Abstract
Background
Heart rate variability (HRV) a feasible predictor of prognosis in cardiovascular outcomes shown to be reduced in people living with HIV (PLWH).
Objective
This study sought to understand the effects of short-term aerobic training (AT) on the resting HRV and endothelial function in this population.
Methods
PLWH performed 24 sessions of AT protocol. The protocol consists of 40 min of treadmill (60 to 80% of the VO2max), 3 times per week, for 8 weeks. HRV (standard deviation of all normal RR intervals - SDNN; root mean square of the successive differences - rMSSD; low frequency - LF; high frequency - HF; LF:HF ratio) and endothelial function parameters were evaluated by EndoPAT system pre and post intervention.
Results
7 men, the median age of the sample was 49 years (range, 38–68 years), completed the protocol. AT improved resting HRV parameters: SDNN (p = 0.02, power analysis (PA) 0.54), rMSSD (p = 0.02, PA = 0.99), LF (p = 0.02, PA = 0.85). HF, LF:HF ratio and endothelial function parameters showed no changes.
Conclusions
The results suggest the short-term AT may improve HRV in men living with HIV.
Introduction
The autonomic nervous system (ANS) plays a key role in cardiovascular homeostasis and may be regarded as a strong predictor of prognosis in cardiovascular outcomes.Citation1–3 In clinical studies, the ANS is often evaluated according to heart rate variability (HRV), which may be assessed using several methods. Among time domain measures, the root mean square of successive differences (rMSSD) is an indicator of parasympathetic activity, while standard deviation of all normal RR intervals (SDNN) reflects sympathetic and parasympathetic activity. In the frequency domain, low frequency (LF) reflects sympathetic and parasympathetic activity, and high frequency (HF) and LF: HF ratio are indicators of parasympathetic activity.Citation1,Citation3 Thus, a decrease in HRV is indicative of vagal control impairment and alteration(s) to sympathovagal balance.Citation4
Previous data have demonstrated that people living with human immunodeficiency virus (PLWH) undergoing antiretroviral therapy exhibit reduced HRV and endothelial dysfunction, which may be associated with the risk for cardiovascular disease (CVD) and mortality.Citation2,Citation5–7 Furthermore, ANS dysfunction demonstrated a positive correlation between the level of physical activity and HRV,Citation3 suggesting that PLWH could benefit from improved fitness. As such, aerobic training (AT) has been used to improve physical fitnessCitation8 and parasympathetic and sympathetic activity in different populations.Citation3,Citation9–11 However, the effects of AT on HRV remain inconclusive in PLWH undergoing antiretroviral therapy. Accordingly, the aim of the present study was to evaluate the effects of short-term AT on resting HRV and endothelial function in PLWH.
Material and methods
Subjects
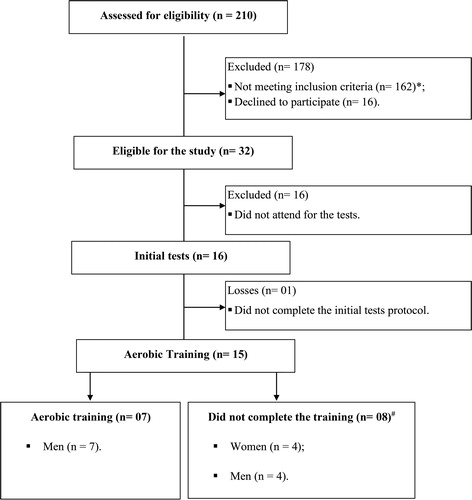
This pre-post pilot study was conducted with PLWH 18–75 years of age, who were recruited at the Department of Infectious Diseases of the Irmandade da Santa Casa de Misericórdia de Porto Alegre, Rio Grande do Sul, Brazil. The study was approved by the Ethics Committee of the Universidade Federal de Ciências da Saúde de Porto Alegre (n° 797.649/14). Participants had a confirmed diagnosis of HIV infection, a viral load < 50 copies/mL, and were > 18 years of age. Exclusion criteria and study losses are shown in . All patients provided informed written consent to participate before data collection.
