Session
01-OP-L-d1B: Oral Presentations Session 1 - Day 1 - Zone B
Presentations
ID: 155/01-OP-L-d1B: 1
Oral Presentation (Onsite)
Topics: NEONATOLOGY
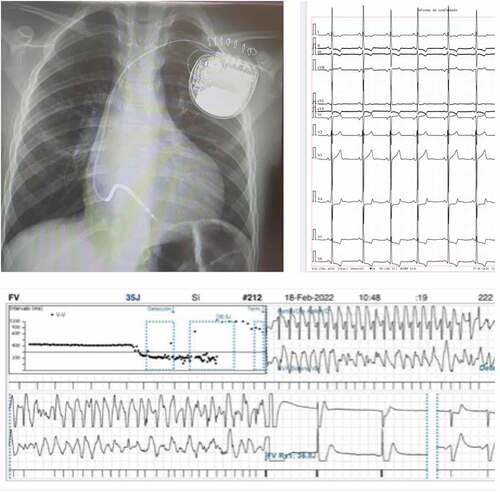
Keywords: Neonatal, Arrhythmia, Cardiology, NICU, Cardiac
A need for standard national framework for managing neonates with an arrhythmia- A 10 year study of neonates with arrhythmias and their outcome from a district general hospital
Stratford, Ana; Ahmed, Ather
Lister Hospital, East and North East Hertfordshire NHS Trust, UK.
Background: Arrhythmias occur in up to 5% of newborns in the first 10 days of life, with the majority being benign and likely to disappear within weeks to months. However, it is important that we identify those with more serious arrhythmias, thereby mandating further intervention. Often neonates with arrhythmias are asymptomatic and picked up incidentally. This led us to review the management of neonatal arrhythmias more closely at our trust to see how we manage these patients and what guidelines are currently in place. We did a retrospective study of newborns admitted to our Neonatal Intensive Care Unit (NICU), with neonatal arrhythmias over the last 10 years, from August 2012 to August 2022.
Methods: We used the BadgerNet electronic patient record system to collect the data and identify patients. We identified a total of 41 patients, of which 85% were term babies. The majority were picked up incidentally, where an abnormal rhythm or heart rate was identified during routine newborn examination (27%), clinical review by the doctor for a different clinical concern (17%) or by a midwife during routine observations (24%). 17% of these patients were admitted to NICU for another clinical reason, such as prematurity or suspected sepsis, and arrhythmia was picked up on routine observations in NICU. 15% of the babies were admitted to NICU due to Antenatal (AN) concerns of an irregular heart rate.
Results: Of all these babies admitted to NICU for further investigations, 71% had an abnormal Electrocardiogram (ECG) finding. Supra-ventricular arrhythmias were noted in 34%, and a different range of ectopics in 35%. All patients with supra-ventricular arrhythmias had been appropriately managed per the Acute Paediatric Life Support (APLS) algorithm. 67% of babies with supra- ventricular tachycardia (SVT) required Adenosine to revert back to normal sinus rhythm, and 53% were started on propranolol. In 20% with AN SVT concerns, maternal Flecainide was administered. 80% of patients were discussed with a tertiary centre regarding further management, and 46% were followed up at the tertiary centre. Regarding further investigations, 61% had blood tests, 32% had a 24- hour ECG tape, and 45% had an echocardiogram. Interestingly, a large number (44%) of patients had positive AN findings of arrhythmia or abnormal heart rate. 71% of all patients had an abnormal ECG postnatally. For those with AN concern, abnormal findings postnatally were found in 78%. 15% of babies had a fetal echocardiogram, all of which had a structurally normal heart, with 33% noted to have an arrhythmia during the scan. Only 17% of babies with known AN arrhythmia concerns were admitted straight to NICU for postnatal monitoring. This triggers the question; should we routinely admit these babies for cardiac monitoring to NICU?
Conclusions: Supra-ventricular arrhythmia in a neonate is life-threatening. Based on our experience and data, we recommend any newborn with an irregular heart rate be admitted to the neonatal unit for cardiac monitoring, including those with antenatal concerns. Service provision for 24-hour ECG in a District General Hospital varies across the United Kingdom. There is no national guidance for managing benign arrhythmias and hence variable practice. We acknowledge that our study population is small size; however, we recommend there should be a standard national framework for managing neonates with arrhythmia to improve patient care and safety.
ID: 225/01-OP-L-d1B: 2
Oral Presentation (Onsite)
Topics: NEONATOLOGY, NEUROLOGY
Keywords: Neonatology, Neurology, Aicardi-Goutières Syndrome, Intracerebral Calcifications, Encephalopathy
Aicardi-Goutières syndrome - a case report on a newborn
Aguiar, Barbara Ribeiro1; Oliveira, Sara Torres2; Cavaco, Hugo1; Prado, Sara Noéme1; Saldanha, Joana1; Quintas, Sofia2
1Department of Pediatrics, Hospital Beatriz Angelo, Portugal; 2Department of Pediatrics, Hospital de Santa Maria, North Lisbon University Hospital Center, Portugal.
Background: Aicardi-Goutières syndrome (AGS) is a rare genetic neurological disorder. It is characterized by nonspecific neurological symptoms and systemic manifestations and is associated with intracerebral calcifications, abnormalities of white matter and cerebral atrophy, cerebrospinal fluid lymphocytosis and high levels of interferon alpha (IFN-α).
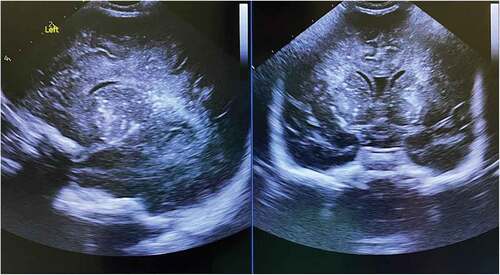
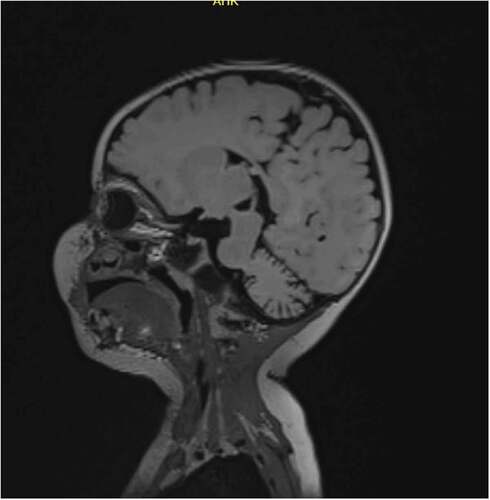
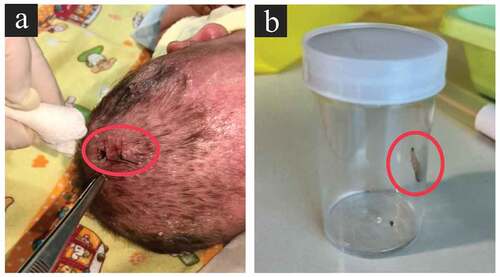
Case Presentation Summary: Male newborn of healthy and nonconsanguineous parents with an uneventful pregnancy. Vaginal birth at 40 weeks gestational age, Apgar scores of 9/10. Birth weight, height, and head circumference on the 50th, 3rd and 15th percentiles, respectively. Multiple petechiae were observed on day 2 of life. Haematological tests revealed thrombocytopenia—63 · 109cells/L (210–650 · 109 cells/L). Head ultrasonography suggested thalamic and periventricular calcifications (Figure ). Computed tomography and magnetic resonance imaging of the brain demonstrated attenuation of cerebral white matter, subcortical atrophy and basal ganglia and periventricular calcifications. The electroencephalogram (EEG) was normal. Intrauterine congenital infection was excluded (TORCH, varicella-zoster virus, human herpes virus 6, enterovirus, parvovirus, and coronavirus). Ophthalmological and neurologic evaluations were normal, and thrombocytopenia resolved by the third week of life. Asymptomatic was discharged and referred to Pediatric Neurology for further investigation, namely cerebrospinal fluid, and genetic analysis. (1) Follow-up at four months of age revealed feeding difficulties, significant neuromotor developmental delay, spastic tetraparesis, dystonia and acquired microcephaly with head circumference below the 3rd percentile. EEG was repeated, now showing a global slowing pattern. Cerebrospinal fluid analysis revealed lymphocytosis, elevated IFN-α and elevated neopterin. At five months of age, pulses of methylprednisolone were started. Genetic analysis identified a homozygous TREX1 gene mutation, and AGS was diagnosed. He maintains feeding difficulties and failure to thrive, with weight below the 3rd percentile and microcephaly. At nine months, we started treatment with a JAK inhibitor (baricitinib), with some minor improvements in neuromotor skills.
Learning Points Discussion: AGS is a rare encephalopathy. The diagnosis is difficult since many of the neurological symptoms are similar to other disorders. The neonatal presentation is extremely rare and is most frequently associated with the TREX gene. This case emphasizes the need to consider AGS as a differential diagnosis in the newborn with intracerebral and basal ganglia calcifications, excluding infections, disorders of calcium and phosphorus metabolism, cerebral folate deficiency and mitochondrial diseases.
ID: 149/01-OP-L-d1B: 3
Oral Presentation (Onsite)
Topics: NEONATOLOGY
Keywords: Anorectal malformation, Imperforate anus, Colonic atresia, VACTERL association, Newborn
Anorectal malformations: a 5-year casuistry
Vieira, Beatriz1; Pinho, Joana2; Lopes, Vilma2; Amaral, Marina3; Rosinha, Céu3; de Sousa, Pinho3; da Silva, Vinhas4; Pereira, Joana3; Teles, Andreia4
1Pediatric Department, Centro Hospitalar da Póvoa de Varzim/Vila do Conde, Portugal; 2Pediatric Department, Centro Hospitalar Vila Nova de Gaia/Espinho, Vila Nova de Gaia, Portugal; 3Pediatric Surgery Department, Centro Hospitalar Vila Nova de Gaia/Espinho, Vila Nova de Gaia, Portugal; 4Neonatology Department, Centro Hospitalar Vila Nova de Gaia/Espinho, Vila Nova de Gaia, Portugal.
Background: Anorectal malformations are a complex group of congenital anomalies involving the distal anus and rectum. Our objective was to evaluate the prevalence, epidemiology, clinical manifestations, diagnosis, treatment and outcome of newborns admitted at a Neonatal Intensive Care Unit of a Portuguese level II hospital with anorectal malformations over 5 years.
Methods: A retrospective descriptive study, with analysis of clinical files of newborns with anorectal malformations, admitted to our unit between 31 January 2017 and 31 January 2022. Statistical software SPSS for Windows was used for recording data and analysing results.
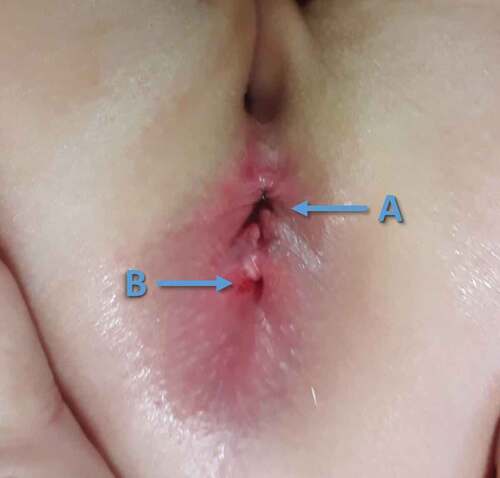
Results: 7 newborns (4 female and 3 male) were diagnosed with anorectal malformations accounting for 0,09% of the births (7/8143) and 0,85% (7/828) of Neonatal Intensive Care Unit admissions. Most patients (71,4%) were normal birth weight. The median gestational age was 39 weeks. Concerning the types of anorectal malformations, there were 2 newborns with vestibular fistula and 2 with rectourethral fistula followed by perineal fistula (1), a complex cloaca spectrum malformation (1) and an anorectal malformation with no fistula (1)—Table . We did not have a defined prenatal diagnosis in any of our cases. Additional anomalies were found in 85.7% and included: genitourinary anomalies (4/7), cardiac anomalies (4/7), gastrointestinal anomalies (3/7) and spinal anomalies (1/7). We found 3 cases of VACTERL association, and one of our cases combined colonic atresia and VACTERL with anorectal malformation. A multi-step approach was performed with a protective colostomy in the first days of life, followed by a delayed repair later (ranging from 5 to 19 months after the first intervention). A posterior sagittal anorectoplasty was the preferred technique to perform the anorectal reconstruction. The survival rate was 100% at discharge. The average length of hospital stay was 22,4 days.
Table
Conclusions: Our study found 3 cases of VACTERL association, an extremely rare condition. Furthermore, one of our cases combined colonic atresia and VACTERL with anorectal malformation, which is a very rare occurrence. Regards the associated anomalies, our incidence was higher than that described in the literature. [1] Anorectal malformations are among the most frequent congenital anomalies encountered in pediatric surgery. It is essential to make a diagnosis and classification in the neonatal period. The neonatologist, pediatric surgeon and radiologist must work together, allowing the diagnosis to be quickly established, the management of associated anomalies and an efficient surgical repair to be rapidly implemented.
ID: 153/01-OP-L-d1B: 4
Oral Presentation (Onsite)
Topics: ALLERGY, IMMUNOLOGY & RESPIRATORY
Keywords: Pneumonia, Chest-Xray, Antibiotics, CAP, LRTI
An audit assessing management of children with suspected community acquired pneumonia
Naguleswaran, Vanessa; Qureshi, Muniba; Ominu-Evbota, Kilali
Mid and South Essex NHS Trust - Basildon Hospital, UK.
Background and Standards: 7% of people in the UK have penicillin resistance; therefore, it is important to give the correct antibiotic to avoid resistance arising. The BTS and NICE guidelines suggest oral amoxicillin as first-line treatment, provided they have no allergies or features of severe community-acquired pneumonia. Many children with respiratory tract infections get additional investigations, including CXR and blood tests; these come with their own risks of radiation and distress. (1) Our set standard is that 100% of children with suspected community-acquired pneumonia should have the correct antibiotic prescribed as per the NICE guidelines and the appropriate investigations as per the BTS guidelines.
Aims: What percentage of children with suspected community-acquired pneumonia have the correct antibiotic (drug, duration, and route) administered per the NICE guidelines? What percentage of children with suspected community-acquired pneumonia have the correct investigations, i.e., chest x-ray and blood tests as per BTS guidelines?
Method: A random selection of approximately 50 patients with suspected community-acquired pneumonia were identified, and their records were checked to identify if they were managed as per the guidelines.
Results: 57 patients were identified; however, 11 were removed based on our exclusion criteria, leaving 46 patients for data analysis. Unfortunately, we did not meet the set standard; only 33% of children had complete, correct management as per NICE /BTS guidelines. Regarding antibiotics, 56.5% of patients had the incorrect antibiotic type prescribed; 100% of patients were given the correct route of antibiotics, and only 32.6% had the correct duration of antibiotics prescribed (see attachment). Regarding the investigation, 41% of patients had a Chest X-ray unnecessarily, and 8.9% had blood tests unnecessarily. 100% of patients with severe Community-Acquired Pneumonia were managed correctly (Table ).
Table
Discussion: Logistical issues identified included incorrect labelling of a patient’s diagnosis and poor documentation of the duration of antibiotics given. Many patients were treated with Co-Amoxiclav, or Clarithromycin as opposed to amoxicillin. Children also had unnecessary investigations exposing them to radiation and distress. Our study could have been a bias due to the small sample size and selection of patients in a one-time frame.
Conclusion: Only 33% of children had complete, correct management as per NICE /BTS guidelines.
Recommendations: We presented our findings to paediatric/Emergency doctors and created a flowchart to guide managing community-acquired pneumonia. Aim to re-audit in one year.
ID: 223/01-OP-L-d1B: 5
Oral Presentation (Onsite)
Topics: DERMATOLOGY, NEONATOLOGY
Keywords: Congenital ichthyoses
Congenital ichthyosis, an unexpected diagnosis
Ferreira Mendes, Joana1; S Rodrigues, Sara1; Strecht Guimarães, Francisca1; Santiago, Flávia2; Caldeira, Teresa2; Andrade, Teresa2
1Centro Hospitalar de Entre Douro e Vouga, Pediatric Department, Portugal; 2Centro Hospitalar de Entre Douro e Vouga, Neonatal Intensive Care Unit, Portugal.
Background: Congenital ichthyoses encompass a heterogeneous group of dermatoses of genetic origin, usually present at birth or of early onset, characterized by hyperkeratosis, scaling, often with skin inflammation and, in some cases, systemic manifestations. The impaired barrier function of the skin is responsible for the majority of complications, like the decreased ability to protect against external assault and transepidermal water loss. The neonatal period is critical, with a high risk of morbidity and mortality.
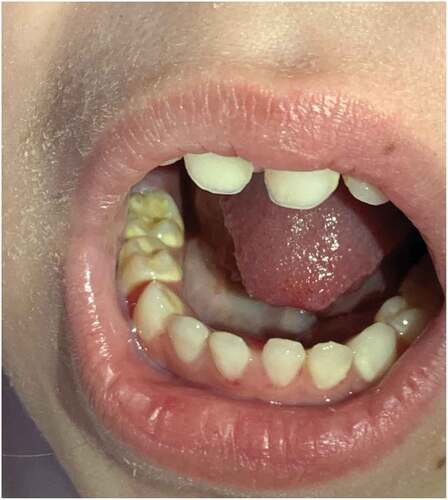
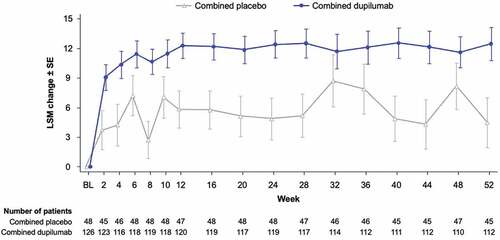
Case Presentation: A first controlled pregnancy from adolescent non-consanguineous parents, with negative serology and innocent prenatal ultrasound, was complicated by threat of preterm labour at the 30th gestation week. Proceeded to tocolysis and complete cycle of corticosteroid therapy. Due to a positive screening of Group B Streptococcus completed Ampicillin-therapy antepartum. (1) A premature female newborn was delivered naturally at 34 gestation-weeks, with membrane rupture 15 hours antepartum, meconium-stained amniotic fluid, body weight of 2020 grams and Apgar score of 9/10. At birth, the newborn presented thick, tense and shiny skin, and lamellar scaling adding to an ectropion and eclabium. (2) By prematurity, suspected ichthyoses and infectious risk, she was admitted to the Neonatal Intensive Care Unit and placed in the humidified incubator. The skin was treated with emollients, bath oil and keratolytic cream (urea 10%), eclabium with vaseline and ectropion with lagophthalmos was lubricated with carbomer eye gel. Due to inflammation and open wound cervical region was treated with topical hydrocortisone. (3) Invasive ventilation was never necessary. On 1st day, due to hypotension associated with decreased urine output, she received two intravenous boluses of normal saline. Given the infectious risk, ampicillin and gentamicin were started. Six days after, and with sterile blood culture, antibiotic therapy was discontinued. (4) At 25 days of life, she presented skin regeneration under scaling areas. She was discharged from the hospital, maintaining the skin treatment and referred to a dermatologist and ophthalmologist. (5) She maintains medical follow-up and presents a positive progression of skin regeneration without complications (Figure ).
Learning Point/Discussion: The diagnosis is based on medical history and physical examination. Early suspicion of congenital ichthyosis and a multidisciplinary approach are decisive in managing neonates with ichthyoses. Since there is no cure for ichthyosis, the aim of management is to treat signs and symptoms and prevent complications. A relationship of trust between the family and the medical team is also essential for long-term treatment, and genetic counselling can be useful for future pregnancies.
ID: 247/01-OP-L-d1B: 6
Oral Presentation (Onsite)
Topics: NEONATOLOGY
Keywords: EOS, antibiotics, neonates, sepsis, therapy.
Early-onset neonatal sepsis: a retrospective population-based cohort study
Rodrigues, Ana Sofia1; Fernandes, Ana Cristina2; De Oliveira, Susana Correia2; Pereira, Marta3; Rodrigues, Sandra2
1Pediatrics Department, Centro Hospitalar do Médio Ave, Vila Nova de Famalicão, Portugal; 2Neonatology Department, Hospital Senhora Oliveira, Guimarães; 3Education Division, Câmara Municipal de Barcelos.
Background: Neonatal sepsis remains a frequent clinical condition with significant morbidity and mortality. The aim of this study is to characterize early-onset neonatal sepsis (EOS) and understand aspects related to it, such as maternal/infant risk factors, clinical findings, laboratory and microbiological profile, antimicrobials susceptibility and outcome.
Methods: A descriptive and retrospective study was conducted between January 2017 and June 2022 at a neonatal intensive care unit. All newborns were diagnosed with EOS: clinical signs and/or laboratory criteria for infection and/or positive blood culture within the first 72 hours of life.
Results: A total of 143 neonates were included, with a balanced gender distribution (53% males). 30% were preterm and, of these, 10% extremely premature. 5.6% were newborns with low birth weight (<2500 g), 9% were very low birth weight (<1500 g), and 12% were extremely low birth weight infants (<1000 g). Most newborns were delivered by cesarean (55%), and 38% required resuscitation immediately after birth. Chorioamnionitis was suspected in 41% and confirmed in 30,5%. Moreover, 30% had premature rupture of the membranes (PROM). In 26% of cases was identified Group B streptococcus (GBS) colonization. The most common clinical findings of EOS were respiratory distress (45%), hypoxemia (29%) and feeding difficulties (26%). About 93% of the patients with EOS presented high levels of C-reactive protein, 6.3% had thrombocytopenia, and 4.2% had alterations in the leukogram. Lumbar puncture was performed in 20% of the newborns, revealing abnormal results in 14%. Positive blood culture was found in 8% of neonates. The commonest organism isolated was GBS (73%), followed by Escherichia coli (27%). Over 97% of the newborns received first-line antimicrobials (ampicillin and gentamicin). This antibiotic regimen was altered in 5% of cases due to clinical worsening (71%) and antimicrobial drug resistance (29%). EOS mortality rate was 3.5% of all premature newborns. In follow-up consultation, 6% of the newborns had developmental delay; half were premature.
Conclusions: EOS remains a common and serious problem for neonates, especially preterm infants. Determining the spectrum of maternal and infant risk factors, clinical features, and laboratory profile of EOS is essential to implement appropriate treatment strategies and to save the lives of many newborns. It is also crucial to know our local patterns of antimicrobial resistance of the most prevalent causative microorganisms in order to choose adequate antibiotic coverage. Our study emphasizes that using ampicillin and gentamicin as the first choice regimen is a good treatment option and presents little resistance.
ID: 176/01-OP-L-d1B: 7
Oral Presentation (Onsite)
Topics: NEONATOLOGY
Keywords: Excessive cry in newborn, testicular torsion, orchiectomy
Excessive crying in newborn is not always a symptom of hunger; a case with neonatal testicular torsion
Hristova, Aleksandra1; Tavcioska, Gabriela2
1General Hospital Kumanovo, Republic of North Macedonia; 2General Hospital Prilep, Republic of North Macedonia.
Introduction: Neonatal testicular torsion is a condition that occurs prenatally and up to 30 days after delivery. It happens when a loose testicle twists around the spermatic chord and cuts off the blood flow to the testicle. Neonatal testicular torsion can be divided into two groups based on the timing of the torsion event, occurring before or after birth. Because of the high morbidity associated with this condition, early recognition and appropriate management are imperative. The incidence of testicular torsion in the neonatal period is 6,1 per 100,000 live births.
Case Report: We report a case of unilateral testicular torsion. In our Department of Gynecology and Obstetrics, a vaginally healthy male newborn was born in 38 G.A ., with a birth weight of 3450 grams and birth length of 50 cm, APGAR score of 8/9. It was a second baby of a 37-year-old woman with negative history of any illnesses before or during pregnancy. After 36 hours of life, the newborn started to cry persistently and disconsolately. The nurse thought the baby was hungry and made him formula milk. After 30 minutes, the baby continued to cry. The mother was trying to breastfeed him but without success. After 3 hours, the nurse gave him milk formula again. Because the baby cried excessively, a pediatrician approached the baby, and she noticed a blue-coloured right-sided hemi scrotum, absent cremasteric reflex and swelling of the right testis was found. Left testis on palpation was normal. Laboratory results were good. Ultrasound examination of the testicles showed an enlarged and heterogenous pattern of the right testis and mild hydrocele testis on the left side. The longitudinal diameter of the right testis was 1,5 cm, and the left testis was 0,8 cm. The right testis showed no perfusion on colour doppler sonography. The newborn was immediately transferred to the Clinic of Pediatric Surgery, where a right orchiectomy was performed.
Conclusion: An excessive cry by a newborn baby is not always attributed to a functional disturbance. Clinical examination is very important for early diagnosis and early management of this condition.
ID: 148/01-OP-L-d1B: 8
Oral Presentation (Onsite)
Topics: NEONATOLOGY
Keywords: Brachial plexus palsy, shoulder dystocia, birth injury, Narakas classification
Neonatal brachial plexus palsy - a seven-year experience
Azevedo, Aida Correia1; Silva, Ana Isabel2; Soares, Henrique1,3; Ferreras, Cristina1
1Department of Neonatology, Centro Hospitalar Universitário de São João, Porto, Portugal; 2Department of Physical Medicine and Rehabilitation, Centro Hospitalar Universitário de São João, Porto, Portugal; 3Department of Gynecology-Obstetrics and Pediatrics, University of Porto Medical School, Porto Portugal.
Introduction: Neonatal brachial plexus palsy (NBPP) is a motor and sensory disturbance of the upper limb related to injuries of the spinal nerves that constitute the brachial plexus, and it usually is a birth complication. NBPP is uncommon, with an incidence that ranges from 0.04 to 0.3% of live births. The only established risk factor for NBPP is shoulder dystocia. Other proposed risk factors don’t have predictive value for the occurrence of NBPP. This study aimed to know the NBPP incidence, characteristics and evolution in a tertiary hospital in Portugal.
Materials and Methods: A retrospective study was conducted in the Neonatology Department of a tertiary hospital. All cases of suspected NBPP occurring between 1 January 2015 and 31 December 2021 were documented, and statistical analysis was carried out using Excel(R).
Results: From a total of 16,507 live births, 52 cases of NBPP were included (incidence = 0,3%). Thirty cases (57,7%) occurred in male newborns, and the median birth weight was 3552 gr (maximum 4610gr/ minimum 2125gr). Regarding maternal history, the median gestational age was 39,2 weeks (maximum 41,3 weeks/minimum 31,9 weeks). Concerning the type of delivery, the majority of the cases (n = 41, 78,8%) occurred in instrumental deliveries, and shoulder dystocia was present in 12 cases (23,1%). Most cases were classified as Narakas type I (n = 42, 80,8%) and none were Narakas type IV. Radiography was the most requested exam, showing clavicle fracture of the affected side in 16 cases (30,8%). Electromyography was performed in 9 cases (17,3%), of which five (55,6%) were Narakas type III. Forty cases (76,9%) required physical/ occupational therapy, two cases (3,8%) surgery and one case (1,9%) botulinum toxin. Complete recovery occurred in 47 cases (90,4%) with a median recovery time of 5,5 months (minimum one month; maximum 14 months).
Conclusions: Our results were concordant with the literature. Some risk factors may be appointed but can occur in their absence. NBPP can be classified according to the severity of the palsy, which can predict the probability of full recovery. Early identification and management are essential to minimize the appearance of sequelae.
ID: 140/01-OP-L-d1B: 9
Oral Presentation (Onsite)
Topics: ALLERGY, IMMUNOLOGY & RESPIRATORY, NEONATOLOGY
Keywords: Neonatal, Pneumothorax, Chest Tube, Percutaneous Pigtail Catheter, Thoracostomy
Percutaneous pigtail catheters for management of neonatal pneumothorax: A better alternative to chest tube thoracostomy?
Vora, Shrenik Jitendrakumar; Goh, Marlene Samantha Sze Minn
KK Women’s and Children’s Hospital, Singapore, Singapore.
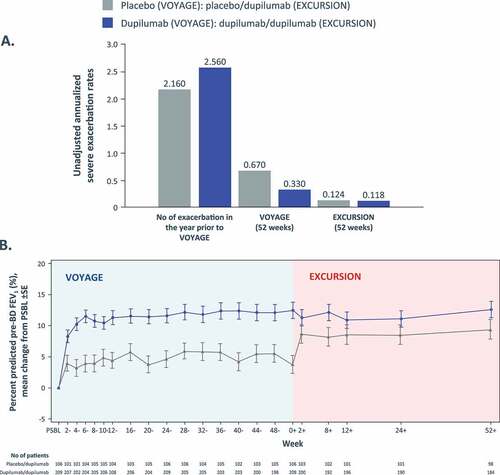
Background: Pneumothorax, the most common air leak syndrome, is potentially a life-threatening condition in neonates with little compensatory pulmonary reserve. Hemodynamically significant pneumothorax requires drainage with large-bore chest tubes, and more recently, the use of modified small-calibre percutaneous pigtail catheter has been suggested as a less invasive approach. This study aims to explicate the effectiveness and safety of both drainage systems in treating neonates with pneumothorax, exploring ease of insertion, rates of air-leak resolution, recurrence rates, and potential procedural complications.
Methods: This was a retrospective observational audit reviewing medical records of new-borns with symptomatic pneumothorax admitted to the tertiary neonatal intensive care unit of KK Women’s and Children’s Hospital, Singapore, between January 2017 and December 2020 and treated with either chest tube or pigtail catheters as the initial treatment approach. Demographic data, details related to pneumothorax, drain-related parameters, and outcome and efficacy parameters were compared among these two intervention methods.
Results: At our institution, the incidence of symptomatic pneumothorax was 0.3% among live-born infants (142 neonates out of 46,585 live births). About 1/3rd of symptomatic pneumothorax neonates needed chest tube drainage at our NICU (51/142). Out of 51 drainage procedures, 27 infants underwent pigtail insertion compared to 24 requiring chest tube thoracostomy. Baseline demographic data, including gestation at birth, birth weight, gender, mode of delivery and APGAR score of ≤5 at 5 minutes of life, were similar in both study groups. The time for radiological clearance and resolution of air leak, duration of drain in-situ, recurrence and complication rate, hospitalization duration and survival rate were also comparable. Group of infants who underwent pigtail insertion required significantly less sedation (51.9% vs 83.3%; p = 0.021) and invasive ventilation (63% vs 95.8%; p = 0.011) than chest tube insertion. Significantly smaller calibre (8.22 ± 1.6Fr vs 9.08 ± 1.44Fr; p < 0.05) catheter was required for pneumothorax drainage with a pigtail catheter. Pigtail catheter insertion was reported to be more operator friendly and requires significantly lesser operator’s post-graduate experience (8 ± 4 years vs 13 ± 8 years; p = 0.015) to achieve successful drainage (Table ).
Table 1. Demographic data, intervention details and outcomes of neonates requiring pneumothorax drainage
Conclusion: In conclusion, pigtail catheters achieved similar success in pneumothorax drainage, but with the usage of smaller- sized catheters, need for less sedation, reduced invasive ventilatory requirements and with no additional complication rates compared to chest tubes. Regarding efficacy and safety, Pigtail catheters are comparatively better alternatives to traditional chest tubes and should be considered the initial treatment of choice in treating neonatal pneumothorax.
ID: 260/01-OP-L-d1B: 10
Oral Presentation (Onsite)
Topics: GENERAL PEDIATRICS, NEONATOLOGY
Keywords: neonatal jaundice; transcutaneous bilirubinometry, screening, phototherapy
The impact of transcutaneous bilirubinometry as a screening tool for neonatal jaundice
Pais Cunha, Inês1; Leite Almeida, Laura1; Rabiço, David1; Silva, Débora1; Soares, Henrique1,2; Santos Silva, Jorge1
1Serviço de Neonatologia, UAG da Mulher e da Criança, Centro Hospitalar Universitário de São João; 2Faculdade de Medicina da Universidade do Porto.
Introductions: Neonatal jaundice (NJ) is frequent and occurs as a result of the deposition of bilirubin in the skin and mucosas exceeding 5 mg/dL in the blood. Its evaluation is essential in the first days of life to determine the need for phototherapy. Transcutaneous bilirubin measurement has proven effective, less painful, and less invasive in the neonatal age group.
Aim: We aimed to determine the prevalence of phototherapy after implementing transcutaneous bilirubinometry in our Perinatology department in 2021.
Methods: Retrospective analysis of newborns born between October and December 2020 and their homologous period in 2021 in a tertiary hospital.
Discussion: We identified 1016 newborns, 518 born in the 4th trimester of 2020 and 498 in the 4th trimester of 2021. The median gestational age was 39 weeks in both periods. The median weight at birth was 3200 g in both periods. In 2020, 53% of newborns were of the male gender, vs 51% in 2021. Globally, phototherapy indication was associated with vacuum-assisted deliveries and cesarian births vs eutopic deliveries (63% vs 37%, p = 0,017). There was a significant increase in the diagnosis of jaundice with the need for phototherapy in 2021, compared to 2020 (24% vs 18%, respectively, p = 0,013). Phototherapy was initiated earlier in 2021 vs 2020 (44 vs 46 hours of life, p = 0,008). Hospitalization was shorter in 2021 compared to 2020 (3 vs 4 days, respectively, p = <0,001).
Conclusion: We detected an increase in the implementation of phototherapy after introducing the transcutaneous method of assessing bilirubin. Furthermore, we also found a decrease in hospital length of stay in 2021. It is important to diagnose neonatal jaundice and implement phototherapy on time. The transcutaneous method has proven to be efficient in this context. Nevertheless, we must keep in mind excessive phototherapy’s side effects.
ID: 254/01-OP-L-d1B: 11
Oral Presentation (Onsite)
Topics: GENERAL PEDIATRICS, COVID-19
Keywords: Routine Immunization, COVID-19, Preventable diseases, Parents Education
“Provision of pediatric vaccination during the COVID-19 pandemic at tertiary care hospital and health care center, Abu Dhabi, UAE”
Abass, Maha; Alsheikh Bakrou, Farah; Hassan, Marwa; Fathalla, Waseem; Khan, Junaid; Fischer, Philip
SSMC/ Mayo Clinic, Abu Dhabi, United Arab Emirates.
Introduction: Currently, COVID-19 is responsible for alterations in pediatric care and during the time of quarantine, pediatric immunizations have been interrupted or delayed.
Objective: To assess compliance and reasons for the delay in pediatrics routine immunizations during the COVID-19 pandemic at a tertiary care hospital and an immunization center.
Method: Review of parents’ knowledge by using the SurveyMonkey application from Sept.2021 to Nov.2021 when they visited SSMC or Baniyas healthcare center. Parents were asked about their child’s age, vaccination status, and reasons for delayed immunizations. Counselling about necessary immunizations was provided, and parents were asked about the value of the counselling and their ongoing plans to immunize their child.
Result: 158 cases were met for counselling. Divided to 6 age groups: 0–1 month, 2–3 months, 4–5 months, 6–12 months, 13–18 months and 19 months—6 years (0.6%, 13.3%, 19%, 31.7%, 22.1%, and 13.3% respectively). 33.5% were up to date in vaccinations, 23.4% were partially vaccinated, and 21.5% received only birth or delayed vaccines. 103 cases of noncompliance (the child was sick 12 %, pandemic surge and delay apportionments 24%, 12 % concerns of COVID −19 exposure and 17 % social beliefs). 85.4% found the counselling informative. Out of 103, after counselling, 93 were willing to follow up.
Conclusion: To reduce the risk of outbreaks of vaccine-preventable diseases, further strategies are required, including immunization tracking, reminders, and awareness campaigns. During the pandemic, many children were under-immunized. With education and encouragement, families quickly became willing to get their children immunized.
ID: 114/01-OP-L-d1B: 12
Oral Presentation (Onsite)
Topics: GENERAL PEDIATRICS, COVID-19
Keywords: Multisystem Inflammatory Syndrome in Children (MIS-C), COVID-19, SARS- CoV-2, Intravenous Immunogobulin (IVIG), Corticosteroid therapy
A meta-analysis on the effectiveness of intravenous immunoglobulin plus corticosteroids vs immunoglobulin alone as initial therapy for COVID-19 associated Multisystem Inflammatory Syndrome in Children (MIS-C)
Carasig, Gianina Louise; Leon-Bala, Marivic; Piczon, Katrina; Tan-ting, Ann Marie; Valencia, Veronica Samantha
Cardinal Santos Medical Center, Philippines.
Background: Multisystem inflammatory syndrome in children (MIS-C) is the most severe pediatric disease associated with Coronavirus disease 2019 (COVID-19) infection, potentially life-threatening, for which the optimal therapeutic strategy remains unknown. There have been extensive observational studies that aim to describe treatment outcomes but have conflicting findings. Evidence is urgently needed to support treatment decisions for children with MIS-C. The assessment of the effectiveness of immunomodulatory medications may guide therapy for this novel disease.
Objective: This study aims to compare intravenous immunoglobulins (IVIG) plus corticosteroids vs IVIG alone as initial therapy in MIS-C in terms of left ventricular dysfunction, inotropic support, adjunctive immunomodulatory treatment, fever course, mechanical ventilator use, admission at the Pediatric ICU, and coronary artery aneurysm.
