Abstract
The potential advantages of sleep concerning suppressing cytokine storms and inflammation in coronavirus disease 2019 (COVID-19) based on its immunopathogenesis are summarized in the current study. COVID-19 as a global pandemic in the past months has afflicted many people. Clinical properties, pathology, and the pathogenesis of acute respiratory disorder caused by coronaviruses or other pathogens are evidence implying the probable contribution of oxidation, excessive inflammation, and excessive immune response, particularly cytokine storm, to the pathology of COVID-19. According to findings by experimental and clinical research on animals and in humans, sleep loss impairs immune function. Sleep loss strongly influences peripheral levels of the immune response’s inflammatory mediators, which is accomplished by the generation of various hormones and mediators during sleep. There are a large number of studies supporting the presence of reciprocal regulation between low-intensity inflammatory response and sleep. By improving sleep quality and at the same time adjusting the circadian rhythm, it may be possible to prevent infections and boost immunity. As a result, sufficient (or even more) sleep duration may lower susceptibility to COVID-19 infection as well as increase antibody levels.
Introduction
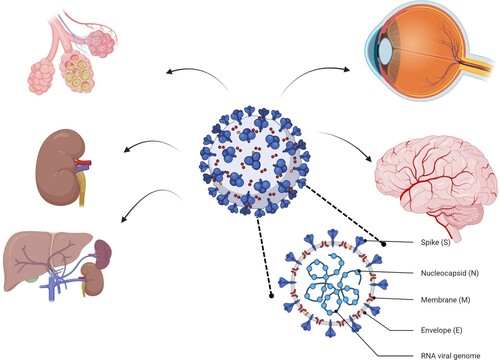
Having appeared in December 2019, coronavirus disease 2019 (COVID-19) is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (Farnoosh et al. Citation2020). This pandemic disease challenged both the world’s healthcare system and influenced many dimensions of human life worldwide (Farzaneh Pour et al. Citation2020). COVID-19 affects various organs of the body (Figure ). The SARS-CoV-2 has the ability to invade respiratory epithelial cells in the lower and upper respiratory tract (Ji et al. Citation2020). Both adaptive and innate immune responses can be involved in coronavirus infections. In the initial infection phases, the generation of type 1 interferons has a more significant role in defending against the virus (Lu et al. Citation2020). Adaptive immunity requires more time to be activated and is done via the generation of neutralizing antibodies by B lymphocytes assisted by T cells. In the development of the vaccine, it is essential to provide this type of immunity (Nikpouraghdam et al. Citation2020). Based on different reports, hyper inflammation has a contribution to the severity of disease and mortality of SARS-CoV-2 patients. If we have a better understanding about the patients at higher risk of pathological inflammation and the specific inflammatory pathways driving the pathology of the disease, then rationale-based clinical treatment strategies can be developed (Tay et al. Citation2020).
Sleep is a state of body and mind that naturally recurs, during which consciousness is altered, sensory activity is inhibited, muscle activity is reduced, and almost the whole voluntary muscles are inhibited during the rapid eye movement (REM) sleep phase (Besedovsky et al. Citation2019). A decreased ability to react to stimuli distinguishes sleep from wakefulness. Our brains are highly active and display different patterns of brain activity during sleep in contrast to a coma or consciousness disorder (Irwin Citation2019; Toda et al. Citation2019). When we are sleeping our body’s systems are mostly in an anabolic mode, which helps restoration of the nervous, immune, muscular, and skeletal systems (Prather Citation2019). These processes are vital for maintaining cognitive function, memory, and mood, which have a crucial role in the functioning of the immune and endocrine systems (Oikonomou and Prober Citation2019). Furthermore, a good night’s sleep can enhance vaccination effectiveness by enhancing the immune response (Besedovsky et al. Citation2019).
A lack of sleep and a disturbed circadian rhythm have been reported in patients suffering from COVID-19, causing insomnia, sleep disturbances, and delirium (Gualano et al. Citation2020; Deng et al. Citation2021; Pun et al. Citation2021). Given the high prevalence of sleep disturbances and delirium among COVID-19 hospitalized patients, it may be reasonable to consider managing sleep in these patients (Zambrelli et al. Citation2020). Here, this review discusses the effects of circadian rhythms and sleep on immune function. Additionally, this review discusses COVID-19 and sleep disturbances with a particular focus on the ability of sleep to regulate inflammation and the immune system.
The role of sleep in COVID-19
The research studies that follow a systems approach of neuroimmunology over the past 15 years have gathered surprisingly strong evidence on the fact that sleep improves immune defense (Huang and Zhao Citation2020). It is consistent with the well-known wisdom of ‘sleep helps to heal’. It has been proved that sleep and the circadian system have a strong regulatory impact on the body’s immune system (Altena et al. Citation2020; Xiao et al. Citation2020). Maintaining a functional immune response during sleep could be an important factor in protecting against COVID-19. The link between sleep and COVID-19 has not been well studied, however, there are a few data to support this relation. For instance, Kim et al. (Citation2021) studied sleep as a risk factor for COVID-19 among healthcare workers (HWCs) in several different countries. In particular, HCWs who work on the front line are vulnerable to infection with COVID-19. It’s important to know whether these people’s sleep patterns affect their risk of infection with COVID-19. An online sleep questionnaire was used in a case–control study to determine participants’ sleeping habits. Having a 1-h longer sleep duration at night decreased the chance of COVID-19 infection by 12%, while people with multiple sleep problems were 88% more susceptible to COVID-19. On the other hand, naps during the day gave a higher chance of COVID-19, but this varied by country, so was not as definitive as it seemed (Kim et al. Citation2021). Supporting the results by Kim et al. (Citation2021), studies published recently show an increased chance of COVID-19 infection in shift workers (Fatima et al. Citation2021; Rizza et al. Citation2021; Rowlands et al. Citation2021).
