Abstract
Background
Preliminary results of a specific semi-rigid prosthesis for metoidioplasty (ZSI® 100D4; Zephyr Surgical Implants, Geneva) have been reported, suggesting a safe procedure that may enhance the metoidioplasty outcomes by stiffening and increasing protrusion of the constructed neo-phallus.
Aim
The objective of the present study was to report the updated surgical results of metoidioplasty with implantation of the ZSI®100D4, along with a comprehensive evaluation of the outcomes including, motivations, sexuality, and urinary function.
Methods
All individuals who underwent a metoidioplasty with implantation of the ZSI®100D4 between August 2017 and January 2021 with at least 1 year of follow-up were included and their data retrospectively collected. They were contacted by telephone between November 2020 and May 2022 and invited to answer a questionnaire exploring motivations, satisfaction with genitals and sexual life, as well as urinary and sexual function.
Results
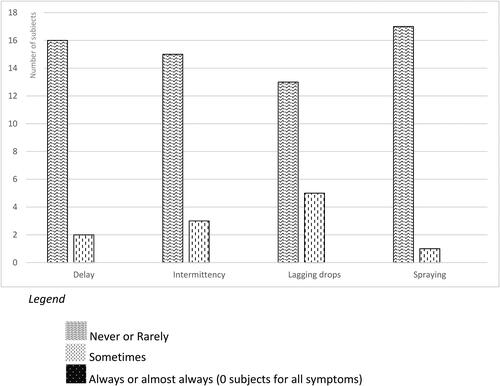
Twenty-one individuals were included and followed-up during a median [IQR] period of 19.5 months [12.8–24.2]. Most individuals (n = 13; 62.0%) had a post-operative complication, the most frequent was wound dehiscence (n = 6; 28.6%). Three urinary fistula (14.3%) were reported, all managed conservatively (Clavien-Dindo grade 2) with a prolonged urinary diversion. Among the 18 individuals who answered the questionnaire, 16 (88.9%) were sexually active, and 11 (61.1%) were engaged in a sexual relationship. The total median [IQR] self-esteem and relationship questionnaire score was 92 [91–97]. The reported urinary symptoms of delay, intermittency, lagging drops and spraying were mostly never or rarely reported. The satisfaction regarding overall genital aspect was highly favorable as 15 (83.3%) individuals reporting being very satisfied or satisfied, although 5 (27.8%) reported being dissatisfied with the size of their genitals.
Conclusion
Implantation of a semi-rigid prosthesis in a metoidioplasty seems a safe procedure, with no reported complications related to the prosthesis. Overall, satisfaction regarding genitals, sexual and urinary function are favorable.
Introduction
There is to date no ideal approach for the construction of a neo phallus for transgender men seeking genital gender affirming surgery (GGAS) (Walton et al., Citation2021). Multiplication of the techniques and the complex evaluation of outcomes make it difficult for individuals opting for a masculinizing GGAS to choose the most appropriate technique, despite the availability of rare decision aid (Özer et al., Citation2018; Scalia et al., Citation2021). Regardless some inherent limitations, metoidioplasty is a one-stage procedure that can provide functional male genitalia (Hage, Citation1996). Despite avoiding extensive scarring of the donor area, metoidioplasty seems nowadays a less frequent option chosen by transgender men compared to phalloplasty (Al-Tamimi et al., Citation2020), this choice possibly being influenced by age and gender identity (Parker et al., Citation2022). However, it has certain advantages such as the absence of donor-site morbidity, fewer surgeries, preserved erogenous sensation (Hadj-Moussa et al., Citation2019) and fewer urethral complications (Ortengren et al., Citation2022), which have been reported to be of high priority for individuals seeking to undergo masculinizing GGAS (Ganor et al., Citation2019; Jacobsson et al., Citation2017). Some technical refinements have been progressively made to the technique to improve its results (Jolly et al., Citation2021), and in 2017 a specific semi-rigid prosthesis for metoidioplasty was marketed (ZSI®100D4; Zephyr Surgical Implants, Geneva). A description of the prosthesis implantation technique and preliminary results have been reported, suggesting a safe procedure (Neuville et al., Citation2021), probably associated with less complications than prosthesis implantation in phalloplasty (Preto et al., Citation2020). Metoidioplasty outcomes in terms of sexual and urinary function may be enhanced by this semi-rigid prosthesis, by stiffening and increasing protrusion of the constructed neo-phallus (Neuville et al., Citation2021). However, outcomes after a longer follow-up are needed, as well as a broader, patient-centered evaluation to provide practical outcomes pertinent for pre-operative counseling.
