Abstract
This study explored the expression of high mobility group box 1 protein (HMGB1) expression in patients with sepsis and its effects on immune function and prognosis. Patients with sepsis (n = 112) were divided into the mild group (MG, n = 59) and severe group (SG, n = 53) according to the disease severity of sepsis. Fifty healthy people who came to our hospital for physical examination at the same time served as the control group (CG). Serum HMGB1, CD4+, and CD8+ expression levels and CD4+/CD8+ ratios were compared between the three groups. The correlation between serum HMGB1 expression, APACHE II score, and MODS score was analyzed. Serum HMGB1 and CD8+ expressions were lower in the CG group than the values in the MG and SG groups, whereas the CD4+ expression and CD4+/CD8+ ratio were higher. Serum HMGB1 expression in sepsis patients was positively correlated with the APACHEII and MODS scores. In addition, the 28-day survival rate of the MG was higher than that of the SG. HMGB1 was highly expressed in the serum of patients with sepsis. HMGB1 expression was positively associated with the severity of sepsis. In addition, HMGB1 was closely related to the immune function and prognosis of patients with sepsis.
KEYWORDS:
Introduction
Sepsis has the characteristics of complexity, change, and rapid disease progress, which can seriously threaten human health and survival (Hotchkiss and Karl Citation2003; Fan et al. Citation2014). Due to the complexity of sepsis, its specific pathogenesis is still unclear. However, sepsis has been associated with excessive release of inflammatory mediators and immune dysfunction, as well as tissue damage and gene polymorphism (Mishnev et al. Citation2016; Shankar-Hari Citation2017). Sepsis is mainly treated by infection control, hormone therapy, and endotoxin targeted therapy, but the mortality of patients with sepsis has not been effectively reduced (Raghu et al. Citation2017). Even with the ongoing improvements in medical science and technology, sepsis remains a difficult problem to overcome (Park et al. Citation2013).
High mobility group box 1 protein (HMGB1) is a nuclear protein that is ubiquitous in eukaryotic cells (Muller et al. Citation2012). HMGB1 plays a very important and critical role in the occurrence and development of sepsis (Stevens et al. Citation2017). One of the main causes of death during sepsis is tissue perfusion dysfunction induced by immune system disorders. This phenomenon is caused by the hyperactivation of immune cells induced by inflammatory mediators, such as HMGB1, which causes immune cells to lose their ability to distinguish between infected cells and normal cells, ultimately leading to immune disorders in patients (Cohen Citation2002).
Mice with sepsis have been treated with anti-HMGB1 (Lee et al. Citation2013), suggesting that HMGB1 may be a therapeutic target for septic shock. Although anti-HMGB1 has a good effect in the animal sepsis model, clinical research on HMGB1 targeted therapy is still in its infancy. To further explore the expression of HMGB1 in patients with sepsis and its effects on immune function and prognosis, the following investigations were conducted.
Materials and methods
General information
The study group comprised 112 patients with sepsis treated at the People's Hospital, Guangxi Zhuang Autonomous Region. They included 61 male patients and 51 female patients. The average age of all patients was (52.31 ± 4.27) years. According to the severity of sepsis, they were divided into a mild group (MG, n = 59) and a severe group (SG, n = 53). The control group (CG) comprised 50 healthy people who came to our hospital for physical examinations at the same time as the patients.
Concerning the inclusion criteria, the SG patients met the Rescue Sepsis Movement (SCC) 2012 Guidelines diagnostic criteria for sepsis (Levy et al. Citation2012). Exclusion criteria included malignant tumor disease, immune system disease, communication impairment, and/or cognitive dysfunction, lack of cooperation with participation requirements of the study. All patients and their families agreed to participate in the experiment and signed the informed consent form. This experiment was approved by the ethics committee of People's Hospital, Guangxi Zhuang Autonomous Region.