Methodology: Published articles reporting treatment outcomes of MIS-C cases were searched through databases of PubMed, The Cochrane Library, Google Scholar, and Research Gate. A structured data extraction form was employed, and the risk of bias was assessed with Newcastle-Ottawa Scale (NOS). Effects of corticosteroids on the desired outcomes were calculated and were reported as pooled odds ratio. Forest plots were generated for each outcome to show variations among studies and pooled analyses for visual presentation.
Results: A total of 1,391 MIS-C cases were initially enrolled from the three included studies, and 890 cases were analyzed. A variety of anti-inflammatory treatments were reported, with the majority of the population having received intravenous immunoglobulin (IVIG) alone. 483 cases were categorized under the IVIG + corticosteroids group, and 407 cases in the IVIG alone group. The risks of the components for hemodynamic support showed no significant difference between the two treatment groups: left ventricular dysfunction (P-value = 0.86), Inotrope use (P-value = 0.65), mechanical ventilator use (P-value = 0.21), and admission at the pediatric ICU (P-value = 0.87). However, initial treatment with IVIG plus corticosteroids, was associated with a more favorable fever course (P- value = < 0.02), less use of adjunctive immunomodulatory therapy (P-value = <0.00001), and less incidence of coronary artery aneurysm (P-value = < 0.04).
Conclusion: Among children and adolescents with MIS-C, initial treatment with IVIG plus glucocorticoids was associated with a more favorable fever course, less use of adjunctive immunomodulatory therapy, and less incidence of coronary artery aneurysm than IVIG alone. However, this study found no evidence that the combination therapy of IVIG and corticosteroid is associated with a favored effect on hemodynamic support of MIS-C patients.
Session
02-OP-L-d1C: Oral Presentations Session 2 - Day 1 - Zone C
Presentations
ID: 217/02-OP-L-d1C: 1
Oral Presentation (Onsite)
Topics: GENERAL PEDIATRICS, INFECTIOUS DISEASES
Keywords: Fever, drug resistance, microbial guidelines, pediatrics infectious disease, antibiotic stewardship, review
“Opportunities for antimicrobial stewardship in caring for febrile pediatric inpatients in Abu Dhabi”
Abass, Maha1; Khan, Junaid1; Fru Nsutebu, Emmanuel2; Fischer, Philip1
1Department of Pediatrics,SSMC/ Mayo Clinic, Abu Dhabi, UAE.; 2Department of Infectious disease, SSMC/ Mayo Clinic, Abu Dhabi, UAE.
Introduction: Fever management guidelines recommend against routine antibiotic prescribing without supportive evidence. Assessing when to use antibiotics may help improve health care and cost utilization.
Objective: To Emphasis on the importance of Guidelines and training for physicians on when to initiate antibiotics and empiric choices based on antibiograms. Education about criteria for initiating antibiotics and stopping antibiotics. To Provide Guidelines and systems to support clinicians in judicious and effective use of biomarkers such as procalcitonin.
Method: Retrospective electronic health record review from Jan.2020 to Jan.2021 with an initial ICD- code for fever. Cases were reviewed for investigations such as inflammatory markers, body fluid cultures, inpatient prescription of antibiotics or upon discharge and for the positive cultures with type of organism, specific antibiotics used, duration and drug resistance to that organism.
Results: 159 cases met the search criteria; of those 105 cases met the criteria of initial diagnosis of previously healthy with fever or other symptoms (Table ). Divided to 5 age groups 0–2 months, 3–12 months, 2–5 years, 6–9 years and ≥10 years (18%, 41.9%, 24.7 %, 5%, and 10% respectively). 100 patients received antibiotics (Table ), 76 of them for >2 days. Out of 105, 7 had positive body fluid cultures and received antibiotics for an average of 6 days (Table ). Of 98 with their cultures negative (23 received antibiotics for ≤2 days, 70 for >2 days, 5 didn’t receive antibiotics).
Table 1. Children admitted with fever
Table 2. Antibiotics used during hospitalization
Table 3. Patients with positive culture results, of total n = 105
Conclusion: As part of good antimicrobial stewardship, clinicians should monitor their own practices. While we identified potential over-initiation and over-prolongation of antibiotic treatment as possible targets for intervention, other centres in the Middle East have found their own specific targets to improve judicious use of antibiotics. Antimicrobial stewardship is essential as we deal with severe infections, healthcare costs, and increasing antimicrobial resistance. Identification of potential sources of overuse of antibiotics, such as over-initiation of treatment for febrile children and excessively long durations of treatment after negative blood culture results, can serve as a means of targeting subsequent antimicrobial stewardship interventions.
ID: 230/02-OP-L-d1C: 2
Oral Presentation (Onsite)
Topics: INFECTIOUS DISEASES, GASTROENTEROLOGY
Keywords: Vaccination, Rotavirus, Gastroenteritis, Public health
10-year experience with rotavirus vaccination in a secondary hospital in Portugal
Oliveira, Joao; Vivas, Inês; Cunha, Inês Pais; Branco, Sofia; Mazeda, Inês; Dinis, Maria José; Oliveira, Gracinda Nogueira
Department of Pediatrics and Neonatology, Centro Hospitalar Póvoa de Varzim - Vila do Conde.
Background: Despite recommendations from WHO and the vaccination commission of the Portuguese Society of Pediatrics, the rotavirus vaccine has not been included in the routine immunization schedule. Real-world effectiveness is variable and challenging to obtain. We aim to assess the efficacy of rotavirus immunization in reducing infection and the rate of hospitalization.
Methods: Retrospective study including all pediatric patients that had viral antigen stool tests performed in our hospital from 2012–2022. The patients were divided into positive and negative for rotavirus. Antigen test results were obtained with the collaboration of the pathology and microbiology departments, and vaccination status, hospitalization and duration of hospitalization were retrieved from electronic medical records. A randomized sample with the same size as the positive group was obtained from the negative group for group control assessment (N = 126).
Results: A total of 1087 viral antigen stool tests were performed, of which 126 (11,6%) were positive for rotavirus. The median age was 16 months (IQR 6–24) for the positive group and 12 months (IQR 4–29) for the negative group. Both groups had the same number of male patients (N = 69, 55%). A total of 81 (32%) patients were vaccinated. The vaccination rate was 15% in the positive group (N = 19) and 49% in the negative group (N = 62). Vaccination was associated with a reduced number of infections (P < 0,0001, OR 0,18–0,34), with only 23% (N = 19) immunized patients presenting with a positive antigen vs 63% (N = 107) of the non-immunized. The rate of hospitalization was also reduced with vaccination (P < 0,0001, OR 0,23–0,43), with 19% (N = 15) of immunized patients requiring hospitalization vs 50% (N = 85) of the non-immunized.
Conclusions: The vaccination rate was low (32%), which might demonstrate the lack of adherence to vaccines that are not included in the national immunization schedule. This study demonstrates the effectiveness of the rotavirus vaccination in preventing infection and hospitalization in our hospital. These results demonstrate the importance of considering the inclusion of the rotavirus vaccine in the routine immunization schedule.
ID: 270/02-OP-L-d1C: 3
Oral Presentation (Onsite)
Topics: GENERAL PEDIATRICS, INFECTIOUS DISEASES
Keywords: Neck mass, Bartonella henselae, Cat-scratch disease, Lymphadenopathy
An unusual neck mass in a teenage boy - a case report
Vivas, Inês; Oliveira, Joao; Mazeda, Inês; Branco, Sofia; Pais-Cunha, Inês; Nogueira Oliveira, Gracinda
Department of Pediatrics, Centro Hospitalar Póvoa de Varzim e Vila do Conde
Background: Superficial masses of the head and neck are a common finding in childhood and are usually benign. However, the broad differential diagnosis includes inflammatory, infectious, congenital, traumatic and even neoplastic etiologies. Some masses cause a lot of concern and unleash extensive investigations.
Case Description: 13-year-old boy was referred to the pediatrician with a 2-month history of a left submandibular mass. Besides fatigue, no other symptoms were reported. There was no history of local trauma, surgery or infection. His medical and family histories were unremarkable. He had a domestic cat for years and a feral kitten for 6 months. The family physician has initiated an 8-day course of amoxicillin/clavulanate with no response, and computed tomography of the head and neck showed a heterogeneous submandibular nodule measuring 3 × 2.5 cm. Physical examination revealed a tender, firm, fixed, well-circumscribed left submandibular mass measuring 4x3cm, and cat scratches on the arms. The rest of the physical exam was normal. Complete blood count, liver function, C-reactive protein, sedimentation rate and chest x-ray were unremarkable. Fine needle aspiration revealed epithelioid necrotizing granulomas (common finding of cat scratch disease—CSD) and was negative both for malignant cells and Mycobacterium tuberculosis (MT). Bartonella henselae IgM and IgG were positive (1:256 and 1:20), further confirming CSD diagnosis (active infection). He completed a 5-day course of azithromycin. At the 2-month follow-up, lymphadenitis had significantly improved (1.5x1cm).
Discussion: Despite having some alarming characteristics, the neck mass investigation ultimately revealed CSD lymphadenitis. Faced with a case of granulomatous lymphadenitis, CSD and MT must be considered for the differential diagnosis, and anamnesis about contact with cats or MT-positive cases should always be asked. To conclude, the authors emphasize the importance of a thorough history and physical examination in order to establish an accurate diagnosis and treatment.
ID: 236/02-OP-L-d1C: 4
Oral Presentation (Onsite)
Topics: GENERAL PEDIATRICS, INFECTIOUS DISEASES
Keywords: Human parechoviruses; Sepsis-like febrile syndromes, Newborn
Humam parechovirus (HPeV), an agent to be aware of in newborn severe illness
Strecht Guimarães, Francisca; Alves Araújo, Sara; Ferreira Mendes, Joana; Aguiar, Benedita; Gomes, Lúcia
Centro Hospitalar de Entre o Douro e Vouga, Pediatric Department, Portugal
Background: Human parechoviruses(HPeV) are common in childhood, especially prevalent under 3 years of age. HPeV can cause a wide spectrum of manifestations, ranging from mild respiratory and gastrointestinal symptoms to severe illnesses such as sepsis-like febrile syndromes, meningitis and encephalitis in very young infants. In Europe, HPeV usually circulates in spring and summer, and despite being common, severe cases remain infrequent. We describe 3 cases of parechovirus disease in newborns in a level II hospital, which occurred between July and August of 2022.
Case: A 12-day-old newborn previously uneventful history was admitted to the emergency room (ER) with a fever of 1 hour, vomiting and irritability. At observation, no other alteration was found. Sepsis work-up and lumbar puncture were performed, and the infant was hospitalized and initiated Ampicillin/Gentamicin. Later, HPeV was detected in the cerebrospinal fluid(CSF) without other findings, including normal ultrasonography, and he presented an improvement. (1) A 17-day-old-newborn previously uneventful history was admitted to ER with a fever for 10 hours and a liquid detection. In that case, no alterations were found at the examination, analytical study and lumbar puncture. He was hospitalized with empirical antibiotherapy with ampicillin and gentamicin. An HPeV was detected in CSF, transfontanelar ultrasonography was normal, and he presented an improvement. (2) A 12-day-old preterm(36 weeks) was observed in ER for less activity, irritability, grunting, and poor feeding starting that day. At observation, she presented hypotonia, hyporeactivity, intermittent horizontal nystagmus and irregular breathing. Sepsis work-up, urine collection and lumbar puncture were performed, and she was admitted to the neonatal intensive care unit(NICU) with ampicillin/gentamicin/cefotaxime for suspected meningitis. On the 2nd day, she initiated seizures and phenobarbital was started. She required NIV with nCPAP, and due to echocardiogram findings, aminergic support was administered. The complementary study revealed an HPeV in CSF and K. pneumoniae in urine culture. (3) As a consequence of worsening seizures and state of convulsive condition, she was transferred to the NICU of a level III hospital for EEG monitoring. During the internment, transfontanelar ultrasonography revealed diffuse hyperechogenicity of the white matter. She gradually improved, and after stabilization and anti-epileptic dose adjustment, she returned to the hospital of origin.
Discussion: The prevalence of severe disease is unknown, especially in newborns; however, clusters have been recently described. It’s an entity that we must not forget when approaching newborns or infants with fever. Considering the cases described, all newborns presented with fever, but only one had sepsis-like conditions associated with addiction to neurological events. The prognosis and long-term neurological effects remain uncertain, and monitoring these patients is important for the early detection of possible complications.
ID: 110/02-OP-L-d1C: 5
Oral Presentation (Onsite)
Topics: INFECTIOUS DISEASES
Keywords: coronavirus, MIS-C, intensive care
Multisystem inflammatory syndrome – could respiratory syncytial virus be a trigger?
Syed, Amir Hamza1; Chochkova, Lyubov Atanasova2; Komitova, Radka Todorova3; Paskalveva, Ivanka Nikolova2; Angelova, Andreana Christova4; Atanasova, Maria Vasileva4
1Faculty of Medicine, Plovdiv Medical University, Bulgaria; 2Department of Pediatrics and Medical Genetics, Faculty of Medicine, Medical University of Plovdiv, Bulgaria; 3Department of Infectious Diseases, Parasitology and Tropical medicine, Faculty of Medicine, Medical University of Plovdiv, Bulgaria; 4Department of Microbiology and Immunology, Faculty of Pharmacy, Medical University of Plovdiv, Bulgaria
Background: Acute coronavirus disease (COVID-19) in children causes a less severe course and lower hospitalisation rate when compared to adults. However, a small subset of paediatric patients develops a rare and novel set of clinical features called multi- system inflammatory syndrome in children (MIS-C). This is of significant concern due to its severity and the necessity of intensive care treatment.
Case Presentation - Summary: A previously healthy three-year-old male presented with seven days of fever, cough and watery diarrhoea with further one-day history of difficulty breathing. A computed tomography (CT) scan of his chest from the referring hospital showed bilateral infiltrations. He was exposed to his father with an undifferentiated respiratory infection three weeks earlier. [1] Physical examination revealed a febrile, toxic-appearing patient who was tachypnoeic, tachycardic, and hypotensive with wheezing on auscultation in both lungs. He was admitted to the paediatric intensive care unit, where he was managed with crystalloid boluses and Milrinone with an adequate response. Echocardiography showed a small pericardial effusion and left ventricular dysfunction without coronaritis. [2] Laboratory investigations showed elevated inflammatory markers, evidence of coagulopathy, and elevated B-type natriuretic peptide. Blood cultures were sterile. The patient had a positive respiratory viral panel for respiratory syncytial virus (RSV), negative SARS-CoV-2 PCR but positive SARS-CoV-2 IgG. [3] The patient received broad-spectrum antibiotics (meropenem and teicoplanin), intravenous immunoglobulin, methylprednisolone and enoxaparin. He was discharged after a hospital stay of 18 days and markedly improved with a tapering steroid regimen over 3 weeks.
Discussion of Learning Points: MIS-C in children is a rare but severe condition linked to COVID-19. [1] Our case serves as a reminder for clinicians to be vigilant and to timely initiate appropriate therapy [2] There remains much to learn about how SARS-CoV-2 triggers an abnormal immune response leading to MIS-C. [3] RSV—is it a coincidence or a trigger?
ID: 224/02-OP-L-d1C: 6
Oral Presentation (Onsite)
Topics: INFECTIOUS DISEASES, GASTROENTEROLOGY
Keywords: Entamoeba dispar; Amebiasis
Persistent Entamoeba dispar infections, what do we expect?
Ferreira Mendes, Joana1; Luís Tomé, Maria2; Alexandra Azevedo, Inês1; Oliveira, Sara1; Almeida, Claudia1; Costa, Miguel1
1Centro Hospitalar de Entre Douro e Vouga, Pediatric Department, Portugal; 2Centro Hospitalar de Vila Nova de Gaia/Espinho, Pediatric Department, Portugal
Background: Several non-pathogenic protozoa may be identified in stool samples sent to the laboratory. However, it is important to be able to distinguish between commensal organisms and those that require treatment. Unlike amebiasis caused by Entamoeba histolytica (E. histolytica), most infections by Entamoeba dispar (E. dispar) are asymptomatic and do not require treatment. However, some strains can induce intestinal damage and liver abscess. E. dispar cannot be morphologically distinguished from E. histolytica. In countries where amoebic infections are endemic, asymptomatic patients incidentally identified with amebae are frequently presumed to have an infection with E. dispar and are not treated. The antigen tests and Polymerase Chain Reaction (PCR) are sensitive and essential to distinguish between both. We describe a case of persistent colonization of E. dispar.
Case Presentation: A 7-year-old boy, previously healthy, was observed at Emergency Room for persistent diarrhoea (2–3 times per day, without blood or mucus) associated with anorexia that persisted even with lactose eviction. No reference to vomit, fever or weight loss. On examination, no alteration was observed. Proceeded to stool collection and reference to Pediatric Gastroenterology consultation. At the consultation, diarrhoea was solved. He had favourable weight-stature evolution, and no more symptoms were referred. The bacteriological and virological faecal studies were negative. The parasitological faecal study, 3 samples, revealed the presence of E. dispar/histolytica with positive PCR for E. dispar. Given that the patient is asymptomatic and E. dispar is a non- pathogenic agent, we decided not to implement treatment and maintain follow-up. During follow-up, the boy remained asymptomatic although, E. dispar persisted in sample analyses. After four years, an analytical study including immunodeficiency showed a slight deficit of immunoglobulin G1 and G3. Considering the decrease in IgG1 and IgG3 and possible immunodeficiency related, treatment with 10 days of metronidazole was proposed but was suspended early for adverse effects. The follow-up was maintained in our consultation for early detection of associated symptoms and the possible need for treatment.
Learning Point/Discussion: The E. dispar disease has a broad spectrum, varying from asymptomatic forms to nondysenteric colitis and, less commonly, amoebic liver abscess. The impact on patients with immunodeficiencies or even in the case of immunosuppressive therapies is not fully understood, so in these cases, it is important to follow them up for early detection of possible disease.
ID: 237/02-OP-L-d1C: 7
Oral Presentation (Onsite)
Topics: INFECTIOUS DISEASES, NEUROLOGY
Keywords: Vertigo, Vestibular Neuronitis, Influenza A
Post-infectious vertigo - a rare but challenging condition in pediatric age
Araújo, Sara Alves1; Ventura, Inês2; Cunha, João Macedo1; Ruano, Luís1; Pinheiro, Marta Isabel1; Monteiro, Joana1; Pinto, Mariana1
1Centro Hospitalar de Entre o Douro e Vouga, Portugal; 2Centro Hospitalar de Vila Nova de Gaia e Espinho
Background: The prevalence of vertigo in pediatric age is low, and it is often difficult to establish. Its etiology is diverse, with vestibular neuritis being one of the principal causes, especially in adolescence. It usually occurs due to vestibular nerve affection during or after a viral infection of the upper airway tract. Its diagnosis, although challenging, is clinical, and the accompanying symptoms are fundamental for determining differential diagnoses.
Case Presentation Summary: A 13-years-old female with a personal history of prematurity was admitted to the emergency department (ED) due to vertigo aggravated with head movements, gait imbalance, nausea and vomiting with three days of evolution. No other associated symptoms, referring to clinical improvement with supine position and sleep. Reported influenza A infection in the week before the onset of symptoms. Objectively she had horizontal nystagmus to the left and a positive Romberg test. Neurology assessment revealed a positive Head Impulse Test with head rotation to the right. The clinical case was also discussed with otorhinolaryngology, establishing the clinical diagnosis of vestibular neuronitis. The patient was discharged home with oral corticosteroid therapy, with clinical improvement during the first week of treatment and partial resolution of the symptoms. After starting steroid weaning, vertigo worsened, with associated frontal headache and tinnitus, motivating a new admission to the ED. The patient was reassessed by Neurology, maintaining horizontal nystagmus in levoversion with fast phase to the left and presenting hyperreflexia and positive Babinski sign. Therefore, she was hospitalized for etiological investigation. Brain and spinal magnetic resonance imaging showed no changes. Corticosteroid therapy was adjusted during hospitalization, with progressive clinical improvement, and she was asymptomatic at discharge, thus validating the diagnosis of peripheral vertigo.
Learning Points and Discussion: The present case illustrates a situation that, although frequent in adulthood, is rare in pediatric age. The sudden clinical onset after a viral infection was decisive in the diagnosis. However, the unexpected clinical course, accompanied by pyramidal signs, led to a diagnostic doubt. Through a thorough clinical history and complementary diagnostic tests, it was possible to exclude potentially serious illness, frame the pyramidal signs in the context of prematurity and validate the initial diagnosis, reinforcing vestibular neuronitis as a probable immune-mediated benign complication of several common viral infections of childhood and adolescence.
ID: 188/02-OP-L-d1C: 8
Oral Presentation (Onsite)
Topics: PUBLIC HEALTH, COVID-19
Keywords: COVID-19, RSV, hospitalizations
What happened to RSV seasonality after the COVID-19 pandemic?
Pais-Cunha, Inês1; Oliveira, João2; Vivas, Inês3; Pais Cunha, Inês3; Branco, Sofia3; Dinis, Maria José3; Oliveira, Gracinda3
1Serviço de Pediatria, Centro Hospitalar Universitário São João, Portugal; 2Serviço de Pediatria, Centro Materno Infantil do Norte, Portugal; 3Serviço de Pediatria, Centro Hospitalar Póvoa de Varzim Vila do Conde.
Introduction: During the COVID-19 pandemic, several interventions were enforced to prevent spreading, namely, mask-wearing and hand hygiene. These measures seemed to impact spreading of other infectious diseases, namely, other respiratory viruses.
Aim: We aimed to compare the seasonality of the Human respiratory syncytial virus (RSV) before and after the pandemic.
Methods: Retrospective analysis of pediatric patients hospitalised due to RSV infection complications from March 2018 to July 2022. We defined the fall-winter period from October to March and the spring-summer period from April to September. Admissions before 11 March 2020 were considered pre-pandemic and post-pandemic after this date.
Results: We included a total of 103 patients, 45% females, with a median age of 3 months (14 days-3 years). At the time of admission: 40% presented with feeding difficulties, 63% with respiratory distress and 2% had their first acute febrile seizure. Regarding comorbidities: 8% had previous wheezing, and 3% were preterm newborns. In the pre-pandemic period, all admissions (n = 72) occurred during the fall-winter period, and there were no cases reported in spring and summer. In the post-pandemic period: no patients were hospitalised in the fall-winter of 2020–2021. Subsequently, admissions were registered during both seasons: 7 patients in spring-summer 2021, 17 patients in fall-winter 2021–2022 and 7 patients in spring-summer 2022. Furthermore, there were no statistical differences between the median length of hospitalisation in the pre and post-pandemic periods (4 days in both periods, p = 0.544).
Discussion and Conclusion: Our study shows the predictable pattern of RSV in the pre-pandemic period, with hospitalisations occurring exclusively in the fall-winter period. On the contrary, following the COVID-19 pandemic outbreak, we noticed a change in this RSV seasonality. (1) During the 2020–2021 fall-winter period, there were no cases of RSV hospitalisation, probably in relation to all the health measures taken at the time. (2) The extraordinary absence of immunity to RSV during this time, along with lifting some of the pandemic restrictions, increased RSV out-of-season activity. This resulted in an increased incidence of infections during the spring and summer periods. Nevertheless, both the virulence of RSV and the hospitalisation length did not seem to change, regardless of the pandemic. These results alert us to the consequences of the pandemic in other viruses’ seasonality. Subsequent studies are needed to understand these epidemiologic shifts better to plan seasonal healthcare measures.
ID: 202/02-OP-L-d1C: 9
Oral Presentation (Onsite)
Topics: ALLERGY, IMMUNOLOGY & RESPIRATORY, COVID-19
Keywords: Asthma, COVID-19, bronchial hyperresponsiveness, Long-Covid
Asthma and SARS-CoV-2 – Acute exacerbations or a long-term problem?
Oliveira, Joao1; Lima, Joana baptista1; Pinto, Diana1,2; Fernandes, Alexandre1,3; Araújo, Ana Rita1,2; Teixeira, Fernanda1,2
1Department of Pediatrics, Centro Materno Infantil do Norte, Centro Hospitalar Universitário do Porto; 2Department of Pediatric Allergology, Centro Materno Infantil do Norte, Centro Hospitalar Universitário do Porto; 3Department of Pediatric infectious diseases and immunodeficiencies, Centro Materno Infantil do Norte, Centro Hospitalar Universitário do Porto.
Background: In 2020, SARS-CoV-2 emerged as a new challenge to the medical community. Its severity was unknown; therefore, many patients with medical conditions, including asthma, were considered at higher risk of severe disease. Hence, additional precautions to prevent SARS-CoV-2 infection in asthmatic patients were taken. However, the association between asthma and SARS- CoV-2 remains unclear.
Objectives: We aimed to evaluate the prevalence of asthma or recurring wheezing in patients diagnosed with SARS-CoV-2 at our tertiary hospital and determine its association with infection severity.
Methods: Retrospective descriptive study including all pediatric patients with a positive SARS-CoV-2 PCR test followed in our hospital between March 2020 to September 2021. The variables included were the diagnosis of asthma, recurring wheezing, hospitalization, symptoms at diagnosis and persistency of symptoms on periodic reevaluations. We defined bronchial hyperresponsiveness (BH) as the combination of asthmatic and recurring wheezing patients.
Results: A total of 242 patients were included; 55,0% (n = 133) were male, with a median age of 48,0 months (IQR 133,0). About 13,2% (n = 32) had bronchial hyperresponsiveness, of which 34,4% (n = 11) were asthmatic and 65,6% (n = 21) had recurring wheezing. There was no significant difference in the severity of the disease or duration of symptoms. BH was associated with an increased risk of respiratory distress at diagnosis (p = 0.003, OR 5.4), symptoms persistency at 4 weeks (p = 0.001, OR 5.2), especially chronic cough and asthenia (p = 0.005, OR 5.9 and p = 0.002, OR 5.9 respectively) and with Long-COVID (p = 0.03, OR 2.5). Asthmatic patients also had an increased risk of asthenia at diagnosis (p < 0.01, OR 17.1) and at 4 weeks (p = 0.001, OR 9.9), chronic cough at 24 weeks (p = 0.013, OR 13.0) and higher risk of Long-Covid (p = 0.004, OR 5.2).
Discussion: In our study, SARS-CoV-2 infection in asthmatic and BH patients was not a risk factor for severe disease or acute exacerbations. However, it was associated with long-term side effects, with asthmatic patients reporting persistent asthenia and cough 6 months after infection. These results demonstrate that the relationship between asthma and SARS-CoV-2 is not linear. Therefore, it is important to perform longer studies on these patients to determine the impact of SARS-CoV-2.
ID: 241/02-OP-L-d1C: 10
Oral Presentation (Onsite)
Topics: ALLERGY, IMMUNOLOGY & RESPIRATORY
Keywords: pneumothorax, cluster, spontaneous pneumothorax, atmospheric pressure, temperature
Clusters of spontaneous pneumothorax - what might influence it?
Azevedo, Aida Correia; Rodrigues, Ana Sofia; Pinto, Filipa; Bordalo, Diana; Fonseca, Paula; Martins, Cecília; Teixeira, Paulo; Carvalho, Sónia; Carvalho, Fernanda
Pediatrics Department, Centro Hospitalar do Médio Ave, Portugal.
Introduction: Pneumothorax results from the presence of air in the pleural space and can be clinically divided into spontaneous pneumothorax (SP) and nonspontaneous. SP can be categorized as primary when it occurs in individuals with no underlying lung disease and secondary. In pediatrics, pneumothorax is mainly primary spontaneous and is relatively uncommon, appearing more often in male adolescents. It has been reported that SP may occur in clusters often influenced by external factors, such as changes in atmospheric pressure, and temperature, among others.
Aim: The study aimed to characterize a cluster of SP in a level two hospital and correlate their occurrence with some external factors.
Methods: A descriptive, retrospective study was conducted between October 2019 and January 2020 in the Pediatrics Department of a level two hospital in Portugal. All SP diagnosed during the established period were included in our study. Statistical analysis was performed.
Results: A total of seven SP were diagnosed during the study period, of which five were primary and two were secondary (one patient had an apical bleb, and the other had bronchiectasis resulting from bronchiolitis obliterans). The median age was 15.4 years old, and the majority of the patients were male (n = 6). Two patients presented recurrence of the pneumothorax during the period of the study. The left side was more affected (n = 6), and three patients required surgery to resolve the pneumothorax. When evaluating some external factors that may explain this cluster of SP, we found that in some cases, there were slight changes in temperature, precipitation, atmospheric pressure, wind and humidity; however, none presented a statistically significant correlation with the occurrence of SP.
Discussion: Our study reported seven cases of SP. When compared to a ten-year casuistry from our Pediatrics Department that reported only nine cases of SP, our number is significantly higher considering the time period; therefore, we considered it to be a cluster. (1) Clusters of SP have been gaining some recognition in literature, and there are some factors, such as sudden changes in atmospheric pressure, variation in temperature, and humidity, among others, that have been appointed as possible causes for the occurrence of SP clusters. Our study found no statistically significant results. However, the external factors that were analyzed concerned a large territorial area, so we cannot completely rule out the causal effect of these factors in the occurrence of SP clusters.
ID: 205/02-OP-L-d1C: 11
Oral Presentation (Onsite)
Topics: NEONATOLOGY
Keywords: very low birth weight infants, neurodevelopmental outcome, comparative study
Very low birth weight infants and neurodevelopmental outcome: a two-point comparative study
Tavares, Catarina Faria1; Alvelos, Rita2; Costa, Raquel Monteiro1; Almeida, Nuno Serra1; Sousa, Pedro Maneira1; Diogo, Clara1; Figueiredo, Cecília1; Andrade, Isabel1
1Centro Hospitalar Tondela Viseu, Portugal; 2Centro Hospitalar do Baixo Vouga, Portugal.
Background: Over the past few decades, improvements in neonatal care have resulted in better survival rates for very low birth weight infants (VLBWIs). Still, survival is not an adequate measure of success in these babies who remain at high risk for behavioural and neurodevelopmental morbidities. Early identification of children at risk for neurodevelopmental impairment can increase access to intervention, potentially influencing the outcome.
Aim: This study aims to analyse the neurodevelopment outcome of VLBW infants born over a seven-year period and compare it with a similar study from the previous decade.
Methods: This retrospective study included VLBWIs born between 2013 and 2019 who were regularly followed up at our hospital. The results were compared with a similar study with the same inclusion criteria and time frame (2000–2006).
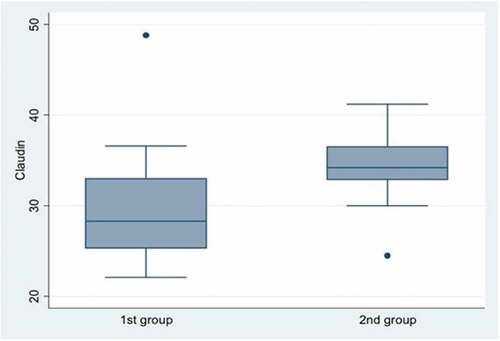
Results: Among the 83 VLBWIs who met the inclusion criteria, 54% were female. There were 34% of VLBWIs from twin pregnancies, and the mean gestational age was 30 weeks (24–37), with an average birth weight of 1160 g (585–1500). (1) Regarding neonatal morbidity, sepsis was the most frequent complication (52%), followed by hyaline membrane disease (36%), persistent ductus arteriosus (28%), bronchopulmonary dysplasia (17%), periventricular leukomalacia (13%) and peri-intraventricular hemorrhage (11%). (2) A total of 89% of the VLBWIs had a neonatal ophthalmologic evaluation, of which 16% had retinopathy of prematurity. Of note, there was one case of microphthalmia and the diagnosis of strabismus in 5% of cases. (3) Nearly all VLBWIs had 18-month follow-ups (98%), and 51% had 5-year follow-ups. During this follow-up, 51% of children were referred to the National System of Early Childhood Intervention, 37% needed physical therapy and 32% speech therapy. Four had cerebral palsy, six had global development delays, thirteen had language delays, and two had attention deficit hyperactivity disorder. (4) From the studied population, 75% underwent formal neurodevelopmental assessment (Ruth Griffiths scale), with a general quotient ranging from 69 to 123 (median of 104). (5) Compared to the previous study, there was a reduction in the number of VLBWIs (139/83). Despite this, the distribution by gender, gestational age and birth weight was similar. Regarding neonatal morbidity, there was an increase in the incidence of sepsis (18%/52%) and patent ductus arteriosus (6%/28%), as well as a slight decrease in IPVH (17%/11%). There was a higher rate of formal neurodevelopment evaluations (51%/75%) with a higher median general quotient score (94/104).
Conclusion: Between the two studies, we have shown a decrease in VLBWIs, partly due to a lower birth rate. On the other hand, there was a higher rate of neurodevelopment evaluations with a higher median score, which can be explained by the increase in resources allowing earlier intervention and, therefore, better outcomes.
ID: 238/02-OP-L-d1C: 12
Oral Presentation (Onsite)
Topics: GENERAL PEDIATRICS, HAEMATOLOGY/ONCOLOGY
Keywords: Autoimmune lymphoproliferative syndrome, immunodeficiency, cytopenias, lymphoproliferation
Autoimmune lymphoproliferative syndrome (ALPS) - A new mutation with an early presentation
Ashworth, Joanna1; Lachado, Ana1,2; Cleto, Esmeralda1,2; Costa, Emilia1,2; Guerra, Isabel1,2
1Pediatric Department Centro Materno Infantil do Norte- Centro Hospitalar e Universitário; 2Paediatric Haematology Unit, Centro Materno-Infantil do Norte (CMIN) - Centro Hospitalar Universitário do Porto (CHUPorto), Portugal (PT).
Background: Autoimmune lymphoproliferative syndrome (ALPS) is an underestimated diagnostic immunodeficiency that should be thought of when non-malignant lymphoproliferation and autoimmunity are present. The prevalence and incidence of this disease are unknown since many cases are undiagnosed due to the phenotypic variability, expression and symptoms that can be attributed to other diagnoses. The pathophysiology involves a disorder of lymphocyte apoptosis, resultant to somatic or germline mutations.
Case Presentation Summary: The authors present an eight-year-old girl diagnosed with ALPS in the first semester of her life. Autoimmunity was the first manifestation, as she had autoimmune hemolytic anemia in the second month of life. At four months of age, in the face of a new cytopenia emergence, spleen enlargement and high level of double negative T-lymphocytes (35.8%), the hypothesis of ALPS was considered. The diagnosis was confirmed after identifying a pathogenic heterozygous mutation (c.736A>G; p.Lys246Glu in exon 9) in the FAS gene, which until now had not been described in the literature. In the perspective of controlling lymphoproliferation and cytopenias without resorting to long-term corticosteroid therapy that she ended up performing only at 16 months of age, she started an antiproliferative T cell agent, sirolimus at 13 months of age.
Learning Points/Discussion: With the description of this case, the authors intend to highlight the possibility of an early presentation of this disease, which has a median age of appearance described in the literature of 2.7–3 years. Some cohorts described the disease onset lymphoproliferation followed by autoimmunity, but autoimmunity can be the first manifestation. In this case, immune cytopenias and lymphoproliferation (splenomegaly) were almost simultaneous. There are two main immunosuppressive agents to treat ALPS, mycophenolate and sirolimus. The choice of the treatment regimen should be based on the underlying phenotype disease and balanced by the associated side effects. Mycophenolate can be the best choice if immune cytopenias are the major manifestation, and sirolimus to control lymphoproliferation and consequent cytopenias. Scientific evidence exists on the efficacy of sirolimus monotherapy in ALPS, suggesting that sirolimus should be considered as a first-line, steroid-sparing treatment for patients needing chronic therapy. It leads to complete and durable responses in most children with refractory multilineage autoimmune cytopenias. Regardless of the child’s age, when cytopenias and lymphoproliferation are present, ALPS should be considered, and its investigation carried out. This way, diagnostic acuity can be improved, and treatment started accordingly, which can positively impact these patients’ lives.
Session
03-OP-L-d1D: Oral Presentations Session 3 - Day 1 - Zone D
Presentations
ID: 277/03-OP-L-d1D: 1
Oral Presentation (Onsite)
Topics: ADOLESCENT MEDICINE, PUBLIC HEALTH
Keywords: Adolescent health, Electronic cigarette; Vape pen; Puff bars; Survey
Disposable electronic cigarette or Puff use among adolescents
Barrense-Dias, Yara1; Cros, Jérémy1; Berthouzoz, Cathy2; Dubuis, Alexandre2; Chok, Lorraine1; Lebon, Luc1; Zürcher, Karin1; Suris, Joan-Carles1
1Center for Primary Care and Public Health (Unisanté), Switzerland; 2Addictions–CIPRET, Promotion santé Valais, Sion, Switzerland.
Background: Released in 2019 in the US market and 2020 in the Swiss market, the disposable electronic cigarette is part of the fifth generation of e-cigarettes. This product is also known as Puff or Puff Bar. This study aims to determine the prevalence rates of Puff use among adolescents in the French-speaking part of Switzerland, as well as their perceptions of this product.
Methods: The questionnaire was shared during the summer of 2022 via social networks through sponsored ads and influencers targeting young people aged between 14 and 25 years old living in the French-speaking part of Switzerland. All youth meeting these criteria, whether or not they used Puff, were asked to participate. The analytic sample included 1340 individuals (52.3% cisgender females, 43.4% cisgender males, and 4.3% transgender). Because the sample was not constructed according to probabilistic principles, weights were calculated to adjust the sample.