Figure 1 Flow diagram of PLWH selection for participation in the aerobic training program. *Co-infection with hepatitis C virus (n = 86), hepatitis B virus (n = 7), diagnosed with psychological disorders (n = 6), cardiac abnormalities (n = 6), absence of ARV adherence (n = 6), human T-lymphotropic virus (n = 5), motor changes (n = 5), pregnancy (n = 3), Chagas disease (n = 2), cognitive impairment (n = 2), severe anemia (n = 2) illicit drug use (n = 1),visually impaired (n = 1) and 30 people living with HIV had 2 or more of these associated changes. #Abandoned training (n = 4), muscle injures (n = 2), cancer diagnosis (n = 1) and drug treatment failure (n = 1).
Anthropometric and clinical data
Body mass (kg), height (meters) and abdominal circumference were measured in the first and final training session. Fasting blood glucose, total cholesterol, triglycerides, HDL-C, LDL-C, T CD4 and viral load were collected from patient’s medical records before and after training protocol.
Cardiopulmonary exercise testing
Cardiopulmonary exercise testing (CPX) was performed using an electric treadmill (Centurion 300, Micromed Biotecnologia, Brasilia, Brazil). The ramp protocol was started at 3 km/h and 0% slope, and both treadmill speed and slope were increased gradually until participant exhaustion. The workload test was designed to obtain maximal oxygen uptake (VO2max) within 8–12 min. The test was concluded when the peak respiratory exchange ratio was > 1.1 and VO2 plateau was reached, even with increasing workload or request of the participant.Citation12 Ventilatory and metabolic parameters were collected by respiration using a spiro-ergometry system (Metalyzer 3B, Cortex Biophysik GmbH, Leipzig, Germany). The average of data points collected during the final 30 s of the test were used to determine peak oxygen uptake (VO2peak) and maximal heart rate (HRmax). CPX was applied pre-intervention, and at 12 and after the 24 exercise training sessions.
HRV and endothelial function
HRV and endothelial function were evaluated using a pulse tonometry device (EndoPAT2000, Itamar Medical, Caesarea, Israel). For both tests, a blood pressure cuff is placed on one upper arm, while the contralateral arm serves as the control. After a 5 min equilibration period, the cuff is inflated to a pressure of 50 mmHg above systolic pressure or 200 mmHg for 5 min, and then deflated to induce a reactive hyperemia.Citation13
Digital pulse amplitude was measured by placing a sensor on the tip of both index fingers with the patient supine. HRV parameters were calculated from the beat-by-beat HR time series over a duration of 10 min. The amplitude of the pulse response was recorded electronically in both index fingers and digitally analyzed using the computerized system (Itamar Medical, Caesarea Israel). SDNN and rMSSD were measured in the time-domain HRV, while LF, HF, and LF:HF ratio were calculated in the frequency-domain, HRV. The accuracy of HRV assessment according to EndoPAT 2000 was previously validated by Linder et al.,Citation14 while endothelial function was evaluated according to the natural logarithm of the RH-PAT index (lnRHI) and augmentation index.
AT
Participants performed AT 3 times per week for a total of 24 sessions. Each session consisted of a 5 min warm-up, 30 min of exercise with load determined by CPX, and 5 min of cool-down.Citation15 From the first to the 12th session, exercise was performed at an HR corresponding to 60–65% of VO2peak and, from the 13th to the 24th sessions, was increased to 75–80% of VO2peak. Exercise intensity was adjusted in the 13th session based on the new CPX.
Statistical analysis
Statistical analysis was performed using GraphPad Prism version 7 (GraphPad Inc, San Diego, CA, USA). Data are expressed as median (range). The Wilcoxon matched-pairs signed rank test was used to compare baseline and post-test values. Differences with p ≤ 0.05 were considered to be statistically significant. Effect size (ES) and study power analysis (PA) were calculated using G*Power version 3.1.9.4.
Results
Fifteen patients were eligible to participate in the present study; however, only 7 men consented to and completed the AT protocol. The median age of the sample was 49 years (range, 38–68 years), the median time of diagnosis and medication use was 93 (range, 12–182) and 93 (range, 10–180) months, respectively.