Indicator detection
In the early morning of the day after admission, 5 ml of fasting venous blood was drawn from each subject. After centrifugation, the serum HMGB1 level was measured by ELISA as dictated by the kit instructions. Next, the immune related cells were detected. Venous blood was treated with EDTA for anticoagulation, diluted with phosphate buffered saline, and 4 ml of lymphocyte separation solution was added to the diluted blood. The supernatant was then centrifuged at a speed of 2000 rpm for 30 min. After centrifugation, the supernatant was discarded, and the cell suspension was prepared. CD4-fluorescein isothiocyanate (FITC) and 20 µL of CD8-allophycocyanin (APC) monoclonal antibodies were added and incubated for 20 min at room temperature (RT) in the dark. Permeabilization solution (0.5 ml) was added and incubated for 30 min at RT in the dark. Finally, the supernatant was discarded and the cells were detected by flow cytometry.
Measurement outcomes
Serum HMGB1 was tested and compared among the three groups of subjects. CD4+ and CD8+ expression levels, and CD4+/CD8+ ratios of the three groups of subjects were compared. Patients with mild and severe sepsis were evaluated for Acute Physiologic Assessment and Chronic Health Evaluation II (APACHE II) (Sadaka et al. Citation2017) and Multiple Organ Dysfunction Score (MODS) (Guo et al. Citation2017). The correlation between serum HMGB1 expression and APACHE II and MODS scores was analyzed. (4) The 28-day survival rate of patients in the MG and SG was recorded and compared. The patients were divided into the survival group and the death group according to the patient survival. Serum HMGB1 expression was determined and compared between the two groups.
Statistical analyses
SPSS18.0 software (Boyi Zhixun (Beijing) Information Technology Co., Ltd.) was used for statistical analysis of the data. The measurement data were expressed using mean ± SD. The two groups were compared using an independent t-test. One-way analysis of variance was used for comparison between groups. The Least Significant Difference test was used for post-analysis, GraphPad Prism 6 software was used to draw the experimental images, and the Kaplan-Meier method was used for survival analysis. Differences with P < 0.05 were considered statistically significant.
Results
General data comparison
There were no significant differences in gender, age, and body mass index between the three groups (P > 0.05). There were no significant differences in heart rate, respiration, and disease causes in patients with different degrees of sepsis (P > 0.05). However, the expression levels of serum leukocyte and C-reactive protein of sepsis patients in the study group were significantly higher than that of the CG group (P < 0.05). The serum leukocyte and C-reactive protein expression levels were significantly higher in the SG group than the levels in the MG group (P < 0.05) (Table ).
Table 1. Comparison of general data.
Serum HMGB1 expression in the three groups of subjects
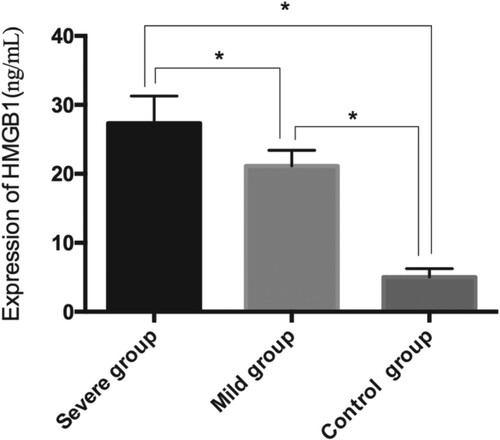
The expression of serum HMGB1 in sepsis patients was 21.15 ± 2.26 ng/mL in MG patients, 27.36 ± 3.91 ng/mL in SG patients, and 5.02 ± 1.24 ng/mL in CG patients. Serum HMGB1 expression in CG patients was lower than that in the MG and SG patients (P < 0.05). Serum HMGB1 expression was lower in MG patients than the level in SG patients (P < 0.05) (Figure ).
