?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Despite the vaccination program’s great effectiveness, pertussis outbreaks are still reported with substantial spatial heterogeneity. Thus, this study aimed to investigate the spatio-temporal patterns of pertussis to determine the hot spots with the high-risk transmission in Vietnam from 2015 to 2019. This study was designed as a cluster case study from December 2019 to October 2020 in Hanoi, Vietnam. Data on 564 pertussis cases were collected via the pertussis case report form of the national immunization program and disease surveillance system of the Hanoi Centers for Disease Control and Prevention (CDC) from 2015 to 2019. Knox Test was applied to assess the risk of spreading epidemics by space and time via a program running on R software. The pertussis incidence per 100 000 population was the highest in the inner city, with an average of 2.96/100000 in 2015. An area with an extremely high risk of infection was located within 200 meters away from the pertussis case and within 40 days, apart from the detecting time (Relative risk (RR) = 3 to 222). Sixty-two hot spot clusters were defined, mainly distributed in the inner city areas, while only a few risk clusters belonged to suburban districts. By using well-defined spatio-temporal distributions, a geographical area of high pertussis transmission risk was identified. Our findings play a fundamental part in developing the ongoing and comprehensive database to complete the disease surveillance system and design effective intervention measures.
Keywords:
1. Introduction
Emerging and re-emerging infectious diseases have received the most attention recently and pose critical public health threats (CitationFuruse). Pertussis (Whooping cough) is a highly contagious respiratory disease caused by Bordetella pertussis and occurs globally in all age groups (CitationKretzschmar et al.,). Notably, pertussis has been reported as one of the top five diseases causing death in children (Ulloa-Gutierrez, Citation2009), one out of ten mortality causes among children under five years old over the world (Yeung et al., Citation2017). Before the existence of the vaccine, whooping cough strongly developed and outbroke with a 3–4 years epidemic cycle in many countries. Since the pertussis vaccine was presented, as well as the proliferation of health care services, the pertussis incidence rate reduced from 150/100 000 in the 1940s to 1/100 000 in the 1970s in the United State population (Cherry, Citation2012).
Currently, the World Health Organization (WHO) estimates 20–40 million cases and 200,000–400,000 deaths caused by pertussis every year worldwide. Even in countries with high immunization coverage, whooping cough remains a significant public health problem. Recent WHO data showed that in 2018, there were still 151,074 reported pertussis cases and approximately 89,000 deaths worldwide. The coverage rate of the diphtheria—pertussis—tetanus (DPT) vaccine only reached 86%.
In Vietnam, pertussis is circulating on a national scale. The average national incidence rate for the 1991–1995 period was 7.5/100 000 people (Institut Pasteur Ho Chi Minh City, Citation2022). Since 1993, the DTP immunization coverage rate has been maintained at over 90% (Institut Pasteur Ho Chi Minh City, Citation2022). This figure reached over 95% from 1997 to 2000, thanks to the improvement in immunization quality. Therefore, the national average incidence decreased to 1.8/100 000 people from 1996 to 2000 (Institut Pasteur Ho Chi Minh City, Citation2022). In recent years, the incidence of pertussis tendency has gradually decreased. However, in 2015, Hanoi witnessed a sudden increase in pertussis cases compared to the previous five-year period (2010–2014). According to Hanoi Hanoi Centers for Disease Control and Prevention (CDC) monitoring report, from 2015 to 2019, nearly 40% of pertussis cases appeared among children under 2-month-old, which was the age group that had not yet received pertussis vaccine in the national immunization program (Ministry of Health, Citation2019).
One common method in analyzing the spatial and temporal patterns of diseases is the Knox test, which focuses on counting points (pairs) of geographic events that occurred within a pre-defined space and time (Theophilides et al., Citation2008). Several previous studies used this method in identifying the transmission models, especially diseases transmitted by vectors such as dengue fever (Moore et al., Citation2005; CitationToan Do et al.,; Tran et al., Citation2004). Regarding pertussis outbreaks, a study by Broutin H et al. (2004) assessed the difference in the spreading model between urban and rural areas of Senegal (Broutin et al., Citation2004). There was a significant association between population density and the occurrence of whooping cough, while no relationship was seen for the geographical distance of regions (Broutin et al., Citation2004).
