Abstract
Tuberculosis (TB) is a serious disease that affects people worldwide, including in Saudi Arabia. The study analyzed the frequency of diagnosed TB cases, age-specific incidence rate, year of diagnosis, and prevalence of TB in Saudi Arabia from 2014 to 2020. Based on the National Tuberculosis Program (NTP) data, 21,120 patients were diagnosed with TB. The mean incidence rate of pulmonary TB and extra-pulmonary TB was approximately 6.92 and 2.33 per 100,000 population, respectively. The highest age-specific incidence rate was observed in the 25–35 year age group. The non-Saudi population (11,086 cases; 52.50%) was significantly more affected by both types of TB compared to the Saudi population (10,034 cases; 47.50%). The male population of Saudi and non-Saudi was significantly more affected by both types of TB. The highest overall mean incidence rate per 100,000 population was observed in the Jeddah and Jazan regions. The study's findings may have implications for supporting public health interventions and implementing a more effective TB control strategy program in Saudi Arabia. It suggests that immigrants from TB-endemic countries and religious visitors from high-risk countries should undergo pre and post-arrival screening for TB to reduce its incidence.
Introduction
Tuberculosis (TB) is considered a re-emerging infectious disease that remains a significant health concern worldwide (Al-Hajoj and Varghese Citation2015). Despite the implementation of wide-ranging control approaches and increased public awareness, tuberculosis remains a significant threat to global public health (Guo et al. Citation2019). TB is caused by the bacterium Mycobacterium tuberculosis, and according to recent statistics, there were approximately 10 million cases of TB in 2020. Sadly, around 1.3 million deaths resulted from this disease (Global Tuberculosis Report Citation2021). In addition, TB may exhibit multi-systemic involvement (Murthy et al. Citation2011; Guler et al. Citation2015), with pulmonary TB being the most common form that affects the lungs. Extra-pulmonary TB, on the other hand, affects other parts of the body. This disease is commonly transmitted from person to person by various routes such as coughing, sneezing, or speaking with a TB-infected individual (Semilan et al. Citation2021; Almatroudi Citation2022). It is worth noting that not every form of TB is communicable, with pulmonary TB being the most transmissible form. Extra-pulmonary TB is less likely to be communicable. Common sites of extra-pulmonary TB include lymph nodes, pleura, and the osteoarticular system (National Tuberculosis Program Citation2021). Several medical factors such as diabetes mellitus, HIV, immunosuppression, kidney failure, and lung cancer are considered risk factors for TB disease (Almatroudi Citation2021). Some non – medical factors can play a role in increasing the incidence of this disease, such as people traveling to a country with a high incidence of TB, and low socioeconomic status (Horna-Campos et al. Citation2011; Murthy et al. Citation2011; Riley Citation2021). Besides, domestic housekeepers and cleaners working in Gulf families who come from high-burden countries are also one of the reasons of increasing prevalence and incidence of this disease in this region (McKenna et al. Citation1996; Calvert et al. Citation2003; Bang et al. Citation2005; Chattu and Mohammad Citation2013; Vayr et al. Citation2018; Shafiei et al. Citation2019; Semilan et al. Citation2021).
The World Health Organization (WHO) has set targets to achieve a 90% decline in the incidence rate of TB and a 95% reduction in deaths caused by TB, with the ultimate goal of total elimination of TB worldwide by the end of 2035 (Sambas et al. Citation2020). According to the global TB mortality data from the WHO, the total number of TB deaths increased between 2019 and 2020. The number of deaths increased from 1.2 million to 1.3 million among HIV-negative people and from 209,000 to 214,000 among HIV-positive people (Global Tuberculosis Report Citation2021). The high death rate of TB in HIV-positive people can occur due to several factors, including HIV weakening the immune system, making it harder for the body to fight off infections like TB.
