Abstract
Background
A sterilization requirement to change legal gender was removed from Swedish law in 2013, facilitating pregnancy in trans masculine individuals. The limited number of studies investigating pregnancy and childbirth among trans masculine individuals indicate increased gender dysphoria and negative experiences of pre- and post-natal healthcare, highlighting a need to improve care. Research focusing on Europe or contexts where sterilization to change legal gender was previously required by national law remains minimal.
Aims
This study aimed to investigate how trans masculine individuals experience healthcare encounters in connection with pregnancy, delivery and nursing, in a setting where mandatory sterilization to change legal gender was recently removed.
Methods
In-depth face-to-face interviews were conducted with 12 trans masculine individuals who attended Swedish prenatal care and delivered a child after the law on legal gender recognition was amended. Thematic content analysis was used.
Results
Providers in gender clinics, antenatal care and delivery were perceived to regard a masculine gender identity and pregnancy as incompatible. The main categories encompassed expectations and experiences of pregnancy related care and participant responses to it. Participants took charge of their care to ensure that their needs were fulfilled. The quality of care was inconsistent.
Discussion
A lack of knowledge, narrow gender norms and the legacy of the former legal sterility requirement limited access to diagnostic evaluation of gender dysphoria, information on reproduction and gender-affirming treatment. Medical safety during pregnancy, childbirth and nursing was impeded, gender dysphoria increased, and participants experienced minority stress. Attempts to avoid microaggressions guided healthcare encounters and birth wishes. Navigating healthcare required considerable attention, personal resources and energy, leaving particularly vulnerable individuals at risk of a lower quality of care. The paper concludes with clinical recommendations.
Introduction
Transgender people may experience a form of distress commonly referred to as gender dysphoria (GD) (Davy & Toze, Citation2018). We use the concept of GD in this paper to refer to subjective experiences of such distress, rather than the DSM-5 diagnosis of GD which has further criteria (American Psychiatric Association, Citation2013). Treatment needs and options for individuals transgender people vary, but may include hormones and gender-affirming surgery. While gender identities have historically been confined to male or female in many clinical settings, identities between and beyond male and female are increasingly being recognized (Richards et al., Citation2016).
Trans masculine individuals are people who were assigned female at birth, and whose gender identity and/or gender expression is male. Most were born with reproductive organs that enable pregnancy (Obedin-Maliver & Makadon, Citation2016) and may want to become parents (Haines et al., Citation2014; von Doussa et al., Citation2015). However, social norms, laws and treatments may pose obstacles. Sterilization is required to change legal gender in several countries (Dunne, Citation2017), and was mandatory in Sweden until 2013 (SFS, 2013, p. 405). Testosterone treatment frequently inhibits ovulation, which usually resumes if testosterone is discontinued (T'Sjoen et al., Citation2019). Contrary to previous beliefs, recent research suggests that prolonged testosterone exposure does not impede fertility (Leung et al., Citation2019). However, trans masculine individuals may be unaware, misinformed, or find it hard to pause testosterone given its gender-affirming properties.
GD may increase during pregnancy (Charter et al., Citation2018; Ellis et al., Citation2015; Light et al., Citation2014), and interaction with healthcare providers (HCPs) can be challenging. In Australia, transgender individuals were barred from fertility clinics (Charter et al., Citation2018). In a US study, participants were surprised by their positive interactions with HCPs in antenatal care, although enhanced reproductive counseling was needed (Ellis et al., Citation2015). Other US studies, show mixed experiences including use of incorrect pronouns, prejudicial services and denial of treatment (Hoffkling et al., Citation2017; Light et al., Citation2014). Studies on how trans masculine individuals experience pregnancy, childbirth and nursing from Europe or contexts where sterilization to change legal gender was recently required in national law remain minimal.
General and mental health disparities in transgender people (Dhejne et al., Citation2016) are explained by the minority stress model, which holds that legal discrimination, lack of social support, and violence and harassment expose minorities (i.e. groups who are seen as subordinate by dominant culture) to chronic stress that adversely affects their health (Hendricks & Testa, Citation2012; Meyer, Citation1995). A study on fear of childbirth among lesbian and bisexual women, and transgender people, found that minority stress produced as a result of experiences with Swedish healthcare increased anxiety (Malmquist et al., Citation2019). Discrimination and bias toward transgender individuals in the health care setting and elsewhere may be communicated through subtle behaviors and statements (Nadal et al., Citation2012). Such expressions of derogatory views toward a minority are labeled microaggressions (Sue, Citation2010a, Citation2010b). Although microaggressions are often unintentional, they have been linked to negative mental health outcomes (Nadal et al., Citation2014).
The described risk of heightened GD in trans masculine individuals during pregnancy and childbirth combined with reports of negative experiences in pre- and post-natal healthcare indicate a need to expand knowledge to optimize care. The aim of the present study was therefore to investigate how trans masculine individuals experience healthcare encounters in connection with pregnancy, delivery and nursing, in a setting where sterilization was recently required to change legal gender.
Swedish transgender and reproductive healthcare and associated laws
In Sweden legal genders are limited to male or female and indicated by the personal identification number. Diagnostic evaluation of GD takes place in gender clinics and the ICD-10 diagnosis Transsexualism, which requires a binary gender identity (World Health Organization, Citation1992), is mainly used. Referrals for gender-affirming treatment are only made after a diagnosis has been established.