The main transmission of pertussis infection is airborne, which is mostly influenced by the size of the droplet as well as several potential factors related to climatic conditions (temperature, evaporation, air pressure or wind velocity; Huang et al., Citation2017; Wang et al., Citation2020). Due to the complex and not fully elucidated pertussis epidemiology, understanding the transmission model and hot spots of high-risk infection is integral in predicting further outbreaks in the future. In the context of Vietnam, where the medical resources are still constrained, investigating the areas with a high incidence of infectious disease by spatial and temporal distributions is essential for designing effective prevention programs in the 2021–2025 period, particularly when should vaccinate the first dose of pertussis vaccine for children. Therefore, this study aimed to analyze the risk of pertussis transmission spatio-temporal patterns in Hanoi, Vietnam, from 2015 to 2019.
2. Methods
2.1. Study settings and subjects
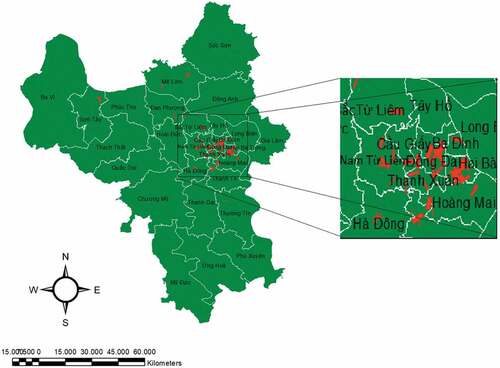
This study was designed as a cluster case study and implemented from December 2019 to October 2020 in Hanoi, Vietnam. Hanoi is the capital of Vietnam, with a total area of approximately 3359 km2, according to the results of the last census in 2020. The total population of Hanoi is about 8.25 million, divided into 12 urban districts, one district-leveled town, and 17 rural districts with 584 communes (168 inner city wards and 416 suburb communes). The areas of urban wards (accounting for 9.5% of Hanoi’s total areas) are much smaller than those of sub-urban communes, but the populations are similar. The population of Hanoi city is unevenly distributed, concentrating in 12 urban districts with 49.2% of the total population. The climate of Hanoi is considered warm and temperate. Hanoi is a city with significant rainfall, especially in August (CitationLee et al.,).
Vietnam provides free pertussis vaccines to children aged 0–6 months old. Pertussis vaccination rates in 2018 of one, three, and four doses were 96.2%, 92.2%, and 71.1%, respectively. The number of children under 1-year-old who needed to be vaccinated with three basic doses of pertussis vaccine was 133,466 children (National Institute of Hygiene and Epidemiology, Citation2018). Pertussis cases were selected in the study if they met the following criteria (CitationFuruse) being diagnosed as clinical pertussis cases or confirmed pertussis cases by doctors of hospitals located in Hanoi from 1st January 2015 to 31st December 2019; (Spokes et al., Citation2010) living in Hanoi from 1st January 2015 to 31st December 2019; and (CitationKretzschmar et al.,) was officially reported to the monitoring system of Hanoi CDC by local health staff. The definition of a clinical pertussis case is a person having a cough lasting at least two weeks with at least one of the following symptoms: Paroxysmal cough; Inspiratory whoop; Posttussive vomiting, which is described as vomiting immediately after a cough without other apparent causes (Gopal Krishnan et al., Citation2019). In addition, a confirmed pertussis case is a case of clinical suspicion of pertussis with the detection of genomic sequences by polymerase chain reaction (PCR) or isolation of bacterial agent Bortadella pertussis from a clinical specimen (Shakib et al., Citation2009). The confirmation test is conducted at the National Hospital of Tropical Diseases, Bach Mai Hospital, Vietnam National Children’s Hospital, and the National Institute of Hygiene and Epidemiology. We excluded participants if they lacked information on age group and vaccination history. The response rate was 100%.