AT decreased body mass [74 (69.5–104.2) versus 71.7 (69–100.50) kg]; p = 0.02; abdominal circumference [98 (64–114) versus 94 (62–108) cm]; p = 0.02; fasting blood glucose [112 (88–128) versus 98 (86–116)] mg/dL; p = 0.02, total cholesterol [208 (178–340) versus 178 (152–228) mg/dL]; p = 0.03; triglycerides [273 (137–296) versus 204 (133–223) mg/dL]; p = 0.02; LDL-C [127 (89–252) versus 109 (85–154) mg/dL]; p = 0.02; and increased in VO2peak [25 (16–45) versus 36 (28–43) ml.kg−1.min−1]; p = 0.03. All participants had undetectable viral load < 50 copies/mL.
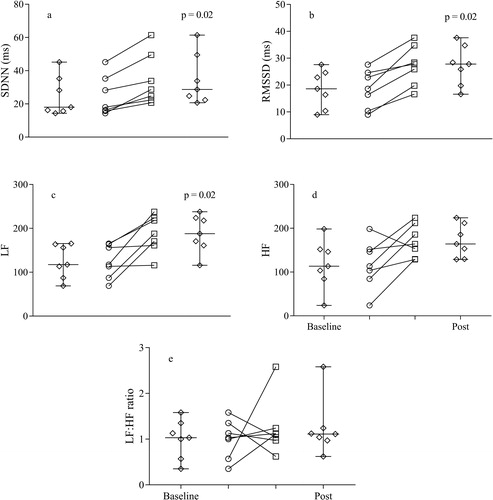
AT increased SDNN (p = 0.02, ES = 0.96, PA = 0.54), rMSSD (p = 0.02, ES = 2.00, PA = 0.99), and LF (p = 0.02, ES = 1.41, PA = 0.85), while HF (ES = 0.91, PA = 0.50) and LF:HF ratio (ES = 0.07, PA = 0.05) demonstrated no changes. Both time and frequency-domain HRV parameters are shown in . There was no significant change in the values of endothelial function (lnRHI = 1.26 [0.57–1.74] versus 1.28 [0.63–1.78]; p = 0.49) and augmentation index (5.50% [-4–14] versus 4% [-7–18]; p = 0.73).
Figure 2 Effects of aerobic training on heart rate variability in PLWH. (A) SDNN: standard deviation of normal sinus rhythm pulse intervals/ms; (B) RMSSD: root mean square of the successive differences/ms; (C) LF: low frequency; (D) HF: high frequency; (E) LF:HF ratio. Diamonds represent the average values. Circles and squares represent individual data before and after for aerobic training. Wilcoxon matched-pairs signed rank test was applied to compare baseline and post values. Statistical significance was defined as p ≤ 0.05.
Discussion
Results of the present study demonstrated that short-term AT may improve HRV in PLWH. The training protocol increased SDNN and rMSSD parameters, with a large ES.Citation16 rMSSD and HF are indexes associated with the parasympathetic system, suggesting improvement in the ANS. Studies have suggested that reduced rMSSD is associated with risk factors for sudden death.Citation5,Citation17 Because HIV infection increases the risk for CVD, including sudden cardiac death,Citation5 is possible that the beneficial effects of AT on the ANS may decrease the risk for CVD.
Additionally, although HF was not significantly increased, is possible that a larger sample size may confirm the positive effect of AT on this particular marker. Thus, using the data obtained in this study (ES, 0.91; alpha error, 0.05), 13 subjects would be needed to reach a PA of 80%. Unfortunately, small sample sizes are typical in studies investigating the effects of exercise training in PLWH. A study involving PLWH did not find effects on HRV parameters after 16 weeks of concurrent training.Citation10 The authors pointed out that the absence of exercise-induced effects could be explained by small sample size and, particularly, reduced volume (20 min) used in the AT program. As such, exercise volume (30 min), as well as the progressive intensity applied in the present study, are in accordance with exercise protocols that improved HRV.Citation11,Citation18 Thus, moderate intensity AT, preferably >20 min per session, should be recommended to improve HRV in PLWH.
The decrease in HRV is associated with dysfunction of ANS cardiac markers and high risks for ventricular arrhythmias and mortality after acute myocardial infarction.Citation16 Information regarding the extent to which AT is capable of affecting morbidity and mortality remains contradictory, largely due to alterations in cardiovascular function.Citation1,Citation19 However, the benefits of AT for classic factors that contribute to CVD risk, such as lipid and glycemic alterations and sedentary lifestyle, have been well documented. Thus, the known benefits of AT for classic CVD risk factors in both healthy individuals and those with chronic diseases were supported by the results of this study.
