Abstract
The outbreak of COVID-19 has posed an unprecedented threat to the functioning of our society and led to a substantial loss of lives. In this paper, we systematically analyzed the World Health Organization (WHO)’s policy framing and management of the pandemic. The performance of the WHO can be evaluated in two aspects: the timeliness of their risk assessment, such as the announcements of a Public Health Emergency of International Concern (PHEIC) and pandemic, and the communication interfaces between the WHO and other stakeholders. Our study reveals that, while the WHO has made timely decisions in risk assessments, there were profound limitations in the current communication interfaces and feedback loops between the WHO, member states and other stakeholders. We recommend redesigning the current alert system so that the level of warning and the accompanying policy recommendations could more accurately reflect the threat and escalating nature of a pandemic outbreak.
1. Introduction
The COVID-19 pandemic in 2020 is one of the most transformative events in the recent history of mankind. This pandemic has virtually halted people’s movement across national borders since mid-March of 2020 and exerted an uneven distribution of impacts geographically (Bailey et al. Citation2020; He Citation2020). At the time of writing (November 14, 2020), there are more than 52 million confirmed cases globally and about 1.3 million deaths (WHO Citation2020a), and global GDP is forecast to decline by 5.2% in 2020 (World Bank Citation2020). In the meantime, the virus continues to spread rapidly (WHO Citation2020b; Worldometer Citation2020). Epidemic impacts of this magnitude have not been seen since the Spanish flu of 1918–19.
Throughout the pandemic, the World Health Organization (WHO) has been active in warning and advising countries. However, many global leaders have criticized the WHO for not providing timely information and correct advice (Hernández Citation2020). Some have even called for an independent investigation of the causes of this pandemic (Japan Times Citation2020; The Australian Citation2020).
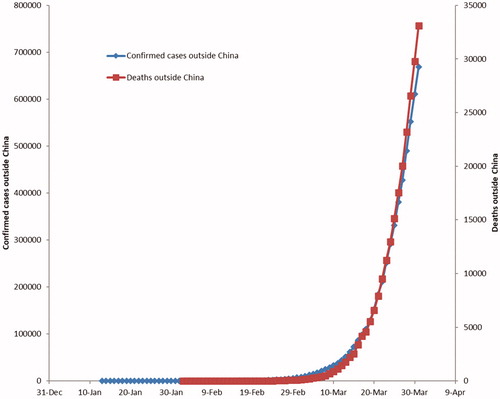
In this paper, we aim to examine the WHO’s policy framing and crisis management strategies between December 31, 2019, when the WHO’s country office in China first noticed the outbreak of a “viral pneumonia” in Wuhan, and March 11, 2020, when the WHO classified the COVID-19 outbreak as a pandemic (WHO Citation2020c). This early period is significant due to the snowball effect of the transmission of COVID-19 (see ), such that an early policy misstep could result in disproportionately adverse impacts later on.
Figure 1. Number of confirmed cases (left axis) and deaths (right axis) due to COVID-19 outside China (January 13-March 31, 2020). Source: WHO situation reports (Citation2020q).
2. Policy problem
The COVID-19 pandemic is a crisis, or an event or series of events that does not usually occur and entails a threat to the core values of a system (Boin Citation2010, 131). In this case, there were early warning signals beforehand; the epidemic outbreak in China was the preceding event before a full-fledged pandemic. During a crisis, leaders should maintain control and make sense of an emerging and devolving situation (Boin Citation2009, 371).
How decision makers manage crises depends on how the crises are framed. According to Stone (Citation1989), policy framing is a political exercise in which different parties compete to establish a dominant narrative of a policy problem. This process affects agenda setting in multiple ways, from determining a root cause of the problem to recommending appropriate solutions. In the case of public health, competing policy frames include public health as a security problem, an economic problem, and as a human rights problem with moral implications (Labonté Citation2008). States predominantly adopt the narrative that public health problems, including the COVID-19 pandemic, are threats to national security. The different frames can also be used in conjunction to generate a more holistic understanding of health policy, which has been referred to as “healthy public policy” by several scholars (Hancock Citation1985; Milio Citation1981). The WHO has recommended to member states to adopt this holistic approach when handling COVID-19.
Another way in which narratives in public health could differ is the severity of the policy problem. However, accurately assessing and describing the severity of a public health problem can be incredibly difficult. When there are too many critical unknowns, the costs-benefit and risk assessments can be highly complex, and the costs and benefits are not distributed proportionately and equitably. At the same time, there could be grave consequences if political leaders apply the wrong framing to a crisis. Downplaying the crisis could lead to inadequate preparation, resulting in a greater loss of lives, whereas an overreaction could entail unnecessary disruptions to social and economic activities and cause widespread panic. In the case of COVID-19, several states who have attempted to downplay the severity of COVID-19 have used “softer” policies, and these same states have some of the most significant numbers of COVID-19 cases in the world (Manchein et al. Citation2020).
The ability to adapt is also important in crisis management. As events unfold rapidly during a crisis, it is not always possible to assess the situation from every perspective (Boin Citation2010, 134–135; Wilkinson Citation2015, 56). Besides the leadership role of the government, civil society also needs to be empowered to self-organize and take initiatives to protect themselves, which complements the response efforts of the government. By adapting policies by reference to evolving knowledge that is co-created by a wide pool of actors, governments and institutions can adaptively manage crises and build resilience against them (Dietz, Ostrom, and Stern Citation2003; Folke et al. Citation2005; Lee Citation1993).
Effective interagency or inter-governmental co-ordination is yet another integral part of response efforts (Boin Citation2009). When managing on a pandemic, the WHO relies on the support and co-operation of its 196 member states, the United Nations, the academic sector, scientific and research institutions, non-governmental organizations and collaborative network such as Global Outbreak Alert and Response Network (GOARN). Since the WHO’s moral standing and credibility to some degree grant it authority to exert influence on the member states, the WHO must, where possible and appropriate, adhere to scientific principles strictly and provide evidence-based policy advice and recommendations.
All the elements as discussed above are necessary for effective governance during COVID-19. Therefore, in our assessment of the WHO’s crisis management, we focused on the WHO’s policy framing and governance mode during COVID-19. Our assessment is based on qualitative and quantitative evidence. The qualitative evidence includes records of the WHO’s media briefings and press conferences, statements of the International Health Regulations (IHR) (2005) Emergency Committee, official government announcements, news reports, academic journals, and commentaries of non-governmental organizations. The quantitative evidence includes official statistical data on the number of affected countries, confirmed cases and deaths of COVID-19. Our systematic assessment includes the tracking of major events and underlying statistical patterns, as well as reviewing the WHO’s COVID-19 responses relative to their responses to SARS in 2003, H1N1 in 2009, and MERS in 2012. Based on our analysis, we proposed three recommendations for improvement.