2.2. Pertussis data
Data on pertussis cases were collected via the “pertussis case report form” of the national immunization program, which covered epidemiological, clinical, and laboratory information from 2015 to 2019. In addition, we also retrospectively reviewed all pertussis cases from different health commune centers reported to the disease surveillance system of the Centers for Disease Control and Prevention (CDC) in Hanoi from January 2015 to the end of December 2019. This is a routine surveillance system for reporting pertussis from (CitationFuruse) local health commune stations to the district health centers when detecting cases of pertussis within 48 hours of receiving the notice; (Spokes et al., Citation2010) district health centers to the CDC in Hanoi to complete the survey form all cases. Data of clinical and confirmed pertussis cases of hospitals at the central level and ministries monitored by the staff of the Hanoi CDC were combined in the data file. All records of patients diagnosed with pertussis living in Hanoi in 2015–2019 and who met the included criteria were selected for the study. The actual collected sample size was 564 cases.
2.3. Data analysis
2.3.1. Descriptive analysis
In order to better understand of pertussis epidemic in Hanoi, Vietnam, we performed a statistical summary of the pertussis data by areas, age groups, and the temporal of monthly pertussis incidences from 2015 to 2019. We used R statistical software to analyze epidemiological characteristics, including the prevalence of pertussis per 100.000 population with qualitative variables; the risk of spatio-temporal epidemic spread; the difference in pertussis prevalence between the two population groups.
2.3.2. Statistic for spatio-temporal clustering analysis
Knox Test was applied to assess the risk of spreading epidemics by space and time via a program running on R statistical software. The Knox approach is used to test the interaction of a defined distance and period to determine a statistically significant cluster (Knox & Bartlett, Citation1964). In epidemiological studies, the Knox test is a method to evaluate and define clusters of outbreaks or groups of disease cases in a unit of space and time (Schmertmann et al., Citation2010).
Assuming there were “n” points in the study settings, there were N = n(n-1)/2 pairs of points. To calculate the number of closed pairs of points within a unit length and a unit time, the Knox statistic test was applied as follows:
and
were the value describing each pair of points within interval units by spatial and temporal, respectively. These two quantities were calculated based on the following calculation:
and
were the spatial and temporal ranges needed to be calculated using the Knox test. The null hypothesis H0 expressed that the distance between pairs of points by temporal independently interacted with the distance by the spatial method. By contrast, the alternative hypothesis Ha presented the distance between pairs of closed points in space tended to be close in time.
To evaluate the statistical significance of the test, we used a null distribution to calculate what percentage of the inversion probabilities of and
were. Regarding the Knox test, we selected the Monte Carlo hypothesis test to calculate the p-value. ArcGIS 10.2 software was utilized for epidemiological analysis and illustrated spatial-temporal cluster analysis.
2.4. Ethical consideration
The study was approved by the Institutional Review Board (IRB) of the School of Preventive Medicine and Public Health, Hanoi Medical University number 5383/QĐ-ĐHYHN, issued on 10th November 2020. The research did not affect the well-being of participants as well as using health services. The collected information was kept entirely confidential and only used for research purposes.
3. Results
Among 564 pertussis cases in five years from 2015 to 2019, 57.3% were males. The under-five-month-old group accounted for the highest percentage (42%), followed by the under-two-month-old group (39.2%). The number of pertussis cases in inner-city areas was higher than that of the suburbs, 52.5% compared to 47.5%, respectively.
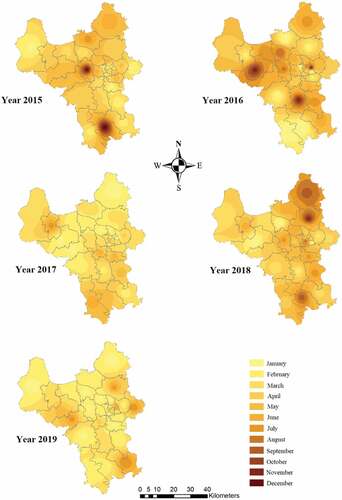
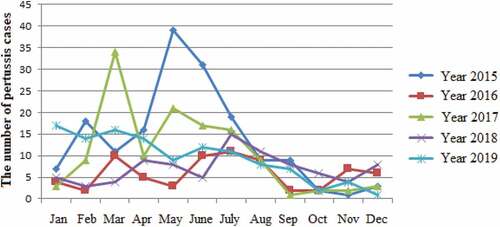
Figure shows a fluctuation in the number of pertussis cases over a year from 2015 to 2019. Although pertussis cases appeared scattered throughout the year, the figure reached a peak from February-March to June and gradually decreased at the end of the year. The transition of outbreak trends was also witnessed from 2015 to 2019. The incidence of pertussis cases was higher in 2015, 2017, and 2019. In addition, in 2015, the outbreak peaked in May, while it reached the highest cases in March 2017 and 2019.
