Abstract
This article discusses the correlation between national policy characteristics and the success in “flattening the curve” of infection of the COVID-19 virus, which is a generally acknowledged measure to contain the worst medical outcomes of a pandemic. While individual cases require careful and granular analysis to properly unpack, the article finds that the best correlation is found when looking at the pattern of choice related to either proactive or reactive approaches to the implementation of containment measures. This is especially evident for countries that have either very low or very high infection rates per million persons. For intermediate rates we find that a variety of institutional, political, and procedural variables intervene in the process.
Introduction
Policy making during a pandemic presents two main challenges: on the one hand it is very complex because it must address multiple policy fields and be implemented at a variety of jurisdictional levels (Bennett and Carney Citation2015), affecting the health care, social, economic, and public security policy fields and creating unique challenges (Carney and Bennett Citation2014; Keller Citation2019). On the other hand, especially early in the pandemic, it requires initial containment responses that often appear out of scale with the early level of threat. At this time, policy makers must rely on limited, emerging scientific knowledge and therefore preexisting beliefs and plans about variables such as disease severity and the impact on the health care system can deeply affect the choices that are made (Rosella et al. Citation2013). Generally, however, containment policies are the approach of choice followed by most jurisdictions faced with a pandemic and the COVID-19 outbreak proved no exception to this rule.
However, containment measures can help reduce transmission but can also be controversial (Smith et al. Citation2012). If we limit our consideration to calculating their economic impact, public officials practically are faced with balancing economic and health risks in what often resembles a zero-sum game (Anderson et al. Citation2020). For example, a lockdown decision like that imposed by the Chinese or Italian governments can have very extensive effects in a globalized world, generally increasing individual costs, work disruptions, increased hospital care, and sick leave (Fan, Jamison, and Summers Citation2016; Gasparini et al. Citation2012). Broadly restricting the capacity of citizens and organizations to operate, work and travel means accepting that an economy will contract significantly, jobs will be lost and major uncertainly will emerge in the world economy (Nicola et al. Citation2020). Hence, policy decisions addressing pandemic management in the health sector create new issues in other policy fields forcing decision-makers and administrator to calculate ancillary cost-benefit distributions. Is it better to approach COVID-19 by keeping the economy running while trying to protect the most vulnerable like Sweden (Pierre Citation2020) and South Korea (Lee, Hwang, and Moon Citation2020) did, implement a mixed model supported by broad financial support (Migone Citation2020) as Canada chose to, or develop a national lockdown as Italy did (Capano Citation2020)?
Practically, pandemic management means that public administrators must deal with everything from regulating social distancing, developing protocols for international trade and travel, creating economic support packages for businesses and individuals, and managing medical responses. All of these possible policy choices involves multiple options in terms of implementation and often requires a granular focus on specific groups like health care workers (Maunder et al. Citation2008) and populations at risk (O’Sullivan and Phillips Citation2019), an example here being how COVID-19 struck the elderly particularly hard (Daoust Citation2020). To further complicate the policy landscape, each of these policies has a broad range of choices available, such as the tensions that have emerged about limiting individual choice through lockdowns and wearing masks, but is also dependent on how prepared a country is at the onset of the pandemic (Capano Citation2020). Each one of these areas can generate complex policy and political issues: both domestically, consider the conflict that emerged about whether wearing masks was necessary in the West (Tso and Cowling Citation2020; Vogel Citation2020), and internationally when countries apply very different approaches, like Canada and the United States did, but traditionally share large flows of tourists, travelers, and commerce.
Hence, national policy responses to pandemics vary (Silva et al. Citation2015) and are politically, culturally, and historically mediated (Tyshenko and Paterson Citation2010) and can be affected by partisan politics (Kushner Gadarian, Goodman, and Pepinsky Citation2020). Furthermore, pandemic management must engage a very large portion of the population to be successful and this presents decision-makers with important challenges in terms of aligning emergency policy-making with their political vision and leadership approaches, working with the extant policy styles that are dominant in their jurisdictions (Richardson, Gustaffson, and Grant Citation1982), and in dealing with the capacity of the institutions that are in charge of the response as was exemplified by the discussion surrounding behavioral choices in the UK in the early stages of the spread of COVID-19 (Sibony Citation2020). This article is divided in three parts: after this introduction, section two briefly discusses our approach to measuring COVID-19 containment responses and presents the data, finally some conclusions are offered.
Measuring COVID-19 containment responses
This article focuses on policy responses aimed at containing the COVID-19 pandemic for the period between January and June 2020. This timeframe is long enough to accommodate a variety of early policy choices but does not extend into a more “routinized” management of the pandemic. Containment interventions and their timing when dealing with influenza pandemics are subject to a mix of costs and results that are not linearly distributed (Hollingsworth et al. Citation2011). For example, Anderson et al. (Citation2020) note how different approaches to pandemic management, and therefore infection rates, carry different mixes of economic/health costs: case isolation means that cases peak early limiting economic issues but could potentially strain the health care system, resulting in more deaths. If social distancing policies are applied throughout the epidemic, this flattens the curve but has greater economic impacts, and a time-limited more effective social distancing is often followed by a new peak in infections, potentially exacerbating the situation. This article chooses, somewhat subjectively but in line with the majority of the countries analyzed, to measure the relative success/failure of these containment polices on the basis of the rate of infection per million persons in each jurisdiction. Measuring policy success is always complicated and subjective (Newman Citation2014), and in particular measuring COVID-19 responses presents a series of complex challenges (George et al. Citation2020), but we believe that this measure can be justified in two ways: on the one hand it has been adopted as a shorthand for success in the containment of the pandemic by a majority of countries around the world. The second is that the data is available for all the countries in the sample even if we are aware of the fact that different jurisdiction record this type of information differently. In terms of selecting which countries were included in our sample, we decided to include all of the OECD countries, Asian countries and as many African and South American countries as we could for which high enough numbers of tests per million inhabitants were in place (only countries that had at least 1,000 tests per million people were included). This meant that we excluded countries that might be very interesting to examine, but that had extremely low tests per million inhabitants, such as Nigeria.
