Eating Disord. 2015;48:535–554.
- Fernandes J, Ferreira-Santos F, Miller K, et al. Emotional processing in obesity: a systematic review and exploratory meta-analysis. Obesity Review. 2018;E19(1):111–120.
- Shriver L, Dollar J, Lawless M, et al. Longitudinal associations between emotion regulation and adiposity in late adolescence: indirect effects through eating behaviors. Nutrients. 2019;11(3):517. doi:10.3390/nu11030517.
- Ruscitti C, Rufino K, Goodwin N, et al. Difficulties in emotion regulation in patients with eating disorders. Borderline Personal Disord Emot Dysregul. 2016;3:3.
- Robinson A, Safer DL, Austin JL, et al. Does implicit emotion regulation in binge eating disorder matter? Eat Behav. 2015;18:186–191.
- Brockmeyer T, Skunde M, Wu M, et al. Difficulties in emotion regulation across the spectrum of eating disorders. Compr Psychiatry. 2014;55(3):565–571.
- Boutelle KN, Braden A, Knatz-Peck S, et al. An open trial targeting emotional eating among adolescents with overweight or obesity. Eat Disord. 2018;26(1):79–91. doi:10.1080/10640266.2018.1418252.
- Leehr EJ, Krohmer K, Schag K, et al. Emotion regulation model in binge eating disorder and obesity - a systematic review. Neurosci Biobehav Rev. 2015;49:125–134.
- Svaldi J, Caffier D, Tuschen-Caffier B. Emotion suppression but not reappraisal increases desire to binge in women with binge eating disorder. Psychother Psychosom. 2010;79(3):188–190.
- Connolly AM, Rieger E, Caterson I. Binge eating tendencies and anger coping: investigating the confound of trait neuroticism in a non-clinical sample. Eur Eat Disord Rev. 2007;15(6):479–486.
- Schag K, Teufel M, Junne F, et al. Impulsivity in binge eating disorder: food cues elicit increased reward responses and disinhibition. PLoS One. 2013;8:e76542.
- Giel KE, Teufel M, Junne F, et al. Food-related impulsivity in obesity and binge eating disorder—A systematic update of the evidence. Nutrients. 2017;9:1170.
- Gianini LM, White MA, Masheb RM. Eating pathology, emotion regulation, and emotional overeating in obese adults with binge eating disorder. Eat Behav. 2013;14:309–313.