 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.ABSTRACT
The Global Solar Ultraviolet (UV) Index provides limited information on health effects due to over-exposure. This study investigated the change in skin physiology in response to solar UV irradiation and the protective efficacy of a sunscreen. Fourteen female participants were divided into two groups, sunscreen users and non-users, and for 8 weeks they received solar irradiation and were monitored for change in the erythema-index (E-index), melanin-index, skin capillary blood flow, skin moisture, transepidermal water loss (TEWL), and skin temperature. The E-index and TEWL responded proportionally to solar radiation and could serve as indices of acute health effects from UV exposure. In the sun-radiated area, the E-index and TEWL measured on the forearm of the non-users were 111.3% and 138.4% of the levels determined for the users, respectively. Although thermal sensation and thermo-physiology were correlated, physiological monitoring was preferred over thermal sensation survey in evaluating the impact of solar UV irradiation.
Introduction
The over-exposure to solar ultraviolet (UV) light has been a great concern, as it often results in adverse health effects that human physiological regulations might not readily compensate for. The solar UV irradiation is biologically active because of its short wavelength (100–400 nm) and great quantum energy, and numerous photo-biological processes may occur when the skin is exposed [Citation1,Citation2]. The exposure of the epidermis to UV irradiation might lead to physiological and biochemical changes in the skin, resulting in erythema [Citation3], epidermal proliferation [Citation4], apoptosis [Citation5], hyperpigmentation [Citation6] and immunosuppression [Citation7,Citation8].
Indicating the level of solar UV irradiation at the Earth’s surface, the Global Solar UV Index (UVI) system is the standard vehicle applied in alerting the UV exposure risk [Citation9]. The UVI is a valuable tool for alerting the hazard from solar UV irradiation and nowadays has been widely used to disseminate information on exposure management to the general public thanks to new technologies, such as smartphone apps [Citation10,Citation11] and UV detection stickers [Citation12]. However, the public understanding of the UVI is limited, particularly when it comes to selection of personal protection in accordance with the health effects of over-exposure. As the UVI increased, a strategy commonly applied to prevent exposure was to either reduce the duration of exposure or to use personal protection to decrease the dose of solar UV radiation reaching the skin and/or eyes [Citation13].
The UVI ranges from 0 to 15 or 16. As the index grade rises, the dose rate of the damaging UV radiation increases as well. When an UVI reading increases to 8–10, the exposure is categorized as ‘Very High’, indicating the presence of a very high risk of harm to unprotected skin and eyes from sun exposure [Citation14,Citation15]. The most commonly known acute effect of excessive solar UV exposure on the skin is erythema, the skin reddening termed sunburn [Citation15]. As the dose rate of the UV irradiation manifested in the UVI increases, typically it takes less time for the erythema to develop on the exposed skin under the same exposure scenarios (e.g. the approximate time of the day when the person is exposed, the level of clothing, and the activities the person is engaged in). For example, Sánchez-Pérez et al. [Citation16] studied the relationship between the UVI and the exposure time for the appearance of first-degree sunburn on different skin types on clear sky days and reported an exposure time of 18 and 35 min at an UVI of 10 and 5 (exposure category ‘moderate’), respectively, for the World Health Organization-classified Type II skin (melano-compromised). The time of sun exposure required for the appearance of erythema was further reduced for the Type I skin (the most sensitive type to solar radiation) in the estimation of being close to 10 min at an UVI of 10. The actual duration of the UV irradiation required to induce erythema at each grade was determined by multiple factors, including the elevation of the sun in the sky, the number of clouds, and the exposed individual’s skin conditions. The skin conditions that could influence the effect of exposure included the level of pigmentation, photosensitivity, frequent appearance of moles or freckles, previous history of sunburn, and a personal or family history of skin cancer [Citation17]. In fact, the WHO [Citation15] did not recommend the use of ‘burn times’ in translating the UVI into precautions to take in protecting against the UV exposure, as such use could result in misinterpretation of a safe level of exposure regardless of these factors of uncertainty. In its current form, the UVI did not causally indicate, in semi- or fully quantitative terms, the health effects the skin sustained when the over-exposure occurred. As global climate change continues, this information is essential if health-based strategies for personal management of solar UV exposure are to be developed, e.g. for choosing a specific level of personal protective equipment. A system of hazard identification for solar UV irradiation using skin-based physiological indices is desired.
The insufficient inclusion of health alerts in the UVI has also delayed proper field evaluation of protective mechanisms for their efficacy [Citation15]. In the current UVI system, only general guidance is provided to highlight protective measures that individuals may consider when remaining outdoors for an extended period of time. However, some issues would arise when these measures were applied in areas of warm-and-humid climates, such as in Taiwan. For instance, the usage of sunscreen in these areas might require a modified strategy―the sunscreen was often washed off quickly from the skin after application due to sweating and as a result, frequent re-application had been required.
Of all epidermal disruptions attributable to solar UV irradiation, the most frequently observed was perhaps the provocation of erythema [Citation18], the redness of the skin caused by dilation and then congestion of skin capillary vessels following solar radiation. The provocation of erythema was a direct and quick response of the skin to harmful UV exposure. The skin pigmentation was also a prominent response that appeared after long-term solar UV radiation. Because of the reproducibility and simplicity in their determination, the erythema and pigmentation were frequently applied in characterizing the skin pathophysiology induced by the UV irradiation and other agents [Citation19,Citation20]. In practice, the degrees of erythema and pigmentation were determined spectroscopically and termed the erythema-index (E-index) and melanin-index (M-index), respectively, to demonstrate the significance of skin reaction [Citation21–23]. As quantifiable indices, the E-index and M-index could potentially serve as health-based indicators in the management of solar UV radiation.
