Abstract
Fever of unknown origin (FUO) is caused by various diseases, making differential diagnosis difficult. This study aimed to determine the clinical features of patients with FUO for use in daily medical practice. Medical records of patients who first visited our department for FUO between January 2008 and December 2017 were reviewed. We classified the diagnostic categories as infection, non-infectious inflammation, neoplasm, others, and unidentified through definitive diagnosis and compared the clinical characteristics of patients who fulfilled the criteria of classical FUO and those who did not. The most prevalent diseases in patients who fulfilled the criteria were adult-onset Still’s disease, Behçet’s disease (BD), and polymyalgia rheumatica, which do not have any specific image inspection or specific serological markers. BD and familial Mediterranean fever were most prevalent in patients who did not fulfill the criteria. All neoplasms fulfilled the criteria of classical FUO. The most useful diagnostic procedure was determined according to the criteria of each disease. The key factor that did not fulfill the criteria was periodic fever continuing for less than 3 weeks. When examining patients with FUO, we should strictly diagnose in accordance with the criteria of each disease and consider diseases that cause periodic fever.
1. Introduction
Fever of unknown origin (FUO) is caused by various diseases and often makes diagnosis difficult. In 1961, Petersdorf and Beeson [Citation1] defined the criteria for FUO as follows: fever of more than 3 weeks’ duration, temperature >38.3 °C on multiple occasions, and an unclear diagnosis after 1 week of inpatient evaluation. In 1991, Durack and Street [Citation2] changed the criterion of ‘an unclear diagnosis after 1 week of inpatient evaluation’ to ‘an unclear diagnosis after 3 outpatient visits or 3 days of inpatient evaluation’ and classified FUO as classical, nosocomial, neutropenic, and human immunodeficiency virus (HIV)–associated FUO [Citation2]. In previous reports [Citation3–6], infections were the most frequent causes of FUO. FUO has some characteristics that obscure the cause of the fever; the focus of infection is unclear without accepting a typical symptom and performing a physical examination, when there are no symptoms except for fever and a certain period is needed for specific symptoms to appear (e.g., in non-infectious inflammatory diseases). Goto et al. [Citation7] reported some critical diseases in patients who did not fulfill the criteria of classical FUO; thus, it is vital to carefully examine all patients with prolonged fever. However, very few studies have focused on the types of critical diseases in patients who do not fulfill the criteria of classical FUO. In recent years, diagnostic techniques such as imaging, serological, and genetic analyses have improved. Positron emission tomography-computed tomography (PET-CT) is one of the important modalities for diagnosing FUO [Citation8]. Genetic analysis is also one important examination for FUO [Citation9]. The progress of these diagnostic techniques may have changed the breakdown of diseases causing FUO. Periodic fever diseases such as familial Mediterranean fever (FMF) have increased due to the progress in diagnostic tools and recognition of diseases, and these diseases do not fulfill the criteria of classical FUO. The aim of this study was to determine the clinical features of patients with FUO, clarify the types of critical diseases in patients who do not fulfill the criteria of classical FUO, and investigate whether patients with unknown fever did not fulfill the criteria of FUO by chance or due to the characteristics of the disease.
2. Materials and methods
2.1. Patient and inclusion criteria
We retrospectively analyzed the medical records of 149 patients who first visited our department for FUO between January 2008 and December 2017. Because of different etiologies of pediatric diseases, we excluded 5 patients who were younger than 15 years and focused on 144 adult patients in this study. We compared patients who fulfilled the criteria of classical FUO with patients who did not fulfill them and analyzed characteristics such as sex, age, definitive diagnosis, duration of fever, fever type, symptoms, examinations, duration from onset to diagnosis, diagnostic procedures, and prognosis. In this study, we used the criteria of classical FUO by Durack and Street [Citation2]: ‘unidentified fever with axillary temperature ≥38 °C at least twice in more than 3 weeks and an unclear diagnosis after 3 outpatient visits or 3 days of inpatient evaluation’ and ‘no evidence of immunodeficiency syndromes including HIV infection.’ The diagnostic categories of FUO were infection, non-infectious inflammation, neoplasm, others, and unidentified by a definitive diagnosis. We also compared patients based on terms (first term, January 2008 to December 2012; second term, January 2013 to December 2017) to analyze the transition of disease and diagnostic procedures as genetic analysis of MEFV was started in our department since 2013. Although the Tel-Hashmer criteria [Citation10] are used overseas as FMF criteria, the Japanese Ministry of Public Welfare suggested the modified Tel-Hashmer criteria [Citation11]. We diagnosed according to the criteria provided by the Investigation and Research Committee 2015 for FMF organized by the Japanese Ministry of Health, Labour and Welfare of Japan.
