ABSTRACT
Purpose
Bilateral cleft lip and palate (BCLP) are severe congenital anomalies. The cleft interferes with the normal growth of the maxilla, leading to deficient midfacial development. The aim of the present study was to evaluate the short-term influence of preoperative nasoalveolar moulding (NAM) therapy on maxillary arch dimensions in patients with BLCP.
Materials and methods
18 newborns (male: 12; female: 6) were recruited who underwent NAM therapy before cheiloplasty. The pre- (T0) and post-NAM (T1) plaster casts of the maxilla were scanned using a laboratory scanner. The measured parameters on the digital casts included premaxilla width, right and left alveolar cleft width, right and left molar region length, anterior interalveolar-, intercanine-, intermolar-, intertuberosity width, palatal length and anterior basal angle.
Results
Both left (p = 0.047) and right (p = 0.019) alveolar clefts significantly reduced in size at T1. A significant expansion in premaxilla width was detected (p = 0.037). Anterior basal angle showed a significant increase too. Except for the intermolar width (p = 0.045), no significant changes were identified in the transversal dimensions.
Conclusion
NAM therapy could potentially serve as an effective tool in mitigating the severity of bilateral cleft deformities at a short-term interval without interfering with maxillary growth. However, long-term studies are required to confirm the effectiveness of the therapy.
Introduction
Cleft lip and palate (CLP) are common congenital malformations, with a global incidence of approximately 1 in 400–500 individuals [Citation1]. The extent of CLP can vary from a small lip cleft to a complete cleft affecting the lip, alveolar crest, and palate, presenting either bilaterally or unilaterally [Citation2]. Amongst various CLP subtypes, bilateral cleft lip and palate (BCLP), a severe variant of CLP, presents numerous intricate challenges to patients and practitioners [Citation3]. It leads to a disrupted and often asymmetric facial development [Citation4]. Furthermore, it can cause not only dental and aesthetic complications but also difficulties in feeding and speech. The treatment process for BCLP can be complex and extended, necessitating numerous surgical procedures often spanning from childhood through adolescence to adulthood [Citation5]. As facial development continues until puberty or even later in some aspects, hence the selection and scheduling of appropriate interventions need to be specifically tailored to each patient. This necessitates a multidisciplinary treatment approach for optimal results, involving various specialists such as general dentists, orthodontists, maxillofacial surgeons, otorhinolaryngologists, paediatricians and speech therapists [Citation6].
Patients with BCLP are often characterized by a protrusive premaxilla which is caused by a tri-segmental alveolar bone defect, where the cleft causes a separation of the premaxilla from the lateral segments [Citation7]. Consequently, this disrupts the growth of the palate, and lead to a deformation of the maxillary segment with midfacial hypoplasia. If this deformity is not corrected orthopaedically, a surgeon might have to perform additional surgical procedures, such as lip adhesion and staging of cleft sides [Citation8]. To overcome this problem, presurgical nasoalveolar moulding (NAM) has emerged as a successful option that applies targeted forces to shape the alveolus, nasal cartilage and columella [Citation9]. Consequently, resulting in a decrease in the cleft width and premaxillary protrusion, improved arch shape, increase in symmetry between the lateral nasal cartilages, and increase in the projections of nasal tip and columella length. The alignment of tissues by the NAM appliance before primary BCLP repair has benefits of improved lip and nasal form, stable long-term outcomes and reduced number of surgical revisions [Citation10]. The efficacy of NAM therapy is significantly enhanced when initiated at the earliest opportunity, optimally within the first month of life [Citation11].
While the influence of NAM on maxillary dimensions in cases of unilateral clefts has been extensively studied, research on BCLP is limited due to its rarity, constituting only 4% of orofacial clefts [Citation12]. Furthermore, the majority of the BCLP studies have focussed primarily on short- and long-term nasolabial morphological changes [Citation13]. Hence, it is crucial to evaluate alterations in maxillary arch dimensions prior to cheiloplasty to quantitatively comprehend the oral structural changes in these patients. Moreover, conflicting evidence exits related to the influence of NAM on maxillary arch, where some studies suggest restrained maxillary growth, while others have reported significantly higher changes in arch dimensions in the first six month [Citation14].