Results: More than 90% of the participants had already heard about Puffs, mostly from friends (76%). Among these participants, 31% were current Puff users (several uses in the last 30 days), 17% were former or occasional users (several uses but not in the last 30 days), 16% were one-time users (one try), and 36% had never used. No differences were found in terms of age, place of birth, place of residence, family structure and socioeconomic status between the four groups. On the contrary, gender differences were found, with cisgender females reporting more being current Puff users. Among youth who had ever used a Puff, the last one was mostly obtained from a kiosk (54%), followed by friends (33%) and, far behind, siblings (4%). Almost 20% did not know the amount of nicotine in their Puff, and 18% reported using nicotine-free Puffs. The top three benefits of the puffs reported were the flavours (62%), smell (39%) and convenience (31%).
Conclusions: This study shows significant Puff use among youth with a strong presence of peers in terms of knowledge and availability. While some regions have established an age limit for acquiring these products, the majority purchase from kiosks, even those under the age of 18. With regard to the attraction of youth to the flavours proposed by these products and the presence, or the lack of knowledge of the presence, of nicotine, it is important to make youth, but also adults, aware of the potential risks in terms of dependence and gateway to other substances.
Funding
Health Promotion and Prevention Department (Unisanté)
ID: 281/03-OP-L-d1D: 2
Oral Presentation (Onsite)
Topics: ADOLESCENT MEDICINE, PUBLIC HEALTH
Keywords: adolescent; mental health; well-being; cross-national; HBSC; gender
Dual continua model of adolescent mental health: cross-national evidence from 45 European countries
Cosma, Alina1; Hammami, Nour2; Chzhen, Kat1
1Trinity College Dublin, Ireland; 2Trent University, Canada.
Background: Most previous studies relied on disease-based models, identifying symptoms of mental illness (e.g., anxiety, depression or behavioural problems), and considered mental health as merely the absence of mental illness. Yet, recent evidence shows that the absence of mental illness is a necessary but not sufficient criterion of optimal mental health.
Method: The Dual-factor Model conceptualises mental health as a complete state comprised of two unique but correlated dimensions (subjective well-being and psychopathology) and uses ratings of subjective well-being and psychopathology to classify people into four categories. Thus, optimal mental health requires a positive sense of well-being in addition to the absence of clinically significant, active mental illness. However, a salient weakness of this model is that it has been tested only on small samples, mainly in North America and the UK, with limited evidence from Ireland and cross-national studies. Therefore, in this study, we will test this framework using large representative cross-sectional data from the Health Behaviour in School-aged Children Study (HBSC) (N > 220,000 participants, age range 11 to 15).
Discussion: Our main research questions are: Is there cross-national variation in the adolescent dual-factor model? What are the main predictors for each class? Are there gender differences? This study is part of an MSCA-IF funded project (GenerationZ; Marie Sklodowska-Curie grant agreement No 101028678) with TCD as a host institution. The project has recently started, and analyses are underway, with results ready to be reported by the EiP conference in December.
ID: 256/03-OP-L-d1D: 3
Oral Presentation (Onsite)
Topics: ADOLESCENT MEDICINE
Keywords: mental health literacy, stigma, help-seeking, adolescence
Examining the effects of mental health literacy, and personal and perceived stigma on adolescent help-seeking intentions.
Goodfellow, Claire1; Sosu, Edward2; Macintyre, Anna2; Knifton, Lee3; Inchley, Joanna1
1University of Glasgow, UK; 2University of Strathclyde, UK; 3Mental Health Foundation, UK.
Background: Adolescence is an especially vulnerable period for the development of mental health problems, and seeking help early from informal or formal sources of support and help promote more positive outcomes. Despite this, many young people who could benefit from support do not seek help. Lack of help-seeking is associated with worse mental health outcomes; it is, therefore, vital to understand mechanisms to improve help-seeking among adolescents. Low help-seeking in adolescence may be due to comparatively lower mental health literacy (MHL). MHL is a multidimensional construct; however, little is known about how discrete dimensions of MHL may influence formal and informal help-seeking among adolescents. Stigma is also a known deterrent to help- seeking though less is known about how stigma and MHL interact within an adolescent population. (1) This research aimed to identify discrete dimensions of MHL and examine how specific forms of stigma and MHL interact to influence help-seeking. Specifically, the extent to which personal stigma mediates the relationship between MHL and intended help-seeking and whether perceived stigma from others (parents and friends) may affect these relationships.
Methods: A cross-sectional survey was used to collect data from adolescents in schools across Scotland (n = 734). Data were analysed using Confirmatory Factor Analysis and Structural Equation Modelling. Group differences in key associations based on age, gender, and SES were also examined.
Results: Analysis identified two distinct forms of MHL: one reflecting adolescents’ knowledge of treatment efficacy and another representing adolescents’ ability to identify a mental health problem. Importantly, while knowledge of treatment efficacy was associated with increased intention to seek formal and informal help, adolescents’ ability to identify a mental health problem was associated with reduced intention to seek informal help. Informal help-seeking intention was strongly associated with formal help- seeking. (1) Personal stigma did not mediate MHL and help-seeking intention. Perceived stigmas from others acted as moderators indicating that MHL is particularly important in promoting help-seeking among adolescents who perceive greater stigma from friends and parents.
Conclusions: This study is novel in identifying that distinct dimensions of MHL have disparate associations with adolescent help- seeking intention. Improving knowledge of treatment efficacy and reducing perceived stigma may be particularly important in promoting formal help-seeking. Furthermore, findings suggest that involving peers and parents in interventions could be effective in promoting help-seeking. The inclusion of parents in such interventions may be particularly important in increasing help-seeking from formal services, in which parents typically act as gatekeepers.
ID: 191/03-OP-L-d1D: 4
Oral Presentation (Onsite)
Topics: ADOLESCENT MEDICINE, PUBLIC HEALTH
Keywords: Adolescent mental health, school, neighbourhood, social characteristics, physical characteristics
Independent associations between residential neighbourhood and school characteristics and adolescent mental health in the Netherlands
Brons, Hilde; Bolt, Gideon; Helbich, Marco; Visser, Kirsten; Stevens, Gonneke
Utrecht University, Netherlands, The
Aim: The aim of this study was twofold.
Method & Results: First, we examined associations between characteristics of the residential neighbourhood and the school and adolescent mental health, including the moderating role of family socioeconomic status (SES) and family support. Nationally representative Dutch data of 2017 from adolescents aged 12–16 (N = 6422) were analysed through cross-classified multilevel models. Findings showed that school characteristics are more strongly linked to adolescent mental health than residential neighbourhood characteristics. More specifically, higher levels of school SES were associated with more hyperactivity-inattention problems, while higher levels of school social disorder were related to more conduct problems and more peer relationship problems. Further, higher levels of school SES were associated with more emotional symptoms only for adolescents with a relatively low family SES. Higher levels of neighbourhood SES were associated with fewer peer relationship problems.
Method & Results: Overall, there was little evidence for the moderating role of family SES or family support. Second, we examined trends of residential neighbourhood and school effects on adolescents’ mental health between 2005 and 2017 using nationally representative Dutch data from adolescents aged 11–16 (N = 26,678). We performed separate analyses for primary school students and secondary school students. Overall, we found relatively stable associations over time between the neighbourhood and school characteristics and adolescent mental health for both primary and secondary school students. There were a few exceptions in which neighbourhood and school effects on adolescent mental health changed over time. For instance, the association between school SES on adolescent hyperactivity-inattention problems for secondary school students became stronger over time.
ID: 156/03-OP-L-d1D: 5
Oral Presentation (Onsite)
Topics: ALLERGY, IMMUNOLOGY & RESPIRATORY, ADOLESCENT MEDICINE
Keywords: smoking prevalence, lung function, teenagers
Smoking prevalence and pulmonary function in smoking and nonsmoking teenage children
Mandadzhieva, Stoilka; Marinov, Blagoi; Kostianev, Stefan
Medical University of Plovdiv, Bulgaria.
Introduction: Smoking is a major environmental risk factor for developing obstructive lung disease. Childhood smokers experience more respiratory symptoms and have poorer lung function than their non-smoking peers. This study aimed to assess the smoking prevalence and whether there is a difference in lung function between smoking and nonsmoking children in the age span of 15–17 years.
Materials and Methods: One hundred sixty-four children (32 male/132 female), mean age = 16.1 ± 0.8 (SD), range 15–17 years, performed pulmonary function testing, including measurement of lung volumes and flows, and single-breath diffusing capacity for carbon monoxide (TLCO). The study also implemented a questionnaire for assessing the children and their parents’ smoking habits.
Results: The percentage of active and passive smokers was very high—42.7% and 64.6%, respectively, and grew with age. Nonsmoking children had greater absolute values for most spirometric indices, but a significant difference was obtained for FEV1/VC% (88.24 vs 91.79, p < 0.05) and MEF25% (106.45 ± 30.90 vs 118.75 ± 36.43, p < 0.05). A tendency for lower diffusing capacity (TLCO) was also apparent. Passive smoking in the family adversely influences the pulmonary function of children, especially in the group of smokers.
Conclusions: Over one-third of the children aged 15–17 years are smokers. The total percentage of smoking teenagers rises with age. Early onset of cigarette smoking, in addition to passive smoking at home, can lead to deteriorated pulmonary function.
ID: 282/03-OP-L-d1D: 6
Oral Presentation (Onsite)
Topics: ADOLESCENT MEDICINE, PUBLIC HEALTH
Keywords: alcohol use; tobacco use; gender; structural determinant; HBSC
Structural gender inequality and gender differences in adolescent substance use: A multilevel study from 45 countries
Cosma, Alina1; Elgar, Frank2; de Looze, Margreet3; Canale, Natale4; Lenzi, Michela4; Inchley, Jo5; Vieno, Alessio4
1Trinity College Dublin, Ireland; 2McGill University, Canada; 3Utrecht University; 4Padova University, Italy; 5University of Glasgow, UK.
Purpose: Although adolescent substance use has declined, young people’s tobacco and alcohol use levels are still among the highest in Europe and North America. Historically, boys reported higher levels of substance use than girls; however, in recent decades, gender convergence in adolescent substance use was observed in some, mostly Western, countries. Previous research has shown associations between societal gender inequality and gender differences in some externalizing behaviors in adolescents. Therefore, there is a need to go beyond individual-level associations and apply a socio-ecological perspective when examining gender differences in adolescent substance use. This study examines whether gender differences in adolescent substance use relate to societal gender inequality.
Methods: Current and lifetime substance use (i.e., alcohol drinking, drunkenness, cigarette smoking) were measured in 11-, 13 and 15-year-olds in the 2017/18 Health Behaviour in School-aged Children study (n = 224,876). Individual data were linked to national gender inequality (Gender Inequality Index, 2018) in 45 countries and regions, and their association was tested using mixed effects (multilevel) logistic regression models.
Results: Large cross-national variations were observed in gender differences in substance use. Greater gender inequality at the country level was associated with heightened gender differences in substance use, however, with different effects depending on the substance type. For most substances, few gender differences emerge in countries characterized by low levels of gender inequality. The largest gender differences were observed in countries characterized by high gender inequality.
Conclusions: Societal gender inequality reflects social and cultural norms that relate to adolescents’ engagement with substance use. Public health policy should target societal factors impacting young people’s behavior.
ID: 266/03-OP-L-d1D: 7
Oral Presentation (Onsite)
Topics: GENERAL PEDIATRICS, PUBLIC HEALTH
Keywords: Dynamometry, Cardiovascular, Percentiles, Overweight, Obesity
Handgrip Strength Dynamometry in children and adolescent health evaluation. The PESCA program percentiles reference
Zárate-Osuna, Fernando1,2,4,5; Quesada-González, Carlos1,3; González-Gross, Marcela1,2; G. Zapico, Augusto1,2
1ImFINE Research Group, Universidad Politécnica de Madrid, Spain; 2Department of Health and Human Performance, Universidad Politécnica de Madrid, Madrid, Spain; 3Departamento de Matemática Aplicada a las Tecnologías de la Información y la Comunicación, Universidad Politécnica de Madrid, Madrid, Spain; 4PESCA Program Coordinator; 5Paediatrics Department, Quirónsalud Hospitals (Alcorcón-Madrid, Toledo).
Background: Handgrip Strength Dynamometry (HSD) has been identified as a useful tool as a health marker. Its relationship with Body Mass Index (BMI) and Body composition allow for obtaining a suitable cardiovascular health approximation for both children and adolescents. Few updated references are available. Therefore, sample-size studies are needed to provide reliable values. In n Spain, the PESCA program protocol has included yearly HSD measures for every child since 2018.
Aim: This study aims to provide a reference HSD table according to age and sex for children and adolescents aged 3 to 15.
Methods: PESCA program yearly covers a 5-step protocol consisting of (1) a questionary, (2) BMI, (3) Body Composition Bioimpedance (BIA), (4) HSD and (5) a Physician Physical Examination. 1772 children and adolescents (47,4% girls) aged 2 to 17 have been included from schools in Madrid and Toledo from October 2018 to May 2022. HSD is measured with a Takei dynamometer (0–100 Kg). Two measures are made 60 seconds apart: the child standing with the arm extended parallel to the trunk (dominant hand) and, on command, exerting the maximum possible force for 10 seconds while he/she is encouraged to give his/her best. Highest measured is recorded. Data analyses were made with 25 v. IBM SPSS (IBM Corporation, Armonk, NY, EUA). The sample is segmented into whole number age for both boys and girls. Average, Standard Deviation and Percentiles are given for each age from 3 to 15.
Results: From a 1772 total sample size, 25 subjects were scheduled as lost values (the subject could not complete properly handgrip technique or data were failure recorded). Thus, children aged 2, 16 or 17 and girls aged 15 were not considered for curves due to insufficient group size. Table and Figure show results for boys and girls.
Table 1. PESCA Handgrip Strength Dynamometry (HSD) percentiles
Conclusions: PESCA program protocol includes HSD as part of cardiovascular health evaluation. Although it is an easy, quick, and not-expensive tool, its clinical use is not common yet in primary care medicine, nor overweight and obesity evaluation. The present study provides a new HSD reference for males and females aged 3–15, which might help to identify children and adolescents at risk, with a need for further clinical and cardiovascular health tracing.
ID: 186/03-OP-L-d1D: 8
Oral Presentation (Onsite)
Topics: GASTROENTEROLOGY
Keywords: connective tissue dysplasia, gastroduodenal pathology, reflux, immunometabolism, children and adolescents
Evidence-based Approaches to the Prevention of Gastrointestinal Pathology in Children and Adolescents with Non-inflammatory hereditary Connective Tissue Disorders
Yakovleva, Inna; Bogmat, Ludmila
Institute for Children and Adolescents Health Care of the National Academy of Medical Sciences, Ukraine
The clinical manifestations of the upper digestive system diseases in adolescents with hereditary connective tissue dysplasia (CTD), such as Ehlers-Danlos, Marfan, and other CTD syndromes, are characterized by motility disorders in the forms of duodenogastric and gastroesophageal refluxes (77%), specific conditions in immune reactivity and low of interstitial collagens with structural changes in gastroduodenal mucosa (Yakovleva, Bogmat, 2017, 2021).
Purpose: To improve the prevention of gastroduodenal pathology in children and adolescents based on the pattern interactions of the immune system indicators and connective tissue (CT) metabolism.
Methods: A total of 155 adolescents 11 to 18 years of age with inflammatory-destructive diseases of the upper gastrointestinal tract were studied. CTD was revealed in 90 adolescents, and another 65 peers without CTD were included in the comparison group. Collagens content in the lamina propria of the gastric-duodenum mucous membrane was evaluated by immunohistochemistry using monoclonal antibodies of collagen I, III, IV, and V types. Biopsy samples were investigated in the luminescent microscope using light filters. Immune homeostasis was determined according to monocyte-phagocyte, cellular, humoral links, antibodies to collagen and elastin, and salivary secretory IgA (sIgA). We used correlation analysis and multiple linear regression as statistical methods for determining causal connections between indicators. A system correlation analysis of indicators of immunity and exchange of connective tissue was carried out using the method of correlation structures (Zosimov, Golik, 2000).
Result: The system correlation analysis revealed depressive (hypocompensatory) modus in the background of the CTD, which is reflected in the destabilization of connections between elements of the immune system and separation of subsystems of immunity (B-, T-system with the macrophage-phagocyte link). According to the pathogenesis pattern (Figure ) and the relationship between collagens and immune indicators, depression of the cellular link of immunity leads to a decrease in the activity of the phagocytic function of macrophages in adolescents with CTD. In turn, this weakens the cleavage of excess collagen by collagenase and the absorption of fragments of collagen fibres by macrophages and reduces the stimulating effect on fibroblasts. This interaction of CT and immune cells leads to excessive growth of collagen in the gastroduodenal mucosa. Morphological analysis confirms the above findings (Yakovleva, 2021). A significantly high sIgA (0,264 g/l, p < 0.001) due to collagen deficiency has a compensatory focus on normalizing CT-metabolism through stimulating the phagocytic function of macrophages as well as reduction of autoimmune processes through a decrease in antibodies to collagen. It has been established that refluxes contribute to decreasing sIgA (r2 = 0,75) through the development of foveolar dysplasia in the mucosa, disturbing the balance in the system of CT- and immunometabolism. (1) To prevent the development of inflammatory-destructive lesions of the gastrointestinal tract in children and adolescents at the earliest stage, we recommend 1. For diagnosis of reflux, when examining children with gastrointestinal complaints, it is necessary to identify external and visceral signs of CTD 2. To diagnose refluxes using a simple method based on the determination of sIgA in saliva (Patent for utility model, UA) 3. Traditional therapeutic complexes should include the correction of psycho-emotional disorders with the mandatory inclusion of prokinetic drugs 4. To correct immune homeostasis, taking into account the depressive (hypocompensatory) modus of its functioning, the most appropriate energy subsidy to immune cells in the form of energy-producing metabolites and stimulation of the T- system immunity to weaken the fibrosis process through direct increasing of phagocytosis ().
Figure 1. The main immunopathogenesis patterns in adolescents with gastroduodenal pathology.

Conclusion: The role of connective tissue metabolism in the progression of gastroduodenal pathology has been established, and prevention approaches have been developed on this evidence basis.
ID: 232/03-OP-L-d1D: 9
Oral Presentation (Onsite)
Topics: GENERAL PEDIATRICS, HAEMATOLOGY/ONCOLOGY
Keywords: Back pain, Adolescents, Ewing’s sarcoma
Back pain in adolescence – a diagnosis to be aware
Branco, Sofia Varela1; Vivas, Inês1; Pais Cunha, Inês2; Oliveira, João Nogueira3; Mazeda, Inês1; Saraiva, Sílvia1
1Department of Pediatrics, Centro Hospitalar Póvoa de Varzim e Vila do Conde - Portugal; 2Department of Pediatrics, Centro Hospitalar Universitário de São João - Portugal; 3Department of Pediatrics, Centro Materno Infantil do Norte - Portugal.
Background: Back pain in adolescents is common. Characterising the pain and identifying red flags are essential to exclude potentially serious conditions.
Case Presentation Summary: A 17-year-old female adolescent with no significant past medical history presented intermittent left posterior thoracic pain of a six-month evolution that worsened and became pleuritic pain accompanied by dyspnea on exertion in the last three months. There was no response to analgesic medication, and trauma was excluded. Cough, fever and weight loss were denied. The patient reported multiple visits to primary health care. Since the physical examination was normal, her family doctor interpreted this back pain as an anxiety problem, and in the last visit, requested spine radiography that revealed mild dorso-lumbar scoliosis (Cobb angle 15°) and also detected a left pulmonary opacity. Due to this finding, chest radiography was performed and showed an extensive left pulmonary opacity with ipsilateral pleural effusion. The adolescent was referred to the emergency department, and the physical examination at the admission yielded a mild skin pallor, a reduced vesicular murmur in the left hemithorax and a left posterior thoracic mass inferior to the shoulder blade. Blood studies were within normal parameters. Computed contrasted tomography of the thorax showed a soft tissue mass (93 cm x 63 cm) with heterogenous enhancement on the sixth posterior costal arch with bone destruction, suggestive of Ewing’s sarcoma (ES). Additionally, a left medium pleural effusion and bilateral metastatic lung nodules were identified. The patient was transferred to the oncology reference centre, and the incisional biopsy confirmed the diagnosis: the histology reported numerous small round blue cells dispersed and arranged in clusters, with round nuclei, fine chromatin and inconspicuous nucleoli; the immunohistochemical analysis showed membranous positivity for CD99, FLI1 and cyclin D1; the molecular pathology detected the EWSR1-FEV rearrangement. Staging procedures identified bone and lung metastases. Treatment with multiagent induction chemotherapy was conducted in accordance with the Euro Ewing 2012 protocol, and the patient is regularly controlled.
Discussion: ES is a rare tumour that mainly affects adolescents (peak of incidence at 15-year-old), and the majority of patients present with locoregional pain that worsens over time. The median time to diagnosis is 3–9 months, and metastasis is the most significant adverse prognostic factor. The presentation of this case pretends to create awareness among physicians to include ES in the differential diagnosis of back pain that is unexplained and persistent in young people.
ID: 280/03-OP-L-d1D: 10
Oral Presentation (Onsite)
Topics: NEUROLOGY
Keywords: Congenital disorders of glycosylation, PMM2-CDG, Cerebellar atrophy
Congenital Disorder of Glycosylation - when to suspect ?
Rodrigues, Ana Sofia1; Friedrich, Sebastian2; Eckenweiler, Matthias3
1Pediatrics Department, Centro Hospitalar do Médio Ave, Vila Nova de Famalicão, Portugal; 2Center for Pediatrics - Department of general pediatrics, adolescent medicine, and neonatology, Medical Center - University of Freiburg, Freiburg im Breisgau, Germany; 3Department of Neuropediatrics and Muscle Disorders, Medical Center - University of Freiburg, Faculty of Medicine, University of Freiburg, Freiburg, Germany.
Introduction: Congenital disorders of glycosylation (CDG) are a group of hereditary diseases characterized by a deficiency of enzymes involved in protein glycosylation1. We describe the clinical case of an infant with CDG type 1a, nowadays designated phosphomannomutase 2 (PMM2)-CDG.
Case Report: A 6-months-old girl was presented to our department with a history of percentile crossing of weight, length and head circumference and developmental delay (Figure ). She was the second child of non-consanguineous parents with irrelevant heredofamilial background. Prenatal ultrasounds were normal, and a karyotype was performed with 46, XX,t(11;18)(q21;q21.1) in the 1st culture and normal in the 2nd culture, probable pseudomosaic. Born at 41 + 3 weeks, vaginally, Apgar score 10/10, birth weight of 3510 g (p40). The postnatal examination was normal, as was the hearing screening. Ophthalmological observation at 4 months revealed strabismus and questionable macular reflex. On admission, she weighed 6000 g (<p3) and presented abnormal fat distribution, “orange-peel” skin, inverted nipples and genitals with labial hypertrophy. Neurological examination showed axial hypotonia with poor head control, hyporeflexia in the lower extremities and palmar grasping reflex still present. Ophthalmological examination revealed strabismus and reduced fixation behaviour but couldn’t confirm the missing macular reflex. Diagnostic findings included hepatopathy (increased transaminases and hyperechoic liver parenchyma), coagulopathy, metabolic and endocrinological disorders. Imaging studies showed cerebellar atrophy in the MRI and a minimal pericardial effusion on echocardiography. Given the potential diagnosis of CDG, a metabolic study was performed. PMM2-CDG was suspected and confirmed by genetic study with a compound heterozygous pathogenic variant in PMM2 (exon 7 (c.574T>C, p.C192r) and exon 8 (c710C>T, Pt237M)).
Conclusion: PMM2-CDG, a rare metabolic disease, is the most frequent form of CDG and is divided into three clinical stages. The patient presented here has an infantile multisystem presentation, which is characterized by cerebellar dysfunction, abnormal fat distribution, inverted nipples, strabismus and hypotonia. Clinical diagnosis of CDG represents a challenge for physicians due to multiple organ involvement and a wide variety of phenotypes. In this case, many of the typical features of PMM2-CDG that are represented should prompt early metabolic and genetic diagnostics.
ID: 154/03-OP-L-d1D: 11
Oral Presentation (Onsite)
Topics: NEUROLOGY
Keywords: migraine, vitamin D3 supplementation, prophylaxis, pediatric, topiramate
The Impact of vitamin d3 supplementation to topiramate therapy on pediatric migraine Prophylaxis
Abdelwahab Elmala, Moustafa Kotb
Nizwa hospital.Pediatric department.Sultanate of Oman.
Background: Vitamin D plays a role in the secretion of chemical mediators involved in migraine pathophysiology. It is unclear whether vitamin D has a specific role in pediatric migraine prevention—still, a need for more studies to evaluate the role of vitamin D3 in pediatric migraine prophylaxis.
Methods: This study was conducted in Nizwa city, Sultanate of Oman, from June 2021 to December 2021. The patients were recruited at Nizwa Hospital. 56 participants completed the study. 34 females (60.7%) and 22 males (39.3%) with ages ranging from 8 to 14 years (mean 10.6 ± 3.4 years). (1) A double-blinded prospective clinical trial was conducted. They were randomly assigned in a 1:1 ratio into 2 groups, one with vitamin D3 supplementation (the supplementation group) and the other without vitamin D supplementation (the placebo group). The supplementation group received topiramate plus one 5000-IU dose of vitamin D3 daily for 6 months. The placebo group received topiramate with a placebo capsule without any effective substances. All participants were inhabitants of Adakhlia Governorate, mainly in Nizwa City, with equal exposure to direct sunlight. The diagnosis of migraine was based on the International Classification of Headache Disorders–III (ICHD-III) diagnostic criteria, with normal vitamin D3 serum level (>30 ng/mL) and no vitamin D3 supplements within the past 3 months. The severity of the headache was determined according to the MIDAS scale as grade I: 0–5, grade II: 6–10, grade III:11–20, and grade IV: 21.19. The primary outcomes were a monthly frequency of headache attacks, a good response to intervention, and a reduction in migraine severity, duration, and disability before and after treatment. A good response to treatment was defined as more than a 50% decrease in the monthly headache attack frequency during follow-up.
Results: Vitamin D3 supplementation with topiramate was more effective than the placebo group in the reduction of monthly frequency (6231.31 vs 9792.24 times, P = .01) and disability score for migraines (17 566.43 vs 25 187.65, P = .04). A good response was observed in 76.13% of patients in the vitamin D3 supplementation group and 53.5% of patients in the placebo group, and vitamin.D3 supplementation was significantly more effective than placebo (P = .01). Side effects were observed in 13.3% and 20% of the intervention group and placebo groups, respectively, P = .5. (1) Comparisons of migraine characteristics before and after intervention in the vitamin D3 supplementation group and placebo group showed that vitamin D3 supplementation with topiramate was more effective than the placebo group in the reduction of monthly frequency, severity, duration, and disability of migraines.
Conclusion: Accordingly, vitamin D3 supplementation may improve pediatric migraine prophylaxis by daily administration of vitamin D 5000 IU as an adjuvant therapy to topiramate. Further randomized controlled trials with larger sample sizes and a longer duration of follow-up are recommended. Vitamin D3 supplementation in pediatric migraine prophylaxis could be a well-tolerated, safe, and effective strategy.
ID: 222/03-OP-L-d1D: 12
Oral Presentation (Onsite)
Topics: PSYCHIATRY
Keywords: ADHD; knowledge; teachers; questionnaire
How much do teachers know about ADHD?
Rodrigues, Ana Sofia1; Pereira, Patrícia G.2; Cerqueira, Daniela2; Pereira, Marta3; Pessanha, Margarida2
1Pediatrics Department, Centro Hospitalar do Médio Ave, Vila Nova de Famalicão, Portugal; 2USF Esposende Norte, ACeS Cávado III - Barcelos/Esposende; 3Education Division, Câmara Municipal de Barcelos.
Background: Attention-deficit hyperactivity syndrome (ADHD) is one of the most common neurodevelopmental disorders affecting school-age children globally. It is characterized by an ongoing pattern of inattention and/or hyperactivity-impulsivity that interferes with functioning or development. The present study aims to describe teachers’ knowledge from a group of schools in an urban area about ADHD through interviews about general information, symptoms/diagnosis and treatment.
Methods: A descriptive cross-sectional study was carried out from November to December 2021, involving 128 teachers from three public schools. Teachers were evaluated by a questionnaire composed of 36 items with three alternative answers (true, false, I don’t know), named the knowledge of attention deficit disorders scale (KADDS), validated for the Portuguese population. It has contained three subscales: general information, symptoms/diagnosis and treatment. All the participants were informed about the study design and provided informed consent.
Results: The questionnaire’s response rate was 37% (128 out of 350). The majority of the teachers were females (74%), between 40 and 60 years of age (87%) and had 20–30 years of experience (63.4%). Teachers’ total mean knowledge score about ADHD was 48.5%. In the subscale of ADHD symptoms/diagnosis, they presented a better score (70.5%), while mean knowledge score for the general information about ADHD was lower (38%). Regarding the subscale of ADHD treatment, teachers answered correctly in about 45.3% of the questions. (1) There were no statistically significant differences between the years of practice and general knowledge about ADHD (r = −.093, p = .304). Also, there was no association between years of practice and the three subscales of the questionnaire (r = −.052, p = .564). Concerning teachers’ age, there was no correlation with general knowledge about ADHD (r = .007, p = .304). However, regarding the subscales of the questionnaire, the younger teachers have more knowledge about symptoms/diagnosis and treatment of ADHD (r = −.151, p = .088; r = −.162, p = .067, respectively).
Conclusion: Teachers are one of the most important agents of socialization during infancy, and their knowledge about this disorder is essential for diagnosis and treatment success. Thus, they present as one of the most important groups that should be sensitized about ADHD and must receive information and training concerning it. According to our study, mean knowledge scores for ADHD general information and ADHD treatment scales were lower than 50%, indicating the need to raise awareness about this disorder and the need for more interventions. In conclusion, the study showed that the younger the teachers are, the more informed they are about ADHD.
Conference Agenda
Session
04-OP-L-d2A: Oral Presentations Session 4 - Day 2 - Zone A
Presentations
ID: 199/04-OP-L-d2A: 1
Oral Presentation (Onsite)
Topics: NUTRITION & DIETS, GASTROENTEROLOGY
Keywords: breastfeeding, infant formula, gastrointestinal, patient-reported outcome measures
A partially hydrolyzed, whey-based, ready-to-feed infant formula is well tolerated by healthy newborns during the immediate postnatal period in Saudi Arabia: a post-market observational study
Hays, Nicholas P.1; Ballarin, Audrey2; Blankenspoor, Madeleine2; Lavalle, Luca2; Sameer, Moustafa3; Sroda, Inez2; Vissers, Yvonne4; Mizyed, Mohammad5
1Nestlé Product Technology Center – Nutrition, Vevey, Switzerland; 2Clinical Research Unit, Nestlé Research, Lausanne, Switzerland; 3Nestlé Medical and Scientific Affairs, Jeddah, Saudi Arabia; 4Nestlé Product Technology Center – Nutrition, Konolfingen, Switzerland; 5Dr. Sulaiman Al Habib Hospital, Riyadh, Saudi Arabia.
Background: Feeding intolerance occurring during the early postnatal period can be distressing for families and may delay discharge from the postnatal ward if symptoms are severe. The purpose of this open-label, single-arm, real-world effectiveness study was to describe the gastrointestinal (GI) tolerance of healthy term formula-fed (exclusively or partially breastfed) infants during the birth hospitalization period.
Methods: Infants (n = 150; 54% female) of mothers who had previously and independently decided to formula feed were enrolled ≤24 hours after birth. All infants were fed with a single formula (halal, ready-to-feed, 100% partially hydrolyzed whey protein-based in line with the protein requirements set in Annex I of Delegated Regulation [EU] 2016/127) until hospital discharge (≤4 days after birth), in accordance with standard practice of the study hospital. Parent-reported GI symptoms and GI-related behaviors were assessed using the Newborn Infant GI Tolerance eDiary (completed daily) and the GI Tract Function sub-scale of the Neonatal Eating Assessment Tool (NeoEAT; completed at discharge). The eDiary was used to record the presence/severity of 9 GI symptoms/behaviors over the previous 24 hours, rated on a scale from 0 (never) to 5 (always) and summarized into 2 domain scores (GI Symptoms, range 0–25; GI Related Behaviors, range 0–20). The NeoEAT was used to evaluate symptoms related to gastroesophageal reflux, swallowing coordination, GI discomfort, and gagging, with scores ranging from 0 to ~140. In both instruments, lower scores indicate fewer symptoms. Safety was assessed using physician-reported adverse events (AEs).
Results: Mean ± SD scores for individual items on the eDiary ranged from 0.12 ± 0.40 (fussiness/irritability) to 1.26 ± 0.90 (spitting- up) for formula-fed infants and 0.13 ± 0.35 (fussiness/irritability) to 1.09 ± 0.64 (gassiness) for mixed-fed infants (Table ), indicating reported incidences of “never” to “almost never” for each GI symptom/behavior. Mean ± SD scores for the GI Tract Function subscale of the NeoEAT questionnaire were 8.6 ± 5.3 for formula-fed infants and 9.9 ± 7.4 for mixed-fed infants, which are substantially lower than the 25th percentile values (24.5 and 28, respectively) observed in a reference population of young infants. Five non-serious AEs were reported: 2 reports of mild vomiting and 3 reports of hematemesis due to swallowed maternal blood during delivery. All AEs were determined to be unrelated or unlikely to be related to study formula by the study investigator.
Table 1. Mean ± SD parent-reported gastrointestinal (GI) symptoms of formula-fed infants during the immediate postnatal period
Conclusions: GI symptoms and behaviors indicative of GI distress were very infrequent and mild in formula-fed infants during the immediate postnatal period. These results indicate that the partially hydrolyzed, whey-based, ready-to-feed infant formula was well accepted and tolerated during this period among healthy newborns in Saudi Arabia.
ID: 126/04-OP-L-d2A: 2
Oral Presentation (Onsite)
Topics: NUTRITION & DIETS, ADOLESCENT MEDICINE
Keywords: vitamin D, osteomalacia, Arab adolescents, nutritional markers
Establishing the Prevalence of osteomalacia in Arab adolescents using nutritional biomarkers of bone health.
Al-Daghri, Nasser M.1; Yakout, Sobhy1; Sabico, Shaun1; Wani, Kaiser1; Aljohani, Naji2; Uday, Suma3; Högler, Wolfgang4
1King Saud University, Riyadh, Saudi Arabia; 2King Fahad Medical City, Riyadh, Saudi Arabia; 3University of Birmingham, Birmingham, UK; 4Johannes Kepler University Linz, Linz, Austria
Objective: The gold standard for osteomalacia diagnosis remains taking a bone biopsy, an invasive procedure that most patients would not agree to. Establishing less invasive diagnostic criteria for this underdiagnosed entity is essential. This study was designed to assess the prevalence of biochemical osteomalacia in Saudi adolescents.
Methods: In this cross-sectional study performed between September 2019 and March 2021, Saudi adolescents aged 12–17 years from 60 different secondary and preparatory year schools in Riyadh, Saudi Arabia, were included. Anthropometrics and fasting blood samples were collected. Biochemical osteomalacia was defined as a combination of any two of the three markers of impaired mineralization, namely; low 25 hydroxyvitamin D (25OHD<30 nmol/l); high serum alkaline phosphatase (age-and sex-specific adjusted reference ranges) and low calcium-phosphate product (<2.41 mmol2/l2).
Results: A total of 2938 Saudi adolescents [1697 girls; mean age (years) 14.8 ± 1.8 and median body mass index, BMI of 23.1 kg/m2 (19.4, 26.4); 1241 boys; mean age 15.1 ± 1.6 and BMI of 24.3 kg/m2 (20.4, 27.1)] participated. Vitamin D deficiency was noted in 58.9% (n = 1731) girls and 31.4% (n = 923) boys (p < 0.001). The overall prevalence of biochemical osteomalacia was 8.6% (n = 252/2938). The prevalence was higher in girls than boys (11.2% vs 5.0%, OR = 2.40, 95% CI 1.8–3.2, p < 0.001). The prevalence of low calcium-phosphate product was also higher in girls than in boys (12.3% vs 6.8% respectively, p < 0.001). In contrast, high ALP was more common in boys than in girls (10.7% vs 7.5%, p = 0.004).
Conclusions: Screening of healthy Saudi adolescents revealed a high prevalence of abnormal mineralization markers suggestive of biochemical osteomalacia, with girls being more affected than boys. The proposed combination of typically altered mineralization markers is, at best, suggestive of osteomalacia until further comparisons with established diagnostic tools are conducted.
ID: 192/04-OP-L-d2A: 3
Oral Presentation (Onsite)
Topics: GENERAL PEDIATRICS, NUTRITION & DIETS
Keywords: Nutrients, myelin, brain, motor development, toddler
Nutrient-driven increases in infant myelination are linked with toddler motor development (CONNECT clinical trial)
Schneider, Nora1; Hartweg, Mickaël2; Beauchemin, Jennifer3,4; D’Sa, Viren3,4; Deoni, Sean3,4
1Nestlé Institute of Health Sciences, Société des Produits Nestlé S.A., Switzerland; 2Clinical Research Unit, Société des Produits Nestlé S.A., Switzerland; 3Department of Pediatrics, Brown University, 02912 Providence, USA; 4Rhode Island Hospital, Hasbro Children’s Hospital, 02903 Providence, USA.