However, the development of erythema and pigmentation were not influenced significantly by the thermal status of the ambient environment. As a result, the E-index and M-index might not be appropriate indices to alert the excessive heat gain from solar exposure that interrupted thermal balance in the body. In contrast, the skin-based physiological properties involved in thermoregulation could better alert the heat stress originating from solar irradiation, as ineffective thermoregulation was frequently associated with severe heat-related diseases and disorders, including heat exhaustion and heat stroke [Citation24]. Chen et al. [Citation25] examined the response of skin-based thermo-physiological properties to thermal conditions in the ambient environment and observed distinct changes in the skin capillary blood flow (SCBF), transepidermal water loss (TEWL), skin moisture, and skin temperature in different stages of metabolic heat dissipation. Among these properties, the blood flow in skin capillaries and arteriovenous anastomoses was conventionally applied in diagnosing the changes in skin microcirculation in response to medical conditions [Citation26,Citation27]. In recent years, the change in skin microvasculature was also applied in evaluating the effect of single doses of UV irradiation using artificial lights [Citation28]. The TEWL was determined by quantitatively evaluating the evaporation of water from skin surface, i.e. across the epidermis [Citation29]. The TEWL was routinely employed in the diagnosis of epidermal integrity, as a consistently elevated value of TEWL signified perturbation in skin barrier functions likely due to skin disorders [Citation30] or a thermoregulatory shock prior to thermal imbalance [Citation25]. The skin moisture and skin temperature were frequently employed in studies of thermal stress thanks to their sensitivity to the change in the thermal environment and their potential to suggest heat exposure risk [Citation25,Citation31,Citation32]. When solar UV exposure occurred, the capillary dilation in dermal microcirculation preceded erythema and contributed to observable changes in the SCBF and TEWL. Accordingly, these skin-based thermo-physiological properties might swiftly respond to solar UV irradiation in a dose-dependent manner.
This study investigated the change in skin-based physiological properties in response to solar UV radiation as people went through their daily routines. The results of physiological monitoring were evaluated to determine if these responses might serve as indicators of solar UV-induced health risk. The physiological properties selected for monitoring in this study included the E-index, M-index, SCBF, TEWL, skin moisture, and skin temperature. In the study, a sunscreen available on the market was evaluated to observe its actual performance protecting against solar UV irradiation when used in a hot-and-humid climate. As a final output, thermal sensation of the participants in association with thermo-physiological progress taking place during solar exposure was examined to suggest the availability of conventional thermal survey as an alternative to thermoregulatory evaluation.
Materials and methods
Study design and participants
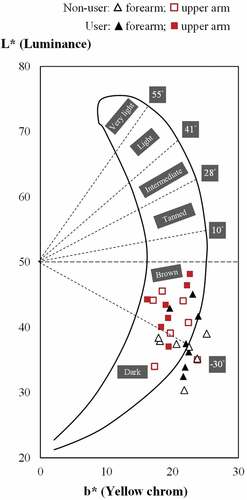
Fourteen females were recruited in this study and divided into two groups, the sunscreen users and the non-users. The age, height, and weight of the seven sunscreen users were 24.3 ± 2.7 years, 159.7 ± 6.2 cm, and 52.4 ± 5.2 kg, respectively, and for the 7 non-users were 21.0 ± 1.3 years, 161.6 ± 5.3 cm, and 51.6 ± 4.3 kg. The constitutive pigmentation of the skin of these participants was determined prior to the study: the individual typology angle (ITA) values [Citation33] based on the colorimetric parameters L* (luminance) and b* (yellow/blue component) as measured on the forearms and the upper arms of the participants ranged between −4.6° and −42.7°. A similar distribution of skin color types was observed between the sunscreen users and the non-users (). Overall, the skin color type for the upper arms of the participants was classified as Brown according to the median ITA (−20.9°) and the color type for the forearms Dark (−31.4°). In general, the skin color types of the participants in this study were darker than those of Caucasian women living in France, the U.S.A. and Russia and those of northeast Asia women living in Shanghai and Guangzhou of China and in Japan [Citation34]. All the participants were required to wear short-sleeved t-shirts and trousers in the field when receiving sunshine and skin monitoring.
Figure 1. Individual typology angle (ITA) values based on the colorimetric parameters L* (luminance) and b* (yellow/blue component) measured on the forearm (black triangle) and the upper arm (red square) of the participants using sunscreen (User; filled) and not using sunscreen (Non-user; blank). The skin color types were classified into six groups, from very light to dark skin, according to ITA values.
The study was conducted according to the guidelines of the Declaration of Helsinki and was approved by the Institutional Review Board, China Medical University College of Public Health, Taichung, Taiwan (98.08.20–2). The experiments conducted in the study complied with the current laws and ethical practices in Taiwan. The participants were briefed on all relevant aspects of the experiments concerning the study purpose, the study design, the anticipated benefits of study, the settings and context in which the study was to be conducted (e.g. the field observations in the sun-radiated area versus in the shadowed area), and the risk potential. Informed consent was obtained and documented from all study participants prior to their participation.