Until 2013 Swedish law mandated sterility before legal gender recognition was granted. Preserved gametes had to be destroyed and castration was required. In 2013 a legal amendment omitted the sterility requirement and fertility preservation became available.
General healthcare covers evaluation and treatment of GD and insemination and IVF for one child. Egg or embryo donation are permitted within a relationship since 2019 (SFS, Citation2018, p. 1283) but surrogacy remains prohibited. Antenatal care is free of charge. A midwife follows the patient until delivery, when hospital-based midwives take over. If a patient requests an elective cesarean for fear of giving birth, counseling is recommended. An obstetrician ultimately decides on the mode of delivery. Breast feeding is strongly recommended for at least 3-6 months and is the norm.
Materials and methods
Study participants and procedure
Representatives from the organizations RFSL and RFSL Youth, working with transgender health and rights, helped plan this study. Eligibility criteria for study participation were (1) assigned female at birth with a self-identification on the male side of the gender spectrum or as non-binary before pregnancy; (2) a wish for masculinizing gender-affirming treatment resulting in a referral for a diagnostic evaluation of GD before or during pregnancy; (3) giving birth after the sterilization requirement was removed in 2013. The organizations RFSL and RFSL Youth, transgender experts, gender clinics and former study participants recruited individuals to the study.
Twelve in-depth face-to-face interviews were carried out across Sweden from December 2016 to January 2019. The first author, a resident in psychiatry with several years of clinical experience from the Stockholm gender clinic, performed all interviews. After demographic information on gender identity, access to gender-affirming treatments, age, occupation and civil status had been collected, interviews started with the question: What was it like for you to undergo pregnancy as a man/trans masculine/non-binary individual? By using an interview guide, the preconception phase, internal and external experiences during pregnancy and childbirth, as well as baby feeding choices were covered. Participants were encouraged to share experiences of healthcare encounters in relation to pregnancy in gender clinics, prenatal care and obstetrics. Results on how participants navigated identity and GD internally and in everyday life will be presented in a separate article. Field notes were taken for a preliminary overview. Saturation was achieved after nine interviews and confirmed by three additional interviews. Interviews lasted 55 − 112 minutes (mean 83 minutes), were digitally recorded and transcribed verbatim.
Twelve participants were included in the study. Many used several terms to describe their gender. In the manuscript they are all referred to as trans masculine, to ensure anonymity. Preferred pronouns and fictive names are used. Demographic information is presented in and . Five participants had undergone more than one pregnancy and could compare the care before and after the legal amendment.
Table 1. Demographic participant information (n = 12).
Table 2. Demographic participant information (n = 12).
Data analysis and positionality
Data was analyzed using inductive thematic content analysis (Burnard, Citation1991; Burnard et al., Citation2008). Inductive analysis was selected, as knowledge on the area of study was limited (Graneheim et al., Citation2017). Initially transcripts were read for an overview. Text units relevant to the aim were then identified, coded and sorted into main- and sub-categories. These were then revised to merge or regroup overlapping categories and identify a common theme. Transcripts were read repeatedly to ensure that no relevant information was misunderstood or lost. Clarifications and excisions (three dots) from quotations are marked with squared brackets.
Recommendations on qualitative research (Tong et al., Citation2007) and established criteria for trustworthiness (Lincoln & Guba, Citation1985) were used. During the analysis the diverse educational backgrounds of the research group members, encompassing reproductive health, psychiatry, transgender health and human rights were an asset. Being female, cisgender, clinicians working in transgender healthcare, placed us in a position of power in relation to the participants. Since positionality affects the research process and knowledge production, (Malterud, Citation2001) the study was designed with the community organizations RFSL and RFSL Youth. Coding and analysis of the interviews were carried out parallel to the data collection, allowing participant narratives to inform subsequent interviews (Strauss & Corbin, Citation1990).
Ethical considerations
The Regional Ethical Review Board of Stockholm, Sweden approved the study, which was performed according to the 1964 Helsinki declaration and its later amendments. Before inclusion oral and written study information was provided and participants signed a consent form. The interviewer was not involved in the healthcare of any participant at the time of the interviews or thereafter. Ethical risks were discussed with RFSL and RFSL Youth. Since interviews could invoke traumatic memories, referral procedures for psychological counseling were established. However, no participant needed these services.
Results
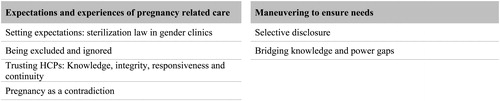
The analysis resulted in two main categories and six sub categories (see ). The main category Expectations and experiences of pregnancy related care highlights participant expectations of healthcare in relation to gender norms concerning pregnancy and perceptions of received care. The actions that participants took to ensure that their health needs were fulfilled are presented in the second main category: Maneuvering to ensure needs.
Expectations and experiences of pregnancy related care
The gender recognition law guided reproductive options and encounters in gender clinics, shaping expectations on reproductive healthcare. HCPs assessed the gender identity of participants against binary gender norms, treating pregnancy with suspicion, in line with previous research on how medicine defines sex and gender, and pathologizes those who deviate from the norm, contributing to the illusion that all transgender individuals are alike (Pearce et al., Citation2019; Riggs et al., Citation2019). Participants expected HCPs in antenatal care and delivery to see and treat them as women, similar to earlier research describing the inseparability of pregnancy and motherhood (Charter et al., Citation2018; Obedin-Maliver & Makadon, Citation2016) or to put an unwarranted focus on their gender, ignoring their real health needs and integrity. Although, many were content with their care, reproductive healthcare was perceived as a woman´s domain, which limited knowledge development among HCPs. While some received excellent care, participants also encountered exoticization, endorsement of binary gender norms, a lack of privacy, and denial of individual needs including the use of incorrect pronouns. These examples have all been described as microaggressions in the previous literature (Nadal et al., Citation2012).