Background: First results from our randomized controlled trial in term infants demonstrated significant differences in myelin structure, volume, and rate of myelination as early as 3 and 6 months of life in favour of higher levels of myelin-relevant nutrients, including docosahexaenoic acid, arachidonic acid, iron, vitamin B12, folic acid as well as sphingomyelin from a uniquely processed whey protein concentrate enriched in alpha-lactalbumin and phospholipids compared to lower levels (1). As observational studies suggest a latency between brain structural and behavioural benefits (2–4), we aimed to explore the relevance of these early myelin differences for later developmental outcomes.
Methods: N = 81 enrolled full-term, neurotypical infants of both sexes were randomized into either the investigational (N = 42) or the control group (N = 39). N = 108 breastfed infants served as a reference group. Myelin measures were derived from MRI scans; language, cognitive and motor development was assessed using Bayley Scales of Infant and Toddler Development, 3rd edition (Bayley-III). Spearman correlations were performed (21 pairs for 3-month myelin correlation with 12-month motor development, 15 pairs for 6-month myelin correlation with 12-month motor development).
Results: We found statistically significant associations between whole brain myelin levels at both 3 and 6 months with motor development at 12 months of age (rho = 0.48, p = 0.03 and rho = 0.62, p = 0.01, respectively). This finding was further supported by more specific correlations of myelin in both fine motor (rho = 0.55, p = 0.04) and gross motor regions (rho = 0.57, p = 0.03) at 6 months with motor development at 12 months of age. No statistically significant correlations were identified for 24 months nor for the language or cognitive scales of the Bayley-III for the age group investigated.
Conclusions: Our findings suggest that nutrient blend containing docosahexaenoic acid, arachidonic acid, iron, vitamin B12, folic acid, as well as sphingomyelin from a uniquely proceed whey protein concentrate enriched in alpha-lactalbumin and phospholipids can impact normal infant brain development through myelination which is positively associated with motor development in toddlers. The significant associations at 12 months may be linked to the rapid increase of motor abilities at that age (5), including critical motor milestones such as standing alone and walking without support (6–8), suggesting sensitive windows for specific developmental areas that may benefit from nutritional interventions. Findings are in line with the suggested latency between brain structural and behavioural maturation.
ID: 150/04-OP-L-d2A: 4
Oral Presentation (Onsite)
Topics: NUTRITION & DIETS, GASTROENTEROLOGY
Keywords: scurvy, vitamin C, ascorbic acid, restrictive diet
Scurvy in a 5-year-old girl – a re-emerging diagnosis?
Azevedo, Aida Correia1; Rodrigues, Ana Sofia1; Feio, Ana1; Faria, João1; Andrade, Beatriz1; Lopes, Susana1; Carvalho, Sónia1; Rolim, Sara2; Sequeira, Alexandra1
1Pediatrics Department, Centro Hospitalar do Médio Ave, Vila Nova de Famalicão, Portugal; 2Pediatrics Department, Barcelos’ Hospital, Barcelos, Portugal.
Background: Scurvy results from vitamin C/ ascorbic acid deficiency and is characterized by fatigue, anaemia, arthralgias, behavioural changes, gingivitis and cutaneous signs such as petechiae and easy bruising. It is a potentially re-emerging diagnosis mainly due to restrictive eating habits (low fruit and vegetable intake).
Case Description: We present a case of a previously healthy 5-year-old girl who presented with perifollicular hyperkeratosis and petechiae in the lower limbs (Figure ), refusal to walk, pain and swelling of the right knee (Figure ) and gingivitis (Figure ) for 1 month. She was an introverted child with almost inexistent communication skills and had a neurodevelopment delay. A dietary history revealed consumption of a restricted diet comprising only chocolate milk at every meal for the past 2 years. Lower limbs x-Ray showed Trummerfeld zone, Frankel’s lines and enlarged metaphyseal margin (Figure ), consistent with scurvy. [1] Diagnosis of scurvy was confirmed by undetectable levels of vitamin C. Iron (49 μg/dL), and vitamin D (19 ng/mL) levels were also low. The child was admitted, and a multidisciplinary approach was initiated with vitamin C and D, iron supplementation, nutrition, psychology and social counselling. She was discharged after 11 days, having recovered remarkably (Figures ) and improved her eating habits, which she currently maintains. Follow-up consultation showed improvement in neurodevelopment delay and restoration of the deficits initially diagnosed.
Figure 4. Lower limbs X-ray showing Trummerfeld zone (arrow), Frankel’s lines (arrow head) and enlarged metaphyseal margin (star)
Conclusion: Scurvy, a disease once very prevalent mainly among sailors, currently persists only in a very restricted group (in developing countries, patients with mental and behavioural illnesses, elderly people living alone, restrictive diets, etc.). It is an easily preventable disease if one’s diet is varied and balanced. A patient’s complete history is crucial for a correct diagnostic approach. The increasingly high prevalence of poor eating habits is alarming; thus, health professionals must actively inquire about it at every opportunity.
ID: 211/04-OP-L-d2A: 5
Oral Presentation (Onsite)
Topics: EMERGENCY PEDIATRICS
Keywords: Diabetic Ketoacidosis, tachypnea, Type 1 diabetes
Beyond the crackles: T1D diagnosis in a ten-month-old infant
Alvelos, Rita Gomes e1; Alferes, Ana Paula1; Tavares, Catarina Faria2; Maurício, Kátia1; Ferrão, Tomás1; Duarte, Carolina1; Rios, Helena1
1Centro Hospitalar do Baixo Vouga, Portugal; 2Centro Hospitalar Tondela-Viseu, Portugal.
Background: In young infants, most pathologies may manifest with atypical symptoms. A variety of different systemic diseases may cause tachypnea. Type 1 Diabetes (T1D) is typically diagnosed around school age, though it may start earlier in life. Diabetic ketoacidosis (DKA) is a common primary manifestation of T1D, with younger children at higher risk, as usual symptoms may be absent or difficult to interpret, delaying the diagnosis.
Case Presentation Summary: A ten-month-old infant presents to the ER with fever, rhinorrhea, coughing, and difficulty breathing. At physical examination, tachypnea and tachycardia were noted, such as basilar crackles and wheezing on pulmonary auscultation, compatible with acute bronchiolitis, which improved after inhaled salbutamol. However, tachypnea sustained. The thoracic radiograph was unremarkable. The child’s overall condition deteriorated with grunting, lethargy, and dehydration signs, emphasizing their Kussmaul breathing. Capillary blood glucose and ketones were then measured and were 485 mg/dl and 7,4 mmol/L, respectively, diagnosing DKA. Appropriate therapy was initiated, and the child was transferred to the intensive care unit.
Learning Points Discussion: Though rarer in younger children, DKA may be a life-threatening primary manifestation of T1M. Concomitant acute disease may act not only as a confounding factor, contributing to a more severe state at diagnosis, but also promote more rapid clinical deterioration. It is important to maintain a high index of suspicion for this pathology in young children presenting to the ER with non-specific symptoms and respiratory manifestations that don’t improve after adequate usual therapy.
ID: 253/04-OP-L-d2A: 6
Oral Presentation (Onsite)
Topics: EMERGENCY PEDIATRICS
Keywords: pertussis, high flow nasal oxygen, respiratory distress
High flow nasal oxygen in management of pertussis in pediatrics
Abdelwahab Elmala, Moustafa Kotb
Nizwa hospital, Oman, Oman
Purpose: The aim of this study is to determine the clinical efficacy of high-flow nasal cannula (HFNC) therapy compared with conventional oxygen therapy in children presented with RD with a diagnosis of pertussis & pertussis like illness.
Background: Pertussis (or whooping cough) is a frequent and important infectious disease of the respiratory tract, mainly caused by the Gram-negative rod bacterium Bordetella pertussis. It is most serious in young infants. It is noted that there is an era of pertussis illness in newborn babies in our country, as the vaccine is only started at the age of 2 months. We noted the younger the age of the affected baby, the more clinical symptoms; most of the cases required admission either to the PICU or HD unit. (1) A high-flow nasal cannula (HFNC) is a relatively new non-invasive ventilation therapy that seems to be well tolerated in children. It is a relatively safe, well-tolerated, and feasible method for delivering oxygen to children, with few reported adverse events. Different mechanisms, including washout of nasopharyngeal dead space, increased pulmonary compliance, and some degree of distending airway pressure, may be responsible for the effect.
Methods: This hospital review was conducted in Nizwa city, Sultanate of Oman, from September 2020 to November 2021. Infants were recruited at Nizwa Hospital. Male and female infants were eligible for enrollment as index cases if they were aged ≤6 months, either with a persistent cough for at least 5 days associated with at least one symptom among respiratory distress, apnea, inspiratory “whooping”, or post tussive vomiting or with a persistent cough and a confirmed case of whooping cough in the entourage. Upon enrollment of index case, nasopharyngeal samples were collected, and data on age, sex, size and weight, birth information, pertussis vaccination history, type and duration of pertussis-related symptoms, biological test results, antibiotic treatment type and duration, previous consultation, family composition and the case of cough in the entourage, animal contact, were collected. All included cases were admitted either to the HD unit or PICU, all requiring oxygen support either to keep accepted saturation or to overcome apneic spells & increased work of breathing. For all, we started low-flow oxygen by nasal prong, which was upgraded to High flow oxygen by nasal cannula; we noted poor response in the first few hours after admission, and most of the cases developed severe RD with hypoactivity & poor feeding. After putting them on high flow nasal cannula, we noted excellent response within A Day; few cases needed CPAP or BiPAP (but later confirmed to have another comorbidity like CHD and/or cardiomyopathy). Follow-up on pertussis- related symptoms, weaning oxygen support, antibiotic treatment, hospitalization, and disease outcome was performed on days 2 and 7 after inclusion.
Results: The results were subsequently analyzed. Results A total of 166 respiratory distress children were enrolled during the study period. Only 11 children (6.62%) failed HFNC therapy, compared with 64 children (38.55%) in a conventional oxygen therapy group. After adjusting for body weight, underlying diseases, and respiratory distress score, there was an 85% reduction in the odds of treatment failure in the HFNC therapy group. Most children in the HFNC therapy group had significant improvement in clinical respiratory score, heart rate, and respiratory rate at 240, 360, and 120 min compared with conventional oxygen therapy.
Conclusion: HFNC therapy revealed a potential clinical advantage in the management of children hospitalized with pertussis & pertussis like illnesses admitted with respiratory distress compared with conventional respiratory therapy. The early use of HFNC in children with moderate-to-severe respiratory distress may prevent endotracheal tube intubation.
ID: 242/04-OP-L-d2A: 7
Oral Presentation (Onsite)
Topics: EMERGENCY PEDIATRICS
Keywords: High flow oxygen; acute bronchiolitis; Intensive Care
High flow oxygen for acute bronchiolitis – too much enthusiasm?
Martins, Beatriz1,2; Andrade, Beatriz1,2; Torres, Erica1,2,4; Albuquerque, Margarida1,2,4; Constant, Carolina2,3,4; Bandeira, Teresa2,3,4
1Serviço de Urgência, Departamento de Pediatria, HSM, Centro Hospitalar e Universitário Lisboa Norte; 2Serviço de Pediatria Médica, Departamento de Pediatria, HSM, Centro Hospitalar e Universitário Lisboa Norte; 3Unidade de Pneumologia Pediátrica, Serviço de Pediatria Médica, Departamento de Pediatria, HSM, Centro Hospitalar e Universitário Lisboa Norte; 4Clínica Universitária de Pediatria, Faculdade de Medicina, Universidade de Lisboa.
Background: High flow oxygen (HFO) can be an option for the support treatment of acute bronchiolitis (AB) outside Pediatric Intensive Care Units (PICU), although there isn’t enough evidence concerning its clinical and/or cost-benefit effectiveness. The aim of this study was to characterize HFO’s use, clinical characteristics, and PICU admission in patients with AB admitted to the Pediatric Emergency Department (PED) or Pediatric Pulmonology Unit (PPU) of a Tertiary Hospital in the pre and during COVID-19 pandemic era.
Methods: Patients with AB, aged less than 24 months, between October 2019 and March 2020 (First Period – standard RSV season) and between May 2021 and May 2022 (Second Period – unusual epidemiologic RSV season during COVID-19 confinement measures), admitted to the PED or PPU of a Tertiary Hospital were included. Clinical characterization of the patients submitted to HFO, risk factors (prematurity, low birth weight, chronic pulmonary disease, congenital heart disease), concomitant bacterial infection and PICU admission were assessed. Statistical analysis was carried out using chi-square and t-student tests.
Results: First Period: 107 cases of AB, median age 2 months (13 days - 20 months), 55% (n=59) male were identified. Eight patients underwent HFO (7%), 5 of which needed Intensive Care (63%). Fourteen other patients that weren’t submitted to HFO were transferred to the PICU (14%). Second Period: 138 cases of AB, median age 3 months (8 days – 23 months), 53% (n=73) male. Twenty patients underwent HFO (14%), 5 of which needed Intensive Care (25%). Ten other patients that weren’t submitted to HFO were transferred to the PICU (8%). No deaths in both periods. Despite the widespread use of HFO in the 2nd Period, the difference wasn’t statistically significant (p=0,08). Globally, the difference in PICU’s admissions between the two periods wasn’t statistically significant (18% 1st period and 11% the 2nd, p=0,12), nor was the difference regarding the admissions at PICU between the patients that underwent HFO and the patients who didn’t (p=0,06).
Conclusions: Despite the widespread use of HFO in the treatment of AB it wasn’t associated with a lower risk of PICU’s admission, in the present study. Without strong evidence supporting the effectiveness of its use, we must be more criterious and reassess its indications.
ID: 201/04-OP-L-d2A: 8
Oral Presentation (Onsite)
Topics: GENERAL PEDIATRICS, EMERGENCY PEDIATRICS
Keywords: maintenance fluid therapy; isotonic solutions; hyponatremia
Maintenance intravenous fluid therapy: the paediatricians choice
Lopes, Vilma; Pinho, Joana; Oliveira, Mariana; Rodrigues, Joana; Cunha, Otília; Rangel, Maria Adriana
Pediatric Department, Centro Hospitalar Vila Nova de Gaia/Espinho, Vila Nova de Gaia, Portugal.
Background: Historically, the gold standard for maintenance intravenous (IV) fluid therapy in children was hypotonic solutions. However, growing evidence in the last few years raises concerns about the risk of hyponatremia, especially in conditions associated with inappropriate antidiuretic hormone release (SIADH). Therefore, recent guidelines state that isotonic solutions are preferred as the first choice.
Aim: This study aims to evaluate which fluid is the first choice in different clinical paediatric scenarios, as well as assess when volume restriction is used concerning the risk for SIADH.
Methods: An anonymous survey was emailed to the medical staff of the paediatric department of a level II hospital. A demographic questionnaire was initially applied, including training information, followed by a series of questions eliciting IV fluid choice and volume in five clinical scenarios (pneumonia, gastroenteritis, meningitis, immediate postoperative and pyelonephritis) in various ages (1 month, 8 months, 4, 6 and 12 years old). Data were analysed using the program SPSS.
Results: A sample of 32 questionnaires was obtained (representing 48% of the paediatricians). Most participants (75%) were in the 25–35 age group, 15,6% were 35–45 years old, 6,3% and 3,1% were 46–55 and 56–65 years old, respectively. About 56% were paediatric residents, and 44% were specialists. All were currently working in the emergency department. Isotonic fluids were selected by the majority of participants (>50%) in four of the five clinical cases. More variability in responses was observed in the scenario involving 1-month-old infant, with 56.3% of participants choosing the hypotonic solution and only 37.5% the isotonic one. About 97% selected fluid volume restriction in the pneumonia scenario, 71.9% in the meningitis scenario and only 12.6% in the postoperative case. There were no significant differences in the fluid choice between residents and specialists, and there was no association between specialists’ seniority and fluid tonicity choice.
Conclusions: In our department, the majority of paediatricians choose isotonic fluids for maintenance fluid therapy in the presented scenarios. The exception was the one month infant case, probably due to the lack of guidelines and clinical consensus in this age group. The fact that most participants selected volume restriction in cases with increased risk of SIADH, with the exception of the postoperative scenario, should alert and remind us of this possible cause for this syndrome. Most of our sample was younger than 35 years old and worked in the emergency department, which can translate to a more up-to-date practice.
ID: 206/04-OP-L-d2A: 9
Oral Presentation (Onsite)
Topics: ENDOCRINOLOGY, EMERGENCY PEDIATRICS
Keywords: diabetes mellitus, ketoacidosis, new-onset, childhood, review
New-onset type 1 Diabetes Mellitus and ketoacidosis in childhood: 14-year review
Mazeda, Inês1; Vivas, Inês1; Branco, Sofia1; Oliveira, João Nogueira2; Cunha, Inês Pais3; Coelho, Elisabete1
1Department of Pediatrics, Centro Hospitalar Da Póvoa De Varzim/Vila Do Conde, Porto - Portugal; 2Department of Pediatrics, Centro Materno Infantil Do Norte, Porto - Portugal; 3Department of Pediatrics, Centro Hospitalar Universitário de São João, Porto - Portugal.
Background: Type 1 diabetes mellitus (T1DM) is one of childhood’s most common chronic endocrine diseases. A steady increase in the incidence of T1DM has been reported worldwide. Children usually present with the classic signs and symptoms resulting from hyperglycemia. Diabetic ketoacidosis (DKA) is the major life-threatening type 1 diabetes complication responsible for elevated morbimortality. The frequencies of DKA at the onset of diabetes range from approximately 15% to 70%. The aim is to describe the clinical presentation and laboratory features of children with newly diagnosed type 1 diabetes mellitus in a secondary care center.
Methods: Retrospective study of hospital records of children with newly diagnosed type 1 diabetes mellitus during the period of 2008–2022 in the Paediatric department of Centro Hospitalar da Póvoa de Varzim/Vila do Conde. The analysis of social, analytic and clinical parameters was performed using SPSS software.
Results: There were 72 children with newly diagnosed type 1 diabetes mellitus (41 boys and 31 girls) with an average age of 9,3 years. The majority of patients were in the age range of 10–14 years. The distribution of cases over the years revealed an increase in the number since 2008, with a peak in 2012 and 2021. There was a predominance of cases during winter-autumn seasons (43% in winter and 24% in autumn). (1) Family background of diabetes was positive in 36% of cases (T1DM 26,9%; T2DM 69,2%; T1 and T2DM 3,8%). When the family history of DM was correlated with the time between the onset of symptoms and diagnosis, no significant statistical differences were observed (p = 0.137). However, the average days between the onset of symptoms and diagnosis was lower in cases with a positive family history of DM (22,4 vs 32). (2) The average duration of presenting symptoms before the hospital encounter was 28 days. Polydipsia, polyuria and weight loss were the most common symptoms. (3) Nineteen cases (26,4%) presented with diabetic ketoacidosis, with a higher percentage of moderate ketoacidosis. The average number of days of hospitalisation of cases with DKA was higher (5,3 vs 4). The distribution of cases over the years was stable (1–3/year), with a peak in 2021 with 6 cases. (4) Anti-GAD antibodies or other positive antibodies were detected in 63,9%.
Conclusions: The commonly recognised symptoms of diabetes were present in most of the children at the time of diagnosis, but the average duration of presenting symptoms before diagnosis was long, and the frequency of diabetic ketoacidosis was high. These findings call for a collaborative effort for the early recognition of symptoms by patients and physicians.
ID: 259/04-OP-L-d2A: 10
Oral Presentation (Onsite)
Topics: ENDOCRINOLOGY
Keywords: type 1 DM, education, HbA1c, glycemic contro
The role of diabetic education in glycemic control in children with type 1 DM
Abdelwahab Elmala, Moustafa Kotb
Nizwa hospital, Oman, Oman.
Background & Purpose: The perfect control of Type I DM in children could depend on other factors rather than insulin, like Diabetic Education. We aim to study the importance of Diabetic Education in glycemic control in children with T1DM.
Methods: This review was recruited at Nizwa Hospital, Sultanate of Oman, from September 2020 to November 2021. The Diabetic Education service started on February 2021 with direct meeting education every 2–3 weeks plus daily availability through WhatsApp. A total of 48 patients were included, 28 females and 20 males, with ages ranging from 8 to 13 years. Families of all children have almost the same social & educational levels. Comparison has been made with them before & after establishing the diabetic education service (5 months before and 10 months after) based on: glucose level, HbA1c levels, emergency phenomena & compliance to insulin use every 3 months at OPD.
Results: Good glycemic control was noted in children who adhered to the Diabetic Education service. The adhered number was 36 patients (75%). The remaining 12 patients (25%) who neglected the Education follow-up had very bad glycemic control & 4 of them developed moderate DKA. Before starting the Education service, good control was noted only in 22 patients (45%) of the total number of recruited children.
Conclusions: Diabetic Education in children has a great role in good glycemic control, which is easy to apply in each medical institute as well as in the community.
ID: 233/04-OP-L-d2A: 11
Oral Presentation (Onsite)
Topics: ENDOCRINOLOGY
Keywords: Hashimoto’s thyroiditis, thyroid function, thyroid autoantibodies
Hashimoto’s thyroiditis in pediatric age – A retrospective study
Branco, Sofia Varela1; Mazeda, Inês1; Oliveira, João Nogueira2; Cunha, Inês Pais3; Vivas, Inês1; Mendes, Isabel1; Oliveira, Gracinda Nogueira1
1Department of Pediatrics, Centro Hospitalar Póvoa de Varzim e Vila do Conde - Portugal; 2Department of Pediatrics, Centro Materno Infantil do Norte - Portugal; 3Department of Pediatrics, Centro Hospitalar Universitário de São João - Portugal.
Background: Hashimoto’s thyroiditis (HT) is the most common form of thyroiditis in pediatric age, with a prevalence in childhood of around 3% and its peak during adolescence. At HT presentation, children are frequently asymptomatic, and the thyroid function may range from euthyroidism to hypothyroidism or, more rarely, hyperthyroidism, depending on the severity of the immunologic damage.
Methods: We retrospectively analysed the clinical records of children and adolescents referred to the pediatric endocrinology clinic of a level 2 hospital with HT between 2017 and 2021. Statistical analysis was performed using IBM SSPS Statistical Software version 27.
Results: A total of 39 children and adolescents (84.6% girls) were included, with a mean age at diagnosis of 13 years. A positive family history of thyroid disease in first-degree relatives was present in 28,2% of cases. The referral to the endocrinology clinic came from primary care in 84,6%, pediatric outpatient clinic in 10,3% and pediatric emergency department in 5,1%. The main reasons for referral were goiter (17 cases), hypothyroidism symptoms (14 cases, being weight gain and fatigue the most common) and findings on thyroid function testing (8 cases). At the time of HT diagnosis, the thyroid function pattern was hypothyroidism in 69,2% of the patients, euthyroidism in 23,1% and subclinical hypothyroidism in 7,7%. The physical examination at diagnosis yielded goiter in 51% of our study population. The thyroid ultrasound detected diffuse heterogenicity in 92,3% of the patients, enlarged thyroid in 66,7% and pseudonodularities and/or hypoechoic micronodules in 61,5%. The presence of both anti-thyroid peroxidase (TPO) and anti- thyroglobulin (Tg) antibodies was found in 72%, and isolated anti-TPO and anti-Tg were found in 15% and 13%, respectively. The most frequent comorbidity was obesity (7 cases). There were 3 cases of alopecia areata, and in 1 case, an association between HT and chronic urticaria was found. Replacement therapy with levothyroxine was performed in 71,8% (all the cases with overt hypothyroidism and one with subclinical hypothyroidism), with thyroid-stimulating hormone (TSH) normalisation in all of them. The median follow-up time was 2,5 years. In our study, no cases of overt/subclinical hyperthyroidism at HT diagnosis were identified, but during the follow-up, we detected 1 case of hyperthyroidism associated with Graves’ disease diagnosis.
Conclusions: In our centre, overt hypothyroidism was the main presentation pattern of HT, and prompt treatment was paramount in preventing complications. In children with euthyroidism or subclinical hypothyroidism, periodic monitoring of thyroid function is recommended due to the risk of deterioration of their thyroid status over time.
ID: 271/04-OP-L-d2A: 12
Oral Presentation (Onsite)
Topics: DERMATOLOGY
Keywords: Ichthyoses, Non-syndromic, Genetic study
Congenital ichthyoses: 2 case reports
Branco, Sofia Varela1; Vivas, Inês1; Vieira, Beatriz1; Cunha, Inês Pais2; Santos, Ana Luísa1; Oliveira, Catarina1; Coelho, Elisabete1
1Department of Pediatrics, Centro Hospitalar Póvoa de Varzim e Vila do Conde - Porto, Portugal; 2Department of Pediatrics, Centro Hospitalar Universitário de São João - Porto, Portugal.
Background: Ichthyoses are a heterogeneous group of skin disorders characterised by dry skin, scaling, hyperkeratosis and frequently associated with erythroderma. They are mainly divided into non-syndromic and syndromic ichthyoses. Among the non- syndromic types, ichthyosis vulgaris and X-linked recessive ichthyosis are the most common, being autosomal recessive congenital ichthyoses, keratinopathic ichthyoses and a few other much rarer.
Case Presentation Summary: Case 1: A full-term male neonate born with an Apgar score of 9–10-10 and birth weight of 3525 g through vaginal delivery. Pregnancy was uneventful, and there was no history of drug intake by the mother during the gestation. Physical examination at birth revealed a diffuse shiny membrane of the skin with erythematous areas and fine white scales. There was also ectropion of both upper eyelids with gross tarsal swelling and lip edema. Further physical examination did not reveal other abnormalities. The newborn was transferred to the neonatal intensive care unit and started parenteral nutrition on the first day of life. He did not require any respiratory support during hospitalisation and presented stable vital parameters. All blood parameters, including septic screenings, were normal. The sequence of the ALOX12B gene identified the heterozygous variants c.T1294C>T and ca. 1405C>T. Based on the clinical and genetic findings, the patient was diagnosed with congenital ichthyosiform erythroderma (CIE). Parental consanguinity or similar illness in the family was denied. (Figure ) Case 2: A full-term male born at 38 weeks of gestation by normal spontaneous vaginal delivery, weighing 3330 g and Apgar score of 9- 9-10. Pregnancy was uneventful, and there was no history of drug intake by the mother during the gestation. Physical examination at birth revealed swelling of the extremities associated with scaly plaques and pronounced erythematous fissures on areas with skin folds. The septic screenings were negative during hospitalisation, and the newborn presented normal vital parameters. The clinical history evidenced that the father had a congenital skin disorder characterised by bullae of the hands and feet during the neonatal period and childhood. Due to these clinical features, a referral to dermatology was made. A skin biopsy and a genetic study with the sequence of the KRT1,2 and 10 genes were performed because of suspected keratinopathic ichthyosis. At the 1-month follow-up, the infant had xerosis and mild peeling of the hands, feet and back (Figure ).
Figure 5. Resolution of the edema of the right knee and perifollicular hyperkertotosis and petechiae in the lower limbs.

Discussion: These two rare forms of non-syndromic ichthyoses highlight the importance of the genetic study on the correct diagnosis, given the large spectrum of mutations in individuals with the same phenotype and clinical characteristics.
Session
05-OP-L-d2B: Oral Presentations Session 5 - Day 2 - Zone B
Presentations
ID: 139/05-OP-L-d2B: 1
Oral Presentation (Onsite)
Topics: RARE DISEASES
Keywords: Glycogen storage disease type Ib, neutropenia, inflammatory bowel disease, SGLT2
Favorable outcome of empagliflozin treatment in two pediatric glycogen storage disease type 1b patients
Spiegel, Ronen1,2; Hexner-Erlichman, Zufit1; Veiga-da-Cunha, Maria3; Zehavi, Yoav1,2; Vadas, Zehava4; Tatur, Sameh1; Sabag, Adi4
1Emek Medical Center, Afula, Israel; 2Ruth and Bruce Rappaport Faculty of Medicine, Technion, Haifa, Israel; 3de Duve Institute, Universite´ Catholique de Louvain, Brussels, Belgium; 4The Proteomic and Clinical Flow Cytometry Unit, Bnai-Zion Medical Center, Haifa, Israel.
Background: Glycogen storage disease type 1b (GSD1b) is an ultra-rare autosomal recessive disorder caused by mutations in the SLC37A4 gene encoding glucose 6 phosphate transporter (G6PT) affecting multiple organs. G6PT is responsible for glucose 6 phosphate influx into the endoplasmic reticulum. Its deficiency results in fasting hypoglycemia with crises of lactic acidosis, hepatomegaly, growth retardation, hyperlipidemia and renal impairment. In addition, patients present neutropenia, neutrophil dysfunction, oral, urogenital and skin infections and a significant predisposition to develop inflammatory bowel disease (IBD). The cause for low neutrophil counts and function is directly related to the toxic effect of cellular accumulation of 1,5-anhydroglucitol (1,5AG) phosphate in neutrophils. Recently, several reports showed that off-label treatment with empagliflozin, an antidiabetic, SGLT2 inhibitor, decreased serum levels of 1,5AG, consequently reducing neutrophil 1,5AG phosphate levels, thus constituting a new therapeutic option for neutropenia and neutrophil dysfunction in patients.
Methods: Off-label treatment with empagliflozin was instituted in two patients after appropriate signed informed consent. The patients were followed clinically. We monitored neutrophil counts and function, plasma 1,5AG levels and renal clearance before and after empagliflozin treatment.
Results: Two GSD1b pediatric patients were studied. A 17 years female patient developed Crohn’s like disease necessitating systemic steroid therapy and regular G-CSF therapy, and an 8 years male patient who had steady non-healing oral lesions and soars. Off-label empagliflozin (0.5 mg/Kg/day) treatment in both patients for 18 and 24 months, respectively, resulted in significant improvement of neutrophil function and counted leading to substantial clinical improvement in both, including remission of IBD in the first patient allowing discontinuation of G-CSF and steroid therapy. Both patients had no hypoglycemic episodes and no additional adverse events. 1,5AG serum levels greatly decreased within two weeks of treatment and remained stable thereafter. [1] In one of our patients, urinary excretion of glucose and 1,5AG under treatment indicated that EMPA caused an impressive increase in glucose and 1,5AG urinary clearance.
Conclusions: Repurposing the glucose-lowering SGLT2 inhibitor empagliflozin, was safe and has led to significant clinical and laboratory improvement. Future studies involving more patients are needed to demonstrate longer-time safety and efficacy.
ID: 234/05-OP-L-d2B: 2
Oral Presentation (Onsite)
Topics: RARE DISEASES, DERMATOLOGY
Keywords: Paediatric Dentistry, Oral Health, Papillon Lefèvre
Papillon Lefèvre Syndrome- the oral manifestations and implications for paediatric patients with this rare genetic condition.
Barrow, Sarah
Leeds Dental Institute, The Leeds Teaching Hospitals NHS Trust, UK.
Background: Papillon Lefèvre Syndrome (PLS) is a rare autosomal recessive inherited condition of keratinisation caused by mutations in the cathepsin C (CTSC) gene. The incidence of PLS is difficult to determine due to its rarity, with some citing one to four per million within the literature. There is no racial or male/female predilection. The severity of this rare syndrome may be related to immunological and microbiologic factors. PLS is characterised by dry, scaly skin lesions (hyperkeratosis), with the palms of the hands and soles of the feet the most commonly affected sites, and the early presentation of severe periodontitis. Other less common manifestations, such as pyogenic skin infections, hyperhidrosis, intracranial calcification and nail dystrophies, have also been reported. Urinary analysis confirms the diagnosis. Treatment often requires a multi-disciplinary approach with both medical and dental specialties essential for improved patient outcomes.
Objective: To provide an overview of the oral manifestations and implications of Papillon Lefèvre in the paediatric population.
Methods: This is a review of the current literature.
Learning Points and Discussion: In most cases, the diagnosis of PLS may not be confirmed until oral manifestations of this condition become apparent. Dentists, therefore, play an integral role in identifying such cases, leading to prompt referral, treatment, and improved patient outcomes. Young patients, typically between the ages of three-five-years old, may present with significant gingival erythema and bleeding, primary tooth mobility and early exfoliation of these teeth. This is due to the destruction of the periodontium, a complex structure surrounding and supporting the teeth. Other less common oral manifestations, including microdontia, root resorption and incomplete root formation, have also been reported. Permanent teeth, in most cases, follow the same sequelae as primary teeth, with the permanent dentition lost in adolescence or early adulthood. To delay the progression of periodontal destruction and eventual loss of teeth, early specialist input is required. Dental treatment such as sub-gingival instrumentation is performed, which aims to reduce the bacterial microflora conducive to disease. Local and systemic antibiotics may be considered in some cases. Treatment with vitamin A derivative (retinoids) has also been helpful in treating some individuals with PLS. On eventual and inevitable loss of the permanent dentition, prosthetic replacement is required. Both dental and medical professionals should be aware of the oral and dermatological manifestations of PLS as early diagnosis and prompt treatment may improve prognosis and, ultimately, a patient’s quality of life.
ID: 189/05-OP-L-d2B: 3
Oral Presentation (Onsite)
Topics: GENERAL PEDIATRICS
Keywords: Nutcracker syndrome; hematuria; ecodoppler
Nutcracker syndrome - a diagnosis to keep in mind
Pais-Cunha, Inês1; Vivas, Inês2; Oliveira, João3; Mazeda, Inês2; Branco, Sofia2; Santos, Ana Luísa2; Madalena, Célia2
1Serviço de Pediatria, Centro Hospitalar Universitário São João, Portugal; 2Serviço de Pediatria, Centro Hospitalar Póvoa de Varzim Vila do Conde, Portugal; 3Serviço de Pediatria, Centro Materno-Infantil do Norte, Portugal.
Introduction: The nutcracker syndrome (NS) is caused by left renal vein (LRV) compression between the superior mesenteric artery (SMA) and the aorta. When significant compression occurs, it can lead to hematuria, orthostatic proteinuria and abdominal or back pain. Nevertheless, in children and adolescents, this condition is frequently asymptomatic. The prevalence and natural history of this disease are still poorly known. Our study aims to describe clinical manifestations, diagnostic approach and evolution of pediatric patients diagnosed with this syndrome.
Methods: Retrospective and descriptive analysis of patients with nutcracker syndrome followed in our hospital’s pediatric nephrology clinic between 2009 and 2022.
Results: A total of 5 patients were identified, 4 of the male gender, with a median age of 9 years (5–16); regarding clinical presentation: 3 patients presented with isolated macroscopic hematuria; one with macroscopic hematuria and back pain and one with isolated microscopic hematuria. Three patients had symptoms related to exercise. The complementary study detected proteinuria in 3 patients upon urine analysis. All patients had negative blood count, kidney function, and infectious and inflammatory parameters. In all patients, the diagnosis of NS was confirmed by doppler ultrasonography. A conservative approach was established in all patients. All patients were kept on active surveillance with a median follow-up period of 5 years (2–10). Two patients had subsequent hematuria episodes during exercise. At discharge time, all patients were asymptomatic and had a normal urine analysis.
Conclusion: Given its unspecific signs and symptoms, diagnosis of NS is challenging and requires a high index of suspicion. Recognizing this entity is important to prevent unnecessary investigation. Although the majority of patients are treated conservatively, some cases may require surgery. Universal diagnosis and treatment guidelines should be implemented in order to identify these patients in time and prevent complications.
ID: 228/05-OP-L-d2B: 4
Oral Presentation (Onsite)
Topics: GENERAL PEDIATRICS
Keywords: Greece, preventive care, student’s health, catch-up vaccinations
Preventive health care policy for students in Greece
Gkountoula, Theodora; Zacharioudaki, Maria; Marinopoulou, Eirini; Giannousi, Elisavet
General Hospital of Rethymno, Greece.
Background: In Greece, a Student’s Personal Health Card (SPHD) is required for enrollment in each education grade. The card is provided by a pediatrician during a health supervision visit at the ages of 4, 6, 9, 12 and 15 years and is valid for 3 years. SPHD is based on clinical examination and the child’s medical and family history, assessed through a thorough questionnaire filled out by the caregiver. The purpose of this study was to evaluate the benefits of SPHD in promoting children’s health and to highlight ways for future improvement.
Methods: A retrospective cohort study was performed, including all children that visited the outpatient pediatric department of a secondary general hospital over a period of 4 years, from September 2018 to August 2022 and an SPHD was administered. The SPHDs were reviewed, and only data that could be standardized, such as age, sex, ethnicity, Body Mass Index (BMI), immunization status and referrals, were analyzed.
Results: In total, 455 SPHDs were evaluated (237 for boys and 218 for girls). Of them, 296 (65%) were locals, and 159 (35%) were immigrants. According to Greek National Immunization Programme, the vaccination coverage was age-appropriate in 381/455 children (83,7%), and 76 received age-appropriate vaccines mainly at 12 years. Vaccination was inadequate in 74/455 children (16,3%), and 71 got catch-up vaccinations. The most missed vaccine was the 2nd dose of varicella at the age of 4, followed by one or both doses of hepatitis A in all age groups and missed adolescent vaccines that were administered at the 15-year visit. Moreover, BMI was not normal in 140/455 (30.8%) of children, 53/455 (11.6%) being obese, and 87/455 (19.12%) being overweight. Regarding referrals, 11,6% were to ophthalmologists due to reduced visual acuity, 11% to cardiologists, mainly children over 12 years for the first cardiologic evaluation, 8,1% to dentists due to dental decay and 5% to orthopaedics due to scoliosis.