Saudi Arabia has undergone massive economic growth in recent years, which has contributed to the progress of social and health services. The arrival of a large number of foreign workers from various parts of the world has also been a contributing factor. Many of these workers came from countries with a high prevalence rate of TB, such as India, Bangladesh, Indonesia, Pakistan, and Yemen. This could be one of the reasons for the increasing incidence of TB in Saudi Arabia, which is measured as a moderate burden country for TB disease (Al-Hajoj and Varghese Citation2015). The current study aimed to analyze the frequency of diagnosed TB cases, the age-specific incidence rate, the year of diagnosis, and the prevalence of TB in various regions of Saudi Arabia. The study was based on the National Tuberculosis Program (NTP) data from 2014 to 2020.
Methods
This study was a cross-sectional study that included retrospective epidemiological data on pulmonary TB and extra-pulmonary TB. The data was based on the National Tuberculosis Program (NTP) from the Public Health Department, Ministry of Health, Kingdom of Saudi Arabia. The data used in compiling this cohort study was collected from January 2014 to December 2020. Since the epidemiological data was collected from the open access public domain through the NTP report, ethical clearance was not required for this study.
The pulmonary and extra-pulmonary TB patient data comprised sex, age, nationality, and regions were included. The TB incidence rate was calculated per 100,000 population for each region from the NTP reports. For the current study, the data was included for both Saudi and non-Saudi populations of Saudi Arabia. The study also calculated the overall percentage of pulmonary and extra-pulmonary TB cases among males and females. To correlate the overall percentage of pulmonary TB and extra-pulmonary TB cases between Saudi/non-Saudi males and Saudi/non-Saudi females, a t – test was conducted. GraphPad Prism software, version 6.0 (La Jolla, CA, USA) was used to draw the box and whisker plot. Microsoft Excel version 2019 was used for graphical presentations, comparisons, and data analysis. The p-value < 0.05 was considered as significant.
Results
Age-specific incidence rates of pulmonary TB and extra-pulmonary TB
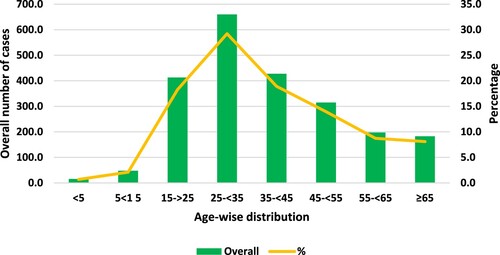
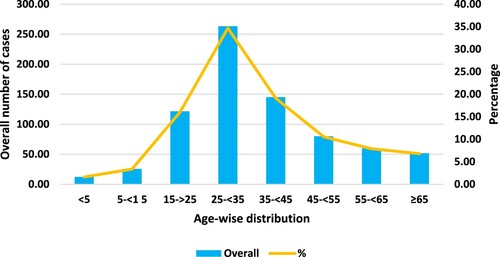
During the period from 2014 to 2020, the Ministry of Health received a total of 21,120 TB cases. Out of these, 15,806 (74.84%) cases were identified as pulmonary TB, while 5,314 (25.16%) cases were categorized as extra-pulmonary TB. From 2014 to 2020, Figures and illustrate that the age group of 25–35 had the highest overall age-specific incidence rate (AIR) and was most frequently affected by both pulmonary TB and extra-pulmonary TB. The occurrence of pulmonary TB and extra-pulmonary TB cases in the same age group 25–35 was 29.2% and 34.69%, respectively. In contrast, the age groups of 0–15 and 55–65 years were observed to have a lower incidence of both pulmonary TB and extra-pulmonary TB.
Incidence of pulmonary TB and extra-pulmonary TB among Saudi and non-Saudi populations
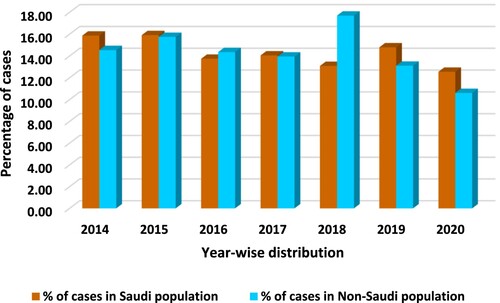
The overall non-Saudi population (8362 cases; 53%) was more affected by pulmonary TB in comparison to the Saudi population (7444 cases; 47%). It was noted that the incidence of pulmonary TB among the non-Saudi population was relatively low during the years 2017, 2019 and 2020. However, in the other years, the incidence of pulmonary TB in the non-Saudi population was slightly higher, but there was no significant difference (p = 0.107; which is greater than α = 0.05) observed on applying the t-test between the number of cases in Saudi and non-Saudi populations, as shown in Figure .
