Abstract
Immune checkpoint inhibitors (ICIs) for various types of malignancy, including non-small-cell lung cancer, have improved prognosis in some cases. Granuloma formation after ICI administration suggests a tumor antigen-specific cytotoxic T cell response with abundant interferon-gamma production, which can be used to estimate the curative effect of ICIs. In this report, we present a case with a resected lung lesion, clinically suspected to be lung cancer, that consisted of a granulomatous lesion. A tumor was also found in the duodenum that was presumed to be derived from the pulmonary pleomorphic carcinoma. Duodenal tumor cells highly expressed PD-L1, suggesting PD-1/PD-L1 axis-mediated immune escape. As expected, pembrolizumab induced a complete response for the duodenal lesion. Interestingly, in histopathological analysis, the duodenal lesion was also replaced by an epithelial granuloma and multinucleated giant cells. We conclude that autoimmunity regressed the untreated primary lung lesion spontaneously, while the metastatic duodenal lesion responded to PD-1 blockade. Tumor-associated epithelioid granulomas, even before ICI administration, may be an important pathological finding indicating an immune response with interferon-gamma production by cytotoxic T cells to the tumor.
1. Introduction
Immune checkpoint inhibitor (ICI)-based cancer immunotherapy is now one of the standard therapeutic approaches for several types of cancer [Citation1]. It is often adopted as first-line treatment and a complete response (CR) to ICI treatment is not uncommon [Citation2]. However, few cases have been reported in which tissue samples were obtained and analyzed histopathologically after CR. Histological examination of lesions after CR may be useful in differential diagnosis, and it may also provide important information to clinicians and pathologists on the histopathological hallmarks of anti-tumor immunity.
In this report, we present a case of primary pulmonary pleomorphic carcinoma with spontaneous regression and its duodenal metastasis, which achieved a histological CR after pembrolizumab-mediated programmed death receptor (PD)-1 blockade.
2. Case report
A 57-year-old man was referred to our hospital after a chest shadow was found on X-ray examination at another hospital. Computed tomography (CT) imaging identified a space-occupying lesion with a maximum diameter of 6 cm in the left pulmonary hilar region, suggesting lung cancer (). No other potential primary lesion was identified. Since a transbronchial ultrasound endoscopy-guided needle biopsy did not provide any malignant findings, a partial resection of the left upper lobe was performed as an excisional biopsy. Histopathological examination of the resected left upper lobe showed no malignant findings in the lung parenchyma. Instead, necrotic tissue surrounded by CD68-positive spindle or epithelioid cells was observed, indicating a necrotizing granuloma (). These findings suggested differential diagnoses of granulomatous lung diseases, including Mycobacterium tuberculosis (TB) or other infections, sarcoidosis, or granulomatosis with polyangiitis (GPA). The patient showed persistent fever and an inflammatory response evidenced by his white blood cell count and serum concentration of C-reactive protein after surgery.
Figure 1. Clinical and pathological images of the lung. (A) Computed tomography image showing a low-intensity lesion measuring approximately 6 cm in the left pulmonary hilum (arrows). (B) Low-power field image of a resected lung specimen with hematoxylin and eosin (HE) staining. The necrotic tissue is within the yellow dotted line. The granulomatous lesion around the necrotic tissue is located between the white and yellow dotted lines. Bar, 500 μm. (C) High-power field image of the granulomatous lesion. Spindle cells are positive for CD68, a histiocytic marker, while cytokeratin, an epithelial marker, is expressed by the remaining lung tissue. Bar, 100 μm.
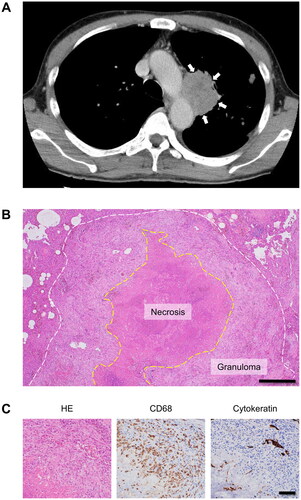
Blood tests were negative for Aspergillus antigen. A TB antigen-specific interferon-gamma (IFNγ) release assay did not indicate TB infection. While the serum level of soluble interleukin-2 receptor was slightly increased, the levels of angiotensin-converting enzyme and myeloperoxidase or proteinase 3 antineutrophil cytoplasmic antibodies were within the normal range. Although obliterating phlebitis was observed, there was no necrotizing angiitis. Later additional histopathological investigations revealed a small number of atypical and less cohesive spindle cells with pan-cytokeratin (clone AE1/AE3) expression in the vessels at the edge of the lesion, indicating the existence of local malignant cells (Supplement Figure 1).