A limitation of the data is that it measures national dimensions: federal jurisdictions like the United States, Canada, or Germany have important sub-national dimensions both in terms of their institutional structures and of the organization of their health care system that are not captured here. Within these limitations we hope to provide a general snapshot for these jurisdictions that can be augmented and refined by further analysis. The resulting sample is composed of 46 countries from all continents, which are presented in below. The table includes the number of confirmed cases, the number of confirmed deaths and the number of tests, all per million population. To facilitate the analysis, countries are somewhat arbitrarily divided in five distinct groups based on how many confirmed cases per million have been reported ().
Table 1. COVID-19 Data for Select Jurisdictions.
Table 2. Ranking of countries by confirmed COVID-19 cases per million.
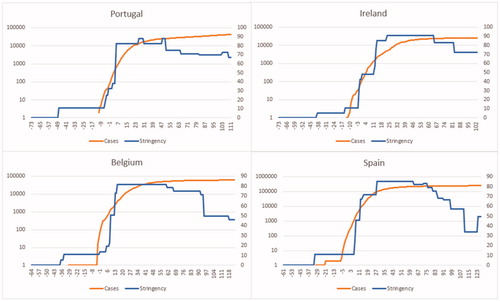
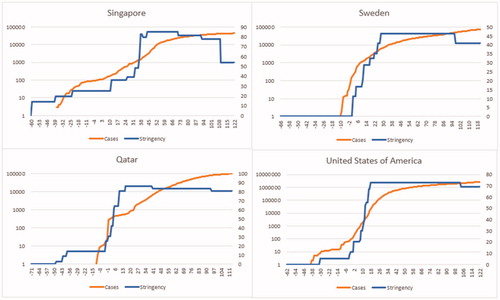
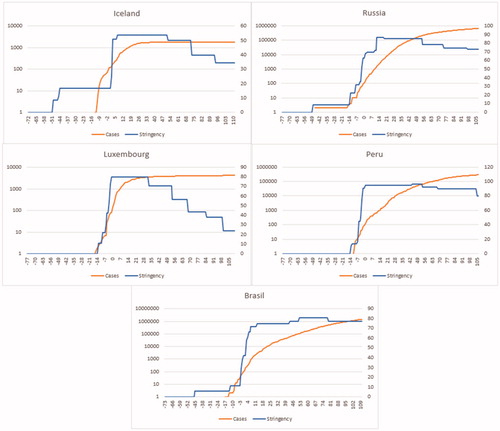
Containment measures have been shown to help with the management of pandemics (Halder, Kelso, and Milne Citation2010; Kelso et al. Citation2013) and can have very important effects for high-risk populations (O’Sullivan and Phillips Citation2019), especially if they are properly contextualized with public engagement (Joint Centre for Bioethics Pandemic Ethics Working Citation2009). However, their application and scope vary among jurisdictions (Ren Citation2020) and they have very broad effects on socio-economic variables (Bonaccorsi et al. Citation2020), which makes their implementation a matter of political and practical debate. This section looks at the correlation between how stringent national policies have been in managing social distancing and public interactions and the rate of growth in the number of confirmed COVID-19 cases. The policy data comes from the Stringency Index developed at the Blavatnik School for Government by Hale, Webster et al. (Citation2020). The data for confirmed cases is charted on a logarithmic scale and the zero value represents the day when the jurisdiction reported at least 100 confirmed cases of COVID-19. This allows us to trace the percentage change in infections – our measure of success being the so called “bending of the curve” – in relationship with the level of stringency of containment policies imposed by the national government. Even within these groups there is variation, this depends on the fact that these measures are very high level and to an extent proxies: for example, the stringency index does not speak to compliance. Furthermore, when discussing containment policies in the field of pandemics, the role of organizations like the World Health Organization (WHO) in setting priorities is very important but, we know that individual jurisdictions retain important degrees of independence in their choices. For example, many countries adopted containment measures as a package and at the same time, contrary to the WHO’s advice of scaling the adoption in the light of the virus’ behavior (Hale, Angrist, et al. Citation2020). Nonetheless, some common trends can be highlighted; we now turn to the analysis of each group of jurisdictions.
Very low rate of infections
Among the countries with very low infection rates as of early July 2020, we can find four patterns. Many intervened early on with containment measures that either kept ahead of the increasing rate of infection, or that matched it closely. A small group, comprising Thailand, South Korea, Japan and Australia lagged the infection rate very early on but escalated their policy intervention as they came close to 100 confirmed cases. Finally, we find a group of five countries that while currently having very low rates of infection per million population, have not managed to slow the growth of the infection. We should note that all of these countries are very diverse institutionally, historically, demographically and in terms of capacity, hinting perhaps at the importance of early intervention above these other variables.