Therefore, the following study was undertaken to assess the immediate impact of NAM therapy on maxillary morphology in patients with BCLP utilizing scanned dental cast models.
Materials and methods
Nasoalveolar moulding technique
The moulding process began with an impression taken during the first few weeks post-birth, utilizing alginate impression material. During this procedure [Citation15], precautions were taken to ensure the airway remained clear and prevent aspiration of the material by depressing the tongue.
The fabrication of the palatal plate was made by technicians in the dental laboratory. The plaster casts were blocked out with wax, then acrylic powder was distributed on the surface, then mixed with the liquid resin. After curing in a high-pressure cooker, all surfaces were polished. As outlined by Chen et al. [Citation16], the inner surface of the guidance plate, which covers the vestibular surface of the premaxillary segment, was lined with a silicon-based denture liner. This liner ensured a constant pressure was applied to the premaxilla.
The inner surface adjustment of the plate was done chairside by orthodontists. Wherever additional pressure was needed, a light cured resin was applied on the surface. In order to create space in the direction of the required growth, material was removed using a handheld bur. The guidance plate was secured in place using denture adhesive and two buttons affixed to the cheeks with adhesive tape. The adhesive tape allowed to approximate the upper lip segments and premaxilla closer together and reduce the size of the fissures. The nasal stents were incorporated also chairside by the orthodontist once the distance between the alveolar segments had been reduced to 5 mm (). They were bent from stainless steel orthodontic wire, and the nasal pads were created from flow composite. If the nasal stent is introduced to a nostril that is overlying a very wide alveolar gap, it may stretch further the nostril rim and increase nostril circumference. This may result in a postsurgical ‘mega-nostril’ [Citation17]. These stents were gradually activated to extend the columella and achieve optimal nasal tip projection. The plate was adjusted weekly to guide the segments towards a more normal position. Alginate impressions were acquired again just after the NAM therapy completion and casts were fabricated.
All NAM devices were produced manually in the dental lab by the same team of dental technicians. Daily use of the NAM device was required. The participation of caregivers was indispensable as their duties included changing the aforementioned adhesive tape and constantly cleaning and repositioning the palatal plate. During the follow-up visits, an orthodontist adjusted the device to guide the growth of the lateral maxillary segments and form the nasal cartilages.
Maxillary arch analysis
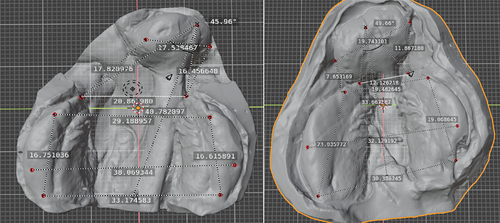
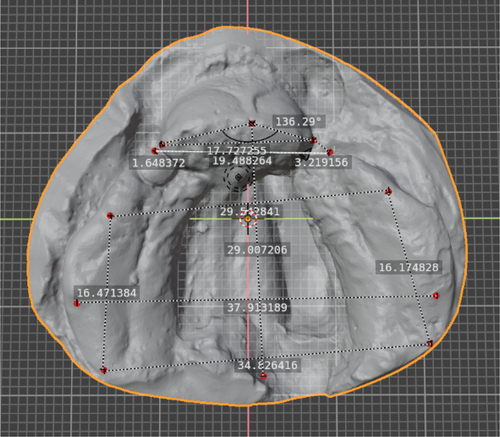
The pre- (T0) and post-NAM (T1) plaster casts of the maxilla were scanned using a D500 3D dental scanner (3Shape GmbH, Düsseldorf, Germany) with a resolution of 0.1 mm. Thereafter, virtual models of the casts were uploaded to Blender software (Version 3.6.5, Blender Foundation, Amsterdam, Netherlands) for the assessment of maxillary arch’s dimensional changes at T0 and T1 time-points. The morphometric analysis was conducted using a method proposed by Mazaheri et al. [Citation18], where 12 landmarks were annotated on the digital models for performing linear and angular measurements (). The measured parameters based on the landmarks included, premaxilla width, right and left alveolar cleft width, right and left molar region length, anterior interalveolar width, intercanine width, intermolar width, intertuberosity width, palatal length and anterior basal angle (). provides an example of a patient with linear and angular dimensional measurements at T0 and T1 time-points. All measurements were performed twice by a single observer with an experience of over 4 years in oral and maxillofacial surgery, at an interval of 1 week for assessing the interobserver reliability.
