Abstract
This research examined whether greening of a geriatric ward may reduce the hospital-induced decline in the independent functioning of elderly patients as measured by changes from admission to discharge in the KATZ-ADL6 and physician assessments at discharge. Using a quasi-experimental design with 4 months of pre- and post-tests, the functional decline in a sample of 54 hospitalized geriatric patients was found to be lower after greening than before greening for both measures. Moreover, an evaluative survey among 15 staff members showed that they appreciated the greening, and believed it to support patient well-being.
Introduction
Functional decline, defined as a deterioration in an individual’s ability to independently and safely perform activities of daily living (ADLs), is a common and serious problem for hospitalized elderly patients. These ADLs include bathing, dressing, using a toilet, transferring out of a bed or chair, continence, and eating without assistance (Katz et al., Citation1963). Functional decline is associated with higher rates of institutionalization, increased mortality, and greater health care expenditure (Hoogerduijn et al., Citation2012; Palese et al., Citation2016). Studies suggest that 30–60% of elderly patients experience functional decline during hospitalization and that this decline is often for reasons unrelated to the patients’ admission diagnoses (Covinsky et al., Citation2003; Rechel et al., Citation2013). Given the worldwide trend of population aging and concurrent increasing demands for elderly healthcare services (Centers for Disease Control Prevention, Citation2003), it is important to learn more about effective ways for alleviating hospital-induced functional decline.
Hospital practices such as device use (IV lines, catheters, cardiac monitors), medical treatments (fMRI scans, lumbar puncture, endoscopies) and low mobilization by excessive bed rest have been implicated as the main causes of functional setbacks during hospital stay (Graf, Citation2006; Panno et al., Citation2000). For many older patients, hospital routines seem to be dangerous rather than protective, resulting in a weakened condition and other iatrogenic disabilities (King, Citation2006; Sourdet et al., Citation2015). The physical environment of hospitals, which is often impersonal, cold, and unfriendly, may, however, also play a role. Indeed, supportive, age-friendly environments can make a significant difference as to how people age and how they respond to disease (World Health Organization, Citation2018). In particular, a physical healthcare environment that incorporates greenery, such as plants and gardens, maybe a key for harnessing the benefits of age-friendly hospital environments (Artmann et al., Citation2017; Ulrich et al., Citation2008).
Much of the previous research on nature-based solutions for healthcare settings has focused on healing gardens and other outdoor natural spaces (Cooper-Marcus & Sachs, Citation2013; Hartig & Marcus, Citation2006; Marcus, Citation2007; Reynolds, Citation2016). This research has indicated many advantages of healing gardens for patients, staff, and visitors, including a reduction of stress, pain, and feelings of depression, enhanced cognitive functioning, increased patient mobility, and higher well-being and satisfaction. Studies among elderly in geriatric care have shown that access to a garden can enhance cognitive functioning (Ottosson & Grahn, Citation2005) and alleviate agitation, ambulation, aggressive behavior and stress levels of patients with Alzheimer’s disease and other forms of dementia (Edwards et al., Citation2013; Ford Murphy et al., Citation2010; Gonzalez & Kirkevold, Citation2014). Furthermore, studies among nursing staff suggest that taking daily work breaks in a hospital garden can reduce stress (Shukor et al., Citation2012), mitigate symptoms of burnout (Cordoza et al., Citation2018), and support well-being and job satisfaction (Naderi & Shin, Citation2008), which in turn may further improve the healthcare experience of patients. A smaller body of evidence suggests that indoor nature-based solutions, such as adding plants and views of real and simulated nature can positively impact patients, staff, and visitors (Beukeboom et al., Citation2012; Dijkstra et al., Citation2008; Raanaas et al., Citation2015). For example, measurements of blood pressure and heart rate of nursing home residents indicated that a view of nature has a calming effect (Tang & Brown, Citation2006). In general, although there is circumstantial evidence for the multiple benefits of nature-based interventions in healthcare settings, there is no direct evidence that greening of a geriatric ward may support a reduction of functional decline in elderly patients.
In the present research, we explored greening of the geriatric ward as a potential way to alleviate functional decline using a quasi-experimental time-series design with pre- and post-tests. In addition, after the greening, a written questionnaire was distributed among staff to gain more insight into their appreciation of the plants and how they evaluate the effects of the plants on their job satisfaction and patient well-being. The staff survey also served as a manipulation check on the success of the green design.
Method
Study location
The study took place at the geriatric ward of a general hospital in the Netherlands. The ward was a nursing ward where elderly patients in need of acute care stay multiple days to undergo observations, examinations, and treatment. The ward was located in an older part of the building complex, which was designed in a classic fashion with patient and staff rooms located along a rectangular hallway, and a reception desk in the middle. The ward included 22 beds in single, double, or 4-person rooms, of which only about 14 were occupied during the research period due to sick calls and lack of personnel. At the start of the study, the ward appeared cluttered and somewhat neglected, with seemingly random decorations hanging on the walls. Staff had done a thoughtful job in creating some nostalgic spaces, where patients and visitors could enjoy historical objects and materials. However, it was clear that the design of the ward had organically developed and that there was no master design plan behind it.