This main category consists of four sub-categories: 1) Setting expectations: Sterilization law in gender clinics; 2) Being excluded and ignored; 3) Trusting HCPs: Knowledge, integrity, responsiveness and continuity; and 4) Pregnancy as a contradiction.
Setting expectations: sterilization law in gender clinics
Several participants had begun to question their gender identity at a time when legal gender recognition required sterility, trapping them between a wish for children and gender-affirming treatment. Although the law did not mandate sterilization for diagnosis, hormonal treatment or chest masculinization surgery participants postponed their evaluation or did not disclose that they considered pregnancy, believing that the gender clinics would regard pregnancy and a male gender as incompatible and deny them treatment. This is exemplified by the following quotation from George:
[Did you mention that you wanted children during the assessment?] No. Back then they were stricter on whom they granted treatment. I knew that I needed hormones and a mastectomy.
When sterilization was still practiced, gender clinics regarded an acceptance of sterilization and a wish for legal gender recognition as diagnostic. Consequently, reproductive aims had to be denied to be diagnosed with Transsexualism, which was a prerequisite for treatment, as Bjorn said:
They told me that as a transsexual you say no to biological children. And then they forced me, particularly towards the end [of the diagnostic evaluation] to deny that I wanted children […] It says in my medical record that they have debated that if I do want a child […] can I truly be transgender?
These narratives suggest that gender clinics acted as guardians of binary gender norms. When mandatory sterilization was abandoned, participants remained apprehensive that HCPs would continue to question their gender identity given their reproductive wishes. Fears were acknowledged as gender clinics posed unwarranted questions, terminated evaluations or postponed treatment decisions during pregnancy, as exemplified by Harley:
[My assessment] was paused when I got pregnant […] it was clear that they wanted to wait to see if I would realize that I did not want to be trans or want transgender healthcare […] I felt that it would have been better to finish it.
While several participants encountered binary gender norms in gender clinics, those who could compare the care before and after the law was amended said it improved, enabling them to request and receive information more openly. To be seen as supportive, gender clinics had to be nonjudgmental of trans masculine pregnancies, understand gender as a spectrum, offer continuity and a low contact threshold.
Being excluded and ignored
Participants felt like outsiders in antenatal care. The language used in consultations, group sessions, information materials and patient forms equated pregnancy with women. Inclusive forms were given to transgender patients only, keeping them as the exception. Inconsistent use of pronouns triggered GD. The institutionalization of motherhood norms was emphasized in the electronic medical record software (EMR), which failed to create a patient file when a male personal identification number was entered. Consequently, legally registered males carried a paper copy of their medical record across clinics. With no EMR, participants were concerned about their safety as standard procedures could not be followed, increasing medical risks. George explained:
In delivery they wanted to make a […] CTG [exam to record fetal heartbeats and uterine contractions] and it was not possible to see the curve on the computer because they were not able to ender my id number. And they had to find a printer to use, but [at first] it did not work because they never use it.
Trusting HCPs: Knowledge, integrity, responsiveness and continuity
As pregnancy was tied to notions of femaleness, knowledge of transgender health in reproductive health services was low. Trust in HCPs depended on their willingness to listen to needs, respect integrity and refrain from unwarranted questions and unnecessary physical exams. While several providers gave adequate attention to the gender identity of participants some appeared uncomfortable, asked intrusive questions or disclosed personal information.
Participants valued when HCPs recognized that their knowledge was limited and took independent responsibility to learn. Some HCPs trained themselves and their colleagues while others merely apologized when making mistakes. Some participants interpreted this as humility, while others saw it as a strategy to escape responsibility, as Iben said:
[The midwife] kept saying, “I will say the wrong thing and you have to correct me”, instead of saying, “This is new to me but I will do my best to say the right thing”. It got really tiring, because all the time they placed the responsibility on me […] rather than seeing their own responsibility.
Knowledge gaps were particularly evident concerning nursing. Some HCPs did not treat GD as a valid reason not to nurse. On the other hand, participants with prior chest masculinization surgery who wanted to nurse found that HCPs did not know if and under what circumstances they would be able to do so. HCPs seemed unprepared when lactation occurred, failed to provide information and to prevent mastitis. John explained:
Early in the pregnancy milk started coming, which was pretty interesting considering that I have done five mastectomies […] the doctors could not explain it.
Fear of bias, denial of privacy and integrity, as well as knowledge gaps was pronounced concerning delivery. Participants changed midwife when transferring from antenatal care to delivery according to standard procedures. The disruption in staff highlighted participant vulnerabilities. Participants were unsure if their needs would be carried forward and expected several shifts of staff, forcing them to come out repeatedly, increasing the risk of maltreatment, which caused anxiety. Some considered induction or a home birth to identify their midwives beforehand, educate them and assess their attitudes. Aiden emphasized the importance of staff continuity and knowledge development by saying:
First, I thought of [a home birth] as an alternative to avoid having to explain myself to a whole bunch of people […] and to be able to meet the midwives beforehand and talk to them, explain all that needs to be said and get a feel for how they are.