Figure 2. Landmarks of maxillary arch: 1. apex of ridge situated on line demarcating labial frenulum and incisive papilla, 2. rightmost boundary of premaxilla, extending from alveolar ridge, 3. Anterior most point on right maxillary segment, 4. distal boundary of canine protuberance on right maxillary segment, 5. Distal boundary of molar protuberance on right maxillary segment, 6. tuberosity point on right maxillary segment, 7. leftmost boundary of premaxilla, extending from the alveolar ridge, 8. Anterior most point on left maxillary segment, 9. distal boundary of the canine protuberance on the left maxillary segment, 10. distal boundary of molar protuberance on right maxillary segment, 11. Tuberosity point on left maxillary segment, 12. reference point located at base of a perpendicular line drawn from landmark 1 to line connecting segments from reference points 6 and 11.
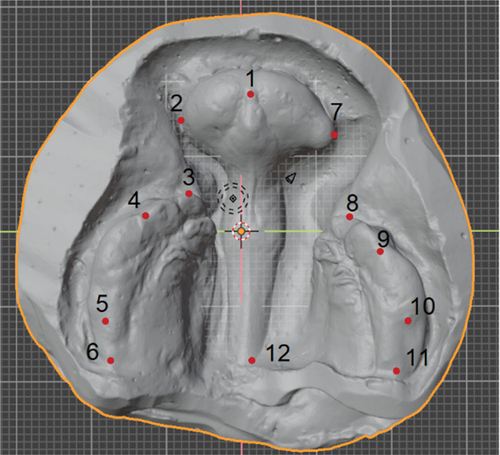
Figure 3. Measurements based on maxillary arch landmarks: premaxilla width (2–7), right (2–3) and left (7–8) alveolar cleft width, right (4–6) and left (9–11) molar region length, anterior interalveolar width (3–8), intercanine width (4–9), intermolar width (5–10), intertuberosity width (6–11), palatal length (1–12) and anterior basal angle (3-1-8).
Statistical analysis
Data were analysed using R Studio 3.4.2 (Boston, MA, USA). Mean and standard deviation values at were calculated for maxillary arch dimensions at both T0 and T1 timepoints. A paired T-test was performed to compare the differences between T0 and T1. Moreover, a two-way analysis of variance (ANOVA) was used to assess maxillary arch dimensions in relation to the alveolar cleft width. A p-value of less than 0.05 was considered as statistically significant. For the sample calculation, we employed Andrew Fisher’s formula with a 95% confidence level, 11.01 confidence interval, and standard deviation of 0.5. These parameters were chosen based on the specific requirements of our study and the available data.
Results
A total of 18 patients (mean age: 12 days ±5) were recruited who underwent preoperative NAM therapy before cheiloplasty. Twelve of the patients were male (66.7%), while six of them were female (33.3%). The frequency of BCLP cases was more considerable among male than female patients, which is consistent with the existing literature indicating that bilateral clefts appear more often in boys than in girls [Citation19].
The therapy was initiated prior to the infants reaching six weeks of age, taking benefit of the nasal cartilages’ malleability. It concluded within 3–4 months, with patients averaging six months of age at completion. At this point, the columella length had increased to 3–5 mm with an optimal contact of the alveolar segments, and lip segments had approximated without tension. illustrates an example of a patient pre- and post-NAM therapy.
Figure 5. Patient with bilateral cleft lip and palate before (left) and after (right) nasoalveolar moulding.