Figure 1. The temporal patterns of the monthly incidence of pertussis cases (clinical and confirmed cases) in Hanoi from 2015 to 2019.
From the year 2015 to 2019, the pertussis incidence per 100000 population was the highest in the inner city in 2015 with an average of 2.96/100,000 and was the smallest in the suburb in 2016 (0.91/100,000 population; Table ). The incidence of pertussis in Hanoi in the inner-city areas was higher than in the suburbs in the past five years (2015 to 2019). The differences were statistically significant (Z-test, p < 0.01).
Table 1. The pertussis incidences (per 100000 population) in Hanoi by areas (from 2015 to 2019)
Figure presents the spatio-temporal characteristics of pertussis outbreaks in Hanoi from 2015 to 2019. The appearance of pertussis cases also exhibited heterogeneity across Hanoi from 2015 to 2019. In 2015, 2016, and 2018, the case of pertussis scattered around the year, while in 2017 and 2019, cases mostly occurred in the first months of the year. Besides, the spatial clustering of high observed incidences which appeared in the last months of the year mainly focused on several districts in the North and South of Hanoi.
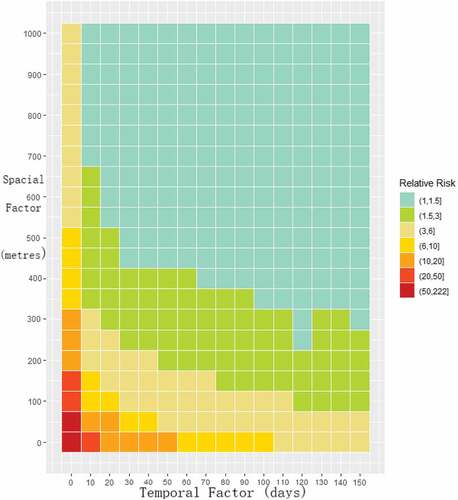
Figure illustrates the spatio-temporal distributions of pertussis transmission relative risk across Hanoi, Vietnam. There was strong evidence of spatial and temporal variability related to the magnitude of the pertussis relative risk. Living in the areas closer in space-time to the pertussis cases associated with developing the disease. People who lived within 50 meters from the pertussis case and had contact with the patient on the first day of detecting pertussis were more likely to experience the disease (RR = 50 to 222) compared to those who did not live in the same space-time. The figure also depicts an area with an extremely high risk of infection, located within 200 meters away from the pertussis case and within 40 days apart from the detecting time (RR = 3 to 222). According to the result of Table , since a case of pertussis occurred, living within 200 meters away and within 42 days apart from detecting time were related to having pertussis (RR = 3.04), with a statistically significant level (p-value <0.01).
Table 2. The spatial-temporal pattern of identifying pertussis transmission risk using the Knox test
Figure describes the distribution of high–risk clusters for pertussis transmission. The red dotted lines connecting the black dots were the high–risk clusters. Based on the cut-off space and time of 500 meters and 100 days, 62 statistically significant clusters were defined, with a p-value of 0.01 according to Monte Carlo simulation. These clusters were mainly distributed in the inner city areas such as Hai Ba Trung, Dong Da, and Thanh Xuan. Several suburbs, such as Me Linh and Son Tay, still had one to two risk clusters.