2.2. Ethics
The protocol of the present study was approved by the institutional review board of Hirosaki University Graduate School of Medicine (number: 2018-1120) and has been performed in accordance with the ethical standards of the WMA Declaration of Helsinki—Ethical Principles for Medical Research Involving Human Subject. All patients were free to opt out.
2.3. Statistical analysis
Data were analyzed using Prism 5 version 5.04 (GraphPad, San Diego, CA, USA). Fisher’s exact test was used to determine differences. P values < 0.05 were accepted as statistically significant.
3. Results
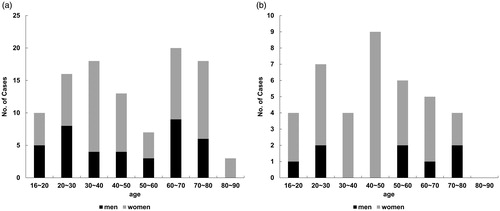
A total of 144 patients were enrolled in this study, including 105 patients (72.9%) who fulfilled the criteria of classical FUO and 39 patients (27.1%) who did not fulfill them. Those who fulfilled the criteria of classical FUO included 39 men (37.1%) and 66 women (62.9%), and the largest age groups comprised patients in their 30 s and 60 s (median age, 45.0 years; range, 16–86 years) (. Those who did not fulfill the criteria of classical FUO included 8 men (20.5%) and 31 women (79.5%), and there was no difference in age in this group ().
Figure 1. Prevalence of fever of unknown origin (FUO) according to age and sex. (a) Patients who fulfilled the criteria of classical FUO (n = 105). (b) Patients who did not fulfill the criteria of classical FUO (n = 39).
The diagnostic categories of the 105 patients who fulfilled the criteria of classical FUO were infection (n = 12, 11.4%), non-infectious inflammation (n = 60, 57.1%), neoplasm (n = 6, 5.7%), others (n = 13, 12.4%), and unidentified (n = 14, 13.3%) (. The diagnostic categories of the first term (January 2008 to December 2012) were infection (n = 6, 14.3%), non-infectious inflammation (n = 22, 52.4%), neoplasm (n = 2, 4.8%), others (n = 7, 16.7%), and unidentified (n = 5, 11.9%) () and those of the second term (January 2013 to December 2017) were infection (n = 6, 9.5%), non-infectious inflammation (n = 38, 60.3%), neoplasm (n = 4, 6.3%), others (n = 6, 9.5%), and unidentified (n = 9, 14.3%) ().
Figure 2. Diagnostic categories of fever of unknown origin (FUO) according to the term. (a) Patients who fulfilled the criteria of classical FUO (n = 105). (b) Patients who fulfilled the criteria of classical FUO from 2008 to 2012 (n = 42). (c) Patients who fulfilled the criteria of classical FUO from 2013 to 2017 (n = 63). (d) Patients who did not fulfill the criteria of classical FUO (n = 39). (e) Patients who did not fulfill the criteria of classical FUO from 2008 to 2012 (n = 13). (f) Patients who did not fulfill the criteria of classical FUO from 2013 to 2017 (n = 26).