Figure 3. A graphical presentation of the overall percentage of pulmonary TB cases between the Saudi and non-Saudi population from 2014 to 2020.
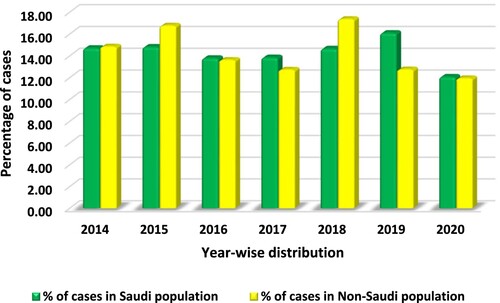
It appears that the overall non-Saudi population (2724 cases; 51.3%) was more affected by extra-pulmonary TB compared to the Saudi population (2590 cases; 48.7%). As per Figure , the overall percentage of extra-pulmonary TB incidences in the non-Saudi population was found to be high in only the year 2018. In the remaining years, the incidence rate was approximately the same in both populations. On applying the t-test, there was no significant difference observed between Saudi and non-Saudi populations in respect to total number of extra-pulmonary TB cases (p = 0.475).
Incidence of pulmonary TB and extra-pulmonary TB between the male and female populations
The total male population (11,216; 71%) was more affected by pulmonary TB than females (4592; 29%) as shown in Table . As well, the total number of males (3528; 66.4%) were also more affected by extra-pulmonary TB than females (1786; 33.6%) as shown in Table . Figure shows that a significant difference was observed between the percentages of Saudi male and female pulmonary TB positive cases (two – tailed; p < 0.000). A significant difference (two – tailed; p < 0.000) in overall percentage was observed between Saudi males (64.48%) and Saudi females (35.52%) affected by extra-pulmonary TB during the same period (Figure ). Interestingly, the highest overall percentage of Saudi male cases found to be positive for pulmonary TB (11.65%) and extra-pulmonary TB (10.12%) was in the year 2019 (Table ).
Figure 5. Box and whisker plot between the overall percentage of Saudi male and Saudi female pulmonary TB cases (p < 0.000) during 2014–2020.
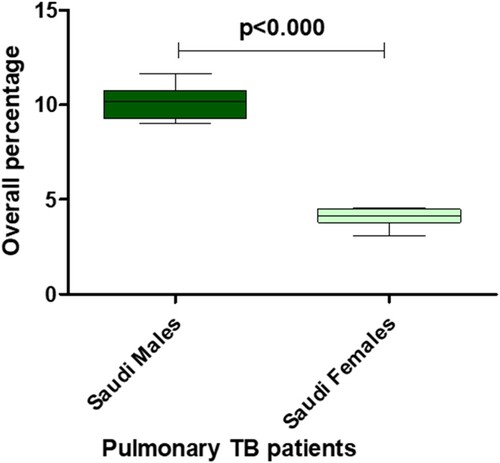
Figure 6. Box and whisker plot between the overall percentage of Saudi male and Saudi female extra-pulmonary TB cases (p < 0.000) during 2014–2020.
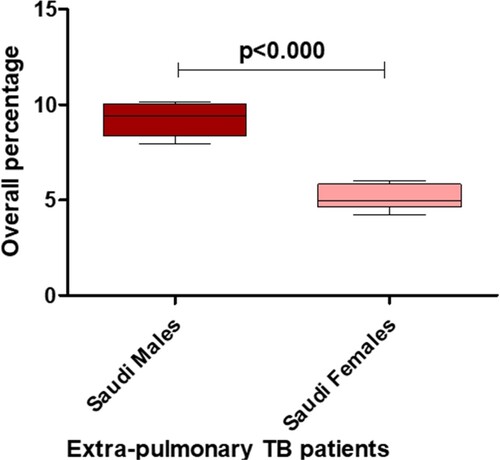
Table 1. Distribution of total number of Saudi and non-Saudi cases infected with pulmonary and extra-pulmonary TB cases with percentage.