The lack of knowledge regarding transgender pregnancies among HCPs made participants uncertain if GD would be considered a valid reason for a cesarean, causing anxiety. Lack of trust in HCPs affected birth wishes, although conclusions on whether a cesarean or vaginal delivery carried less risk varied. Bjorn explained how earlier mistreatment by HCPs affected his birth wishes by saying:
I fear that there will be someone there to forcibly castrate me, who forcibly sterilizes me when I have been put to sleep, when I cannot defend myself. And of course, I know that it is really irrational, but it is that year [in evaluation] when it was taken for granted that they could do it against my will.
In the end, most participants appreciated their delivery since their HCPs focused on its medical aspects rather than their gender, used pronouns correctly and asked about needs. However, positive healthcare experiences were often attributed to the personal interest of an individual clinician rather than a systematic approach of the clinic and therefore did not affect healthcare expectations.
Pregnancy as a contradiction
While many HCPs were respectful and professional, some treated pregnancy and a masculine gender as incompatible. HCPs questioned the gender of participants explicitly or indirectly. Some were puzzled or less accommodating when participants came out as transgender. Physical appearances and the ability to be red as masculine affected healthcare encounters. Those who had not received any masculinizing treatments felt that HCPs did not take their gender identity seriously, as Harley recalled:
You are seen as less transgender. If I had gone through assessment and taken testo [testosterone] for a while and then wanted to have a child, I would probably have received completely different reactions […] that your trans identity is made invisible is particularly hard […] what you say is never enough […] they don’t care what you say […] it is worst when you have come out to yourself and others but it has stopped there because your looks have not changed yet, and then you are not taken seriously.
Similarly, participants who had undergone gender-affirming treatment argued that coming out would have been harder without it, as their gender would have been easier to question. Some noted that HCPs failed to realize that they were pregnant. Consequently, David had to wait in the emergency department during premature labor. He said:
When we went to the hospital reception [my friends said]; “Eh, our friend he's pregnant. He's having a baby, the baby's coming”. And the hospital people were like, “He's having a baby?” […] My friends kept trying to make them understand. So, it took a while for them to attend to me. By the time they [did] I was actually three centimeters open. [By then it] was already too late. It was the he pronoun, father [that confused them]
The perceived incompatibility between pregnancy and masculinity also affected information transfers. Only one participant had discussed breastfeeding with their plastic surgeon prior to chest surgery. This participant had planned a breast reduction to avoid coming out as transgender. The fact that nursing was only discussed when the patient was assumed to be female, highlights how gender norms render trans masculine pregnancies unthinkable, affecting care.
Maneuvering to ensure needs
Based on earlier experiences and low expectations, participants took responsibility for their needs, rather than relying on HCPs to do so. Meeting needs was often reduced to avoiding triggers of GD and microaggressions. Responses to mistreatment were emotional, cognitive and behavioral, in line with previous research on microaggressions (Nadal et al., Citation2014). Participants felt angry, sad, anxious and helpless, misunderstood and invalidated. Cognitive strategies included rationalizing the behaviors of HCPs and attempts to predict their actions. Behavioral responses included adjusted disclosure, confrontation, education of HCPs and attempts to select and appease them. Balancing power differences required strategic skills and knowledge of healthcare routines, draining participants of energy and leaving the vulnerable behind, as described in the sub-categories: 1) Selective disclosure; and 2) Bridging knowledge and power gaps.
Selective disclosure
Some participants had kept their female legal gender marker to be able to act female and lower the risk of unwarranted attention to their gender, enabling HCPs to pay better attention to their health and the wellbeing of their child. Charlie illustrated this by saying:
It was a very conscious decision [to refrain from changing legal gender]. If you pass as a woman, even if you are a very masculine woman it is easier for others, they do not have to get stressed […] Sometimes other things are more important than your gender identity.
Those who broke multiple norms practiced selective disclosure to avoid maltreatment. Being born outside of Sweden, divorced or single, attracted to women, vegan or vegetarian, living with a disability or not wanting others to know the sex of your child could potentially alienate HCPs. Some tried to read the attitudes of HCPs to weigh disclosure options, as Kylar exemplified:
I always started to get a feel for the terrain, maybe talked about something that does not concern me personally to see how it is received, like transgender care […] closing in on the topic in big circles […] to give me the option to back off and still get treated reasonably well if they cannot handle it.
Bridging knowledge and power gaps
Ensuring needs involved overcoming knowledge and power gaps. Participants educated HCPs. Some argued that it was their own active efforts and social status that granted them quality care, as Aiden said:
I have done a lot of work, preparing for all contacts, to make it work smoothly. I think it has been smooth, but I believe it is because I have made a lot of effort and because I am a privileged person.
Participants with medical training questioned decisions that interfered with their needs. Others brought friends for support or sought information on rights and medical issues, preparing to fight, which put them on edge. Another approach was to act assertive or threaten to report discriminatory actions, as Lennon emphasized:
I believe that our self-confidence [made a difference]. The strategy to be assertive to make others docile. If I’m insecure there will be room for you to show much more uncertainty, but if I remain calm and secure and show that I’m like confident in what I’m saying, then you will accept or follow more easily.