3. Discussion
3.1. The decision-making processes of the WHO and the emergency committee
The WHO’s determination of the status of the COVID-19 outbreak was an intricate process. Three different parties were involved, namely the external experts through the IHR (2005) Emergency Committee (EC) process, the WHO’s internal epidemiological team, and the Director-General and his senior management team. Although the major decisions were made by different parties, epidemiological data suggests that they are consistent (see Appendix I and II).
Like any other United Nations entities or supranational institutions, the WHO has institutionalized check and balance mechanisms. Therefore, it is generally not possible for any member, except for the Director-General under specific circumstances, to override the decision-making process without triggering alarms. The WHO’s modus operandi is akin to dispersed governance in that the WHO largely relies on the cooperation and support of Member States and other non-governmental organizations to gather information, commit to pandemic preparedness, and implement policy decisions. The IHR (2005) requires the member states to abide by the agreed institutional framework, but there is a lack of effective enforceability mechanisms (Kamradt-Scott Citation2019). If a member state refuses to conform to the WHO’s policy recommendations, there is limited recourse available to the WHO or its member states.Footnote1
The independence and internationally representative character of the WHO Secretariat are enshrined in the WHO Constitution. According to Article 35 (WHO, 2005a), “[t]he paramount consideration in the employment of the staff shall be to assure that the efficiency, integrity and internationally representative character of the Secretariat shall be maintained at the highest level,” whereas in Article 37, “[e]ach Member of the Organization on its part undertakes to respect the exclusively international character of the Director-General and the staff and not to seek to influence them.” The same principles also prevail in the EC mechanism.
The procedures, terms of reference, composition of the EC as well as decision instruments pertinent to the Public Health Emergency of International Concern (PHEIC) are detailed in the International Health Regulations (IHR) (2005) Articles 12, 47, 48, 49 and Annex II. In the process of deliberation of a PHEIC, the WHO Director-General is obligated to seek the views of the State Party where the epidemic event arises as well as the Emergency Committee, as stated in Article 12 of the IHR. Articles 47, 48 and 49 of the IHR also provide that the WHO shall maintain the IHR expert roster, which consists of experts in all relevant fields of expertise, and that the EC should be selected by the Director-General on the basis of relevant expertise and experience and with due regard to the principles of equitable geographical representation.
When the EC is convened, the WHO Secretariat also requires members and advisors of the EC to disclose any conflicts of interest, and those who are deemed to have conflicts of interest would not be permitted to participate in the decision-making process (WHO Citation2020l). This mechanism ensures that the EC makes recommendations independently and objectively.
The EC for the COVID-19 outbreak in January 2020 comprised of 15 members: 9 members (60%) had an academic background, 5 members came from government or quasi-governmental bodies, and 1 member was affiliated with the International Civil Aviation Organization (ICAO). In terms of geographical distribution, 5 members (33.3%) came from the Western Pacific region (except China), 3 from Europe, 2 from Southeast Asia and 2 from the Americas. The remaining 3 members were from the Eastern Mediterranean region, African regions and China respectively (WHO Citation2020d). The EC’s composition is noticeably diverse, ensuring that balanced and unbiased decisions can be made.
3.2. Comparison to WHO’s decisions during the H1N1 outbreak
There were speculations that the WHO delayed the declaration of a Public Health Emergency of International Concern (PHEIC) as well as the characterization of a pandemic during COVID-19. According to the IHR (2005), a PHEIC “means an extraordinary event which […] constitute[s] a public health risk to other States through the international spread of disease and […] potentially requires a coordinated international response] (p. 9). PHEIC is also currently the only and highest level of alert in accordance with the IHR. The definition of a pandemic, in contrast, is not outlined in the IHR (2005), but the WHO has delineated six phases of a pandemic influenza (WHO Citation2009b).
We examined the validity of these allegations by comparing the WHO’s decisions with similar incidents in the past. Since the IHR (2005) came into effect, five public health emergencies have been deemed PHEICs, namely the 2009 H1N1 pandemic, the wild poliovirus in 2014, the 2014 West African Ebola epidemic, the Zika emergency of 2015–16, and the 2018–19 outbreak of Ebola in Kivu (Science Media Centre Citation2020). Considering the transmission dynamics and the risk of spread, the 2009 H1N1 influenza pandemic is the most relevant comparison to the outbreak of COVID-19 in 2020.
and Appendix II provide a succinct comparison of the epidemiological considerations underlying the major decisions of the WHO within the first three months of the H1N1 and COVID-19 outbreaks. The timing difference between the first case detected outside the country of origin and the declaration of a PHEIC was 11 days for H1N1 and 17 days for COVID-19. As for the timing difference between the declaration of a PHEIC and the announcement of pandemic, it was 47 days during the H1N1 outbreak, whereas 41 days had passed during the COVID-19 outbreak. Furthermore, the number of confirmed cases outside the country of origin two days prior to the announcement of pandemic was 26,563 for H1N1 and 28,673 for COVID-19. Therefore, evidence indicates that the WHO had applied consistent epidemiological criteria in announcing a PHEIC and pandemic in both outbreaks.
Figure 2. Timelines of global events within the first three months of the H1N1 and COVID-19 outbreaks.
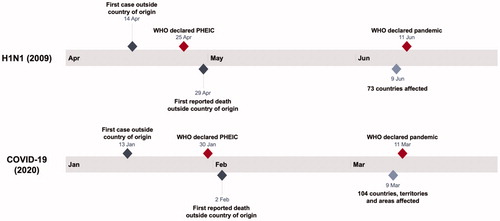
It is important to note that the genome sequence of SARS-CoV-2 already became available on January 12, 2020 (Lu et al. Citation2020) and hence did not delay the WHO’s decision making compared to H1N1, whose sequence was obtained on April 25, 2009 (WHO Citation2009a). Such shared informationFootnote2 is important during declared or imminent health emergencies and as a core component of routine surveillance and public health preparedness.
Notwithstanding this evidence, it is not certain whether the epidemiological criteria for the H1N1 pandemic remain applicable to the COVID-19 outbreak. According to epidemiological data during the early stages of the outbreak, it appears that COVID-19 tends to cause more severe symptoms than the H1N1 influenza, as about 18% of COVID-19 cases can be classified as serious illness or death (WHO Citation2020e).Footnote3 In contrast, many H1N1 patients recovered rapidly even without medical care. Considering the severity of COVID-19, the WHO could have recommended additional precautionary measures, such as issuing travel advisories to affected areas, as they did during SARS (WHO Citation2003, Citation2006).Footnote4
3.3. The WHO’s recommended policy measures for COVID-19
We used NVivo to characterize word frequency in the transcripts of Director-General Tedros’ speeches from January 22 to March 12, 2020.Footnote5 Several consistent themes emerged, including the need for accurate information, the preparation of funding and supplies, and the potential socio-economic consequences. Throughout February 2020, the WHO also maintained the stance that while China’s proactive policy responses have conferred a “window of opportunity,” it is uncertain how long such a window will last. Dr. Tedros further urged all nations to prepare for the arrival of coronavirus. He recommended a blended, comprehensive approach to break the chain of transmission, which includes active case detection, contact tracing, and provision of risk communication at points of entry (WHO Citation2020f). The most important theme was one of “solidarity,” a word Dr. Tedros used 43 times between late January and early March. It is evident from this language that Dr. Tedros and the WHO made concerted efforts to encourage global unity at a time of crisis in order to coordinate policy efforts against COVID-19.