Immune system homeostasis is influenced by circadian rhythms and sleep. Therefore, a deregulated circadian rhythm could increase the risk of COVID-19, leading to a proinflammatory state. A shift in daily routines and an irregular sleep–wake cycle can make HCWs at the frontline particularly prone to developing circadian rhythm problems. SARS-CoV-2 virus-induced COVID-19 may be reduced by improved sleep duration and sleep efficiency (Meira et al. Citation2020).
Studies using cross-sectional methods as well as experiments with experimentally induced sleep restriction have found that disrupted sleep and circadian rhythms reduce antibody responses. This results in impaired cell-mediated immunity in response to a variety of vaccines when the sleep duration is shorter. In pandemics such as the current COVID-19, sleep disturbances can be a problem as a result of these times. A recent study indicated that people either slept less or slept longer than they did before the COVID-19 pandemic (Batool-Anwar et al. Citation2021). Over 20% of the residents of China infected with COVID-19 actually met the criteria for clinical insomnia, as evidenced by data collected during the outbreak. Furthermore, those individuals also reported spending over 1 h awake during the night. It was also found that individuals at greater risk for SARS-CoV-2, including HCWs, suffered from higher levels of insomnia (Kim et al. Citation2021). Susceptibility to infection as well as vaccination outcomes are negatively affected by this (Madison et al. Citation2021). To boost vaccination success, it is more important than ever before that people sleep for at least 7 h every night. Before vaccination, sleep and circadian-based interventions may be beneficial to optimize healthy sleep and circadian alignment.
There is persuasive evidence from the limited human studies that circadian alignment and efficient sleep contribute to vaccination outcomes, but more studies are needed. To address the pressing need to gain more knowledge on this matter, Lammers-van der Holst and colleagues initiated a study to analyze the link between sleep and circadian compliance with immune response to COVID-19 vaccination (Lammers-van der Holst et al. Citation2022).
The link between sleep and inflammation
The role of circadian rhythm in immune function
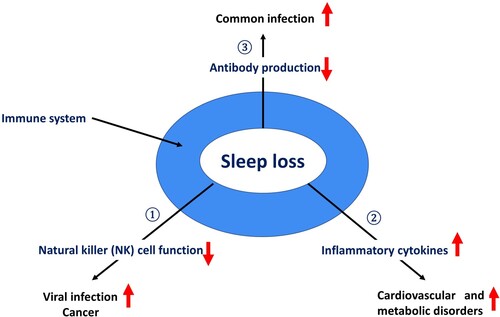
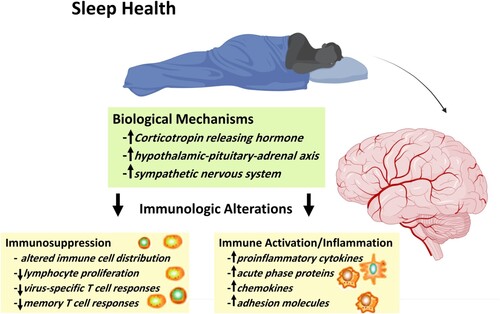
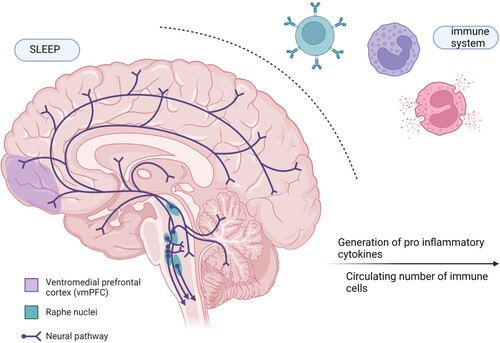
The circadian system and sleep have a significant regulatory impact on immune functions. According to studies on the normal sleep–wake cycle, immune factors, such as the generation of proinflammatory cytokines and the numbers of undifferentiated naïve T cells, peak in early nocturnal sleep, while circulating numbers of immune cells with immediate effects or functions, such as cytotoxic natural killer (NK) cells and anti-inflammatory cytokines, peak in activity in alertness during the day (Figure ) (Besedovsky et al. Citation2019).
Figure 2. Correlation between sleep and immune system, the immune system is presented alongside the brain, emphasizing the link between sleep and the immune system.
Entirely dissecting the sleep influence from the circadian rhythm is difficult. However, the impact of nocturnal sleep has been compared with the impact of 24-h periods of wakefulness, and it has been indicated that sleep functions as a facilitator in T cells extravasation and their probable redistribution to lymph nodes (Besedovsky et al. Citation2012; Besedovsky et al. Citation2019). In addition, previous works have demonstrated that sleep has an enhancing impact on cytokines, which promotes the interaction between T helper (Th) cells, like IL-12 and antigen presenting cells (APC) (Liu et al. Citation2020). It was revealed that following experimental vaccinations against hepatitis A, sleep in the night strongly and persistently increased antibody titers and the number of antigen-specific Th cells (Besedovsky et al. Citation2012). Based on a research finding, sleep has a special role in forming immunological memory. It seems that its role is particularly related to the phase of slow wave sleep (SWS) and the associated proinflammatory endocrine milieu. It is shown by low concentrations of catecholamine and cortisol, as well as high growth hormone and prolactin levels (Morris et al. Citation2012).