The green intervention
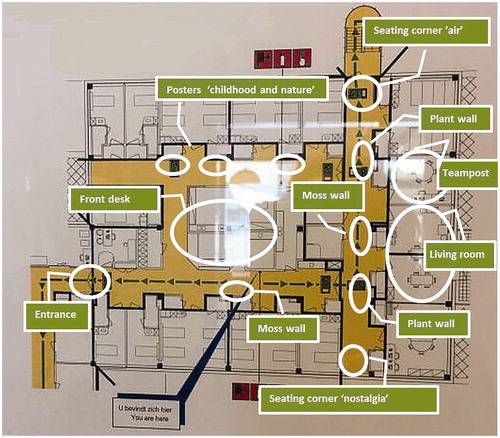
The intervention applied to all publicly accessible areas of the ward, including the main living room, corridors, and seating corners, and to staff areas. Patient rooms were not included in the greening. A detailed plan for greening the designated areas was developed by a landscape architect specialized in the design of healing environments. (Deckers, Citation2018, see for a floor plan). The design plan was informed by the outcomes of a kickoff meeting with hospital staff, a literature study, and the spatial layout and possibilities of the ward. Starting from key dimensions of healing, age-friendly environments like familiarity, security, orientation and elicitation of memories, the design aimed to improve the legibility of the ward, restoration, sensory stimulation, and distraction from disease and death (Chiou & Chen, Citation2009; Huisman et al., Citation2012; Schweitzer et al., Citation2004; Van den Berg, Citation2005).
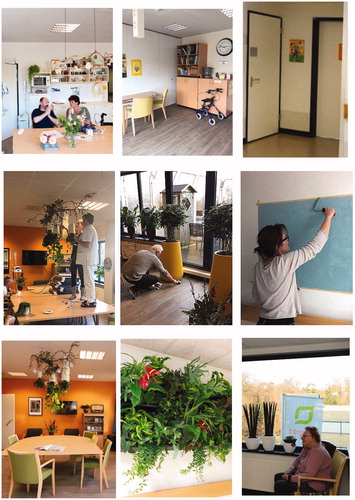
The final design included the placement of two large “green walls” with living plants and two moss walls in the corridors and the addition of small and large potted plants in the living room and reception desk and team post. Plant species included Calathea, Epipremnum, Spathiphyllum, Schefflera, Philodendron, Senecio rowleyanus, and Dracaena. Additionally, the hallways were re-decorated using nature themes, referring to “air” (with blue painted walls and birds’ nests), “childhood” (with pictures and decorations referring to children and nature), and “nostalgia” (with plants in hand-crocheted pots and embroidered paintings). gives an impression of the various areas before, during, and after the greening.
Patient study
Sample
The target study population consisted of all elderly patients (65+) who were admitted to the geriatric nursing ward during the baseline and follow-up periods. The main criterion for inclusion was that the patient would be able to visit the living room and other public areas during her/his stay, independently, or with the help of family or staff. Other inclusion criteria were that the hospital stay of the patient would entirely fall within either the baseline or follow-up period (patients who stayed in the hospital during the greening were excluded) and that the patient’s length of stay in the hospital would be at least 48 hours.
Patients were recruited after they were admitted to the ward, based on observations of their mobility by nursing staff. When a patient was seen to venture outside her or his room, the research coordinator asked the patient and her/his caregivers whether they would be willing to share part of their patient data for participation in a study on “improving the quality of the geriatric ward.” All participating patients and/or their caregiver(s) gave written informed consent after having read a brochure about the research provided by the research coordinator and after having been reassured that their data would be treated anonymously and confidentially and that they would be allowed to withdraw from the study at any moment without having to give any reasons and without consequences.
The enrollment of patients turned out to be slower and more challenging than expected. During the entire research period, the ward was understaffed and not all beds were occupied. Moreover, patients were less mobile than expected due to an ongoing overall deterioration in the elderly hospital patient population. Within the available time-frame of 4 months before and 4 months after greening, we were able to include 28 patients (mean age 83.7 years, 54% female) during baseline, and 26 patients (mean age 83.5 years, 69% female) during follow-up. An a-priori power analysis indicated that 35 patients per group would have been necessary to detect a difference of 1 point in functional decline (measured by difference scores on the KATZ-ADL6) with a standard deviation of 1.5, with α = .05 and a power of 80%. This means that the study was somewhat underpowered.
It was time-wise and logistically not feasible to collect data on the number of patients who were eligible for study enrollment, or the number of eligible patients who declined study enrollment. However, according to the research coordinator, the majority of patients who were eligible and were approached were willing to participate, and even appreciated the possibility to contribute to the study.
Patient outcome measures
The primary outcome measure consisted of The Katz’ Index of Independence in Activities of Daily Living (KATZ-ADL6; Katz et al., Citation1963), which measures the degree of independent functioning in six areas (bathing, dressing, toileting, moving indoors, continence and feeding). Patients receive a score of 0 = yes, 1 = no for their independence in these six areas. A score of 0 means complete independence and a score of 6 strong dependence. Additionally, information on institutionalization (0 = no, 1 = yes) was copied from the patient’s intake and outtake forms. Difference scores between intake and outtake were calculated as an indicator of change in functioning, with higher scores indicating more decline. For the purpose of the present research, the physician in charge also rated patient’s functional decline directly at hospital discharge on a scale ranging from 1 to 5, with 1 = no decline/improvement, 2 = little decline, 3 = moderate decline, 4 = large decline, and 5 = very large decline.