Table 2. Total number of pulmonary and extra-pulmonary TB cases with percentage between the Saudi male and Saudi female population with the yearly distribution.
Similar to the Saudi population, the trend was also noted among non-Saudi males and females. According to Figure , the overall percentage of non-Saudi males (70.41%) affected by pulmonary TB was significantly higher than females (29.59%) (p < 0.000). From Figure , it can be observed that during the same period, the difference in the overall percentage affected by extra-pulmonary TB was statistically significant (p < 0.000) between non-Saudi males (68.21%) and non-Saudi females (31.79%). As per Table , it can be seen that in 2018, there were more non-Saudi male cases of pulmonary TB (13%) and extra-pulmonary TB (12.74%) recorded than non-Saudi females.
Figure 7. Box and whisker plot of the overall percentage of non-Saudi males and non-Saudi females with pulmonary TB (p < 0.000) from 2014 to 2020.
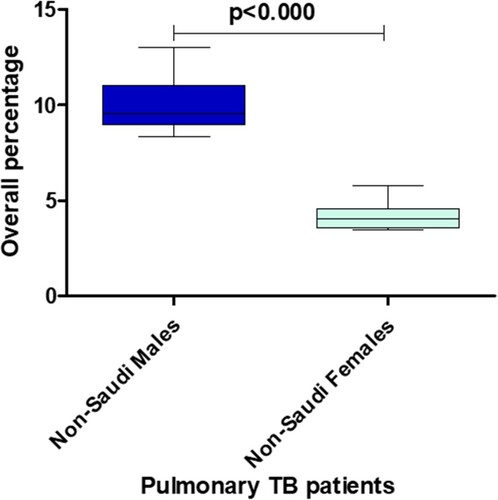
Figure 8. Box and whisker plot of the overall percentage of non-Saudi males and non-Saudi females with extra-pulmonary TB (p < 0.000) from 2014 to 2020.
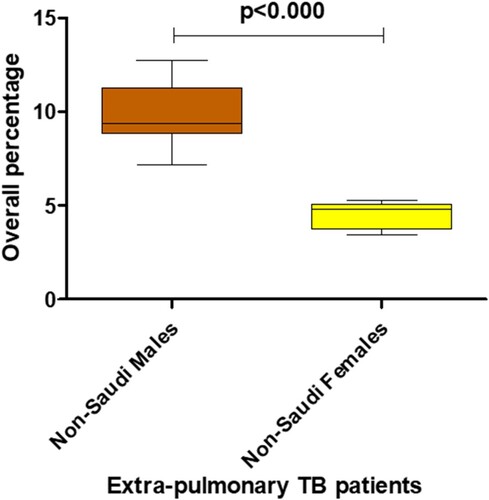
Table 3. Total number of pulmonary and extra-pulmonary TB cases with percentage between the non-Saudi male and non-Saudi female populations with the yearly distribution.
Incidence rate of pulmonary TB and extra-pulmonary TB among the different regions of Saudi Arabia
According to Figures and , the year 2015 had the highest incidence rate per 100,000 population of both types of TB, followed by the years 2014 and 2018. It can be observed that the maximum mean incidence rate per 100,000 population affected by pulmonary TB was noticed in Jeddah (13.77) and Jazan (11.18) during the years 2014–2020 (Figure ). Regions like Al-Ahsa, Bishah, Hail, and Al-Jouf were less affected by pulmonary TB, with mean incidence rates of around 2.59, 2.57, 2.69 and 2.53, respectively.
Figure 9. The total incidence rate of TB patients per 100,000 population in Saudi Arabia from 2014 to 2020.