At the same time, there were noticeable changes in the WHO’s advice and wording. One of the changes concerned the WHO’s stance on travel restrictions. On January 23, January 30, and February 4, 2020, the WHO placed emphasis on the need to maintain unimpeded international traffic and trade. Dr. Tedros maintained that border closure actions imposed by some member states are an overreaction and not buttressed by science and evidence. He also expressed unwavering confidence in the effectiveness of China’s policy measures to curb the outbreak. Concerning the travel and trade restrictions, Dr. Tedros explicitly stated that the WHO opposed any restrictions for travel and trade or other measures against China (WHO Citation2020g).Footnote6 While the IHR (2005) sought to limit the public health measures to those “that are commensurate with and restricted to public health risks, and which avoid unnecessary interference with international traffic and trade,” it is difficult to operationalize this principle when the WHO and its member states strive to cope with an unusual outbreak.
In addition, the statement of the IHR EC released on January 30 cited section 5 of Article 43 of IHR: “A state party implementing additional health measures that significantly interfere with international traffic shall inform WHO, within 48 h of implementation, of such measures and their health rationale unless these are covered by a temporary or standing recommendation.” By February 12, 2020, the recommendations had been shifted from refraining from any trade and travel bans to upholding the “free pratique” principle for ships, which is to allow ships to enter port and declare that they are not carrying disease, and providing “proper care for all travelers, in accordance with the [IHR]” (WHO Citation2020h).
While the WHO might have crafted its advices and recommendations on travel and trade based on the best knowledge and evidence at that time, these advices were no longer heeded by most of the WHO member states subsequent to the WHO announcement of pandemic on March 11, 2020. In fact, the IHR Article 43-1 provided that State Parties shall not be precluded from implementing health measures which achieve the same or greater level of health protection than WHO recommendations, and many member states rightly did so on public health grounds (Harvey et al. Citation2020). Although some countries managed to contain the spread of COVID-19 within their territories with decisive and rigorous policy measures, variations in the coping measures adopted by different member states of the WHO have caused confusions, and failed to eradicate or contain COVID-19. Apparently, COVID-19 managed to exploit any lines of weaknesses resultant from the incoherent and disjointed policy responses of different jurisdictions.
It is now scientifically clear that aggressive measures such as the lockdown adopted by Wuhan, Hubei Province, China on January 20, 2020 (Yuan et al. Citation2020) and the Vo’ municipality of Italy on February 21, 2020 (Lavezzo et al. Citation2020) as well as the quarantine of the Diamond Princess Cruise (Mallapaty Citation2020; Moriarty Citation2020) are highly effective to suppress disease spreading. In light of this information, it appears that the EC adopted a relatively lax attitude in response to the COVID-19 outbreak, especially regarding travel restrictions. Even though COVID-19 is less lethal, given its higher rate of transmission and still high morbidity, we would have expected that the WHO would issue travel advisories for COVID-19, just as they did for SARS on April 2, 2003. Based on the available evidence, we believe that the confidence of the EC in the containment of the outbreak could be attributed to two reasons. Firstly, there were only less than 100 confirmed cases and no deaths outside of China on January 30, 2020. Secondly, China had already adopted stringent measures to regulate people’s movements in Wuhan and Hubei province and imposed exit screening measures across China’s ports and airports. In the meantime, the EC also advised that the WHO Director-General should monitor the situation closely and provide recommendations in view of this rapidly evolving situation.
The WHO also modified their stance on the purchase and use of face masks by the general public to prevent the spread of COVID-19, although they did so after the period we studied. Until early March, Dr. Tedros emphasized the need to supply surgical masks primarily to health workers and COVID-19 patients. According to the transcripts, the emphasis was made at a time when there was a global shortage of masks and other equipment, which was exacerbated by the hoarding of masks. However, this reasoning was inconsistent when compared to other media provided by the WHO during this time period. In the interim guidance report issued on January 29, 2020, the WHO stated that the potential negative consequences of someone without COVID-19 wearing a mask included “unnecessary cost, procurement burden and […] a false sense of security that can lead to neglecting other essential measures such as hand hygiene practices” (WHO Citation2020i). This position was even more extreme in a short video uploaded on YouTube, which claimed that people without the common symptoms of COVID-19 “do not have to wear masks, because there is no evidence that they protect people who are not sick” (WHO Citation2020j). It is now evident that face masks can largely reduce the risk of infection (Chu et al. Citation2020), and the attitude of WHO was not consistent with “preparing for the worst” (Global Preparedness Monitoring Board Citation2019). The WHO has since revised its position on masks: while they maintain that only health workers and other vulnerable subpopulations should wear medical masks, they now recommend that ordinary people without health restrictions or symptoms should wear fabric masks to protect themselves and others if local authorities have advised them to do so (WHO Citation2020k).
3.4. The severity of COVID-19 as framed by the WHO
The most obvious change in language pertained to the categorization of the COVID-19 outbreak, especially regarding its severity. On the statement of the EC released on January 30, 2020 (see Appendix I), the EC raised several key observations. Firstly, there are still many unknowns. Secondly, global coordinated effort is needed to enhance preparedness. Lastly, there is a risk of further international exportation of cases from the country of origin (WHO Citation2020g). This language is consistent with statements by earlier ECs during other epidemic outbreaks such as the 2009 H1N1 pandemic and MERS (Eccleston-Turner and Kamradt-Scott Citation2019; Mullen et al. Citation2020). This, along with the fact that the EC declared a PHEIC only when COVID-19 met the IHR (2005) criteria for a PHEIC, suggests the current EC followed IHR (2005) protocol.
On February 28, 2020, when there were 4,691 confirmed cases and 67 deaths outside China, the WHO upgraded their risk assessment at the regional and global levels from “high” to “very high.” According to the WHO, this decision was made by internal epidemiological specialists who are not at the senior management level (WHO Citation2020f).
On March 11, 2020, when the WHO announced a pandemic, Dr. Tedros lamented that the WHO were “deeply concerned both by the alarming levels of spread and severity, and by the alarming levels of inaction” (WHO Citation2020m).