At 8 months after the first visit, abdominal CT showed thickening of the duodenal wall (). Gastrointestinal endoscopy revealed a type 2 tumor in the third portion of the duodenum. The duodenal biopsy specimen consisted predominantly of polygonal cells with an abundant amount of pale eosinophilic cytoplasm, irregular nuclear contour, and increased chromatin, suggesting a malignant tumor (). The tumor cells did not express caudal type homeobox 2, a marker for intestinal differentiation (data not shown). Although the tumor cells were positive for cytokeratin 7, no other typical diagnostic markers for pulmonary adenocarcinoma or squamous cell carcinoma were detected (data not shown). A SWI/SNF-related, matrix-associated, actin-dependent regulator of chromatin, subfamily A, member 4 (SMARCA4)-deficient tumor was also excluded, indicating pleiotropic carcinoma probably originating from the lung. Since more than 50% of the tumor cells highly expressed programmed death ligand 1 (PD-L1), pembrolizumab monotherapy was started as first-line treatment for metastatic pulmonary pleomorphic carcinoma ().
Figure 2. Clinical and pathological images of the duodenum. (A) Computed tomography image showing duodenal wall thickening (arrow). (B) More than 50% of tumor cells with a pleomorphic appearance are positive for PD-L1 (clone: 22C3). (C) Low-power field image of the resected duodenum specimen with HE staining. An epithelioid granulomatous lesion is observed in the submucosa (within the dotted line). Bar, 500 μm. (D) High-power field image of the epithelioid granulomatous lesion with prominent lymphocyte infiltration. Arrows indicate multinucleated giant cells. Bar, 100 μm.
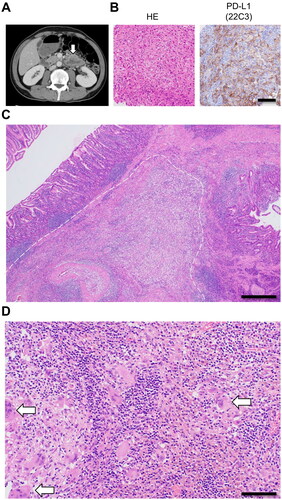
After two cycles of pembrolizumab, the patient visited our hospital complaining of fatigue. Hematological examination suggested anemia due to hemorrhage. Gastrointestinal endoscopy found bleeding from the tumor and a partial duodenectomy was performed. Histopathological examination of the resected duodenum found no residual malignancy but instead revealed an epithelioid granuloma with multinucleated giant cells (). After discharge from our hospital, pembrolizumab administration was resumed and there has been no recurrence as of 3 months after discharge.
3. Discussion
In this case, examination of a surgically resected lung specimen indicated that the lesion consisted of necrotic tissue surrounded by CD68-positive granuloma cells. Additional histological investigation revealed pan-keratin-positive tumor emboli around the granulomatous lesion, indicating the previous existence of malignant cells there. In addition, there was no evidence of any granuloma-forming diseases such as TB infection or sarcoidosis as determined by Ziehl-Neelsen staining, detection of TB-specific IFNγ-secreting T cells, and serum concentration of angiotensin-converting enzyme. Although GPA-like granulomatous autoimmune disease was also included as a potential diagnosis, there was no evidence of GPA indicated by typical biomarkers or histological findings. We concluded that the lung tumor cells regressed spontaneously by means of autoimmunity. The duodenal metastatic lesion expressed high levels of PD-L1, suggesting PD-1/PD-L1 axis-mediated immune escape. After PD-1 inhibition by pembrolizumab administration, no malignant cells were detected in the resected duodenal lesion. Instead, this lesion was replaced by a granuloma composed of multinucleated giant cells and epithelioid cells, indicating that a histological CR had been obtained.
As reported previously, tumors with a high mutation burden tend to be sensitive to ICI-mediated cancer immune therapy [Citation3]. Morphologically, pulmonary pleomorphic carcinoma shows, as its name implies, pleomorphic and bizarre nuclei, suggesting an increased mutation burden. Numerous studies have reported the successful treatment of pulmonary pleomorphic carcinoma [Citation4,Citation5]. Although a putative primary pulmonary lesion was likely to have been established in the present case, the immune tolerance of the tumor cells appears to have been broken by some unknown trigger(s). This type of autoimmune-mediated almost complete and spontaneous anti-tumoral response has been reported rarely for decades [Citation6]. Unfortunately, we could not investigate the exact mechanism by which the tumor cells escaped from immune surveillance and later became susceptible to it.