Due to ethics regulations, it was not possible to obtain information on the patients’ medical records including the reason for admission and the treatment received. However, we had access to data on the length of stay (as a proxy of the seriousness of the illness) and admission data including gender, age, ethnicity, delirium score, the use of assistive devices, problems with cognitive functioning in six domains including attention, memory, perception, thinking action, orientation (score 1–6), mood state (0 = happy, neutral or varying, 1 = sad, anxious or panicky), and the reliance on help from caregivers, such as family, nurses or daycare facilities. Additionally, at discharge, the senior nurse, in consultation with practice nurses and activity therapists, estimated the frequency with which the patient was observed to visit the living room and other public areas (on a 4-point scale ranging from 1 = never to 4 = very often).
Staff survey
Sample
The staff survey was targeted at all personnel of the geriatric ward, including doctors, nurses, secretaries, activity therapists, and health assistants who had been working at the ward long enough to evaluate the impact of the greening. At the time of the study, this target population was estimated to comprise about 25 people working full-time or part-time. The survey consisted of a paper-based written questionnaire that was distributed by the senior nurse. Staff who were willing to participate were informed by the senior nurse about the aim of the study and they were assured that their data would be treated anonymously and confidentially. They were also told that by filling in the questionnaire they would provide their consent to participate in the study. Following this procedure, a total of 15 staff members (mean age 41.5 years, 92% female) completed the survey, a response rate of 60%.
Survey questions
The questionnaire followed a format similar to the ones used in previous evaluations of green interventions among various populations and settings (e.g., Beukeboom et al., Citation2012; Van den Berg & Van Duijn, Citation2014). The questions from the previous surveys were adapted for the specific study context, and encompassed five themes:
Appreciation of the plants
In part 1, respondents were first asked whether they appreciate that plants were placed on the ward (yes/no/no opinion). Second, respondents rated their agreement with five statements on possible benefits of the plants relating to the atmosphere, the social climate, stress-reduction, air quality, and esthetics, using a 5-point scale ranging from 1 = totally disagree, to 5 = totally agree. Respondents were also asked to indicate whether they had noticed any other (positive or negative) effects of the plants and if so, to give a description. Finally, respondents indicated whether they wanted the plants to stay (yes/no/no opinion).
Evaluation of the ward
In part 2, respondents were first asked to spontaneously describe the ward before and after greening with a maximum of three words. Second, respondents were asked to select any applicable items from a checklist of 11 possible positive and negative changes in the ward since the greening, such as “less boring,” “more natural,” “messier,” and “less safe.” Third, they were asked to give a grade on a scale of 1–10 to the ward as it appeared before, and after, the greening.
Job satisfaction
Part 3 of the questionnaire assessed the possible impact of the greening on respondents’ job satisfaction as indicated by feelings of burnout and work engagement. Burnout was measured with the exhaustion and cynism scales from the Maslach Burnout Inventory-General Scale (Maslach et al., Citation1986). Work engagement was measured with the vigor and dedication scales from the Work Engagement Scale (Schaufeli et al., Citation2002). Each scale consisted of five items. Sample items are “I feel used up at the end of a working day” (exhaustion), and “I am enthusiastic about my work” (dedication). For the purpose of this study, an adapted response format was used that asked the respondent to indicate for each statement whether it has become more or less applicable since the greening of the ward, using a 5-point scale ranging from 1 = much less applicable, and 5 = much more applicable. The reliabilities (Cronbach’s α) of all scales were good: .98 for exhaustion and cynicism, .95 for vigor, and .97 for dedication.
Patient well-being
In part 4, staff was first asked to grade patient well-being before and after the greening on a scale of 1–10. Second, they assessed the meaning and significance of the greened ward as a place for patient well-being using the 14-item Person-Centred Climate Questionnaire – staff version (Edvardsson et al., Citation2008). Sample items are “A place where patients feel welcome,” and “A place which feels homely even though it is an institution.” Respondents were asked to indicate for each statement whether it has become more or less applicable since the greening of the ward, using a 5-point scale ranging from 1 = much less applicable, and 5 = much more applicable. The reliability of the scale was good, α = .81.
Background characteristics
The questionnaire concluded with questions about respondents’ background characteristics, including, gender, age, profession, contract hours, and length of employment.
Procedure
The hospital participated in this study as part of a larger research program on “Green Healthy Hospitals” supported by the Dutch Topsector Horticulture and Starting Materials. The collection of patient data for baseline measurements started in July 2018 and continued for 4 months. The greening intervention took place during two days beginning of November 2018 and was carried out by the principal researcher together with the landscape architect with the help of technical and medical staff. Small and large potted plants were donated by a collective of plant growing companies, who also arranged the transport of the plant materials to the hospital. The plant and moss walls and other materials were paid from the research budget. Follow-up data collection of patient data started directly after the greening and continued 4 months until the end of March 2019. Data collection for the staff survey took place 3 months after the greening in February/March 2019.