The objective of the present study was therefore to report a comprehensive evaluation of the outcomes of metoidioplasty with implantation of a semi-rigid prosthesis, including updated surgical outcomes, as well as motivations, sexuality, and urinary function.
Methods
Surgical care
Individual care was carried according to the 7th version of Standards of Care of the World Professional Association for Transgender Health (WPATH) (Coleman et al., Citation2012). In our university hospital the different techniques for masculinizing GGAS as well as the associated advantages and disadvantages are discussed with transgender men during several consultations. The techniques available are metoidioplasty, supra-pubic pre-expanded phalloplasty (Terrier et al., Citation2020), radial forearm free flap phalloplasty, anterolateral thigh flap phalloplasty, and latissimus dorsi flap phalloplasty. Since 2017, the ZSI®100D4 (EC certificate no.15749) has been approved by the medical device departments of our institution and was proposed as an option to individuals seeking a metoidioplasty procedure, after an explanation of its theoretical advantages and potential complications. Metoidioplasty and implantation of the prosthesis were usually performed during the same surgical procedure but could also be considered during a second stage.
The surgical technique consisted firstly in the dissection of the clitoris for its complete releasing. If requested, a vaginectomy could be performed by vaporization and circular closure at the same time. Urethral lengthening was usually performed combining an onlay vaginal graft harvested during the vaginectomy and two labia minora flaps, one shaped in a ring flap and the other used for ventral closure. The prostheses were implanted following usual steps of semi-rigid penile prosthesis implantation (bilateral cavernotomy, corpus cavernosum dilatation, prosthesis implantation, closure). Prosthesis implantation was performed before urethral reconstruction and placement of the vaginal graft to prevent contamination. Scrotoplasty using two Martius labial fat pad could also be associated at the same operative time. A complete description of the technique and postoperative management has been described elsewhere (Neuville et al., Citation2021).
Data collection
All individuals who underwent a metoidioplasty with implantation of a semi-rigid prosthesis (ZSI®100D4) during August 2017 and January 2021 and who had at least 1 year of follow-up were included. General and surgical characteristics (including surgical complications graded according to the Clavien-Dindo classification (Clavien-Dindo et al., Citation2009)) were retrospectively collected from the medical files. All those included were contacted by telephone between November 2020 and May 2022 and invited to answer the study questionnaire. The latter could be filled out either during a telephone interview or after a routine consultation by an investigator who was not the surgeon of the interviewed individual.
This post-operative questionnaire was developed for the purpose of the study (supplemental Appendix 1). It was composed of 3 sections organized chronologically and corresponding to the pre-, per- and post-operative periods. The pre-operative section explored the motivations with two open-ended questions, as well as the importance of voiding in a standing position, and satisfaction regarding genitals and sexual life using a 5-point Likert scale. The per-operative section analyzed the pain with a 5-point Likert scale and the true length of work leave. The post-operative section explored satisfaction with genitals and sexual life, sensitivity, and frequency of orgasm using a 5-point Likert scale; an open-ended question explored the types of sexual activities that involve genitals engaged in. The post-operative section also included the Self-esteem and relationship (SEAR) questionnaire (Cappelleri et al., Citation2004), that provides a 0–100 score for four subscales (sexual relationship, confidence, self-esteem, overall relationship) and the total score; 0 being the lowest score and 100 the highest. Post-operative urinary function was explored by one open-ended question on the position for usual voiding, comfort when urinating in public restrooms using a 5-point Likert scale, and four questions regarding delay, intermittency, lagging drops and spraying using a 5-point frequency scale from “never” to “always.” Three of these four questions were extracted from the Lower Urinary Tract Symptom (LUTS)-score that has already been used in the urinary evaluation after phalloplasty (Paganelli et al., Citation2023). A question regarding spraying was added owing to the frequency of this reported in the metoidioplasty literature (Djordjevic, Citation2018; Djordjevic et al., Citation2019). The post-operative section also included open-ended questions regarding the advantages and disadvantages of the prosthesis and any regrets the patient may have.
Data analysis
A descriptive analysis of the quantitative data was conducted; continuous variables were reported using median [IQR], and categorical variables using number (%). The qualitative data from the open-ended questions in the questionnaire were analyzed using an inductive approach. No themes were developed considering the small sample size and the rather specific questions, but efforts were made to report quotations that directly shared the voices of the individuals who underwent the surgical procedure.