All landmark placements and measurements showed an excellent reliability (ICC: 0.99). describes the mean changes of maxillary dimensions at T0-T1 time-intervals. Both left (p = 0.047) and right (p = 0.019) alveolar clefts significantly reduced in size at T1. A significant increase in premaxillary width was also observed (p = 0.037) with a slight non-significant reduction in palatal length (p = 0.305). Apart from intermolar width (p = 0.045), no significant changes were observed for anterior inter-alveolar, canine, and tuberosity widths. In addition, NAM therapy resulted in a significantly high change in anterior basal angle (p = 0.043).
Table 1. Maxillary arch dimensional changes following nasoalveolar moulding. Statistical significance (*), p < 0.05.
While assessing the impact of cleft severity on maxillary dimensions, the findings suggested that a decrease in the cleft size caused a significant reduction in premaxilla width (p-value <0.001). Moreover, the reduction in cleft size also showed a significant increase (p-value <0.001) in anterior basal angle. No other significant findings were detected (p > 0.05).
Discussion
Patients with BCLP require a combination of surgical and non-surgical treatments to achieve the desired functional and aesthetic outcome [Citation20]. There are several presurgical procedures designed to reduce the deformity, NAM playing a key role in restoring the defect as a part of the treatment plan [Citation21]. While NAM can bring the cleft segments closer together in preparation for surgical closure in unilateral cases, it’s crucial to evaluate its impact on the maxillary arch in BCLP patients. This aspect has been the subject of only a few studies due to the low incidence of BCLP [Citation22]. Therefore, this study was conducted to assess the changes in maxillary dimensions following NAM therapy. The analysis of the maxillary arch was conducted using laser-scanned digital models, a method that has demonstrated high reliability and validity for such assessments [Citation23].
The influence of NAM therapy on midface and maxillary arch parameters is currently a topic of ongoing debate. Research conducted by Tankittiwat et al. [Citation24] demonstrated that NAM therapy could potentially increase the length of the alveolus. Ross [Citation25] proposed that orthopaedic correction could accelerate the transversal growth of the maxilla, subsequently reducing the size of the cleft. In a long-term study spanning up to 18 years, Grayson and his team [Citation26] found that this non-surgical intervention did not hinder the growth of the maxillary arch. This finding was corroborated by a study conducted by Lee et al. [Citation27], which followed patients from ages 9 to 13 years and concluded that NAM therapy did not affect midface growth. Moreover, it was reported that NAM therapy promoted normal facial growth in 60% of patients with clefts. However, contrasting findings were presented by Ras et al. [Citation28], who suggested that the forces exerted during distraction could potentially disrupt the growth centre of the premaxilla, thereby impeding normal midface growth. This was further supported by a long-term study by Alhayyan et al., which confirmed that NAM therapy did not influence midface symmetry [Citation29].
The findings of the present study suggested a significant increase in premaxilla width, which was in agreement with a prior study, where the authors identified significant influence of alveolar bone apposition on premaxilla dimensions, linked with incisor development and eruption [Citation30]. Additionally, our findings observed an enlargement in both intermolar and intertuberosity widths. A comparison of maxillary arch development in children with BCLP and those without clefts during their initial four years of life by Heidbuchel et al. [Citation31], revealed increased tuberosity width in both cohorts, suggesting that the NAM appliance likely does not hinder maxillary arch growth. Conversely, the intercanine width in the present study exhibited a negligible and statistically insignificant increase, aligning with earlier studies that reported minor changes in intercanine width in BCLP patients and slight width alterations in children without clefts. Kiya et al. [Citation32], who investigated a fixed active plate combined with an elastic chain, also reported an insignificant rise in intercanine width. The most plausible explanation for these observations could be that the cleft defect potentially restricts growth in the anterior region compared to the posterior region. Furthermore, our study found an increase in the anterior basal angle and a significant enhancement in angulation due to cleft defect reduction, which subsequently improved premaxilla rotation. These findings suggest that the premaxilla might have moved closer to the palate medially, thereby reducing the size of the cleft.
