Abstract
Western countries that were first to administer the COVID-19 vaccination report cases of vaccine-induced axillary lymphadenitis with high FDG uptake. However, no such findings have been reported from any Asian countries. We report here a confusing case of a 31-year-old female cancer survivor with high FDG uptake in her axillary lymph nodes, suggesting recurrence, following mRNA COVID-19 vaccination. Although the value of SUVmax was elevated (12.7), additional imaging revealed that her lymphatic lesions were benign, and they resolved spontaneously. This case of a strong immune reaction to COVID-19 vaccination in regional lymph nodes is the first reported in a Japanese patient. We should be aware of this new mimic and optimize diagnostic imaging methods accordingly in the era of COVID-19.
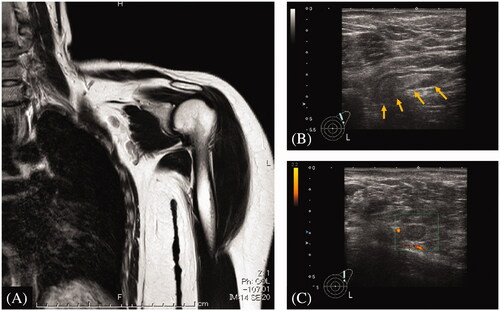
A 31-year old woman with a history of metastatic Ewing sarcoma treated with radical local resection, 5 courses of chemotherapy, and tandem high-dose chemotherapy 14 years earlier presented with right flank pain, the same site as the primary lesion. Since she had just received an annual follow-up CT scan indicating no evidence of recurrence or second malignancy, we conducted further studies. PET-CT scan revealed a focus of significantly increased FDG uptake (SUVmax, 12.7), in the range of malignancy, on her left axillary lymph nodes (). She didn’t present with accompanying symptoms such as fever, malaise, or localized axillary pain. We suspected relapse or secondary tumor and considered biopsy. However, because she had received the Pfizer mRNA COVID-19 vaccination in the left deltoid muscle three weeks before the PET-CT scan, we chose close follow-up as the course of action. Her flank pain naturally resolved in four weeks, and the MRI and US conducted after PET-CT confirmed lymph node hilum, suggesting an inflammatory lesion rather than metastatic lymph node swelling (). We concluded that her lymphadenitis with extremely high SUV was the result of a strong immune response to the COVID-19 vaccine.
Figure 1. (A) 3 D MIP 18F-FDG PET image in coronal view shows increased uptake in the left axillary lymph nodes (SUVmax, 12.7). In the left deltoid muscle, no increase in FDG uptake was observed. (B) Axial view shows the same finding as the 3 D MIP image.
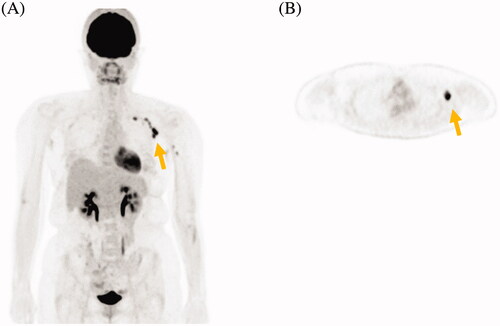
Figure 2. (A) MRI T2-weighted image shows enlarged lymph nodes with normal hilum. (B) The ultrasonographic image shows enlarged lymph nodes (3.5 mm × 9 mm, yellow arrows) with cortical hypertrophy. The nodal hilum was confirmed to be normal. (C) Color doppler image shows normal intranodal and perinodal blood flow.
To the best of our knowledge, this case of lymphadenitis with high FDG uptake caused by COVID-19 vaccine is the first reported in a Japanese patient. This case raises two important clinical questions: (1) Is COVID-19 vaccine-related regional lymphadenitis a common phenomenon among Japanese people? (2) What is the optimal way to assess lymphatic metastasis or relapse in a patient during or after cancer treatment in this era of the COVID-19 pandemic?
Although COVID-19 vaccine-induced axillary lymphadenitis has been reported in the US and European countries, where vaccination was initiated earlier, no such observation has been reported from Asian countries, including Japan [Citation1–4]. The severity of COVID-19 infection is known to vary between ethnic groups, as inherent genetic differences contribute to differing immune responses to the virus that affect the course of the disease [Citation5]. A cohort study of 650 Israeli patients showed that axillary lymphadenitis after COVID-19 vaccination was common but involved only a mild to moderate increase in FDG uptake [Citation4]. Whether the immune response to the vaccine differs between races is unclear, but our case shows that a Japanese individual had a significant immune reaction in lymph nodes adjacent to the vaccination site, with a significantly higher FDG uptake than previously reported [Citation4].
COVID-19 vaccination should be recommended for cancer patients because of their immunocompromised status [Citation6]. These patients undergo frequent imaging evaluation to assess their disease status, both during and after cancer treatment. Although there have been reports of FDG accumulation in lymph nodes after conventional vaccination like flu, the resolution generally occurred within 2 weeks, so the interval between imaging and vaccination only needed to be 2 weeks. However, according to a study in the elderly, high FDG uptake in lymph nodes due to this novel mRNA vaccine remains in about 40% of patients 7 weeks after vaccination [Citation7]. Thus, increased FDG accumulation induced by COVID-19 vaccination is a more confusing finding for their clinicians. Undoubtedly, more clinicians will encounter this new mimic in the near future. Thus, recognizing this phenomenon is important, both for accurate diagnosis and to arrange the appropriate interval between imaging tests and vaccination.
In conclusion, we present the first Japanese case of significant axillary lymphatic FDG accumulation caused by the COVID-19 vaccine. The SUVmax was equivalent to that observed in malignant disease, but the clinical course was self-limiting. Awareness of this new mimic and careful assessment of axillary lymphadenitis are important during the era of COVID-19. The accumulation of further cases is needed to examine this phenomenon across ethnic groups.
Geolocation information
This study was conducted at Shizuoka Cancer Center, Shizuoka, Japan, located at 35.1563°N, 138.8843°E.
Acknowledgments
The authors would like to thank Enago (www.enago.jp) for the English language review.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Singh B, Kaur P, Kumar V, et al. COVID-19 vaccine induced axillary and pectoral lymphadenopathy on PET scan. Radiol Case Rep. 2021;16(7):1819–1821.
- Eifer M, Eshet Y. Imaging of COVID-19 vaccination at FDG PET/CT. Radiology. 2021;299(2):E248.
- Seban RD, Champion L, Deleval N, et al. Immune response visualized in vivo by [18F]-FDG PET/CT after COVID-19 vaccine. Diagnostics. 2021;11(4):676.
- Bernstine H, Priss M, Anati T, et al. Axillary lymph nodes hypermetabolism after BNT162b2 mRNA COVID-19 vaccination in cancer patients undergoing 18F-FDG PET/CT: a cohort study. Clin Nucl Med. 2021;46(5):396–401.
- Tal Y, Adini A, Eran A, et al. Racial disparity in Covid-19 mortality rates – a plausible explanation. Clin Immunol. 2020;217:108481.
- Ribas A, Sengupta R, Locke T, et al. Priority COVID-19 vaccination for patients with cancer while vaccine supply is limited. Cancer Discov. 2021;11(2):233–236.
- Eshet Y, Tau N, Alhoubani Y, et al. Prevalence of increased FDG PET/CT axillary lymph node uptake beyond 6 weeks after mRNA COVID-19 vaccination. Radiology. 2021;300(3):E345–E347.