Ethics
This study is part of a larger one evaluating phallus reconstruction in our center (ClinicalTrials.gov Identifier: NCT04314141, ID-IRB:2020-A00076-33). All individuals gave informed consent. The study was conducted in accordance to the ethical principles of trans-related research (Adams et al., Citation2017; Vincent, Citation2018).
Results
General characteristics and surgical outcomes
Twenty-one individuals were included and followed-up for a median [IQR] 20 months [13; 24]. The included population was young (median [IQR] age at surgery of 33 [29; 41]) and had a median [IQR] duration of 6 [4; 8] years of hormonotherapy before the metoidioplasty procedure (). All (n = 21; 100%) individuals previously had an ovariohysterectomy. Almost all individuals (n = 19; 91%) had a scrotoplasty, 16 (84%) during the same procedure, and 3 (16%) during an additional procedure. No testicular prosthesis was implanted during scrotoplasty.
Table 1. General and surgical characteristics.
Most individuals (n = 13; 62%) experienced a post-operative complication, the most frequent was wound dehiscence (n = 6; 29%) often situated at the junction of the 2 scrotoplasty flap. There was 1 major complication (5%; grade 3b); a post-operative hematoma that needed surgical evacuation. The 3 urinary fistula (14%) were managed conservatively (grade 2; ) with a prolonged urinary diversion, leading to an extended work leave in those cases (median [IQR] duration of work leave of 30 [30; 90] days).
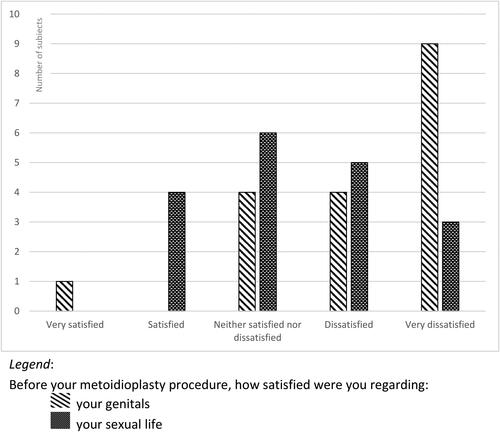
Motivations
The post-operative questionnaire was completed by 18 patients (86%), 3 were unreachable at time of the study. To the open-ended question “why did you chose this type of reconstructive surgery,” the main cited answers were a surgery associated with fewer complications than a phalloplasty procedure (n = 10/18; 56%), and the preservation of sensitivity (n = 5; 28%). To the open-ended question “what were your expectations regarding the prosthesis,” 16 individuals (89%) cited the theoretical advantages presented during the pre-operative consultation (i.e. a stake to support the metoidioplasty and the possibility to limit post-operative shrinkage), without expectations unlikely to be fulfilled as notably, ability for penetrative intercourse or length augmentation. Thirteen (72%) individuals reported being dissatisfied or very dissatisfied with their genitals before the metoidioplasty procedure (). Voiding in a standing position was reported as important or very important for 13 (72%), moderately important for 1 (6%), and of little importance for 4 (22%) individuals.
I was looking for the satisfaction of having male genitalia, even a little one.
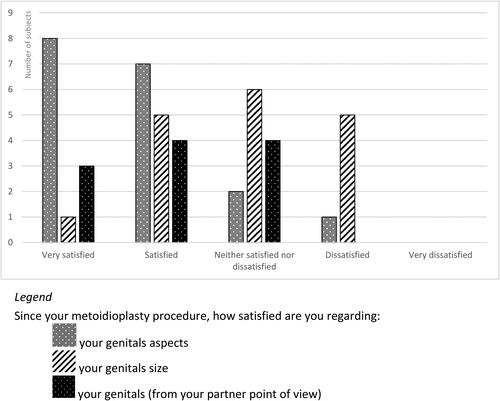
Regrets and feedbacks
The satisfaction regarding overall genital aspect was favorable as 15 (83%) individuals reporting being very satisfied or satisfied; 5 (28%) reported being dissatisfied with the size of their genitals (). To the question “do you have any regrets regarding your surgical procedure,” 16 (89%) answered not at all, 1 (6%) no, and 1 (6%) individual a lot. To the open-ended question “according to you, what are the advantages and disadvantages of the prosthesis,” 3 (17%) mentioned the pain as a disadvantage, and 8 (44%) mentioned the enhancement of voiding.
I fell pain during yoga.
It helps to avoid putting it [urinating] all over the place.