Participants who felt incapable of challenging clinicians due to power differences resulting from a lack of knowledge, dependency on HCPs, or a perceived lack of strategic negotiation skills or self-esteem often saw no option but to endure. Some argued that they could not expect HCPs to adjust the care to meet their needs. HCPs often failed to ask about wishes and act on ill-timed requests. Raising needs required communication skills and knowledge about the health system, as illustrated by Frankie, a participant with autism, who gave birth vaginally as he did not understand the assessment process for an elective cesarean. He remembered wanting to escape or die during the delivery, equated the vaginal exams to rape, and had strong anxiety. His experiences highlight how the quality of care was dependent on the abilities of the individual patient to understand and maneuver the healthcare system. Frankie explained:
I was a little late [in requesting a caesarean because] I don´t know how it works. Should you go there a month in advance and tell them that you want a caesarean? […] She [midwife in antenatal care] just said that it exists […] I asked people I know, but no one was able to tell me how to get it.
Dependency made it difficult to criticize HCP. To manage emotional reactions participants rationalized the behaviors of disrespectful HCPs, blaming knowledge gaps or medical considerations. Blocking out parts of what HCPs said, such as inappropriate pronouns, and still grasp the relevant information required energy and experience, as Lennon recalled:
[We tried to] create as little friction as possible, so we did not fight […] we never insisted that they should not gender me […] but just sighed and moved on […] and I am so accustomed to queer read [reinterpret] things, or add a norm filter to […] make it feel less. […] Since they read me as female, they give me information in a particular way, and I can absorb the information because I am so used to look past the fact that they are wrong.
Other participants adopted a friendly attitude and stressed their will to cooperate with the staff to avoid being perceived as a burden. This steered the focus from their pregnancy toward the staff, as Kylar explained:
I felt that I had to be nice so that they did not feel that I was a liability […] because they need to take a lot of things into consideration […] I had to be nice when all I really wanted to do was focus on giving birth.
Participants turned to peers for information on medical issues such as nursing after chest surgery and testosterone effects on egg quality. Community groups, including transnational networks on social media offered security, information and support when HCPs failed to do so, increasing resilience.
Discussion
This qualitative interview study explored how trans masculine individuals experience healthcare encounters in relation to pregnancy, childbirth and nursing in a setting where mandatory sterility was recently abandoned. The findings indicate that the former sterility requirement reinforced the notion that a trans masculine identity and pregnancy are incompatible. This narrow understanding of gender affected the diagnostic procedure and limited access to evaluation and treatment for GD although these aspects were beyond the scope of the law. In antenatal and obstetrical care, the positioning of a masculine identity and pregnancy as mutually exclusive affected knowledge development, patient security and interaction with HCPs, leaving participants feeling excluded and ignored at the same time as their gender was at the focus of attention. By embodying a challenge to the gender binary and notions of a uniform transgender experience, participants challenged the professionalism of HCPs and the organization of care. Navigating healthcare to ensure needs was stressful and required considerable attention, personal resources and energy, leaving the most vulnerable at risk of a lower quality of care.
The sterility requirement posed a barrier to care, as participants believed that gender clinics would refrain from diagnosing and treating them for GD, given their reproductive aims. Sterilization was an expected step in the gender-affirming process. This illustrates how law and medical practices get intertwined as they simultaneously frame and reflect one another. Similar findings were made in the UK where the law on gender recognition required sterilization only, but influenced medical practice so that the more extensive intervention of hysterectomy became standard medical procedure, as pregnancy in men was rendered unthinkable (Toze, Citation2018).
After mandatory sterility was abandoned, concerns that pregnancy would affect diagnostics persisted. Several participants met acceptance and support while others perceived a reluctance to diagnose them as gender clinics posed additional questions or stopped evaluations during pregnancy. While a thorough evaluation is necessary for diagnostic accuracy and to minimize treatment regrets (Landen et al., Citation1998; Wiepjes et al., 2018), it remains to be determined if pregnancy poses a risk in this regard. No previous studies have indicated such risks and no participant in this study changed their wish for gender-affirming treatment. Interrupting evaluation cuts access to transgender health experts who could provide support if GD increases during pregnancy, which previous studies indicate that it may do (Charter et al., Citation2018; Light et al., Citation2014). If new gender identity insights emerge, those should also be considered important to explore.
Participants were hesitant to discuss reproductive aims and nursing with HCPs. An earlier study on baby feeding options found that transgender individuals refrained from asking about nursing to safeguard access to surgery (MacDonald et al., Citation2016), highlighting that information may be forsaken when HCPs are perceived as gatekeepers. Adjusted disclosure to protect access to treatment has been previously described (Cohen-Kettenis & Gooren, Citation1999; Linander et al., Citation2019; MacDonald et al., Citation2016). An authoritarian evaluation and treatment process for GD has been found to limit the information upon which diagnostic decisions are made, decreasing their validity (Fisk, Citation1974; Nieder et al., Citation2016; Pimenoff & Pfäfflin, Citation2011). If patients feel unable to raise what they perceive as controversial concerns, this can limit the information HCPs receive, impeding medical safety (Doyle et al., Citation2013). The ways that different assessment frameworks for GD affect diagnostic accuracy, mental health and the risk of treatment regrets require exploration.