In addition to improvement in classic CVD risk factors, we also observed a significant increase in VO2peak, which demonstrated enhancement in the functional capacity of PLWH. A study reported a positive correlation between VO2max and the time domain of HRV variables, indicating that AT promotes incremental improvement in HRV and demonstrated a positive association between VO2max and parasympathetic tone.Citation3 Although correlation analyses were not performed in this pilot study due to the small sample size, improvements in VO2peak were, nevertheless, obtained, along with an increase in HRV variables, thus corroborating these results.
We did not observe an improvement in endothelial function. Conversely, a meta-analysis reported that exercise training—especially AT and/or combined—may improve endothelial function in patients with diabetesCitation20; however, differences were not statistically significant when compared to those in the control group.Citation20 Furthermore, it is important to note that, in PLWH, endothelial dysfunction may be associated with other deleterious factors, such as an inflammatory environment and viral load, thus supporting its characterization as a complex challenge.Citation6,Citation7
Because this was a pilot study, results of the present investigation must be interpreted carefully. In addition to inferential tests, we included ES and PA to enhance the robustness of the data obtained. The complexity of factors underlying the health status of this particular patient population characterizes this as a complex intervention. The methods and protocol were, nevertheless, proven to be appropriate, although adherence to and acceptability of the protocol represent the primary challenges to implementation.
Results of the present study suggest that AT may improve HRV and the ANS, and decrease the influence of this system’s impairment on cardiac function in PLWH. Nevertheless, studies including a control group and a larger sample size(s) are needed to confirm our findings.
Disclosure statement
The are no relevant conflicts of interest to disclose.
Additional information
Funding
Notes on contributors
Candissa Silva da Silva
Candissa Silva da Silva, PhD, is Physiotherapist at Hospital de Clínicas de Porto Alegre (HCPA), Porto Alegre, Brazil. She works with emphasis on the respiratory and motor rehabilitation of hospitalized patients. She has experience in the field of Physiotherapy, investigating, especially cardiopulmonary rehabilitation, respiratory physiotherapy and cardiovascular diseases.
Luís Fernando Deresz
Luís Fernando Deresz, PhD, is an Adjunct Professor of the Physical Education department, Post-Graduation Program in Sciences Applied to Health and Coordinator of the Research Group Science, Health and Physical Performance at the Universidade Federal de Juiz de Fora, Campus Governador Valadares. Governador Valadares, Brazil. He has experience in the field of physical education, with an emphasis on physical training in special populations, investigating, especially, the effects of physical training on cardiovascular risk.
Giovana de Marchi Castelli
Giovana de Marchi Castelli, Physiotherapist, acts as distance education analyst at support Program for Institutional Development of Support Program for Institutional Development of the Unified Health System (PROADI-SUS) at Hospital Moinhos de Vento, Porto Alegre, Brazil.
Gilson Pires Dorneles
Gilson Pires Dorneles, PhD, is a postdoctoral researcher at the Cellular and Molecular Immunology Laboratory at Universidade Federal de Ciências da Saúde de Porto Alegre linked to the Postgraduate Program in Health Sciences. His line of research comprises the following topics: exercise physiology and immunology, sports training, obesity, immune system, inflammatory processes, exercise prescription for individuals with chronic non-communicable degenerative diseases and cardiopulmonary evaluation.
Letícia Mignoni
Letícia Mignoni, is a Physiotherapist at UFCSPA, Porto Alegre, Brazil.
Pedro Dal Lago
Pedro Dal Lago, PhD, is an Associate Professor at Department of Physiotherapy, Post-Graduation Program in Health Sciences, Post-Graduation Program in Rehabilitation Sciences at Universidade Federal de Ciências da Saúde de Porto Alegre. His projects involving applied clinical research, bench and animal experimentation move into the area of translational research with a focus on pathophysiology and non-pharmacological resources applied to cardiorespiratory diseases. His line of research comprises the following topics: cardiopulmonary rehabilitation, respiratory physiotherapy, animal models of cardiovascular diseases, heart failure, physical exercise and inspiratory muscle training.