Sexuality
Eight (44%) individuals reported being dissatisfied or very dissatisfied with their sex life before the metoidioplasty procedure (). There were 16 (89%) who were sexually active and 11 (61%) were engaged in a sexual relationship. The median [IQR] total SEAR score was 92 [91; 97], composed of a very high SEAR Self-esteem score (median [IQR] of 100 [100; 100]), and a high SEAR Sexual Relationship (85 [0; 89]) and Overall Relationship scores (100 [0; 100]), despite a score of 0 for the individuals who were not engaged in a sexual relationship. Among the 16 individuals who reported to be sexually active, 12 (75%) reported reaching orgasm always or frequently, and 4 (25%) never or rarely. Among the 11 individuals who reported sexual relationships, the sexual activities reported involved friction (n = 11; 100%), penetration (n = 2; 18%) and receiving fellatio (n = 8; 73%).
The prosthesis allows, among others, fellatio, penetration, different positions… Considering the length I don’t risk hurting my partner! But it makes me discover a new sexuality since I no longer need to use a strap-on dildo to have pleasure.
Genital sensitivity since the metoidioplasty procedure was reported as more sensitive for 10 (56%), a lot more sensitive for 1 (6%), no difference for 5 (28%), and less sensitive for 2 (11%) individuals.
Urinary function
The reported urinary symptoms of delay, intermittency, lagging drops and spraying were mostly reported to occur never or rarely (). To the question “in which position do you usually void,” 5 (28%) answered sitting, 9 standing (50%), 3 (17%) either sitting or standing, and 1 (6%) standing with the help of a urination device. To the question “how comfortable are you for urinating in public restrooms,” 5 (28%) answered very comfortable, 3 (17%) comfortable, 3 (17%) neither comfortable nor uncomfortable, 4 (22%) uncomfortable, and 3 (17%) very uncomfortable. All 8 individuals who were comfortable or very comfortable to urinate in public restrooms reported voiding in a standing position.
Discussion
General characteristics and surgical outcomes
The present study includes a larger sample and has a longer follow-up than the initial report of ZSI®100D4 prosthesis implantation during a metoidioplasty (Neuville et al., Citation2021). No complication associated with the prosthesis was reported (no infection nor erosion), supporting the safety of implantation. However, complications of the procedure were frequent; wound dehiscence remained the most frequent complication, still minor, and only one patient experienced a major complication (surgical evacuation of a hematoma).
Motivations
The main motivation cited for undergoing a metoidioplasty was a less morbid surgery compared to a phalloplasty procedure, noteworthy a negative motivation aiming to avoid rather to gain, which highlights the limitations of currently available procedures for masculinizing GGAS; the second was preservation of the sensitivity, which is consistent with the main priorities of transmasculine individuals seeking genital affirmation (Ganor et al., Citation2019). In addition, individuals who opted for a prosthesis implantation did not have expectations unlikely to be fulfilled, suggesting that the pre-operative counseling was effective but also underlining the importance of this phase for new medical devices, for which a lack of data and the potential associated complications must not be concealed by the novelty appeal.
Regrets and feedbacks
Satisfaction regarding overall aspect of genitals was highly favorable, consistently with that reported elsewhere for metoidioplasty (Bizic et al., Citation2019; Djordjevic et al., Citation2019). The only individual who reported being dissatisfied with the aspect of his genitals and having regrets was the one who had to undergo surgical revision and suffered from scar retraction. This single case did not allow us to analyze the factors associated with dissatisfaction regarding genitals, but is coherent with the association between dissatisfaction and self-reported complications reported in a larger study from the European Network on the Investigation of Gender Incongruence (van de Grift et al., Citation2018).