4. Discussion
To our knowledge, this is one of the very first studies in Vietnam to evaluate Spatio-temporal distributions in the spread of pertussis outbreaks at different time points among the urban populations. A geographical area of high pertussis transmission risk with well-defined space and time was identified. In addition, we investigated different spread patterns of outbreaks from 2015 to 2019 by area and month in a year.
Using the Knox test method, we found a significant result related to spatial-temporal pertussis transmission in Hanoi, Vietnam. Local areas with a high density of cases were within 200 meters from the pertussis cases and 40 days apart from the detecting time. Previous evidence showed that after 7–10 days of the incubation period, patients start with the catarrhal phase of the clinical course, which is the most accessible contagious period and can last up to three weeks (Yeung et al., Citation2017). In addition, person-to-person is the most common form of transmission via respiratory droplets or nasal/throat secretions of pertussis patients (Black, Citation1997; Yeung et al., Citation2017). The bacteria is in the droplets that fall within 2 meters radius under different conditions (Xie et al., Citation2007). As pertussis is highly communicable, according to our results, the risk of infecting the disease remains for people who contact within 200 meters and have an exposure time of more than a month.
Although pertussis vaccine coverage in Vietnam is very high, with an average of receiving four doses of 92.2%, recent evidence revealed the possibility of the occurrence of pertussis re-emergence, especially in reinfected cases among adults (CitationChiappini et al.,). Possible reasons relevant in light of recent studies suggest the role of genetic changes in circulating pertussis bacteria strains (Cherry, Citation2012) and restricted protection from pertussis (period of 5–8 years) whether having natural infection or vaccination (CitationHealy et al.,). Therefore, without repeat pertussis vaccination, the disease can appear in adults as an atypical presentation or asymptomatic “transient carriers”. A study by De Melker et al. in the Netherlands (2006) pointed out that only 0.01 infection cases were reported, and there were still many undetected sources of infection in the community (De Melker He et al., Citation2006). However, the diagnosis of pertussis cases is often ignored due to similar respiratory symptoms in adults, such as non-specific chronic cough, which may trigger the dangerous infection in other close-contact people. The key differentiating factors of pertussis are disease progression (three phases), usually occurring within 21 days (Melvin et al., Citation2014). Thus, identifying space and time cut-off of high pertussis risk using spatio-temporal analysis is vital in limiting disease transmission in the community. In addition, pertussis is a highly contagious respiratory disease with a higher risk of infection in the inner city due to a higher population density than in suburban areas. This finding is in agreement with the results of a previous study conducted in Hanoi in 2015–2016 (Thi Khanh Linh et al., Citation2017). Since pertussis is a respiratory-transmitted disease that is mostly affected by environmental factors, further studies are needed to assess how the changes in meteorological factors impact the development of infectious pathogens.
We also found 62 clusters in Hanoi statistically significant had a higher risk of pertussis transmission compared to other areas in Hanoi. These clusters were mostly located in urban districts such as Nam Tu Liem, Dong Da, Thanh Xuan, Ha Dong, Hai Ba Trung, Cau Giay, while only a few clusters belonged to suburban areas (Me Linh, Son Tay, Gia Lam). Besides, the incidence of pertussis in Hanoi in the inner-city areas was statistically significant higher than that of the suburbs in the past five years (2015 to 2019). The difference can be explained by the high population density in inner-city areas where residential areas, commercial centers, offices are concentrated, leading to the increasing possibility of contact between high-risk subjects. Our findings are consistent with previous studies which revealed respiratory-borne diseases, for example, pertussis and measles, were more likely to appear in urban areas compared to rural parts (Broutin et al., Citation2004; CitationCrespo et al; Grenfell, Citation1998). Notably, there was no difference in whooping cough incidence between the two regions if the population density was similar (Broutin et al., Citation2004). Another explanation for differences was related to vaccination coverage, which was found higher in urban areas (Vickers et al., Citation2006). Several previous studies used the spatio-temporal method to analyze the spread of infectious diseases through hosts, especially dengue fever. A study by Su Bee Seng et al. conducted in Malaysia found that thirty-one spatio-temporal clusters within 200 meters and 14 days apart statically significant had a higher risk of dengue fever (Moore et al., Citation2005). In Vietnam, a study by Do Thanh Toan et al. carried out in Hanoi determined that 6 per 14 (42.29%) districts of Hanoi had statistically significant cluster models, which were within 1,000 meters radius and lasted up to 29 days (CitationToan Do et al.,).
