Abstract
Purpose
The aim of this study was to review the fit and assess the accuracy of tooth-supported single and multi-unit zirconia fixed dental prostheses.
Background
The fit of zirconia restorations has been reported in several studies, but the accuracy of the manufacturing process is seldom discussed or used when drawing conclusions on the fit.
Materials and methods
A literature search of articles published in PubMed between 2 March 2013 and 1 February 2018 was performed using clearly defined inclusion and exclusion criteria. 841 articles were found and 767 were excluded after screening the title and abstract. After full-text analysis another 60 articles were excluded which left 14 articles to be included for data extraction. Fit was the mean of distances reported in the studies and accuracy was the fit minus the pre-set spacer
Results
For marginal gap of single crowns and multi-unit FDPs combined, the fit was 83 μm and the accuracy was 59 μm. The internal gap fit was 111 μm and the accuracy 61 μm. For the total gap, the fit was 101 μm, and the accuracy of the zirconia restorations was 53 μm.
Conclusions
Within the limitations of the present systematic review the fit of zirconia single crowns and multi-unit FDPs may be regarded as clinically acceptable, and the accuracy of the manufacturing of zirconia is ∼60 μm for marginal, internal, and total gap. Also, digital impressions seem to be associated with a smaller gap value.
Keywords:
Introduction
The fit of dental restorations is an important factor for the longevity of tooth-supported dental prostheses. A poor fit can affect the cement junction and result in dissolution, which may result in the loosening of the restoration or secondary caries [Citation1]. Also, crowns with the poor marginal fit on subgingivally placed margins may increase bacterial retention and cause gingival inflammation [Citation2].
There is no consensus on what is regarded as clinically acceptable fit, for marginal fit several authors suggest ∼100 μm [Citation1,Citation3–6]. For internal fit, McLean and von Fraunhofer considered 120 μm clinically acceptable for dental restorations cemented with polycarboxylate cement [Citation1,Citation5]. Even though the internal discrepancies may be well over 200–300 μm most authors conclude that the results from their in vitro fit studies are clinically acceptable when the mean marginal gap is below or close to 120 μm [Citation7–11]. The tooth-crown interface is divided into different areas; marginal, chamfer, axial, and occlusal. There are several areas or distances used to assess the marginal fit of the restoration, it can be measured as the marginal gap, the vertical marginal discrepancy, the horizontal marginal discrepancy, and the absolute marginal discrepancy [Citation12]. The internal fit can be divided into discrepancy at the chamfer or cervical area, axial discrepancy and occlusal discrepancy, or as a mean of all the measuring areas/points [Citation13,Citation14].
The fit of a restoration can be measured using destructive techniques, where the crown or multi-unit fixed dental prosthesis (FDP) is cemented onto dies and embedded with, for example, epoxy resin, sectioned and analyzed microscopically [Citation15,Citation16]. Non-destructive techniques are also used, such as; clinical examination using an explorer, direct view of the crown margin using a microscope or scanning electron microscopy (SEM) [Citation17,Citation18], the silicone or impression replica method [Citation5,Citation19], micro-computed tomography (micro-CT) [Citation20], and optical three-dimensional (3D) scanning [Citation21].
In order to evaluate the accuracy of a restoration, the settings for the marginal and internal spacer must be provided. Otherwise, the measurements only reflect the total deviation from the master model, however, since tooth-supported restorations seldom are manufactured with a 0 µm spacer setting, the results do not represent the accuracy. The results from the fit measurements should, therefore, be regarded as the fit, and the results minus the cement spacer setting, the accuracy.
Zirconia crowns and multi-unit FDPs are predominantly made using computer-aided design-computer aided manufacturing (CAD-CAM). A systematic review on the fit of CAD-CAM restorations of different materials found marginal gaps between 39–201 µm and internal gaps ranging from 23 to 230 µm [Citation22].
Aim
The aim of this study was to review the fit and assess the accuracy of tooth-supported single and multi-unit zirconia fixed dental prostheses.