Sexuality
Evaluating the outcomes of metoidioplasty requires an analysis of the post-operative sexual well-being, which may comprehend several debatable criteria that vary among the few studies reporting such analysis (Özer et al., Citation2022). This debate applies to the criteria of the present study, but we believe that the analysis of a graded sexual satisfaction, orgasm frequency, perceived genital sensitivity along with the type of sexual activities and the SEAR questionnaire provides a comprehensive evaluation of the sexual outcomes. Sexual satisfaction is one of the most common criteria used for the evaluation of the sexual outcomes (Özer et al., Citation2022). It has been consistently reported as high after a metoidioplasty, be this in one of the rare longitudinal studies before and after GGAS (van de Grift et al., Citation2017), in studies that do not provide of the method used for evaluation (Stojanovic et al., Citation2017; Vukadinovic et al., Citation2014), and in the present study that found a high SEAR sexual relationship score. However, this constant high sexual satisfaction must be considered in the light of the important pre-operative dissatisfaction (van de Grift et al., Citation2016), likewise reported herein, but also in the light of the expectations of the individuals who undergo metoidioplasty (McClelland, Citation2010). Although the design of the present study did not allow us to provide an in-depth analysis of the sexual expectations, preservation of the erogenous sensation was reported as a frequent motivation for the procedure and overall individuals reported favorable self-perceived genital sensitivity, consistent with that reported elsewhere (Bizic et al., Citation2019), which may explain the sexual satisfaction found. In addition, the ability to attain orgasm has been reported as associated with sexual satisfaction (Wierckx et al., Citation2011) and even if the small number of subjects included herein did not allow to test such an association, a majority of the sexually active individuals reported herein not having challenges to reach orgasm. A more general note is that satisfaction is calculated among those who are sexually active and that herein this represented the majority of patients, indicating that this was obtained by most individuals who underwent the surgical procedure.
The expected erectile capacity of genitals after metoidioplasty was largely unexplored before the study reported by Khorrami et al. (Citation2022) that investigated erectile and sexual function in 15 individuals who had a metoidioplasty, as well as their attitudes toward using erectile dysfunction medication; 80% of them faced challenges with their ability to achieve or maintain erections. The use of erectile medication after metoidioplasty reported by Khorrami et al. raised the question of what the expected erectile function of a metoidioplasty is. The ZSI®100D4, which was initially designed for stiffening and increasing protrusion for the neo-phallus to limit post-operative shrinking and enhance handling, may also have benefits as a pro-erectile device (although it limits the possibility of pro-erectile medication by compromising all corpus cavernosum tissue). These benefits in erectile function may explain, at least in part, the slightly greater proportion of penetrative intercourse reported in the present study compared to that found (<2%) in the largest studies evaluating this outcome (Stojanovic et al., Citation2017; Takamatsu & Harashina, Citation2009); friction was nevertheless the most frequent reported sexual activity herein. The report of pro-erectile medication use after metoidioplasty (Khorrami et al., Citation2022) raises the question of a possible stepwise approach for prosthesis implantation, for example after failure of pro-erectile medication as it is commonly done in cis-men. This approach is currently possible, acknowledging the fact that it would lose the potential benefit of the limitation of post-operative shrinking.
Urinary function
Considering urinary outcomes, we report a low rate of fistulas and no stenosis, similar to that reported elsewhere for metoidioplasty (Djordjevic et al., Citation2019; Kjölhede et al., Citation2019). However, although fistulas reported were all managed without surgical revision, in such cases work leave was extended for the duration of suprapubic urinary diversion. These low rates of urinary complications must be interpreted carefully considering that the follow-up herein was a maximum 2 years. For instance, a study focusing on urethral complications after metoidioplasty with a median follow-up of nearly 4 years reported fistulas in 36.5% of patients and stenosis in 18.9% (Waterschoot et al., Citation2021), but it is of note that urethral lengthening in metoidioplasty corresponds to the pars fixa in phalloplasty urethral construction for which urethral complications have been reported in less than 10% after a mean 5 years follow-up (Paganelli et al., Citation2023). In addition, functional urinary outcomes were overall favorable. Obstructive symptoms were less frequently reported than in urethral lengthening in phalloplasty (Paganelli et al., Citation2023), supporting the difference in outcomes in terms of urinary function between these techniques (Ortengren et al., Citation2022). It is also of note that we evaluated the voiding position with an open-ended question of usual habit (“in which position do you usually void”), rather than the ability of individuals to urinate standing as it is the case in the literature (Ortengren et al., Citation2022). This approach may have led to different outcomes, as only half of the individuals reported usually voiding while standing (and one individual reported using a urinary device for standing urination) compared to a 100% sometimes reported (Bizic et al., Citation2019). In addition, less than half reported being comfortable in public restrooms, which, taken together, illustrates that functional outcomes require more subtle evaluation than that is currently the case.
Limitations
This study presents some limitations, including the retrospective collection of the surgical data. We also used a non-validated questionnaire reflecting the authors experience in GGAS, but which could have been enhanced by a co-construction of the evaluation tools. In addition, some questions concerned the pre-operative period, and the answers may be limited by memory bias. Also, the semi-rigid prosthesis was implanted during the metoidioplasty procedure, we were therefore not able to analyze the benefits associated with the prosthesis separated from those associated with the metoidioplasty.