Sunscreen use
In this study, the non-users did not use any sunscreen on their skin. The sunscreen users applied approximately 4 mL on the forearm and upper arm skin 30 min prior to each outdoor monitoring session, covering the skin with sunscreen at a thickness of 2 mg/cm2. The sunscreen used was of a sun protection factor of 30 and a protection grade of UVA (PA) of PA+++. For individuals with brown-to-dark skin, it was recommended [Citation35–37] to use a sunscreen of SPF of at least 30 in addition to seeking shade and wearing sun-protective clothing when staying outdoors to protect from solar UV irradiation. As in the study, the field experiments simulated a short-term exposure scenario (10 min) during the day, the use of sunscreen of an SPF of 30 should be sufficient and was in compliance with the recommendations from agencies and organizations such as the USEPA and the AIM at Melanoma [Citation14,Citation38]. The ingredients with proportions identified in the label of the sunscreen included octocrylene (10.00%), drometrizole trisiloxane (4.00%), butyl methoxydibenzoylmethane (2.50%), ethylhexyl triazone (2.00%), titanium dioxide (0.83%). Additional ingredients included aqua/water, glycerin, alcohol denat, propylene glycol, C12-15 alkyl benzoate, cyclohexasiloxane, cyclopentasiloxane, ethylhexylglycerin, triethanol amine, acrylates/C10-30 alkyl acrylate crosspolymer, dimethiconol, PEG/PPG-18/18 dimethicone, glycine soja/soybean oil, tocopherol, pentasodium ethylenediamine tetramethylene phosphonate, aluminum hydroxide, stearic acid, vitreoscilla ferment, limonene, CI15985/yellow 6, CI16035/red 40, parfum/fragrance. All participants were instructed not to use moisturizers, cosmetics, ointments, or products for skin protection on the skin sites during the course of study so to minimize potential interference.
Monitoring of solar UV light-induced changes in skin physiology and thermal sensation
In this study, the E-index and M-index were dedicated spectroscopic indices of skin reactions to solar UV irradiation, while the SCBF, skin moisture, TEWL, and skin temperature were indicators of thermoregulatory changes that alarmed potential thermal imbalance in the body due to exposure to elevated environmental heat present together with intensive UV radiation. The E-index and M-index were measured using the Cortex® DSM II ColorMeter (Cortex Technology, Hadsund, Denmark). The SCBF was measured using the Moor VMS-LDF tissue blood flow and temperature monitor (Moor Instruments, Devon, UK). The skin moisture, TEWL, and skin temperature were measured using the Cortex® DermaLab System (Cortex Technology, Hadsund, Denmark), with the readings of TEWL and skin temperature being taken by a TEWL probe and those of skin moisture by a flat-head moisture probe. The physiological readings were taken at two skin sites: the outer forearm approximately 10 cm from the wrist and the clothing-covered inner side of the upper arm 15 cm from the elbow. The observations made on the forearm represented the condition of the skin receiving direct solar radiation and those on the upper arm the condition of the un-exposed skin.
The questionnaire surveying thermal sensation in this study was a Chinese interpretation of the version published in the ANSI/ASHARE Standard 55–2020 ‘Thermal Environmental Conditions for Human Occupancy’ originally developed by the American National Standards Institute (ANSI)/the American Society of Heating, Refrigerating and Air-Conditioning Engineers (ASHRAE) [Citation39]. In the questionnaire, the thermal sensation was graded on a 7-point scale, with a thermal sensation vote (TSV) of 3, 2, 1, 0, −1, −2, or −3 corresponding to the sensation of ‘hot’, ‘warm’, ‘slightly warm’, ‘neutral’, ‘slightly cool’, ‘cool’, or ‘cold’, respectively. The ‘neutral’ vote indicated thermal neutrality.
The air temperature, relative humidity, and globe temperature in the ambient environment when solar exposure and skin evaluation took place were monitored using the CENTER 314 Temperature/Humidity Datalogger (Center Technology Corp., Taipei, Taiwan). The air movement was observed using the hot-wired TSI Model 8386 Air Velocity Meter (TSI Incorporated, St. Paul, MN, USA).
Experimental procedures
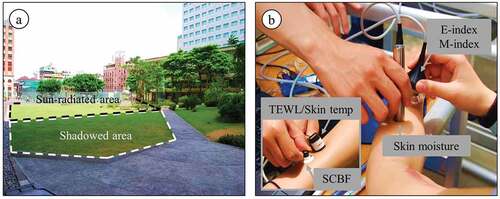
Each participant in this study attended field observation sessions twice a week (Monday and Thursday) for 8 weeks. Individual sessions took place between 10 am and 2 pm on the field day. In each session, the participants first sat for 10 min in an area fully radiated by the sun on the campus of China Medical University (Taichung, Taiwan; )), and at the end of exposure received measurement of skin physiology ()). The participants then moved to a shadowed area about 80 m away from where they were exposed to sunlight. In the shadowed area, the participants remained seated for another 20 min, and were measured for the physiological properties again. At the end of monitoring in the sun-radiated and shadowed zones, the participants were gauged for their thermal sensation towards the ambient environment using the thermal questionnaire. The radiant heat as manifested in the mean radiant temperature in the sun-radiated area was significantly greater than the level in the shadowed area (), with the median globe temperature in the sun-radiated area being 5.5°C higher than its counterpart in the shadowed area (P < 0.001, Mann-Whitney U-test).
Table 1. Distribution of climatic variables in the sun-radiated and shadowed area.
Figure 2. (a) The sun-radiated and shadowed areas where field observations in this study took place in Taichung, Taiwan; (b) measurement of the erythema-index (E-index), melanin-index (M-index), skin capillary blood flow (SCBF), skin moisture, transepidermal water loss (TEWL), and skin temperature on the forearm skin.