Material and method
Search strategy
In the present study, the search was performed on 1 February 2018 in PubMed, and limited to English, Swedish, Danish and Norwegian languages published between 2 March 2013 and 1 February 2018. The searches and terms were:
(((FDP [Title/Abstract] OR fixed partial denture [Title/Abstract] OR FPD [Title/Abstract]) OR ((prosthesis [Title/Abstract] OR prostheses [Title/Abstract]) AND ((‘dental health services’ [MeSH Terms] OR (‘dental’ [All Fields] AND ‘health’ [All Fields] AND ‘services’ [All Fields]) OR ‘dental health services’ [All Fields] OR ‘dental’ [All Fields]) OR (‘dentistry’ [MeSH Terms] OR ‘dentistry’ [All Fields])))) OR (crown [Title/Abstract] OR crowns [Title/Abstract] OR bridge [Title/Abstract] OR bridges [Title/Abstract])) AND (zirconia [Title/Abstract] OR zirkonia [Title/Abstract] OR ZRO2 [Title/Abstract] OR Y-TZP [Title/Abstract] OR ‘zirconium dioxide’ [Title/Abstract] OR ‘Yttria stabilized tetragonal zirconia polycrystals’ [Title/Abstract] OR 3Y-TZP [Title/Abstract]) AND (‘2013/02/03’ [PDat]: ‘2018/02/01’ [PDat])
Inclusion criteria
Language (English, Swedish, Danish or Norwegian).
Studies of tooth-supported prostheses.
Fit assessment described.
Measurement techniques described.
Material (Zirconia).
Pre-set cement spacer described.
Chamfer or round shoulder preparations.
Exclusion criteria
Studies not meeting all inclusion criteria.
Studies of implant-supported prostheses.
Studies measuring fit after ceramic veneering.
Studies measuring only the marginal gap.
Studies where internal adjustments were made before a fit assessment.
Selection of studies
The titles were screened and abstracts from the studies found in the search described above, considering the inclusion criteria. After selection, the full texts of the studies were acquired. The full-text publications were screened according to the inclusion and exclusion criteria and 14 studies were included for data analysis ( and ). The data collected from the studies were; Author, Year, in vivo/in vitro, Abutment teeth, Restoration type, Restoration material, Number of specimens per group, Preparation type, Cement spacer at margin, Cement spacer internal, Impression type, Scanner, CAD software, CAM machine, Fit assessment method, Number of measuring points per abutment, Die material, Restoration manufacturing method, Marginal gap, Cervical gap, Axial gap, Occlusal gap, Internal gap and Total gap. In studies where an internal or total gap was not reported but axial and occlusal values were, the internal and total gap values were calculated by the author. In this review, Holmes et al. definition of the marginal gap were used [Citation12]. The internal gap was the mean of all the available internal measuring points (cervical, chamfer, axial, and/or occlusal) and the total gap was the mean of all the measuring points available in the studies (marginal, cervical, chamfer, axial, occlusal).
Figure 1. Search strategy of the systematic review. 841 articles were found and 767 were excluded after screening of title and abstract. After full-text analysis another 60 articles were excluded which left 14 articles to be included.
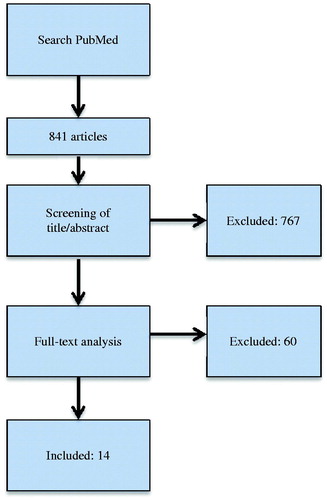
Table 1. Overview of the included studies and their setting parameters and results.
Two of the studies did not use an impression, the master model was scanned using a lab scanner and the restorations placed on the master model. The studies were included but the impression method used in those studies was grouped with the digital impression technique.
Statistical analysis
Descriptive data are presented as numbers and frequencies. Mean values were calculated as weighted values based on the individual group mean value and the number of test specimens per group. The fit was the mean of distances reported in the studies and accuracy was the fit minus the pre-set spacer.