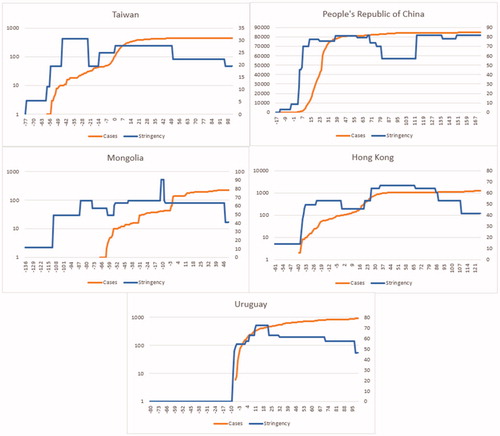
In the first subgroup are present Taiwan, the People’s Republic of China (PRC), Mongolia, Hong Kong and Uruguay (see ), countries that always moved proactively with regard to the infection pattern with their containment policies. One of the distinctive elements in this group is that there are relatively different levels of stringency in their approaches: from the very low stringency approach in Taiwan, where policy-makers relied on collective efforts, trust in institutions that was built on the experiences of the 2003 SARS pandemic, and on early intervention (Huang Citation2020), to the more stringent one in the PRC (Mei Citation2020).
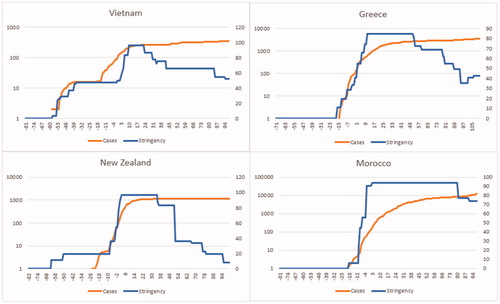
In the second subgroup we find that early on containment policies lagged the rate of infection but they were followed by patterns of policy escalation, which appear to have curbed the pandemic (see below).
Explaining these results is likely to be more complex, with elements such as compliance, leadership, and capacity coming into play, but we can certainly note a similar pattern to the one highlighted above. The exception being Vietnam, which seems to have fallen behind the stringency curve not once, but twice and yet has managed to do extremely well because of very good communication and a high level of early cooperation among all stakeholders (La et al. Citation2020). Early movers seem to have enjoyed a strong return on their policy investment and most of them either never reached very high stringency levels, like Taiwan and Mongolia, or were able to decrease them, like Vietnam, Greece and New Zealand.
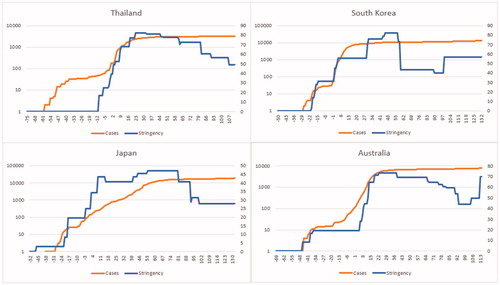
The countries in the third subgroup lagged the growing infection rate early on but responded by sharply escalating at a time when very few cases were confirmed and this appears to have been a successful approach. Japan, Australia, Thailand and South Korea (See below) all have proven the importance of knowledge from previous pandemics and strong institutional structures that reacted proactively to the virus’ dynamics (Bello Citation2020; Lee, Hwang, and Moon Citation2020; Moloney and Moloney Citation2020; Tashiro and Shaw Citation2020).
These four jurisdictions present relatively similar dynamics in terms of policy approach and, with the exception of Australia, they all proactively escalated their containment policies well before the country reached 100 confirmed cases.
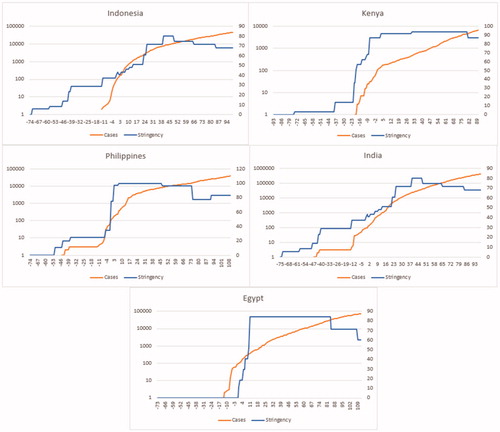
The final subgroup of countries comprises jurisdictions that have low infection rates and, with the exception of Egypt, appeared to have acted proactively with their containment policies but that still have been unable to “flatten the curve.” More granular research is needed to explain these dynamics but it is unlikely to be a coincidence that all of these jurisdictions are developing nations that have very high urban densities and have economic and health care dynamics are likely to force many people into difficult choices between containment and economic survival (Ntoumi and Velavan Citation2020).
Ultimately, countries that managed the COVID-19 pandemic using early policy (See ) interventions proactively and managed to engage the public like Taiwan (Huang Citation2020), Greece (Tsiotas and Magafas Citation2020) and New Zealand (Duckett Citation2020; Wilson Citation2020) have reaped very important benefits, including a uniformly extremely low rate of death per million people; this extends even to countries that have struggled to reduce the rate of growth in the number of new infections.