Statistical analysis
The data describing the distribution of physiological properties and TSV in response to solar radiation were first partitioned into groups of sunscreen users and non-users and confirmed for non-normality using the Kolmogorov–Smirnov test. Further analysis on the solar UV radiation-related change in skin physiology among the participants in the sun-radiated area vs. in the shadowed area, on the skin of the forearms vs. the upper arms, and between using and not using sunscreen were performed using the non-parametric Mann-Whitney U-test. The Spearman’s rank correlation (rho) was analyzed to investigate the agreement between the change in UVI and those in physiological properties. The same analysis was repeated to examine the correlation between the change in TSV and those in skin physiology, with the data being partitioned by the use of sunscreen (users vs. non-users) and the area of monitoring (sun-radiated vs. shadowed). All statistical analysis was performed using the Statistical Analysis System (SAS) statistical software, version 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
Effects of solar radiation on skin-based thermoregulatory properties
As the results of physiological monitoring show (), the SCBF on both skin sites (the outer forearm and the inner upper arm) of the participants as measured in the sun-radiated area were lower than their counterparts taken in the shadowed area (P < 0.05; Mann-Whitney U-test). The medians of the SCBF measured on the forearm and upper arm when the participants stayed in the sun-radiated area were 21.1 and 27.5 perfusion units (PU), 67.8% and 69.4% of the levels determined in the shadowed area for the forearm (31.1 PU) and for the upper arm (39.6 PU), respectively. In contrast, the TEWL of the participants in direct sunlight were significantly greater than those taken in the shadowed area (P < 0.05). The median TEWL values for the forearm and the upper arm determined in the sun-radiated area were 72.3 and 57.3 g/m2/hr, 324.2% and 286.5% of the levels observed for the forearm (22.3 g/m2/hr) and for the upper arm (20.0 g/m2/hr) in the shadowed area, respectively. The skin moisture and skin temperature measured in the sun-radiated area and in the shadowed areas were not significantly different.
Figure 3. Skin physiology measured on the forearm (left) and the upper arm (right) of the participants using sunscreen (User) and not using sunscreen (Non-user) as determined in the sun-radiated area (white box) and in the shadowed area (shadowed box): (a) skin capillary blood flow (SCBF); (b) skin moisture; (c) transepidermal water loss (TEWL); (d) skin temperature. Values shown in the box plot were the 5th, 25th, 50th, 75th, and 95th percentiles of the distribution. * denotes a significant difference (P < 0.05) between readings taken from users and from non-users.
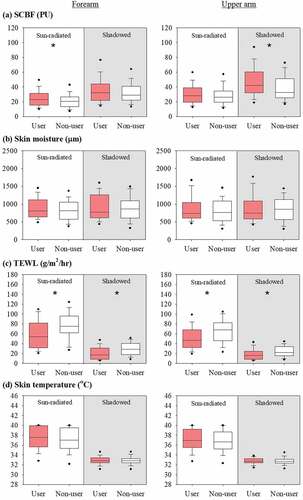
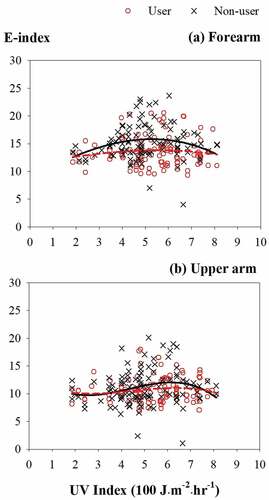
When the participants were in direct sunlight, the SCBF, TEWL, and skin temperature at both skin sites were positively correlated to the intensity of solar UV irradiation (rho = 0.14–0.26; Spearman’s rank correlation). As shows, the TEWL of the participants at both skin sites when not using sunscreen was significantly higher than those of the participants using sunscreen (P < 0.05). In the sun-radiated area, the medians of TEWL measured on the forearm and upper arm of the participants not using sunscreen were 75.3 and 68.1 g/m2/hr, 138.4% and 146.5% of the levels determined on the forearm (54.4 g/m2/hr) and the upper arm (46.5 g/m2/hr), respectively, for the users. The SCBF on the forearm of the users were higher than their counterparts for the non-users (P < 0.05), with the median values on the forearms of the users and non-users being 23.3 and 20.6 PU, respectively. The skin moisture and temperature did not appear to be influenced by the use of sunscreen between these two groups. Furthermore, the SCBF, skin moisture, TEWL and skin temperature taken in the sun-radiated zone from the two skin sites were significantly correlated (rho = 0.33–0.92).
Figure 4. Distribution of the transepidermal water loss (TEWL) measured on (a) the forearm and (b) the upper arm of the participants using sunscreen (User; red circle) and not using sunscreen (Non-user; black cross) by the UV Index as determined in the sun-radiated area. Red dashed line and black solid line represent the cubic regression of the TEWL against the UV Index for users and non-users, respectively.
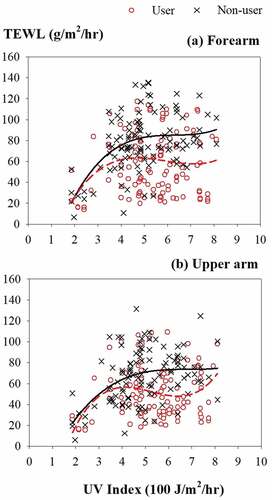
When the participants stayed in the shadowed area, their SCBF, skin moisture, and TEWL were not significantly correlated to the UVI. Similar to the observation made in the sun-radiated zone, the TEWL on the skin of sunscreen users were significantly lower than the levels determined for the non-users (P < 0.05). The medians of the TEWL measured on the forearm and upper arm of the participants not using sunscreen were 28.9 and 22.4 g/m2/hr, 166.1% and 137.3% of the levels for the non-users on the forearm (17.4 g/m2/hr) and the upper arm (16.3 g/m2/hr), respectively. For the SCBF, skin moisture, and skin temperature, the difference between the users and non-users was not statistically significant. The levels of SCBF, skin moisture, TEWL, and skin temperature between the forearm and the upper arm of the participants in the shadowed area were significantly correlated (rho = 0.48–0.92).