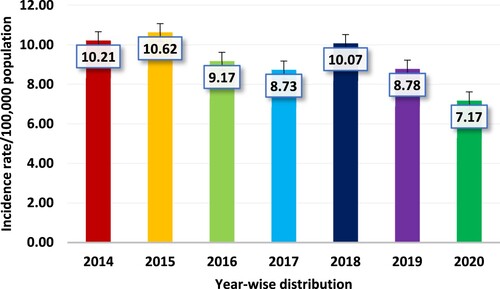
Figure 10. Graphical presentation of the total incidence rate per 100,000 population between pulmonary TB (PTB) and extra-pulmonary TB (Ex-PTB) in Saudi Arabia during 2014–2020.
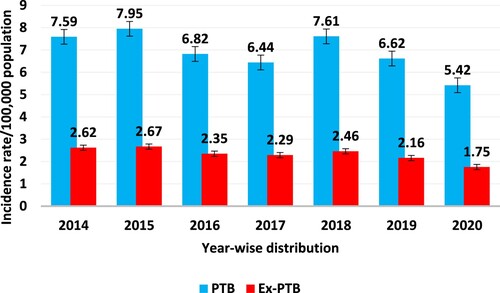
Figure 11. Graphical presentation of the mean incidence rate per 100,000 population in various regions of Saudi Arabia between pulmonary TB and extra-pulmonary TB cases during 2014–2020.
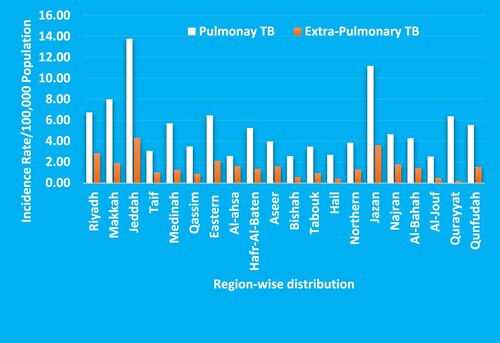
As well, the mean incidence rate per 100,000 population affected by extra-pulmonary TB was also higher in Jeddah (4.33) and Jazan (3.63) in the same time interval (Figure ). The population of Al-Qassim, Bishah, Tabouk, Hail, Al-Jouf, and Qurayyat regions of Saudi Arabia were less affected by extra-pulmonary TB than other regions.
Discussion
In accordance with the Global Tuberculosis Report Citation2021 by WHO, TB persists as a foremost health issue globally, and it was ranked among the top 10 causes of mortality worldwide (Global Tuberculosis Report Citation2021). It is also the major cause of death from a single infectious agent and the number of cases of this disease increased from 5.8 million new cases in 2012 to 10 million new cases in 2019 (Global Tuberculosis Report Citation2021). It is supposed that the increase in reported cases of TB is primarily due to an increase in the number of cases reported by both the public and private sectors (Global Tuberculosis Report Citation2021). The total number of pulmonary and extra-pulmonary TB cases in the Kingdom of Saudi Arabia in 2018, was 3364 cases with an incidence rate of 10.07 per 100,000. Moreover, in 2019 and 2020 there were 3004 cases with an incidence rate of 8.7 per 100,000 and 2511 cases with an incidence rate of 7.1 per 100,000 respectively. The present study aims to identify the AIR pattern from 2014 to 2020 among TB patients in Saudi Arabia. This is the first detailed epidemiological study that assessed the chronological distribution of pulmonary and extra-pulmonary TB cases among Saudi/non-Saudi males and females in different regions of Saudi Arabia, which is based on the NTP report of Saudi Arabia.
According to the current study, the highest age-specific overall mean for both pulmonary and extra-pulmonary TB was observed in the age group of 25–35 years. On the other hand, the lowest age-specific overall mean for TB was detected in the age groups of 0–15 and 55–65 years. It is interesting to note that another study based on the Saudi population has reported similar findings. The study found that the highest number of infections among the male non-Saudi population was observed in the age groups of 25–35 and 35–45, followed by 45–55 (El-Masry and Muzaheed Citation2022). The difference in the number of cases in the different age groups might be due to socioeconomic status, where in these age groups, there are a large number of unskilled workers who tend to live in crowded areas (Noykhovich et al. Citation2019).