In the context of cleft width, a decrease was observed at T1, a finding that aligns with previous studies that utilized NAM devices and fixed active plates in conjunction with elastic chains as per Grayson’s presurgical NAM for BCLP treatment. The primary factor contributing to the reduction in cleft severity could be attributed to the use of lip strapping and a retraction plate [Citation33]. Concurrently, a slight decrease in palatal length was noted, potentially due to the elongation of the alveolar ridge as a result of maxillary growth. However, the actual impact of the NAM remains unclear due to the challenge in differentiating between therapeutic effects and natural growth, given the absence of a control group and ethical constraints [Citation34].
The NAM therapy in present study was initiated before the six-week mark, as this therapy is believed to be more beneficial when started as soon as possible after birth [Citation35]. The high level of hyaluronic acid in a newborn makes the cartilage extremely flexible, susceptible, and adaptable to new positions. The outlined surgical protocol is both straightforward and effective in managing the premaxilla and has shown satisfactory results in addressing the dental arch. Despite the labour-intensive nature of this treatment sequence, it offers a solution for the complex task of treating BCLP. The NAM protocol could be a valuable addition to the array of tools available to a cleft surgeon [Citation36].
Medical institutions that do not employ presurgical orthopaedic therapy before primary lip surgery have observed that around 83% of patients are prone to developing a noticeable anterior overbite between the ages of 5 and 7 years. This is attributed to the downward shift of the premaxilla and could potentially increase the frequency of surgeries needed to reposition the premaxilla during secondary alveolar bone graft procedures [Citation37]. Some researchers have reported that approximately half of their patients with BCLP require surgery to reposition the premaxilla. However, NAM therapy can present several challenges, including feeding difficulties, skin irritation, and caregivers’ inability to correctly position and secure the appliance. These factors can adversely impact the expected outcomes of the treatment. Despite this, prior studies indicate that while the care burden for patients undergoing NAM treatment is relatively high, caregivers remain dedicated to improving the therapy’s effectiveness [Citation38].
The research encountered several limitations. Firstly, the retrospective design of the study inherently introduced potential confounding bias. Furthermore, the absence of a control group may have inadvertently biased the findings. Ideally, a group without NAM should have been included at the same time points. However, this is difficult to achieve in a single institution where most patients follow the same treatment protocol. Secondly, the study’s generalizability may be restricted due to the recruitment of patients with BCLP from a single craniofacial centre. To obtain more generalizable results, future multicenter trials should be conducted that follow similar treatment protocol. Thirdly, the limited sample size due to the low incidence of the deformity and short-term follow-up necessitates further studies to evaluate long-term outcomes with a larger sample. The incidence of facial cleft in the Hungarian population is 2.02‰ [Citation39], further limiting the available pool of potential subjects. Additionally, logistical constraints such as age-related movements of patients and the need for proper evaluation of plaster samples further reduced our effective sample size.
Despite these challenges, we took proactive measures to optimize our sample size. Collaborating with a research team in Belgium, we aimed to augment our sample by leveraging their resources and patient pool. The ongoing collection of data on current and future patients will eventually enhance this study’s statistical robustness. Fourthly, performing intraoral impressions on an infant at the specified time points carries some risks to the patient and may result in precision variations. The advent of small intraoral scanning devices may provide a safer and more precise dataset, eliminating the need for a physical impression. Lastly, this study only evaluated the maxillary arch. It would be intriguing to assess both short- and long-term nasolabial soft tissue morphology, dentition emergence, occurrence of impacted or ectopic tooth buds, and occlusal function.
The NAM therapy demonstrated a substantial decrease in the maxillary arch deformity associated with BCLP. Moreover, this device played a crucial role in aligning the premaxilla without hindering maxillary growth. The alignment facilitated by this device could lead to superior surgical outcomes by enabling a tension-free closure of the lip segments.
Author contributions
Conceptualization, Krisztián Nagy; Methodology, Dominika Magyar; Validation, Krisztián Nagy, Laura Pálvölgyi; Formal Analysis, Laura Pálvölgyi; Investigation, Gwen Swennen, Krisztián Nagy; Resources, Gwen Swennen, Krisztián Nagy; Writing, Dominika Magyar, Laura Pálvölgyi; Review & Editing, Sohaib Shujaat, Krisztián Nagy; Supervision, Krisztián Nagy.