Serum CD4+ and CD8+ expression and CD4+/CD8+ ratio in MG, SG, and CG patients
Serum CD4+ and CD8+ expression and the CD4+/CD8+ ratios in the MG patients was 32.5 ± 3.6 ng/mL, 25.2 ± 3.8 ng/mL, and 1.29 ± 0.11, respectively. The respective values in the SG patients were 27.7 ± 4.8 ng/mL, 27.5 ± 3.5 ng/mL, and 1.01 ± 0.12. The respective values in the CG patients were 37.3 ± 4.1 ng/mL, 22.2 ± 3.8 ng/mL, and 1.68 ± 0.10, respectively. The expression of CD4+ in the MG and SG patients was lower than that in the CG patients. The expression of CD8+ and the CD4+/CD8+ ratio were higher in the MG and SG patients than that in the CG patients (both P < 0.05). The expression of CD4+ and CD8+ in SG patients was lower and higher, respectively, than that in MG patients. The CD4+/CD8+ ratio was also lower than that in the MG (P < 0.05) (Table ).
Table 2. Immune related indicators of the three groups of patients.
Comparison of APACHE II and MODS scores in MG and SG patients
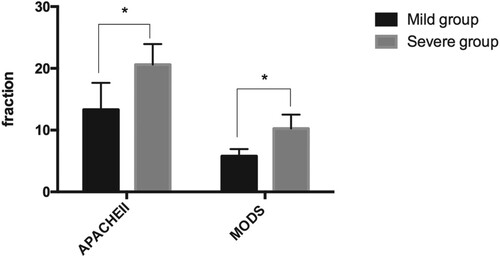
The APACHE II score and the MODS score was 13.32 ± 4.35 and 5.79 ± 1.15, respectively, in the MG patients and 20.62 ± 3.31 and 10.27 ± 2.23, respectively, in the SG patients. MG patients had lower APACHE II scores and MODS scores than SG patients (both P < 0.05) (Figure ).
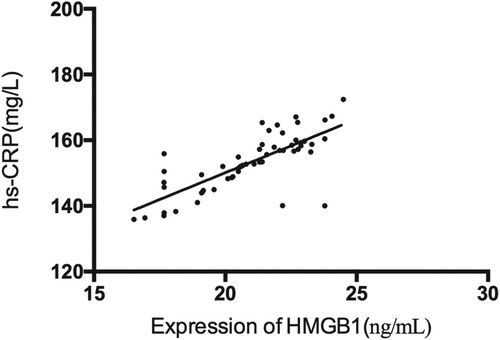
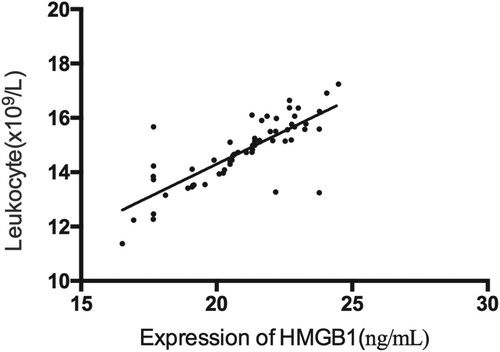
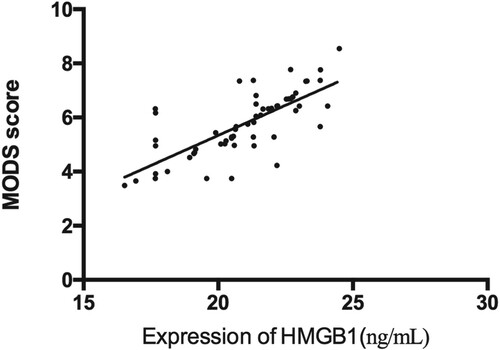
Correlation analysis of serum HMGB1 expression, APACHE II score, MODS score and inflammatory factors in patients with sepsis
Serum HMGB1 expression in sepsis patients was positively correlated with the APACHE II score (r = 0.681, P < 0.05) and MODS score (r = 0.746, P < 0.05). Serum HMGB1 expression in sepsis patients was positively correlated with the serum leukocyte (r = 0.758, P < 0.05) and hs-CRP (r = 0.786, P < 0.05) (Figures ).