The research was coordinated by the principal researcher who designed the study and prepared the study protocol and materials in collaboration with co-researchers. Patient recruitment and data collection were carried out by a senior administrative nurse, who actively approached mobile patients who were visiting the living room and other public areas and asked them if they were willing to participate in the study. If necessary, the patient’s caregivers were also consulted. After obtaining consent, the senior nurse copied relevant intake data from the digitally stored patient anamnesis form to a printed form supplied by the research team. At discharge, the form was completed with discharge data taken from the patient’s daily hospital status supplemented with observations of the nursing staff and the physician in charge. At the end of the follow-up period, the senior nurse also invited staff to participate in the survey, and if they were willing to participate handed out the questionnaire and asked it to be returned to her personally. The senior nurse took care that all data were stored in a secure and locked place, and handed over to the researchers in a safe manner.
Based on a detailed protocol of the proposed study, the Medical Ethical Committee of VU Medical Center Amsterdam stated that, according to Dutch legislation, the Medical Research Involving Human Subjects Act does not apply to this study (letter d.d.11 July 2018, ref nr. 2018-362). As such, no ethical approval was required.
Data analysis
Statistical analyses were performed using SPSS version 26. Patient data were screened for differences in the composition of baseline and follow-up groups using one-way ANOVAs. Effects of the green intervention on changes in the KATZ-ADL6 scores were tested using MANOVA repeated measures analysis with time (intake, outtake) as within-subjects factor and condition (before, after) as a between-subjects factor, with a number of cognitive problems at intake as a covariate. The effects of the green intervention on outtake scores were analyzed with covariate-adjusted one-way ANOVA and crosstabs. Responses to the staff survey were analyzed using descriptive statistics and frequency distributions.
Results
Patient study
Sample characteristics
As shown in , all patients enrolled in the study were natively Dutch, varying in age between 68 and 97 years. The length of hospital stay varied between 2 and 34 days, and the large majority relied on assistive devices and caregivers. The follow-up group had a higher score on the KATZ-ADL6 and more cognitive problems at intake than the baseline group, and they also somewhat more often relied on assistive devices. According to staff observations, the majority of patients visited the living room often or very often. There were no differences between the two groups in the perceived frequency of visits to the living room and other public areas, indicating that the greening did not stimulate patients to become more active and visit these areas more often.
Table 1. Characteristics of patient groups at baseline (before greening) and follow-up (after greening).
Preliminary analyses indicated cognitive functioning as a relevant covariate, with more cognitive problems at intake associated with more functional decline. Analyses of the effects of greening on the functional decline were therefore conducted with and without cognitive functioning as a covariate.
Functional decline
Patients generally showed a less functional decline after the greening than before the greening, as indicated by intake–outtake scores on the KATZ-ADL6 as well as by physician assessments at outtake. As shown in , during baseline patients on average showed a slight decline in independent functioning on the KATZ-ADL6 scale, while during follow-up, they showed a slight improvement in independent functioning. This difference, as indicated by a Time × Condition interaction, was significant without adjustment for covariates, F(1, 52) = 4.12, p = .048, ηp2 = .07, as well as after adjustment for cognitive problems at intake, F(1, 51) = 5.61, p = .022, ηp2 = .10. As illustrated in , before greening 32.1% of the patients showed a functional decline according to the KATZ-ADL6, while after greening only 11.5% showed a functional decline.
Figure 3. Percentages of patients before and after greening with different levels of functional decline according to the KATZ-ADL intake–outtake scores and according to the physician at outtake.
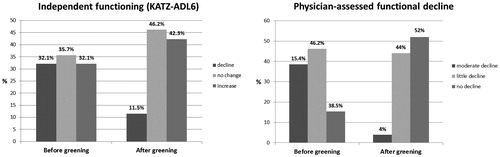
Table 2. Unadjusted means with standard deviations, means adjusted for cognitive problems at intake, and percentages for patient measures of functional decline, with p-values for the effect of greening.
Crosstabs analyses for each of the six activities of the KATZ-ADL6 separately showed that the largest reduction in functional decline was found for being able to transfer out of bed or a chair (24.1% decline before greening, 0% after greening) and independent bathing (10.7% decline before greening, 0% after greening).
Physician-assessed functional decline changed from low-to-moderate during baseline, to no-to-low during follow-up. This difference between the groups was significant without adjustment for covariates, F(1, 49) = 18.86, p < .001, ηp2 = .28, and after adjustment for cognitive problems at intake, F(1, 48) = 32.13 p < .001, ηp2 = .40. As illustrated in , before greening 84.7% of the patients showed a little or moderate decline during their hospital stay according to the physician, while after greening only 48% showed a functional decline.
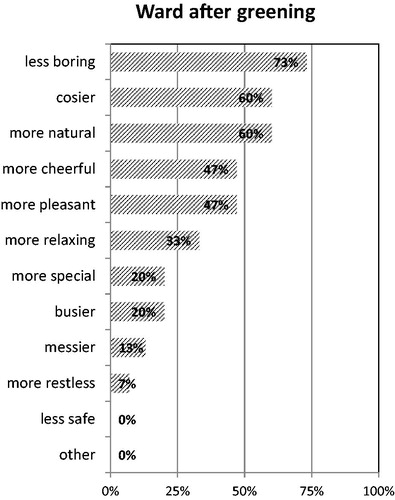
Figure 4. List of terms to describe the ward after greening in the order of the frequency with which they were selected by respondents from a checklist of 11 items (staff survey).