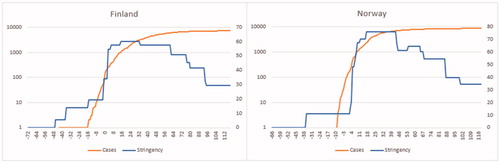
Low rate of infections
Only Finland and Norway reported infection rates between 1000 and 2000 people per million and both show some lagging in the early phase of containment policy with a quick escalation at the point when infection neared 100 people. It should also be noted that Finland did escalate quickly its stringency policies and compliance allowed them to later not reach as high a peak of stringency as some other countries had to (See below).
However, what is in place in both countries is the use of evidence informed decision making linked to health institutes (Fretheim, Brurberg, and Forland Citation2020; Moisio Citation2020) and, especially in the Finnish case, a very strong intervention of the state that framed the discussion around COVID-19 as a national security issue (Moisio Citation2020). This has apparently enabled an effective containment policy even if more granular analysis would be needed to unpack the process.
Moderate rate of infections
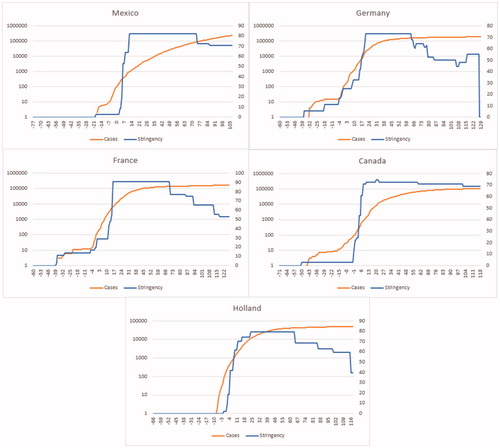
This group represents various policy approaches (See below). The Netherlands initially embraced a policy aimed at developing herd immunity, but sharply reversed course later. Other jurisdictions, like Germany and Canada, instead attempted to match policy changes to increased rates of confirmed infections in a bid to maintain the capacity of their decentralized medical systems (Kirchhof Citation2020; Migone Citation2020), whereas in Mexico the impact of the virus was complicated by low levels of trust in the capacity of the authorities to handle the emergency and by the very much delayed response that the federal political structure, especially President López Obrador chose in the face of the pandemic. In turn this may be due to the state of flux in the institutional structure of the country at the onset of the pandemic (Caldera-Villalobos et al. Citation2020). In the case of Mexico, these variables may account for the fact that the country could not significantly reduce its rate of infection. Five of these jurisdictions tended to lag their policy responses. Various explanations are possible: from the complexity in managing federal and decentralized systems, to political and institutional dynamics. In France, further to the lag in containment policies, issues of compliance and political divisions seem to have reduced the effectiveness of the interventions (Ghanchi Citation2020).
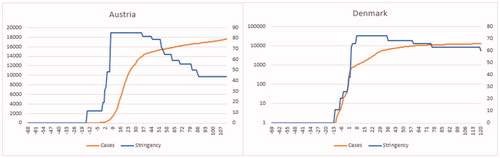
Austria and Denmark, however show a similar pattern to countries in the low and very low categories, and implemented relatively strict containment policies that led the infection rate (See below).
More granular research will be needed to assess both the policy patterns and to unpack some of the health outcomes like the very broad range in mortality per million population in this group, but containment policies, even if they do not lead the infection rate by much, can be very effective, especially if communication with citizens is clear and open and trust levels are high (Moshammer et al. Citation2020; Olagnier and Mogensen Citation2020).
High rate of infections
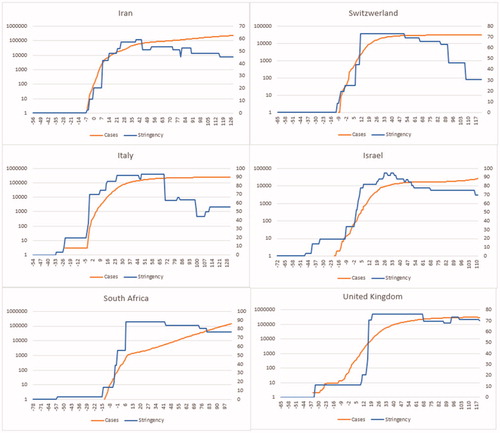
This group has both much higher rates of infection per million and higher mortality rates while containment policies include different approaches: ranging from Great Britain where the initial approach was to create immunity in the population (Kirchhof Citation2020) to Israel where disproportionate policy responses prevailed (Maor, Sulitzeanu-Kenan, and Chinitz Citation2020). Italy itself is a complex case to unpack because capacity gaps among institutions are dramatic (Gatto et al. Citation2020) and where regionally delivered health care meant very different approaches at the local level (Capano Citation2020), with Lombardy taking on a more reactive approach and paying an enormous price for it. Within this group are Iran and South Africa, two countries that have been unable to “flatten the curve.” In Iran, insufficient institutional coordination and lack of access to personal protective equipment and medicines limited the effectiveness of contextual containment policies (Raoofi et al. Citation2020), further reinforcing the perception that the long term evolution of the pandemic will depend on a variety of dynamics, including preparedness (Gilbert et al. Citation2020). The patterns in the containment policies for these countries are not dramatically different from some of the ones we have seen in the group showing moderate infection rates, Germany and Holland being good examples of these better results, and yet we find both higher infection rates and, at least in the cases of Iran and South Africa, difficulty in flattening the rate of infection (See below).