Although the incidence of pertussis fluctuated from 2015 to 2019, disease cases mostly appeared in the spring-summer (February to August) and gradually decreased in the last year. This finding is coincident with a previous study by (Nguyen Thi Dinh et al. Citation2017, Dinh et al., Citation2018), which showed that the number of pertussis hospitalized cases focused from February to July, while in the southern region, it appeared from March to August (Pham Thai Son et al., Citation2019; Son et al., Citation2019). This can be explained by the fact that the season of those months is rainy with high humidity in both the North and the South, which creates favorable conditions for bacteria development, especially the spread of respiratory-borne diseases.
To our best knowledge, this study is one of the first attempts to investigate the spatio-temporal model of pertussis spreading risk for disease control and prevention in Hanoi, Vietnam. By using the existing data, our findings play a fundamental part to continue developing the ongoing and comprehensive database to complete the disease surveillance system. When detecting a confirmed pertussis case, proactive preventive measures on a large scale should be taken at least 200 meters and approximately 42 days after exposure. In addition, although pertussis prevention is implemented in all areas of Hanoi, the priority actions should be focused on urban districts with high population densities to avoid the spread to other center districts and from the inner city to suburban areas. Further studies covering an ensemble of socio-ecological and ecosystem stress should be considered, in order to investigate the effect of environmental factor changes on the transmission of pertussis.
Several limitations should be acknowledged in the study. First, we retrospectively used the available data, which may lead to missing participants’ information. To overcome this limitation, all data collection processes were evaluated and monitored by well-training researchers. Recall bias should be considered, related to the initiation time of pertussis and vaccination history. Although all districts being are provided with the global positioning system (GPS) coordinates finders, using and converting decimal coordinates into standard records are minor problems that may trigger errors in determining and analyzing the location of patients on the map.
5. Conclusion
By using the comprehensive existing health data and well-defined spatio-temporal statistics, our study presented the hot spots with the highest risk of pertussis infection in Hanoi, Vietnam. These findings are critical evidence to enhance our understanding of space-time pertussis spread models and inform policymakers to allocate more effective strategies containing the outbreaks.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data that support the findings of this study are available on request from the corresponding author, Anh Kim Dang. The data are not publicly available.
Additional information
Funding
References
- Black, S. (1997, April). Epidemiology of pertussis. The Pediatric Infectious Disease Journal, 16(4 Suppl), S85–12. https://doi.org/10.1097/00006454-199704001-00003
- Broutin, H., Elguero, E., Simondon, F., & Guégan, J. (2004). Spatial dynamics of pertussis in a small region of Senegal. Proceedings of the Royal Society of London Series B: Biological Sciences, 271(1553), 2091–2098. https://doi.org/10.1098/rspb.2004.2847
- Cherry, J. D. (2012). Epidemic pertussis in 2012 — The resurgence of a vaccine-preventable disease. New England Journal of Medicine, 367(9), 785–787. https://doi.org/10.1056/NEJMp1209051
- Cherry, J. D. (2012, May). Why do pertussis vaccines fail? Pediatrics, 129(5), 968–970. https://doi.org/10.1542/peds.2011-2594
- Chiappini, E., Stival, A., Galli, L., & de Martino, M. Pertussis re-emergence in the post-vaccination era. BMC Infectious Diseases, 13(1), 151. https://doi.org/10.1186/1471-2334-13-151
- Crespo, I., Soldevila, N., Munoz, P., Godoy, P., Carmona, G., & Dominguez, A. Geographical differences in whooping cough in Catalonia, Spain, from 1990 to 2010. BMC Public Health, 14(1), 268. https://doi.org/10.1186/1471-2458-14-268
- de Melker He, Versteegh, F. G., Schellekens, J. F., Teunis, P. F., Kretzschmar, M., & Demelker, H. (2006, August). The incidence of Bordetella pertussis infections estimated in the population from a combination of serological surveys. The Journal of Infection, 53(2), 106–113. https://doi.org/10.1016/j.jinf.2005.10.020
- Dinh, N. T., Lam, N. V., & An, P. N. (2018). Clinical & epidemiological characteristics of the pertussis in children in National hospital of Pediatrics in 2017. Pediatrics Journal, 1(11), 35–41.