Conclusions: The obligation of schools to collect SPHDs for all students ensures that all children participating in education have continuity in preventive care from preschool through adolescence. Catch-up vaccinations, screening for visual acuity and referral for preventive cardiologic evaluation were found to be the most important benefits. More must be done towards obesity, mental health and behavioural problems that were not systematically recorded, and referrals were rare. Standardized screening tools for these disorders should be implemented to improve the efficacy of SPHD in promoting children’s health and well-being.
ID: 163/05-OP-L-d2B: 5
Oral Presentation (Onsite)
Topics: RHEUMATOLOGY
Keywords: IgA vasculitis, nephritis, necrosis, bullae, ulcerations
Systematic analysis of the impact of severe skin changes in IgA vasculitis on the clinical course of the disease in a large international cohort
Sestan, Mario1; Kifer, Nastasia1; Sozeri, Betul2; Demir, Ferhat2; Ulu, Kadir2; Silva, Clovis A.3; Campos, Reinan T.3; Batu, Ezgi Deniz4; Koker, Oya5; Sapina, Matej6; Srsen, Sasa7; Held, Martina1; Gagro, Alenka8; Rodrigues Fonseca, Adriana9; Rodrigues, Marta9; Rigante, Donato10; Filocamo, Giovanni11; Baldo, Francesco11; Heshin-Bekenstein, Merav12; Giani, Teresa13; Kataja, Janne14; Frkovic, Marijan1; Ozen, Seza4; Jelusic, Marija1
1University of Zagreb School of Medicine, University Hospital Centre Zagreb, Zagreb, Croatia; 2University of Health Sciences, Umraniye Training and Research Hospital, Istanbul, Turkey; 3Pediatric Rheumatology Unit, ICr-HC-FMUSP, Faculdade de Medicina da Universidade de São Paulo, São Paulo, Brazil; 4Department of Pediatrics, Hacettepe University, Ankara, Turkey; 5Department of Pediatric Rheumatology, Marmara University-Pendik Training and Research Hospital, Istanbul, Turkey; 6Department of Paediatrics, Josip Juraj Strossmayer University of Osijek, Medical Faculty and Faculty of Dental Medicine and Health Osijek, University Hospital Centre Osijek, Osijek, Croatia; 7Department of Paediatrics, University of Split School of Medicine, University Hospital Centre Split, Split, Croatia; 8Department of Paediatrics, Children’s Hospital Zagreb, University of Zagreb School of Medicine Zagreb, Croatia; Josip Juraj Strossmayer University of Osijek, Medical Faculty Osijek, Osijek, Croatia; 9Universidade Federal do Rio de Janeiro, Instituto de Puericultura e Pediatria Martagão Gesteira, Rio de Janeiro, Brazil; 10Department of Life Sciences and Public Health, Fondazione Policlinico Universitario A. Gemelli IRCCS, Rome, Italy; Università Cattolica Sacro Cuore, Rome, Italy; 11Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico, Milan, Italy; 12Pediatric Rheumatology Service, Dana Dwek Children’s Hospital, Tel Aviv Medical Center, Tel Aviv University, Tel Aviv, Israel; 13AOU Meyer, Florence, Italy; 14Department of Paediatrics and Adolescents Medicine, Turku University Hospital, Turku, Finland.
Introduction: Although skin changes in IgA vasculitis (IgAV) are most commonly typical, only 2% of children may present severe changes, including hemorrhagic vesicles, bullae, ulcerations and/or necroses.
Objectives: We investigated whether such changes were also associated with a more severe clinical course of the disease and the need for more intensive therapy.
Methods: The retrospective multinational study was conducted in 14 tertiary university medical centers. Patients were diagnosed according to the EULAR/PRES/PRINTO criteria. Data were analyzed descriptively and using the Fisher’s exact and χ2 test.
Results: A total of 64 patients with the most severe cutaneous manifestations in IgAV were included in the study, of which 41 (64.1%) were male, with a mean (standard deviation, SD) age of 8.49 (4.06) years at the disease onset. They were older than the control group of 596 IgAV patients who did not develop bullae or necrosis, with a mean (SD) age of 7.17 (3.57) years. The median (25–75p) time from the onset of the first symptom to the first bullous/necrotic change was 5 (2–10.5) days. The total duration of bullous/necrotic changes was 10 (7–16) days. The most important triggers of IgAV were infections, which were present in 68.8% of patients. The distribution of bullae and necroses followed the distribution of the purpuric changes. Scars and pigmentation changes persisted in 48.5% of children. The patients with severe cutaneous manifestations developed nephritis more frequently (40.6% vs 20.6%, p = 0.001), particularly with a combination of hematuria and proteinuria. The renal disease outcome was worse than the control group (p = 0.001). They were more likely to have an affected gastrointestinal system (64.1% vs 45.5%, p = 0.007) and to develop the most severe gastrointestinal manifestations (p < 0.001). The majority of these patients (90.6%) were treated: 84.4% of them received systemic glucocorticoids with a median (25–75p) cumulative dose of methylprednisolone 12 (6–88.7) mg/kg for a median (25–75p) of 12.5 (4–30) days, while 57.8% were treated with nonsteroidal anti-inflammatory drugs for 7 (3.5–18.5) days. Other drugs were administered sporadically. They were significantly more frequently treated with systemic glucocorticoids (84.4% vs 37.2%, p < 0.001).
Conclusion: This is the largest international cohort study showing that IgAV patients with severe cutaneous manifestations developed nephritis with worse renal outcome more frequently compared to the controls, requiring systemic glucocorticoids. These patients also presented severe gastrointestinal involvement.
Funding
Croatian Science Foundation, IP-2019-04-8822.
ID: 261/05-OP-L-d2B: 6
Oral Presentation (Onsite)
Topics: PUBLIC HEALTH, EMERGENCY PEDIATRICS
Keywords: Child poverty, social determinants of health, family wellbeing
The family wellbeing project: combating health inequalities in a UK paediatric emergency department
Cowling, Isabel; Rehman, Shazia; Dutton, Fran; Bird, Christopher; Wright, Katie
Birmingham Women’s and Children’s NHS Foundation Trust, UK.
Background: Child poverty is a significant public health challenge, affecting the health and welfare of children and young people worldwide. In the UK, there are currently over four million children living in poverty, which constitutes around 30% of the population (1). Child poverty is associated with a wide range of adverse physical and psychological outcomes, in addition to poor long-term social and educational opportunities (2). It is, therefore, a key, modifiable determinant of child health. The Emergency Department at Birmingham Children’s Hospital has 65,000 annual attendances and serves one of the most deprived areas in the UK. The family well- being project was created to identify and combat health inequalities for children and families within our local population.
Methods: A screening tool was developed containing three questions relating to food, housing and safety concerns. Questionnaires were distributed to families in the waiting room by departmental interpreters over a six-week period between 17:00, 21:00 from Monday to Friday. Families answering yes to any question were signposted to family well-being resources and offered an Early Help referral (community family support services). This study was deemed a departmental audit of a quality improvement project.
Results: 110 questionnaires were completed from August to September 2022. 76% of families (n = 84) responded yes to one or more screening questions. 61% of families (n = 67) had concerns relating to food insecurity, 46% (n = 50) had housing problems and 8% (n = 9) had safety concerns. 84 families were contacted by Early Help coordinators and signposted to well-being resources. This resulted in the completion of 42 family connect forms (referrals) for further assessment of needs and access to community support services. Common themes identified included: financial difficulties, benefits advice, temporary accommodation, overcrowded and unsafe living conditions, and parenting support.
Conclusions: Clinicians play an important role in identifying and addressing the impacts of child poverty in clinical practice. The pilot demonstrated the importance of routine enquiry on issues with finance, housing and safety in our population, enabling timely referral to Early Help for family support. New integrated care boards should explore this model to address the social determinants of child health.
ID: 207/05-OP-L-d2B: 7
Oral Presentation (Onsite)
Topics: GENERAL PEDIATRICS, NEONATOLOGY
Keywords: kidney, newborn, malformation, CAKUT, diagnosis
Congenital anomalies of the kidney and urinary tract (CAKUT) - Diagnosis and follow-up
Mazeda, Inês1; Branco, Sofia1; Oliveira, João Nogueira2; Cunha, Inês Pais3; Reis, Armando4; de Castro, Ribeiro4; Santos, Ana Luísa1; Madalena, Célia1
1Department of Pediatrics, Centro Hospitalar Da Póvoa De Varzim/Vila Do Conde, Porto - Portugal; 2Department of Pediatrics, Centro Materno Infantil Do Norte, Porto - Portugal; 3Department of Pediatrics, Centro Hospitalar Universitário de São João, Porto - Portugal; 4Department of Urology, Centro Materno Infantil Do Norte, Porto - Portugal.
Background: Congenital anomalies of the kidney and urinary tract (CAKUT) constitute 20 to 30% of all malformations identified in the prenatal period, with the overall rate of 0,3 to 1,6 per 1000 newborns. CAKUT are the most common cause of chronic kidney disease and end-stage renal disease in the pediatric population. The goal of prenatal screening is to identify pathologic conditions that would require postnatal therapy in order to prevent or delay these complications.
Aim: This study aims to describe a population of newborns with a prenatal diagnosis of CAKUT and their clinical and imagiologic outcomes.
Methods: Retrospective study of medical reports of infants born at Centro Hospitalar da Póvoa de Varzim/Vila do Conde, Portugal, from 2017 to 2021. Hydronephrosis was defined as anteroposterior diameter of the renal pelvis (APD) ≥ 5 mm and has been classified as mild (5–9 mm), moderate (≥10–14 mm) or severe (≥15 mm). Parenquyma and kidney structure, dilatation of calices or ureters, and bladder morphology were also considered.
Results: There were 231 newborns with a prenatal diagnosis of CAKUT, of which 66,2% were male. Hydronephrosis was diagnosed by prenatal ultrasound in 95,7% (39,4% bilateral), in a total of 298 kidneys (73,5% with mild, 17,1% with moderate and 3,7% with severe hydronephrosis). In 37%, there was no postnatal ultrasound hydronephrosis confirmation. The postnatal diagnosis included: transient hydronephrosis (38,5%), ureteropelvic junction (8,2%), vesicoureteral reflux (3%), megaureter (2,2%), renal agenesis (1,3%), multicystic dysplastic kidney (1,3%) and renal fusion (0,4%). Surgery was performed in 3% of patients. Acute pyelonephritis episodes were observed in 9,9% of the patients.
Conclusions: Correct identification and adequate follow-up of at-risk patients is a challenge. Although most of the hydronephrosis detected in the prenatal period do not correspond to significant nephro-urological pathology, early ultrasound diagnosis is important in detecting severe malformations and preventing complications.
ID: 286/05-OP-L-d2B: 8
Oral Presentation (Onsite)
Topics: ADOLESCENT MEDICINE, COVID-19
Keywords: Pandemic Impact, Adolescent mental well-being, HBSC
The ongoing impact of the pandemic period on the mental and behavioral well-being of adolescents in Israel
Harel-Fisch, Yossi
Faculty of Education, Bar Ilan University, Israel.
Background: The COVID-19 pandemic broke out in Israel in March 2020. Like in most infected countries, the government imposed restrictions that included shutdowns of schools, businesses and community activities, home curfews, social distancing and more. With one wave following the other, the 2-year ongoing pandemic period significantly impacts the lives and well-being of children and youth. Evidence from sales and police data indicated a significant increase in the purchase of alcohol and online drugs, suggesting an increase in psychoactive substance use in the population.
Method: The latest national school-survey data were from the May-July 2019 HBSC study that was carried out several months before the pandemic outbreak. To investigate the impact of the pandemic on the mental and behavioural well-being of youth, we implemented a follow-up national representative survey in May-July 2021, one and a half years into the pandemic period. Data gathering was challenging due to unstable school functioning, and in some cases, zoom-based online administration to sampled classrooms was used. Data from 2021 were compared to the HBSC data from 2019 to assess the impact of the pandemic.
Results: Finding show (a) a significant decrease in positive life satisfaction (from 41% to 28%), (b) a significant increase in mental distress (from 25% to 40%), (c) a significant decrease in binge drinking (from 14% to 6%) and (d) a significant decrease in drug use (e.g., Cannabis from 11% to 8%).
Conclusion: While the effect of the pandemic on mental well-being was expected, the decline in substance use was indicative that the increase in alcohol and drug purchases reflected increased use by adults, not youth. Alcohol and drug use by adolescents is mainly motivated by and in context with peer socializing and nightlife patterns. Since all community and entertainment facilities were shut down, youth were not exposed to recreational and social activities that are associated with alcohol and drug use. Currently, our big concern is that post-pandemic might bring a renewed engagement of youth in alcohol and drug-related recreational social activities, a change that might result in significant increases in substance use.
ID: 135/05-OP-L-d2B: 9
Oral Presentation (Onsite)
Topics: GENERAL PEDIATRICS, PUBLIC HEALTH
Keywords: children, sepsis, novel, improvement tool, Vocera team sepsis
Vocera Team Sepsis: strong improvement tool in acute sepsis management in children; 2022 updates
Ashour, Rasha Ahmed1,2,3; Kiat-Floro, Joy1; Zaghmout, Lin1; Paggao, Bok1; Akram, Azmi1; Al-khori, Fatima1; Sharma, Sachin1; Janahi, Mohammad1; Al Hammadi, Ahmed1
1Sidra medicine, Qatar; 2Weill Cornell Medical College - Qatar; 3College of Medicine Qatar University
Background: Sepsis is a life-threatening condition that complicates severe infection. Not recognized and treated early can lead to multi-organ failure, shock, and death. [1] Since 2018, Sidra Medicine has shared the Qatar National Goal to reduce mortality due to sepsis and septic shock through increased healthcare provider compliance to the sepsis six bundle of care. Sepsis management has remained a high-priority focus over the past two years. The sepsis care pathway and electronic sepsis screening tool were implemented in all inpatient units. Multiple challenges were identified, including nurses’ confidence in using the sepsis screening tool, difficult vascular access in children, delay in physician response within the busy inpatient units, and poor compliance with the documentation. [2] The “Team Sepsis” initiative in the inpatient pediatric wards is a novel improvement step for sepsis management in children. A multidisciplinary team was established at the end of March 2022 and aimed to reduce the number of preventable sepsis- related deaths to zero. The initial phase assisted in identifying unforeseen challenges. A 30% increase in administering intravenous (IV) antibiotics within the golden hour was noted in the pediatric med.
Methodology: Sidra Medicine’s pediatric inpatient non-critical care units provide a focused ward round structure with a multidisciplinary team at the bedside, enabling a collective review of the patient. [1] “Team Sepsis” was implemented on 23 March 2022 in the pediatric medical and surgical inpatient units. The “Team Sepsis” core members include Clinical Nurse Leader (CNL), Vascular Access Management Team (VMT), Senior Residents, on-call Clinical Fellows, and on-call Physicians. [2] Simulations were conducted accordingly by the clinical nurse facilitators (CNF) and resident physicians, in coordination with the sepsis program leads, Sidra IMT (Vocera and (SCS)—Security Control System) team, and service & security operation centre (SSOC). A Team sepsis workflow () was created, reviewed, and socialized to assist with the simulations and implementation.
Results: “Team Sepsis” is actively used in inpatient medical units. Quarter two (Q2- April, May, and June) indicated that 42% of the confirmed sepsis patients received IV antibiotics within the golden hour, and no cases of preventable sepsis deaths were reported. Challenges identified within the initial phase included a lack of clinician’s documentation impacts the accurate assessment of compliance data for order sets and Sepsis bundle, inadequate vascular access management team (VMT) coverage, delayed activation of the “Team Sepsis” in Vocera and resistance within some of the inpatient units to adopt the “Team Sepsis” when a physician is present in the department.
Conclusion: “Team Sepsis” is a promising improvement initiative in sepsis management in children. Initial phase evaluation indicated no reported preventable sepsis-related deaths and a significant percentile improvement of confirmed sepsis patients receiving their IV antibiotics within the golden hour. The following steps for the third quarter (Q3) of 2022 include 1. Re-education on the updated sepsis workflow, 2. continue to monitor and measure outcomes of implementing “Team Sepsis” using Vocera and SSOC Emergency “66”, and 3. share compliance rates with each department.
ID: 193/05-OP-L-d2B: 10
Oral Presentation (Onsite)
Topics: GENERAL PEDIATRICS
Keywords: Infective Endocarditis, dental, general anaesthetic
Audit of the care pathway of patients at increased risk of infective endocarditis requiring dental treatment under General Anaesthetic at Leeds Dental Hospital
Al-Diwani, Hiba1; McDonnell, Sinead2; Balmer, Richard1
1Paediatric Dentistry, University of Leeds, UK; 2Leeds Teaching Hospitals NHS Trust, Leeds, UK.
Background: Infective Endocarditis (IE) is a rare but potentially fatal infection of the endocardium. Children with both acquired and, more commonly, congenital cardiac defects are at increased risk of IE, which can be caused by bacteraemia. Oral disease and its treatment are considered possible causes of bacteraemia, although many routine daily activities also have the potential to introduce infective organisms into the bloodstream. Due to the significant morbidity and mortality associated with IE, attempts to prevent this infection have been made over the years. National guidelines in the UK have been implemented and reviewed for decades, with hospitals developing their own local protocols and standards to prevent this life-threatening complication in children with known cardiac disease.
Aim: This audit aimed to assess the care pathway from referral to treatment for children at increased risk of infective endocarditis who required comprehensive dental treatment under general anaesthetic (GA) due to pain and/or infection from oral disease.
Methods: The clinical records of patients at increased risk of IE who had dental treatment under general anaesthesia were reviewed retrospectively. A data sheet was used to record the length of the patient pathway from referral to treatment and the accuracy of the referral and triage process in line with locally agreed standards. The data was inputted into an excel spreadsheet and analysed to assess whether we met the agreed standards to treat these children as a high priority.
Results: The first cycle showed that we were falling short of the agreed standards, which state that patients at increased risk of IE should be offered their first date for dental surgery within 12 weeks of referral. However, this was only true for 11% of patients, with the average wait from referral to treatment being 31 weeks in 2017. Despite some improvements in the pathway in the second cycle, the average wait was still 30 weeks in 2021.
Conclusions: The audit shows that the agreed standards are not being met in each domain, and the pathway for cardiac patients at increased risk of Infective Endocarditis is significantly longer than expected despite some minor improvements in the pathway compared with 2017. IE may be preventable for children at increased risk if their oral disease is treated promptly and effectively. Recommendations were made to improve the referral triage process through an electronic referral management system to help shorten waiting times. A locally agreed standard operating procedure detailing a protocol for listing patients at increased risk of IE was developed and disseminated to the clinical team with the aim of ensuring patients are offered their dental surgery within 12 weeks of the original referral. Further audit cycles are planned to continue evaluating these interventions’ effectiveness and identify areas for further development to ensure we meet this target and provide care to this vulnerable patient group in a timely manner.
ID: 288/05-OP-L-d2B: 11
Oral Presentation (Onsite)
Topics: ADOLESCENT MEDICINE, PUBLIC HEALTH
Keywords: Emergency Department, non-suicidal self-injuries, retrospective cross-sectional study
Admissions to Emergency Departments for non-suicidal self-injuries behaviors among adolescents in Italy: an eleven year retrospective cross-sectional study
Borraccino, Alberto1; Onorati, Roberta2; Mamo, Carlo2
1Department of Public Health and Paediatrics, University of Torino, Italy; 2Regional Public Health Observatory, Epidemiology Unit, Local Health Board TO3, Piedmont Region.
Background: Self-injurious thoughts and behaviour (SITB) pose a threat to adolescents’ health, increasing the risk of non- conservative behaviours. SITBs can be further divided into suicidal and non-suicidal self-injuries (NSSIs), which refer to “the direct and deliberate destruction of one’s own body tissue in the absence of lethal intent”, [3] which are additionally recognised as competitive risk factors for suicidal behaviour. NSSIs can be caused by multiple factors, among which social contagion, interpersonal stressors, as well as emotional dysregulation and adverse experiences in developmental ages appear to be the most frequent. The most common schemes are cutting, scratching, burning, or incising and scraping. In recent years, there has been a call for improved assessment and risk management skills of injurious behaviour in emergency departments (EDs). Particularly in Italy, EDs represent the primary source of healthcare, especially for young people. Unfortunately, to date, there is a lack of longitudinal epidemiological data in Italy on trends in admissions of adolescents to the ED for NSSI.
Aim: The aim of this study is to describe the frequency and type of access to ED among the population between the ages of 10 and 19 years in the Piedmont region of Italy by using official administrative ED data.
Methods: A retrospective cross-sectional study was conducted on all available medical records of patients aged between 10 and 19 years accessing EDs in the Piedmont Region. Data were obtained from the Ministerial database of health information for the period January 2011—September 2021. All EDs accesses were included, and all records flagged to be a potential NSSI case at triage were selected. Gender and age proportion of ED hospitalisation due to NSSI was calculated for 100 thousand accesses in each year of observation, and overall methods and severity at admittance were described.
Results: A total of 1,417,154 ED visits occurred over the study period, with an NSSI rate of 46.1 cases per 100.000 ED accesses. NSSI events shifted from 42.6 to 22.8 between 2011 and 2013, then increased consistently to 89.1 for every 100000 admissions in 2020 to decrease to 63.6 in the first 9 months of 2021. NSSI were more frequent in girls throughout the whole period, except in 2013 and 2015; overall, girls showed a significantly higher risk of admission (RR = 1.23; 95%CI 1.1–1.4), which was more than doubled in the year 2020. 80% of the patients accessed ED spontaneously, while 15% accessed through an ambulance. The most frequent methods reported were coded as undefined complaints in nearly 40% of all EDs admissions and traumatic conditions (37% in males and 26% in females); intoxication or poisoning was reported in less than 4% of admissions. ED Severity was roughly similar among genders, and four-fifths of all NSSIs were non-life-threatening occurrences registered as white or green codes.
Conclusion: NSSIs represent a public health issue and deserve specific attention due to the dramatic increase registered in the last seven years. According to other studies, this phenomenon appears to be more frequent in girls than in boys also in Italy, and observed differences account for a higher and most alarming increase. Due to the inherent limitations of the information source used, it is credible that the observed phenomenon is likely to be underestimated.
ID: 216/05-OP-L-d2B: 12
Oral Presentation (Onsite)
Topics: RARE DISEASES, HAEMATOLOGY/ONCOLOGY
Keywords: Testicular tumor, Paediatric; Orchidectomy; Testicular sparing surgery.
Paediatric testicular tumors – A 15 year experience.
Santos, Mafalda Ferreira1; Leite, Filipa2
1Centro Hospitalar Tondela-Viseu; 2Instituto Português de Oncologia do Porto.
Background: Testicular tumour is a rare malignancy that demonstrates variability in histopathologic features, treatment protocols, and outcomes based on the patient’s age at presentation. The objective is to report our 15-year experience highlighting management and outcome(s) of paediatric testicular tumours.
Methods: All males (<19 years) with an index diagnosis of testicular tumours at a tertiary center between 2006–2020 were identified. Data were collected regarding age at diagnosis, disease stage, surgical operations, tumour biology and outcome(s).
Cases Report: A total of 15 male patients were identified. The median age at primary diagnosis was 8,7 years (0–16 years). Five tumours were benign, and 10 were malignant. Seven cases (47%) were recorded in pre-pubertal children and eight (53%) in post- pubertal males. In the pre-pubertal group (0–11 years) (n = 7)—four cases of germ cell tumours were recorded, all yolk sac lesions. One male with sex cord-stromal tumour that included one juvenile granulosa cell tumour. One miscellaneous primary testicular tumour, notably a leiomyosarcoma and a tumour-like lesion of the testis—one case of epidermoid cyst. In the post-pubertal male cohort (>12 years) (n = 8), five cases of germ cell tumours were diagnosed, that included one teratoma and four with mixed germ cell tumours. Two males had sex cord-stromal tumours: Leydig cell tumour. One case of paratesticular tumour—rhabdomyosarcoma. Serum alpha1-fetoprotein (AFP) was clearly elevated in 3 of 4 yolk sac tumours. Human chorionic gonadotrophin was elevated in one case of mixed germ cell tumour but remained within normal limits concerning the other entities. High inguinal orchidectomy was the standard surgical method. Dependent on tumour histology, stage and the recommended treatment schedule, postoperative chemotherapy was added. Testis-sparing surgery was performed in 3 boys with primary testicular tumours. Three patients had metastatic disease at presentation (20%). Relapses were not observed. During a median follow-up of 5 years, all patients survived event free.
Learning Points and Discussion: To our knowledge, this is one of the largest study series of paediatric testicular tumours in Portugal. The germ cell tumours constitute the great majority of these lesions, and the other entities are rare, even exceptional. Survival for paediatric testicular tumours is generally excellent. Delayed presentation, however, with a malignant testicular tumour may be associated with poor outcome(s).
Session
06-PT-L-d2C: Poster Presentations Session 6 - Day 2 - Zone C
Presentations
ID: 158/06-PT-L-d2C: 1
Poster presentation (Onsite)
Topics: INFECTIOUS DISEASES
Keywords: Bacteremia, children, claudication, Staphylococcus pseudintermedius
A case of bacteremia in a limping child
Katsaras, Georgios1; Chatziravdeli, Vasiliki2; Psaroulaki, Evdokia1; Tsakonas, Nikolaos3; Tsitsani, Pelagia1
1Pediatric Department, General Hospital of Pella-Hospital Unit of Edessa,Greece; 2Orthopaedics Department, Ippokratio General Hospital of Thessaloniki, Thessaloniki, Greece; 3Orthopaedics Department, General Hospital of Pella—Hospital Unit of Edessa, Edessa, Greece.
Background: Bacteremia is considered healthcare-associated in children with indwelling devices, immunodeficiency and regular hospital-based interventions. We present an interesting and initially misleading case of bacteremia in a school-age child.
Case Report: A 10-year-old female presented to the pediatric emergency department (PED) with intermittent claudication and low- grade fever (T: 37.7 oC) for two days. There was no history of trauma or other chronic diseases. Clinical examination revealed subtle pain in passive movement s of the right hip and pain in weight bearing. Lower limbs were well perfused and neurovascularly intact with no obvious swelling or erythema. Laboratory tests (WBC, Biochemical, urine analysis) were normal, with negative inflammatory markers (CRP, ESR). Hip X-rays (face and frog lateral) and abdominal ultrasonography were also uneventful. The patient was discharged with instructions for bed rest, anti-inflammatory therapy, and re-evaluation in case of persistent or worsening symptomatology. Following 2 days, the patient presented again with persistent claudication and high-grade fever (T: 39.9 oC). She was hemodynamically stable, conscious and oriented. On examination, there were multiple superficial abrasions in the lower extremities from dog playing, and a more detailed history revealed that the father was involved in animal breeding. Laboratory exams showed elevated CRP (4.44 mg/dl) and ESR (36). Blood cultures were taken, and she was started on IV antibiotics (clindamycin & cefotaxime). The patient improved clinically, and inflammatory markers decreased within 48 hours of treatment. Staphylococcus pseudintermedius was isolated in the blood culture, which is an emerging zoonotic pathogen of canine origin that causes an array of severe diseases, including bacteremia and endocarditis. The patient completed 10 days of IV antibiotic treatment and was discharged asymptomatic with negative inflammatory markers and per os amoxicillin/ clavulanic acid according to the antibiogram. MRΙ was conducted after discharge and revealed bone marrow oedema of the right acetabulum. The patient discontinued antibiotic treatment after 15 days since she was clinically well with normal laboratory values and an MRI without a definitive diagnosis of osteomyelitis.
Learning Points Discussion: Children presenting with limping and low-grade fever should always be treated cautiously. Transient synovitis is a diagnosis of exclusion and is rare in children over 7 years—old. Bone and joint infection and bacteremia should be considered and ruled out in cases when the patient is febrile for several days with persisting claudication (Figure ).
ID: 279/06-PT-L-d2C: 2
Poster Presentation (Onsite)
Topics: GENERAL PEDIATRICS, GASTROENTEROLOGY
Keywords: anal canal duplication, congenital anomaly
A revealing handstand – case report of an anal canal duplication
Tavares, Catarina Faria1; Costa, Inês Silva1; Pereira, Helena1; Horta, Patrícia1; Carvalho, Graça2; Salgado, Conceição1
1Centro Hospitalar Tondela Viseu, Portugal; 2Hospital CUF Viseu.
Introduction: Anal canal duplication (ACD) is the rarest congenital anomaly of the gastrointestinal tract. ACD is defined as a second anal orifice located posterior to the true anus, ending blindly and without connection to the anorectum, and is usually tubular. More than 90 percent of these cases occur in females and are often diagnosed and treated in childhood. However, some cases remain undiagnosed until adulthood because patients are often asymptomatic, and the anomaly sometimes goes unnoticed during routine examinations.
Case Report: A five-year-old female was presented for medical consultation because she noticed an extra-opening canal in the perineal area for the first time while the child was performing a handstand. The patient was asymptomatic, and her past medical history was unremarkable. On perineal examination, a 5 mm in diameter orifice was found in the midline, about 1 cm posterior to her normal anus, and she was referred to pediatric surgery consultation. The child was further evaluated with a colonoscopy which confirmed an anal canal duplication, about 2 cm in length, ending blindly and without connection with the anorectum. Upon further investigation, the ACD was found to be an isolated finding, and no associated pathologies were identified. The duplicated anal canal was excised via mucosal stripping using a posterior sagittal approach. The postoperative course was uneventful. There was no evidence of recurrence during the follow-up period (Figure ).
Discussion: This report aims to raise awareness of the importance of a regular pediatric consultation for a detailed physical examination, including all anatomic areas, from birth until early adulthood since this is the best way to identify such rare conditions. The lack of knowledge of this entity, as well as its asymptomatic presentation, may lead to a delay in diagnosis. Once diagnosed, surgical correction is usually undertaken, with an excellent prognosis.
ID: 113/06-PT-L-d2C: 3
Poster Presentation (Onsite)
Topics: GENERAL PEDIATRICS, EMERGENCY PEDIATRICS
Keywords: Pediatrics, cardiomyopathy, hypertrohic, death, desfibrillator
Hypertrophic cardiomyopathy in children: a silent threat.
Ortigado, Alfonso1; Castaño, Elisa1; Gutiérrez-Larraya, Federico2; Cartón, Antonio2; Sánchez, Raúl3; Ortigado-López, Alfonso4
1Department of Pediatrics, University Guadalajara Hospital, Guadalajara Spain; 2Department of Pediatric Cardiology, University La Paz Hospital, Madrid, Spain; 3Department of Pediatric Cardiac Surgery, University La Paz Hospital, Madrid, Spain; 4Biotechnology, Pharmacy Faculty, San Pablo-CEU University, Madrid, Spain.
Background: hypertrophic cardiomyopathy (HCM) is defined as left ventricular (LV) hypertrophy in the absence of abnormal loading conditions (valve disease, congenital heart disease or hypertension). The aetiology is heterogeneous (inborn errors of metabolism, neuromuscular disorders, malformation syndromes) and can guide the diagnosis. Patients with sarcomeric protein disease may be asymptomatic, but the lifelong risk of adverse events exists, especially sudden cardiac death (SCD).
Case Presentation Summary: We report a previously healthy 6-year-old female from Cameroon, referred to a paediatric cardiologist due to an asymptomatic murmur. Parenteral consent was obtained. Her family history was unremarkable, although her father´s information was unknown. The physical examination was normal, with no dysmorphic features or evidence of any systemic or metabolic disorder, only an innocent murmur. [1] 12-lead electrocardiography (ECG) demonstrated voltage criteria for LV hypertrophy, LV left-axis deviation and lateral precordial repolarization abnormalities. Echocardiography showed concentric LV hypertrophy, the presence of LV wall thickness > 2 standard deviations above the body surface area-corrected mean, without outflow tract obstruction. The genetic testing reported carrying 2 pathogenic variants (genes MYH7 and TTR). The study was completed with chest X-ray, ambulatory ECG monitoring, cardiovascular magnetic resonance imaging and exercise stress testing. [2] Atenolol was the initial drug chosen, we considered this patient a high-risk case, and the implantable cardioverter defibrillator (ICD) placement was indicated for primary prevention. The outcome of this patient showed a syncope with rapid onset while playing at school, with an absence of prodromes. The transient loss of consciousness and postural tone were short, and the recovery was complete and “spontaneous”. Although the event seemed innocent, it really was a life-threatening emergency. The ICD detected symptomatic sustained monomorphic ventricular tachycardia and stopped the irregular heartbeats with an electric shock (Figure ).
Learning Points Discussion: [1] ECG helps as a first filter to identify asymptomatic patients. [2] Echocardiography remains the gold standard for diagnosis. [3] Clinical management represents a challenge to the paediatric cardiologist. [4] Syncope is a major risk factor for subsequence SCD in HCM.[5] ICD therapy has been shown to be effective in preventing SCD from ventricular arrhythmias.
ID: 182/06-PT-L-d2C: 4
Poster Presentation (Onsite)
Topics: GENERAL PEDIATRICS, ENDOCRINOLOGY
Keywords: Scrotal hair; Infancy; Androgens; Testosterone
Isolated scrotal hair in infancy: a benign phenomenon?
Pinho, Joana1; Vieira, Beatriz2; Mazeda, Inês2; Oliveira, Gracinda2
1Department of Pediatrics, Centro Hospitalar Vila Nova de Gaia/Espinho, Portugal; 2Department of Pediatrics, Centro Hospitalar Póvoa de Varzim/Vila do Conde, Portugal.
Background: Scrotal hair growth in infants is a rarely described condition that can be alarming for both parents and physicians. The appearance of pubic hair on a male infant usually suggests a true excess of circulating androgens, which could arise from, for example, congenital adrenal hyperplasia or adrenal tumour. However, the development of isolated scrotal hair alone, in the absence of other androgen-related signs or symptoms, could simply be a benign phenomenon.
Case Presentation Summary: A previously healthy two-month-old boy is brought to the clinic by his mother to assess a number of dark coarse scrotal hairs that appeared during the preceding week. On examination, no other signs of androgenization or secondary features of sexual development were noted, specifically no penile or testes enlargement or growth acceleration. The neurological and psychomotor development was normal. Investigations showed testosterone, 17-OHP (17-hydroxyprogesterone), androstenedione, cortisol, ACTH (adrenocorticotropic hormone), TSH (thyroid-stimulating hormone), free T4 (thyroxine) LH (luteinizing hormone) and FSH (follicle-stimulating hormone) concentrations within the normal ranges; only DHEA-S (dehydroepiandrosterone sulfate) was decreased (7 µg/dL; normal range: 31–214 µg/dL). After differential diagnosis, the diagnosis of transient isolated scrotal hair development was made. On follow-up, scrotal hair gradually decreased since 6 months of age and completely disappeared by the age of 12 months. Subsequent linear growth was always normal.
Learning Points Discussion: Current evidence suggests that the development of isolated scrotal hair alone, without other signs of androgenization, is most likely a benign phenomenon. It could be explained by an increased sensitivity of androgen receptors in scrotal hair follicles to the normal physiological high concentrations of testosterone seen in early infancy. Scrotal hair diminishes when concentrations of androgens gradually decrease later in infancy, leading to spontaneous resolution. Even though this seems to be a benign condition, the authors emphasize that all patients need full urgent investigation and differential diagnosis as isolated scrotal hair development is still a diagnosis of exclusion.
ID: 240/06-PT-L-d2C: 5
Poster Presentation (Onsite)
Topics: GENERAL PEDIATRICS
Keywords: RAP, retroperitoneal ganglioneuroma
Rear cause of recurrent abdominal pain in children; case report of 8 year old girl with retroperitoneal ganglioneuroma
Hristova, Aleksandra1; Stojanovska, Matilda2
1General Hospital Kumanovo, Republic of North Macedonia; 2General Hospital Kumanovo, Republic of North Macedonia.
Introduction: RAP is defined as at least 3 episodes of pain that occur over at least 3 months and affect the child’s ability to perform normal activities. The cause of RAP may be functional and organic (5–10%): helicobacter infection, eosynophilic oesophagytis, carbohydrate intolerance, abdominal migraine, IBD and surgical conditions.
Case Report: We present an 8-year-old girl with RAP for about 3 years. Abdominal ultrasonography had been performed by family doctor at the age of 6 years and misdiagnosed as acute enlargement of a lymph node. The girl continued to experience abdominal discomfort; thus, another abdominal ultrasound was performed. The result was a homogenous mass within the paraumbilical region with well-defined borders and a loop with non-pathological vascularization with dimensions: of 40 × 26 mm. We consulted a surgeon and received a recommendation for abdominal CT: an oval hyperdense mass with dimensions 41 × 37 mm was noticed within the left mesograstric region in the level of bifurcation of a. iliaca communis. The case was forwarded to the pediatric surgery clinic, where further analysis was performed. The laboratory findings were within the reference values. MRI showed a demarcated heterogeneous formation with dimensions 43 × 35 mm in the L3—L5 level of the left retroperitoneal region adjacent to m. ileopsoas. Surgical resection was performed, and the tumour was completely removed. The pathophysiological finding was retroperitoneal ganglioneuroma.