Although “PHEIC” is the technical term used by the EC and WHO to objectively classify a disease, declaring a pandemic has widespread social consequences (WHO Citation2009b). As Dr. Tedros stated at the March 11 press conference, the word “pandemic,” “if misused, can cause unreasonable fear, or unjustified acceptance that the fight is over, leading to unnecessary suffering and death” (WHO Citation2020m). As a result, the WHO has been hesitant to classify diseases as pandemics without good reason to do so. At the same time, failing to declare a disease as a PHEIC or as a pandemic could lead to valuable time, money and especially lives being lost.
In the case of COVID-19, other health experts have noted that the novel coronavirus technically qualified as a pandemic weeks before the WHO officially declared it as one, simply because of the wide geographical spread of the cases (McKeever Citation2020). Around this time, the WHO also internally raised their global risk assessment of COVID-19 (WHO Citation2020f). Furthermore, according to the WHO situation report on March 4, 2020, “there were 12,669 confirmed cases outside China and 214 deaths[, and] 76 countries were affected” by that date (WHO Citation2020n). In light of this information, the WHO could have made the decision to declare a pandemic one week before they did so in order to galvanize global action at an earlier stage. However, based on the WHO’s actions during past pandemics, as well as the number of COVID-19 cases outside the country of origin at the time of the announcement, the WHO’s pandemic declaration on March 11 was still sufficiently timely to raise global attention.
At the same time, it is important to recognize that the WHO’s framing and perception of the risks posed by a new virus heavily depends on the information from the State Parties. For COVID-19, one of the most important pieces of information is the daily number of cases and deaths. However, the provision of data is not as objective of a process as it appears to be. Numbers and statistics are, in fact, often manipulated for political purposes, especially for establishing a dominant narrative of a policy issue (Stone Citation2012). This was reflected when Doctor Li Wenliang was threatened with legal punishment in China for warning of a new potential SARS-like outbreak (BBC Citation2020), as well as when the United Kingdom had manipulated testing numbers (Hughes and Giles Citation2020). There are also unintentional cases of underreporting caused by the lack of testing capacity, whether it is because a country lacks the technology or has bureaucratic obstacles. A prominent example of the latter is the case of the United States, which faced regulatory hurdles from agencies including the Food and Drug Administration and the Centers for Disease Control and Prevention (Shear et al. Citation2020).
Furthermore, the WHO’s narrative is only one of many competing policy narratives. In a typical media cycle, it is challenging for the mass media and the general public to consistently focus on a single issue, especially when there is a lack of dramatic changes to the state of affairs (Howlett, Ramesh, and Perl Citation2009). When the mass media and the global civil society misperceived that there have not been significant changes to the outbreak of COVID-19 during most of time in February 2020, the media attention and the society’s preparedness to the COVID-19 outbreak wavered over time. This caused the window of opportunity for COVID-19 to narrow during the last week of February and the first week of March.Footnote7 As for the states, several prominent world leaders have actively shared misinformation about the severity of COVID-19, and political tensions between states have also arisen. As a result, the WHO has made numerous attempts to correct the false information and promote solidarity at a time of political division, but to varying degrees of success. Since the WHO’s narrative is not always the dominant narrative among certain communities, this impedes the WHO’s ability to coordinate global action and leads to noncompliance with the WHO’s recommended policy measures. This too could be one reason why the COVID-19 outbreak became uncontrollable.
In the next section, we propose some recommendations for management of future pandemics.
4. New directions and recommendations for improvement
4.1. The need for a multi-level warning system instead of the current PHEIC system
Under the IHR (2005), the PHEIC is the only and highest level of alert (cf. IHR Articles 12, 48 & 49). The only other option is to not declare a PHEIC, making the decision binary (McCloskey and Heymann Citation2020). Also, a PHEIC event can encompass both regional epidemics such as Ebola, and pandemics such as H1N1 influenza of 2009 and COVID-19. Cognitively, member states, the mass media and the general public can face hardships to distinguish between the actual level of threat posed to them by a regional outbreak such as Ebola and a global outbreak such as COVID-19.
Tackling future epidemics and pandemics will require profound institutional changes, such as amendments to the IHR (2005) and an integrated, multi-stepped warning system that can accurately reflect the escalating nature of an outbreak. The different levels of alerts should align with specific policy recommendations to member states and the global civil society. An example of such a scale is the color-coded “Disease Outbreak Response System Condition” (DORSCON) scale used in Singapore for disease outbreaks (Government of Singapore Citation2020). Utilizing more than two categories would help to strike a balance between alerting and reassuring the public, and the color code could also make it easier for decision makers as well as the general public to assess the risk of the disease.
Furthermore, while the PHEIC can continue to serve as a baseline global emergency warning, additional layers of pandemic alert should be provided. These different levels of alert should be determined based on factors such as lethality, risk of impact and risk of spread. The specific recommendations associated with the levels of pandemic alert could also include the best practices on social distancing, wearing a mask, travel advisories and border management strategies.
Under the current PHEIC arrangement, the Emergency Committee (EC) related to a particular epidemic outbreak is to be reconvened every 3 months after a PHEIC was declared (WHO Citation2020o), and that the WHO Director-General has the discretion to decide if it is necessary to reconvene the EC at an earlier date. However, in a rapidly evolving situation, epidemiological risk assessments and the corresponding policy recommendations could have drastically changed within 3 months. For instance, during the COVID-19 outbreak, the advices provided by the EC on January 30, 2020 were rendered ineffective by around late February or early March. Therefore, we recommend that the Chair of the EC should also be empowered to decide when an EC meeting should be reconvened once the PHEIC has come into effect.
4.2. The need to assess both the severity and likelihood of a “pandemic scenario” during the early stages of epidemic outbreak
While the WHO and other public health authorities did not have full knowledge of the severity and transmission dynamic of COVID-19 during the early stages of the outbreak, there were some early warning indicators with respect to its transmission dynamics and pandemic potential. For instance, during the period from January 23, 2020 to January 30, 2020, the number of confirmed cases in Mainland China increased from 574 cases to 7736 cases, and the compounded daily growth rate was 45.0%. Furthermore, the number of deaths in China increased from 17 cases to 170 cases; on a compounded daily growth rate basis, the growth rate was 38.9%. Although the statistics during the early stage of the outbreak may be inaccurate and are subject to the influence of factors such as variations in case definition and inadequate medical resources, such a pattern of spread evidently appears to be faster than coronavirus outbreaks in the past, such as SARS in 2003 and MERS in 2012.
In addition, earlier statistics from Mainland China indicated that roughly 20% of the confirmed cases were in critical or serious conditions and about 2%–3% of patients died.Footnote8 The preliminary data suggests a combination of high transmissibility and moderate level of lethality of COVID-19, which poses a grave threat to the public health systems all over the world.