It is interesting to note that the study found no significant difference in the overall percentage of both types of TB between the Saudi and non-Saudi populations. Although the study did not find a significant difference in the overall percentage of both types of TB between the Saudi and non-Saudi populations, it observed that non-Saudi residents of Saudi Arabia were more affected by pulmonary as well as extra-pulmonary TB as compared to Saudi nationals. Another study has reported similar findings that most non-Saudis in the country come from countries like India, Pakistan, Indonesia, Bangladesh, and Yemen, which have a higher burden of TB cases in comparison to other countries (Abouzeid et al. Citation2012). The majority of them are lower-earning workers and they prefer to live in the same area to avail the transportation provided by the company and this may be one of the reasons for transmitting this disease easily among workers (Kashyap et al. Citation2016; General Authority for Statistics Citation2021). The other possible reason for the high incidence among workers is the fear of being deported or losing their jobs if they are diagnosed with an infectious disease like TB; most non-Saudi workers try to avoid medical treatment or proper diagnosis, which could also be a factor in increasing the TB incidence rate in Saudi Arabia (Semilan et al. Citation2021).
As per the NTP report, the total male population affected by pulmonary and extra-pulmonary TB was observed to be more in comparison to females. There is a significant difference in the prevalence of pulmonary and extra-pulmonary TB between Saudi males and females from 2014 to 2020 (p < 0.0001). The prevalence of the overall percentage of non-Saudi males and non-Saudi females affected by pulmonary and extra-pulmonary TB in the same time frame showed the same trends, with a statistically significant difference (p < 0.0001). It is interesting to note that two studies have shown similar findings regarding the prevalence of TB among males and females. The study conducted by Semilan et al., which found that males were more affected by TB than females, is concerning (Semilan et al. Citation2021). The higher prevalence of TB among males may be due to their higher participation in the workforce and exposure to different environments such as companies, offices, and markets where the risk of TB transmission may be higher. The TB incidence rate per 100,000 population remained quite stationary during the studied period except for 2020. The lower incidence rate of TB in 2020 may be due to the measures taken to control the COVID-19 pandemic, such as the widespread use of face masks and restrictions on international travel. These measures may have inadvertently helped to reduce the spread of TB as well.
The incidence rate of pulmonary TB was observed to be higher in comparison to extra-pulmonary TB in the studied years. In addition, the highest incidence rates of pulmonary and extra-pulmonary TB were identified in Jeddah (a city located near to Makkah) and Jazan regions with the Riyadh and Dammam regions also. Other studies have found similar results regarding the incidence of TB in the Makkah region compared to other parts of Saudi Arabia. This highlights the need for targeted efforts to address the issue of TB in this region, such as increased awareness campaigns and resources for TB prevention and treatment. The high incidence of TB in the Makkah region could be due to various factors, such as the large number of immigrants and workers in the area (Abouzeid et al. Citation2012; Alzahrani et al. Citation2012; Almutairi et al. Citation2018). The influx of large numbers of pilgrims from other parts of the world, particularly from developing countries, could contribute to the spread of TB in Saudi Arabia. So, this region may be more susceptible to the transmission of tuberculosis (Ahmed et al. Citation2016; Saati et al. Citation2021). The National Tuberculosis Program and healthcare services must target populated areas, with special attention to non-Saudi workers who are at high risk of TB. By focusing efforts on these areas and populations, we can help to prevent and control the spread of the disease.
Conclusions
According to the study's findings, both male Saudi and non-Saudi populations were more affected by TB compared to females. This suggests that targeted efforts to improve TB control measures should prioritize the male population in both Saudi and non-Saudi communities. The age group of 25–35-year-olds had the highest overall AIR of pulmonary and extra-pulmonary TB. The highest overall mean incidence rate of TB cases was reported in the Jeddah and Jazan regions, followed by Riyadh, Makkah, and Eastern regions. The study's findings have important implications for TB control efforts in Saudi Arabia. By providing valuable epidemiological information on TB incidence rates among both Saudi and non-Saudi populations, the study can help guide the development of targeted interventions and policies to address this public health issue. Based on the study's findings, it may be recommended that immigrants to Saudi Arabia from high-risk countries should prioritize regular health check-ups to reduce the incidence of tuberculosis. This can help identify and treat cases of TB early, potentially preventing the spread of the disease to others. This is especially important given the higher risk of TB transmission in certain regions of Saudi Arabia, such as the Makkah region.