Aside from cases, like Great Britain, where policy decisions were made against containment early on, this group appears to suggest that institutional and capacity factors coupled with even a mild lag in the containment stringency can lead to problematic results.
Very high rate of infections
Finally, we grouped jurisdictions that recorded rates of infection above 4500 persons per million. These countries can be further divided in two subgroups: the first chose a reactive approach, with containment policies lagging the infection rate and often allowing a relatively steep increase in confirmed cases to go unchecked early (See ). The second group, composed of Russia, Iceland, Luxembourg, Peru and Brazil while showing a proactive approach failed to moderate the growth in infections. Another commonality is that a variety of these countries continue to struggle with climbing infection rates.
Among the jurisdictions in this group we find countries like Sweden (Pierre Citation2020) and the United States (Rocco, Béland, and Waddan Citation2020) where the choice was to be reactive and others, like Singapore, where failure to protect migrant workers, who live in cramped conditions and tend to be “forgotten” by official policy, from infection seem to have driven the results (Woo Citation2020) (See ).
The second subgroup includes countries that, at least formally, show a pattern of proactive containment policies (See ) but that in some cases like Brazil under President Bolsonaro had politically mixed messages (Crokidakis Citation2020) or because of the size and density of their population, like Luxembourg, presented a more complex challenge in unpacking the causal patterns. In Peru, for example, the application of containment measures was able to sharply mitigate the infection rate, but it could not prevent the enormous strain that the pandemic placed on the medical system (Gonzales-Castillo et al. Citation2020). The Russian example demonstrates the importance of leadership in highly centralized and usually proactive systems. While focused on sending medical help to foreign countries and closing access from China early on, the Russian leadership initially minimized the threat of the virus for Russia and the following measures remained uncoordinated, with continued communication issues (Åslund Citation2020).
In Iceland the focus was on widespread tracing and testing aiming at ensuring the viability of the health care system and protecting the most vulnerable members of society (Sen-Crowe, McKenney, and Elkbuli Citation2020), which appears to have been successful in that the mortality rate is very low considering the extremely high rate of infection.
This group seems to suggest that reactive policy approaches to containment of COVID-19, whether this depended on poor communication, institutional and political dissonance, lack of trust or a specific choice, led to very high numbers of infections and very often high death rates. A specific note must be made for Brazil and Russia: in both countries the top political leadership minimized the threat of the virus at every turn but the policy stringency still led the number of infections early on. It seems logical to assume that many people would have disregarded public health notices in the face of contrasting communication from their leaders and this underscores the importance of correct communication during a pandemic from the authorities.
Conclusions
This article aims to provide a high-level snapshot of possible correlations between either anticipatory or reactive approaches to COVID-19 containment policies and the rate of confirmed cases in various jurisdictions. At the same time, these categories are grounded in complex structural foundations and simple incremental adjustments are unlikely to make too much of a difference in outcomes. As such, the results are general and we should be cautious with them: while COVID-19 responses in the various jurisdictions were reviewed as part of the research, much more in-depth analysis is needed to understand and explain specific results. However, some general comments can be put forward. First, countries that acted early and proactively fared better. This appears to hold independently from how strict the final policies were: Australia, Japan and South Korea targeted early on the spread of the disease and generally the Stringency Index was relatively low. Countries like Spain and Belgium ramped up their policy measures dramatically but appear to have done so after the window of opportunity had closed and very stringent rules seem to have had limited effect on medical outcomes. With the exception of the first group, we find that the mortality rate per million population is very broadly distributed. Countries that have basically the same infection rate per million like Italy and Israel or Belgium and Iceland have staggeringly different mortality rates. While the reporting of causes of death differs among countries many of these variations seem to imply that once the initial window is missed the relative difference in factors like treatment capacity, the protection offered to vulnerable populations, and the effectiveness of the health care system have important effects. Another trend that is evident through the various groups is that, outside countries like the United States and Sweden where the early policy approach was not containment, the countries that are struggling most with reducing infection rates are developing ones, replicating the pattern that is evident within countries where people in more precarious economic conditions are hit harder (Patel et al. Citation2020).
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Anderson, R. M., H. Heesterbeek, D. Klinkenberg, and T. D. Hollingsworth. 2020. “How Will Country-Based Mitigation Measures Influence the Course of the COVID-19 Epidemic?” Lancet (London, England) 395 (10228): 931–934. doi:10.1016/S0140-6736(20)30567-5.
- Åslund, A. 2020. “Responses to the COVID-19 Crisis in Russia, Ukraine, and Belarus.” Eurasian Geography and Economics 0 (0): 1–14. 10.1080/15387216.2020.1778499.
- Bello, W. 2020. How Thailand Contained COVID-19 - FPIF. Foreign Policy In Focus June 3. https://fpif.org/how-thailand-contained-covid-19/
- Bennett, B., and T. Carney. 2015. “Planning for Pandemics: Lessons from the Past Decade.” Journal of Bioethical Inquiry 12 (3): 419–428. doi:10.1007/s11673-014-9555-y.