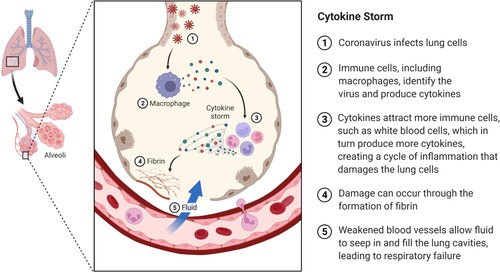
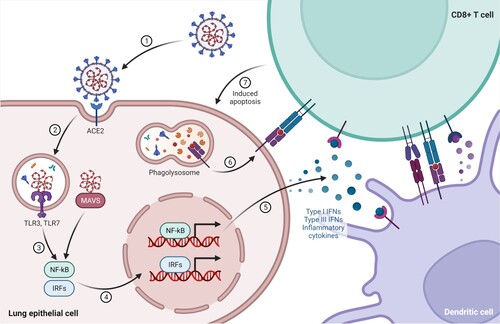
During an infection, both adaptive and innate immune cells contribute synergistically to the antiviral response. It is essential that the host’s adaptive and innate immunity demonstrate effective antiviral responses, such as the production of various proinflammatory cytokines and the activation of CD4+ and CD8+ T cells, in order to control viral replication, limit viral spread and inflammation, and eliminate infected cells (Krieger et al. Citation2020). As a result of the overproduction of early response proinflammatory cytokines (IL-6, TNF-α, IL-1β) a cytokine storm occurs, which leads to increased risk of multi-organ failure, vascular hyperpermeability, and often death if high concentrations of cytokine are unabated over time (Figure ) (Hannan et al. Citation2020).
Figure 3. Schematic representation of SARS-CoV-2-driven signaling pathways contributing to hyper inflammation in COVID-19. ACE2: angiotensin-converting enzyme 2, TLR: Toll-like receptor, NF-κB: nuclear factor kappa-light-chain-enhancer of activated B cells, IRFs: interferon regulatory factors, MAVS: mitochondrial antiviral-signaling, IFN: interferon.
Lack of any elevation in lymphocytes in reaction to sleep loss has not been found by most studies. In a study on sleep deprivation, increased white blood cell (WBC) counts were considered an indication of activation of host defense (Nunes et al. Citation2018). Moreover, IL-1β, TNF-α, and IL-6 were found to be increased in acute sleep deprivation, though the specific mediators could vary in different conditions (Gozal et al. Citation2017). In addition, it was shown that changes in the inflammatory system happen as a reaction to controlled experimental partial sleep deprivation, or decreased sleep time in people who commonly have an about 8-h night sleep (Sward et al. Citation2018). Based on recent research, the subjects who were allowed to sleep just 2 h twice daily (in the afternoon and at night), did not show any elevation in TNF-α, IL-6, or TNF-α receptors for four days (Bakour et al. Citation2017). Another study showed that night sleep reduction by 2 h for 7 nights increased TNF-α in healthy men but the same thing was not observed among women, while IL-6 increased in both sexes (Uchino et al. Citation2019). When the relation between sleep loss and inflammation is considered, it should be noticed that there is not much information about the cytokine source(s) that are being measured in peripheral blood (Yin et al. Citation2017). Cytokines could be generated by macrophages, monocytes, neutrophils, adipocytes, and endothelial cells. In addition, it should be noted that the relative contribution of cytokines to circulating levels, obviously under sleep deprivation conditions, is not clear (Lin et al. Citation2016). For finding the origin of sleep loss-associated inflammation it is necessary to conduct studies indicating that restriction of nightly sleep to 4 h resulted in elevated monocyte generation of IL-6 and TNF-α mRNA (Gouveris et al. Citation2018). Although IL-6 and TNF-α are not merely produced by monocytes, monocytes are strong generators, and it is a mechanistic pathway activated by sleep loss (Figure ) (Chen et al. Citation2018).
The role of inflammation in COVID-19
A large amount of interleukin (IL)-2, IL-10, IL-7, interferon gamma-induced protein 10 (IP-10), granulocyte-colony stimulating factor (G-CSF), monocyte chemoattractant protein-1 (MCP1), tumor necrosis factor (TNF-α), and macrophage inflammatory protein 1 (MIP1) have been reported in COVID-19 patients (Figure ) (Bouadma et al. Citation2020; Wang et al. Citation2020a). In some patients with COVID-19, the cytokines are produced and released in an uncontrolled manner, called cytokine storm, which ultimately results in a severe proinflammatory situation in the patients that are in critical condition (Huang et al. Citation2020). Some characteristics of COVID-19, including serological markers, clinical symptoms, and the cytokine profile are similar to secondary hemophagocytic lymphohistiocytosis, which is mainly induced by viral infection (Mathew et al. Citation2020). Moreover, as the other significant evidence, there is a relationship between the COVID-19 severity and the proinflammatory cytokine levels and subsets of immune cells. There is no doubt that the obvious and most efficient therapy for COVID-19 would be the antiviral agents directly targeting SARS-CoV-2 (Schett et al. Citation2020). The search for an effective COVID-19 vaccine continues even though some pharmaceutical companies in a few countries have succeeded (Lee et al. Citation2020; Hosseini et al. Citation2021). However, as mentioned earlier to improve COVID-19 vaccine efficacy, sleep quality and sleep duration should be considered.