All authors agree to be accountable for all aspect of the work.
Ethical approval
This retrospective study was conducted in compliance with the World Medical Association Declaration of Helsinki on medical research. Ethics approval was acquired from the Medical Ethics Committee of Semmelweis University and St John’s Hospital Bruges-Oostende (Ethical Committee approval No. 265/2019). Written informed consent was obtained from the parents/guardians of all patients before enrolment in the study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Salari N, Darvishi N, Heydari M, et al. Global prevalence of cleft palate, cleft lip and cleft palate and lip: A comprehensive systematic review and meta-analysis. J Stomatol Oral Maxillofac Surg. 2022 Apr;123(2):110–120. doi: 10.1016/j.jormas.2021.05.008 Epub 2021 May 24. PMID: 34033944.
- Martin SV, Swan MC. An essential overview of orofacial clefting. Br Dent J. 2023 Jun;234(12):937–942. doi: 10.1038/s41415-023-6000-9 Epub 2023 Jun 23. PMID: 37349450.
- Hattori Y, Pai BC, Saito T, et al. Long-term treatment outcome of patients with complete bilateral cleft lip and palate: a retrospective cohort study. Int J Surg. [cited 2023 Jun 1];109(6):1656–1667. doi: 10.1097/JS9.0000000000000406 PMID: 37073546; PMCID: PMC10389451.
- Bartzela TN, Carels C, Maltha JC. Update on 13 Syndromes affecting craniofacial and dental structures. Front Physiol. [cited 2017 Dec 14];8:1038. doi: 10.3389/fphys.2017.01038 PMID: 29311971; PMCID: PMC5735950.
- Morris L. Management of the protuberant premaxilla: where does it fit in? Curr Opin Otolaryngol Head Neck Surg. 2019 Aug;27(4):302–309. doi: 10.1097/MOO.0000000000000558 PMID: 31219831.
- Hartzell LD, Kilpatrick LA. Diagnosis and management of patients with clefts: a comprehensive and interdisciplinary approach. Otolaryngol Clin North Am. 2014 Oct;47(5):821–852. doi: 10.1016/j.otc.2014.06.010 PMID: 25213284.
- Millard DR Jr, editor. Bilateral Cleft Anatomy In: cleft Craft. In: Bilateral and Rare Deformities. Vol. II. Boston (MA): Little Brown; 1977. p. 19–39.
- Manosudprasit M, Wangsrimongkol T, Pisek P, et al. Pre-surgical nasoalveolar molding technique: a literature review. J Med Assoc Thai. 2014 Oct;97(10):S17–24. PMID: 25816533.
- Grayson BH, Maull D. Nasoalveolar molding for infants born with clefts of the lip, alveolus, and palate. Semin Plast Surg. 2005 Nov;19(4):294–301. doi: 10.1055/s-2005-925902 PMCID: PMC2884748.
- Rubin MS, Clouston S, Ahmed MM, et al. Assessment of presurgical clefts and predicted surgical outcome in patients treated with and without nasoalveolar molding. J Craniofac Surg. 2015 Jan;26(1):71–75. doi: 10.1097/SCS.0000000000001233 PMID: 25534051; PMCID: PMC4289121.
- Shetty V, Thakral A, Sreekumar C. Comparison of early onset nasoalveolar molding with patients who presented for molding up to 1 year of age. J Oral Maxillofac Surg. 2016 Apr;74(4):811–827. doi: 10.1016/j.joms.2015.08.004 Epub 2015 Aug 11. PMID: 26341679.
- Woo AS. Evidence-based medicine: Cleft palate. Plast Reconstr Surg. 2017 Jan;139(1):191e–203e. doi: 10.1097/PRS.0000000000002854 PMID: 28027255.