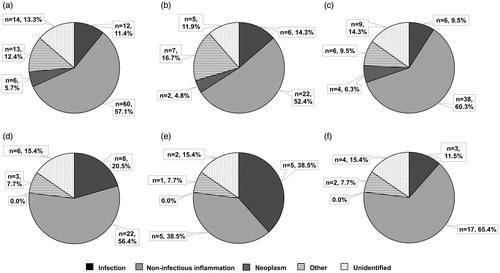
The diagnostic categories of the patients who did not fulfill the criteria of classical FUO were infection (n = 8, 20.5%), non-infectious inflammation (n = 22, 56.4%), others (n = 3, 7.7%), and unidentified (n = 6, 15.4%); none of the patients had neoplasm (. The diagnostic categories of the first term were infection (n = 5, 38.5%), non-infectious inflammation (n = 5, 38.5%), others (n = 1, 7.7%), and unidentified (n = 2, 15.4%) () and those of the second term were infection (n = 3, 11.5%), non-infectious inflammation (n = 17, 65.4%), others (n = 2, 7.7%), and unidentified (n = 4, 15.4%) ().
There was no significant difference between the first and second terms in patients who fulfilled the criteria (): infection, 14.3% vs. 9.5% (p = .4298); non-infectious inflammation, 52.4% vs. 60.3% (p = .4298); neoplasm, 4.8% vs. 6.3% (p = 1.0000); others, 16.7% vs. 9.5% (p = .3664); unidentified, 11.9% vs. 14.3% (p = .7786) and in patients who did not fulfill the criteria (): infection, 38.5% vs. 11.5% (p = .0896); non-infectious inflammation, 38.5% vs. 65.4% (p = .1721); others, 7.7% vs. 7.7% (p = 1.0000); unidentified, 15.4% vs. 15.4% (p = 1.0000). There was also no significant difference between the patients who fulfilled and did not fulfill the criteria of FUO in the first term (): infection, 14.3% vs. 38.5%, p = .1061; non-infectious inflammation, 52.4% vs. 38.5%, p = .5279; neoplasm, 4.8% vs. 0%, p = 1.0000; others, 16.7% vs. 7.7%, p = .6639; unidentified, 11.9% vs. 15.4%, p = .6639) and in the second term (): infection, 9.5% vs. 11.5%, p = .7171; non-infectious inflammation, 60.3% vs. 65.4%, p = .8111; neoplasm, 6.3% vs. 0%, p = .3172; others, 9.5% vs. 7.7%, p = 1.0000; unidentified, 14.3% vs. 15.4%, p = 1.0000. However, in patients who fulfilled the criteria of FUO, the total number of patients increased from 42 in the first term to 63 in the second term due to an increase in the number of non-infectious inflammation diseases; in patients who did not fulfill the criteria of FUO, the total number of patients increased from 13 in the first term to 26 in the second term, and there was a decrease in infection and an increase in non-infectious inflammation in the second term compared with those in the first term. Moreover, there was no case of neoplasms in patients who did not fulfill the criteria of classical FUO.
3.1. Causes of disease in patients with unidentified fever
In patients who fulfilled the criteria of classical FUO, the most prevalent diseases of the first term were adult-onset Still’s disease (AOSD, n = 4) and Behçet’s disease (BD, n = 4) and those of the second term were AOSD (n = 7), polymyalgia rheumatica (PMR, n = 7), and BD (n = 6) ().
Table 1. The diagnosis of unknown fever in the cases who fulfilled the criteria of classical FUO.
In patients who did not fulfill the criteria of classical FUO, the most prevalent diseases of the first term were pelvic infections (n = 2) and systemic lupus erythematosus (SLE, n = 2) and those of the second term were FMF (n = 7) and BD (n = 5). Theese diseases did not fulfill the criteria of FUO because the duration of fever was less than 3 weeks and the temperature was lower than 38.3 °C (). FMF was significantly prevalent in patients who did not fulfill the criteria of FUO (n = 1 and n = 7, respectively; p = .0004) ( and ).
Table 2. The diagnosis of unknown fever in the cases who did not fulfill the criteria of classical FUO.