- Furuse, Y. Analysis of research intensity on infectious disease by disease burden reveals which infectious diseases are neglected by researchers. Proceedings of the National Academy of Sciences of the United States of America, 116(2), 478–483. https://doi.org/10.1073/pnas.1814484116
- Gopal Krishnan, S., Fun, W. H., Ramadras, M. D., Yunus, R., Lye, Y. F., Sararaks, S., & Cartelle Gestal, M. (2019). Pertussis clinical case definition: Time for change in developing countries? PLoS One, 14(7), e0219534. https://doi.org/10.1371/journal.pone.0219534
- Grenfell, G. (1998). Cities and villages: Infection hierarchies in a measles metapopulation. Ecology Letters, 1(1), 63–70. https://doi.org/10.1046/j.1461-0248.1998.00016.x
- Healy, C. M., Rench, M. A., Castagnini, L. A., & Baker, C. J. (41). Pertussis immunization in a high-risk postpartum population. Vaccine, 27, 5599–5602. https://doi.org/10.1016/j.vaccine.2009.07.030
- Huang, X., Lambert, S., Lau, C., Soares Magalhaes, R. J., Marquess, J., Rajmokan, M., Milinovich, G., & HU, W. (2017). Assessing the social and environmental determinants of pertussis epidemics in Queensland, Australia: A Bayesian spatio-temporal analysis. Epidemiology and Infection, 145(6), 1221–1230. https://doi.org/10.1017/S0950268816003289
- Institut Pasteur Ho Chi Minh City. Pertussis. Ho Chi Minh, Viet Nam2014 [ cited 2022 10 March]; Available from: http://www.pasteurhcm.gov.vn/news/benh-ho-ga-88.html
- Knox, E. G., & Bartlett, M. S. (1964). The detection of space-time interactions. Journal of the Royal Statistical Society. Series C, Applied Statistics, 13(1), 25–30. https://doi.org/10.2307/2985220
- Kretzschmar, M., Teunis, P. F., Pebody, R. G., & Murray, M. Incidence and reproduction numbers of pertussis: Estimates from serological and social contact data in five European countries. PLoS medicine, 7(6), e1000291. https://doi.org/10.1371/journal.pmed.1000291
- Lee, H. S., Nguyen-Viet, H., Nam, V. S., Lee, M., Won, S., Duc, P. P., & Grace, D. Seasonal patterns of dengue fever and associated climate factors in 4 provinces in Vietnam from 1994 to 2013. BMC Infectious Diseases, 17(1), 218. https://doi.org/10.1186/s12879-017-2326-8
- Melvin, J. A., Scheller, E. V., Miller, J. F., & Cotter, P. A. (2014, April). Bordetella pertussis pathogenesis: Current and future challenges. Nature Reviews. Microbiology, 12(4), 274–288. https://doi.org/10.1038/nrmicro3235
- Ministry of Health. Conference report of national immunization program. 2019.
- Moore, A. B., Seng, S., & Chong, A. K. Eds. 2005. Geostatistical modelling, analysis and mapping of epidemiology of Dengue Fever in Johor State, Malaysia (pp. 109–123).17th Annual Colloquium of the Spatial Information Research Centre (SIRC 2005: A Spatio-temporal Workshop), 2005-11. Dunedin, New Zealand.
- National Institute of Hygiene and Epidemiology. Report of the national immunization program in 2018. 2018.