Impact of sleep modification on the complications caused by COVID-19
A variety of hormones, including melatonin, cortisol, and insulin, vary across the 24-h day and are highly regulated by the circadian and sleep–wake cycles that affect other systems such as the immune system (Figure ) (Hajali et al. Citation2019). The interaction between T cells and APC is critically supported by the endocrine milieu during early sleep, an improved generation of IL-12, Th1/Th2 cytokine balance shift to Th1 cytokines, and increasing proliferation of Th cells (Pazarlı et al. Citation2021). The movement of naïve T cells to lymph nodes is also facilitated in this way. Consequently, the endocrine milieu probably encourages the initiation of Th1 immune responses during early sleep, which finally has a supportive role in forming persistent immunological memory (Belingheri et al. Citation2021). It seems that its role is particularly related to the phase of SWS and the associated proinflammatory endocrine milieu. Persistent sleep compression and the associated stress response cause proinflammatory cytokines to be persistently produced, which can be best defined as chronic low-grade inflammation. Moreover, it leads to immunodeficiency. Both conditions have adverse impacts on health (Zhang et al. Citation2020).
Sleep and diabetes
Insulin is known for its regulatory role in blood sugar levels. The pancreas produces this essential hormone that helps the body to utilize the sugar, or glucose, taken from food. Glucose is regarded as a major energy source for the body (Lo Martire et al. Citation2020). However, if it is excessive in the bloodstream, it can be harmful to the body’s health. For this reason, insulin is secreted often when the blood glucose levels are too high, to help store glucose in the liver for being used later (Nilakanthan et al. Citation2016). This is why binging on sugar snacks is not recommended before going to bed. When the blood sugar level is high, it would be difficult to sleep (Lavrentaki et al. Citation2019). It has been proven that inadequate sleep contributes to obesity and diabetes (Cajochen et al. Citation2003; Xie et al. Citation2017; Zhang et al. Citation2019). Diabetes mellitus (DM) is characterized by chronic hyperglycemia as a result of an imbalance between carbohydrate, lipid and protein metabolism (Parameswaran and Ray Citation2022). Research has demonstrated that reductions in insulin sensitivity and glucose tolerance were associated with total or partial sleep restriction for a few days in humans (Spiegel et al. Citation1999; Tasali et al. Citation2008). Also, in a recent prospective cohort study by Wang et al. (Citation2020b) they examine the relationship between sleep duration and all-cause and cause-specific mortality in people with type 2 diabetes. Study participants included 273,029 adults in the National Health Interview Survey from 2004 to 2013, including 248,817 without diabetes and 24,212 with type 2 diabetes whose names were linked to a mortality database through 31 December 2015. They showed that those with diabetes and extreme sleep duration had a higher absolute mortality rate (≤5 h/day, 215.0 per 10,000 person-years; ≥10 h/day, 363.5 per 10,000 person-years). The authors concluded that there was an increased risk of death due to all causes or condition-specific mortality in people with type 2 diabetes who slept less or more than 7 h/day. COVID-19 patients with diabetes may have a reduced immune response, more severe infections, and worse outcomes from diabetes-associated inflammatory disease (Hussain et al. Citation2020).
Sleep and thyroid function
The location of the thyroid gland is just below the larynx. It makes two hormones, triiodothyronine (T3) and thyroxine (T4). T3 and T4 help regulate the metabolic rate, digestive function, and development of the brain (Park et al. Citation2019). They are both important, particularly with regard to mood. When the thyroid gland is not adequately active (hypothyroidism) or too active (hyperthyroidism), some problems may happen with it (Bruyneel et al. Citation2019). Both of these conditions have a long list of side effects, and oddly there is an association between these conditions and poor sleep. Hyperthyroidism in some patients can almost stimulate the nervous system and make you feel restless (Sriphrapradang et al. Citation2019). Consequently, getting sleep or staying asleep would be difficult. On the other hand, hypothyroidism is usually linked to lethargy and fatigue feelings (Ikegami et al. Citation2019). It might be thought that fatigue feelings may make sleep easier but this is not the case, because hypothyroidism sometimes can increase the risk of suffering from a sleep disorder. For instance, it is estimated that about 30% of people with hypothyroidism suffer from sleep apnea (Kim et al. Citation2019). Additionally, Kim et al. (Citation2019) investigated the association of subclinical thyroid dysfunction with sleep duration using representative data from the sixth Korea National Health and Nutrition Examination Survey, conducted from 2013 to 2015. Among 4945 participants (2543 males and 2402 females), three groups were distinguished: short sleepers (less than 7 h per day), normal sleepers (7–8 h per day), and long sleepers (more than 8 h per day). According to their findings, both shorter and longer sleep durations increase the risk of subclinical thyroid dysfunction compared to optimal sleep durations.