- Bonaccorsi, G., F. Pierri, M. Cinelli, F. Porcelli, A. Galeazzi, A. Flori, A. L. Schmidth, et al. 2020. “Economic and Social Consequences of Human Mobility Restrictions Under COVID-19 (SSRN Scholarly Paper ID 3573609).” Social Science Research Network. 10.2139/ssrn.3573609. doi:10.1073/pnas.2007658117
- Caldera-Villalobos, C., I. Garza-Veloz, N. Martínez-Avila, I. Delgado-Enciso, Y. Ortiz-Castro, G. A. Cabral-Pacheco, and M. L. Martinez-Fierro. 2020. “The Coronavirus Disease (COVID-19) Challenge in Mexico: A Critical and Forced Reflection as Individuals and Society.” Frontiers in Public Health 8: 337. doi:10.3389/fpubh.2020.00337.
- Capano, G. 2020. “Policy Design and State Capacity in the COVID-19 Emergency in Italy: If You Are Not Prepared for the (Un)Expected, You Can Be Only What You Already Are.” Policy and Society 39 (3): 326–344. doi:10.1080/14494035.2020.1783790.
- Carney, T., and B. Bennett. 2014. “Framing Pandemic Management: New Governance, Science or Culture?” Health Sociology Review 23 (2): 136–147. doi:10.1080/14461242.2014.11081968.
- Crokidakis, N. 2020. “COVID-19 Spreading in Rio De Janeiro, Brazil: Do the Policies of Social Isolation Really work??” Chaos Solitons Fractals 136: 109930. doi:10.1016/j.chaos.2020.109930.
- Daoust, J.-F. 2020. “Elderly People and Responses to COVID-19 in 27 Countries.” Plos ONE 15 (7): e0235590. doi:10.1371/journal.pone.0235590.
- Duckett, S. 2020. “Governance Lessons from COVID-19.” Australian Health Review : A Publication of the Australian Hospital Association 44 (3): 335. doi:10.1071/AHv44n3_ED1.
- Fan, V. Y., D. T. Jamison, and L. H. Summers. 2016. The Inclusive Cost of Pandemic Influenza Risk (Working Paper No. 22137; Working Paper Series). Cambridge, MA: National Bureau of Economic Research. 10.3386/w22137.
- Fretheim, A., K. G. Brurberg, and F. Forland. 2020. “Rapid Reviews for Rapid Decision-Making During the Coronavirus Disease (COVID-19) Pandemic, Norway, 2020.” Eurosurveillance 25 (19), 13–15. doi:10.2807/1560-7917.ES.2020.25.19.2000687.
- Gasparini, R., D. Amicizia, P. L. Lai, and D. Panatto. 2012. “Clinical and Socioeconomic Impact of Seasonal and Pandemic Influenza in Adults and the Elderly.” Human Vaccines & Immunotherapeutics 8 (1): 21–28. doi:10.4161/hv.8.1.17622.
- Gatto, M., E. Bertuzzo, L. Mari, S. Miccoli, L. Carraro, R. Casagrandi, and A. Rinaldo. 2020. “Spread and Dynamics of the COVID-19 Epidemic in Italy: Effects of Emergency Containment Measures.” Proceedings of the National Academy of Sciences of the United States of America 117 (19): 10484–10491. doi:10.1073/pnas.2004978117.
- George, B., B. Verschuere, E. Wayenberg, and B. L. Zaki. 2020. “A Guide to Benchmarking COVID‐19 Performance Data.” Public Administration Review 80 (4): 696–700. doi:10.1111/puar.13255.
- Ghanchi, A. 2020. “Adaptation of the National Plan for the Prevention and Fight against Pandemic Influenza to the 2020 COVID-19 Epidemic in France.” Disaster Medicine and Public Health Preparedness : 1–3. 10.1017/dmp.2020.82.
- Gilbert, Marius, Giulia Pullano, Francesco Pinotti, Eugenio Valdano, Chiara Poletto, Pierre-Yves Boëlle, Eric D’Ortenzio, et al. 2020. “Preparedness and Vulnerability of African Countries Against Importations of COVID-19: A Modelling Study.” The Lancet 395 (10227): 871–877. doi:10.1016/S0140-6736(20)30411-6.
- Gonzales-Castillo, J. R., L. Varona-Castillo, M. G. Dominguez-Morante, and V. R. Ocaña-Gutierrez. 2020. “Pandemia de la COVID-19 y las Políticas de Salud Pública en el Perú: marzo-Mayo 2020/COVID-19 Pandemic and Public Health Policies in Peru: March–May 2020.” Revista de Salúd Publica; Bogota 22 (2): 1–9.
- Halder, N., J. K. Kelso, and G. J. Milne. 2010. “Analysis of the Effectiveness of Interventions Used During the 2009 a/H1N1 Influenza Pandemic.” BMC Public Health 10 (1): 168. doi:10.1186/1471-2458-10-168.
- Hale, T., S. Webster, A. Petherick, T. Phillips, and B. Kira. 2020. Oxford COVID-19 Government Response Tracker. Oxford: Blavatnik School of Government.
- Hale, T., N. Angrist, B. Kira, R. G. Goldszmidt, A. Petherick, and T. Phillips. 2020. Pandemic Governance Requires Understanding Socioeconomic Variation in Government and Citizen Responses to COVID-19 (SSRN Scholarly Paper ID 3641927). Social Science Research Network. https://papers.ssrn.com/abstract=3641927
- Hollingsworth, T. D., D. Klinkenberg, H. Heesterbeek, and R. M. Anderson. 2011. “Mitigation Strategies for Pandemic Influenza A: Balancing Conflicting Policy Objectives.” PLoS Computational Biology 7 (2): e1001076. doi:10.1371/journal.pcbi.1001076.