- Harrison LM, Hallac RR, Derderian CA. Three-dimensional analysis of bilateral cleft lip and palate nasal deformity. Cleft Palate Craniofac J. 2021 Jan;58(1):105–113. doi: 10.1177/1055665620940190 Epub 2020 Jul 21. PMID: 32691613.
- Dunworth K, Porras Fimbres D, Trotta R, et al. Systematic Review and Critical Appraisal of the Evidence Base for Nasoalveolar Molding (NAM). Cleft Palate Craniofac J. 2022 Nov;4(4):654–677. doi: 10.1177/10556656221136325 Epub ahead of print. PMID: 36330703.
- Nemes B, Fábián G, Nagy K. Management of prominent premaxilla in bilateral cleft lip and alveolus. The Cleft Palate Craniofac J. 2013;50(6):744–746. doi: 10.1597/12-019
- Chen KT, Noordhoff MS, Liao YF, et al. An integrated approach to the primary lip/nasal repair in the bilateral cleft lip and palate. Noordhoff Craniofac Found. 2008:24–38.
- Shetye PR, Grayson BH. NasoAlveolar molding treatment protocol in patients with cleft lip and palate. Semin Orthod. 2017;23(3):261–267. doi: 10.1053/j.sodo.2017.05.002
- Mazaheri M, Harding RL, Cooper JA, et al. Changes in arch form and dimensions of cleft patients. Am J Orthod. 1971 Jul;60(1):19–32. doi: 10.1016/0002-9416(71)90179-5 PMID: 5281449.
- Harville EW, Wilcox AJ, Lie RT, et al. Cleft lip and palate versus cleft lip only: are they distinct defects? Am J Epidemiol. 2005;162(5):448–453. doi: 10.1093/aje/kwi214
- McIntyre JK, Sethi H, Schönbrunner A, et al. Number of surgical procedures for patients with cleft lip and palate from birth to 21 years old at a single children’s hospital. Ann Plast Surg. 2016 May;76(3):S205–8. doi: 10.1097/SAP.0000000000000765 PMID: 27070669.
- Shetye PK, Grayson BH. Nasoalveolar molding treatment protocol in patients with cleft lip and palate. Semin Orthodont. 2017;23(3):261–267. doi: 10.1053/j.sodo.2017.05.002
- Ocak I, Akarsu-Guven B, Karakaya J, et al. Effects of nasoalveolar molding on maxillary arch dimensions and malocclusion characteristics in primary dentition patients with cleft lip and palate. Int J Paediatr Dent. [2023 Jun 23];34(1):94–101. doi: 10.1111/ipd.13102 Epub ahead of print. PMID: 37351851.
- Verma S, Singh S, Verma K, et al. Three dimensional changes of maxillary arch in unilateral cleft lip and palate patients following comprehensive orthodontic treatment on digital study models. J Orthod Sci. [2022 May 4];11(1):19. doi: 10.4103/jos.jos_191_21 PMID: 35754411; PMCID: PMC9214443.
- Tankittiwat P, Pisek A, Manosudprasit M, et al. Function of nasoalveolar molding devices in bilateral complete cleft lip and palate: A 3-Dimensional maxillary arch Analysis. Cleft Palate Craniofac J. 2021 Nov;58(11):1389–1397. doi: 10.1177/1055665621990184 Epub 2021 Mar 4. PMID: 33657892.
- Ross RB. Growth of the facial skeleton following the Malek repair for unilateral cleft lip and palate. Cleft Palate Craniofac J. 1995 May;32(3):194–198. doi: 10.1597/1545-1569_1995_032_0194_gotfsf_2.3.co_2 PMID: 7605786.
- Grayson BH, Shetye PR. Presurgical nasoalveolar moulding treatment in cleft lip and palate patients. Indian J Plast Surg. 2009 Oct;42(S 01):S56–61. doi: 10.4103/0970-0358.57188 PMID: 19884682; PMCID: PMC2825057.
- Lee CT, Grayson BH, Cutting CB, et al. Prepubertal midface growth in unilateral cleft lip and palate following alveolar molding and gingivoperiosteoplasty. Cleft Palate Craniofac J. 2004 Jul;41(4):375–380. doi: 10.1597/03-037.1 PMID: 15297999.