Effects of solar UV irradiation on skin spectroscopic indices
As shows, the E-index determined for the forearm skin of the participants when staying in the sun-radiated area were greater than those measured in the shadowed area (P < 0.05; Mann-Whitney U-test), supporting the usage of the E-index as a health-based indicator of solar UV irradiation. The median of the E-index determined on the forearms of the sunscreen users and non-users were 13.3 and 14.8 in the sun-radiated area, 6.4% and 8.0% greater than the levels determined in the shadowed area for the users (12.5) and the non-users (13.7), respectively. The levels of M-index examined on the forearm were of a similar level to those evaluated on the upper arm when they were measured in the sun-radiated area, suggesting that the M-index was not an appropriate candidate for indicating the health impact from short-term, peak exposure of solar UV irradiation. In the sun-radiated zone, the E-index and M-index of the participants were positively correlated to the UVI (rho = 0.13 and 0.20; Spearman’s rank correlation). The use of sunscreen affected the E-index on the forearm skin (P < 0.05)―the E-index on the forearm of the non-users was significantly higher than those of the users (). In the sun-radiated area, the median of the E-index measured on the forearm of the participants not using sunscreen was 14.8, 111.3% of the level determined for the users (13.3). The M-index on both skin sites was also lower when the sunscreen was used, however the difference was not statistically significant. Both the E- and M-index monitored on the forearm and the upper arm were correlated when the readings were taken in the sun-radiated zone (rho = 0.57 and 0.35).
Figure 5. Skin spectroscopic indices measured on the forearm (left) and the upper arm (right) of the participants using sunscreen (User) and not using sunscreen (Non-user) as determined in the sun-radiated area (white box) and in the shadowed area (shadowed box): (a) the erythema-index (E-index); (b) the melanin-index (M-index). Values shown in the box plot were the 5th, 25th, 50th, 75th, and 95th percentiles of the distribution. * denotes a significant difference (P < 0.05) between readings taken from users and from non-users.
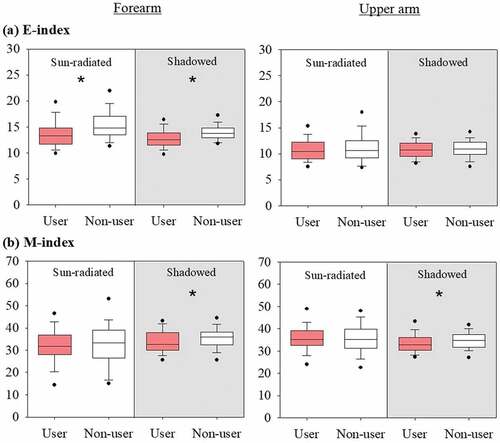
Figure 6. Distribution of the erythema-index (E-index) measured on (a) the forearm and (b) the upper arm of the participants using sunscreen (User; red circle) and not using sunscreen (Non-user; black cross) by the UV Index as determined in the sun-radiated area. Red dashed line and black solid line represent the cubic regression of the E-index against the UV Index for users and non-users, respectively.
Effects of solar UV radiation on thermal sensation
The thermal sensation of the participants toward the ambient environment, as manifested in the TSV, was significantly different between the perceptions surveyed in the sun-radiated area and in the shadowed area (P < 0.05; Mann-Whitney U-test). In the sun-radiated area, the sensation of all participants was primarily warm, with the TSV cast for ‘slightly warm’, ‘warm’, and ‘hot’ in total being 67.6% of the total votes cast. Furthermore, the warm sensation was more significant among the users of sunscreen. In the user group, the aforementioned three grades of TSV accounted for 73% of the overall votes, likely reflecting the reduced dissipation of body heat into the ambient air via evaporative cooling as a result of sunscreen use. In the shadowed area, the thermal sensation was largely of neutrality─for all participants the TSV cast for ‘neutral’ was 58.9%. In addition, in the shadowed area the TSV cast by the sunscreen users for the three grades of warm sensation accounted for 40.5% of all votes, 13.6% greater than its counterpart cast by the non-users. The TSV of all participants were positively correlated with the UVI at the time of field monitoring (rho = 0.20; Spearman’s rank correlation), particularly in the sun-radiated zone (rho = 0.29).
Discussion
In this study, the skin-based non-invasive physiological properties were examined and quantified for their response to solar radiation. The skin injuries clinically manifested as a result of excessive solar irradiation, e.g. tissue inflammation, were not considered, as a major aim here was to evaluate the pertinence of the examined physiological properties to serve as a quantifiable health indicator of solar UV irradiation. These properties reacted to solar UV irradiation either as a result of solar energy absorption (the E- and M-index) or as a part of human thermo-physiological response to release excess body heat gaining from solar irradiance so as to maintain thermal balance (the SCBF, skin moisture and TEWL). This array of properties were attempted as health indicators in this study as their responses to solar UV radiation complemented each other and together described how the co-exposure to solar UV energy and concomitant environmental heat might present a health risk to the exposed individuals.