Delirium and insomnia
Sleep is essential to both an individual’s emotional and physical health. Comprehensive evidence shows that insufficient sleep contributes to delirium, depression, and insomnia (Cajochen et al. Citation2003; Xie et al. Citation2017; Zhang et al. Citation2019). Melatonin and cortisol are the two main sleep pattern regulating hormones. Cortisol is usually referred to as a ‘stress hormone’ and adrenal glands produce it. It helps regulate the metabolism and reduce inflammation. When cortisol is released, blood sugar levels and blood pressure are raised for preparing for physical activity (Mannino et al. Citation2019). We usually experience a cortisol spike early in the morning as part of the circadian rhythm, which helps us to wake up and feel refreshed. With the progression of the day, there is a gradual decline in cortisol levels as there is more release of melatonin in the hours before bedtime (Rubin et al. Citation2020). Melatonin, also known as the sleep hormone, is produced by the pineal gland, and it cooperates with cortisol. When natural light diminishing is detected by optic nerves, these nerves send a message to the hypothalamus that induces melatonin release for helping relaxation and feeling drowsy for sleep. Cortisol levels generally decrease by increasing melatonin levels and vice-versa (Yu and Tan Citation2019).
It has been reported that patients with COVID-19 are likely to suffer from sleep disturbances and delirium (Gualano et al. Citation2020; Deng et al. Citation2021; Pun et al. Citation2021). The physical, cognitive, and social functioning of patients can be adversely affected by these conditions. The pathogenesis of delirium is poorly understood, in part because it is a complex condition. However, several factors are suspected to contribute to its occurrence, such as neurotransmitter imbalances, inflammatory cytokines, and tissue hypoxia. Deprivation of sleep can be a modifiable risk factor, but it can also be the result of delirium (Zhang et al. Citation2019; Zambrelli et al. Citation2020). The intensive care unit (ICU) can benefit from the use of melatonin or melatonin receptor agonists to reduce delirium and improve sleep quality. As melatonin is known to be safe, it is a promising first-line therapy for sleep–wake rhythms and consciousness disturbances to avoid the increased risks associated with benzodiazepines and antipsychotics, which can worsen delirium in the elderly (Zhang et al. Citation2019; Zambrelli et al. Citation2020).
COVID-19, the pandemic that is taking place at the moment, is brought into perspective by these findings. A few studies have found that sleep and circadian rhythms contribute to susceptibility to infection with the SARS-CoV-2 virus, and their findings are consistent with those in the literature. The evidence found in the literature indicates that at least 7 h of sleep every night may reduce the risk of contracting COVID-19. This is, however, a more difficult task than it sounds. Particularly high-risk workers, like HCWs, suffer from severe insomnia. A circadian rhythm disorder can easily develop due to working night shifts, irregular sleep schedules, and changes in daily routines. Vaccination immunity is likely to be improved through the introduction of sleep and circadian-based interventions, which will translate into an improvement in global health. Further research in this area is needed due to the paucity of research to date.
Conclusions
On the basis of COVID-19’s immunopathogenesis, the reviewed literature revealed the crucial role of sleep and sleep quality in suppressing inflammation and cytokine storms. Therefore, it is promising to use it as an anti-inflammatory factor in COVID-19 patients. In these studies, sleep-related variables, such as sleeping duration, were found to be critical to immune function. To decrease the risk of getting infected with viruses, an individual should get at least 7 h of sleep every night. By doing this, the immune system will be strengthened and immune function will be improved. Many people today experience many forms of circadian disruption. These range from mild weekend sleep disruptions to severe rotating night shift work, which puts many individuals at risk of being relatively immune compromised as a result. According to this review, sufficient sleep and circadian alignment contribute to optimal immune health. Despite advances in current knowledge, there are still gaps that will require further research. Studying differences between individuals based on habits and chronotypes of sleep could be of interest in the future. For example, one possibility would be to study differences between morning and evening types or to understand social jetlag, a phenomenon that occurs when one’s biological rhythm diverges from their social life. Lastly, it is crucial to understand how a healthy immune system and sleep are correlated across several time dimensions to develop interventions that ensure optimum immune function.
Acknowledgements
The respective figures were generated from online software BioRender available at https://app.biorender.com/. K.H., H.E., M.K., A.H., G.F., T.B., and M.A. contribute equally to the conception and design, or analysis and interpretation of the data; the drafting of the paper, revising it critically for intellectual content; and the final approval of the version to be published; and that all authors agree to be accountable for all aspects of the work.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Data sharing is not applicable to this article as no new data were created or analyzed in this study.
References
- Altena E, Baglioni C, Espie CA, Ellis J, Gavriloff D, Holzinger B, Schlarb A, Frase L, Jernelöv S, Riemann D. 2020. Dealing with sleep problems during home confinement due to the COVID-19 outbreak: practical recommendations from a task force of the European CBT-I Academy. J Sleep Res. 29(4):e13052.
- Bakour C, Schwartz S, O’Rourke K, Wang W, Sappenfield W, Couluris M, Chen H. 2017. Sleep duration trajectories and systemic inflammation in young adults: results from the national longitudinal study of adolescent to adult health (add health). Sleep. 40(11):1–9.
- Batool-Anwar S, Robbins R, Ali SH, Capasso A, Foreman J, Jones AM, Tozan Y, DiClemente RJ, Quan SF. 2021. Examining changes in sleep duration associated with the onset of the COVID-19 pandemic: who is sleeping and who is not? Behav Med. 1–10.