Figure 3. Correlation analysis between serum HMGB1 expression and APACHE II score in patients with sepsis. There was a positive correlation between serum HMGB1 expression and APACHE II score in patients with sepsis (r = 0.681, P < 0.05).
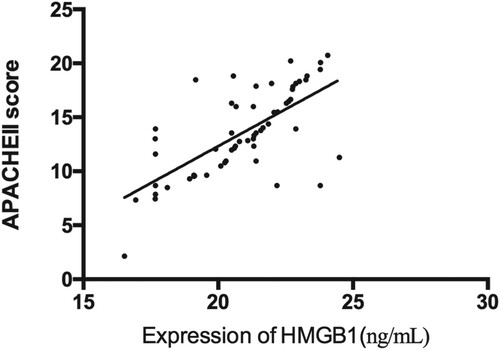
Figure 4. Correlation analysis between serum HMGB1 expression and MODS score in patients with sepsis. There was a positive correlation between serum HMGB1 expression and MODS score in patients with sepsis (r = 0.746, P < 0.05).
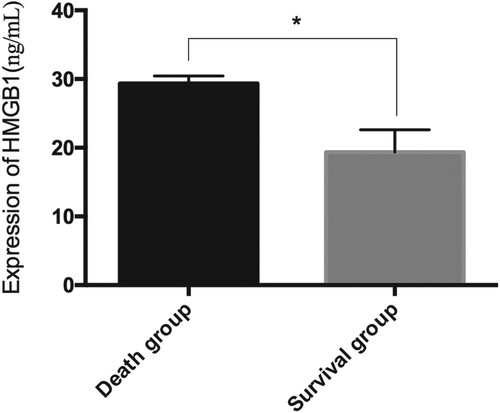
Relationship between serum HMGB1 expression and survival rate in patients with sepsis
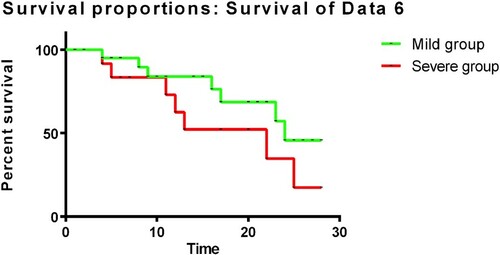
Within 28 days after admission, 68 patients died and 44 survived. Serum HMGB1 expression level was 29.35 ± 1.09 ng/mL in those who died and was significantly lower (19.36 ± 3.27) ng/mL in those who survived (P < 0.05). In total, 20 MG and 43 SG patients died. Their 28-day survival rate was 57.53% and 18.87%, respectively. The 28-day survival rate was significantly higher in the MG patients compared to the SG patients (P < 0.05). (Figures and )
Discussion
As an infectious disease, sepsis is usually characterized by the presence of bacteria or infected lesions associated with high incidence and high mortality (Dellinger et al. Citation2008; Freund et al. Citation2017). Despite many clinical efforts, the efficacy of the anti-inflammatory treatment of sepsis remains poor and the complication and mortality rates continue to increase (Tiruvoipati et al. Citation2012). HMGB1 has attracted increasing attention in recent years as a late inflammatory mediator in the pathophysiology of patients with sepsis (Wang et al. Citation2017). A previous study (Lan et al. Citation2017) indicated that HMGB1 is released 16–24 h after sepsis onset. The late release time and extended duration of HMGB1 provides an abundant time window for clinical treatment, and is thus likely to become a new target for sepsis treatment.