With the benefit of hindsight, the epidemiological team or the Emergency Committee of the WHO could have projected the consequences of a pandemic scenario and advised the WHO Direct-General to propose rigorous global responses accordingly. Furthermore, since there are no proven vaccines or therapeutics to COVID-19 throughout the early stages of the outbreak, there is a lack of effective means to contain or mitigate the impacts of COVID-19. As such, the benefits, costs and risks of maintaining unfettered international connectivity need to be assessed carefully.
In the usual epidemiological development scenarios, most diseases usually have low lethality or low transmissibility (see Appendix III). Whilst some dangerous diseases such as Ebola and MERS have a high death rate, they are more difficult to transmit from person to person, and most of the human-to-human transmission cases occurred in the setting of close contacts such as family members and caregivers. As such, the overall impacts of these diseases are not high, and the containment measures adopted by public health systems are usually effective. While SARS had relatively high death rates (about 15%) and a moderate level of transmissibility, since most patients of SARS have clearly identifiable symptoms such as high fever and a relatively short incubation period, it did not spread significantly across national borders. Even so, superspreading events were highly substantial for both SARS and MERS (Kucharski and Althaus Citation2015; Lloyd-Smith et al. Citation2005).
On the other end of the spectrum, many common diseases such as measles, the H1N1 influenza pandemic of 2009, and seasonal influenza can be transmitted relatively easily, yet the severity and mortality of such diseases tend to be low, with death rates of no more than 0.1% to 0.2%. Therefore, mitigation approaches such as the use of vaccines and therapeutics are often applied to tackle those diseases.
However, the Spanish flu of 1918–19 and COVID-19 are in a distinctive category (see Appendix III). On one hand, these two diseases have strong transmission dynamics; there is even evidence that COVID-19 may be transmitted via airborne particles (Setti et al. Citation2020). In addition, COVID-19 is characterized by an incubation period of 5 to 7 days on average, rendering entry- and exit screening ineffective (Quilty et al. Citation2020). On the other hand, these two diseases were also moderate in severity and recorded a 2% to 3% death rate among those confirmed cases. Transmission data modeling has shown that superspreading is significant for COVID-19 (Endo et al. Citation2020; Frieden and Lee Citation2020). As such, conventional public health measures that successfully dealt with typical epidemic outbreaks, such as simple testing, tracing and isolation are not as effective for the COVID-19 and Spanish flu outbreak.
Therefore, when conventional containment strategies no longer function properly, a paradigm shift is required for public health experts and the WHO officials to approach the policy problem in a novel way. We can draw insights on crisis management from the Dutch Safety Board and its postmortem assessment of the tragedy of the crash of the Malaysian Flight MH17 in Ukraine (Dutch Safety Board Citation2015, 249). In the report, it was proposed that risk assessments should not merely be made from a statistical perspective of likelihood; rather, qualitative aspects, including the severity of a possible incident, should also be assessed. Another dimension of assessment was whether an extreme-case scenario is conceivable, even though the probability of occurrence is low. When an extreme risk is involved, such events must be terminated immediately, or should not be undertaken.
Similarly, the WHO could have called for more drastic responses to prevent the worst-case scenario of an uncontrollable pandemic with no known cure. Under these circumstances, additional public health measures such as universal masking, entry screening, quarantine of travelers who recently visited the affected regions regardless of their present health conditions, and aggressive border management measures may be warranted.
Although some of these measures would necessarily impede international traffic and trade, they can be justified from the perspective of the paramount importance of protecting the health of all peoples. In fact, such a principle is enshrined in the WHO Constitution. Furthermore, there were common interests between public health authorities and the trade and travel industries, for which failures to curb an epidemic outbreak at the early stages will inflict disproportionately larger economic and social costs to a wide range of stakeholders. It was estimated that global economic losses in the first quarter of 2020 alone amounted to US$280bn. Such losses would be greater than the economic losses from SARS (2003, US$30–40bn), Ebola (2014–2016, US$53bn), MERS in South Korea (2015, US$10bn), and H1N1 influenza pandemic (2009, US$45–55bn) combined (Global Preparedness Monitoring Board Citation2020; Schar et al. Citation2018).
Moreover, a healthy human capital is pivotal in building a strong, resilient economy in the long run. Therefore, the WHO as well as member- and nonmember states should consider reassessing the tradeoffs that are present in public health crises to deliver more effective policies.
4.3. The need to improve the communication processes and feedback loops between the WHO, its 196 member states, and global civil society
Throughout the month of February, the WHO Director-General and the leadership team consistently raised a cautionary note in their press conferences. According to their assessments, while the stringent policy measures taken by China had provided a “window of opportunity,” it was crucial for the rest of the world to step up preparation efforts to detect, treat and isolate cases should COVID-19 arrive on their shores.
Yet, the discourse of the WHO appeared not to resonate with the political leadership or public health agencies of most of the member states, at least during January 2020 and most of February 2020. For instance, as revealed in a question raised by a journalist at the WHO media briefing session of February 24, 2020, no new measures had been implemented, and there was not even an apparatus to screen the temperatures of travelers at the airport of Geneva, where the headquarters of the WHO were located (WHO Citation2020p).
There was also visible dissonance between the WHO’s advice and the member states’ responses. On one hand, the WHO raised red flags on a daily basis since late January 2020, and the WHO Director-General used vivid language such as the “common enemy to humanity” during the press conference of February 11, 2020. On the other hand, many agencies, from the member states and the airport authorities to other authorities at the point of entry alike, adopted a business-as-usual approach to tackle the imminent threat.
One possibility for this incongruity could have been that the use of terminology to describe COVID-19 was different between the WHO and its member states. As stated before, while the PHEIC is the only and the highest level of alert under the IHR (2005), it is uncertain whether all member states regarded the PHEIC declaration in January as a sufficient clear trigger for instigating additional public health measures (Harvey et al. Citation2020, 4).
Another possible flaw in the WHO’s communication strategy was that the WHO Director-General may have placed too much of a focus on commending China’s efforts to contain COVID-19 at several press conferences in late January and even late February. As a result, the member states and civil society could have misinterpreted his message as “given what has been done by China, we rest assured that the virus would be highly unlikely to reach our shores.” Even though the WHO Director-General altered his language considerably by early February 2020 in his description of COVID-19, the first impression of his assurance message could have already been ingrained in the minds of the audience. It was only until March 11, 2020, when the pandemic was announced by the WHO, that the whole world woke up to the reality of an imminent threat. In retrospect, the WHO Director-General could have focused on the grave risks posed by COVID-19 when PHEIC was declared in late January 2020.
5. Conclusion
Throughout the COVID-19 outbreak, the WHO has committed to transparency and provided essential support to front-line medical staffs around the world. Such unceasing efforts and devotion deserve thanks. In the meantime, our analysis reveals that the current IHR (2005) institutional framework is inadequate to cope with some categories of epidemic outbreaks, especially illnesses with high transmissibility and relatively high level of severity.