3.2. Duration from onset to diagnosis
We compared the duration from the disease onset to diagnosis between the first and second terms in each category of classical FUO (). Those who fulfilled the criteria of classical FUO, except unidentified, included 91 patients (37 patients [40.7%] in the first term and 54 patients [59.3%] in the second term), and those who were diagnosed in less than 59 days included 52 patients (22 patients [59.5%] in the first term and 30 patients [55.6%] in the second term). More than half of the patients were diagnosed in less than 59 days. Meanwhile, the number of patients who needed more than 180 days to be diagnosed was 5 in the first term (13.5%) and 3 in the second term (5.6%). The diagnoses were chronic active Epstein–Barr virus infection, AOSD, microscopic polyangiitis, Sjögren’s syndrome, and BD in the first term and dermatomyositis, fibromyalgia, and Crohn’s disease in the second term.
Table 3. Duration till diagnosis from the onset.
Patients who did not fulfill the criteria of classical FUO, except unidentified, were 33 patients (11 patients [33.3%] in the first term and 22 patients [66.7%] in the second term), and patients diagnosed in less than 59 days were 18 patients (10 patients [90.9%] in the first term and 8 patients [36.4%] in the second term). Meanwhile, none of the patients needed more than 180 days to be diagnosed in the first term, but 11 patients (50.0%) needed more than 180 days to be diagnosed in the second term. All 11 patients who needed more than 180 days had periodic fever, and the diagnoses were FMF (n = 7), BD (n = 3), and rheumatoid arthritis (RA) (n = 1).
3.3. Diagnostic procedures
In patients who fulfilled the criteria of classical FUO, image inspection (n = 5, 41.7%) and blood tests (n = 4, 33.3%) for infections, diagnostic criteria (n = 46, 76.7%) for non-infectious inflammatory diseases, and pathological examinations (n = 3, 50.0%) and image inspections (n = 3, 50.0%) for neoplasms were the most useful diagnostic tools. In patients who did not fulfill the criteria of classical FUO, blood tests (n = 2, 25.0%) and bacteriological examinations (n = 2, 25.0%) for infection and diagnostic criteria (n = 21, 95.5%) for non-infectious inflammatory disease were the most helpful diagnostic tools ().
Table 4. Diagnostic procedures.
In patients who fulfilled the criteria of classical FUO, 52 patients (49.5%) underwent PET-CT for the diagnosis of FUO. PET-CT was useful for diagnosis and exclusion of neoplasm. Furthermore, PET-CT supported the diagnosis in 9 patients with AOSD and 3 with PMR. In patients who did not fulfill the criteria of classical FUO, 11 patients (28.2%) underwent PET-CT, which supported the diagnosis in 2 patients with AOSD ().
Table 5. The proportion of PET-CT.
3.4. Prognosis
Patients who fulfilled and did not fulfill the criteria of classical FUO except neoplasm had good prognosis. Most of the unidentified patients had spontaneous remission and were suspected to have some viral infections.
3.5. Patients who did not fulfill the criteria of classical FUO
Thirteen (33.3%) of the 39 patients who did not fulfill the criteria of classical FUO had periodic fever, and the diagnoses were FMF (n = 7), BD (n = 4), RA (n = 1), and psychogenic fever (n = 1). In patients who fulfilled the criteria of FUO, 3 (2.9%) of 105 had periodic fever, and there were significantly more instances of periodic fever in patients who did not fulfill the criteria (2.9% vs 33.3%, p < .0001). Although the fever duration was short, the period needed for differential diagnosis from disease onset was long: 10 of 13 patients needed more than 180 days to be diagnosed (). In FMF patients, MEFV mutations occurred in exon 2 (E148Q/E148Q homo, n = 2; E148Q hetero, n = 1; L110P hetero/E148Q hetero, n = 1; L110P homo/E148Q homo, n = 1), and, in exons 1 and 3 (E84K hetero/R410 hetero, n = 1), one had no mutation and one of 7 patients had typical FMF.
Table 6. Duration of fever and duration from the onset to diagnosis in periodic fever patients.