At follow-up, 17.9% fewer patients went from independent living to institutionalization than during baseline, but this difference did not reach significance.
Staff survey
Appreciation of the plants
Staff members appreciated the plants being placed on the ward, and all but two respondents indicated they would like the plants to stay (with the remaining two respondents selecting “no opinion”). As shown in , the staff generally agreed with the statements about the positive effects of the plants. They agreed most with the statement that the plants made the ward more esthetically attractive, and a large majority agreed with the statements that the plants improved the social climate at the ward and supported stress-reduction. The overall impact of the plants on the general atmosphere was also judged positively. There was less support, however, for the statement that the plants improved air quality; most respondents rated the effects on air quality as neutral, and some even rated it as negative.
Table 3. Means (minimum, maximum) for outcome variables used in the staff survey, with percentages of respondents giving an answer that indicates an improvement (↑), no change (–) or a deterioration (↓) due to the greening.
Eight staff members responded to the question of whether they had noticed any additional effects of the plants. Five of the comments were positive, saying that “everybody gets positive,” “it provides a topic for conversation,” “most people passing by like the plants,” “personnel from other wards are interested,” and “visitors and patients like it.” Three comments were negative, two of them referring to the hassle related to the maintenance of the plants, and one about the plants making the ward look darker.
Evaluation of the ward
When asked to describe the ward as it appeared before greening in three words, respondents only used negative or neutral words like “boring” (mentioned 8 times), “empty” (mentioned 8 times), and “messy” (mentioned 5 times). The ward as it appeared after greening was predominantly described in positive words like “cosy” (mentioned 7 times), “tidied” (mentioned 5 times) and a variety of other terms including “friendly,” “lively,” “open,” “natural,” and “colorful.” Three respondents described the ward after greening as “busy” and “full.”
Respondents selected mostly positive terms from a list of 11 positive and negative terms to describe the ward after greening. As shown in , “less boring” was the most chosen term, followed by “cosier,” “more natural,” “more cheerful,” and “more pleasant.” The most chosen negative terms were “messier” and “busier.”
Respondents on average gave a score of 6.1 on a scale of 1-10 to the ward as it looked like before greening, while they scored the ward as it looked like after greening an 8.0, a significant difference, F(1, 13) = 101.01, p < .001, ηp2 = 0.89. All respondents gave the ward after greening, compared to as it looked like before greening, a higher score, with a minimum increase of 1 and a maximum increase of 3.
Job satisfaction
As shown in , staff generally did not notice any change in their job satisfaction since the greening of the ward. Only two respondents reported some improvement (i.e., reduction) in burnout complaints, and only four respondents reported some improvement in work engagement. None of the respondents reported a deterioration in job satisfaction.
Patient well-being
Respondents on average gave a score of 6.8 on a scale of 1-10 for patient well-being before greening, and a 7.6 after greening, a significant difference, F(1,13) = 18.47, p < .001, ηp2 = 0.61. Three respondents did not notice a difference in patient well-being, the remaining respondents gave higher scores to patient well-being after greening, with a maximum increase of 2.
As shown in , the average score on the Person-Centred Climate Questionnaire was well above the midpoint of the scale, indicating an improvement in the extent to which the wards support patient well-being after greening. Only two respondents reported no improvement, and none of the respondents reported a deterioration in the ward climate.
Discussion
We evaluated the effects of greening a geriatric ward on patients and staff. After greening, the functional decline in elderly patients as measured by intake–outtake scores of independent functioning and as judged by the physician at discharge was substantially reduced. There also was a substantial but non-significant reduction in the number of patients going from independent to institutionalized living. The intervention was positively evaluated by staff members. They generally agreed with statements about the positive effects of plants and described and rated the ward as it appeared after greening more positively than as it appeared before. Staff also thought that the greening had made the ward more supportive of patient well-being. They did, however, not notice any positive effects on their own job satisfaction. A few staff members made negative comments regarding the hassle with the maintenance of the plants, and about plants making the ward darker, busier, and messier. These findings strengthen the evidence base for the benefits of interior plants (Bringslimark et al., Citation2009; Van den Berg & Van den Berg, Citation2015) and extend current knowledge by examining a reduction in functional decline as a thus far unidentified benefit of greening.
The positive effects of the greening on patients’ functional decline are in line with previous studies showing that contact with plants and visits to nature provides multiple benefits for elderly populations (Kabisch et al., Citation2017). These studies suggest that in later stages of life when an individual’s social network becomes smaller nature becomes more important as a means to connect with other living beings (Thauvoye et al., Citation2018). Childhood memories of nature experiences also become more salient and treasured during old age and have been found to be an important precondition for older people to reap the cognitive benefits of living near green space (Cherrie et al., Citation2018). In addition, the elderly also profit from the mood-improving and stress-reducing effects of plants as they have been found across age groups (Hartig et al., Citation2014). Nevertheless, although there is evidence from previous research to build a case for positive effects of greening a geriatric ward on functional decline, the details of the pathways involved remain unknown, and cannot be answered on the base of the present study.