However, we report a complete surgical analysis of an innovative metoidioplasty procedure, along with a patient-centered comprehensive evaluation, attempting to reflect a more realistic and practical analysis of GGAS outcomes.
Conclusion
Implantation of a semi-rigid prosthesis in a metoidioplasty seems to be a safe procedure, with no reported complication related to the prosthesis. Satisfaction regarding genitals, sexual, and urinary function were overall favorable. The next step is to conduct a comparative study to determine more precisely the benefits directly attributable to the prosthesis.
wijt_a_2279273_sm7587.docx
Download MS Word (22 KB)Disclosure statement
Paul Neuville and Nicolas Morel-Journal are consultant for Zephyr Surgical Implants.
Additional information
Funding
References
- Adams, N., Pearce, R., Veale, J., Radix, A., Castro, D., Sarkar, A., & Thom, K. C. (2017). Guidance and ethical considerations for undertaking transgender health research and institutional review boards adjudicating this research. Transgender Health, 2(1), 165–175. https://doi.org/10.1089/trgh.2017.0012
- Al-Tamimi, M., Pigot, G., Elfering, L., Özer, M., Haseth, K. D., Grift, T. V. D., Mullender, M., Bouman, M.-B., & Sluis, W. V. D. (2020). Genital gender-affirming surgery in transgender men in The Netherlands from 1989 to 2018: The evolution of surgical care. Plastic and Reconstructive Surgery, 145(1), 153e–161e. https://doi.org/10.1097/PRS.0000000000006385
- Bizic, M. R., Stojanovic, B., Joksic, I., & Djordjevic, M. L. (2019). Metoidioplasty. The Urologic Clinics of North America, 46(4), 555–566. https://doi.org/10.1016/j.ucl.2019.07.009
- Cappelleri, J. C., Althof, S. E., Siegel, R. L., Shpilsky, A., Bell, S. S., & Duttagupta, S. (2004). Development and validation of the Self-Esteem And Relationship (SEAR) questionnaire in erectile dysfunction. International Journal of Impotence Research, 16(1), 30–38. https://doi.org/10.1038/sj.ijir.3901095
- Clavien, P. A., Barkun, J., de Oliveira, M. L., Vauthey, J. N., Dindo, D., Schulick, R. D., de Santibañes, E., Pekolj, J., Slankamenac, K., Bassi, C., Graf, R., Vonlanthen, R., Padbury, R., Cameron, J. L., & Makuuchi, M. (2009). The Clavien-Dindo classification of surgical complications: Five-year experience. Annals of Surgery, 250(2), 187–196. https://doi.org/10.1097/SLA.0b013e3181b13ca2
- Coleman, E., Bockting, W., Botzer, M., Cohen-Kettenis, P., DeCuypere, G., Feldman, J., Fraser, L., Green, J., Knudson, G., Meyer, W. J., Monstrey, S., Adler, R. K., Brown, G. R., Devor, A. H., Ehrbar, R., Ettner, R., Eyler, E., Garofalo, R., Karasic, D. H., … Zucker, K. (2012). Standards of care for the health of transsexual, transgender, and gender-nonconforming people, version 7. International Journal of Transgenderism, 13(4), 165–232. https://doi.org/10.1080/15532739.2011.700873
- Djordjevic, M. L. (2018). Novel surgical techniques in female to male gender confirming surgery. Translational Andrology and Urology, 7(4), 628–638. https://doi.org/10.21037/tau.2018.03.17
- Djordjevic, M. L., Stojanovic, B., & Bizic, M. (2019). Metoidioplasty: Techniques and outcomes. Translational Andrology and Urology, 8(3), 248–253. https://doi.org/10.21037/tau.2019.06.12
- Ganor, O., Taghinia, A. H., Diamond, D. A., & Boskey, E. R. (2019). Piloting a genital affirmation surgical priorities scale for trans masculine patients. Transgender Health, 4(1), 270–276. https://doi.org/10.1089/trgh.2019.0038
- Hadj-Moussa, M., Agarwal, S., Ohl, D. A., & Kuzon, W. M. (2019). Masculinizing genital gender confirmation surgery. Sexual Medicine Reviews, 7(1), 141–155. https://doi.org/10.1016/j.sxmr.2018.06.004