In a snowballing epidemic outbreak, containing the virus could be increasingly difficult over time. To avert the worst-case scenario of a pandemic, the member states of the WHO and global civil society must be alerted and mobilized at the earliest opportunity. An integrated, multi-level warning system is essential for this task.
Acknowledgments
We are grateful to the Robert Koch Institute for sharing the clinical observations with us. Besides, we heavily referenced the open-sourced data from the WHO situation reports, WHO dashboard on COVID-19, the WHO transcripts on media briefings and Worldometer in our analysis. We are grateful to these information providers.
Disclosure statement
We declare that there are no conflicts of interest.
Notes
1 Other than the binding requirements, such as to disclose the details and scientific rationale of additional health measures, as stipulated in Article 43 of the IHR (2005).
2 The Nagoya Protocol aims at the fair and equitable sharing of benefits arising from the use of genetic resources for public health and makes reference to the IHR (2005). Timely sharing of pathogens and benefits enables identification of the pathogen, a sound risk assessment, initiation of evidence-based interventions and the subsequent development and deployment of countermeasures such as diagnostics, vaccines and therapeutics (WHO, Citation2019).
3 For example, 17.9% of the confirmed cases in China were either severe cases or deaths on January 31, 2020.
4 During the outbreak of SARS in 2003, WHO recommended persons travelling to the affected areas such as Hong Kong and certain parts of China to consider postponing all but essential travel.
5 All transcripts are available at https://www.who.int/dg/speeches.
6 The full sentence from Dr. Tedros’s response: “As I said it earlier, we should have actually expressed our respect and gratitude to China for what it’s doing. It has already done incredible things to limit the transmission of the virus to other countries. And where respect is due, then you don’t punish. Meaning if anyone is thinking about taking measures, it’s going to be wrong. And WHO doesn’t recommend, and actually opposes, any restrictions for travel and trade or other measures against China.”
7 According to the WHO situation reports, 26 countries were affected by COVID-19 on February 21, 2020. This increased rapidly to 113 countries, territories and areas by March 11, 2020.
8 It is noted that the death rate estimates have limitations (WHO, Citation2020s). The estimates of death rate of COVID-19 is complicated as it has a long cycle. For instance, according to the Robert Koch Institute, the average duration between symptom onset and Intensive Care Unit (ICU) admission of German patients in a study was 9 days, whereas the average duration of stay in ICU was 18 days (Robert Koch Institute, Citation2020).
References
- Bailey, D., J. Clark, A. Colombelli, C. Corradini, L. D. Propris, B. Derudder, U. Fratesi, et al. 2020. “Regions in a Time of Pandemic.” Regional Studies 54 (9): 1163–1174. doi:10.1080/00343404.2020.1798611.
- BBC. (2020). “Li Wenliang: Coronavirus death of Wuhan Doctor Sparks Anger.” BBC News, February 7. https://www.bbc.com/news/world-asia-china-51409801.
- Boin, A. 2009. “The New World of Crises and Crisis Management: Implications for Policymaking and Research.” Review of Policy Research 26 (4): 367–377. doi:10.1111/j.1541-1338.2009.00389.x.
- Boin, A. 2010. “Designing Resilience: Leadership Challenges in Complex Administrative Systems.” Designing Resilience. University of Pittsburgh Press. https://www.jstor.org/stable/j.ctt5hjq0c.11.
- Chu, Derek K., Elie A. Akl, Stephanie Duda, Karla Solo, Sally Yaacoub, Holger J. Schünemann, Derek K. Chu, et al. 2020. “Physical Distancing, Face Masks, and Eye Protection to Prevent Person-to-Person Transmission of SARS-CoV-2 and COVID-19: A Systematic Review and Meta-Analysis.” The Lancet 395 (10242): 1973–1987. doi:10.1016/S0140-6736(20)31142-9.
- Dietz, T., E. Ostrom, and P. C. Stern. 2003. “The Struggle to Govern the Commons.” Science (New York, N.Y.) 302 (5652): 1907–1912. doi:10.1126/science.1091015.
- Dutch Safety Board. 2015. MH17 Crash. The Hague: Dutch Safety Board.
- Eccleston-Turner, M., and A. Kamradt-Scott. 2019. “Transparency in IHR Emergency Committee Decision Making: The Case for Reform.” BMJ Global Health 4 (2): e001618. doi:10.1136/bmjgh-2019-001618.
- Endo, A., S. Abbott, A. J. Kucharski, and S. Funk. 2020. “Estimating the Overdispersion in COVID-19 Transmission Using Outbreak Sizes outside China.” Wellcome Open Research 5: 67. doi:10.12688/wellcomeopenres.15842.3.
- Folke, C., T. Hahn, P. Olsson, and J. Norberg. 2005. “Adaptive Governance of Social-Ecological Systems.” Annual Review of Environment and Resources 30 (1): 441–473. doi:10.1146/annurev.energy.30.050504.144511.
- Frieden, T. R., and C. T. Lee. 2020. “Identifying and Interrupting Superspreading Events—Implications for Control of Severe Acute Respiratory Syndrome Coronavirus 2.” Emerging Infectious Diseases 26 (6): 1059–1066. doi:10.3201/eid2606.200495.
- Global Preparedness Monitoring Board 2019. A World at Risk: Annual Report on Global Preparedness for Health Emergencies. Global Preparedness Monitoring Board. https://apps.who.int/gpmb/assets/annual_report/GPMB_annualreport_2019.pdf.
- Global Preparedness Monitoring Board. 2020. Global Preparedness Monitoring Board Calls on G7 and G20 Leaders to Support $8bn Call to Scale-up Global Response to COVID-19. Geneva: Global Preparedness Monitoring Board.
- Government of Singapore. 2020. “What do the Different DORSCON Levels Mean.” http://www.gov.sg/article/what-do-the-different-dorscon-levels-mean
- Hancock, T. 1985. “Beyond Health Care: From Public Health Policy to Healthy Public Policy.” Canadian Journal of Public Health 76 (1): 9–11.
- Harvey, F., W. Ammar, H. Endo, G. R. Gupta, J. Konyndyk, P. Matsoso, and T. Tam. 2020. Interim report on WHO’s response to COVID-19 January-April 2020. IOAC. https://www.who.int/publications/m/item/interim-report-on-who-s-response-to-covid—january—april-2020.
- He, Y. 2020. “A Look at Post-pandemic Global Governance.” https://valdaiclub.com/a/highlights/a-look-at-post-pandemic-global-governance/.
- Hernández, J. C. 2020. “Trump Slammed the W.H.O. Over Coronavirus. He’s Not Alone.” New York Times, April 8. Retrieved from https://www.nytimes.com/2020/04/08/world/asia/trump-who-coronavirus-china.html.