The finding that greening positively influenced staff descriptions and evaluations of the ward is consistent with previous research on the benefits of plants in the workplace (Evensen et al., Citation2015; Kaplan, Citation1993; Shibata & Suzuki, Citation2004; Shin, Citation2007). Most of this research has, however, focused on offices instead of hospitals. An important difference between office workers and hospital staff is that the latter has a broad perspective on job satisfaction in which not only their own well-being but also that of the patients plays an important role. Indeed, hospital staff may even be more concerned with patient well-being than with their own well-being. From this perspective, it is interesting that staff showed awareness of the benefits of the plants for the well-being of patients, but generally did not notice any effect on their own functioning.
Limitations and suggestions for future research
A general limitation is the small sample size for both the patient and staff study. Nevertheless, although the patient study was underpowered, we were able to detect significant changes in the primary outcome variables. A major limitation of the patient study is that patients were not randomly assigned to intervention and control conditions. It is therefore not possible to draw causal conclusions on the effects of the greening on patients’ functional decline. Alternative explanations for the findings cannot be excluded, including potential nonequivalence of groups at baseline and follow-up (i.e., on variables not assessed, such as the seriousness of illness). There were no differences between the samples at baseline and follow-up in the length of stay as a proxy of the seriousness of the illness. However, length of stay may also be influenced by factors such as the availability of places in nursing homes, and it cannot be ruled out that the samples were nonequivalent in terms of the seriousness of the illness. Another potentially confounding factor relates to the occurrence of events and changes in hospital practices that reduced functional decline and that are unrelated to the intervention. However, the major factors (like medical procedures) that influence functional decline are structural in nature and there were no indications of changes in these factors during the study period.
Another limitation of the patient study concerns the fact that hospital staff who were responsible for data collection and assessed functional decline were not blind to the intervention, which may have posed a threat to internal and external validity by introducing selection bias. The recruitment procedure did not include the registration of data on the total number of eligible patients and the number of eligible patients who declined, which further hampers critical appraisal of the validity of the study. Furthermore, the greening intervention was combined with a “clean-up” of the ward, which makes it difficult to disentangle any effects of the plants and natural materials from the general effects of the cleaning and tidying. The intervention also mostly formed a decorative intervention that did not invite the patients or staff to interact with the plants. This may have limited patients and staff in their ability to form an emotional bond with nature.
Responses of staff showed much consensus and were therefore easy to interpret. A limitation of the staff survey is that it relied on staff’s own impressions of the effects of the greening, instead of assessing a change over time with pre- and post-measurements
To examine prolonged change regarding the benefits of ward greening for patients and staff, future studies with larger samples and longer follow up periods should be conducted. Random assignment of patients to intervention and control wards is also recommended, as well as the use of more objective measures of staff functioning, such as sick leave records. To gain more insight into the relative effects of greening, control conditions with other interventions like, for example, artwork or the creation of a nostalgic environment might be included. By including the benefits of green in staff educational programs, or by using designs that include greening of patient rooms and invite sensory interaction with the plants, the potential benefits of plants may be more fully realized.
Conclusion
Greening provides an unobtrusive and low-cost solution for enhancing the physical environment of a geriatric ward. This research is the first to suggest that greening can reduce functional decline and make the ward a more attractive place for patients and staff. These are important findings given the world-wide trends of population aging and increasing demands of elderly on healthcare services.
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Artmann, M., Chen, X., Iojă, C., Hof, A., Onose, D., Poniży, L., Lamovšek, A. Z., & Breuste, J. (2017). The role of urban green spaces in care facilities for elderly people across European cities. Urban Forestry & Urban Greening, 27, 203–213. https://doi.org/10.1016/j.ufug.2017.08.007
- Beukeboom, C. J., Langeveld, D., & Tanja-Dijkstra, K. (2012). Stress-reducing effects of real and artificial nature in a hospital waiting room. The Journal of Alternative and Complementary Medicine, 18(4), 329–333. https://doi.org/10.1089/acm.2011.0488
- Bringslimark, T., Hartig, T., & Patil, G. G. (2009). The psychological benefits of indoor plants: A critical review of the experimental literature. Journal of Environmental Psychology, 29(4), 422–433. https://doi.org/10.1016/j.jenvp.2009.05.001
- Centers for Disease Control Prevention. (2003). Trends in aging–United States and worldwide. Morbidity and Mortality Weekly Report, 52(6), 101.
- Cherrie, M. P. C., Shortt, N. K., Mitchell, R. J., Taylor, A. M., Redmond, P., Thompson, C. W., Starr, J. M., Deary, I. J., & Pearce, J. R. (2018). Green space and cognitive ageing: A retrospective life course analysis in the Lothian Birth Cohort 1936. Social Science & Medicine, 196, 56–65. https://doi.org/10.1016/j.socscimed.2017.10.038
- Chiou, S.-T., & Chen, L.-K. (2009). Towards age-friendly hospitals and health services. Archives of Gerontology and Geriatrics, 49, S3–S6. https://doi.org/https://doi.org/10.1016/S0167-4943(09)70004-4 https://doi.org/10.1016/S0167-4943(09)70004-4
- Cooper-Marcus, C., & Sachs, N. A. (2013). Therapeutic landscapes: An evidence-based approach to designing healing gardens and restorative outdoor spaces. John Wiley & Sons.