Limitations of the study
The data used in this study were acquired from the National Tuberculosis Program, Public Health Department, Ministry of Health, and Kingdom of Saudi Arabia. Limitations include information on drug resistance and clinical data regarding treatment and follow up of the patients was not available. The pulmonary and extra-pulmonary TB patient data only comprised sex, age, nationality, and regions in this study.
Acknowledgements
The Researchers would like to thank the Deanship of Graduate Studies and Scientific Research at Qassim University for financial support (QU-APC-2024-9/1).
Data availability statement
The raw data that support the findings of this study are available in National Tuberculosis Program, Public Health Department, Ministry of Health, Kingdom of Saudi Arabia at https://www.moh.gov.sa/en/Ministry/Statistics/book/Pages/default.aspx’. Additional supporting information is publicly available in the figshare repository at https://doi.org/10.6084/m9.figshare.25931920.v1
.Disclosure statement
sNo potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Abouzeid MS, Zumla AI, Felemban S, Alotaibi B, O’Grady J, Memish ZA. 2012. Tuberculosis trends in Saudis and non-Saudis in the Kingdom of Saudi Arabia–a 10 year retrospective study (2000–2009). PLoS One. 7(6):e39478. doi:10.1371/journal.pone.0039478.
- Ahmed MM, Velayati AA, Mohammed SH. 2016. Epidemiology of multidrug-resistant, extensively drug resistant, and totally drug resistant tuberculosis in Middle East countries. Int J Mycobacteriol. 5:249–256. doi:10.1016/j.ijmyco.2016.08.008.
- Al-Hajoj S, Varghese B. 2015. Tuberculosis in Saudi Arabia: the journey across time. J Infect Dev Ctries. 9:222–231. doi:10.3855/jidc.5296.
- Almatroudi A. 2021. A retrospective cohort study of lung cancer incidences and epidemiological analysis in Saudi Arabian Population from 2006 to 2016. Int J Environ Res Public Health. 18:11827. doi:10.3390/ijerph182211827.
- Almatroudi A. 2022. Non-coding RNAs in tuberculosis epidemiology: platforms and approaches for investigating the Genome’s Dark matter. Int J Mol Sci. 23:4430. doi:10.3390/ijms23084430.
- Almutairi FM, Tayeb T, Alhakeem R, Saeed AB, Assiri A, McNabb SJN. 2018. Distribution and determinants of tuberculosis in the Kingdom of Saudi Arabia from 2005 to 2012. J Epidemiol Glob Health. 7(Suppl 1):S23–S28.
- Alzahrani AG, Choudhry AJ, Al Mazroa MA, Turkistani AH, Nouman GS, Memish ZA. 2012. Pattern of diseases among visitors to Mina health centers during the Hajj season, 1429 H (2008 G). J Infect Public Health. 5(1):22–34. doi:10.1016/j.jiph.2011.10.003.
- Bang KM, Weissman DN, Wood JM, Attfield MD. 2005. Tuberculosis mortality by industry in the United States, 1990–1999. Int J Tuberc Lung Dis. 9:437–442.
- Calvert GM, Rice FL, Boiano JM, Sheehy JW, Sanderson WT. 2003. Occupational silica exposure and risk of various diseases: an analysis using death certificates from 27 states of the United States. Occup Environ Med. 60:122–129. doi:10.1136/oem.60.2.122.
- Chattu VK, Mohammad A. 2013. Tuberculosis an important global health issue in this era—A cross sectional study of epidemiology of TB among South Asian workers in Saudi Arabia. Indian J Public Health. 4:278. doi:10.5958/j.0976-5506.4.2.060.
- El-Masry OS, Muzaheed. 2022. Incidence and assessment of demography-related risk factors associated with pulmonary tuberculosis in Saudi Arabia: a retrospective analysis. Pak J Med Sci. 38(4Part-II):850–854.