- Howlett, M., M. Ramesh, and A. Perl. 2009. Studying Public Policy: Policy Cycles and Policy Subsystems. 3rd ed. Oxford: Oxford University Press.
- Hughes, L., and C. Giles. 2020. “Matt Hancock Criticised by Regulator over UK Coronavirus Testing Figures.” Financial Times, June 3. https://www.ft.com/content/2c32d72f-8bf3-4a46-8c2a-8781721cc0db.
- Japan Times. 2020. “Japan Joins Calls for Probe into WHO's Coronavirus Response.” https://www.japantimes.co.jp/news/2020/05/16/national/japan-investigation-who-coronavirus-response-china/
- Kamradt-Scott, Adam. 2019. “The International Health Regulations (2005): Strengthening Their Effective Implementation and Utilisation.” International Organizations Law Review 16 (2): 242–271. doi:10.1163/15723747-01602002.
- Kucharski, A. J., and C. L. Althaus. 2015. “The Role of Superspreading in Middle East Respiratory Syndrome Coronavirus (MERS-CoV) Transmission.” Eurosurveillance 20 (25): 21167. doi:10.2807/1560-7917.ES2015.20.25.21167.
- Labonté, R. 2008. “Global Health in Public Policy: Finding the Right Frame?” Critical Public Health 18 (4): 467–482. doi:10.1080/09581590802443588.
- Lavezzo, E., E. Franchin, C. Ciavarella, G. Cuomo-Dannenburg, L. Barzon, C. D. Vecchio, A. L. Rossi, et al. 2020. “Suppression of a SARS-CoV-2 Outbreak in the Italian Municipality of Vo'.” Nature 584 (7821): 425–429. doi:10.1038/s41586-020-2488-1.
- Lee, K. N. 1993. Compass and Gyroscope: Integrating Science and Politics for the Environment. Washington, D. C.: Island Press. http://www.vlebooks.com/vleweb/product/openreader?id=none&isbn=9781597268608&uid=none.
- Leung, Gabriel, and Joseph Wu. 2020. “Estimating Clinical Severity of COVID-19 Amongst Symptomatic Cases from the Transmission Dynamics in Wuhan.” Paper presented at the University of Hong Kong Media Conference, March 6, 2020.
- Lloyd-Smith, J. O., S. J. Schreiber, P. E. Kopp, and W. M. Getz. 2005. “Superspreading and the Effect of Individual Variation on Disease Emergence.” Nature 438 (7066): 355–359. doi:10.1038/nature04153.
- Lu, R., X. Zhao, J. Li, P. Niu, B. Yang, and H. Wu Tan. 2020. “Genomic Characterisation and Epidemiology of 2019 Novel Coronavirus: Implications for Virus Origins and Receptor Binding.” The Lancet 395 (10224): 565–574. doi:10.1016/S0140-6736(20)30251-8.
- Mackenzie, John, and David Smith. 2020. “COVID-19: A Novel Zoonotic Disease Caused by a Coronavirus from China: what we Know and What we Don't.” Microbiology Australia 41 (1): 45. doi:10.1071/MA20013.
- Mallapaty, S. 2020. “What the Cruise-Ship Outbreaks Reveal about COVID-19.” Nature 580 (7801): 18–18. doi:10.1038/d41586-020-00885-w.
- Manchein, C., E. L. Brugnago, R. M. da Silva, C. F. O. Mendes, and M. W. Beims. 2020. “Strong Correlations between Power-Law Growth of COVID-19 in Four Continents and the Inefficiency of Soft Quarantine Strategies.” Chaos (Woodbury, N.Y.) 30 (4): 041102. doi:10.1063/5.0009454.
- McCloskey, B., and D. L. Heymann. 2020. “SARS to Novel Coronavirus - old lessons and new lessons.” Epidemiology and Infection 148 (e22): e22–4. doi:10.1017/s0950268820000254.
- McKeever, A. 2020. “Coronavirus is Officially a Pandemic. Here's Why that Matters.” https://www.nationalgeographic.com/science/2020/02/how-coronavirus-could-become-pandemic-and-why-it-matters/.
- Milio, N. 1981. Promoting Health through Public Policy. Philadelphia: Davis.
- Moriarty, L. F. 2020. “Public health responses to COVID-19 outbreaks on cruise ships — worldwide, February–March 2020.” MMWR. Morbidity and Mortality Weekly Report 69 (12): 347–352. doi:10.15585/mmwr.mm6912e3.
- Mullen, L., C. Potter, L. O. Gostin, A. Cicero, and J. B. Nuzzo. 2020. “An Analysis of International Regulations Emergency Committees and Public Health Emergency of International Concern Designations.” BMJ Global Health 5 (6): e002502. doi:10.1136/bmjgh-2020-002502.
- Quilty, B. J., S. Clifford, S. Flasche, CMMID nCoV working group, and R. M. Eggo, 2020. “Effectiveness of Airport Screening at Detecting Travellers Infected with Novel Coronavirus (2019-nCoV).” Eurosurveillance 25 (5), pp.1-5. doi:10.2807/1560-7917.ES.2020.25.5.2000080.
- Robert Koch Institute. 2020. Email correspondence between the authors and the Institute on September 11. 2020.
- Schar, D. L., G. M. Yamey, C. C. Machalaba, and W. B. Karesh. 2018. “A Framework for Stimulating Economic Investments to Prevent Emerging Diseases.” Bulletin of the World Health Organization 96 (2): 138–140. doi:10.2471/BLT.17.199547.
- Science Media Centre. 2020. “Expert Reaction to WHO Decision not to Declare the China Coronavirus Outbreak a PHEIC (Public Health Emergency of International Concern).” https://www.sciencemediacentre.org/expert-reaction-to-who-decision-not-to-declare-the-china-coronavirus-outbreak-a-pheic-public-health-emergency-of-international-concern/
- Setti, L., F. Passarini, G. De Gennaro, P. Barbieri, M. G. Perrone, M. Borelli, J. Palmisani, et al. 2020. “Airborne Transmission Route of COVID-19: Why 2 Meters/6 Feet of Inter-Personal Distance Could Not Be Enough.” International Journal of Environmental Research and Public Health 17 (8): 2932. doi:10.3390/ijerph17082932.
- Shear, M. D., A. Goodnough, S. Kaplan, S. Fink, K. Thomas, and N. Weiland. 2020. “The lost month: How a failure to test blinded the U.S. to COVID-19.” New York Times, March 28. Retrieved from https://www.nytimes.com/2020/03/28/us/testing-coronavirus-pandemic.html.
- Stone, D. A. 1989. “Causal Stories and the Formation of Policy Agendas.” Political Science Quarterly 104 (2): 281–300. doi:10.2307/2151585.
