Abstract
Background
The global shift in healthcare during the COVID-19 pandemic led to challenges in the care of people living with HIV.
Methods
We conducted a retrospective study that aimed to delineate sociodemographic, clinical characteristics and outcomes, of people living with HIV diagnosed with ocular syphilis.
Results
Fifty-three people living with HIV were identified with ocular syphilis. Thirty-eight (71.6%) presented ocular symptoms. Twenty-three (43.3%) underwent lumbar puncture, 5 (9.4%) were positive for neurosyphilis. Forty-seven (88.6%) received treatment, 32 (68%) received standard treatment with aqueous crystalline penicillin G, and 15 (31.9%) were treated with alternative regimens due to the impossibility of hospitalization. Six (11.3%) individuals were lost to follow-up and/or did not receive treatment. Eighteen (56.2%) out of 32 individuals in the aqueous crystalline penicillin G group experienced serological response, 5 (15.6%) experienced treatment failure, and 9 (28.1%) were lost to follow-up. In the alternative therapy group, 12 out of 15 individuals (80%) experienced serological response. One (6.7%) experienced treatment failure, and 2 (13.3%) were lost to follow-up.
Conclusions
During the COVID-19 health emergency in Mexico, alternative treatments for ocular syphilis demonstrated favorable clinical outcomes amid challenges in accessing hospitalization.
Introduction
Reported syphilis cases increased by 80% in the United States (US) between 2018 and 2022 (rising from 115,000 to more than 207,000), compounding a decades-long upward trend [Citation1]. Consequently, ocular syphilis (OS) is also on the rise. Reports describing large groups of individuals with OS treated in the 1990s and 2000s indicated that this was a rare diagnosis, accounting for <2% of all cases. In contrast, more recent reports describing cohorts of up to 85 individuals with OS in the US, Europe, and Australasia suggest the condition is re-emerging, consistent with the increasing incidence of the systemic infection [Citation2]. In addition to this, restrictive measures for COVID‐19 might have different effects or impact on syphilis, from the access to a confirmatory test to the possibility of hospitalization to treat ocular and/or neurosyphilis resulting in the need of ambulatory options for these individuals [Citation3].
According to the Centers for Disease Control and Prevention (CDC), OS manifestations should be treated with a 10–14 day scheme of aqueous crystalline penicillin G (ACPG) 18–24 million units [Citation4]; however, alternative regimen are described as second or third line therapy. Intravenous (IV) ceftriaxone, 2 g daily 10–14 days, has been described having the same efficacy as ACPG with complete clinical response after 1 month and serological response at 6 months in neurosyphilis (central nervous system, otic, and/or ocular involvement) in people living with HIV [Citation5]. In syphilitic uveitis, intravenous ceftriaxone 14–21 days, supplemented with intramuscular benzathine penicillin 7.2 million units, showed improvement of best corrected visual acuity, intraocular inflammation and resolution of findings on multimodal imaging approach following treatment [Citation6]. Intramuscular (IM) procaine penicillin G 2.4 million units plus probenecid 500 mg four times a day for 10–14 days is recommended as an alternative therapy; if compliance is achieved, treatment outcomes have shown no difference with ACPG in individuals with neurosyphilis [Citation4,Citation7].
The purpose of this study is to describe the outcomes of ocular syphilis treated with ACPG or ambulatory regimens in people living with HIV during the COVID-19 health emergency.
Methods
Design
We conducted an observational retrospective study between March 2020 and May 2023 among people living with HIV and OS who received medical care at Clínica Especializada Condesa Iztapalapa in Mexico City, Mexico. The information was collected from the standard medical records of the patients.
Patient consent statement
The design of this study was approved in accordance with the local standards of Clínica Especializada Condesa Iztapalapa, which is under the oversight of its medical management.
Study population
The study enrolled 53 people living with HIV aged 18 and above who were diagnosed with ocular syphilis. We included individuals with a new diagnosis of HIV infection, readmission due to stopping treatment, and others with regular follow-up. Ocular syphilis was defined as active intraocular inflammation in the presence of a positive Treponemal test (anti-Treponema pallidum antibodies) and a reactive Rapid Plasma Reagin (RPR) test. It is important to mention that all individuals with a new HIV diagnosis or re-entry into care undergo syphilis screening based on the reverse algorithm as standard practice in our center. For individuals with a history of syphilis and post-treatment serological response monitoring, RPR is performed every 6 months.
Collected information
Information from 53 individuals was collected, including age, gender, HIV serological status (CD4+ lymphocyte count and viral load), treatment for HIV infection, RPR/anti-T. pallidum antibodies results, inflammatory ocular findings and/or symptoms at the time of diagnosis, and cerebrospinal fluid (CSF) analysis of those on whom a lumbar puncture was performed. We divided the individuals into two groups, individuals who received treatment with ACPG 24 million units IV daily for 14 days, and individuals with alternative regimes.