We found that serum HMGB1 expression was lower in CG patients than in MG and SG patients, and that serum HMGB1 expression was lower in MG patients than in SG patients. These observations suggest that HMGB1 expression in the serum of patients with sepsis is higher than that in healthy people, and that HMGB1 expression is progressively greater with the progressive severity of sepsis. The analysis of factors related to inflammation revealed that serum HMGB1 expression in patients with sepsis was positively correlated with the expressions of leukocyte and hs-CRP, which also indicates the aggravation of sepsis. In one study (An et al. Citation2018) HMGB1 expression in the serum of patients with sepsis was investigated. The authors reported that as sepsis worsened, serum HMGB1 expression increased, consistent with the present indication. However, the specific mechanism of HMGB1 expression in sepsis patients remains unclear. We speculate that increased HMGB1 expression may be related to factors, such as shift of bacterial endotoxin in patients under acute stress (Rhodes et al. Citation2017). Another study (Harris et al. Citation2012) found that HMGB1 levels in the liver, small intestine, and other tissues of sepsis patients was increased within 24 h after the onset of sepsis, indicating that HMGB1 expression was closely related to the organ function damage mediated by endotoxin. However, the specific underlying mechanism is unclear.
Because the occurrence and development of sepsis is closely related to the immune function of the body (Tipoe et al. Citation2018), we compared the immune function related indicators of the patients. CD4+ expression in MG and SG patients was lower than that in CG patients, whereas CD8+ expression was higher. The CD4+/CD8+ ratio in the MG and SG patients was also lower than that in CG patients. CD4+ expression in SG patients was lower than that in MG patients, whereas the CD8+ expression was higher in SG patients than the level in MG patient. The CD4+/CD8+ ratio was also lower than that in the MG. These observations suggested that the immune function of patients with sepsis was inhibited compared with that in healthy people. A previous study (Kragstrup et al. Citation2017) demonstrated that immune dysfunction is also one of the key factors in the pathogenesis of sepsis and is characterized by reduction in the number of immune cells and a decline in cell function. T lymphocytes play a very important role in the immune dysfunction of cells. T cells are further divided into CD4+ helper T lymphocytes and CD8+ cytotoxic T lymphocytes with a specific killing effect on the target cells, which respectively recognize antigen peptides on MHC class II and class I molecules. Therefore, the T lymphocyte response, as a critical link in the adaptive immune response, also increases the susceptibility of the body to sepsis and aggravates sepsis severity (Kasten et al. Citation2010; Unsinger et al. Citation2010). Generally, CD4+ and CD8+ will be maintained in a dynamic balance under normal circumstances, and the strength of cellular immune function can be reflected by their ratio (Chalmin et al. Citation2018). However, the relationship between HMGB1 and immune function has not been elaborated. To explore the relationship between the prognosis of patients with HMGB1 expression and sepsis, the APACHE II and MODS scores of the SG were compared, and the relationship between these scores and HMGB1 expression was analyzed. MG patients displayed lower APACHE II and MODS scores than SG patients. Serum HMGB1 expression and APACHE II and MODS scores were positively correlated in patients with sepsis. MG patients had lower APACHE II scores and MODS scores than those of SG patients.
Finally, the relationship between the survival rate and serum HMGB1 in patients with sepsis was explored. Serum HMGB1 expression was lower in survivors than in those who died. The 28-day survival rate was higher in the MG patients compared to the SG patients. These results suggested that HMGB1 expression in patients with sepsis was closely related to the prognosis. Many studies have used different methods to target HMGB1 in animal experiments, and most have achieved good results. Many animal experiments have shown that antagonism of HMGB1 can improve the symptoms of animal models and reduce mortality (Lan et al. Citation2017). These results indicate that HMGB1 and the prognosis of sepsis are closely related.
In summary, HMGB1 was found to be highly expressed in the serum of patients with sepsis and increased as the severity of sepsis increased. HMGB1 expression was also closely related to the immune function and prognosis of patients with sepsis, which may be a prognostic factor for sepsis patients and a new target for sepsis treatment. However, this study also has certain limitations. First, the relationship between the immune function and HMGB1 in patients with sepsis was not explored in detail, and the specific mechanism of action remains unclear. Secondly, due to the lack of relevant literature on anti-HMGB1 treatment in clinical trials, further verification is still needed regarding whether HMGB1 can be used as a prognostic factor for sepsis patients. These problems will be further explored to accurately explain the role of HMGB1 in sepsis and its mechanism.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- An S, Qin B, Lu G, Fan Y, Jia B. 2018. Effect of high mobility group protein B1 on the immune function of regulatory T cells. J Pract Med. 34(17):2912–2915.