Conclusion: Recurrent abdominal pain requires a rigorous approach towards proper diagnosis in a timely manner.
ID: 116/06-PT-L-d2C: 6
Poster Presentation (Onsite)
Topics: GENERAL PEDIATRICS
Keywords: congenital malformations, pregnant women, antenatal death, logistic regression analysis, modeling
Results of using logistic regression to model and predict congenital fetal malformations in mothers with a history of antenatal fetal death
Mamedzade, Gulnara; Huseynova, Saadat
Scientific Research Institute of Obstetrics and Gynecology, Azerbaijan.
Background: The prevention of congenital malformations of the fetus (CM) continues to be the focus of attention of specialists worldwide and remains relevant. This is due to the serious socio-medical significance that congenital pathology has acquired in modern society. In recent years, logistic regression analysis has often been used to correlate relationships between two or more variables.
Aim: The study aims to create a logistic model for predicting fetal CM based on risk factors in mothers with a history of antenatal fetal death.
Material and Methods: We studied 665 mothers who gave birth to children with congenital malformations, of which 532 (80.0%) women had a history of antenatal death of the fetus (main group), 133 (20.0%) had no history of antenatal death (control group). Analyzed: age, city/region, gestational period, number of abortions, cases of non-developing pregnancies, miscarriages, fetal abnormalities, levels of alpha-fetoprotein (AFP), human chorionic gonadotropin (hCG), unconjugated estriol (NE). [1] Statistical processing of the material was carried out in the Statistical system of the Microsoft Excel program. When processing the data, the method of logistic regression (ROC-analysis) was used, and sensitivity and specificity were determined. Differences were considered statistically significant at p < 0.05.
Results: When calculating the area under the ROC-curve, corresponding to the relationship between the development of congenital malformations and variables: age, gestational period and recurrent miscarriage, ROC-analysis revealed the following characteristics: for age—AUC = 0.602, Se—0.470, Sp—0.365, р < 0.001.95 % CI: 0.550–0.653; for the gestational period—AUC = 0.667, Se—0.603, Sp—1.139, p < 0.001, 95% CI: 0.622–0.713; for miscarriage—AUC = 0.466, Se—0.244, Sp—0.354, p = 0.055, 95% CI: 0.394–0.498. At the same time, high sensitivity and specificity were observed in the first trimester. The results of ROC-analysis in assessing the variables AFP, hCG and NE showed low diagnostic value. So, for AFP—AUC = 0.515, p = 0.859, 95% CI: 0.362–0.669, hCG—AUC = 0.602, p = 0.229, 95% CI: 0.446–0.759; for NE—AUC = 0.456, p = 0.607, 95% CI: 0.308–0.604. Therefore, the logistic model based on the variable gestational age had a medium diagnostic value; in other cases, the model had a low diagnostic value.
Conclusion: Logistic regression analysis can be used to model and predict CM in mothers with a history of antenatal fetal death. However, further research is needed to improve the model.
ID: 129/06-PT-L-d2C: 7
Poster Presentation (Onsite)
Topics: GENERAL PEDIATRICS, ALLERGY, IMMUNOLOGY & RESPIRATORY
Keywords: Asthma, Education
Teaching programme to help school students recognise and manage Asthma exacerbations
Chandran, A1; Conte, A1; Elayar, K1; Khan, A1; Mehta, S1; Miah, F1; Nagaraj, R1; Oworu, E1; Park, JS1; Saliba, L1; Sivaranjan, V1; Suri, S1; Tandanu, E1; Coppel, J2; Kearney, J2; Herbert, S3
1Medical Students, Kings College University, London (joint first authors); 2Asthma Innovation Research (AIR) Trustees (registered charity no. 1168495); 3Kings College Hospital, London.
Background: Asthma & Lung UK statistics demonstrate that 10% of children have asthma, equating to around 3 in every UK school classroom. Additionally, the National Review of Asthma Deaths 2014 highlighted that up to 80% of paediatric deaths due to asthma occurred out of the hospital. Therefore parents, children, and teachers should be educated about managing asthma. However, formal asthma education remains absent at all stages of the UK school curriculum. Asthma Innovation Research (AIR) is a charity that provides such education to schools free of charge.
Method: In 13 March 2022 Kings College University Year 2 medical students delivered a targeted asthma education programme aimed at school-age children in the UK as part of AIR’s project. Nationally, 8 schools were included in the programme with children between the ages of 6 and 14. They received 20-minute presentations on asthma, with particular emphasis on recognising an asthma exacerbation and initial treatment in the pre-hospital setting.
Aim: The aim of the presentations was not only to improve the children’s knowledge of asthma but also to reduce the stigma around the condition. The key acute management learning points included calling for help and/or dialling “999” and giving the blue inhaler. Children’s knowledge was tested with the same quiz before and after the teaching.
Results: The pre- and post-teaching quizzes received 841 and 623 responses. We demonstrated an improvement in inhaler knowledge; 96% of students knew the function of a “blue inhaler” after the presentation compared to only 58% beforehand. Similarly, for the “brown inhaler” 91% understood its function afterwards, compared to only 33% at the beginning. Before the teaching session, 33% of students were unable to recognise an asthma exacerbation which improved to 9%, and 24% didn’t know what to do if they saw someone having an exacerbation which improved to 8%.
Conclusions: After our teaching sessions, the student’s ability to recognise and start initial management of an asthma exacerbation increased. These findings suggest that asthma education in schools has a potential role in preventing asthma deaths and that medical students represent a low-cost option for spreading such a programme across the UK.
ID: 104/06-PT-L-d2C: 8
Poster Presentation (Onsite)
Topics: COVID-19
Keywords: COVID-19, pediatric emergency, pediatric hospital admission
Impact of COVID-19 on the Pediatric Emergency Flow: Experience from Kuwait
Alazmi, Marzouq; Elhassanin, Ahmed Farag
Adan hospital, MOH, Kuwait, Kuwait
Introduction: Children require unique and special emergency health care, especially in countries where young people constitute a large portion of their population, like Kuwait. Starting from December 2019, the COVID-19 pandemic has spread worldwide from Wuhan, China affecting more than 13 million people; since then, all medical services have been affected. [1] There were many challenges to the medical services, including the large number of patients coming to the hospital, the quality of patients and delayed seeking medical advice from the fear of catching infections in the medical facilities. [2] In Kuwait, the lockdown started in March 2020 from partial to complete for variable periods. As the entire world started to decrease the restriction and precautions, Kuwait began doing the same on 15 June 2020. As a major third-level pediatric emergency unit serving an area of more than 750,000 people, we noticed marked changes in the quantity and quality of sick children coming to our emergency unit.
Aim: This study aims to clarify the changes in the pediatric emergency service during the lockdown period (from 15 March 2020 to 15 July 2020) and compares these data with a similar period in the previous year.
Materials and Methods: Adan Hospital is one of the major Kuwaiti governmental hospitals serving a population of 750,000. There were 160,715 child visits to the pediatric emergency unit (PEU) in 2019, not including trauma cases or children more than 12 years. From the monthly statistical reports from 15 March to 15 July 2019 and 2020, we collected the total number and the diagnosis of patients visiting the Adan hospital PEU. Also, we collected the number and diagnosis of patients admitted to the pediatric emergency unit observation (PEUO) and those admitted to the hospital. We compared the data collected in 2019 and 2020 [during the period of lockdown due to COVID-19). Different degrees of lockdown ranged from partial to complete from 15 March 2020 to 15 July 2020.
Results: Total number of visits to PEU and the classified causes of these visits are shown in Table . There was a significant drop (P = <0.05) in the number of total visits to PEU in 2020 compared with 2019. This significant decrease was also observed in patients who came with AGE, URTI, chest problems and other neonatal problems. Whereas there was no significant decrease in the number of patients who came with rule-out sepsis (R/O sepsis) and seizures. Table shows the numbers of patients needing PEOU and those needing admission to the hospital. Excluding patients suspected to be COVID-19 from our statistical report, there was a significant decrease (P = <0.05) in the number of patients who needed PEUO care in the year 2020 compared with the year 2019. This decrease was observed clearly in patients presented with AGE, chest problems and other neonatal problems, whereas patients with seizures and R/O sepsis showed no significant decrease.
Table 1. Absolute numbers of visits to PEU during the period (March 15th to July 15th) in the years 2019 and 2020
Table 2. Patients admitted to the PEUO and to the hospital during the period (March 15th to July 15th) in the years 2019 and 2020
ID: 115/06-PT-L-d2C: 9
Poster Presentation (Onsite)
Topics: RARE DISEASES, COVID-19
Keywords: Pericardial Effusion, Pericardiostomy, Multisystem Inflammatory Syndrome in Children, Covid-19
Massive Pericardial Effusion in a 9-year old female with COVID-19 Associated Multisystem Inflammatory Syndrome in Children (MIS-C)
Carasig, Gianina Louise; Subido-Cariño, Maria Tricia
Cardinal Santos Medical Center, Philippines.
Introduction: Coronavirus disease 2019 (COVID-19) is a global pandemic that has had a catastrophic effect on the human population, with approximately 20% experiencing severe or critical disease. Children generally have a milder clinical course and more favourable outcome compared to adults. However, a growing number of countries have been describing cases of a systemic hyperinflammatory condition defined as a multi-system inflammatory syndrome in children (MIS-C). The constellation of clinical presentations of COVID-19 infection in children keeps evolving, and this case report may serve as a useful reference to other pediatricians caring for children affected by COVID-19. Pediatricians should be mindful of the probability of COVID-19 infection leading to Multisystem Inflammatory Syndrome in Children (MIS-C) and its complications, such as pericardial effusion that could possibly develop into pericardial tamponade.
Case Presentation: This is a case of a previously healthy 9-year-old female who tested positive for SARS-CoV-2 two weeks prior and presented with pericardial effusion, pleural effusion, and ascites in the setting of fever, cough, diarrhoea, and edema. The inflammatory response involving the cardiovascular, pulmonary, and gastrointestinal systems and the elevated inflammatory markers support the diagnosis of MIS-C. IV-gammaglobulin, Methylprednisolone, and Aspirin were started. However, 2d echocardiography showed progression of pericardial effusion, with evidence of right atrial and ventricular wall collapse, on the verge of cardiac tamponade. Hence patient was referred to an Interventional Pediatric Cardiologist who performed an Emergency pericardiostomy tube insertion.
Differentials: Variable degrees of cardiac involvement during and after COVID-19 infection have been reported in recent literature. Pericardial effusion has been identified as one of the more common cardiovascular complications in MIS-C. Data about the spectrum of cardiac presentation of COVID-19 infection in children is limited, and the frequency of severe pericardial effusion requiring drainage is still unknown. In the Philippines, this will be the 1st reported case of MIS-C presenting with edema, ascites, pleural effusion and massive pericardial effusion requiring emergency pericardiostomy tube insertion.
Discussion: This case report involves a child with no underlying cardiac disease who developed massive pericardial effusion as a COVID-19-associated MIS-C complication requiring pericardiostomy tube insertion. This was necessary to prevent cardiac tamponade, which is a medical emergency. As knowledge about novel manifestations of COVID-19 in children is evolving, reporting is necessary to better equip clinicians in recognizing the spectrum of symptoms of MIS-C, which is imperative for the timely initiation of appropriate management.
ID: 172/06-PT-L-d2C: 10
Poster Presentation (Onsite)
Topics: INFECTIOUS DISEASES, COVID-19
Keywords: Covid-19, adolescent, vaccine, myopericarditis
Post Covid-19 vaccine myopericarditis – a case report
Strecht Guimarães, Francisca; Ferreira Mendes, Joana; Silva, Joana; Amaral Pinheiro, Teresa
Centro Hospitalar de Entre o Douro e Vouga, Portugal.
Background: The issue of vaccinating all healthy children against COVID-19 is more difficult than for adults as the balance of risks and benefits remains controversial. As with any vaccine, there are potential side effects of the COVID-19 vaccine (C19V). Some cases of pericarditis and myocarditis have been reported after administering the second dose of mRNA vaccines, particularly in male adolescents.
Case Presentation: A male adolescent, 10 years old, with atopy, went to the emergency department of a level II hospital due to thoracalgia and dyspnea beginning that day. Symptoms worsened with activities. There was no history of fever or any respiratory symptoms. He had no history of a previous infection or use of any medication. He had received the first dose of the C19V two days earlier. He was hemodynamically stable and only reported discomfort with palpation of the upper half of the sternum. Cardiac and pulmonary auscultation were normal. The analytical study revealed increased heart enzymes (Troponin I 60.0 ng/l; NT-pro BNP 94.9 pg/mL) and lactate dehydrogenase (DHL) 259 U/L. Electrocardiogram presented with sinus rhythm and an apparent ST-segment elevation, with no other abnormal findings. He was referred to a pediatric cardiology consult. Echocardiogram was normal. He was prescribed ibuprofen and recommended to avoid sports for three months. One week later, he was asymptomatic.
Learning Points/Discussion: Myopericarditis is a rare infection in children. It is mostly caused by common viral infections, autoimmune diseases, intoxications/medications, or severe allergies. In this case, there was no previous infection or personal history that seemed to justify the myopericarditis other than the first dose of the C19V. To our knowledge, this is the first case of myopericarditis reported after the first C19V dose.
ID: 157/06-PT-L-d2C: 11
Poster Presentation (Onsite)
Topics: COVID-19
Keywords: Covid-19 disease, infants, arrhythmias, cardiogenic complications, Supraventricular tachycardia (SVT)
Supraventricular tachycardia (SVT) in an infant with Covid-19 infection
Tsitsani, Pelagia; Stylianidou, Margarita; Xylouri, Garyfallia; Psaroulaki, Evdokia; Oikonomou, Evaggelos; Katsaras, Georgios
Pediatric Department,General Hospital of Pella-Hospital Unit of Edessa, Greece.
Background: SARS-COV-2 (Covid-19) infection has been associated with the occurrence of arrhythmias. Pathophysiological mechanisms that increase the risk of arrhythmias range from direct myocardial damage to extracardiac involvement. According to current reviews, cardiovascular issues during acute Covid-19 infection in children are not common. Nevertheless, further investigation is required to determine which viral genotype shifts and in which specific pediatric populations the incidence increases. We present a case of paroxysmal supraventricular tachycardia (SVT) in an infant in the context of Covid-19 infection.
Case Presentation Summary: A 56-day-old male infant presented to the Emergency Department due to severe restlessness, decreased feeding, tachycardia, and fever for 24 hours. Clinical examination revealed poor general condition, pallor, perioral cyanosis, dry mucous membranes, acrocyanosis, febrile decimal motion (37.5 °C) and a capillary refill time of 4 sec. The patient was placed under continuous recording of vital signs (monitoring), and an increased heart rate of 330 beats/ minute was found, with no P waves on the ECG, at which point the diagnosis of paroxysmal SVT was made. Laboratory testing revealed elevated mononuclear cells (970/ μL) and thrombocytosis (409,000/μL) with an unaffected red blood cell count. He was placed on oxygen, and Valsalva manoeuvres were performed with ice packs applied to the face, with subsequent reversal of the tachycardia. The performance of the Covid-19 Rapid test and PCR established the diagnosis of Covid-19 infection, and he was transferred to the Covid-19 unit of a tertiary hospital. He relapsed, and an electrophysiological study and a heart ultrasound were performed without abnormal findings. He has been prescribed propranolol for a year and is clinically rhythm reviewed in our department.
Learning Points Discussion: Case reports and small series have described cardiogenic shock, myocarditis, pericarditis, and arrhythmias associated with Covid-19 infection in children. Arrhythmias include ventricular tachycardia, atrial tachycardia and first- degree atrioventricular block. Hemodynamic consequences of the Covid-19 disease in infancy, combined with the not fully elucidated sequelae of the disease, as well as the increased percentages of seriously ill infants from Covid-19 compared to older children, makes the pediatrician’s vigilance imperative.
ID: 151/06-PT-L-d2C: 12
Poster Presentation (Onsite)
Topics: EMERGENCY PEDIATRICS
Keywords: Foreign body, ingestion, endoscopic removal, children
Interesting case of an ingested foreign body in a 4-year-old child
Tsitsani, Pelagia; Katsaras, Georgios; Samartzi, Petrina; Psaroulaki, Evdokia; Xylouri, Garifallia
Pediatric Department, General Hospital of Pella-Hospital Unit of Edessa,Greece.
Background: Ingestion of foreign bodies is a frequent cause of admission to the Pediatric Emergency Department. If the foreign body is not expelled naturally, it may lead to perforation of the gastrointestinal (GI) tract—intestinal ischemia. Preschoolers of both sexes, adolescent boys, and children with psychological impairment are at the highest risk. We present an interesting case of a swallowed foreign body (a coin of New Year’s Eve cake), a surgical emergency.
Case Presentation Summary: A 4-year-old female child presented with reported epigastric discomfort and nausea for 48 hours. The patient was afebrile, hemodynamically stable, with excellent consciousness and good orientation. Clinical examination revealed abdominal flatulence with deep bowel sounds without positive Mac Burney, Blumberg and Rovsig signs. Blood work was performed with normal findings and negative markers of inflammation. Due to the worsening clinical picture with a reported urge to defecate without the child being able to act, we focused on taking a detailed history. According to the child’s testimony, the parents revealed possible ingestion of a coin a fortnight ago (New Year’s Eve) from a cake, but it was doubtful whether it had passed spontaneously through the GI tract. A plain abdominal x-ray in the upright position revealed the presence of a radiopaque foreign body in the rectum. At that point, she was referred to a pediatric surgery clinic. The removal was performed emergently in the operating room under general anaesthesia. It was a cast-bronze king-pie coin that had shrunk on its way through the intestinal tract and eventually hooked into the rectosigmoid. The patient’s recovery was uneventful (Figure ).
Learning Points Discussion: Accidentally received foreign bodies should always be on the pediatrician’s mind, and thorough history should be insisted upon. Most swallowed foreign bodies will harmlessly pass through the GI tract, but some may become lodged, traumatize the mucosa or cause caustic burn injury. Particular attention has to be paid to coins, sharp objects, food bolus, caustic liquids, batteries, and magnets, as they can lead to life-threatening complications. Endoscopic removal of the foreign body is a safe and effective approach in experienced centres. When foreign body ingestion is suspected, radiological examination of the neck, chest and/or abdomen is required depending on the history, the type of the referred ingested item and the existing clinical symptoms.
ID: 124/06-PT-L-d2C: 13
Poster Presentation (Onsite)
Topics: EMERGENCY PEDIATRICS
Keywords: Synovial Arteriovenous Malformations, Quadriceps muscles atrophy, prominent cutaneous superficial veins on lower limb
Right knee synovial arteriovenous malformations in a 30 months old Kuwaiti boy
Alazmi, Marzouq1; Elhassanin, Ahmed Farag2
1Adan hospital, MOH, Kuwait, Kuwait; 2Faculty of Medicine, Elmsnoura university.
Introduction: Arteriovenous malformations (AVMs) are congenital abnormal communication between arteries and veins with one or more fistulae. Synovial AVMs are rare. The possibility of synovial AV malformations should be considered in patients having recurrent painful hemarthrosis with normal coagulation parameters. AVMs have different presentations as arthralgia, limited joint movement or swelling (hemarthrosis). Many complications can happen as chronic synovitis, progressive cartilage damage and secondary osteoarthritis.
Case Report: Nawaf is a 30-month-old Kuwaiti boy. He presented with a one-year history of intermittent right-sided limping without associated fever. There was no history of trauma, skin rash or other joint affection. On examination, there was no fever or skin rash. Cardiac, chest, and abdominal examinations were normal. A joint examination showed swollen right knee joints with decreased range of movement but no redness or hotness. Right quadriceps muscle atrophy was noticed, especially when compared to the left side (). There were also prominent cutaneous superficial veins on the right lower limb ().
Discussion: All laboratory investigations were negative except elevated D-Dimer. MRI with angiography showed features of extensive right lower limb arteriovenous malformation around the knee joint. There were tortuous vessels in the proximal and distal aspect of the right intermodal part of the right vastus medialis and lateralis and between the right gastronemius and solius muscles with associated atrophy in these muscles. Some vessels extended into the intra-artuicular space of the right knee joint. Two hematomas were seen between the solius and flexor muscles and anterior to popliteus muscle ()
ID: 268/06-PT-L-d2C: 14
Poster Presentation (Onsite)
Topics: ADOLESCENT MEDICINE, PUBLIC HEALTH
Keywords: Adolescent health, Alcohol use, Survey, Abstention Differences between abstainers, light, and heavy drinkers
Suris, Joan-Carles; Chok, Lorraine; Barrense-Dias, Yara
Center for Primary Care and Public Health (Unisanté), Switzerland.
Background: The aim of this research is to determine the characteristics of abstainers and light drinkers compared to heavy drinkers.
Methods: Data were drawn from the GenerationFRee cohort, carried out in the canton of Fribourg, Switzerland, among post- mandatory students between 2014–15 (mean age 16) and 2018–19 (mean age 19) (4 waves). We defined Abstainers as those never having drunk alcohol, Light drinkers as those having drunk alcohol but not having been drunk and Heavy drinkers as those having been drunk in the past 30 days. With these three groups, 5 alcohol use trajectories emerged, and we compared Abstainers (N = 432, 26.8%, 57.4% females), Light (including Light, Late-onset light and Undecided drinkers; N = 458; 28.9%, 54.3% females), and Heavy drinkers (N = 732, 44.5%, 34.5% females) on personal, familial, academic, behavioral and health-related variables. All significant variables at the bivariate level (p < .05) were included in a multinomial logistic regression using heavy drinkers as the reference category. Results are presented as relative risk ratios (RRR) with 95% confidence interval.
Results: In the bivariate analysis, groups differed in gender, family structure, academic track, residence, place of birth, and current tobacco and cannabis use. No differences were found for age, academic results, relationship with mother or father, socioeconomic status, physical or mental health, monthly income, physical activity or social support. (1) At the multivariate level, compared to Heavy drinkers, Light drinkers were significantly more likely to be females (RRR: 2.38 [1.74:3.25]) and to live in an urban setting (3.03 [2.16:4.27]), and less likely to be Swiss-born (0.39 [0.22:0.68]), to smoke (0.18 [0.13:0.26]) or use cannabis (0.35 [0.20:0.61]). (2) Abstainers were significantly more likely to be females (2.60 [1.91:3.53]), younger (0.87 [0.79:0.96]), in high school (1.65 [1.14:2.38]) and living in an “intact” family (1.47 [1.05:2.05]) in an urban setting (1.94 1.38:2.73]). They were also less likely to be Swiss-born (0.41 [0.23:0.72]) and to smoke (0.19 [0.14:0.27]) or use cannabis (0.11 [0.06:0.22]).
Conclusions: Both light drinkers and abstainers differ from heavy drinkers. Culture may be behind being more frequently non- Swiss-born, and rural residence is a known risk factor for drinking. The fact that abstainers are more likely to live in an “intact” family may reflect a higher level of monitoring by their parents. Importantly, they are less likely to use other substances. Prevention messages in the sense that non-drinking can also be cool could be ways to moderate alcohol use among youths and, through it, the use of other substances.
Funding
Swiss National Science Foundation.
ID: 177/06-PT-L-d2C: 15
Poster Presentation (Onsite)
Topics: RHEUMATOLOGY
Keywords: Henoch-Schönlein purpura, glutathione S-transferases, polymorphisms
Influence of glutathione S-transferase (GST) polymorphisms in patients with Henoch-Schönlein purpura
Held, Martina1; Juras, Ana2; Sestan, Mario1; Kifer, Nastasia1; Srsen, Sasa3; Gagro, Alenka4; Frkovic, Marijan1; Huljev Frkovic, Sanda1; Crkvenac Gornik, Kristina2; Jelusic, Marija1
1Department of Pediatrics, University of Zagreb School of Medicine, University Hospital Centre Zagreb, Zagreb; 2Department of laboratory diagnostics, University of Zagreb School of Medicine University Hospital Centre Zagreb, Zagreb; 3Department of Pediatrics, University of Split School of Medicine, University Hospital Centre Split, Split; 4Children’s Hospital Zagreb, Josip Juraj Strossmayer University of Osijek, Medical Faculty Osijek, Zagreb, Croatia
Background: Henoch-Schönlein purpura (HSP) is the most common childhood vasculitis and, being a multifactorial disease in the pathogenesis of which, genetic factors might also play an important role. Glutathione S-transferases (GSTs) are metabolic enzymes protecting cells against oxidative stressors in the environment by detoxifying a potentially toxic and carcinogenic electrophiles. Deletions in GSTs reduce detoxification enzymatic activity and thus can aggravate the susceptibility to various diseases. The aim was to investigate the influence of GSTA1, GSTM1 and GSTT1 genes polymorphism on HSP susceptibility, especially to different disease phenotypes.
Methods: Clinical data were collected from three Croatian tertiary centers for pediatric rheumatology. GSTA1, GSTM1, and GSTT1 polymorphisms were detected in patients and controls. DNA was extracted from whole blood samples using the QIAGEN QIAamp kit. GSTA1 (−69C>T) was examined by the polymerase chain reaction-restriction fragment length polymorphism (PCR-RFLP) method, whereas the GSTM1 and GSTT1 were determined by the PCR method.
Results: The pilot study included 107 patients diagnosed with HSP, of whom 56 were girls and 51 were boys, with a median age at the time of diagnosis of 6.25 (4.5–8.0) years, as well as 75 sex and age-matched controls. All patients had a purpuric rash, 75,7% had arthralgia or arthritis, 36,5% had affected gastrointestinal system, while 31,7% of patients developed Henoch-Schönlein purpura nephritis (HSPN). The frequencies of GSTM1 (−) null allele and GSTT1 null (−) allele in HSP patients were 56,1% and 26,2%, respectively. There was no statistically significant difference in the null genotype distribution of GSTM1 and GSTT1 between groups (CI 0.49–1.62, OR 0.89, p = 0.714; CI 0.35–1.44, OR 0.70, p = 0.335). The frequency of GSTA1 C/C, GSTA1 C/T and GSTA1 T/T genotypes in HSP patients were 36,5%, 44,8% and 18,7% respectively. There was no statistically significant differences in genotype frequencies between patients and controls (CI 0.83–3.00, OR 1.38, p = 0.167; CI 0.33–1.09, OR 0.60, p = 0.09; CI 0.55–2.65, OR 1.20, p = 0.639). Patients with gastrointestinal involvement had a statistically significant difference in the null genotype distribution of GSTM1 compared with patients without (CI 0.15–0.81, OR 0.35, p = 0.014).
Conclusion: Our pilot study provides evidence that the examined polymorphisms were not associated with increased individual susceptibility for HSP, although the GSTM1 genotype proved involved in gastrointestinal manifestations of HSP. For precise evaluation of results, it is necessary to include larger study populations; however, this study offers some essential information for further research.
Funding
Croatian Science Foundation Project IP-2019-04-8822.
ID: 267/06-PT-L-d2C: 16
Poster Presentation (Onsite)
Topics: ADOLESCENT MEDICINE, PUBLIC HEALTH
Keywords: Adolescent health, Primary care professionals, Survey; HEEADSSS
Adolescent behavioral risk screening in primary care: physician’s point of view
Eisner-Fellay, Taslina; Suris, Joan-Carles; Barrense-Dias, Yara
Center for Primary Care and Public Health (Unisanté), Switzerland.
Background: Properly addressing psychosocial risk factors and detecting their presence raises the odds of preventing consequences. Primary care professional training is part of the prevention programs which have been shown to reduce those risks. This study examines physicians’ self-reported risk behavior and social environment screening in adolescents and young adults. It aims to highlight which elements hinder or improve screening abilities among physicians.
Methods: Data were obtained through an online self-reported questionnaire sent out to primary care physicians (PCP) in the French-speaking part of Switzerland in 2018. The final sample considered for analysis included 456 respondents. The questions were directed to child well visits and routine checkups. Participants were asked whether they screened youths from three age groups (10–14 y/o, 15–20 y/o and 21–25 y/o) for the HEEADSSS (Home environment, Education and employment, Eating, peer-related Activities, Drugs, Sexuality, Suicide/mental health, and Safety from injury and violence) topics. Groups were created according to the number of topics screened: none/few (0-1-2); average (3-4-5); above average (6-7-8). Groups were compared on sociodemographic variables, experience regarding adolescent health, discussing confidentiality and barriers to screening (e.g., insufficient consultation time, patient compliance, reimbursement issues, etc. Data were analyzed through a bivariate analysis using Chi-square tests and multinomial logistic regression. At the multivariate level, four models were created.
Results: The majority of physicians partook in preventive screening for 3–5 topics. The most prevalent topics discussed were education (80%) and activities (58%) for the 10–14 y/o; home (64%), education (78%) and activities (66%) for the 15–20 y/o and finally education (70%) and activities (65%) for the 21–25 y/o. Physicians reported the primary consultation motive as well as a lack of available time, as having a high impact on their screening habits. Physicians’ experience in adolescent health and having discussed confidentiality were related to an increase in the number of topics screened for. Having discussed confidentiality remained a significant variable throughout all the models.
Conclusions: Most physicians screen youths preventively for at least three risk behaviors. Barriers such as lack of consultation time and prioritization issues have been found to be critical according to physicians but do not hinder screening habits. Self-efficacy and having discussed confidentiality have been found to be essential factors. Improving physicians’ self-efficacy during training as well as through youth’s feedback on one’s practice, could be useful tools to improve screening habits.
ID: 218/06-PT-L-d2C: 17
Poster Presentation (Onsite)
Topics: RARE DISEASES, HAEMATOLOGY/ONCOLOGY
Keywords: Liver mesenchymal hamartoma, hepatic tumor, infant liver tumor, elevated AFP
Diagnostic challenges of liver mesenchymal hamartoma – case report.
Santos, Mafalda Ferreira1; Leite, Filipa2
1Centro Hospitalar Tondela-Viseu; 2Instituto Português de Oncologia do Porto.
Background: Liver mesenchymal hamartoma (LMH) is a rare, benign tumour that presents as a cystic, slow-growing mass, usually within the first two years of life. Few cases demonstrate abnormal levels of alpha-fetoprotein (AFP).
Case Report: We report a case of a 12-month-old female, previously healthy, that presented to the pediatric emergency department with abdominal distention. Abdominal ultrasound and computed tomography (CT) were performed and revealed a large, intra-peritoneal lesion with a thick wall, multiple cysts of variable size and solid septa. Magnetic resonance imaging (MRI) was also performed. The lesion was surgically resected. Prior to surgery, the alpha-fetoprotein (AFP) was elevated and decreased after operative resection. Histopathology confirmed the diagnosis of LMH.
Learning Points And Discussion: Diagnosis of LMH should be suspected in children under the age of 5 years with a suggestive medical history of abdominal distension. High AFP levels with an infantile hepatic mass may indicate a more malignant process but do not exclude LMH. Surgery is the treatment of choice with an excellent prognosis.
Session
07-OP-V-d2C: Oral Presentations Session 7 - Day 2 - Zone C
Presentations
ID: 198/07-OP-V-d2C: 1
Oral Presentation (Virtual)
Topics: ALLERGY, IMMUNOLOGY & RESPIRATORY
Keywords: Asthma
Dupilumab improves clinical efficacy outcomes in children (6–11 years) with moderate-to-severe asthma and high eosinophils at baseline
Jackson, Daniel J.1; Hamelmann, Eckard2; Roberts, Graham3,4,5; Bacharier, Leonard B.6; Altincatal, Arman7; Gall, Rebecca8; Ledanois, Olivier9; Jacob-Nara, Juby A.10; Radwan, Amr8; Rowe, Paul J.10; Deniz, Yamo8
1University of Wisconsin School of Medicine and Public Health, Madison, WI, USA; 2Children’s Center Bethel, University of Bielefeld, Bielefeld, Germany; 3University of Southampton Faculty of Medicine, Southampton, UK; 4NIHR Southampton Biomedical Research Centre, Southampton University Hospital NHS Foundation Trust, Southampton, UK; 5David Hide Asthma and Allergy Centre, St Mary’s Hospital, Isle of Wight, UK; 6Monroe Carell Jr. Children’s Hospital at Vanderbilt University Medical Center, Nashville, TN, USA; 7Sanofi, Cambridge, MA, USA; 8Regeneron Pharmaceuticals, Inc., Tarrytown, NY, USA; 9Sanofi, Paris, France; 10Sanofi, Bridgewater, NJ, USA.
Background: Children with moderate-to-severe asthma often remain symptomatic despite standard-of-care treatments, and patients with elevated eosinophil levels frequently have increased rates of exacerbations and worse asthma control. In the phase 3 LIBERTY ASTHMA VOYAGE study (NCT02948959), treatment with dupilumab, a fully human monoclonal antibody that blocks the shared receptor component for IL-4 and IL-13, was generally well tolerated and resulted in fewer exacerbations and improved lung function vs placebo in children aged 6–11 years with uncontrolled moderate-to-severe asthma. This post hoc analysis evaluates dupilumab efficacy in patients with baseline blood eosinophils (≥500 cells/µL) enrolled in the VOYAGE study.
Methods: Patients received add-on dupilumab (100/200 mg by body weight at randomization) or matched add-on placebo every 2 weeks (q2w) for 52 weeks. Endpoints included annualized rate of severe exacerbations and least squares mean (LSM) change from baseline in pre-bronchodilator (pre-BD) percent predicted forced expiratory volume in one second (ppFEV1).
Results: In participants with baseline blood eosinophils ≥500 cells/µL, add-on dupilumab significantly lowered annualized exacerbation rates (0.249 [95% CI 0.156–0.397]; n = 126) compared with add-on placebo (0.749 [0.453–1.239]; P < 0.001; n = 48) and significantly improved pre-BD ppFEV1 vs placebo at Week 12 (LSM difference [95% CI] 6.47 percentage points [2.27–10.66]; P < 0.01) and at Week 52 (LSM difference [95% CI] 7.98 percentage points [2.17–13.78]; P < 0.01) at Week 52 (Figure ).
Conclusion: Dupilumab significantly reduced severe exacerbations and improved lung function as assessed by pre-BD ppFEV1 vs placebo in children with moderate-to-severe asthma and baseline blood eosinophils ≥500 cells/µL.
ID: 168/07-OP-V-d2C: 2
Oral Presentation (Virtual)
Topics: ALLERGY, IMMUNOLOGY & RESPIRATORY
Keywords: Asthma
Dupilumab long-term safety, clinical efficacy, and impact on biomarker levels in children with asthma: liberty asthma excursion
Bacharier, Leonard B1; Maspero, Jorge F2; Katelaris, Constance H3,4; Fiocchi, Alessandro G5; Gagnon, Remi6; de Mir, Ines7; Guilbert, Theresa8; Jackson, Daniel J9; Li, Ning10; Akinlade, Bolanle11; Laws, Elizabeth10; Mannent, Leda P12; Maloney, Jennifer11; Tawo, Kelsey10; Khokhar, Faisal A11; Hardin, Megan13; Abdulai, Raolat M13; Lederer, David J11; Robinson, Lacey B13.
1Monroe Carell Jr Children’s Hospital at Vanderbilt, Nashville, TN, USA; 2Fundación CIDEA, Buenos Aires, Argentina; 3Campbelltown Hospital, Campbelltown, NSW, Australia; 4Western Sydney University, Sydney, NSW, Australia; 5Bambino Gesù Children’s Hospital IRCCS, Rome, Italy; 6Clinique Spécialisée en Allergie de la Capitale, Quebec, QC, Canada; 7Hospital Universitari Materno infantil Vall d’Hebron, Barcelona, Spain; 8Cincinnati Children’s Hospital and University of Cincinnati, Cincinnati, OH, USA; 9University of Wisconsin School of Medicine and Public Health, Madison, WI, USA; 10Sanofi, Bridgewater, NJ, USA; 11Regeneron Pharmaceuticals, Inc., Tarrytown, NY, USA; 12Sanofi, Chilly-Mazarin, France; 13Sanofi, Cambridge, MA, USA.
Background: Dupilumab, a fully human monoclonal antibody, blocks the shared receptor component for interleukin (IL) 4 and Il-13. The efficacy and safety of dupilumab in 6–11-year-old children with uncontrolled, moderate to severe asthma was demonstrated up to 52 weeks in VOYAGE (NCT02948959). The EXCURSION open-label extension study (NCT03560466) assessed dupilumab long-term safety and efficacy in children who completed VOYAGE.
Methods: 365 patients rolled over from VOYAGE into EXCURSION and received add on SC dupilumab 100/200 mg every two weeks (q2w) or 300 mg q4w (body-weight tier based) for 52 weeks. Treatment-emergent adverse events (TEAE), annualized asthma exacerbation rate (AER), and change from parent study baseline (PSBL) in percent predicted (pp) FEV1, ppFVC, FEV1/FVC, ppFEF 25–75%, blood eosinophil count and total serum IgE were assessed.