This study raises concerns regarding medical safety. Knowledge gaps among HCPs made participants turn to peers for medical advice. HCPs did not expect lactogenesis after chest masculinization surgery, failed to provide information on nursing and to prevent mastitis. The exclusion of legal males from the EMR limited information transfers between clinics and disabled standard procedures, posing a risk to patient security. The notion that only women get pregnant prevented the timely diagnosis of premature labor. As noted in a previous study, gynecological problems will only be identified as the cause of abdominal pain when HCPs perceive patients as female, why pregnancy complications in trans masculine patients risk being misdiagnosed (Stroumsa et al., Citation2019). Gender binary and cisnormative assumptions were thus associated with medical risks.
Gender norms also affected the quality of the patient-provider relationship. Previous experiences of stigma and discrimination by HCPs alerted participants to discover and react to microaggressions, such as invalidations of their gender identity and needs, increasing anxiety. Such hypervigilance explains why adverse health outcomes persist beyond microaggression exposure (Nadal et al., Citation2014). Microaggressions were common. Participants were misgendered, met exoticization, had their integrity ignored, and encountered assumptions of a uniform transgender experience, all of which have been categorized as microaggressions in previous research (Nadal et al., Citation2012) Fear of such responses made participants apprehensive of meeting new HCPs, which guided requests for caesareans, vaginal deliveries, home births, and inductions. These results add to previous studies that link birth wishes in transgender individuals to traumatization by HCPs (Hoffkling et al., Citation2017; Light et al., Citation2014).
According to the minority stress model, individuals of minority groups are exposed to stressors which dominant groups are not (Meyer, Citation1995). A stressor is a stimulus which threatens the ability of an individual to function properly. An individual who is unable to predict or control such a stressor, is likely to experience stress (Koolhaas et al., Citation2011). The participants of this study were reluctant to come out to an unfamiliar HCP during childbirth, since they were uncertain if HCPs would disrespect them based on their gender identity, causing distress. Participants strived to meet the midwives that would attend to their delivery beforehand to gauge their attitudes, predict their actions, and mitigate the risk of inconsiderate, intrusive, invalidating and demeaning comments or treatment by educating them on transgender health issues. The anxiety and fear of maltreatment that a lack of staff continuity resulted in highlight participants’ exposure to minority stress, and indicate the potential benefits of continuity care models, where a team of midwives follow the patient throughout antenatal care and delivery (Forster et al., Citation2016).
Many participants were happy with their care. This must be interpreted in relation to their low expectations and considerable efforts to guide HCPs. Resilience involved seeking independent information and peer support. Well-articulated, educated and strategic participants, who were actively involved in their care, seem to have had their needs acknowledged to a larger extent than those with mental health problems or language difficulties, pronouncing their vulnerability even further.
Conclusions
The findings of this study show that trans masculine gestational individuals experience minority stress and microaggressions in Swedish healthcare, exacerbated by the former gender recognition law and binary gender norms. Access to quality care was dependent on the engagement and negotiation skills of the individual patient, leaving particularly vulnerable individuals behind. Although results cannot be generalized, they may be used to inform healthcare. The findings call for individualized, inclusive, respectful and knowledgeable healthcare that does not treat a masculine identity and pregnancy as mutually exclusive. Gender clinics should develop knowledge to support patients with GD during pregnancy and ensure a low threshold for contact. Reproductive HCPs should pay attention to protect the privacy and integrity of their patients, use gender sensitive language and actively enquire about needs including fears concerning delivery to reduce the risk of inequitable care. Extra attention should be paid to individuals who might be unable to articulate their needs and concerns to avoid that they are disadvantaged. HCPs should enhance their knowledge on nursing after chest masculinization surgery. Continuity of care models should be considered to decrease hypervigilance. Cooperation with transgender support groups may support resilience in patients and knowledge development in clinics. HCPs working in contexts where sterilization is required to access legal gender recognition should pay attention to the risk that the legal framework might impede their medical judgment.
Ethical approval
The Regional Ethical Review Board of Stockholm, Sweden approved the study. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards
Informed consent
Informed consent was obtained from all individual parties included in the study.
Acknowledgments
We want to thank all study participants, RFSL, RFSL Youth and the healthcare professionals who recruited participants to this study. We are grateful that Psychiatry Southwest and ANOVA, Center of Andrology, Sexual Medicine and Transgender Medicine, Karolinska University Hospital in Stockholm, Sweden allotted time for the corresponding author to conduct this study.
Conflict of interest
The authors declare they have no conflict of interest.