- Belingheri M, Paladino ME, Riva MA. 2021. Working schedule, sleep quality, and susceptibility to coronavirus disease 2019 in healthcare workers. Clin Infect Dis. 72(9):1676.
- Besedovsky L, Lange T, Born J. 2012. Sleep and immune function. Pflugers Arch. 463(1):121–137.
- Besedovsky L, Lange T, Haack M. 2019. The sleep-immune crosstalk in health and disease. Physiol Rev. 99(3):1325–1380.
- Bouadma L, Wiedemann A, Patrier J, Surénaud M, Wicky PH, Foucat E, Diehl JL, Hejblum BP, Sinnah F, de Montmollin E, et al. 2020. Immune alterations in a patient with SARS-CoV-2-related acute respiratory distress syndrome. J Clin Immunol. 40(8):1082–1092.
- Bruyneel M, Veltri F, Poppe K. 2019. Prevalence of newly established thyroid disorders in patients with moderate-to-severe obstructive sleep apnea syndrome. Sleep Breath. 23(2):567–573.
- Cajochen C, Kräuchi K, Wirz-Justice A. 2003. Role of melatonin in the regulation of human circadian rhythms and sleep. J Neuroendocrinol. 15(4):432–437.
- Chen L, Deng H, Cui H, Fang J, Zuo Z, Deng J, Li Y, Wang X, Zhao L. 2018. Inflammatory responses and inflammation-associated diseases in organs. Oncotarget. 9(6):7204–7218.
- Deng J, Zhou F, Hou W, Silver Z, Wong CY, Chang O, Huang E, Zuo QK. 2021. The prevalence of depression, anxiety, and sleep disturbances in COVID-19 patients: a meta-analysis. Ann N Y Acad Sci. 1486(1):90–111.
- Farnoosh G, Alishiri G, Hosseini Zijoud SR, Dorostkar R, Jalali Farahani A. 2020. Understanding the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease (COVID-19) based on available evidence – a narrative review. J Mil Med. 22(1):1–11.
- Farzaneh Pour M, Karimi M, Rezayat P, Bolandian M, Mirzaei Nodoushan M, Esmaeili Gouvarchin Ghaleh H. 2020. A review of the mechanisms involved in the immunopathogenesis of SARS-CoV-2. J Mil Med. 22(2):147–160.
- Fatima Y, Bucks RS, Mamun AA, Skinner I, Rosenzweig I, Leschziner G, Skinner TC. 2021. Shift work is associated with increased risk of COVID-19: findings from the UK biobank cohort. J Sleep Res. 30(5):e13326.
- Gouveris H, Bahr K, Jahn C, Matthias C, Simon P. 2018. The apnea-hypopnea index underestimates systemic inflammation in women with sleep-disordered breathing. J Womens Health (Larchmt). 27(7):920–926.
- Gozal D, Khalyfa A, Qiao Z, Akbarpour M, Maccari R, Ottanà R. 2017. Protein-tyrosine phosphatase-1B mediates sleep fragmentation-induced insulin resistance and visceral adipose tissue inflammation in mice. Sleep. 40(9):1–10.
- Gualano MR, Lo Moro G, Voglino G, Bert F, Siliquini R. 2020. Effects of Covid-19 lockdown on mental health and sleep disturbances in Italy. Int J Environ Res Public Health. 17(13):4779.
- Hajali V, Andersen ML, Negah SS, Sheibani V. 2019. Sex differences in sleep and sleep loss-induced cognitive deficits: the influence of gonadal hormones. Horm Behav. 108:50–61.
- Hannan MA, Rahman MA, Rahman MS, Sohag AAM, Dash R, Hossain KS, Farjana M, Uddin MJ. 2020. Intermittent fasting, a possible priming tool for host defense against SARS-CoV-2 infection: crosstalk among calorie restriction, autophagy and immune response. Immunol Lett. 226:38–45.
- Hosseini A, Esmaeili Gouvarchin Ghaleh H, Aghamollaei H, Fasihi Ramandi M, Alishiri G, Shahriary A, Hassanpour K, Tat M, Farnoosh G. 2021. Evaluation of Th1 and Th2 mediated cellular and humoral immunity in patients with COVID-19 following the use of melatonin as an adjunctive treatment. Eur J Pharmacol. 904:174193.
- Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, et al. 2020. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 395(10223):497–506.
- Huang Y, Zhao N. 2020. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. 288:112954.
- Hussain A, Bhowmik B, do Vale Moreira NC. 2020. COVID-19 and diabetes: knowledge in progress. Diabetes Res Clin Pract. 162:108142.
- Ikegami K, Refetoff S, Van Cauter E, Yoshimura T. 2019. Interconnection between circadian clocks and thyroid function. Nat Rev Endocrinol. 15(10):590–600.
- Irwin MR. 2019. Sleep and inflammation: partners in sickness and in health. Nat Rev Immunol. 19(11):702–715.
- Ji W, Wang W, Zhao X, Zai J, Li X. 2020. Cross-species transmission of the newly identified coronavirus 2019-nCoV. J Med Virol. 92(4):433–440.
- Kim H, Hegde S, LaFiura C, Raghavan M, Luong E, Cheng S, Rebholz CM, Seidelmann SB. 2021. COVID-19 illness in relation to sleep and burnout. BMJ Nutr Prev Health. 4(1):132–139.