An increasing number of reports have identified granulomatous reactions, especially in cases in which ICI-mediated cancer immunotherapy is effective [Citation7,Citation8]. Nevertheless, few reports have described histological analysis of resected specimens after a complete response to ICIs. In addition, the current case is the first report showing the pleomorphic carcinoma being replaced by granulation as a natural course. This is probably because spontaneous regression itself is uncommon, and surgically resection of such case is further rare. After careful exclusion of other granuloma-forming diseases, an epithelioid granuloma may be a hallmark of the histopathological effect of the ICI-induced anti-tumor effect. A type 1 immune response should commonly underlie this phenomenon as well as TB infection or sarcoidosis. IFNγ, a cytokine applied for the diagnosis of TB infection, would a key factor for granuloma formation by ICIs. In the present case, the granulomatous lesion in the lung formed before ICI administration. Therefore, the presence of granulomas spatiotemporally coexisting with malignancy would suggest a type 1 immune response with tumor antigen-specific CTLs, indicating a potential predictive marker for successful treatment with PD-1 blockade.
The anti-tumor response in this case may be attributed to the high immunogenicity of pleomorphic carcinoma. However, not all pleomorphic carcinomas can be eliminated by autoimmunity. Therefore, the systemic immune status of the host would also have been involved as well as tumor immunogenicity. Does systemic type 1-deviated inflammation, as an opposite notion to systemic type 2 inflammation in patients with atopic disorders, exist? [Citation9,Citation10] Although this point is not well understood, clinical or subclinical infection or enterobacterial flora in addition to genetic background may be profoundly involved. Further investigation into systemic type 1-deviated inflammation is required. We believe that knowledge and expertise obtained in autoimmune and allergic diseases will help in elucidating this problem.
In conclusion, we have shown that the presence of a significant immunological anti-tumor effect for pulmonary pleomorphic carcinoma and its metastatic lesion with and even without PD-1 blockade. A granulomatous lesion may be a histopathological hallmark of the ICI-induced anti-tumor effect. We also propose that pathologists should be vigilant and remark on the presence of granulomas associated with malignancy in this new era of ICI treatment. Further accumulation of similar cases is required.
Informed consent
Appropriate written consent was obtained from the patient.
Supplemental Material
Download MS Word (12.7 KB)Supplemental Material
Download TIFF Image (3.1 MB)Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Kubo T, Shinkawa T, Kikuchi Y, et al. Fundamental and essential knowledge for pathologists engaged in the research and practice of immune checkpoint inhibitor-based cancer immunotherapy. Front Oncol. 2021;11:679095.
- Iacovelli R, Ciccarese C, Schutz FA, et al. Complete response to immune checkpoint inhibitors-based therapy in advanced renal cell carcinoma patients. A meta-analysis of randomized clinical trials. Urol Oncol. 2020;38(10):798.e17–798.e24.
- Yarchoan M, Hopkins A, Jaffee EM. Tumor mutational burden and response rate to PD-1 inhibition. N Engl J Med. 2017;377(25):2500–2501.
- Babacan NA, Pina IB, Signorelli D, et al. Relationship between programmed death receptor-ligand 1 expression and response to checkpoint inhibitor immunotherapy in pulmonary sarcomatoid carcinoma: a pooled analysis. Clin Lung Cancer. 2020;21(5):e456–e63.
- Honjo O, Kubo T, Sugaya F, et al. Severe cytokine release syndrome resulting in purpura fulminans despite successful response to nivolumab therapy in a patient with pleomorphic carcinoma of the lung: a case report. J Immunother Cancer. 2019;7(1):97.
- Kumar T, Patel N, Talwar A. Spontaneous regression of thoracic malignancies. Respir Med. 2010;104(10):1543–1550.
- Gkiozos I, Kopitopoulou A, Kalkanis A, et al. Sarcoidosis-like reactions induced by checkpoint inhibitors. J Thorac Oncol. 2018;13(8):1076–1082.
- Kubo T, Hirohashi Y, Keira Y, et al. Identification of characteristic subepithelial surface granulomatosis in immune-related adverse event-associated enterocolitis. Cancer Sci. 2021;112(3):1320–1325.
- Lloyd CM, Snelgrove RJ. Type 2 immunity: expanding our view. Sci Immunol. 2018;3(25):eaat16040.
- Pucci S, Incorvaia C. Allergy as an organ and a systemic disease. Clin Exp Immunol. 2008;153 Suppl 1(Suppl 1):1–2.