- Schmertmann, C. P., Assucaon, R. M., & Potter, J. E. (2010, August). Knox meets Cox: Adapting epidemiological space-time statistics to demographic studies. Demography, 47(3), 629–650. https://doi.org/10.1353/dem.0.0113
- Shakib, J. H., Wyman, L., Gesteland, P. H., Staes, C. J., Bennion, D. W., & Byington, C. L. (2009, Nov-December). Should the pertussis case definition for public health reporting be refined? Journal of Public Health Management and Practice: JPHMP, 15(6), 479–484. https://doi.org/10.1097/PHH.0b013e3181af0ac3
- Son, P. T., Xuan, T. N., & Dung, P. T. T. (2019). Epidemiological, clinical characteristics, and treatment for children with pertussis admitted in Children hospital 2, Ho Chi Minh City in 2018. Preventive Medicine, 11(29), 69. http://www.tapchiyhocduphong.vn/tap-chi-y-hoc-du-phong/2019/11/dac-diem-dich-te-hoc-lam-sang-can-lam-sang-va-dieu-tri-o-benh-nhi-mac-benh-ho-ga-o81E20866.html
- Spokes, P. J., Quinn, H. E., & McAnulty, J. M. (2010, Jul-August). Review of the 2008-2009 pertussis epidemic in NSW: Notifications and hospitalisations. New South Wales Public Health Bulletin, 21(7–8), 167–173. https://doi.org/10.1071/NB10031
- Theophilides, C. N., Binkowski, E. S., Ahearn, S., & Paul, W. S. (2008, September 1). A comparison of two significance testing methodologies or the knox test. The International Journal of Geoinformatics, 4. https://www.researchgate.net/publication/258438190_A_Comparison_of_two_Significance_Testing_Methodologies_or_the_Knox_Test
- Thi Khanh Linh, N., Hai Dang, L., & Quang Thai, P. (2017). Epidemiological, clinical and some factors related to complications of pertussis in Hanoi in 2015-2016. Journal of Preventive Medicine, 27(6), 61. http://www.tapchiyhocduphong.vn/tap-chi-y-hoc-du-phong/2017/06/dac-diem-dich-te-hoc-lam-sang-va-mot-so-yeu-to-lien-quan-den-bien-chung-cua-benh-o81E205C1.html
- Toan Do, T. T., Hu, W., Quang Thai, P., Hoat, L. N., Wright, P., & Martens, P. Hot spot detection and spatio-temporal dispersion of dengue fever in Hanoi. Vietnam. Glob Health Action, 6(1), 18632. https://doi.org/10.3402/gha.v6i0.18632
- Tran, A., Deparis, X., Dussart, P., Morvan, J., Rabarison, P., Remy, F., Polidori, L., & Gardon, J. (2004, April). Dengue spatial and temporal patterns, French Guiana, 2001. Emerging Infectious Diseases, 10(4), 615–621. https://doi.org/10.3201/eid1004.030186
- Ulloa-Gutierrez, R. (2009, March). Pertussis vaccination in newborns. Expert Review of Vaccines, 8(2), 153–157. https://doi.org/10.1586/14760584.8.2.153
- Vickers, D., Mainar-Jaime, R. C., & Pahwa, P. (2006, Nov-December). Pertussis in rural populations of Saskatchewan (1995 to 2003): Incidence, seasonality, and differences among cases. Canadian Journal of Public Health. Revue Canadienne de Sante Publique, 97(6), 459–464. https://doi.org/10.1007/BF03405228
- Wang, Y., Xu, C., Ren, J., Zhao, Y., Li, Y., Wang, L., & Yao, S. (2020, October). The long-term effects of meteorological parameters on pertussis infections in Chongqing, China, 2004-2018. Scientific Reports, 10(1), 17235. https://doi.org/10.1038/s41598-020-74363-8
- Xie, X., Li, Y., Chwang, A. T., Ho, P. L., & Seto, W. H. (2007, June). How far droplets can move in indoor environments–revisiting the Wells evaporation-falling curve. Indoor Air, 17(3), 211–225. https://doi.org/10.1111/j.1600-0668.2007.00469.x
- Yeung, K. H. T., Duclos, P., Nelson, E. A. S., & Hutubessy, R. C. W. (2017, September). An update of the global burden of pertussis in children younger than 5 years: A modelling study. The Lancet Infectious Diseases, 17(9), 974–980. https://doi.org/10.1016/S1473-3099(17)30390-0