- Kim W, Lee J, Ha J, Jo K, Lim DJ, Lee JM, Chang SA, Kang MI, Kim MH. 2019. Association between sleep duration and subclinical thyroid dysfunction based on nationally representative data. J Clin Med. 8(11):2010.
- Krieger E, Vissichelli N, Leichtle S, Kashioris M, Sabo R, Brophy D, Wang X-Y, Kimbal P, Neale M, Serrano MG. 2020. Immunological determinants of clinical outcomes in COVID-19: a quantitative perspective. arXiv preprint arXiv:200506541.
- Lammers-van der Holst HM, Lammers GJ, van der Horst GTJ, Chaves I, de Vries RD, GeurtsvanKessel CH, Koch B, van der Kuy HM. 2022. Understanding the association between sleep, shift work and COVID-19 vaccine immune response efficacy: protocol of the S-CORE study. J Sleep Res. 31(2):e13496.
- Lavrentaki A, Ali A, Cooper BG, Tahrani AA. 2019. Mechanisms of endocrinology: mechanisms of disease: the endocrinology of obstructive sleep apnoea. Eur J Endocrinol. 180(3):R91–r125.
- Lee CH, Pinho MP, Buckley PR, Woodhouse IB, Ogg G, Simmons A, Napolitani G, Koohy H. 2020. Potential CD8+ T cell cross-reactivity against SARS-CoV-2 conferred by other coronavirus strains. Front Immunol. 11:579480.
- Lin WC, Huang CC, Chen HL, Chou KH, Chen PC, Tsai NW, Chen MH, Friedman M, Lin HC, Lu CH. 2016. Longitudinal brain structural alterations and systemic inflammation in obstructive sleep apnea before and after surgical treatment. J Transl Med. 14(1):139.
- Liu K, Chen Y, Wu D, Lin R, Wang Z, Pan L. 2020. Effects of progressive muscle relaxation on anxiety and sleep quality in patients with COVID-19. Complement Ther Clin Pract. 39:101132.
- Lo Martire V, Caruso D, Palagini L, Zoccoli G, Bastianini S. 2020. Stress & sleep: a relationship lasting a lifetime. Neurosci Biobehav Rev. 117:65–77.
- Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, Wang W, Song H, Huang B, Zhu N, et al. 2020. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 395(10224):565–574.
- Madison AA, Shrout MR, Renna ME, Kiecolt-Glaser JK. 2021. Psychological and behavioral predictors of vaccine efficacy: considerations for COVID-19. Perspect Psychol Sci. 16(2):191–203.
- Mannino G, Caradonna F, Cruciata I, Lauria A, Perrone A, Gentile C. 2019. Melatonin reduces inflammatory response in human intestinal epithelial cells stimulated by interleukin-1β. J Pineal Res. 67(3):e12598.
- Mathew D, Giles JR, Baxter AE, Greenplate AR, Wu JE, Alanio C, Oldridge DA, Kuri-Cervantes L, Pampena MB, D’Andrea K, et al. 2020. Deep immune profiling of COVID-19 patients reveals patient heterogeneity and distinct immunotypes with implications for therapeutic interventions. bioRxiv.
- Meira ECM, Miyazawa M, Gozal D. 2020. Putative contributions of circadian clock and sleep in the context of SARS-CoV-2 infection. Eur Respir J. 55(6):2001023.
- Morris CJ, Aeschbach D, Scheer FA. 2012. Circadian system, sleep and endocrinology. Mol Cell Endocrinol. 349(1):91–104.
- Nikpouraghdam M, Jalali Farahani A, Alishiri G, Heydari S, Ebrahimnia M, Samadinia H, Sepandi M, Jafari NJ, Izadi M, Qazvini A, et al. 2020. Epidemiological characteristics of coronavirus disease 2019 (COVID-19) patients in IRAN: a single center study. J Clin Virol. 127:104378.
- Nilakanthan S, Metri K, Raghuram N, Hongasandra N. 2016. Effect of 6 months intense yoga practice on lipid profile, thyroxine medication and serum TSH level in women suffering from hypothyroidism: a pilot study. J Complement Integr Med. 13(2):189–193.
- Nunes JOF, Apostolico JS, Andrade DAG, Ruiz FS, Fernandes ER, Andersen ML, Keller AC, Rosa DS. 2018. Sleep deprivation predisposes allergic mice to neutrophilic lung inflammation. J Allergy Clin Immunol. 141(3):1018–1027.e1014.
- Oikonomou G, Prober DA. 2019. Linking immunity and sickness-induced sleep. Science. 363(6426):455–456.
- Parameswaran G, Ray DW. 2022. Sleep, circadian rhythms, and type 2 diabetes mellitus. Clin Endocrinol (Oxf). 96(1):12–20.
- Park S, Zhu J, Altan-Bonnet G, Cheng SY. 2019. Monocyte recruitment and activated inflammation are associated with thyroid carcinogenesis in a mouse model. Am J Cancer Res. 9(7):1439–1453.
- Pazarlı AC, Ekiz T, İlik F. 2021. Coronavirus disease 2019 and obstructive sleep apnea syndrome. Sleep Breath. 25(1):371.
- Prather AA. 2019. Chapter 24 – sleep, stress, and immunity. In: Grandner MA, editor. Sleep and health. London, United Kingdom: Academic Press; p. 319–330.