Additional information
Funding
References
- American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders. (5th ed.). 10.1176/appi.books.9780890425596
- Burnard, P. (1991). A method of analysing interview transcripts in qualitative research. Nurse Education Today, 11(6), 461–466. 10.1016/0260-6917(91)90009-y
- Burnard, P., Gill, P., Stewart, K., Treasure, E., & Chadwick, B. (2008). Analysing and presenting qualitative data. British Dental Journal, 204(8), 429–432. 10.1038/sj.bdj.2008.292
- Charter, R., Ussher, J. M., Perz, J., & Robinson, K. (2018). The transgender parent: Experiences and constructions of pregnancy and parenthood for transgender men in Australia. International Journal of Transgenderism, 19(1), 64–77. 10.1080/15532739.2017.1399496
- Cohen-Kettenis, P. T., & Gooren, L. J. (1999). Transsexualism: A review of etiology, diagnosis and treatment. Journal of Psychosomatic Research, 46(4), 315–333. 10.1016/s0022-3999(98)00085-3
- Davy, Z., & Toze, M. (2018). What Is Gender Dysphoria? A Critical Systematic Narrative Review. Transgender Health, 3(1), 159–169. 10.1089/trgh.2018.0014
- Dhejne, C., Van Vlerken, R., Heylens, G., & Arcelus, J. (2016). Mental health and Gender Dysphoria: A review of the literature. International Review of Psychiatry (Abingdon, England)), 28(1), 44–57. 10.3109/09540261.2015.1115753
- Doyle, C., Lennox, L., & Bell, D. (2013). A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. British Medical Journal Open, 3(1), e001570. https://doi.org.proxy.kib.ki.se/10.1136/bmjopen-2012-001570
- Dunne, P. (2017). Transgender sterilisation requirements in Europe. Medical Law Review, 25(4), 554–581. 10.1093/medlaw/fwx028
- Ellis, S. A., Wojnar, D. M., & Pettinato, M. (2015). Conception, pregnancy, and birth experiences of male and gender variant gestational parents: It's how we could have a family. Journal of Midwifery & Women's Health, 60(1), 62–69. 10.1111/jmwh.12213
- Fisk, N. M. (1974). Editorial: Gender dysphoria syndrome - The conceptualization that liberalizes indications for total gender reorientation and implies a broadly based multi-dimensional rehabilitative regimen. The Western Journal of Medicine, 120(5), 386–391.
- Forster, D. A., McLachlan, H. L., Davey, M. A., Biro, M. A., Farrell, T., Gold, L., Flood, M., Shafiei, T., & Waldenstrom, U. (2016). Continuity of care by a primary midwife (caseload midwifery) increases women's satisfaction with antenatal, intrapartum and postpartum care: Results from the COSMOS randomised controlled trial. BMC Pregnancy and Childbirth, 16(1), 28. 10.1186/s12884-016-0798-y
- Graneheim, U. H., Lindgren, B. M., & Lundman, B. (2017). Methodological challenges in qualitative content analysis: A discussion paper. Nurse Education Today, 56, 29–34. 10.1016/j.nedt.2017.06.002
- Haines, B. A., Ajayi, A. A., & Boyd, H. (2014). Making trans parents visible: Intersectionality of trans and parenting identities. Feminism & Psychology, 24(2), 238–247. 10.1177/0959353514526219
- Hendricks, M., & Testa, R. (2012). A conceptual framework for clinical work with transgender and gender nonconforming clients: An adaptation of the minority stress model. Professional Psychology - Research & Practice, 43(5), 460–467. 10.1037/a0029597
- Hoffkling, A., Obedin-Maliver, J., & Sevelius, J. (2017). From erasure to opportunity: a qualitative study of the experiences of transgender men around pregnancy and recommendations for providers. BMC Pregnancy and Childbirth, 17(Suppl 2), 332https://doi.org/10.1186/s12884-017-1491-5
- Koolhaas, J. M., Bartolomucci, A., Buwalda, B., de Boer, S. F., Flügge, G., Korte, S. M., Meerlo, P., Murison, R., Olivier, B., Palanza, P., Richter-Levin, G., Sgoifo, A., Steimer, T., Stiedl, O., van Dijk, G., Wöhr, M., & Fuchs, E. (2011). Stress revisited: A critical evaluation of the stress concept. Neurosci Biobehav Rev, 35(5), 1291–1301. 10.1016/j.neubiorev.2011.02.003
- Landen, M., Walinder, J., & Lundstrom, B. (1998). Clinical characteristics of a total cohort of female and male applicants for sex reassignment: A descriptive study. Acta Psychiatrica Scandinavia, 97(3), 189–194. 10.1111/j.1600-0447.1998.tb09986.x
- Leung, A., Sakkas, D., Pang, S., Thornton, K., & Resetkova, N. (2019). Assisted reproductive technology outcomes in female-to-male transgender patients compared with cisgender patients: A new frontier in reproductive medicine. Fertility and Sterility, 112(5), 858–865. 10.1016/j.fertnstert.2019.07.014
- Light, A. D., Obedin-Maliver, J., Sevelius, J. M., & Kerns, J. L. (2014). Transgender men who experienced pregnancy after female-to-male gender transitioning. Obstetrics and Gynecology, 124(6), 1120–1127.10.1097/aog.0000000000000540
- Linander, I., Alm, E., Goicolea, I., & Harryson, L. (2019). It was like I had to fit into a category": Care-seekers' experiences of gender regulation in the Swedish trans-specific healthcare. Health (London, England : 1997), 23(1), 21–38. 10.1177/1363459317708824
- Lincoln, Y., & Guba, E. (1985). Naturalistic Inquiry. Sage Publications.
- MacDonald, T., Noel-Weiss, J., West, D., Walks, M., Biener, M., Kibbe, A., & Myler, E. (2016). Transmasculine individuals' experiences with lactation, chestfeeding, and gender identity: A qualitative study. BMC Pregnancy and Childbirth, 16, 106. 10.1186/s12884-016-0907-y
- Malmquist, A., Jonsson, L., Wikstrom, J., & Nieminen, K. (2019). Minority stress adds an additional layer to fear of childbirth in lesbian and bisexual women, and transgender people. Midwifery, 79, 10255110.1016/j.midw.2019.102551
- Malterud, K. (2001). Qualitative research: Standards, challenges, and guidelines. Lancet (London, England), 358(9280), 483–488. 10.1016/s0140-6736(01)05627-6
- Meyer, I. H. (1995). Minority stress and mental health in gay men. Journal of Health and Social Behavior, 36(1), 38–56.