4. Discussion
The results of this study showed that the most frequent diseases in patients who fulfilled the criteria of classical FUO were AOSD, BD, and PMR. Patients who fulfilled the criteria of FUO showed bimodality in their 30 s and 60 s (). AOSD and BD were the most frequent diseases in patients in their 30 s, and PMR, MPA, and malignant lymphoma were most frequent in patients in their 60 s. Patients at these ages are susceptible to the disease, which is the reason for the bimodality. In patients who did not fulfill the criteria of classical FUO, the most frequent diseases were FMF, BD, and SLE. There were patients who had periodic fever among those who did not fulfill the criteria of classical FUO, and they needed a longer time for diagnosis. All cases of neoplasm fulfilled the criteria of FUO; hence, differential diagnosis of neoplasm was considered important in classical FUO.
In previous reports [Citation3–7], infections were most frequent in patients with FUO. Compared with previous reports, the rate of non-infectious inflammation was 57.1%, which accounted for half of the total in this study, but it was because the major field of our department is rheumatology. Neoplasm had a declining trend in previous reports [Citation3–5,Citation7,Citation12], and, in this study, the rate of neoplasm was 5.7% and had a low frequency. The decrease in the rate of neoplasm was likely due to the progress of imaging analysis. The rate of unidentified cases was 13.3%, and the trend was similar to that of previous reports [Citation3,Citation4,Citation12]. Although there were a certain number of unidentified cases in all previous reports, most of the unidentified cases in our study had spontaneous remission and good prognosis. There were also patients with unidentified category of FUO who experienced stress, and the possibility that psychiatric elements affected the body temperature was suggested; however, these patients were not diagnosed by a psychotherapist [Citation13].
Analysis of the cause of disease based on term revealed that in patients who fulfilled the criteria of classical FUO, non-infectious inflammations increased between the first and second terms, although there was almost no difference in the diagnostic categories between the first and second terms. The prevalence of diagnostic categories had increased in AOSD (4 patients in the first term, 7 patients in the second term), BD (4 patients in the first term, 6 patients in the second term), PMR (1 patient in the first term, 7 patients in the second term), and MPA (2 patients in the first term, 5 patients in the second term). In patients who did not fulfill the criteria of classical FUO, infections decreased and non-infectious inflammations increased between the first and second terms. All cases of FMF were diagnosed in the second term, and these results were due to the progress in diagnostic tools and recognition of diseases. We had diagnosed typical cases of FMF before 2008. In this study, we excluded the cases that were already diagnosed as FMF before visiting our hospital. Because the diagnosis of FMF is based on clinical symptoms, diagnosing it is not easy, especially in atypical cases of FMF with long duration of fever. In addition, the significance of hetero mutations was unknown. We did not recognize well that FMF patients who present atypical phenotypes such as long duration of fever and had mutations, except exon 10, are not rare in Japan. To diagnose these cases, FMF should be considered and the patients should be treated with colchicine, as well as undergo genetic analysis.
The results also showed that periodic fever diseases such as FMF were increasing in recent years, and these diseases were important for the differential diagnosis of patients who did not fulfill the criteria of classical FUO.
Fukuhara et al. [Citation3] analyzed the duration from the onset of classical FUO until diagnosis from 1982 to 1988, and 16 (37.2%) of 43 patients were diagnosed in less than 59 days. In the present study, more than half of the patients who fulfilled the criteria of classical FUO were diagnosed in less than 59 days, suggesting that some of the diagnostic tools were implemented in recent years. However, 8 patients needed more than 180 days to be diagnosed. In particular, among patients who did not fulfill the criteria of classical FUO, 11 patients needed more than 180 days to be diagnosed. All of these cases have a pattern of periodic fever. When diagnosis is difficult, patients should be referred to a medical institution that could provide more detailed examinations and hospitalize them immediately to monitor the patterns of fever.