- Pun BT, Badenes R, Heras La Calle G, Orun OM, Chen W, Raman R, Simpson BK, Wilson-Linville S, Hinojal Olmedillo B, Vallejo de la Cueva A, et al. 2021. Prevalence and risk factors for delirium in critically ill patients with COVID-19 (COVID-D): a multicentre cohort study. Lancet Respir Med. 9(3):239–250.
- Rizza S, Coppeta L, Grelli S, Ferrazza G, Chiocchi M, Vanni G, Bonomo OC, Bellia A, Andreoni M, Magrini A, et al. 2021. High body mass index and night shift work are associated with COVID-19 in health care workers. J Endocrinol Invest. 44(5):1097–1101.
- Rowlands AV, Gillies C, Chudasama Y, Davies MJ, Islam N, Kloecker DE, Lawson C, Pareek M, Razieh C, Zaccardi F, et al. 2021. Association of working shifts, inside and outside of healthcare, with severe COVID-19: an observational study. BMC Public Health. 21(1):773.
- Rubin LH, Langenecker SA, Phan KL, Keating SM, Neigh GN, Weber KM, Maki PM. 2020. Remitted depression and cognition in HIV: the role of cortisol and inflammation. Psychoneuroendocrinology. 114:104609.
- Schett G, Sticherling M, Neurath MF. 2020. COVID-19: risk for cytokine targeting in chronic inflammatory diseases? Nat Rev Immunol. 20(5):271–272.
- Spiegel K, Leproult R, Van Cauter E. 1999. Impact of sleep debt on metabolic and endocrine function. Lancet. 354(9188):1435–1439.
- Sriphrapradang C, Pinyopodjanard S, Suntornlohanakul O, Nimitphong H, Chirakalwasan N, Saetang S, Anothaisintawee T, Siwasaranond N, Manodpitipong A, Chailurkit LO, et al. 2019. Lack of associations between thyroid function and obstructive sleep apnea severity in adults with prediabetes and diabetes mellitus. Sleep Breath. 23(3):963–967.
- Sward M, Kirk C, Kumar S, Nasir N, Adams W, Bouchard C. 2018. Lax eyelid syndrome (LES), obstructive sleep apnea (OSA), and ocular surface inflammation. Ocul Surf. 16(3):331–336.
- Tasali E, Leproult R, Ehrmann DA, Van Cauter E. 2008. Slow-wave sleep and the risk of type 2 diabetes in humans. Proc Natl Acad Sci U S A. 105(3):1044–1049.
- Tay MZ, Poh CM, Rénia L, MacAry PA, Ng LFP. 2020. The trinity of COVID-19: immunity, inflammation and intervention. Nat Rev Immunol. 20(6):363–374.
- Toda H, Williams JA, Gulledge M, Sehgal A. 2019. A sleep-inducing gene, nemuri, links sleep and immune function in Drosophila. Science. 363(6426):509–515.
- Uchino BN, Landvatter J, Cronan S, Scott E, Papadakis M, Smith TW, Bosch JA, Joel S. 2019. Self-rated health and inflammation: a test of depression and sleep quality as mediators. Psychosom Med. 81(4):328–332.
- Wang X, Fang X, Cai Z, Wu X, Gao X, Min J, Wang F. 2020a. Comorbid chronic diseases and acute organ injuries are strongly correlated with disease severity and mortality among COVID-19 patients: a systemic review and meta-analysis. Research (Wash D C). 2020:2402961.
- Wang Y, Huang W, O’Neil A, Lan Y, Aune D, Wang W, Yu C, Chen X. 2020b. Association between sleep duration and mortality risk among adults with type 2 diabetes: a prospective cohort study. Diabetologia. 63(11):2292–2304.
- Xiao H, Zhang Y, Kong D, Li S, Yang N. 2020. The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID-19) in January and February 2020 in China. Med Sci Monit. 26:e923549.
- Xie Z, Chen F, Li WA, Geng X, Li C, Meng X, Feng Y, Liu W, Yu F. 2017. A review of sleep disorders and melatonin. Neurol Res. 39(6):559–565.
- Yin M, Chen Y, Zheng H, Pu T, Marshall C, Wu T, Xiao M. 2017. Assessment of mouse cognitive and anxiety-like behaviors and hippocampal inflammation following a repeated and intermittent paradoxical sleep deprivation procedure. Behav Brain Res. 321:69–78.
- Yu GM, Tan W. 2019. Melatonin inhibits lipopolysaccharide-induced inflammation and oxidative stress in cultured mouse mammary tissue. Mediators Inflamm. 2019:8597159.
- Zambrelli E, Canevini M, Gambini O, D’Agostino A. 2020. Delirium and sleep disturbances in COVID-19: a possible role for melatonin in hospitalized patients? Sleep Med. 70:111.
- Zhang Q, Gao F, Zhang S, Sun W, Li Z. 2019. Prophylactic use of exogenous melatonin and melatonin receptor agonists to improve sleep and delirium in the intensive care units: a systematic review and meta-analysis of randomized controlled trials. Sleep Breath. 23(4):1059–1070.
- Zhang R, Wang X, Ni L, Di X, Ma B, Niu S, Liu C, Reiter RJ. 2020. COVID-19: melatonin as a potential adjuvant treatment. Life Sci. 250:117583.