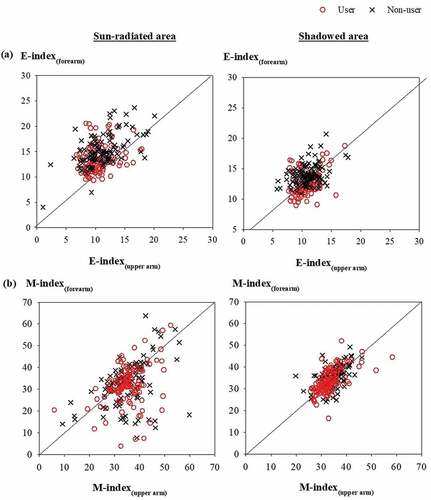
The indices E-index and M-index were included in this study to evaluate the effectiveness of skin spectroscopy as a means of alerting harmful solar UV irradiation. The E-index and M-index were frequently evaluated together when investigating the effect of UV irradiation on the skin, as their changes were typically associated, respectively, with the acute and chronic adverse responses of the skin to solar exposure. For instance, an elevated E-index was commonly evaluated with inflammatory reactions in the epidermal layers as a result of sunburn. The E-index quantitatively describes the alteration in visible light absorption and reflection in the superficial dermis and epidermis as a result of erythematous reaction originating from an increase in hemoglobin and oxyhemoglobin, the two major chromophores for visible light [Citation40]. The quantification of another chromophore, the melanin, in the human skin underlines the determination of the M-index. While the E-index and M-index both reflected color change in specific chromophores, these two indices responded differently to solar UV irradiation. compares the distribution of the E-index and M-index taken on the forearms of the participants to those measured on the upper arms. In the sun-radiated area, for the E-index, 89% of the values on the forearms were greater than their counterparts on the upper arms, suggesting an authentic impact of solar UV radiation in the development of erythema on the directly exposed skin. In contrast, for the M-index approximately 50% of the values measured on the forearms were less than those observed on the upper arms. The symmetrical distribution of the M-index centering on the equivalent line in ) suggests that the M-index was not significantly influenced by the short-term solar UV irradiation. Park et al. [Citation20] examined the time course of skin color changes, as expressed in the E- and M-index, following a single exposure to the UV originating from a fluorescent sunlamp of broad-band UVA and UVB radiation. They reported that the E-index reached the maximum at day 1 and decreased gradually thereafter. In contrast, the M-index increased slowly until day 7 after the exposure. In our study, the M-index did not qualify as an indicator of acute health effect from peak UV exposure probably due to its slow yet prolonged response toward solar UV irradiation.
Figure 7. Distribution of (a) the erythema-index (E-index(forearm)) measured on the forearm by the E-index (E-index(upper arm)) measured on the upper arm and of (b) the melanin-index (M-index(forearm)) on the forearm by the M-index (M-index(upper arm)) on the upper arm for the participants using sunscreen (User; red circle) and not using sunscreen (Non-user; black cross) as determined in the sun-radiated area (left) and in the shadowed area (right).
In comparison, the thermo-physiological properties in this study responded to both the direct impact of solar UV energy and the heat gain from the ambient environment. Among these properties, the TEWL effectively responded to solar exposure and facilitated an evaluation on the efficacy of sunscreen use. In the events of thermoregulation to relieve body heat (Chen et al. [Citation25]), the SCBF first surged in response to the excess heat and increased the capillary flows on the skin surface, preparing the body for heat transfer from the skin to the ambient environment. As an intermediate vehicle of heat release, the fluids in the capillary vessels were then partially released as moisture into the epidermis and next as water vapor into the ambient air, resulting in an increase in the TEWL. Simultaneously, the SCBF was returned to near the baseline. As the heat transfer completed, the skin temperature was returned to the baseline too to allow for a regain of thermal balance. In this study, the relatively lower SCBF and greater TEWL of the participants in the sun-radiated area as compared to the levels determined in the shadowed area attested to the requirement of an advanced thermoregulation via evaporative cooling to release a significant level of heat gain from solar radiation. For the sunscreen users, their skin was burdened with less radiative heat gain, and likely this lessened heat load was sufficiently relieved via blood perfusion in the skin tissues and then via the exchange of convective heat between the body and the environment. As a result, a more prominent change in the SCBF was observed among the sunscreen users than on the non-users. The significantly higher TEWL among the non-users as compared to those of the users also suggested that for the non-users a more vigorous thermoregulatory response to release radiative heat gain was required. However, as the duration of solar exposure in this study was confined to 10 min in each field session, only limited thermal burden from solar exposure was anticipated. A more vigorous thermoregulation with advanced regulation in both the SCBF and TEWL would be expected if the participants endured a longer period of exposure, even when the sunscreen was used. Wolf et al. [Citation28] observed the time courses of change in skin erythema index and cutaneous vascular conductance (CVC) for 8 h after broad-spectrum UVR irradiation on the forearms of adults using or not using SPF 50 sunscreen. The erythema index increased immediately post-irradiation in a linear pattern, but the CVC did not increase above baseline for the first 4–6 h. Both the erythematous development and change in CVC were more significant in the adults not using sunscreen. In our study, the field session for each participant was completed in 30 min, and thus we did not find a change in the SCBF in accordance with the course of change in the CVC that Wolf et al. reported. Evidently, for interpreting the health response to solar irradiation, the SCBF did not serve well as an index, considering the delay in its post-irradiation response.
The development of sunburn and excessive suntan on the skin could be reduced, at least partially, when personal protection was applied. In practice, however, the use of personal protection should be exercised with caution, as in hot-and-humid areas of the globe some protective strategies might not be readily feasible. In these areas, solar UV radiation and environmental heat both contributed to the thermal stress that people experienced when remaining outdoors. Clothing would not serve well as a personal adaptive strategy, as excess outfits would burden the wearers with thermal discomfort [Citation41]. Sunscreens presented a pragmatic solution to the users, as they were convenient to use and allowed for appropriate heat exchange between human body and the thermal environment. To identify the trend in acute erythematous development on the skin following peak exposures to solar irradiation when the sunscreen was used, the increase in the E-index (∆E-index) in each measurement from the level determined in the preceding measurement was compared between the groups using sunscreen and not using sunscreen. For the measurements on the forearm and the upper arm, the ∆E-index were linearly regressed to the use of sunscreen (dummy variable, SS; using sunscreen: 1; not using: 0), the UVI in the current measurement, and the level of the E-index determined in the preceding measurement (E-index(preceding)) to yield:
In EquationEquation (1)(1)
(1) and EquationEquation (2)
(2)
(2) , the positive coefficients for the variable UVI indicated an increase in the E-index as solar UV exposure continued, while the negative ones for the SS demonstrated the efficacy the sunscreen provided to alleviate erythema development. The slowdown in the increase of the E-index when using sunscreen was more prominent in the forearm skin where direct exposure to sunlight occurred―the coefficient for SS on the forearm was 3.43 folds of the value determined on the upper arm. Similar models were not attempted to describe the change in the M-index, as the results of this study did not suggest the M-index for indicating the health effect from short-term UV radiation.