- Cordoza, M., Ulrich, R. S., Manulik, B. J., Gardiner, S. K., Fitzpatrick, P. S., Hazen, T. M., Mirka, A., & Perkins, R. S. (2018). Impact of nurses taking daily work breaks in a hospital garden on burnout. American Journal of Critical Care, 27(6), 508–512. https://doi.org/10.4037/ajcc2018131
- Covinsky, K. E., Palmer, R. M., Fortinsky, R. H., Counsell, S. R., Stewart, A. L., Kresevic, D., Burant, C. J., & Landefeld, C. S. (2003). Loss of independence in activities of daily living in older adults hospitalized with medical illnesses: Increased vulnerability with age. Journal of the American Geriatrics Society, 51(4), 451–458. https://doi.org/10.1046/j.1532-5415.2003.51152.x
- Deckers, F. (2018). Vergroenen afdeling geriatrie ziekenhuis Tergooi Blaricum [greening of a geriatric ward at Hospital Tergooi in Blaricum], from http://fhreja.nl/?portfolio=tergooi-ziekenhuis-blaricum
- Dijkstra, K., Pieterse, M. E., & Pruyn, A. (2008). Stress-reducing effects of indoor plants in the built healthcare environment: The mediating role of perceived attractiveness. Preventive Medicine, 47(3), 279–283. https://doi.org/10.1016/j.ypmed.2008.01.013
- Edvardsson, D., Sandman, P. O., & Rasmussen, B. (2008). Swedish language Person‐centred Climate Questionnaire–patient version: Construction and psychometric evaluation. Journal of Advanced Nursing, 63(3), 302–309. https://doi.org/10.1111/j.1365-2648.2008.04709.x
- Edwards, C. A., McDonnell, C., & Merl, H. (2013). An evaluation of a therapeutic garden’s influence on the quality of life of aged care residents with dementia. Dementia, 12(4), 494–510. https://doi.org/10.1177/1471301211435188
- Evensen, K. H., Raanaas, R. K., Hagerhall, C. M., Johansson, M., & Patil, G. G. (2015). Restorative elements at the computer workstation: A comparison of live plants and inanimate objects with and without window view. Environment and Behavior, 47(3), 288–303. https://doi.org/10.1177/0013916513499584
- Ford Murphy, P., Miyazaki, Y., Detweiler, M. B., & Kim, K. Y. (2010). Longitudinal analysis of differential effects on agitation of a therapeutic wander garden for dementia patients based on ambulation ability. Dementia, 9(3), 355–373. https://doi.org/10.1177/1471301210375336
- Gonzalez, M. T., & Kirkevold, M. (2014). Benefits of sensory garden and horticultural activities in dementia care: A modified scoping review. Journal of Clinical Nursing, 23(19–20), 2698–2715. https://doi.org/10.1111/jocn.12388
- Graf, C. (2006). Functional decline in hospitalized older adults: It’s often a consequence of hospitalization, but it doesn’t have to be. The American Journal of Nursing, 106(1), 58–67. https://doi.org/10.1097/00000446-200601000-00032
- Hartig, T., & Marcus, C. C. (2006). Essay: Healing gardens—places for nature in health care. The Lancet, 368, S36–S37. https://doi.org/10.1016/S0140-6736(06)69920-0
- Hartig, T., Mitchell, R., de Vries, S., & Frumkin, H. (2014). Nature and Health. Annual Review of Public Health, 35, 207–228. https://doi.org/10.1146/annurev-publhealth-032013-182443
- Hoogerduijn, J. G., Buurman, B. M., Korevaar, J. C., Grobbee, D. E., de Rooij, S. E., & Schuurmans, M. J. (2012). The prediction of functional decline in older hospitalised patients. Age and Ageing, 41(3), 381–387. https://doi.org/10.1093/ageing/afs015
- Huisman, E. R. C. M., Morales, E., van Hoof, J., & Kort, H. S. M. (2012). Healing environment: A review of the impact of physical environmental factors on users. Building and Environment, 58, 70–80. https://doi.org/10.1016/j.buildenv.2012.06.016
- Kabisch, N., van den Bosch, M., & Lafortezza, R. (2017). The health benefits of nature-based solutions to urbanization challenges for children and the elderly - A systematic review. Environmental Research, 159, 362–373. https://doi.org/10.1016/j.envres.2017.08.004
- Kaplan, R. (1993). The role of nature in the context of the workplace. Landscape and Urban Planning, 26(1–4), 193–201. https://doi.org/10.1016/0169-2046(93)90016-7
- Katz, S., Ford, A., Moskowitz, R., Jackson, B., & Jaffe, M. (1963). Studies of illness in the aged. The index of ADL: A standardized measure of biological and psychosocial function. JAMA, 185(12), 914–919. https://doi.org/10.1001/jama.1963.03060120024016
- King, B. D. (2006). Functional decline in hospitalized elders. Medsurg Nursing: Official Journal of the Academy of Medical-Surgical Nurses, 15(5), 265–271.
- Marcus, C. C. (2007). Healing gardens in hospitals. Interdisciplinary Design and Research e-Journal, 1(1), 1–27.
- Maslach, C., Jackson, S. E., Leiter, M. P., Schaufeli, W. B., & Schwab, R. L. (1986). Maslach burnout inventory (Vol. 21). Consulting Psychologists Press.