- Nadal, K., Davidoff, K., Davis, L., & Wong, Y. (2014). Emotional, behavioral, and cognitive reactions to microaggressions: Transgender perspectives. Psychology of SexualOorientation andGgender Diversity, 1(1), 72–81. 10.1037/sgd0000011
- Nadal, K. L., Griffin, K. E., Wong, Y., Hamit, S., & Rasmus, M. (2014). The impact of racial microaggressions on mental health: Counseling implications for clients of color. Journal of Counseling & Development, 92(1), 57–66. 10.1002/j.1556-6676.2014.00130.x
- Nadal, K. L., Skolnik, A., & Wong, Y. (2012). Interpersonal and systemic microaggressions toward transgender people: Implications for counseling. Journal of LGBT Issues in Counseling, 6(1), 55–82. 10.1080/15538605.2012.648583
- Nieder, T. O., Elaut, E., Richards, C., & Dekker, A. (2016). Sexual orientation of trans adults is not linked to outcome of transition-related health care, but worth asking. International Review of Psychiatry, 28(1), 103–111. 10.3109/09540261.2015.1102127
- Obedin-Maliver, J., & Makadon, H. J. (2016). Transgender men and pregnancy. Obstetric Medicine, 9(1), 4–8. 10.1177/1753495X15612658
- Pearce, R., Moon, I., Gupta, K., & Steinberg, D. L. (2019). The emergence of trans: Cultures, politics and everyday lives. Routlege.
- Pimenoff, V., & Pfäfflin, F. (2011). Transsexualism: Treatment outcome of compliant and noncompliant patients. International Journal of Transgenderism, 13(1), 37–44. 10.1080/15532739.2011.618399
- Richards, C., Bouman, W. P., Seal, L., Barker, M. J., Nieder, T. O., & T'Sjoen, G. (2016). Non-binary or genderqueer genders. Int Rev Psychiatry), 28(1), 95–102. 10.3109/09540261.2015.1106446
- Riggs, D. W., Pearce, R., Pfeffer, C. A., Hines, S., White, F., & Ruspini, E. (2019). Transnormativity in the psy disciplines: Constructing pathology in the Diagnostic and Statistical Manual of Mental Disorders and Standards of Care. The American Psychologist, 74(8), 912–924. 10.1037/amp0000545
- SFS (2013). 405. Lag om ändring i lagen (1972:119) om fastställande av könstillhörighet i vissa fall. Socialdepartementet. https://www.riksdagen.se/sv/dokument-lagar/dokument/svensk-forfattningssamling/lag-1972119-om-faststallande-av_sfs-1972-119
- SFS (2018). 1283. Lag om ändring i lagen (2006:351) om genetisk integritet m.m. Socialdepartementet. https://www.lagboken.se/views/pages/getfile.ashx?portalId=56&docId=3285711&propId=5
- Strauss, A. L., & Corbin, J. M. (1990). Basics of qualitative research: Grounded theory procedures and techniques. Sage Publications.
- Stroumsa, D., Roberts, E. F. S., Kinnear, H., & Harris, L. H. (2019). The power and limits of classification - A 32-year-old man with abdominal pain. The New England Journal of Medicine, 380(20), 1885–1888. 10.1056/NEJMp1811491
- Sue, D. W. (2010a). Microaggressions and marginality: Manifestation, dynamics, and impact. Wiley.
- Sue, D. W. (2010b). Microaggressions in everyday life: Race, gender, and sexual orientation. Wiley.
- Tong, A., Sainsbury, P., & Craig, J. (2007). Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. International Journal for Quality in Health Care : journal of the International Society for Quality in Health Care, 19(6), 349–357. 10.1093/intqhc/mzm042
- Toze, M. (2018). The risky womb and the unthinkability of the pregnant man: Addressing trans masculine hysterectomy. Feminism & Psychology, 28(2), 194–211. 10.1177/0959353517747007
- T'Sjoen, G., Arcelus, J., Gooren, L., Klink, D. T., & Tangpricha, V. (2019). Endocrinology of transgender medicine. Endocrine Reviews, 40(1), 97–117. 10.1210/er.2018-00011
- von Doussa, H., Power, J., & Riggs, D. (2015). Imagining parenthood: the possibilities and experiences of parenthood among transgender people. Culture, Health & Sexuality, 17(9), 1119–1131. 10.1080/13691058.2015.1042919
- Wiepjes, C. M., Nota, N. M., de Blok, C. J. M., Klaver, M., de Vries, A. L. C., Wensing-Kruger, S. A., de Jongh, R. T., Bouman, M. B., Steensma, T. D., Cohen-Kettenis, P., Gooren, L. J. G., Kreukels, B. P. C., & den Heijer, M. (2018). The Amsterdam cohort of gender dysphoria study (1972-2015): Trends in prevalence, treatment, and regrets. The Journal of Sexual Medicine, 15(4), 582–590. 10.1016/j.jsxm.2018.01.016
- World Health Organization (1992). International statistical classification of diseases and related health problems (10th ed.). Author.