Surveying thermal sensation using questionnaires is an approach commonly practiced to explore intuitive recognition of indoor environmental quality [Citation25,Citation31,Citation42] and of thermal comfort when wearing protective clothing [Citation43]. This technique has been shown to connect thermal perceptions with thermoregulation when the surveyed participants experienced a thermal transient in an indoor space [Citation25]. However, the consistency between thermal perceptions and thermoregulation in an outdoor environment was subject to interferences from presence of meteorological factors and choice of personal adaptive behaviours. In this study, the thermal sensation of the participants toward solar UV radiation corresponded differently to the physiological changes, depending on the stage the change took place in thermoregulation. Overall, the TSV was moderately correlated to the TEWL when the sunscreen was not used and to the skin temperature regardless if the sunscreen was used (). The robust correlation of skin temperature with TSV reflected that the function of skin temperature as thermoreceptors was in sync with the perception of thermal status [Citation25]. The TSV was poorly correlated with SCBF and skin moisture. The SCBF and skin moisture represented, respectively, the initial and intermediate stages of thermoregulatory progress. The levels of body heat released in these stages were less than those in the later stages of heat dissipation, and thus these properties were more amenable to the influence from factors other than those of environmental relevance. These results suggested that cautions should be exercised when translating questionnaire-based survey results into human thermo-physiological responses, particularly when subjective perceptions were considered for application in heat stress evaluation in the ambient environment.
Table 2. Spearman’s rank coefficients of correlation between thermal sensation vote and skin physiology1.
Conclusions
This study investigated the change in skin-based physiological properties in response to solar UV irradiation and the efficacy of sunscreen protecting against harmful UV radiation. Among the observed physiological properties, the E-index and TEWL responded swiftly and proportionally to solar radiation and thus might serve as health-based indices of solar UV exposure and complement the current UVI. The correlation between the TSV and all of the examined skin physiology was statistically significant only when the participants did not use sunscreen, suggesting that physiological monitoring might be preferred over thermal sensation survey for examining impact of solar UV irradiation when the sunscreen was used for protection. Future studies are required to identify physiological properties for indicating chronic health effects from solar UV exposure.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data presented in this study are available from the corresponding author on request.
Additional information
Funding
References
- Dupont E, Gomez J, Bilodeau D. Beyond UV radiation: a skin under challenge. Int J Cosmet Sci. 2013;35(3):224–232.
- Svobodová A, Vostálová J. Solar radiation induced skin damage: review of protective and preventive options. Int J Radiat Biol. 2010;86(12):999–1030.
- Poon TS, Barnetson RS, Halliday GM. Prevention of immunosuppression by sunscreens in humans is unrelated to protection from erythema and dependent on protection from Ultraviolet A in the face of constant Ultraviolet B protection. J Invest Dermatol. 2003;121(1):184–190.
- Kondo S, Kono T, Sauder DN, et al. IL-8 gene expression and production in human keratinocytes and their modulation by UVB. J Invest Dermatol. 1993;101(5):690–694.
- Aufiero BM, Talwar H, Young C, et al. Narrow-band UVB induces apoptosis in human keratinocytes. J Photochem Photobiol B: Biol. 2006;82(2):132–139.
- Stanojević M, Stanojević Z, Jovanović D, et al. Ultraviolet radiation and melanogenesis. Arch Oncol. 2004;12(4):203–205.
- Narbutt J, Lesiak A, Skibinska M, et al. Suppression of contact hypersensitivity after repeated exposures of humans to low doses of solar simulated radiation. Photochem Photobiol Sci. 2005;4(7):517–522.
- Steerenberg PA, Daamen F, Weesendorp E, et al. No adaptation to UV-induced immunosuppression and DNA damage following exposure of mice to chronic UV-exposure. J Photochem Photobiol B:Biol. 2006;84(1):28–37.
- Heckman CJ, Liang K, Riley M. Awareness, understanding, use, and impact of the UV index: a systematic review of over two decades of international research. Prev Med. 2019;123:71–83.
- Dillane D, Balanay JAG. Comparison between EPA UV index app and UV monitor to assess risk for solar ultraviolet radiation exposure in agricultural settings in Eastern North Carolina. J Occup Environ Hyg. 2021;18(1):16–27.
- Nicholson A, Murphy M, Walker H, et al. Not part of my routine: a qualitative study of use and understanding of UV forecast information and the SunSmart app. BMC Public Health. 2019;19(1):1127.
- Horsham C, Ford H, Hacker E. Promoting sunscreen use in adolescents playing outdoor sports using UV detection stickers. Prev Med Rep. 2020;19:101166.
- Lucas RM, Neale RE, Madronich S, et al. Are current guidelines for sun protection optimal for health? Exploring the evidence. Photochem Photobiol Sci. 2018;17(12):1956–1963.
- United States Environmental Protection Agency (EPA): UV index description [Internet]. Washington (DC): EPA; 2021 Nov 16 cited 2022 Aug 29]. Available from 2022 Aug 29: https://www.epa.gov/enviro/uv-index-description.
- World Health Organization (WHO). World Meteorological Organization, United Nations Environment Programme, International Commission on Non-Ionizing Radiation Protection. Global solar UV index: a practical guide. Genève: WHO; 2002.
- Sánchez-Pérez JF, Vicente-Agullo D, Barberá M, et al. Relationship between ultraviolet index (UVI) and first-, second- and third-degree sunburn using the Probit methodology. Sci Rep. 2019;9(1):733.