References
- Spiers JP, Silke B, McDermott U, et al. Time and frequency domain assessment of heart rate variability: a theoretical and clinical appreciation. Clin Auton Res. 1993; 3(2):145–158.
- McIntosh RC. A meta-analysis of HIV and heart rate variability in the era of antiretroviral therapy. Clin Auton Res. 2016; 26(4):287–294.
- Kocher MH, Hetzler RK, Shikuma CM, et al. Autonomic function is associated with fitness level in HIV-infected individuals. Jacobs J AIDS HIV. 2015; 1(1):1–14.
- Vanderlei LC, Pastre CM, Hoshi RA, Carvalho TD, Godoy MF. Basic notions of heart rate variability and its clinical applicability. Rev Bras Cir Cardiovasc. 2009;24(2):205–217.
- Hsue PY, Waters DD. HIV infection and coronary heart disease: mechanisms and management. Nat Rev Cardiol. 2019; 16(12):745–759.
- Sinha A, Ma Y, Scherzer R, et al. Role of T‐cell dysfunction, inflammation, and coagulation in microvascular disease in HIV. J Am Heart Assoc 2016;5(12):e004243.
- Dysangco A, Liu Z, Stein JH, et al. HIV infection, antiretroviral therapy, and measures of endothelial function, inflammation, metabolism, and oxidative stress. PLoS One. 2017; 12(8):e0183511.
- Ibeneme S, Omeje C, Myezwa H, et al. Effects of physical exercises on inflammatory biomarkers and cardiopulmonary function in patients living with HIV: a systematic review with meta-analysis. BMC Infect Dis. 2019; 19(1):359–380.
- Villafaina S, Collado-Mateo D, Fuentes JP, et al. Physical exercise improves heart rate variability in patients with type 2 diabetes: a systematic review. Curr Diab Rep. 2017; 17(11):110.
- Pedro RE, Guariglia DA, Okuno NM, et al. Effects of 16 weeks of concurrent training on resting heart rate variability and cardiorespiratory fitness in people living with HIV/AIDS using antiretroviral therapy: a randomized clinical trial. J Strength Cond Res. 2016; 30(12):3494–3502.
- Bellavere F, Cacciatori V, Bacchi E, et al. Effects of aerobic or resistance exercise training on cardiovascular autonomic function of subjects with type 2 diabetes: A pilot study. Nutr Metab Cardiovasc Dis. 2018; 28(3):226–233.
- Balady GJ, Arena R, Sietsema K, et al. Clinician's Guide to cardiopulmonary exercise testing in adults: a scientific statement from the American Heart Association. Circulation 2010;122(2):191–225.
- Onkelinx S, Cornelissen V, Goetschalckx K, Thomaes, et al. Reproducibility of different methods to measure the endothelial function. Vasc Med. 2012; 17(2):79–84.
- Linder JR, Stauss HM, Gindes H, et al. Finger volume pulse waveforms facilitate reliable assessment of heart rate variability, but not blood pressure variability or baroreflex function. BMC Cardiovasc Disord. 2014; 14:180.
- Hand GA, Phillips KD, Dudgeon WD, et al. Moderate intensity exercise training reverses functional aerobic impairment in HIV-infected individuals. AIDS Care. 2008; 20(9):1066–1074.
- Cohen J. Statistical Power Analysis for the Behavioral Sciences–Second Edition. 12 Lawrence Erlbaum Associates Inc. Hillsdale, New Jersey, 13; 1988.
- Novak JL, Miller PR, Markovic D, et al. Risk assessment for sudden death in Epilepisy: the sudep-7 inventory. Front Neurol 2015;6:252.
- Ricca-Mallada R, Migliaro ER, Piskorski J, et al. Exercise training slows down heart rate and improves deceleration and acceleration capacity in patients with heart failure. J Electrocardiol. 2012; 45(3):214–219.
- Limberg JK, Dube S, Kuijpers M, et al. Effect of hypoxia on heart rate variability and baroreflex sensitivity during hypoglycemia in type 1 diabetes mellitus. Clin Auton Res. 2015; 25(4):243–250.
- Qiu S, Cai X, Sun Z, et al. Exercise training and endothelial function in patients with type 2 diabetes: a meta-analysis. Cardiovasc Diabetol. 2018; 17(1):64.