- General Authority for Statistics. 2021. [accessed 2021 Feb 19]. https://www.stats.gov.sa/en.
- Global Tuberculosis Report. 2021. WHO report. Geneva: World Health Organization.
- Guler SA, Bozkus F, Inci MF, Kokoglu OF, Ucmak H, Ozden S, Yuksel M. 2015. Evaluation of pulmonary and extrapulmonary tuberculosis in immunocompetent adults: a retrospective case series analysis. Med Princ Pract. 24(1):75–79. doi:10.1159/000365511.
- Guo Z, Xiao D, Wang X, Wang Y, Yan T. 2019. Epidemiological characteristics of pulmonary tuberculosis in mainland China from 2004 to 2015: a model-based analysis. BMC Public Health. 19(1):219. doi:10.1186/s12889-019-6544-4.
- Horna-Campos OJ, Consiglio E, Sánchez-Pérez HJ, Navarro A, Caylà JA, Martín-Mateo M. 2011. Pulmonary tuberculosis infection among workers in the informal public transport sector in Lima, Peru. Occup Environ Med. 68:163–165. doi:10.1136/oem.2009.051128.
- Kashyap RS, Nayak AR, Husain AA, Shekhawat SD, Satav AR, Jain RK, Raje DV, Daginawala HF, Taori GM. 2016. Impact of socioeconomic status and living condition on latent tuberculosis diagnosis among the tribal population of Melghat: a cohort study. Lung India. 33:372. doi:10.4103/0970-2113.184868.
- McKenna MT, Hutton M, Cauthen G, Onorato IM. 1996. The association between occupation and tuberculosis. A population based survey. Am J Respir Crit Care Med. 154:587–593. doi:10.1164/ajrccm.154.3.8810591.
- Murthy KAS, Kiran HS, Cheluvaraj V, Balaji B. 2011. Young lady with a swelling over the back: a rare case of tuberculosis. Iran J Med Sci. 36:318–321.
- National Tuberculosis Program. 2021. Kingdom of Saudi Arabia, Manual. Accessed at https://www.moh.gov.sa/Documents/National-TB-program.pdf.
- Noykhovich E, Mookherji S, Roess A. 2019. The risk of tuberculosis among populations living in slum settings: a systematic review and meta-analysis. J Urban Health. 96:262–275. doi:10.1007/s11524-018-0319-6.
- Riley L. 2021.Tuberculosis: natural history, microbiology, and pathogenesis. Up To Date. T.W. Post (editor). (Up to Date Inc., 2021) [accessed 2021 Feb 19]. https://www.Uptodate.com/contents/tuberculosis-natural-history-micro biology-and-pathogenesis.
- Saati AA, Khurram M, Faidah H, Haseeb A, Iriti M. 2021. A Saudi Arabian public health perspective of tuberculosis. Int J Environ Res Public Health. 18(19):10042. doi:10.3390/ijerph181910042.
- Sambas MFMK, Rabbani U, Al-Gethamy MMM, Surbaya SH, Alharbi FFI, Ahmad RGA, Qul HKH, Nassar SMS, Maddah AKMA, Darweesh BAK. 2020. Prevalence and determinants of multidrug-resistant tuberculosis in Makkah, Saudi Arabia. Infect Drug Resist. 13:4031–4038. doi:10.2147/IDR.S277477.
- Semilan HM, Abugad HA, Mashat HM, Wahab MMA. 2021. Epidemiology of tuberculosis among different occupational groups in Makkah region, Saudi Arabia. Sci Rep. 11(1):12764. doi:10.1038/s41598-021-91879-9.
- Shafiei M, Ghasemian A, Eslami M, Nojoomi F, Rajabi-Vardanjani H. 2019. Risk factors and control strategies for silicotuberculosis as an occupational disease. New Microbes New Infect. 27:75–77. doi:10.1016/j.nmni.2018.11.002.
- Vayr F, Martin-Blondel G, Savall F, Soulat JM, Deffontaines G, Herin F. 2018. Occupational exposure to human Mycobacterium bovis infection: a systematic review. PLoS Negl Trop Dis. 12.