- Naderi, J. R., & Shin, W.-H. (2008). Humane design for hospital landscapes: A case study in landscape architecture of a healing garden for nurses. HERD, 2(1), 82–119. https://doi.org/10.1177/193758670800200112
- Ottosson, J., & Grahn, P. (2005). A comparison of leisure time spent in a garden with leisure time spent indoors: On measures of restoration in residents in geriatric care. Landscape Research, 30(1), 23–55. https://doi.org/10.1080/0142639042000324758
- Palese, A., Gonella, S., Moreale, R., Guarnier, A., Barelli, P., Zambiasi, P., Allegrini, E., Bazoli, L., Casson, P., Marin, M., Padovan, M., Picogna, M., Taddia, P., Salmaso, D., Chiari, P., Frison, T., Marognolli, O., Benaglio, C., Canzan, F. … Saiani, L. (2016). Hospital-acquired functional decline in older patients cared for in acute medical wards and predictors: Findings from a multicentre longitudinal study. Geriatric Nursing, 37(3), 192–199. https://doi.org/10.1016/j.gerinurse.2016.01.001
- Panno, J. M., Kolcaba, K., Holder, C., & Hunt, A. H. (2000). Acute Care for Elders (ACE): A holistic model for geriatric orthopaedic nursing care. Orthopaedic Nursing, 19(6), 53.
- Raanaas, R. K., Patil, G., & Alve, G. (2015). Patients’ recovery experiences of indoor plants and viewsof nature in a rehabilitation center. Work, 53(1), 45–55. https://doi.org/10.3233/WOR-152214
- Rechel, B., Grundy, E., Robine, J.-M., Cylus, J., Mackenbach, J. P., Knai, C., & McKee, M. (2013). Ageing in the European Union. The Lancet, 381(9874), 1312–1322. https://doi.org/10.1016/S0140-6736(12)62087-X
- Reynolds, L. (2016). A valued relationship with nature and its influence on the use of gardens by older adults living in residential care. Journal of Housing for the Elderly, 30(3), 295–311. https://doi.org/10.1080/02763893.2016.1198740
- Schaufeli, W. B., Martinez, I. M., Pinto, A. M., Salanova, M., & Bakker, A. B. (2002). Burnout and engagement in university students: A cross-national study. Journal of Cross-Cultural Psychology, 33(5), 464–481. https://doi.org/10.1177/0022022102033005003
- Schweitzer, M., Gilpin, L., & Frampton, S. (2004). Healing spaces: Elements of environmental design that make an impact on health. The Journal of Alternative and Complementary Medicine, 10(1), 71–83. https://doi.org/10.1089/1075553042245953
- Shibata, S., & Suzuki, N. (2004). Effects of an indoor plant on creative task performance and mood. Scandinavian Journal of Psychology, 45(5), 373–381. https://doi.org/10.1111/j.1467-9450.2004.00419.x
- Shin, W. S. (2007). The influence of forest view through a window on job satisfaction and job stress. Scandinavian Journal of Forest Research, 22(3), 248–253. https://doi.org/10.1080/02827580701262733
- Shukor, S. F. A., Stigsdotter, U. K., Lottrup, L., & Nilsson, K. (2012). Employees’ use, preferences, and restorative benefits of green outdoor environments at hospitals. Alam Cipta, 5(2), 77–92.
- Sourdet, S., Lafont, C., Rolland, Y., Nourhashemi, F., Andrieu, S., & Vellas, B. (2015). Preventable iatrogenic disability in elderly patients during hospitalization. Journal of the American Medical Directors Association, 16(8), 674–681. https://doi.org/10.1016/j.jamda.2015.03.011
- Tang, J. W. S., & Brown, R. D. (2006). The effect of viewing a landscape on physiological health of elderly women. Journal of Housing for the Elderly, 19(3–4), 187–204. https://doi.org/10.1300/J081v19n03_10
- Thauvoye, E., Vanhooren, S., Vandenhoeck, A., & Dezutter, J. (2018). Spirituality and well-being in old age: Exploring the dimensions of spirituality in relation to late-life functioning. Journal of Religion and Health, 57(6), 2167–2181. https://doi.org/10.1007/s10943-017-0515-9
- Ulrich, R. S., Zimring, C., Zhu, X., DuBose, J., Seo, H.-B., Choi, Y.-S., Quan, X., & Joseph, A. (2008). A review of the research literature on evidence-based healthcare design. HERD, 1(3), 61–125. https://doi.org/10.1177/193758670800100306
- Van den Berg, A. E. (2005). Health impacts of healing environments: A review of the benefits of nature, daylight, fresh air and quiet in healthcare settings. Foundation 200 years University Hospital Groningen.
- Van den Berg, A. E., & Van den Berg, M. M. H. E. (2015). Health benefits of plants and green space: Establishing the evidence base. Acta Horticulturae, 1093, 19–30. https://doi.org/10.17660/ActaHortic.2015.1093.1
- Van den Berg, A. E., & Van Duijn, B. (2014). Planten in justitiële inrichtingen. [Plants in forensic-psychiatric institutions] (Report 14908). Fytagoras.
- World Health Organization. (2018). The global network for age-friendly cities and communities: Looking back over the last decade, looking forward to the next. World Health Organization.