Results: Dupilumab was well tolerated, and the safety profile was consistent with the parent study. 85 (68.0%; placebo/dupilumab) and 147 (61.3%; dupilumab/dupilumab) of all EXCURSION patients experienced TEAEs, with 3 (1.3%) in the dupilumab/dupilumab group leading to treatment discontinuation. Median blood eosinophil count (Q1:Q3) decreased throughout EXCURSION to below the PSBL at Week 52, by −30 (−260:70) cells/µL for placebo/dupilumab (n = 105), and −140 (−410:10) cells/µL for dupilumab/dupilumab (n = 191). Total serum IgE declined substantially throughout EXCURSION, with a median percent change from PSBL to Week 52 of −80.0% (278.0 IU/mL; n = 114) for placebo/dupilumab and −89.9% for dupilumab/dupilumab (339.0 IU/mL; n = 219). The unadjusted AER for patients with type 2 asthma (baseline blood eosinophils ≥150 cells/µL or FeNO ≥20 ppb) was 0.124 for placebo/dupilumab and 0.118 for dupilumab/dupilumab (). Mean change from PSBL ppFEV1 (%) in EXCURSION at Weeks 2/52 was +8.7/+9.4 in placebo/dupilumab (mean PSBL 78.7%), and +11.3/+12.6 in dupilumab/dupilumab (mean PSBL 76.9%) (). Mean change from PSBL ppFVC (%) in EXCURSION Weeks 2/52 was +3.7/+4.4 in placebo/dupilumab (mean PSBL 92.7%), and +5.4/+6.9 in dupilumab/dupilumab (mean PSBL 91.9%). Mean change FEV1/FVC (%) from PSBL at EXCURSION Weeks 2/52 was +4.6/+4.5 in placebo/dupilumab (mean PSBL 74.2%), and +5.6/+5.4 in dupilumab/dupilumab (mean PSBL 73.4%). Mean change from PSBL ppFEF25-75% (L/s) at EXCURSION Weeks 2/52 was +13.5/+15.5 in placebo/dupilumab (mean PSBL 55.6 L/s), and +17.9/+17.4 in dupilumab/dupilumab (mean PSBL 53.8 L/s).
Conclusions: Long-term use of dupilumab was well tolerated, with a decline in type 2 biomarker levels, including blood eosinophils and total serum IgE. Efficacy observed in VOYAGE among patients with type 2 asthma was sustained in EXCURSION over an additional 52 weeks, including rapid improvement in patients initiating dupilumab.
ID: 142/07-OP-V-d2C: 3
Oral Presentation (Virtual)
Topics: PUBLIC HEALTH
Keywords: oral health, general anaesthetics, waiting times
Impact of waiting times for paediatric dental general anaesthetic on patient quality of life
Grange, Esme
Salisbury District Hospital, UK
Background: This study investigated the effect of long waiting times associated with COVID-19 on children scheduled to have dental general anaesthetics at Salisbury District Hospital. Waiting times, pain, sleep, social factors, missed school and work, antibiotic use, previous dental general anaesthetics and treatment changes were recorded.
Method: Parents were invited to complete a survey based on the Child Oral Health Quality of Life Questionnaire immediately after their child’s treatment.
Results: 49 children were included. The mean waiting time was 312.5 days. During the waiting period, 80% of parents stated that their child experienced pain, 73% recorded eating and drinking difficulty and 65% recorded sleep disturbance. 78%, 59% & 61% stated that their child’s mood, social behaviour and concentration were affected, respectively. 43% of children had missed school, 29% of parents missed work, and 45% of children received antibiotics. The majority (69%) of treatments remained unchanged. 10% had received a previous dental general anaesthetics.
Conclusion: Waiting times are exceedingly long at Salisbury District Hospital but vary greatly. Many children are suffering during their wait, and parents missing work may have broader implications for the community. Actions have been implemented to improve the high repeat dental general anaesthetic rate; however, greater access to community and paediatric services would be beneficial.
ID: 170/07-OP-V-d2C: 4
Oral Presentation (Virtual)
Topics: ALLERGY, IMMUNOLOGY & RESPIRATORY
Keywords: Interleukin 6, nephrotic syndrome, genotype, polymorphism
Interleukin-6 gene polymorphism in kuwaiti Arab children with idiopathic nephrotic syndrome
Aleisa, Amal A.; Alrushood, Maysoun; Kashyap, Sumedha; Haider, Mohammad
Kuwait university-college of medicine, Kuwait.
Background: Idiopathic Nephrotic syndrome (INS) is an immune-mediated disease with unresolved theories of pathogenesis. IL-6 is a vital pro-inflammatory cytokine involved in etiology of many autoimmune diseases. Gene polymorphism of IL-6 controls the expression and function of IL-6 and, therefore, might have an effect on the pathogenesis and clinical pattern of INS. (1) This study aims to determine the frequency and association of IL-6 gene polymorphisms with INS and its effect on the disease pattern in Kuwaiti children of Arab ethnic background.
Methods: Genotypes of the IL-6 gene polymorphisms were analyzed using PCR-RFLP in 157 INS patients and 64 age and sex- matched controls. Clinical data of all subjects were reviewed.
Results: A total of 157 INS (134 steroid-sensitive and 23 steroid-resistant) patients with a mean age was 7.6 ± 4.3 years were studied. Male: Female ratio was 2:1. The CC genotype of IL-6 gene polymorphism was detected in 75% of the INS patients compared to 68% of the controls (P = 0.42). The heterozygous GC genotype was detected in 19% of INS patients compared to 28% of the controls (P = 0.19). The GG genotype was detected in 6% of INS patients and 3% of the controls (P = 0.52). The C-allele frequency in homozygous and heterozygous forms was found in 84.7% of INS patients compared to 82.8% of the controls (P = 0.72). The G-allele frequency in homozygous and heterozygous forms was found in 15.2% of INS patients compared to 17% of the controls (P = 0.72). No significant difference was found in any of the allele frequencies between SS and SR sub-groups when compared with each other or when compared to the controls.
Conclusion: Our data show no role of IL-6 gene polymorphisms on the clinical pattern or response to steroids in Kuwaiti children with INS.
ID: 258/07-OP-V-d2C: 5
Oral Presentation (Virtual)
Topics: PUBLIC HEALTH, COVID-19
Keywords: HBSC, gender identity, mental health, trans, gender non-conforming
Mental Health of gender-conforming and non-conforming Adolescents in Luxembourg
Heinz, Andreas1; Catunda, Carolina2; Willems, Helmut2
1IU Internationale Hochschule, Germany; 2University of Luxembourg.
Background: In industrialised countries, there is a growing group of adolescents whose gender identity does not match the sex identified at birth. However, in many health and well-being surveys, gender non-conforming adolescents cannot be identified as a subgroup because gender identity is not asked. In the present study, sex and gender identity were asked separately to determine whether gender-conforming adolescents differ from gender non-conforming adolescents in terms of their health and well-being.
Methods: In the Luxembourg HBSC 2022 survey, students in secondary schools were selected at random and surveyed in the classroom (N = 7,130). To assess the congruence of sex and gender identity, biological sex at birth was asked (male or female) and compared with gender identity (boy, girl, none/other). Health and well-being were measured using standard HBSC instruments (e.g., PSS-4, WHO-5; GAD-2 HBSC-SCL).
Results: Congruence of sex and gender identity was determined for 6427 students aged 12–18. In 3.5% of the students, both did not match (i.e. gender non-conforming). The percentage of gender non-conforming students depended on the language of the questionnaire (English 9.4%, German/French 3.2%), sex at birth (male 1.4%, female 5.4%), but not age. Gender non-conforming students rated their health more often as “poor” compared to their gender-conforming peers (9.9% vs 2.2%). They were much more likely to have multiple psychosomatic complaints (82.9% vs 52.2%), higher levels of stress (PSS-4 mean: 9.8 versus 7.2) and lower life satisfaction (Cantril mean: 5.6 vs 7.2). In addition, they were more likely to have felt lonely in the past 12 months, to have shown symptoms of depression, and to have planned and attempted suicide. Gender non-conforming students were also more likely to report that Covid-19 had a negative impact on various areas of their lives than gender-conforming students (e.g., on mental health and relationship with family and friends).
Conclusions: The association between the language of the questionnaire and not identifying with the sex identified at birth suggests that gender (non-) conformity is culturally shaped. The mental health of gender non-conforming students is lower in all aspects examined. To analyse the health and well-being of gender non-conforming youth, it is important to ask about both sex and gender identity in surveys.
ID: 215/07-OP-V-d2C: 6
Oral Presentation (Virtual)
Topics: HAEMATOLOGY/ONCOLOGY, COVID-19
Keywords: anti-SARS-CoV-2 vaccine; child; swelling; hemangioma
Not everything is as it seems …
Azevedo, Inês Alexandra1; Torrão, Helena2; Maia, Ana3; Maia, Iris3; Costa, Miguel1
1Pediatric Department of Centro Hospitalar de Entre Douro e Vouga, Portugal; 2Radiology Department of Instituto Português Oncologia do Porto Francisco Gentil, Portugal; 3Pediatric Department of Instituto Português Oncologia do Porto Francisco Gentil, Portugal.
Background: The anti-SARS-CoV-2 vaccine was administered to millions of people in a short time, placing challenges in monitoring adverse reactions. The appearance of signs/symptoms with a temporal relationship with the vaccine can interfere with their assessment and with the diagnosis of other pathologies. The most frequently described effects are mostly benign, such as headache, fever, myalgia, arthralgia, asthenia, adenopathy and/or pain.
Case Presentation Summary: An eight-year-old girl, previously healthy, was observed by a Pediatrician due to a 4 weeks-long left axillary swelling noticed 2 weeks after the administration of 1st dose of the anti-SARS-CoV-2 vaccine. She doesn´t have any other symptoms. Trauma and recent infectious were denied. On physical examination, she had an oval mass, with 5 × 5 cm, hard, painless, adherent to the deep planes, and without inflammatory signs. (1) Analytical study was normal, and axillary ultrasound showed an oval mass, with a heterogeneous texture, with multiple septations and hypoechoic elements, suggesting a probable atypical adenopathy conglomerate in the context of a vaccine reaction. Therefore, she was medicated with amoxicillin + clavulanic acid and anti- inflammatory for one week. (2) Upon re-evaluation, as the mass presented similar characteristics, the case was discussed with Pediatric Oncology and was referred for evaluation by the specialty. Axillary ultrasound was repeated and showed heterogeneous formation, with cystic foci and areas of vascularization with rare foci of calcification, and MRI confirmed a lesion suggestive of low-flow vascular malformation. The child was submitted to surgical excision, and histology showed intramuscular hemangioma.
Discussion: Hemangiomas are benign tumours of the vascular endothelium characterized by a growth phase and an involution phase. Despite being benign and self-limiting in nature, some hemangiomas can cause complications. (1) This clinical case highlights the fact that, despite the temporal relationship with the anti-SARS-CoV-2 vaccine, in the face of persistent mass and warning signs, other etiologies should always be excluded.
ID: 235/07-OP-V-d2C: 7
Oral Presentation (Virtual)
Topics: INFECTIOUS DISEASES
Keywords: Candida spp, pediatric invasive candidiasis, mortality, risk factors
Pediatric Invasive Candidiasis: a 12-year retrospective study in a tertiary care hospital
Pedrosa, Inês1; Monteiro, Teresa2; Almeida, Teresa3; Faria, Carolina4; Reis-Melo, Ana4; Tavares, Margarida4
1Department of Pediatrics, Centro Hospitalar de Leiria, Portugal; 2Department of Pediatrics, Centro Hospitalar Universitário do Algarve, Portugal; 3Department of Clinical Pathology, Centro Hospitalar Universitário São João, Portugal; 4Pediatric Infectious Diseases and Primary Immunodeficiencies Unit, Centro Hospitalar Universitário São João, Portugal.
Background: Invasive candidiasis (IC) is a major cause of morbimortality, mainly among children with underlying medical conditions. Rates of IC are increasing worldwide, probably due to the prolonged survival of immunocompromised patients and the increased use of invasive devices. We aim to describe the epidemiology and clinical disease of IC in a tertiary pediatric hospital.
Methods: Retrospective audit of culture-confirmed Candida isolates from a tertiary hospital’s Microbiology department over a 12- year period. Patients’ demographic, clinical characteristics and causative Candida species were analyzed. We divided patients into age groups: >28 days to <1 year (infants) and 1 to <18 years of age (children/adolescents). The study period was divided into 2 periods (2010–2015; 2016–2021) to analyze trends over time.
Results: There were 40 potential episodes of IC, 7 of which were excluded (6 contaminants; 1 without available chart information). Overall, 33 IC episodes were included (31 bloodstream, 1 CSF and 1 pleural effusion isolate). The median age was 21 months (39.4% infants; 60.6% children/adolescents), with a predominance of the female sex (57.6%). At diagnosis, most patients were in the general pediatric ward (39.4%), ICU (27.3%) or haematology-oncology unit (18.2%). The median length of stay was 44 days (range 4–788). Almost half of the patients required admission to ICU during their hospital stay (48.5%). The most common species were Candida parapsilosis (45.5%) and Candida albicans (39.4%). The predisposing factors for IC were CVC use (93.9%), parenteral nutrition (51.5%), bacteremia (57.5%), mechanical ventilation (39.4%), immunosuppression (33.3%), major surgery (33.3%) and neutropenia <500/uL (12.1%). The comorbidities more frequently identified were malignancy (33.3%), prematurity (27.3%) and gastrointestinal disease (12.1%). Antifungal treatment was given in 90.9% of cases (66.7% Amphotericin B, 16.7% Fluconazole), with a mean duration of 23 days (range 8–45). The all-cause mortality rate at 30 days was 21.2% (n = 7), and no significant differences between age groups and time periods were found. Higher mortality rates were reported among patients in ICU (p = 0.046), with concomitant bacteremia (p = 0.041) and recovering from major surgery (p = 0.049).
Conclusions: These results provided us with an insight into the clinical and fungal epidemiology of IC in our hospital. Remarkably, non-albicans Candida species were the leading cause of IC (60.6%), with C. parapsilosis being responsible for 45.5% of total cases, independently of ward type and age groups. The overall mortality rate is similar to other studies in pediatric settings, and the significant risk factors related with the mortality rate were ICU hospitalization, bacteremia and major surgery.
ID: 130/07-OP-V-d2C: 8
Oral Presentation (Virtual)
Topics: INFECTIOUS DISEASES, EMERGENCY PEDIATRICS
Keywords: Mastoiditis, Brain abscess, Otogenic infection
Primary conservative management of a paediatric otogenic cerebellar abscess
Qureshi, Muhammad Hamza1; Elbadawey, Morouge2; Reda, Mohamed3
1Darlington Memorial Hospital, UK; 2St George’s Medical School; 3Sheikh Shakhbout Medical City.
Background: Mastoiditis, dural sinus thrombosis and intracranial abscess formation are complications of otitis media. Traditionally intradural suppurative collections are drained by neurosurgeons, with the primary otogenic source of infection addressed either simultaneously or soon afterwards by otorhinolaryngologists. A new trend in neurosurgery is to treat small brain abscesses conservatively, providing drainage of the primary site. We present the first report of an otogenic brain abscess in a child successfully treated with conservative management of the collection.
Case Presentation Summary: A previously healthy 4-year-old girl presented with right-sided otomastoiditis. After initially responding to IV antibiotics, her condition deteriorated, and imaging revealed a right-sided small cerebellar abscess and lateral sinus thrombosis. The otomastoiditis and venous sinus thrombosis were surgically treated, but the cerebellar abscess was managed with further IV antibiotics and completely resolved at 6 months.
Learning Points Discussion: Intracranial and cranial complications should be considered in any case presenting with mastoiditis as a complication of acute otitis media. Changes in neurosurgical opinion are altering the preferred management of otogenic brain abscesses. This case demonstrates a small cerebellar abscess can be successfully managed conservatively in a child provided adequate drainage of the infective source.
ID: 197/07-OP-V-d2C: 9
Oral Presentation (Virtual)
Topics: NUTRITION & DIETS
Keywords: young children formula, L. reuteri, gastrointestinal tolerance
Real-world effectiveness of young child formula containing Limosilactobacillus reuteri on gastrointestinal tolerance and related behaviors in toddlers: a cross-sectional observational study
Estorninos, Elvira1; Cohen, Sarah2; Reichert, Heidi2; Lebumfacil, Jowena3; Jankovic, Ivana4; Chen, Yipu4; Egli, Delphine4
1Las Pinas Doctors Hospital, Las Pinas City, Philippines; 2EpidStrategies, Katy, TX, USA; 3Wyeth Nutrition, Makati City, Philippines; 4Société Des Produits Nestlé SA, Switzerland.
Background: Gastrointestinal tolerance is an important measure of digestive comfort. This study assessed the effectiveness of young child formula (YCF) containing Limosilactobacillus (previously Lactobacillus) reuteri (DSM 17938) (LR) on digestive comfort in a real-world setting.
Methods: A cross-sectional, single timepoint, interview-based observational study was conducted among mothers of healthy toddlers born full-term. Children aged 12–36 months, free of any major chronic illness or food allergy, had no major changes to their current feeding regimen for at least 2 weeks prior to enrollment. Gastrointestinal tolerance, associated behaviours and stool characteristics were collected via the Gut Comfort Questionnaire. Toddlers were assigned to feeding groups based on their current feeding regimen, including YCF with LR (N = 150), YCF containing other pre/probiotics (N = 61), YCF containing no pre/probiotics (N = 173), and non-YCF users (N = 38). Mean differences (MD) and 95% confidence intervals (CI) were computed using ANOVA models.
Results: The Gut Comfort composite score was significantly lower, indicating lower gastrointestinal distress, in the YCF with LR group compared to non-YCF users (MD = −1.83, 95% CI: −3.20; −0.45, p = 0.01), YCF users with other pre/probiotics (MD = −1.29, 95% CI: −2.44; −0.14, p = 0.028), and YCF without pre/probiotics (MD = −1.41, 95% CI: −2.26; −0.57, p = 0.001). For individual tolerance measures, children receiving YCF with LR had lower parental reports of fussiness and irritability, constipation, and difficulty passing stools, compared with non-YCF users; lower reports of constipation and difficulty passing stools, compared with users of YCF containing other pre/probiotics; and lower reports of fussiness and irritability, constipation, problematic sleeping, diarrhea and gassiness, compared with users of YCF with no pre/probiotics. The frequency of crying was the lowest in the YCF with LR users compared with all other groups, and the appetite scale was the highest compared to other groups except non-YCF users. Stool consistency scores were similar between YCF with LR and non-YCF users, but higher (i.e., harder) for YCF with LR users when compared with YCF containing other pre/probiotics (MD = 0.21, 95% CI: 0.01; 0.41, p = 0.042) and YCF with no pre/probiotics users (MD = 0.15, 95% CI: 0.01; 0.30, p = 0.041). The majority of stools passed by children in all feeding groups were formed. Caregivers’ opinion of YCF with LR was overwhelmingly “Very good” to “Excellent” (97.6% and 96%, respectively).
Conclusions: In this real-world observational study, children consuming YCF with LR had better digestive comfort and associated behaviours than non-YCF users and children consuming YCF with other pre/probiotics or no pre/probiotics. YCF with LR also had high satisfaction ratings from caregivers.
ID: 162/07-OP-V-d2C: 10
Oral Presentation (Virtual)
Topics: NEUROLOGY
Keywords: Friedreich’s ataxia; respiratory function
Respiratory function in Friedreich’s Ataxia
Martinuzzi, Michela2; Vinante, Elena1; Colombo, Elena1; Paparella, Gabriella1; Martinuzzi, Andrea1
1IRCCS “E. Medea”, Department of Neurorehabilitation, 31015 Conegliano, Italy; 2Sandwell and West Birmingham NHS tFoundations trust, UK.
Background: Friedreich’s ataxia (FRDA) is an inherited, rare, progressive disorder in children and young adults. It is characterized by ataxia, loss of gait, scoliosis, cardiomyopathy, dysarthria, and dysphagia, with reduced life expectancy. Alterations of respiratory dynamics and parameters are frequently observed. However, there are few dated studies with small cohorts in the literature. (1) We report the objective analysis of the respiratory condition of both early and late-stage FRDA patients, looking for correlations with the motor, skeletal, speech and genetic aspects of this condition.
Materials and Methods: This retrospective observational study is based on the collection of clinical and instrumental respiratory data of 44 subjects with molecularly defined FRDA attending a tertiary rehabilitation centre in Italy. The following parameters were recorded: FVC (forced vital capacity), FEV1 (forced expiratory volume in 1s), TI (Tiffeneau index), MIP (maximal inspiratory pressure), MEP (maximal expiratory pressure), PCF (peak cough flow) and PEF (peak expiratory flow). The analysis was carried out using Pearson’s correlation test, ANOVA and Post Hoc tests.
Results: Data show the presence of a recurrent restrictive pattern of respiratory dysfunction, with a reduction of forced vital capacity (2.84 L +- 0.86, 74.83% +- 18.21 of predicted) and of flow and pressure parameters. 80% of participants were below the minimum values for MEP and 66.7% for MIP. Cough was found to be potentially inefficient in 15/44. 6 patients were found to have mild obstructive sleep apnoea (OSA) and one severe OSA. The severity of the respiratory condition correlates with disease severity (p < 0.001 for FVC, FEV1 and MEF) duration (p > 0.04 for FVC), pneumophonic capacity (p > 0.001 for FVC and FEV) and with severity of the thoracic scoliotic curve (p < 0.020). There was no correlation between respiratory measures and GAA expansion.
Conclusion: The complex condition of incoordination and hyposthenia in FRDA affects daytime and night-time respiratory efficiency. We show that the respiratory deficit and the inefficiency of cough are a prevalent clinical problem deserving of early consideration.
ID: 200/07-OP-V-d2C: 11
Oral Presentation (Virtual)
Topics: EMERGENCY PEDIATRICS
Keywords: Emergency, Febrile, Oncology, CXR
The role of CXR in investigation of febrile paediatric oncology patients presenting to the emergency department
Guinness, Freya; Abdul Nabi, Sarah; El Kebbi, Ola; Khamis, Mohamad; Tamim, Hani; Sawaya, Rasha D.
HSE, Ireland.
Introduction: Fever is a common presenting complaint to the emergency department (ED) in paediatric oncology patients. While bacteraemia has been extensively studied in this population, pneumonia has not. Several studies suggest that chest x-ray (CXR) does not have a role in the investigation of neutropaenic fever in the absence of respiratory symptoms, however, this has not been studied in non-neutropaenic patients.
Aim: We aimed to look at the diagnostic yield of CXRs in all paediatric oncology patients, irrespective of their ANC level, presenting with fever to the ED, as well as to identify predictive features of radiographic pneumonia.
Methods: This is a secondary analysis of a retrospective cohort study of acutely febrile paediatric cancer patients younger than 18 years, presenting to a tertiary center from 2014 to 2018. We included one randomly selected febrile visit per patient. We defined fever as a single oral temperature ≥38°C. Data on patient characteristics and outcomes were collected. Our primary outcome was radiographic pneumonia; our secondary outcome was whether a CXR was done or not. Definite radiographic pneumonia was defined as a report mentioning a consolidation, pleural effusion, infiltrate, or pneumonia. Possible radiographic pneumonia was defined as a report with “infiltrate VS atelectasis”, or possible pneumonia mentioned by the radiologist. Anything else was considered negative for pneumonia. Statistical analysis was done using SPSS, where both outcomes were analysed.
Results: We reviewed a total of 664 charts and included data from 342 febrile pediatric patients in our analysis. Of these, 64 (N = 18.7%) had a CXR performed. 16 (N = 25%) had radiographic pneumonia while 48 (N = 75%) did not. Patients were significantly more likely to have a CXR performed if they presented with upper respiratory tract symptoms or cough (p < 0.001 for both). Patients were also more likely to have a CXR if they were asymptomatic upon admission to the PED (p < 0.001) or if they had abnormal lung auscultation at the bedside (p = 0.003). However, neither cough nor shortness of breath nor an abnormal lung exam were significant predictors of a positive CXR (0.17, 0.43 and 1, respectively). Patients with radiographic pneumonia were found to be significantly older (4.29 vs 6 years, p = 0.03), with a longer time since their last chemotherapy (15 vs 7 days, p = 0.005), and were given intravenous (IV) bolus in the PED (87.5% vs 56.3%, p = 0.02).
Conclusion: In our sample, CXR was not commonly performed in the initial investigation of febrile PED cancer patients unless respiratory symptoms or abnormal lung examination were noted. However, these were not significant predictors of radiographic pneumonia. Further studies are needed to identify better predictors of pneumonia in this high-risk population.
ID: 214/07-OP-V-d2C: 12
Oral Presentation (Virtual)
Topics: GASTROENTEROLOGY, EMERGENCY PEDIATRICS
Keywords: abdominal pain; adolescent; epiploic appendagitis
Acute abdominal pain: not always so obvious
Azevedo, Inês Alexandra; Cardoso, Rosa; Mendes, Joana; Almeida, Claudia; de Figueiredo, Catarina Matos; Pereira, Magalys
Pediatric Department of Centro Hospitalar de Entre Douro e Vouga, Portugal.
Background: Acute abdominal pain is a frequent cause of seeking medical care in Pediatrics. The origin has a wide spectrum of possibilities, and it is important to recognize its etiology for the correct diagnostic and therapeutic approach.
Case Presentation Summary: A 17-year-old male with obesity (BMI 35.2 kg/m2), insulin-resistance (HOMA-IR 13.2) and vitamin D deficiency under treatment with metformin and vitamin D was observed at the Pediatric Emergency Department due to abdominal pain in the lower quadrants since the day before. Intestinal transit and diuresis are maintained with normal characteristics. No history of fever or recent infections. No other associated symptoms. (1) On physical examination, he presented a globose abdomen with adipose panniculus, and the left iliac region was painful, with defense. An enema was performed, with an output of a moderate amount of stool. For maintaining abdominal pain, an analytical study was performed without significant changes. The abdominal ultrasound documented a hyperechogenic area in the left iliac region, with 4.5 × 2 cm, in the adipose planes adjacent to the anterior abdominal wall. The abdomen and pelvis computed tomography confirmed the diagnosis of epiploic appendagitis. Outpatient treatment with anti-inflammatory and esomeprazole was recommended. He presented good clinical evolution, with a complete resolution of symptoms in 2 weeks.
Discussion: Epiploic appendagitis is normal outpouchings of peritoneal fat on the surface of the colon. The evolution is usually benign, self-limited, and complete resolution usually occurs without surgical intervention. This is usually diagnosed incidentally in children undergoing imaging for acute abdominal pain. The differential diagnosis consists of other causes of acute abdominal pain. So, inaccurate diagnosis can lead to unnecessary hospitalizations, antibiotic therapy, and surgical intervention.
ID: 164/07-OP-V-d2C: 13
Oral Presentation (Virtual)
Topics: GENERAL PEDIATRICS, ENDOCRINOLOGY
Keywords: diabetes mellitus, neonatal diabetes, sulphonylurea
Sweet babies: fifteen year experience of neonatal diabetes in a tertiary Irish paediatric diabetes centre
Woon, Yuxin; Holcroft, Lorna; Somers, Eric; Cody, Declan; O’ Connell, Susan M
Department of Diabetes & Endocrinology, Children’s Hospital Ireland at Crumlin, Dublin, Ireland.
Background: Neonatal diabetes mellitus (NDM) is a rare form of diabetes presenting before six months of age.1 It is typically a monogenic form of diabetes and presents as permanent neonatal diabetes mellitus (PNDM), transient neonatal diabetes mellitus (TNDM) or syndromic neonatal diabetes. Accurate genotyping is important for prognostic counselling and as those with a mutation in genes encoding subunits of the KATP channel may be responsive to treatment with sulphonylureas.
Aim: To review the phenotypes, genotypes and management of eight children with NDM at the largest Irish paediatric diabetes centre. METHODS: We interrogated our database for cases of NDM with known genetic mutations between 2006–2021.
Results: Eight cases of NDM were treated—4 each of PNDM and TNDM. All 4 PNDM cases were due to a KCNJ11 gene mutation. 3 TNDM cases were due to 6q24 methylation defects, and 1 due to an ABCC8 mutation. 5 cases were responsive to sulphonylurea therapy.
Discussion: Treatment with sulphonylurea was more successful in cases where the medication was started at a younger age. Cases with 6q24 methylation defects presented with a similar phenotype of IUGR, prematurity and TNDM. Fifty per cent of cases reviewed presented diabetic ketoacidosis, all of which had activating KATP channel mutations. The genetic diagnosis had implications for the family members of our patients. All of our TNDM were off insulin within the first year of life and given advice on possible recurrence of diabetes mellitus later in life.
Conclusion: Due to increased awareness of personalised medicine, early genetic diagnosis of NDM guides treatment and informs prognosis and future risk for the patient and their families.
Session
08-PT-L-d2D: Poster Presentations Session 8 - Day 2 - Zone D
Presentations
ID: 255/08-PT-L-d2D: 1
Poster Presentation (Onsite)
Topics: RARE DISEASES, ENDOCRINOLOGY
Keywords: SPINK1 mutation, morbid obesity, pancreatitis
Combined SPINK1 mutations induce early onset severe chronic pancreatitis in a morbidly obese child
Abass, Maha1; Al Shamsi, Aisha2; Jan, Iftikhar3,4; Yasin Masalawala, Mohammed Suhail5; Deeb, Asma1,4
1Paediatric Endocrinology Division, Sheikh Shakhbout Medical City, Abu Dhabi, UAE; 2Clinical Genetics Department, Tawam Hospital, Al Ain, UAE; 3Paediatric Surgery Division, Sheikh Shakhbout Medical City, Abu Dhabi, UAE; 4College of Medicine and Health Sciences, Khalifa University of Science and Technology, Abu Dhabi, United Arab Emirates.; 5Clinical Trial Unit, Sheikh Shakhbout Medical City, Abu Dhabi, UAE.
Background: The most frequent causes of pancreatitis classically have been known to be gallstones or alcohol. However, genetics can also play a key role in predisposing patients to both chronic and acute pancreatitis. The serine protease inhibitor Kazal type 1 (SPINK 1) gene is known to be strongly associated with pancreatitis. Patients with these underlying genetic mutations can have severe diseases with a high morbidity rate and frequent hospitalization.
Case Presentation Summary: We report an Arab girl who presented with acute pancreatitis at the age of 7 years, progressing to recurrent chronic pancreatitis over a few years. She had severe obesity from the age of 4 years and developed type 2 diabetes at the age of 12. She had normal biliary system anatomy. Genetic analysis showed that she had combined heterozygous mutations in the SPINK1 gene (SPINK1, c.101A>G p.(Asn34Ser) and SPINK1, c.56–37 T > C). Her parents were first-degree cousins, but neither had obesity. Mother was detected to have the same mutations. She had type 2 diabetes but never presented with pancreatitis. This case is the first to be reported from the Arab region, with these combined mutations leading to recurrent chronic pancreatitis. It illustrates the importance of diagnosing the underlying genetic mutation in the absence of other known causes of pancreatitis. Considering the absence of pancreatitis history in the mother who did not have obesity but harboured the same mutations, we point out that severe obesity might be a triggering factor of pancreatitis in the presence of the mutations in the SPINK1 gene in this child. While this is not an assumption from a single patient, we show that not all carriers of this mutation develop the disease, even within the same family. Triggering factors like severe obesity might have a role in developing the disease.
Learning Points Discussion: Acute recurrent pancreatitis and chronic pancreatitis are uncommon in children but might be underdiagnosed. Biliary tract anomalies and dyslipidaemias are known causative factors for pancreatitis, but pancreatitis can be seen in children with intact biliary system. Genetic diagnosis should be sought in children with pancreatitis in the absence of known underlying predisposing factors. SPINK1 mutations can predispose to early-onset severe recurrent pancreatitis and acute pancreatitis.
ID: 213/08-PT-L-d2D: 2
Poster Presentation (Onsite)
Topics: ENDOCRINOLOGY, NEONATOLOGY
Keywords: Endocrinology; Neonatology; Congenital Adrenal Hyperplasia; Genital Ambiguity; Salt-wasting Crisis
Congenital adrenal hyperplasia in the neonatal period - a case report
Aguiar, Barbara Ribeiro1; Sutre, Ana Filipa2; Bethencourt, Noslen3; Oliveira, Vanusa4; Fernandes, Djamila3; Sanches, Mitza3
1Pediatric Department, Beatriz Angelo Hospital, Portugal; 2Pediatric Department, Santarem Hospital, Portugal; 3Pediatric Department, Agostinho Neto University Hospital, Praia, Santiago Island, Cape Verde; 4Internal Medicine Department, Agostinho Neto University Hospital, Praia, Santiago Island, Cape Verde.
Background: Congenital adrenal hyperplasia (CAH) is an inherited autosomal recessive disorder caused by a deficit of enzymes involved in steroidogenesis. The diagnosis can be suspected in the newborn in the presence of genital ambiguity or clinical signs suggestive of a salt-wasting crisis.
Case Presentation Summary: We present the case of a newborn who was the first child from healthy, young and non- consanguineous parents, with adequate pregnancy surveillance. No chronic diseases were running in the family. (1) The obstetric ultrasounds apparently didn’t show changes, and it has been identified as a female fetus. Eutocic delivery in Cape Verde at 39 weeks gestation, Apgar scores 9 at 1st minute and 10 at 5th minute. The physical examination revealed genital ambiguity. The abdominal ultrasound showed a uterus with adequate characteristics and a bilateral inguinal canal with hypoechoic images of 9x3mm and 9x2mm—“adenopathies or testicles”. The patient was discharged home with the indication for follow-up in Endocrinology and Neonatology appointments. (2) At 19 days of life, the patient presented to the emergency department with severe electrolyte imbalance. The parents reported a three-day history of poor feeding, vomiting, lethargy and hypotonia. No fever was noted. The blood test showed hyponatraemia (Na+ 107 mmol/L), hyperkalaemia (K + 8.1 mmol/L) and glycemia 64 mg/dL. A probable diagnosis of CAH with a salt-wasting crisis was made, and the newborn commenced treatment. Clinical and analytical stability was verified 48 hours after the start of treatment. The karyotype was 46,XX and the diagnosis of CAH secondary to 21-hydroxylase (21-OH) deficiency was confirmed by molecular studies (basal 17α-hydroxyprogesterone 38.6 ng/mL; normal value 7.06 ± 3.78 ng/mL). The newborn was discharged home with hydrocortisone, fludrocortisone and sodium chloride. At 9 months of age, under treatment, the patient is clinically well and maintains genital ambiguity, with a phallus of 2 cm (Figure ). The ultrasound was not repeated, and the patient is awaiting surgery.
Learning Points Discussion: Genital ambiguity is associated with the simple virilizing type of 21-OH deficiency. The classic form of CAH with salt-wasting should be suspected in the presence of hypotonia, vomiting and diarrhea between the first and fourth week of life. Substitution treatment can be life-saving and should be immediately instituted in any neonate when there is a suspicion of an acute salt-wasting crisis.
ID: 122/08-PT-L-d2D: 3
Poster Presentation (Onsite)
Topics: RARE DISEASES, ENDOCRINOLOGY
Keywords: Alopecia, end-organ resistance, vitamin D, 1, 25(OH)2 vitamin D3, refractory rickets
Vitamin D-dependent rickets type II with alopecia: a rare case report
Al Saleh, Abdullah Saleh
Ministry of the National Guard, Health Affairs/King Abdualziz Medical City/Riyadh/ Saudi Arabia.
Introduction: Vitamin D-dependent rickets (VDDR) type II, also known as hereditary vitamin D-resistant rickets type II (VDDRII), is a rare autosomal recessive disorder caused by a mutation in the vitamin D receptor gene, leading to end-organ resistance to 1,25(OH)2 vitamin D3. A patient with this condition presents with refractory rickets and growth retardation during the first year of life. This condition is frequently associated with alopecia totalis. The recommended treatment is supraphysiological doses of 1,25(OH)2 vitamin D3 and high doses of oral or intravenous calcium.
Case Report: A 15-month-old Saudi female visited the clinic for routine one-year vaccination. The baby demonstrated normal gross motor developmental milestones. On physical examination, the baby’s weight was 8 kg (5th percentile based on WHO, length was 71 cm (< 3rd percentile based on WHO), and she had a normal head circumference. She had alopecia totalis and evidence of rickets physically. Laboratory investigations and X-rays were done. Genetic testing confirmed the diagnosis of autosomal recessive VDDRIIA. She was referred to a pediatric endocrinologist who started: Alfacalcidol drops (3 μg daily), vitamin D3 (1000 IU daily) and oral calcium gluconate (1200 g/day). At the 6-month follow-up, the patient showed improvement in her laboratory findings. The patient was also referred to a pediatric dermatologist who recommended no intervention for the alopecia totalis (Figures ).
Discussion: When nutritional rickets are detected, other etiologies of rickets are often not considered. This thinking results in the delayed initiation of treatment, resulting in severe growth retardation and deformities. Red flag signs suggesting a non-nutritional etiology are early onset of rickets, severe deformity, associated failure to thrive, and the presence of alopecia. VDDRII is a rare disorder caused by target organ resistance to 1,25(OH)2 vitamin D, the biologically active form of vitamin D. VDDRII is diagnosed through findings of elevated circulating levels of 1,25(OH)2 vitamin D. Patients with VDDRII present with early-onset rickets, hypocalcemia, and associated total body alopecia. The alopecia may be present at birth or within the first few months of life and progresses to alopecia totalis by childhood. Alopecia is generally not responsive to treatment. The use of intravenous high-dose calcium infusions followed by a high dose of oral calcium is an effective treatment method for VDDRII. The treatment is more effective if started early during the course of the disease and leads to early healing and better growth with prevention of bone deformities.