In patients who fulfilled and did not fulfill the criteria of classical FUO, the most useful diagnostic procedure was determined according to the criteria of each disease. Especially in non-infectious inflammation, the most prevalent diseases of FUO such as AOSD, BD, and PMR did not have any specific image inspection or serological markers, including antinuclear antibody and rheumatoid factor. Therefore, we strictly diagnosed in accordance with the criteria of each disease. Fifty-two (49.5%) of 105 patients who fulfilled the criteria of classical FUO had undergone PET-CT, which was useful for diagnosing neoplasms such as malignant lymphoma and breast cancer in this study. Patients with AOSD showed increased fluorodeoxyglucose (FDG) accumulation in the bone marrow, spleen, and lymph nodes [Citation8,Citation14,Citation15]. As a diagnosis of AOSD, we have any specific biomarker and definitive findings of images. The key to diagnosing AOSD is to exclude other positive diseases that may cause FUO. Therefore, PET-CT findings may support the diagnosis of AOSD by excluding infection, solid tumors, or other non-infectious inflammatory diseases in addition to detecting the presence or absence of accumulation in the bone marrow. Patients with PMR showed increased FDG accumulation in the bone nodules, femoral trochanter, and spinous process [Citation8,Citation16]. PET-CT was considered as one of the supportive tools for diagnosis of non-infectious inflammation. In this study, 9 of 11 patients with AOSD and 3 of 5 patients with PMR who fulfilled the criteria of classical FUO and 2 of 2 patients with AOSD who did not fulfill the criteria of classical FUO showed characteristics of FDG accumulation ().
Thirty-nine patients did not fulfill the criteria of classical FUO, and, in these cases, the fever was lower than 38.3 °C or the duration of fever was less than 3 weeks. In the former cases, the duration of diagnosis was not relatively long, but the latter cases showed a tendency to need a longer duration until diagnosis. Thirteen of 39 patients had periodic fever, and these patients needed a particularly long period to be diagnosed because the duration of fever was only a few days. The longest duration to diagnose was 9 years (). FMF, which was frequent in patients who did not fulfill the criteria of classical FUO, is an inherited autoinflammatory disease characterized by recurrent febrile episodes and inflammation in the form of sterile polyserositis [Citation17]. Because of genetic analysis of MEFV mutations, many FMF patients have been reported in Japan [Citation18–20]. Typical FMF is characterized by a fever duration as short as 1–3 days, with spontaneous remission. In this study, only 1 patient had typical FMF and most cases of FMF were atypical. Patients with atypical FMF who present with atypical phenotypes such as long duration of fever and have mutations, except exon 10, are not rare in Japan [Citation20]. However, even in atypical FMF, it is rare to have fever for more than 3 weeks. Therefore, many patients with FMF do not fulfill the criteria of classical FUO and spend a long time without detailed examination. In this study, most patients who needed a long duration for diagnosis spent several years before they visited a hospital to undergo detailed examination. It was considered that the presence of periodic fever in patients with FUO was revealed due to the comparison of patients who fulfilled the criteria of classical FUO and those who did not fulfill them. As the diseases causing periodic fever are recognized, periodic fever becomes an important factor in FUOs. When examining patients who have FUO, we should pay attention not only to patients who fulfill the criteria of classical FUO but also to patients who do not fulfill them. In patients who do not fulfill the criteria of FUO, periodic fever is important as a differential diagnosis, and focusing on periodic fever leads to improved diagnostic precision. We also should consider the position of periodic fever in the criteria of FUO.
There are some potential limitations in our study. The population of our study is small, and the diseases of the patients pose inherent bias because this study was conducted at a university hospital where the researchers’ specialization was rheumatology. The other limitation is the study’s retrospective design. A study with a large population is necessary to observe patients with FUO and determine the most useful diagnostic tools. Thereby, new criteria for periodic fever in FUO may be established. In addition, new criteria for FUO that take into account patterns of fever including periodic fever are expected in the near future.
In conclusion, the results of this study showed that the rate of neoplasm had declined, and more than half of the patients were diagnosed relatively early after their first visit. As the results show, diseases that can lead to definitive diagnosis are increasing due to the progress in disease recognition and diagnostic tools. However, some patients needed more than 180 days for diagnosis, and we should be considerate about these patients. The presence of periodic fever that does not fulfill the criteria of classical FUO was identified; therefore, we should consider including periodic fever in the criteria of FUO. Our study results may be helpful in updating the criteria of FUO, which can assist in the early diagnosis of diseases with periodic fever that usually take a long time to be diagnosed.