Statistical analysis
We provide detailed descriptions of cases of OS, including symptoms, clinical evaluation, outcomes, and other clinically relevant data. All analyses were descriptive, and no hypothesis testing was conducted. Continuous variables were presented as median (IQR), while categorical variables were described as counts and percentages over the entire sample or the corresponding subgroup. No imputation methods were applied to missing data. Data were analyzed using SPSS software (version 27; IBM SPSS Corp., Armonk, NY, USA).
Results
Fifty-three people living with HIV were identified with OS. At the time of diagnosis, 15 (28.3%) had an HIV-1 viral load of <1000 copies/mL, with a median of 189 CD4+ cells/µL (95.2–295.5) and 23 (43.4%) fewer than 200 CD4+ cells/µL). Forty-six individuals (86.7%) had an RPR titer >1:32, and 28 (52.8%) were initially diagnosed in a latent and/or indeterminate duration stage. Thirty-eight (71.6%) individuals in the sample presented ocular symptoms, while 15 (28.3%) were asymptomatic. Twenty-three (43.3%) underwent lumbar puncture, of which 5 (9.4%) individuals had reactive VDRL in CSF. The most common clinical symptoms were decreased visual acuity in 29 (54.7%) cases, myodesopsia in 9 (17%) cases, red eye in 3 (5.7%) cases, and central scotoma in 3 (5.7%) cases. The most common clinical findings during the ophthalmologic examination were vitritis in 38 cases (71.7%), choroiditis in 34 cases (64.2%), vascular sheathing in 31 cases (58.5%), and anterior uveitis in 18 cases (34%).
Forty-seven (88.6%) individuals received treatment (), of which 32 (68%) received standard treatment with ACPG, and 15 (31.9%) were treated with alternative regimens due to the impossibility of hospitalization for the COVID-19 pandemic. Six (11.3%) people were lost to follow-up and/or did not receive treatment. Eighteen (56.3%) out of 32 people in the ACPG group experienced serological response, 5 (15.6%) experienced treatment failure, and 9 (28.1%) were lost to follow-up. In the alternative therapy group, 11 individuals (73.3%) received procaine penicillin plus probenecid; 2 (13.3%) received ceftriaxone, and 2 (13.3%) received procaine penicillin plus doxycycline. Twelve out of 15 individuals (80%) experienced serological responses (). One individual experienced treatment failure, and 2 (13.3%) were lost to follow-up. The person who experienced treatment failure received aqueous IM procaine penicillin plus probenecid.
Figure 1. Outcomes of PLWH with ocular syphilis treated with ACPG vs. alternative treatment. PLWH: people living with HIV; ACPG: aqueous crystalline penicillin.
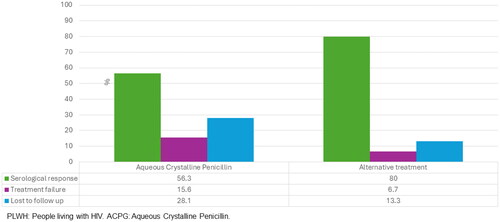
Table 1. Demographic and clinical characteristics of PLWH with ocular syphilis.
Discussion
The COVID-19 pandemic impacted the timely care of other diseases, including STDIs. Similar to other reports that have described the increase in syphilis during and after the pandemic [Citation8,Citation9], in this retrospective study we observed an increase in cases of ocular syphilis in people living with HIV, especially after the first year of confinement due to COVID-19.
The association of untreated HIV infection with a low CD4+ cell count is the most frequent profile of the individuals in our study. This may be due to the fact that they are people with a recent HIV diagnosis or abandonment of antiretroviral therapy (ART) and who do not have regular clinical follow-up, as well as sexually transmitted infections (STIs) screening tests. Unlike other reports where the CD4+ T lymphocyte count is usually close to normal [Citation2,Citation10,Citation11], our population showed a low CD4+ cell count. This may be due to the frequent diagnosis of HIV infection in advanced stages in Mexico. In addition, the COVID-19 pandemic favored the abandonment of ART due to the universal measures of social distancing and lack of care services, and difficulty in HIV and STIs diagnostic tests, causing a delay in new diagnoses. Latent syphilis and elevated RPR titers have been common in people with OS. These findings are confirmed in our sample. It is important to highlight that 30% of people with OS were asymptomatic. At our center, ophthalmologic examination is a standard practice if the RPR titers are ≥1:32, even if the individual is asymptomatic; this was decided for academic purposes. Therefore, we suggest an ophthalmological evaluation in individuals without virological control, low CD4+ counts (<200 CD4+ cells/µL), and RPR titers >1:32.