- Hage, J. J. (1996). Metaidoioplasty: An alternative phalloplasty technique in transsexuals. Plastic and Reconstructive Surgery, 97(1), 161–167. https://doi.org/10.1097/00006534-199601000-00026
- Jacobsson, J., Andréasson, M., Kölby, L., Elander, A., & Selvaggi, G. (2017). Patients’ priorities regarding female-to-male gender affirmation surgery of the genitalia-a pilot study of 47 patients in Sweden. The Journal of Sexual Medicine, 14(6), 857–864. https://doi.org/10.1016/j.jsxm.2017.04.005
- Jolly, D., Wu, C. A., Boskey, E. R., Taghinia, A. H., Diamond, D. A., & Ganor, O. (2021). Is clitoral release another term for metoidioplasty? A systematic review and meta-analysis of metoidioplasty surgical technique and outcomes. Sexual Medicine, 9(1), 100294–100294. https://doi.org/10.1016/j.esxm.2020.100294
- Khorrami, A., Kumar, S., Bertin, E., Wassersug, R., O’Dwyer, C., Mukherjee, S., Witherspoon, L., Mankowski, P., Genoway, K., & Kavanagh, A. G. (2022). The sexual goals of metoidioplasty patients and their attitudes toward using PDE5 inhibitors and intracavernosal injections as erectile aids. Sexual Medicine, 10(3), 100505–100508. https://doi.org/10.1016/j.esxm.2022.100505
- Kjölhede, A., Cornelius, F., Huss, F., & Kratz, G. (2019). Metoidioplasty and groin flap phalloplasty as two surgical methods for the creation of a neophallus in female-to-male gender-confirming surgery: A retrospective study comprising 123 operated patients. JPRAS Open, 22, 1–8. https://doi.org/10.1016/j.jpra.2019.07.003
- McClelland, S. I. (2010). Intimate justice: A critical analysis of sexual satisfaction: intimate justice. Social and Personality Psychology Compass, 4(9), 663–680. https://doi.org/10.1111/j.1751-9004.2010.00293.x
- Neuville, P., Carnicelli, D., Paparel, P., Ruffion, A., & Morel-Journel, N. (2021). Metoidioplasty with implantation of a specific semirigid prosthesis. The Journal of Sexual Medicine, 18(4), 830–836. https://doi.org/10.1016/j.jsxm.2021.01.177
- Ortengren, C. D., Blasdel, G., Damiano, E. A., Scalia, P. D., Morgan, T. S., Bagley, P., Blunt, H. B., Elwyn, G., Nigriny, J. F., Myers, J. B., Chen, M. L., & Moses, R. A. (2022). Urethral outcomes in metoidioplasty and phalloplasty gender affirming surgery (MaPGAS) and vaginectomy: A systematic review. Translational Andrology and Urology, 11(12), 1762–1770. https://doi.org/10.21037/tau-22-174
- Özer, M., Pigot, G. L. S., Bouman, M.-B., van de Grift, T. C., Elfering, L., van Mello, N. M., Al-Itejawi, H. H. M., Buncamper, M. E., & Mullender, M. G. (2018). Development of a decision aid for genital gender-affirming surgery in transmen. The Journal of Sexual Medicine, 15(7), 1041–1048. https://doi.org/10.1016/j.jsxm.2018.04.644
- Özer, M., Toulabi, S. P., Fisher, A. D., T’Sjoen, G., Buncamper, M. E., Monstrey, S., Bizic, M. R., Djordjevic, M., Falcone, M., Christopher, N. A., Simon, D., Capitán, L., & Motmans, J. (2022). ESSM position statement “sexual wellbeing after gender affirming surgery.” Sexual Medicine, 10(1), 100471–100471. https://doi.org/10.1016/j.esxm.2021.100471
- Paganelli, L., Morel-Journel, N., Carnicelli, D., Ruffion, A., Boucher, F., Maucort-Boulch, D., Paparel, P., Terrier, M., & Neuville, P. (2023). Determining the outcomes of urethral construction in phalloplasty. BJU International, 131(3), 357–366. https://doi.org/10.1111/bju.15915
- Parker, A., Blasdel, G., Kloer, C., Kimberly, L., Shakir, N., Robinson, I., Bluebond-Langner, R., & Zhao, L. C. (2022). Postulating penis: What influences the interest of transmasculine patients in gender affirming penile reconstruction techniques? The Journal of Sexual Medicine, 19(2), 385–393. https://doi.org/10.1016/j.jsxm.2021.10.013
- Preto, M., Blecher, G., Timpano, M., Gontero, P., & Falcone, M. (2020). The Frontier of Penile Implants in Phalloplasty: Is the ZSI 475 FTM what we have been waiting for? International Journal of Impotence Research, 33(7), 779–783. https://doi.org/10.1038/s41443-020-00396-2