Acknowledgments
We thank all the staff of our hospital and the patients. We also thank Dai Kishida for the valuable help and support with the genetic analysis of Mediterranean fever. We would also like to thank Editage (www.editage.com. . . . . . . ) for English language editing.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Pertersdorf RG, Beeson PB. Fever of unexpected origin-report on 100 cases. Medicine. 1961;40:1–30.
- Durack DT, Street AC. Fever of unknown origin-reexamined and redefined. Curr Clin Top Infect Dis. 1991;11:35–51.
- Fukuhara H, Tamaki K, Nakamura H, et al. A retrospective study of hospitalized patients with fever of unknown origin during six years (in Japanese). Kansennsyogaku Zasshi. 1990;64(3):335–341.
- Shoji S, Imamura A, Imai Y, et al. Fever of unknown origin: a review of 80 patients from the Shin’etsu area of Japan from 1986–1992. Intern Med. 1994;33(2):74–76.
- Ryuko H, Otsuka F. A comprehensive analysis of 174 febrile patients admitted to Okayama University Hospital. Acta Med Okayama. 2013;67(4):227–237.
- Yamanouchi M, Uehara Y, Yokokawa H, et al. Analysis of 256 cases fever of unknown origin. Intern Med. 2014;53(21):2471–2475.
- Goto M, Koyama H, Takahashi O, et al. A retrospective review of 226 hospitalized patients with fever. Intern Med. 2007;46(1):17–22.
- Yamashita H, Kubota K, Mimori A. Clinical value of whole-body PET/CT in patients with active rheumatic disease. Arthritis Res Ther. 2014;16(4):423.
- Stojanov S, Kastner DL. Familial autoinflammatory diseases: genetics, pathogenesis and treatment. Curr Opin Rheumatol. 2005;17(5):586–599.
- Livneh A, Langevitz P, Zemer D, et al. Criteria for the diagnosis of familial Mediterranean fever. Arthritis Rheum. 1997;40(10):1879–1885.
- The criteria provided by the investigation and Research committee for FMF organized by the Japanese Ministry of Public Welfare, 2015.
- Iikuni Y, Okada J, Kondo H, et al. Current fever of unknown origin 1982–1992. Intern Med. 1994;33(2):67–73.
- Oka T. Psychogenic fever: how psychological stress affects body temperature in the clinical population. Temperature. 2015;2(3):368–378.
- Dong M, Wang C, Zhao K, et al. 18F-FDG PET/CT in patients with adult-onset Still’s disease. Clin Rheumatol. 2015;34(12):2047–2056.
- Yamashita H, Kubota K, Takahashi Y, et al. Clinical value of 18F-fluoro-dexoxyglucose positron emission tomography/computed tomography in patients with adult-onset Still’s disease: a seven-case series and review of the literature. Mod Rheumatol. 2014; 24:645–650.
- Yamashita H, Kubota K, Takahashi Y, et al. Whole-body fluorodeoxyglucose positron emission tomography/computed tomography in patients with active polymyalgia rheumatica: evidence for distinctive bursitis and large-vessel vasculitis. Mod Rheumatol. 2012;22(5):705–711.
- Ben-Chetrit E, Levy M. Familial Mediterranean fever. Lancet. 1998;351(9103):659–664.
- Migita K, Uehara R, Nakamura Y, et al. Familial Mediterranean fever in Japan. Medicine. 2012;91(6):337–343.
- Kunimatsu J, Maeda J, Watanabe R, et al. Fever of unknown origin in the outpatient setting: a retrospective analysis of 30 cases of Mediterranean fever (in Japanese). Jpn J Clin Immunol. 2016;39(2):130–139.
- Migita K, Izumi Y, Jiuchi Y, et al. Familial Mediterranean fever is no longer a rare disease in Japan. Arthritis Res Ther. 2016;18(1):175.