- Huang, I. Y.-F. 2020. “Fighting COVID-19 Through Government Initiatives and Collaborative Governance: The Taiwan Experience.” Public Administration Review 80 (4): 665–670. doi:10.1111/puar.13239.
- Joint Centre for Bioethics Pandemic Ethics Working. 2009. “Public Engagement on Social Distancing in a Pandemic: A Canadian Perspective.” The American Journal of Bioethics 9 (11): 15–17. doi:10.1080/15265160903197598.
- Keller, A. 2019. “The Challenges of Building Pandemic Response Systems Based on Unique Cases 2003 SARS, 2009 A(H1N1) and 2014 Ebola Epidemic.” In Managing the Global Health Response to Epidemics: Social Science Perspectives, edited by M. Bourrier, N. Brender, and C. Burton-Jeangros, 21–69. London: Routledge.
- Kelso, J. K., N. Halder, M. J. Postma, and G. J. Milne. 2013. “Economic Analysis of Pandemic Influenza Mitigation Strategies for Five Pandemic Severity Categories.” BMC Public Health 13: 211. http://dx.doi.org.ezproxy.lib.ryerson.ca/10.1186/1471-2458-13-211. doi:10.1186/1471-2458-13-211.
- Kirchhof, P. 2020. “A Tale of Two Countries: How Decentralized Organization and Long-Term Investment Build Resilient Healthcare Systems.” European Heart Journal. Quality of Care & Clinical Outcomes 6 (3): 201–203. qcaa036. doi:10.1093/ehjqcco/qcaa036.
- Kushner Gadarian, S., S. W. Goodman, and T. B. Pepinsky. 2020. Partisanship, Health Behavior, and Policy Attitudes in the Early Stages of the COVID-19 Pandemic (SSRN Scholarly Paper ID 3562796). Social Science Research Network. 10.2139/ssrn.3562796.
- La, V.-P., T.-H. Pham, M.-T. Ho, M.-H. Nguyen, K.-L. P. Nguyen, T.-T. Vuong, H.-K T. Nguyen, et al. 2020. “Policy Response, Social Media and Science Journalism for the Sustainability of the Public Health System amid the COVID-19 Outbreak: The Vietnam Lessons.” Sustainability 12 (7): 2931. doi:10.3390/su12072931.
- Lee, S., C. Hwang, and M. J. Moon. 2020. “Policy Learning and Crisis Policy-Making: Quadruple-Loop Learning and COVID-19 Responses in South Korea.” Policy and Society 39 (3): 363–381. doi:10.1080/14494035.2020.1785195.
- Maor, M.,. R. Sulitzeanu-Kenan, and D. Chinitz. 2020. “When COVID-19, Constitutional Crisis, and Political Deadlock Meet: The Israeli Case from a Disproportionate Policy Perspective.” Policy and Society 39 (3): 442–457. doi:10.1080/14494035.2020.1783792.
- Maunder, R. G., M. Leszcz, D. Savage, M. A. Adam, N. Peladeau, D. Romano, M. Rose, and R. B. Schulman. 2008. “Applying the Lessons of SARS to Pandemic Influenza.” Canadian Journal of Public Health = Revue canadienne de sante publique 99 (6): 486–488. doi:10.1007/BF03403782.
- Mei, C. 2020. “Policy Style, Consistency and the Effectiveness of the Policy Mix in China’s Fight Against COVID-19.” Policy and Society 39 (3): 309–325. doi:10.1080/14494035.2020.1787627.
- Migone, A. R. 2020. “Trust, but Customize: Federalism’s Impact on the Canadian COVID-19 Response.” Policy and Society 39 (3): 382–402. doi:10.1080/14494035.2020.1783788.
- Moisio, S. 2020. “State Power and the COVID-19 Pandemic: The Case of Finland.” Eurasian Geography and Economics : 1–8. 10.1080/15387216.2020.1782241.
- Moloney, K., and S. Moloney. 2020. “Australian Quarantine Policy: From Centralization to Coordination with Mid-Pandemic COVID-19 Shifts.” Public Administration Review 80 (4): 671–682. doi:10.1111/puar.13224.
- Moshammer, H., M. Poteser, K. Lemmerer, P. Wallner, and H.-P. Hutter. 2020. “Time Course of COVID-19 Cases in Austria.” International Journal of Environmental Research and Public Health 17 (9): 3270. doi:10.3390/ijerph17093270.
- Newman, J. 2014. “Measuring Policy Success: Case Studies from Canada and Australia.” Australian Journal of Public Administration 73 (2): 192–205. doi:10.1111/1467-8500.12076.
- Nicola, M., Z. Alsafi, C. Sohrabi, A. Kerwan, A. Al-Jabir, C. Iosifidis, M. Agha, and R. Agha. 2020. “The Socio-Economic Implications of the Coronavirus Pandemic (COVID-19): A Review .” International Journal of Surgery (London, England) 78: 185–193. doi:10.1016/j.ijsu.2020.04.018.
- Ntoumi, F., and T. P. Velavan. 2020. “COVID-19 in Africa: Between Hope and Reality.” The Lancet Infectious Diseases. doi:10.1016/S1473-3099(20)30465-5.