Currently, the CDC and European Guideline on the management of syphilis recommends, as an alternative treatment regimen for neurosyphilis, OS, and otosyphilis, IM procaine penicillin once daily plus oral probenecid and in the United Kingdom guidelines it is recommended as the first line of treatment. These recommendations are based on data from studies that showed treponemicidal concentrations in cerebrospinal fluid [Citation12–14]. More recently, the combination of IM procaine penicillin plus oral probenecid has shown similar effectiveness to IV ACPG for neurosyphilis, regardless of HIV status [Citation7]. Based on these data and the limitations of hospitalizations due to the COVID-19 pandemic, this alternative treatment was the one that was mainly prescribed to our population. However, there are no clinical trials that have explored the effectiveness of IM procaine penicillin plus oral probenecid specifically for OS. Although the number of people included is low, in our report, we obtained the same effectiveness with IM procaine penicillin vs. IV penicillin G in the serological response.
Some limitations of our study need to be highlighted. This retrospective observational study, involving a small cohort and lacking standardized clinical or laboratory follow-up due to the COVID-19 pandemic, highlights that our centers primarily provide outpatient care without hospitalization facilities. In cases requiring hospitalization, patients are referred to various institutions within our city. It is important to note that there is limited data on HIV history and antiretroviral treatment. It is also important to highlight that not all individuals had a puncture with CSF analysis due to the lack of hospitals available for procedures and care of these people. However, the treatment of choice as well as the alternative for OS and neurosyphilis is the same. Although alternative treatments favored by the health emergency of the pandemic, mainly IM procaine penicillin plus probenecid, showed similar effectiveness to IV ACPG, it is not enough to draw definitive conclusions. Prospective studies are necessary to determine the efficacy of the clinical and serological response with these alternative regimens for the treatment of OS.
Conclusions
The COVID-19 pandemic meant that people living with HIV did not have access to first-line treatment for OS. Alternative treatments, such as IM procaine penicillin plus probenecid, produced favorable outcomes in the setting of limited access to hospitalization. Clinical trials are necessary to explore the effectiveness of alternative treatments for OS and neurosyphilis, even in the setting of limited resources.
Authors contributions
Conceptualization and design of the study: EPB, JCRA, and PRB. Data acquisition: EPB, JCRA, PRB, KGVM, GEGM, BGF, AGR, and RACF. JCRA, EPB, and PRB prepared the article. All authors have read and agreed to the published version of the manuscript.
Acknowledgements
We thank Andrea Gonzalez Rodríguez (Clínicas Especializadas Condesa, Mexico City) for assistance in data sharing agreement administration.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- CDC. Surveillance report 2022 [last reviewed 2024 Jan 30].
- Furtado JM, Arantes TE, Nascimento H, et al. Clinical manifestations and ophthalmic outcomes of ocular syphilis at a time of re-emergence of the systemic infection. Sci Rep. 2018;8(1):12071.
- Liu M, Zhou J, Lan Y, et al. A neglected narrative in the COVID-19 pandemic: epidemiological and clinical impacts of the COVID-19 outbreak on syphilis. Clin Cosmet Investig Dermatol. 2023;16:2485–2496.
- CDC. Sexually transmitted infections treatment guidelines 2021 [last reviewed 2024 Jan 16].
- Bettuzzi T, Jourdes A, Robineau O, et al. Ceftriaxone compared with benzylpenicillin in the treatment of neurosyphilis in France: a retrospective multicentre study. Lancet Infect Dis. 2021;21(10):1441–1447.
- Agostini FA, Queiroz RP, Azevedo DOM, et al. Intravenous ceftriaxone for syphilitic uveitis. Ocul Immunol Inflamm. 2018;26(7):1059–1065.
- Dunaway SB, Maxwell CL, Tantalo LC, et al. Neurosyphilis treatment outcomes after intravenous penicillin G versus intramuscular procaine penicillin plus oral probenecid. Clin Infect Dis. 2020;71(2):267–273.
- Stafford IA, Coselli JO, Wilson DF, et al. Comparison of sexually transmitted infections and adverse perinatal outcomes in underserved pregnant patients before vs during the COVID-19 pandemic in Texas. JAMA Netw Open. 2022;5(2):e220568.
- Stanford KA, Almirol E, Schneider J, et al. Rising syphilis rates during the COVID-19 pandemic. Sex Transm Dis. 2021;48(6):e81–e83.
- Cope AB, Mobley VL, Oliver SE, et al. Ocular syphilis and human immunodeficiency virus coinfection among syphilis patients in North Carolina, 2014–2016. Sex Transm Dis. 2019;46(2):80–85.
- Li JZ, Tucker JD, Lobo AM, et al. Ocular syphilis among HIV-infected individuals. Clin Infect Dis. 2010;51(4):468–471.
- Dunlop EM, Al-Egaily SS, Houang ET. Production of treponemicidal concentration of penicillin in cerebrospinal fluid. Br Med J. 1981;283(6292):646–646.
- Rolfs RT, Joesoef MR, Hendershot EF, et al. A randomized trial of enhanced therapy for early syphilis in patients with and without human immunodeficiency virus infection. The syphilis and HIV study group. N Engl J Med. 1997;337(5):307–314.
- Kingston M, French P, Higgins S, et al. UK national guidelines on the management of syphilis 2015. Int J STD AIDS. 2016;27(6):421–446.