- Cancer Research UK. The UV index and sunburn risk [Internet]. London (UK): Cancer Reserarch UK; 2021 Jun 2 cited 2022 Aug 29]. Available from 2022 Aug 29: https://www.cancerresearchuk.org/about-cancer/causes-of-cancer/sun-uv-and-cancer/the-uv-index-and-sunburn-risk.
- Waterston K, Naysmith L, Rees JL. Physiological variation in the erythemal response to ultraviolet radiation and photoadaptation. J Invest Dermatol. 2004;123(5):958–964.
- Matias AR, Ferreira M, Costa P, et al. Skin colour, skin redness and melanin biometric measurements: comparison study between Antera® 3D, Mexameter® and Colorimeter®. Skin Res Technol. 2015;21(3):346–362.
- Park SB, Huh CH, Choe YB, et al. Time course of ultraviolet-induced skin reactions evaluated by two different reflectance spectrophotometers: dermaSpectrophotometer and Minolta spectrophotometer CM-2002. Photodermatol Photoimmunol Photomed. 2002;18(1):23–28.
- Huang MW, Lo PY, Cheng KS. Objective assessment of sunburn and minimal erythema doses: comparison of noninvasive in vivo measuring techniques after UVB irradiation. EURASIP J Adv Signal Process. 2010;2010(1):483562.
- Wan M, Hu R, Xie X, et al. Skin erythema, pigmentation and hydration kinetics after ultraviolet radiation-induced photodamage in Southern Chinese women. Photochem Photobiol. 2017;93(5):1276–1281.
- Kim HO, Kim HR, Kim JC, et al. A randomized controlled trial on the effectiveness of epidermal growth factor-containing ointment on the treatment of solar lentigines as adjuvant therapy. Medicina (B Aires). 2021;57(2):166.
- Bouchama A, Knochel JP. Heat stroke. N Engl J Med. 2002;346(25):1978–1988.
- Chen CP, Hwang RL, Chang SY, et al. Effects of temperature steps on human skin physiology and thermal sensation response. Build Environ. 2011;46(11):2387–2397.
- Terada K, Miyai N, Maejima Y, et al. Laser Doppler imaging of skin blood flow for assessing peripheral vascular impairment in hand-arm vibration syndrome. Ind Health. 2007;45(2):309–317.
- Eicke BM, Milke K, Schlereth T, et al. Comparison of continuous wave Doppler ultrasound of the radial artery and laser Doppler flowmetry of the fingertips with sympathetic stimulation. J Neurol. 2004;251(8):958–962.
- Wolf ST, Berry CW, Stanhewicz AE, et al. Sunscreen or simulated sweat minimizes the impact of acute ultraviolet radiation on cutaneous microvascular function in healthy humans. Exp Physiol. 2019;104(7):1136–1146.
- Fluhr JW, Feingold KR, Elias PM. Transepidermal water loss reflects permeability barrier status: validation in human and rodent in vivo and ex vivo models. Exp Dermatol. 2006;15(7):483–492.
- Alexander H, Brown S, Danby S, et al. Research techniques made simple: transepidermal water loss measurement as a research tool. J Invest Dermatol. 2018;138(11):2295–2300.
- Cravello B, Ferri A. Relationships between skin properties and environmental parameters. Skin Res Technol. 2008;14(2):180–186.
- Xiong J, Lian Z, Zhou X, et al. Potential indicators for the effect of temperature steps on human health and thermal comfort. Energy Build. 2016;113:87–98.
- Chardon A, Cretois I, Hourseau C. Skin colour typology and suntanning pathways. Int J Cosmet Sci. 1991;13(4):191–208.
- Bino SD, Bernerd F. Variations in skin colour and the biological consequences of ultraviolet radiation exposure. Br J Dermatol. 2013;169(Suppl 3):33–40.
- Agbai ON, Buster K, Sanchez M, et al. Skin cancer and photoprotection in people of color: a review and recommendations for physicians and the public. J Am Acad Dermatol. 2014;70(4):748–762.
- Passeron T, Lim HW, Goh CL, et al. Photoprotection according to skin phototype and dermatoses: practical recommendations from an expert panel. J Eur Acad Dermatol Venereol. 2021;35(7):1460–1469.
- Tsai J, Chien AL. Photoprotection for skin of color. Am J Clin Dermatol. 2022;23(2):195–205.
- AIM at melanoma: what is ultraviolet radiation? [Internet]. Frisco (TX): AIM at Melanoma; 2022 Jan 19 cited 2022 Aug 29]. Available from 2022 Aug 29: https://www.aimatmelanoma.org/melanoma-101/prevention/what-is-ultraviolet-uv-radiation.
- American National Standards Institute (ANSI); American Society of Heating, Refrigerating and Air-Conditioning Engineers, Inc. (ASHRAE). Thermal Environmental Conditions for Human Occupancy. Atlanta: ANSI/ASHRAE;2020. Standard No. ANSI/ASHRAE 55-2020.
- Pearse AD, Edwards C, Hill S, et al. Portable erythema meter and its application to use in human skin. Int J Cosmet Sci. 1990;12(2):63–70.
- Andersen PA, Buller DB, Walkosz BJ, et al. Environmental variables associated with vacationers’ sun protection at warm weather resorts in North America. Environ Res. 2016;146:200–206.
- Chen CP, Hwang RL, Liu W, et al. The influence of air-conditioning managerial scheme in hybrid-ventilated classrooms on students’ thermal perception. Indoor Built Environ. 2015;24(6):761–770.
- Lin YC, Chen CP. Thermoregulation and thermal sensation in response to wearing tight-fitting respirators and exercising in hot-and-humid indoor environment. Build Environ. 2019;160:106158.