- Ras F, Habets LL, van Ginkel Fc, et al. Longitudinal study on three-dimensional changes of facial asymmetry in children between 4 to 12 years of age with unilateral cleft lip and palate. Cleft Palate Craniofac J. 1995 Nov;32(6):463–468. doi: 10.1597/1545-1569_1995_032_0463_lsotdc_2.3.co_2 PMID: 8547285.
- AlHayyan WA, Pani SC, AlJohar AJ, et al. The effects of presurgical nasoalveolar molding on the midface symmetry of children with unilateral cleft lip and palate: A long-term follow-up study. Plast Reconstr Surg Glob Open. [2018 Jul 9];6(7):e1764. doi: 10.1097/GOX.0000000000001764 PMID: 30175004; PMCID: PMC6110686.
- Shetty V, Agrawal RK, Sailer HF. Long-term effect of presurgical nasoalveolar molding on growth of maxillary arch in unilateral cleft lip and palate: randomized controlled trial. Int J Oral Maxillofac Surg. 2017 Aug;46(8):977–987. doi: 10.1016/j.ijom.2017.03.006 Epub 2017 Apr 14. PMID: 28416097.
- Heidbuchel KL, Kuijpers-Jagtman AM, Kramer GJ, et al. Maxillary arch dimensions in bilateral cleft lip and palate from birth until four years of age in boys. Cleft Palate Craniofac J. 1998 May;35(3):233–239. doi: 10.1597/1545-1569_1998_035_0233_madibc_2.3.co_2 PMID: 9603558.
- Kiya K, Oyama T, Sone Y, et al. A novel active intraoral appliance for presurgical orthopaedic treatment in patients with complete bilateral cleft lip and palate. J Plast Reconstr Aesthet Surg. 2015 May;68(5):632–637. doi: 10.1016/j.bjps.2014.12.022 Epub 2014 Dec 24. PMID: 25616991.
- Pool R, Farnworth TK. Preoperative lip taping in the cleft lip. Ann Plast Surg. 1994 Mar;32(3):243–249. doi: 10.1097/00000637-199403000-00003 PMID: 8192382.
- Rossell-Perry P, Olivencia-Flores C, Delgado-Jimenez MP, et al. Surgical nasoalveolar molding: A rational treatment for bilateral cleft lip nose and systematic review. Plast Reconstr Surg Glob Open. [2020 Sep 24];8(9):e3082. doi: 10.1097/GOX.0000000000003082 PMID: 33133938; PMCID: PMC7544269.
- Rau A, Ritschl LM, Mücke T, et al. Nasoalveolar molding in cleft care–experience in 40 patients from a single centre in Germany. PLOS ONE. [2015 Mar 3];10(3):e0118103. doi: 10.1371/journal.pone.0118103 PMID: 25734535; PMCID: PMC4347986.
- Nagy K, Mommaerts MY. Postoperative wound management after cleft lip surgery. Cleft Palate Craniofac J. 2011 Sep;48(5):584–586. doi: 10.1597/09-242 Epub 2010 Aug 13. PMID: 20815719.
- Traube IMD*; Cutting CBM, Grayson BHD, Shetye PRD, MDS†. Effect of one-stage bilateral cleft lip, nose, and alveolus repair following nasoalveolar molding on the premaxilla position at preadolescence: An 8-year retrospective study. J Craniofac Surg. 2023 January/February;34(1):198–201. doi: 10.1097/SCS.0000000000007976
- Magyar D, Nemes B, Pálvölgyi L, et al. The burden of care in nasoalveolar molding treatment in cleft patients. Indian J Plast Surg. [2022 Mar 10];55(1):87–91. doi: 10.1055/s-0042-1744219 PMID: 35444738; PMCID: PMC9015833.
- Nagy K. Objektív módszerek az arc veleszületett rendellenességeit célzó sebészi kezelések értékelésében [Objective methods in the evaluation of surgical treatments aimed at congenital anomalies of the face] [ thesis]. 2012.