Results
The fourteen studies included in the analysis for this review presented fifteen results for single crowns, seven for three-unit FDPs, seven for four-unit FDPs, and one for six-unit FDPs. Four different fit measuring techniques were used; the silicone replica technique (18 results), the cement and section technique (eight results), the 3D scan technique (Four results), and the Micro-CT technique (Two results) (). The scanners, CAM machines and zirconia materials used are described in .
Table 2. Overview of the intraoral scanners (IOS), laboratory scanners, CAM systems, and zirconia materials used in the included studies.
For the marginal gap of single crowns and multi-unit FDPs combined, the fit was 83 μm and the accuracy was 59 μm. The internal gap fit was 111 μm and the accuracy 61 μm. For the total gap, the fit was 101 μm, and the accuracy of the zirconia restorations was 53 μm (). Eleven of the results were for restorations made from conventional impressions and 19 results were from digital impressions ().
Table 3. Fit and accuracy of the zirconia restorations in μm, for marginal, internal, and total gap.
Table 4. Fit and accuracy of zirconia restorations in μm, for marginal, internal, and total gap according to impression technique.
Discussion
The purpose of this systematic review was to evaluate the fit and assess the accuracy of tooth-supported single and multi-unit zirconia fixed dental prostheses. The fit of the zirconia FDPs was within the range (max 120 μm) most researchers deem clinically acceptable [Citation1,Citation5,Citation7–11]. In an earlier review on the fit of CAD-CAM restorations, published in 2014, the marginal gaps ranged from 39 to 201 µm and the internal gaps from 23 to 230 µm [Citation22]. These results are in accordance with the findings of the present study. In this review, based on studies published between 2013 and 2018, the marginal gaps ranged from 48 to 141 µm and the internal gaps from 59 to 238 µm. An improvement in the fit results could perhaps have been hypothesized due to the developments in CAD-CAM technology. However, this could not be seen in this comparison. It may be since, in the review by Boitelle, other materials such as glass-ceramics and alloys were included which could have affected the results. The choice of restorative material has been shown to influence the marginal fit, in a study by Rödiger et al. with the same settings spacer for all materials, zirconia copings had significantly larger marginal gaps compared to titanium and cobalt-chromium copings [Citation23]. Many of the included studies in this review aimed to compare the fit results of restorations from conventional and digital impressions [Citation9,Citation24–29]. When the results were compared according to the impression technique, the fit and accuracy for all three fit assessment areas were slightly smaller for the digital impression technique. This supports the results from other studies on digital impressions, where single crowns and multi-unit FDPs up to 8-units from digital impressions have shown comparable or lower fit values compared to conventional impressions [Citation30–32].
When comparing the results from different studies one must be aware of the complexity due to the methods and parameters used [Citation33]. In this review, all the restorations were produced using CAM-milling, however, four intraoral scanners and several laboratory scanners were used. Also, nine different milling machines were named in the studies and five studies failed to mention what machine was used. The choice of milling machine may affect the fit of restorations, Kirsch et al. compared five-, and four-axis milling machines and found higher trueness in machines with five-axes [Citation34]. Regarding the zirconia materials used in the studies, eleven different zirconia materials were found and four were not disclosed. For the fit assessment, nine studies used the silicone replica technique, three studies used the cement and sectioning technique, two used the 3D scan technique, and one used the Micro-CT technique. These parameters would be interesting to compare using factor analysis, however, in the present review, there were too few results from each factor to conduct a meaningful analysis. Hence, the results in this review should only be regarded as descriptive. If a stricter inclusion protocol could be used and enough studies would meet the criteria, the before mentioned and other parameters such as; cementation pressure, tooth, preparation type, type of master model and material, could be compared and analyzed.