- O’Sullivan, Tracey L., and Karen P. Phillips. 2019. “From SARS to Pandemic Influenza: The Framing of High-Risk Populations.” Natural Hazards (Dordrecht, Netherlands) 98 (1): 103–117. doi:10.1007/s11069-019-03584-6.
- Olagnier, D., and T. H. Mogensen. 2020. “The Covid-19 Pandemic in Denmark: Big Lessons from a Small Country.” Cytokine & Growth Factor Reviews 53: 10–12. doi:10.1016/j.cytogfr.2020.05.005.
- Patel, J. A., F. B. H. Nielsen, A. A. Badiani, S. Assi, V. A. Unadkat, B. Patel, R. Ravindrane, and H. Wardle. 2020. “Poverty, Inequality and COVID-19: The Forgotten Vulnerable.” Public Health 183: 110–111. doi:10.1016/j.puhe.2020.05.006.
- Pierre, J. 2020. “Nudges Against Pandemics: Sweden’s COVID-19 Containment Strategy in Perspective.” Policy and Society 39 (3): 478–493. doi:10.1080/14494035.2020.1783787.
- Raoofi, A., A. Takian, A. A. Sari, A. Olyaeemanesh, H. Haghighi, and M. Aarabi. 2020. “COVID-19 Pandemic and Comparative Health Policy Learning in Iran.” Archives of Iranian Medicine 23 (4): 220–234. doi:10.34172/aim.2020.02.
- Ren, X. 2020. “Pandemic and Lockdown: A Territorial Approach to COVID-19 in China, Italy and the United States.” Eurasian Geography and Economics : 1–12. 10.1080/15387216.2020.1762103.
- Richardson, J., G. Gustaffson, and J. Grant. 1982. “The Concept of Policy Style.” In Policy Styles in Western Europe, edited by J. Richardson, 1–14. Crows Nest: George Allen & Unwin.
- Rocco, P., D. Béland, and A. Waddan. 2020. “Stuck in Neutral? Federalism, Policy Instruments, and Counter-Cyclical Responses to COVID-19 in the United States.” Policy and Society 39 (3): 458–477. doi:10.1080/14494035.2020.1783793.
- Rosella, L. C., K. Wilson, N. S. Crowcroft, A. Chu, R. Upshur, D. Willison, S. L. Deeks, et al. 2013. “Pandemic H1N1 in Canada and the Use of Evidence in Developing Public Health Policies-A Policy Analysis.” Social Science & Medicine (1982) 83 (Complete): 1–9. doi:10.1016/j.socscimed.2013.02.009.
- Sen-Crowe, B., M. McKenney, and A. Elkbuli. 2020. “COVID-19 Response and Containment Strategies in the US, South Korea, and Iceland: Lessons Learned and Future Directions.” The American Journal of Emergency Medicine 38 (7): 1537–1539. doi:10.1016/j.ajem.2020.04.072.
- Sibony, A.-L. 2020. “The UK COVID-19 Response: A Behavioural Irony?” European Journal of Risk Regulation 11 (2): 350–358. doi:10.1017/err.2020.22.
- Silva, M. L., L. Perrier, J. M. Cohen, W. J. Paget, A. Mosnier, and H. M. Späth. 2015. “A Literature Review to Identify Factors That Determine Policies for Influenza Vaccination.” Health Policy (Amsterdam, Netherlands) 119 (6): 697–708. doi:10.1016/j.healthpol.2015.04.006.
- Smith, M. J., C. M. Bensimon, D. F. Perez, S. S. Sahni, and R. E. G. Upshur. 2012. “Restrictive Measures in an Influenza Pandemic: A Qualitative Study of Public Perspectives.” Canadian Journal of Public Health 103 (5): e348–e352. doi:10.1007/BF03404439.
- Tashiro, A., and R. Shaw. 2020. “COVID-19 Pandemic Response in Japan: What is behind the Initial Flattening of the Curve?” Sustainability 12 (13): 5250. doi:10.3390/su12135250.
- Tsiotas, D., and L. Magafas. 2020. “The Effect of anti-COVID-19 Policies on the Evolution of the Disease: A Complex Network Analysis of the Successful Case of Greece.” Physics 2 (2): 325–339. doi:10.3390/physics2020017.
- Tso, R. V., and B. J. Cowling. 2020. “Importance of Face Masks for COVID-19 – a Call for Effective Public Education.” Clinical Infectious Diseases. . 1-4. doi:10.1093/cid/ciaa593.
- Tyshenko, M. G., and C. Paterson. 2010. SARS Unmasked: Risk Communication of Pandemics and Influenza in Canada. MontrealandKingston: McGill-Queen’s University Press.
- Vogel, L. 2020. “Who Should Wear a Face Mask? Experts Weigh in on Canada’s COVID-19 Response.” CMAJ : Canadian Medical Association Journal = journal de l'Association medicale canadienne 192 (16): E440–E441. doi:10.1503/cmaj.1095863.
- Wilson, S. 2020. “Pandemic Leadership: Lessons from New Zealand’s Approach to COVID-19.” Leadership 16 (3): 279–293. doi:10.1177/1742715020929151.
- Woo, J. J. 2020. “Policy Capacity and Singapore’s Response to the COVID-19 Pandemic.” Policy and Society 39 (3): 345–362. doi:10.1080/14494035.2020.1783789.