- Scalia, P., Tighe, K. M., Elwyn, G., Bagley, P. J., Blunt, H. B., Boh, B., Walters, O. C., & Moses, R. A. (2021). A systematic review of decision aids for gender affirming therapy. Translational Andrology and Urology, 10(6), 2574–2582. https://doi.org/10.21037/tau-20-1000
- Stojanovic, B., Bizic, M., Bencic, M., Kojovic, V., Majstorovic, M., Jeftovic, M., Stanojevic, D., & Djordjevic, M. L. (2017). One-stage gender-confirmation surgery as a viable surgical procedure for female-to-male transsexuals. The Journal of Sexual Medicine, 14(5), 741–746. https://doi.org/10.1016/j.jsxm.2017.03.256
- Takamatsu, A., & Harashina, T. (2009). Labial ring flap: A new flap for metaidoioplasty in female-to-male transsexuals. Journal of Plastic, Reconstructive & Aesthetic Surgery: JPRAS, 62(3), 318–325. https://doi.org/10.1016/j.bjps.2008.11.038
- Terrier, M., Morel-Journel, N., Carnicelli, D., Ruffion, A., Terrier, J.-E., Maucort-Boulch, D., Paganelli, L., & Neuville, P. (2020). Suprapubic phalloplasty in transmen: Surgical results and critical review. International Journal of Impotence Research, 33(7), 754–761. https://doi.org/10.1038/s41443-021-00426-7
- van de Grift, T. C., Cohen-Kettenis, P. T., Steensma, T. D., De Cuypere, G., Richter-Appelt, H., Haraldsen, I. R. H., Dikmans, R. E. G., Cerwenka, S. C., & Kreukels, B. P. C. (2016). Body satisfaction and physical appearance in gender dysphoria. Archives of Sexual Behavior, 45(3), 575–585. https://doi.org/10.1007/s10508-015-0614-1
- van de Grift, T. C., Pigot, G. L. S., Boudhan, S., Elfering, L., Kreukels, B. P. C., Gijs, L. A. C. L., Buncamper, M. E., Özer, M., van der Sluis, W., Meuleman, E. J. H., Bouman, M.-B., & Mullender, M. G. (2017). A longitudinal study of motivations before and psychosexual outcomes after genital gender-confirming surgery in transmen. The Journal of Sexual Medicine, 14(12), 1621–1628. https://doi.org/10.1016/j.jsxm.2017.10.064
- van de Grift, T. C. v d., Elaut, E., Cerwenka, S. C., Cohen-Kettenis, P. T., & Kreukels, B. P. C. (2018). Surgical satisfaction, quality of life, and their association after gender-affirming surgery: A follow-up study. Journal of Sex & Marital Therapy, 44(2), 138–148. https://doi.org/10.1080/0092623X.2017.1326190
- Vincent, B. W. (2018). Studying trans: Recommendations for ethical recruitment and collaboration with transgender participants in academic research. Psychology & Sexuality, 9(2), 102–116. https://doi.org/10.1080/19419899.2018.1434558
- Vukadinovic, V., Stojanovic, B., Majstorovic, M., & Milosevic, A. (2014). The role of clitoral anatomy in female to male sex reassignment surgery. TheScientificWorldJournal, 2014, 437378–437377. https://doi.org/10.1155/2014/437378
- Walton, A. B., Hellstrom, W. J. G., & Garcia, M. M. (2021). Options for masculinizing genital gender affirming surgery: A critical review of the literature and perspectives for future directions. Sexual Medicine Reviews, 9(4), 605–618. https://doi.org/10.1016/j.sxmr.2021.07.002
- Waterschoot, M., Hoebeke, P., Verla, W., Spinoit, A.-F., Waterloos, M., Sinatti, C., Buncamper, M., & Lumen, N. (2021). Urethral complications after metoidioplasty for genital gender affirming surgery. The Journal of Sexual Medicine, 18(7), 1271–1279. https://doi.org/10.1016/j.jsxm.2020.06.023
- Wierckx, K., Van Caenegem, E., Elaut, E., Dedecker, D., Van de Peer, F., Toye, K., Weyers, S., Hoebeke, P., Monstrey, S., De Cuypere, G., & T’Sjoen, G. (2011). Quality of life and sexual health after sex reassignment surgery in transsexual men. The Journal of Sexual Medicine, 8(12), 3379–3388. https://doi.org/10.1111/j.1743-6109.2011.02348.x