In the systematic review by Boitelle, only about 50% of the 26 included studies reported the cement spacer settings [Citation22]. In this review only 14 studies were included of the 74 that were originally analyzed in full-text, 25 of the 60 excluded studies did not report the settings. It is important to disclose as much information as possible about the production process and fit assessment technique in the materials section since the settings and parameters may affect the results and conclusions [Citation35]. As an example, it would be a mistake to conclude that a technique or material with a spacer setting of 40 μm and a fit result of 70 μm is more accurate than a technique or material with a spacer setting of 60 μm and a fit result of 80 μm. The first technique is 30 μm from the aimed at spacer setting and the second technique 20 μm. Therefore; the accuracy is higher in technique 20 μm from the setting. In a study by Wettstein et al., the conclusion was that metal-ceramic FDPs had significantly smaller internal gaps compared to zirconia FDPs. However, when taking the spacer into consideration, the only significant difference found was that zirconia FDPs had a significantly smaller occlusal gap [Citation35]. Other studies report the spacer settings but fail to use them when drawing conclusions [Citation36,Citation37].
The majority of the included studies used the silicone replica technique for fit assessment; the advantages of this technique are that it can be used both in vivo and in vitro, and it does not require expensive equipment. The disadvantages are that it is restricted to a two-dimensional analysis of the fit and only the specific points chosen are used. Also, there is a risk of rupture of the light-body material when removing the restoration and it is important to place the restoration and section the replica correctly [Citation6,Citation16]. Nevertheless, the method is considered reliable, although it may overestimate the gap with two to 11% [Citation19,Citation38].
The 3D scan technique can provide a 3D view of the fit, which can be used for both quantitative and qualitative assessments. It can also be used to isolate and measure the fit in specific areas or sections [Citation32,Citation39]. However, it is unclear if studies using the 3D scan technique presents results for the absolute marginal gap or marginal gap [Citation40]. The 3D scan technique may not be the most suitable technique for measuring the absolute marginal gap due to uncertainty in if the outermost edge of the restoration margin is captured with the scanner [Citation41]. Measuring the marginal gap could result in a smaller gap value than represented by the absolute marginal gap, earlier studies on milled CoCr and zirconia have found absolute marginal gaps of 185–260 μm [Citation16,Citation32] and 94–181 μm [Citation42].
The accuracy of zirconia FDPs was ∼60 μm for MG, IntG and TotG. The dental laboratories could perhaps use this information when designing restorations, by changing the spacer settings to improve the fit. However, these results are based on a wide range of different scanners, design software, and CAM machines, all with several parameters that can affect the fit of a restoration. The dental laboratories should do their own tests and measure the accuracy of the restorations they manufacture and adapt the spacer settings accordingly. The easiest method would be the silicone replica technique.
Conclusions
Within the limitations of the present systematic review, the fit of zirconia single crowns and multi-unit FDPs may be regarded as clinically acceptable, and the accuracy of the manufacturing of zirconia is ∼60 μm for marginal, internal, and total gap. Also, digital impressions seem to be associated with a smaller gap value.
Acknowledgements
Torgny Alstad is acknowledged for statistical support and librarians Helen Sjöblom and Carina Torildsson at the Biomedicine Library, University of Gothenburg are acknowledged for great assistance with the literature search.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- McLean JW. Polycarboxylate cements. Five years’ experience in general practice. Br Dent J. 1972;132(1):9–15.
- Felton DA, Kanoy BE, Bayne SC, et al. Effect of in vivo crown margin discrepancies on periodontal health. J Prosthet Dent. 1991;65(3):357–364.
- Fonseca JC, Henriques GE, Sobrinho LC, et al. Stress-relieving and porcelain firing cycle influence on marginal fit of commercially pure titanium and titanium-aluminum-vanadium copings. Dent Mater. 2003;19(7):686–691.
- Han HS, Yang HS, Lim HP, et al. Marginal accuracy and internal fit of machine-milled and cast titanium crowns. J Prosthet Dent. 2011;106(3):191–197.
- McLean JW, von Fraunhofer JA. The estimation of cement film thickness by an in vivo technique. Br Dent J. 1971;131(3):107–111.
- Fransson B, Øilo G, Gjeitanger R. The fit of metal-ceramic crowns, a clinical study. Dent Mater. 1985;1(5):197–199.
- Borba M, Cesar PF, Griggs JA, et al. Adaptation of all-ceramic fixed partial dentures. Dent Mater. 2011;27(11):1119–1126.
- Reich S, Wichmann M, Nkenke E, et al. Clinical fit of all-ceramic three-unit fixed partial dentures, generated with three different CAD/CAM systems. Eur J Oral Sci. 2005;113(2):174–179.