- Chalmin F, Bruchard M, Vegran F, Ghiringhelli F. 2018. Regulation of T cell antitumor immune response by tumor induced metabolic stress. Cell Stress. 3(1):9–18. doi: https://doi.org/10.15698/cst2019.01.171
- Cohen J. 2002. The immunopathogenesis of sepsis. Nature. 420(6917):885–891. doi: https://doi.org/10.1038/nature01326
- Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R, Reinhart K, Angus DC, Brun-Buisson C, Beale R, et al. 2008. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008. Intensive Care Med. 34(1):17–60. doi: https://doi.org/10.1007/s00134-007-0934-2
- Fan L, Strasser-Weippl K, Li JJ, St Louis J, Finkelstein DM, Yu KD, Chen WQ, Shao ZM, Goss PE. 2014. Breast cancer in China. Lancet Oncol. 15(7):e279–e289. doi: https://doi.org/10.1016/S1470-2045(13)70567-9
- Freund Y, Lemachatti N, Krastinova E, Van Laer M, Claessens YE, Avondo A, Occelli C, Feral-Pierssens AL, Truchot J, Ortega M, et al. 2017. Prognostic accuracy of sepsis-3 criteria for in-hospital mortality among patients with suspected infection presenting to the emergency department. Jama. 317(3):301–308. doi: https://doi.org/10.1001/jama.2016.20329
- Guo J, Tao W, Tang D, Zhang J. 2017. Th17/regulatory T cell imbalance in sepsis patients with multiple organ dysfunction syndrome: attenuated by high-volume hemofiltration. Int J Artif Organs. 40(11):607–614. doi: https://doi.org/10.5301/ijao.5000625
- Harris HE, Andersson U, Pisetsky DS. 2012. HMGB1: a multifunctional alarmin driving autoimmune and inflammatory disease. Nat Rev Rheumatol. 8(4):195–202. doi: https://doi.org/10.1038/nrrheum.2011.222
- Hotchkiss RS, Karl IE. 2003. The pathophysiology and treatment of sepsis. N Engl J Med. 348(2):138–150. doi: https://doi.org/10.1056/NEJMra021333
- Kasten K, Seitz A, Unsinger J, Hildeman D, Hotchkiss R, Caldwell C. 2010. IL-7 promotes T cell viability, enhances immunity, and improves survival in sepsis. J Surg Res. 158(2):209–210. doi: https://doi.org/10.1016/j.jss.2009.11.114
- Kragstrup TW, Juul-Madsen K, Christiansen SH, Zhang X, Krog J, Vorup-Jensen T, Kjaergaard AG. 2017. Altered levels of soluble CD18 may associate immune mechanisms with outcome in sepsis. Clin Exp Immunol. 190(2):258–267. doi: https://doi.org/10.1111/cei.13016
- Lan KC, Chao SC, Wu HY, Chiang CL, Wang CC, Liu SH, Weng TI. 2017. Salidroside ameliorates sepsis-induced acute lung injury and mortality via downregulating NF-kappaB and HMGB1 pathways through the upregulation of SIRT1. Sci Rep. 7(1):12026. doi: https://doi.org/10.1038/s41598-017-12285-8
- Lee W, Ku SK, Bae JS. 2017. Zingerone reduces HMGB1-mediated septic responses and improves survival in septic mice. Toxicol Appl Pharmacol. 329:202–211. doi: https://doi.org/10.1016/j.taap.2017.06.006
- Lee W, Ku SK, Kim TH, Bae JS. 2013. Emodin-6-O-beta-D-glucoside inhibits HMGB1-induced inflammatory responses in vitro and in vivo. Food Chem Toxicol. 52:97–104. doi: https://doi.org/10.1016/j.fct.2012.10.061
- Levy MM, Artigas A, Phillips GS, Rhodes A, Beale R, Osborn T, Vincent JL, Townsend S, Lemeshow S, Dellinger RP. 2012. Outcomes of the Surviving Sepsis Campaign in intensive care units in the USA and Europe: a prospective cohort study. Lancet Infect Dis. 12(12):919–924. doi: https://doi.org/10.1016/S1473-3099(12)70239-6