- Stone, D. A. 2012. Policy Paradox: The Art of Political Decision Making. 3rd ed. W. W. Norton.
- The Australian. 2020. “WHO Panel Must Look at Every Aspect of COVID-19.” https://www.theaustralian.com.au/commentary/editorials/who-panel-must-look-at-every-aspect-of-covid19/news-story/eee55c45d6a4d06acea3ea47ce92783d.
- WHO. 2005a “Constitution of the World Health Organization.” https://www.who.int/about/who-we-are/constitution.
- WHO. 2005b. “International Health Regulations.” 3rd Ed. https://www.who.int/ihr/publications/9789241580496/en/.
- WHO. 2003. “WHO Extends Its SARS-Related Travel Advice to Beijing and Shanxi Province in China and to Toronto, Canada.” https://www.who.int/mediacentre/news/notes/2003/np7/en/.
- WHO. 2006. SARS: How a Global Pandemic Was Stopped. Manila: WHO Regional Office for the Western Pacific. Retrieved from https://apps.who.int/iris/bitstream/handle/10665/207501/9290612134_eng.pdf?sequence=1&isAllowed=y.
- WHO. 2009a. Viral Gene Sequences to Assist Update Diagnostics for Swine Influenza A(H1N1). Atlanta: The WHO Collaborating Centre for Influenza.
- WHO. 2009b. “The WHO Pandemic Phases.” In Pandemic Influenza Preparedness and Response: A WHO Guidance Document. Geneva: World Health Organization. https://www.ncbi.nlm.nih.gov/books/NBK143061/.
- WHO. 2011. “Implementation of the International Health Regulations (2005). Report of the Review Committee on the Functioning of the IHR (2005) in relation to Pandemic (H1N1) 2009.” Report by the Director-General. https://apps.who.int/gb/ebwha/pdf_files/WHA64/A64_10-en.pdf
- WHO. 2019. The Public Health Implications of Implementation of the Nagoya Protocol: Report by the Director-General. World Health Organization. https://apps.who.int/gb/ebwha/pdf_files/WHA72/A72_32-en.pdf.
- WHO. 2020a. “WHO Coronavirus Disease (COVID-19) Dashboard.” https://covid19.who.int.
- WHO. 2020b. “Coronavirus Disease (COVID-19) Weekly Epidemiological Update and Weekly Operational Update.” https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports.
- WHO. 2020c. “Timeline of WHO’s Response to COVID-19.” https://www.who.int/news-room/detail/29-06-2020-covidtimeline
- WHO. 2020d. “List of Proposed Members and Advisers to International Health Regulations (IHR) Emergency Committee for Pneumonia due to the Novel Coronavirus 2019-nCoV.” http://www.who.int/ihr/procedures/novel-coronavirus-2019/ec-22012020-members/en/
- WHO. 2020e. “Novel Coronavirus (2019-nCoV) Situation Report-11.” World Health Organization. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200131-sitrep-11-ncov.pdf?sfvrsn=de7c0f7_4
- WHO. 2020f. “Coronavirus Press Conference 28 February, 2020.” World Health Organization.
- WHO. 2020g. “Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV) 30 January 2020.” https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov)
- WHO. 2020h. “WHO Director-General's Opening Remarks at the Media Briefing on Ebola and COVID-19 Outbreaks.” https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-ebola-and-covid-19-outbreaks
- WHO. 2020i. “Advice on the Use of Masks in the Community, during Home Care and in Health Care Settings in the Context of the Novel Coronavirus (2019-nCoV) Outbreak.” World Health Organization. https://apps.who.int/iris/bitstream/handle/10665/330987/WHO-nCov-IPC_Masks-2020.1-eng.pdf?sequence=1&isAllowed=y
- WHO. 2020j. “Can Masks Protect Against the New Coronavirus Infection?” WHO (Director). (Feb 6).[Video/DVD]
- WHO. 2020k. “Advice on the Use of Masks in the Context of COVID-19.” World Health Organization. https://apps.who.int/iris/bitstream/handle/10665/332293/WHO--nCov-IPC_Masks-2020.4-eng.pdf?sequence=1&isAllowed=y2019
- WHO. 2020l. “Statement on the Meeting of the International Health Regulations (2005) Emergency Committee Regarding The Outbreak of Novel Coronavirus 2019 (n-CoV) on 23 January 2020.” https://www.who.int/news-room/detail/23-01-2020-statement-on-the-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov)
- WHO. 2020m. “WHO Director-General's Opening Remarks at the Media Briefing on COVID-19 - 11 March 2020.” Retrieved from https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—11-march-2020
- WHO. 2020n. “Coronavirus disease 2019 (COVID-19) situation report –44.” World Health Organization. Retrieved from https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200304-sitrep-44-covid-19.pdf?sfvrsn=93937f92_6
- WHO. 2020o. “WHO Director-General's opening remarks at the media briefing on COVID-19 - 1 May 2020.” Retrieved from https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—1-may-2020
- WHO. 2020p. “Coronavirus Disease (COVID-19) Press Conference.” World Health Organization.
- WHO. 2020q. “Situation report on COVID-19, various dates between January and March 2020.” https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports.
- WHO. 2020r. “Media briefings on COVID-19, various dates between January and March 2020.” https://www.who.int/emergencies/diseases/novel-coronavirus-2019/media-resources/press-briefings/6.
- WHO. 2020s. “Scientific Brief – Estimating mortality from COVID-19 (August 4, 2020).” https://www.who.int/news-room/commentaries/detail/estimating-mortality-from-covid-19.
- Wilkinson, K. 2015. “Can Crisis Ever Be Good for Policy Design?” In Designing Public Policy for co-Production: Theory, Practice and Change, edited by C. Durose and L. Richardson. Bristol: Policy Press. doi:10.1332/policypress/9781447316695.003.0005.
- World Bank. 2020. “The Global Economic Outlook during the COVID-19 Pandemic: A Changed World.” https://www.worldbank.org/en/news/feature/2020/06/08/the-global-economic-outlook-during-the-covid-19-pandemic-a-changed-world
- Worldometer. 2020. “Worldometer.” https://www.worldometers.info/coronavirus/
- Yuan, Z., Y. Xiao, Z. Dai, J. Huang, Z. Zhang, and Y. Chen. 2020. “Modelling the Effects of Wuhan’s Lockdown During COVID-19, China. Bulletin of the World Health Organization, 98 (7), 484–494. doi:10.2471/BLT.20.254045.
Appendix I.
Mechanism for determining the status of events by the WHO in 2020
Appendix II.
Comparison of the timing of WHO major decisions during the H1N1 pandemic of 2009 and the COVID-19 pandemic of 2020
Appendix III.
The matrix of severity and transmission dynamics