- Keul C, Stawarczyk B, Erdelt KJ, et al. Fit of 4-unit FDPs made of zirconia and CoCr-alloy after chairside and labside digitalization–a laboratory study. Dent Mater. 2014;30(4):400–407.
- Quante K, Ludwig K, Kern M. Marginal and internal fit of metal-ceramic crowns fabricated with a new laser melting technology. Dent Mater. 2008;24(10):1311–1315.
- Huang Z, Zhang L, Zhu J, et al. Clinical marginal and internal fit of metal ceramic crowns fabricated with a selective laser melting technology. J Prosthet Dent. 2015;113(6):623–627.
- Holmes JR, Bayne SC, Holland GA, et al. Considerations in measurement of marginal fit. J Prosthet Dent. 1989;62(4):405–408.
- Colpani JT, Borba M, Della Bona A. Evaluation of marginal and internal fit of ceramic crown copings. Dent Mater. 2013;29(2):174–180.
- Beuer F, Aggstaller H, Richter J, et al. Influence of preparation angle on marginal and internal fit of CAD/CAM-fabricated zirconia crown copings. Quintessence Int. 2009;40(3):243–250.
- Sorensen JA. A standardized method for determination of crown margin fidelity. J Prosthet Dent. 1990;64(1):18–24.
- Örtorp A, Jönsson D, Mouhsen A, et al. The fit of cobalt-chromium three-unit fixed dental prostheses fabricated with four different techniques: a comparative in vitro study. Dent Mater. 2011;27(4):356–363.
- Groten M, Axmann D, Pröbster L, et al. Determination of the minimum number of marginal gap measurements required for practical in vitro testing. J Prosthet Dent. 2000;83(1):40–49.
- Sundar MK, Chikmagalur SB, Pasha F. Marginal fit and microleakage of cast and metal laser sintered copings–an in vitro study. J Prosthodont Res. 2014;58(4):252–258.
- Falk A, von Steyern P, Fransson H, et al. Reliability of the impression replica technique. Int J Prosthodont. 2015;28(2):179–180.
- Nakamura K, Mouhat M, Nergård JM, et al. Effect of cements on fracture resistance of monolithic zirconia crowns. Acta Biomater Odontol Scand. 2016;2(1):12–19.
- Holst S, Karl M, Wichmann M, et al. A new triple-scan protocol for 3D fit assessment of dental restorations. Quintessence Int. 2011;42(8):651–657.
- Boitelle P, Mawussi B, Tapie L, et al. A systematic review of CAD/CAM fit restoration evaluations. J Oral Rehabil. 2014;41(11):853–874.
- Rödiger M, Schneider L, Rinke S. Influence of material selection on the marginal accuracy of CAD/CAM-fabricated metal- and all-ceramic single crown copings. BioMed Res Int. 2018;2018:1–8.
- Cetik S, Bahrami B, Fossoyeux I, et al. Adaptation of zirconia crowns created by conventional versus optical impression: in vitro study. J Adv Prosthodont. 2017;9(3):208–216.
- Kocaağaoğlu H, Kilinç HI, Albayrak H. Effect of digital impressions and production protocols on the adaptation of zirconia copings. J Prosthet Dent. 2017;117(1):102–108.
- Pedroche LO, Bernardes SR, Leão MP, et al. Marginal and internal fit of zirconia copings obtained using different digital scanning methods. Braz Oral Res. 2016;30(1):e113.
- Almeida e Silva JS, Erdelt K, Edelhoff D, et al. Marginal and internal fit of four-unit zirconia fixed dental prostheses based on digital and conventional impression techniques. Clin Oral Invest. 2014;18(2):515–523.
- Ueda K, Beuer F, Stimmelmayr M, et al. Fit of 4-unit FDPs from CoCr and zirconia after conventional and digital impressions. Clin Oral Invest. 2016;20(2):283–289.
- Su TS, Sun J. Comparison of marginal and internal fit of 3-unit ceramic fixed dental prostheses made with either a conventional or digital impression. J Prosthet Dent. 2016;116(3):362–367.