- Mishnev OD, Grinberg LM, Zairatyants OV. 2016. Actual problems of the pathology of sepsis: 25 years in search of a consensus. Arkh Patol. 78(6):3–8. doi: https://doi.org/10.17116/patol20167863-8
- Muller L, Jaber S, Molinari N, Favier L, Larché J, Motte G, Lazarovici S, Jacques L, Alonso S, Leone M, et al. 2012. Fluid management and risk factors for renal dysfunction in patients with severe sepsis and/or septic shock. Crit Care. 16(1):R34. doi: https://doi.org/10.1186/cc11213
- Park EJ, Jang HJ, Tsoyi K, Kim YM, Park SW, Kim HJ, Lee JH, Chang KC, Deng JC. 2013. The heme oxygenase-1 inducer THI-56 negatively regulates iNOS expression and HMGB1 release in LPS-activated RAW 264.7 cells and CLP-induced septic mice. PLoS One. 8(10):e76293. doi: https://doi.org/10.1371/journal.pone.0076293
- Raghu A, Komorowski M, Celi LA, Szolovits P, Ghassemi M. 2017. Continuous state-space models for optimal sepsis treatment-a deep reinforcement learning approach. arXiv preprint.
- Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, Kumar A, Sevransky JE, Sprung CL, Nunnally ME, et al. 2017. Surviving Sepsis Campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med. 43(3):304–377. doi: https://doi.org/10.1007/s00134-017-4683-6
- Sadaka F, EthmaneAbouElMaali C, Cytron MA, Fowler K, Javaux VM, O'Brien J. 2017. Predicting mortality of patients with sepsis: a comparison of APACHE II and APACHE III scoring systems. J Clin Med Res. 9(11):907–910. doi: https://doi.org/10.14740/jocmr3083w
- Shankar-Hari M. 2017. How could we enhance translation of sepsis immunology to inform immunomodulation trials in sepsis? Crit Care. 21(1):125. doi: https://doi.org/10.1186/s13054-017-1715-0
- Stevens NE, Chapman MJ, Fraser CK, Kuchel TR, Hayball JD, Diener KR. 2017. Therapeutic targeting of HMGB1 during experimental sepsis modulates the inflammatory cytokine profile to one associated with improved clinical outcomes. Sci Rep. 7(1):5850. doi: https://doi.org/10.1038/s41598-017-06205-z
- Tipoe TL, Wu WKK, Chung L, Gong M, Dong M, Liu T, Roever L, Ho J, Wong MCS, Chan MTV, et al. 2018. Plasminogen activator inhibitor 1 for predicting sepsis severity and mortality outcomes: a systematic review and meta-analysis. Front Immunol. 9:1218. doi: https://doi.org/10.3389/fimmu.2018.01218
- Tiruvoipati R, Sultana N, Lewis D. 2012. Cardiac troponin I does not independently predict mortality in critically ill patients with severe sepsis. Emerg Med Australas. 24(2):151–158. doi: https://doi.org/10.1111/j.1742-6723.2011.01530.x
- Unsinger J, McGlynn M, Kasten KR, Hoekzema AS, Watanabe E, Muenzer JT, McDonough JS, Tschoep J, Ferguson TA, McDunn JE, et al. 2010. IL-7 promotes T cell viability, trafficking, and functionality and improves survival in sepsis. J Immunol. 184(7):3768–3779. doi: https://doi.org/10.4049/jimmunol.0903151
- Wang H, Cui Z, Sun F, Ding H. 2017. Glucan phosphate inhibits HMGB-1 release from rat myocardial H9C2 cells in sepsis via TLR4/NF-small ka, CyrillicB signal pathway. Clin Invest Med. 40(2):E66–E72. doi: https://doi.org/10.25011/cim.v40i2.28197