- Haddadi Y, Bahrami G, Isidor F. Accuracy of crowns based on digital intraoral scanning compared to conventional impression-a split-mouth randomised clinical study. Clin Oral Invest. 2019;23(11):4043–4050.
- Nedelcu R, Olsson P, Nyström I, et al. Accuracy and precision of 3 intraoral scanners and accuracy of conventional impressions: a novel in vivo analysis method. J Dent. 2018;69:110–118.
- Svanborg P, Skjerven H, Carlsson P, et al. Marginal and internal fit of cobalt-chromium fixed dental prostheses generated from digital and conventional impressions. Int Dent J. 2014;2014:534382.
- Nawafleh NA, Mack F, Evans J, et al. Accuracy and reliability of methods to measure marginal adaptation of crowns and FDPs: a literature review. J Prosthodont. 2013;22(5):419–428.
- Kirsch C, Ender A, Attin T, et al. Trueness of four different milling procedures used in dental CAD/CAM systems. Clin Oral Invest. 2017;21(2):551–558.
- Wettstein F, Sailer I, Roos M, et al. Clinical study of the internal gaps of zirconia and metal frameworks for fixed partial dentures. Eur J Oral Sci. 2008;116(3):272–279.
- Dahl BE, Rønold HJ, Dahl JE. Internal fit of single crowns produced by CAD-CAM and lost-wax metal casting technique assessed by the triple-scan protocol. J Prosthet Dent. 2017;117(3):400–404.
- Benic GI, Sailer I, Zeltner M, et al. Randomized controlled clinical trial of digital and conventional workflows for the fabrication of zirconia-ceramic fixed partial dentures. Part III: marginal and internal fit. J Prosthet Dent. 2019;121(3):426–431.
- Segerström S, Wiking-Lima de Faria J, Braian M, et al. A validation study of the impression replica technique. J Prosthodont. 2019; 28(2):e609–e616.
- Kuhn K, Ostertag S, Ostertag M, et al. Comparison of an analog and digital quantitative and qualitative analysis for the fit of dental copings. Comput Biol Med. 2015;57:32–41.
- Boitelle P, Tapie L, Mawussi B, et al. Evaluation of the marginal fit of CAD-CAM zirconia copings: comparison of 2D and 3D measurement methods. J Prosthet Dent. 2018;119(1):75–81.
- Svanborg P, Andersson M, Reinedahl T, et al. Comparison of the 3D triple-scan protocol and the impression replica technique for 3-unit tooth-supported fixed dental prostheses. Biomater Investig Dent. 2019;6(1):32–34.
- Kohorst P, Junghanns J, Dittmer MP, et al. Different CAD/CAM-processing routes for zirconia restorations: influence on fitting accuracy. Clin Oral Invest. 2011;15(4):527–536.
- Cunali RS, Saab RC, Correr GM, et al. Marginal and internal adaptation of zirconia crowns: a comparative study of assessment methods. Braz Dent J. 2017;28(4):467–473.
- Miura S, Inagaki R, Kasahara S, et al. Fit of zirconia all-ceramic crowns with different cervical margin designs, before and after porcelain firing and glazing. Dent Mater J. 2014;33(4):484–489.
- Nelson N, K S J, Sunny K. Marginal accuracy and internal fit of dental copings fabricated by modern additive and subtractive digital technologies. Eur J Prosthodont Restor Dent. 2017;25(1):20–25.
- Lee JY, Choi SJ, Kim MS, et al. Effect of span length on the fit of zirconia framework fabricated using CAD/CAM system. J Adv Prosthodont. 2013;5(2):118–125.
- Dahl BE, Dahl JE, Rønold HJ. Internal fit of three-unit fixed dental prostheses produced by computer-aided design/computer-aided manufacturing and the lost-wax metal casting technique assessed using the triple-scan protocol. Eur J Oral Sci. 2018;126(1):66–73.
- Memarian M, Sadighpour L, Nosratpour R, et al. Marginal adaptation and internal fit of posterior 3-unit zirconia FPDs fabricated with different CAD/CAM systems. Eur J Prosthodont Restor Dent. 2017;25(2):79–85.