Conclusion: VDDRII is a rare hereditary autosomal recessive disease originating from mutations in the vitamin D receptors. Clinical manifestations are identical to Vitamin D-deficiency rickets (except alopecia), whereas hypocalcemia and high values of 1.25- dihydroxyvitamin D in serum were characteristic in laboratory findings regarding VDDRII. Treatment is long-lasting with the administration of high doses of calcium and a constant dosage of calcitriol.
ID: 184/08-PT-L-d2D: 4
Poster Presentation (Onsite)
Topics: HAEMATOLOGY/ONCOLOGY
Keywords: meningococcal vaccine, hemolytic anemia, auto-immune
Autoimmune hemolytic anemia – possible association with meningococcal-ACWY vaccine?
Lopes, Vilma; Borges, Joana Pires; Rangel, Maria Adriana; Pinto, Rui
Pediatric Department, Centro Hospitalar Vila Nova de Gaia/Espinho, Vila Nova de Gaia, Portugal.
Background: Autoimmune hemolytic anemia (AIHA) is an uncommon manifestation in paediatric age and is frequently associated with a previous viral or bacterial infection. Vaccination has also been reported as a possible trigger.
Case Presentation Summary: 6-year-old healthy female was admitted to the emergency department with jaundice since the previous day. A detailed clinical history excluded other associated symptoms, including coluria, acholia, fever or other constitutional symptoms. Aside from jaundice, physical examination was unremarkable. Ten days before, she had been inoculated with the meningococcal vaccine against the serogroups A, C, W, and Y (Nimenrix®). There was no recent history of infectious intercurrence, drug or herbal supplements intake or travelling. The blood workup showed a normocytic normochromic anaemia with hemoglobulin of 11,4 g/dL, with 51,960/uL reticulocyte count and normal white blood cell and plaquet counts. The biochemical evaluation revealed an unconjugated hyperbilirubinemia, serum LDH of 482 U/L with haptoglobin <10 mg/dL. Liver and kidney function were normal, and c- reactive protein and erythrocyte sedimentation rates were negative. Urinalysis showed no evidence of coluria. The direct antiglobulin test was strongly positive (3/4) for IgG (2/4) and C3d (3/4). The coagulation screen blood test was normal. The diagnosis of AIAH was established, and she was admitted to the Paediatric Department. Given the good clinical impression and mild anemia with no hemodynamic repercussions, no immediate directed treatment was started. The investigation proceeded to identify possible underlying disorders. An extended immune-haematological and microbiological investigation was performed and showed no relevant results. The abdominal ultrasound was normal. Serial analytic re-evaluations showed gradual haemoglobin improvement and normalization of LDH and haptoglobin. The jaundice resolved completely, and bilirubin normalized after ten days. No other symptoms appeared. She kept follow-up in Pediatric Consultation, and to date, she has had no clinical or analytical relapse.
Learning Points Discussion: In the reported case, the short time lag between vaccination and the onset of symptoms strongly suggests a causal relationship. Furthermore, other alternative explanations for the occurrence of AIHA were not found. A report of this adverse reaction was submitted to Portugal’s national drug and health products authority (Infarmed) and was scored by specialized professionals as “Probable”. To our knowledge, no published reports of this adverse reaction are not mentioned in the vaccine’s European Public Assessment Report. (1) This report aims to alert clinicians to this possible adverse event following the ACWY vaccine to instruct patients about alarming signs and symptoms.
ID: 147/08-PT-L-d2D: 5
Poster Presentation (Onsite)
Topics: INFECTIOUS DISEASES
Keywords: myiasis, cutaneous myiasis, pediatric patients, maggots, mechanical removal
Cutaneous myiasis of the scalp: a case report
Razak, Rien Anggraini1,2; Hannanu, Firdaus Fabrice2; Dahlan, Fith3; Julison, Albert4
1General Physician Department, Primaya Hospital Makassar, Indonesia; 2Medical Faculty of Hasanuddin University, Makassar, Indonesia; 3Pediatric Department, Primaya Hospital Makassar, Indonesia; 4Surgery Department, Primaya Hospital Makassar, Indonesia.
Background: Myiasis is a rare disease with higher prevalence in low socioeconomic regions of tropical and subtropical countries. Although myiasis has been widely distributed in South Sulawesi for years, many hospitals still do not have standard operating procedures for managing myiasis. This report aimed to increase awareness and provide insight into its appropriate management.
Case Presentation Summary: A three-month-old boy was admitted to the hospital with a boil-like nodular lesion on his scalp of four-days duration that ruptured with the discharge of six larvae. The patient had suffered from a cradle cap for one month, with a history of visiting a crowded traditional market. The lesion was previously diagnosed as furunculosis, yet the advised topical and broad-spectrum antibiotic did not provide relief. Physical examination revealed a redness raised opening (diameter 1 cm) with pus at the centre of the swelling. Crusty yellow patches on the entire surface of the scalp were also observed. One larva was discharged after the nodule was squeezed. Laboratory examination revealed leukocytosis. Based on these findings, the working diagnosis was cutaneous myiasis with a secondary bacterial infection. The patient was treated with 1) mechanical larva extraction followed by surgical debridement and saline irrigation, 2) regular renewal of wound dressing, 3) petroleum jelly, and 4) antibiotics. Despite the aggressive treatment, 1–3 larvae were still reported on daily observation until the second mechanical larva extraction was held 12 days after the first extraction. One week following the second extraction, no more larvae were found on the scalp, and clinical improvement was reported. After 16 days of hospitalization, the patient was discharged with no further complications (Figure ).
Learning Points Discussion: Myiasis remains a problem in South Sulawesi. Poor hygiene, lack of access to entomologists, and availability of drugs of choice have become the biggest challenges in eliminating the disease. Although no specific line of treatment has been advised, oral and topical off-label application of Ivermectin was reported to be the drug of choice to treat wound myiasis effectively. Unfortunately, in our case, Ivermectin was unavailable at the time, both at the hospital and province levels. Nevertheless, despite the prolonged recovery time, aggressive debridement and mechanical larvae extraction succeeded in removing all the larvae on the patient’s scalp, with significant clinical improvement. This case report recommends considering myiasis as a differential diagnosis in future furuncular skin lesions and providing Ivermectin to prevent complications from myiasis, especially in endemic areas.
ID: 167/08-PT-L-d2D: 6
Poster Presentation (Onsite)
Topics: INFECTIOUS DISEASES
Keywords: RSV, cost-effectiveness, preterm, prophylaxis
New analysis on the cost-effectiveness of palivizumab for the prevention of severe respiratory syncytial virus (RSV) infection in infants born 29-31 weeks’ gestational age (wGA)
Keary, Ian1; Paes, Bosco2; Fullarton, John1; Rodgers-Gray, Barry1; Tarride, Jean-Eric2; Carbonell-Estrany, Xavier3
1Violicom Medical Limited, UK; 2McMaster University, Hamilton, Ontario, Canada; 3Hospital Clinic, Barcelona, Spain.
Background: Palivizumab remains the only licensed intervention for the prevention of severe RSV infection in high-risk infants, including those born <35wGA. Up until 2015, the Canadian Paediatric Society (CPS) recommended all otherwise healthy infants born ≤32 wGA and <6 months at the start of the RSV season receive prophylaxis. 1 Since 2015, however, palivizumab use has largely been restricted to those otherwise healthy infants born ≤30wGA and <6 months old (reaffirmed in 2021). 2 The objective of this study was to provide an up-to-date economic analysis of palivizumab versus no prophylaxis in 29–31wGA infants using Canadian costs.
Methods: A systematic review of previous economic models of palivizumab in 29–31wGA infants and expert clinical input informed the development of a new cost-utility model. Infants were assumed to follow a semi-Markov process having either an RSV hospitalisation (RSVH), emergency room/outpatient-attended RSV infection, or were uninfected/non-medically attended. Hospitalised infants could be admitted to the ICU (17.9%), and ICU-admitted infants could die (0.43%). All non-hospitalised and surviving hospitalised infants could experience respiratory morbidity for up to 18 years across a lifetime time horizon; duration and rates of morbidity were calculated according to RSV infection and palivizumab status. The RSVH rate in non-prophylaxed infants was 5.9%, which was reduced by 63.3% by palivizumab. Palivizumab costs (assuming 50 mg: CAN$752; 100 mg: $1,505) were calculated from Canadian birth statistics. The base case assumed the inclusion of indirect costs, no vial sharing, and 18 years’ respiratory morbidity (1.5% discounting). A cost per quality-adjusted life-year (QALY) of ≤$50,000 was considered cost-effective.
Results: Palivizumab was highly cost-effective ($29,579/QALY) in 29–31wGA infants in the base case and remained so when respiratory morbidity was limited to 13 ($37,343/QALY) or 6 ($50,352/QALY) years (Table ). In deterministic sensitivity analyses (±20% on main variables) the model was most sensitive to utility scores, long-term morbidity rates, palivizumab cost, and palivizumab efficacy. Probabilistic sensitivity analyses (10,000 iterations) resulted in incremental costs of $30,857/QALY, with a 0.76 probability of palivizumab being cost-effective at a $50,000 willingness-to-pay threshold. Vial sharing (5% wastage) considerably improved cost- effectiveness in the base case ($21,438/QALY). The exclusion of discounting ($26,443/QALY) and indirect costs ($28,525/QALY) had a relatively negligible impact on cost-effectiveness.
Conclusions: This new analysis, incorporating a comprehensive assessment of the burden of RSV, demonstrated that palivizumab is highly cost-effective in 29–31wGA infants versus no prophylaxis using Canadian healthcare costs. As commonly employed in clinical practice, Vial sharing significantly improved the cost/QALY.
ID: 119/08-PT-L-d2D: 7
Poster Presentation (Onsite)
Topics: NUTRITION & DIETS, NEONATOLOGY
Keywords: Breastfeeding, Human milk donation, Human milk banking, Ambulatory human milk donor, Muslim countries
Ambulatory human milk donation, a continuous experience
Alnaqeeb, Niran1; Tolba, Azza2; Elhassanin, Ahmed3; Azab, Ayman4
1Adan hospital, MOH, Kuwait, Kuwait; 2Adan hospital, MOH, Kuwait, Kuwait; 3Adan hospital, MOH, Kuwait, Kuwait, Faculty of Medicine, Mansoura university, Egypt; 4Adan hospital, MOH, Kuwait, Kuwait.
Background: Human milk banking is prohibited in Muslim countries due to religious issues. In Adan hospital-Kuwait, every effort is made to initiate and maintain breastfeeding starting from the antenatal period.
Method: An innovative human milk donation (HMD) Policy was implemented in 2000. Despite this early start, only a few preterm babies received this donated human milk every year due to many issues such as; low availability of the volunteering mothers, reluctance to accept the idea of HMD due to religious factors and the most crippling obstacle was the time factor. In an attempt to improve the HMD policy, the ambulatory human milk donation (AHMD) Policy was started in 2019. AHMD policy includes some antenatal steps such as antenatal counselling for pregnant women, especially those expecting to have a preterm or sick baby, finding ambulatory donors who may accept the idea, usually from the lactation clinic, lactating mothers who accept the idea to be a donor, laboratory tests were done, demonstrative materials about the religious and social Issues for HMD were supplied. After delivery, instructions were given to donors about how to express their human milk and transfer it in sterile containers to the lactation unit. This donor milk was kept in the AHMD freezer to be ready for the recipient baby.
Results: To our delight, after three years of implementation of the AHMD policy, the number of preterm and sick babies received their first feed from ambulatory human milk increased significantly and also the experience of our team to overcome the obstacles, especially the time factor issue, had much improved.
ID: 137/08-PT-L-d2D: 8
Poster Presentation (Onsite)
Topics: NEONATOLOGY
Keywords: necrotizing enterocolitis, claudin-3, preterm infants
Claudin-as a biomarker for early diagnosis of necrotizing enterocolitis in preterm infants.
Huseynova, İlaha
Azerbaijan Medical University, Azerbaijan,Baku.
Introduction: Necrotizing enterocolitis (NEC) is a severe and polyetiological disease with a high specific density in perinatal causes of death among preterm, especially very low and extremely low birth weight infants. Notwithstanding numerous studies and the use of modern clinic guidance in this aspect, NEC remains one of the actual problems in neonatology.
Aim: This study aims to define the role of claudin-3 in the early diagnosis of NEC in preterm infants.
Material and Methods: 45 preterm infants suspected of NEC in the neonatal intensive care unit (NICU) were included in the study. The clinic, laboratory, and imaging techniques were used to confirm the diagnosis in all preterm infants suspected of NEC. All examined neonates were compared in two groups: the 1st group, of 31 infants, did not develop NEC and the 2nd group, of 14 infants who developed NEC. In both groups, urinary claudin-3 levels were measured by the enzyme-linked immunosorbent assay (ELISA) method. Urine collectors obtained urine from all included neonates. In 1st group gestational age was min 26, max 36; mean 30,61; st. D 2,67; birth weight min 800 g, max 2200 g, mean 1413,7; st. D 424,4; in 2nd group gestational age was min 26, max 34; mean 29, 14; st.D 2,77; birth weight min800, max1640g; mean 1207,9;st. D 288,18. [1] Statistical analyses were performed in an SPSS20 Windows system. According to the abnormal distribution of claudin-3 levels, the Wilcoxon Mann-Whitney method was used.
Results: Claudin-3 levels in the 1st group were mean 29,3 (95 confidence interval 27,2–31,4), st. D 5,71;in 2nd group were mean 34,4(95 confidence interval 32,0–36,8), st. D 4,12. [1] After ranking mean levels, there was statistically high diagnostic accuracy among claudin levels of these neonates, p = 0,002 (Figure ). The sensitivity (86%) and specificity (71%) of claudin-3 were determined by ROC analysis.
Conclusion: Thus, we can conclude that increased levels of claudin-3 in urine reflect a loss of tight junctions. Tight junction loss, one of the main components of the intestinal barrier, can lead to NEC. Accordingly, we can confirm NEC by increased levels of claudin-3 in urine in preterm infants with suspicion of NEC. [1] These findings suggest that using urinary claudin-3 as a noninvasive marker for early diagnosis of NEC in preterm infants is appropriate.
ID: 183/08-PT-L-d2D: 9
Poster Presentation (Onsite)
Topics: NEONATOLOGY
Keywords: Necrotizing Enterocolitis, prematurity, intestinal inflammation
Necrotizing Enterocolitis – retrospective analyses of 5 years in a Neonatal Intensive Care Unit
Pinho, Joana1; Vieira, Beatriz2; Lopes, Vilma1; Torres, Jacinto3; Costa, Conceição3
1Department of Pediatrics, Centro Hospitalar Vila Nova de Gaia/Espinho, Portugal; 2Department of Pediatrics, Centro Hospitalar Póvoa de Varzim/Vila do Conde; 3Department of Neonatology, Centro Hospitalar Vila Nova de Gaia/Espinho, Portugal.
Background: Necrotizing enterocolitis (NEC) is a severe idiopathic and multifactorial disease characterised by inflammatory bowel mucosa and ischemic necrosis. NEC is one of the most gastrointestinal emergencies in newborn infants, and it´s an important cause of mortality and morbidity in preterms, especially in very low birth weight (VLBW) infants, with high mortality rates (15–30%).
Aim: This study aims to analyse and describe the cases of NEC in our hospital and draw a comparison between our data and literature.
Methods: Retrospective analysis of clinical data from newborns in our Neonatal Intensive Care Unit diagnosed with NEC between January 2016 and December 2020. We analysed epidemiological data, clinical manifestations, laboratory and radiologic findings, management and complications.
Results: We found 21 cases of NEC. 33.3% in newborns with gestational age (GA)<28 weeks; 33.3% with GA [28–32[weeks; 29.6% with GA [32–37[weeks and 4.8%≥37 weeks. New-borns VLBW were 61.9%(n = 13). In five newborns (23.8%), prenatal glucocorticoid was not administered. In 7 cases, one stopped his diet completely, while the other six only did a trophic diet. In 12 infants, their diet was non-human milk. Ibuprofen was used to treat patent arterial duct in 5 newborns (23.8%). (1) Diagnosis was made at 14.4 ± 11.3 days. All of the subjects developed abdominal distension and tenderness; 13 cases (61.9%) showed increased gastric residual volume (>25%), 42.9% developed vomiting, and 38.1%(n = 8) had rectal bleeding. Abdominal wall erythema was found in 4 infants (19%). Respiratory instability occurred in 52.4% (n = 11) and hypotension in 38.1%(n = 8). Bacteriemia was found in 19.0% (n = 4) and C-Reactive Protein was positive in 76.2% (n = 16). The main laboratory findings were hyperglycaemia (61.9%; n = 13), thrombocytopenia (52.4%; n = 11), metabolic acidosis (52.4%; n = 11) and hyponatremia (52.4%; n = 11). Dilated loops (95.2%; n = 11), sentinel loops (47.6%; n = 10), pneumatosis (38.1%; n = 8) and pneumoperitoneum (23.8%; n = 5) were the findings of the abdominal radiographic imaging. (2) According to Bell staging, 5 infants (23.8%) had suspected NEC (stage IA and IB), 6(28.6%) had proven NEC (IIA and IIB), and 10(47.6%) infants had advanced NEC (IIIA and IIIB). (3) All infants made bowel rest during 10.2 ± 5.0 days. Twenty infants (95.2%) did empiric antibiotic therapy for about 15.8 ± 7.4 days. As a first approach, 4 (19.0%) needed abdominal drain, and 4 were submitted to abdominal surgery (19.0%). (4) Intestinal narrowing occurred in 23.8%(n = 5), all submitted to surgery. Poor long-term growth and neurodevelopment were found in 2 infants (9.5%). One of the infants in this sample died (4.8%).
Conclusions: Most of the results are in accordance with what is suggested in the literature. Only the mortality rate was lower (4.8% in our study versus 15% in the literature).
ID: 100/08-PT-L-d2D: 10
Poster Presentation (Onsite)
Topics: NEONATOLOGY
Keywords: perinatal hypoxia, hypoxic-ischemic encephalopathy, neonatal death, neutrophil gelatinase-associated lipocalin, kidney injury molecule-1
NGAL and KIM-1 are beneficial biomarkers for the early prediction of neonatal death in small birth weight infants with hypoxic-ischemic encephalopathy
Panakhova, Nushaba1; Akhundova, Afag1; Huseynova, Saadat2; Hajiyeva, Adila3; Adilova, Aytekin1
1Azerbaijan Medical University; 2Scientific Research Institute of Obstetrics and Gynecology, Azerbaijan; 3Scientific Research Institute of Pediatrics.
Introduction: Perinatal hypoxia causes multi-organ dysfunction resulting in renal and neurological compromise with about 1.4% of hypoxic-ischemic encephalopathy (HIE) and almost 20% of neonatal death. Early recognition of acute kidney injury (AKI) is important to facilitate appropriate fluid and electrolyte management for a stable biochemical milieu and reduce neonatal mortality and morbidity.
Aim: The study aimed to confirm whether higher levels of AKİ markers—urinary neutrophil gelatinase-associated lipocalin (NGAL), kidney injury molecule-1 (KIM-1) are associated with increased mortality risk in HİE neonates.
Materials and Methods: The study included low birth weight neonates with HIE divided into 2 groups: 1st group—41 died neonates, and 2nd group—196 survived neonates. ELISA assays of KIM-1 in urine and NGAL in plasma were performed on days 1 and 7.
Results: Median level of NGAL was 119.4 ± 21.7 ng/ml and 187.63 ± 16,5 ng/ml on the 1st and 7th days of life, respectively, in the 1- st group versus 122.1 ± 12.1 ng/ml and 151.4 ± 14.3 ng/ml (18.6–60.5) in 2nd group. KIM-1 was 0.48 ± 0.06 ng/ml and 0.99 ± 0.3 ng/ml on the 1st and 7th days of life, respectively, in the 1-st group versus 0.86 ± 0.16 ng/ml and 09 ± 0.21 ng/ml in 2nd group (1.8–4.6). Despite the absence of a statistically significant difference in terms of sensitive markers of AKI between compared groups, the deceased newborns were characterized by a significant increase in the level of both markers in the dynamics of the early neonatal period (p < 0.05).
Conclusions: Increased levels of NGAL and KIM-1 in the dynamic of the early neonatal period of small birth weight infants with HIE are associated with neonatal mortality.
ID: 210/08-PT-L-d2D: 11
Poster Presentation (Onsite)
Topics: NEUROLOGY
Keywords: Refractory benign idiopathic intracranial hypertension
Case of benign idiopathic intracranial hypertension refractory to medical therapy, managed with ventriculoperitoneal shunt insertion: a case report
Al Karaghouli, Yusur Turky1,2; Fathalla, Waseem Mahmoud2
1Abu Dhabi Health Service Company, United Arab Emirates; 2Sheikh Shakhbout Medical City, United Arab Emirates.
Introduction: Benign idiopathic intracranial hypertension usually presents with headache and transient obscuration of vision. The diagnosis is made based on clinical criteria, including symptoms, signs and characteristic neuroimaging findings consistent with IIH. The urgency of managing benign IIH is to avoid permanent vision loss, which may be seen in 15% of the patients.
Objectives: Report a case of benign idiopathic intracranial hypertension that was refractory to pharmacological management and necessitated surgical intervention with restoration of vision and resolution of bilateral papilledema.
Clinical Case: A 12 years old girl, previously healthy, with a BMI above the 99th centile, initially presented with a 1-year history of nonspecific, throbbing headache associated with decreased visual acuity and photopsia of a couple of weeks duration. Physical examination was unremarkable, with an intact neurological exam; however, a formal ophthalmological examination revealed bilateral grade IV papilledema with enlarged blind spots and increased intraocular pressure in both eyes. MRI brain and MRV brain were normal. (1) A lumbar puncture showed an opening pressure of 36 cmH2O, and cerebrospinal fluid analysis was done to rule out infectious aetiologies. She was initially started on IV Acetazolamide for 48 hours and then switched to oral Acetazolamide. (2) She was followed up in the paediatrics neurology and ophthalmology outpatient clinics for almost 2 months while on Acetazolamide in addition to Topiramate. Mild improvement in symptoms was seen; however, ophthalmological examinations showed persistent grade IV papilledema, and a repeat lumbar puncture still showed an elevated opening pressure of 23 mmH2O. The patient underwent surgical intervention with VP shunt insertion, which improved symptoms with complete resolution of her papilledema.
Conclusion: A patient on medical therapy for benign idiopathic intracranial hypertension needs careful follow-up. Surgical interventions, including optic nerve sheath fenestration or cerebrospinal fluid shunting procedures, should be explored for those patients whose clinical condition does not improve as expected.
ID: 109/08-PT-L-d2D: 12
Poster Presentation (Onsite)
Topics: NEUROLOGY
Keywords: intranasal midazolam, intravenous diazepam, seizure, child
Efficacy and safety of intranasal midazolam versus intravenous diazepam for acute childhood seizures: a meta-analysis of randomized controlled trials
Espinoza, Mary Trisha Merced; Valencia, Maria Antonia Aurora
University of Santo Tomas Hospital, Philippines.
Background: A seizure is a life-threatening event in children requiring prompt control and early termination since prolonged seizure episodes carry the risk of complications and increased mortality. Intranasal midazolam has been an area of curiosity due to its ease of administration and ability to reach peak plasma and CSF concentration within minutes.
Objective: To summarize the results of published studies examining the efficacy and safety of intranasal midazolam versus intravenous diazepam for acute childhood seizures. Design: Meta-analysis. Participants: The population of interest was pediatric patients less than 18 years old with acute seizure. Intervention: The exposure variable was intranasal midazolam.
Methods: Randomized Controlled Trials determining the Efficacy and Safety of Intranasal Midazolam versus Intravenous Diazepam were reviewed by three appraisers. Study information such as seizure cessation rate, time from admission to treatment initiation, time to seizure control, and side effects were gathered in an abstraction form. Stata MP version 16 software was used to perform the meta- analysis. The risk of bias was assessed using the Review Manager (RevMan 5.4) software. (1) Main Outcome Measured: The main outcome measured was the proportion of patients who achieved seizure control, and the secondary outcomes are the following: mean time from hospital admission to treatment initiation, treatment initiation to seizure cessation, hospital admission to seizure cessation and proportion of patients who experienced side effects.
Results: Only seven studies with a total population of 464 patients met the eligibility criteria. The risk ratio was presented for seizure cessation rate, while the weighted mean difference was presented for other secondary outcome measures. This meta-analysis did not show statistically significant results for seizure cessation rate (p = 0.89) and time to seizure cessation. The time from hospital arrival to treatment initiation was significantly shorter for IN midazolam (p = 0.04). While adverse reactions were infrequently observed in the studies included.
Conclusion: Although seizures were controlled more rapidly with intravenous diazepam, intranasal midazolam was just as safe and efficacious. The overall results favoured intranasal midazolam due to its ease of administration and its effectiveness as a noninvasive intervention for the control of acute seizures in children.
ID: 203/08-PT-L-d2D: 13
Poster Presentation (Onsite)
Topics: RARE DISEASES, NEUROLOGY
Keywords: TANGO2 Gene Mutation
Homozygous variant in TANGO2 gene presenting with acute encephalopathy and rhabdomyolysis: a case report.
Al Karaghouli, Yusur Turky1,2; Fathalla, Waseem Mahmoud1
1Sheikh Shakhbout Medical City; 2Abu Dhabi Health Service Company, United Arab Emirates.
Introduction: TANGO2-related metabolic encephalopathy and arrhythmias (TRMEA) is a rare autosomal recessive genetic disorder first reported in 2016 with less than 100 reported cases. TRMEA has a wide phenotypic spectrum, including acute metabolic crises, rhabdomyolysis, muscle weakness, ataxia, intellectual delay, dysarthria and cardiac arrhythmias (prolonged QT interval and Torsade de pointes).
Objectives: Report a case of TRMEA with acute encephalomyopathic crisis related to a novel TANGO-2 variant, and raise awareness about this life-threatening manifestation.
Clinical Case: A 5 years old boy developed acute encephalopathy and rhabdomyolysis 3 days after undergoing a surgical procedure. His creatine kinase level was more than 40,000 IU/L with no hyperammonemia. EEG was abnormal, and ECG showed prolonged QTc interval; echocardiography did not show any cardiomyopathy. He required paediatric intensive care for the management of his encephalopathy and rhabdomyolsis (with double hydration and alkalinisation). He returned to his baseline upon discharge and follow-up. (1) His records indicated normal development until the age of 18 months, when he had an episode of unprovoked seizure, after which he developed lower limbs’ hyperreflexia, spasticity and unsteady gait. Extensive investigations were non-yielding; whole Genome Sequencing revealed a homozygous variant of uncertain significance in the TANGO2 gene, which is compatible with his acute crisis.
Conclusion: TANGO2-related acute encephalomyopathic crisis should be considered in patients presenting with otherwise unexplained acute encephalopathy and myoglobulinuria. Conversely, patients diagnosed with TANGO2-related disorders should be cautioned about acute deterioration provoked by stress or intercurrent illness.
ID: 175/08-PT-L-d2D: 14
Poster Presentation (Onsite)
Topics: NEUROLOGY
Keywords: night terror, epilepsy, oxcarbazepine
Night terror or epilepsy?- a case report
Tavchioska, Gabriela1; Hristova, Aleksandra2
1General hospital Prilep, North Macedonia, Republic of; 2General hospital Kumanovo, North Macedonia, Republic of
Background: Diagnosing an abnormal paroxysmal event during sleep presents a challenge for paediatricians in resource-limited settings.
Case Presentation: a 10-year-old male child was referred by a family doctor because of unclear events during a sleep that started 6 months ago. Five times during the six months, the child sat in bed while sleeping shouted and blinked his eyes. The child was born from a normal pregnancy, with normal psychomotor development. Investigations such as biochemical tests, ECG, EEG and MR of the brain were done. Unfortunately, video EEG is not available in my hospital. EEG findings were spike slow wave complexes in F2-F8, F8-T4, T4-T6 and T6-O2, which were more frequent during photostimulation. The rest of the investigations had normal findings. Antiepileptic therapy was started with oxcarbazepine with no side effects. The child is seizures free 8 months.
Conclusion: Night terror and seizures can be distinguished with proper clinical evaluation and diagnostic testing.
ID: 269/08-PT-L-d2D: 15
Poster Presentation (Onsite)
Topics: ADOLESCENT MEDICINE, PUBLIC HEALTH
Keywords: Cannabis consumption, Health Behaviour in School-aged children (HBSC)
Profiles of cannabis consumption among school-aged children in Luxembourg
Lopes Ferreira, Joana; Catunda, Carolina
University of Luxembourg, Luxembourg.
Background: Cannabis is the most widely used illegal drug globally, with almost 200 million users in 2019. This use is associated with many negative health consequences and social problems, such as low school performance and other drug use. Cannabis use can be particularly harmful if it starts early, if it’s excessive or if it occurs associated with other forms of problematic behaviours. (1) A lot of health behaviours, good or bad, emerge during adolescence and remain through the life course. Changing unhealthy behaviours in adolescence would significantly impact society, such as reducing the load of disease, injuries, and economic costs. (2) The objective of this study is to explore cannabis consumption profiles and the factors related to it during adolescence.
Methods: This study is based on the 2017/2018 Health Behaviour in School-aged Children Luxembourg survey. Participated 6 880 adolescents, aged 12 to 18-year-old, that attended schools in Luxembourg that teach according to the national. Adolescents answered if they used cannabis during their lifetime and during the past month. Following, they were categorized into 4 groups: 1. never consumed cannabis in a lifetime; 2. consumed in a lifetime but not in the past month; 3. non-daily use during the past month and; 4. daily use (or almost) during the past month. To compare and characterize the groups, descriptive and bivariate analyzes were undertaken, as well as their significance level.
Results: Results show that most of the adolescents (81.8%) never consumed cannabis in their lifetime; 9.4% declared a consumption during their lifetime but not the past month; 6.6% used during the past month, non-daily; and 2.2% used (almost) daily during the past month. Different profiles emerge between the groups, particularly with regard to socio-demographic characteristics and risky behaviours. In the case of social relationships and indicators of health and well-being, differences exist but are not as pronounced. Boys, older students and those who do not live with both parents are more likely to be part of groups that have used cannabis. In addition, most risk behaviours show a dose-response relationship with cannabis use. The increase in risky behaviours translates into not only a greater likelihood of using cannabis but also a greater frequency of use.
Conclusion: The four different profiles evolve gradually with the frequency of cannabis consumption. This dose-effect relationship has been highlighted between cannabis consumption and the other variables present but is especially true for risk behaviours. Prevention strategies should distinguish adolescents from each of these groups, starting in early adolescence and focus on risk behaviours as a whole.
ID: 262/08-PT-L-d2D: 16
Poster Presentation (Onsite)
Topics: ADOLESCENT MEDICINE
Keywords: adolescents, health literacy, physical activity
The relationship between HL levels and physical activity in Polish schoolchildren aged 13-17.
Kleszczewska, Dorota1; Dzielska, Anna2; Mazur, Joanna3
1Institute of Mother and Child Foundation, Poland; 2Department of Child and Adolescent Health, Institute of Mother and Child, 01–211 Warsaw, Poland; 3Department of Humanization in Medicine and Sexology, Collegium Medicum, University of Zielona Gora, 65–729 Zielona Gora, Poland.
Background: Insufficient physical activity (PA) poses a severe threat to the health and well-being of people in various age groups, including children and youth. Despite numerous campaigns, educational programmes, and interventions, on a global scale, approximately 81% of teens aged 11 to 17 fail to meet WHO recommendations and exhibit significant PA deficiencies. It has been argued that the higher the level of health literacy (HL) in young people, the more likely they are to engage in health-promoting behaviours and avoid ones that are a threat to health. So far, domestic analyses of the health benefits of improving HL levels have focused primarily on the relationship between the overall evaluation of physical and psycho-social health and avoidance of risk behaviours.
Objective: The paper’s objective is to present an analysis of the relationship between PA and HL in Polish youth.
Material and Methods: The data have been sourced from the Health Behaviour in School-aged Children (HBSC) study carried out in Poland in 2018. The sample consists of three age groups: 13-, 15-, and 17-year-olds (2144, 1933, and 1700 respondents, respectively), including 52.4% girls and 47.6% boys. Their HL was measured using the HLSAC scale consisting of 10 questions (Paakkari et al.) ranging from 10 to 40. The mean index value was 30.64 (SD = 4.55). The three defined intervals comprised 11.0%, 74.4%, and 14.6% of respondents. The moderate-to-vigorous-physical-activity (MVPA) and vigorous-physical-activity (VPA) indicators were used to measure physical activity. Two dichotomous outcome variables were defined, where 1 stands for MVPA at least 60 minutes of moderate to intensive PA 7 days a week, and VPA as high-intensity exercises performed outside of school classes at least twice a week. Respectively 13.0% and 59.0% of the respondents met those criteria. A comparison of the marginal HL categories revealed an MVPA improvement of 6.1% and a VPA improvement of 16.2% (see: Table ). Multi-factor logistic regression analysis indicated that compared to low levels, high HL levels significantly increase the likelihood of improvement in PA, as adjusted for gender, age, family wealth, and self-rated health. As far as VPA is concerned, even average HL levels display a protective effect.
Conclusion: The relationship between HL and PA in school-aged children has been confirmed. Activities that increase HL in children and youth may result in arresting the unfavourable trend for physical activity to decline in the young generation.
ID: 265/08-PT-L-d2D: 17
Poster Presentation (Onsite)
Topics: GASTROENTEROLOGY
Keywords: Functional abdominal pain, irritable bowel syndrome, primary care
Home-based hypnotherapy for children with functional abdominal pain and irritable bowel syndrome in primary care: design of a randomised-controlled trial
Ganzevoort, Ilse Nadine1; Fokkema, Tryntsje1; Mol-Alma, Harma J.1; Heida, Anke1; van der Veen, Adriëlla L.1; Benninga, Marc A.2; Vlieger, Arine M.3; Berger, Marjolein Y.1; Holtman, Gea A.1
1University Medical Center Groningen, Groningen, the Netherlands; 2Emma Children’s Hospital, Amsterdam UMC, University of Amsterdam, the Netherlands; 3St. Antonius Hospital, Nieuwegein, the Netherlands.
Background: Children often present to primary care with functional abdominal pain (FAP) or irritable bowel syndrome (IBS). These functional abdominal gastrointestinal diseases cannot be explained by organic disease and are often caused by interactions between biological, psychological and social factors. General practitioners (GP) usual care in the Netherlands, according to the Dutch Society of GPs guideline for FAP, consists of communication, education and reassurance. However, around half of the children still report abdominal complaints after one year, underlining the difficulty of treatment. Hypnotherapy is often used in paediatric care. Hypnotherapy involves a therapist inducing a hypnotic state by guiding a patient to respond to suggestions. Suggestions focus on changes in physiology, sensations, emotions, thoughts, or behaviour. While hypnotherapy has an evidence base in paediatric care, it lacks evidence in primary care. Therefore, this study will investigate the (cost) effectiveness of home-based hypnotherapy for children with FAP or IBS in primary care.
Methods: Children aged 7–17 years presenting with FAP or IBS in primary care are currently recruited to participate in this pragmatic, randomised, controlled trial and will be assessed over 12 months. The control group will receive care as usual from their GP, while the intervention group will receive care as usual plus 3 months of home-based hypnotherapy (Figure ). Home-based hypnotherapy consists of daily listening to standardised hypnosis exercises via a website. The primary outcome is the proportion of children with adequate relief from abdominal pain/discomfort at 12 months, analysed on an intention-to-treat basis. Secondary outcomes include adequate pain relief at 3 and 6 months, the severity of pain/discomfort, pain frequency and intensity, daily functioning and impact on function, anxiety and depression, pain beliefs, sleep disturbances, school absence, somatisation, and health care use and costs. We must include 200 children to determine a 20% difference in those with adequate relief (55% control vs 75% intervention).
Results: The recruitment is ongoing until September 2023. Results are expected in 2024.
Conclusions: Home-based hypnotherapy is a simple-to-use intervention and could potentially aid GPs in the management of children with FAP or IBS. Home-based hypnotherapy at an early stage could lead to a better prognosis, prevent unnecessary referrals and reduce costs. Besides this trial, we will perform a qualitative study including children, parents and GPs to investigate facilitators and barriers for implementation in primary care.
ID: 212/08-PT-L-d2D: 18
Poster Presentation (Onsite)
Topics: GENERAL PEDIATRICS
Keywords: Echinococcus, hydatid cyst, brain cyst
Intracranial hydatid cyst in a ten-year-old boy presented in paediatric emergency department
Louka, Magdalini; Kollia, Elissavet; Antonopoulos, Stavros; Ioannidou, Loukia
“Aghia Sophia” Childrens’ Hospital, Greece
Background: Cystic echinococcosis is a parasitic infestation of Echinococcus, with dogs being the definite primary hosts. Cysts can develop in various organs, mainly the liver and lungs, whereas intracranial hydatid cysts (IΗC) account only for 0.5–3% of all cases of CE. Prevalence is higher in endemic regions like Mediterranean countries, South America, North Africa and Australia. We report a case of giant IΗC in a ten-year-old boy from Greece, presenting with intermittent headache and vomiting.
Case Presentation Summary: The ten-year-old boy presented in our paediatric Emergency Department (ED) with a chief complaint of vomiting episodes over the last month, for which he was recently hospitalised and managed as per acute gastroenteritis. Further history revealed the onset of episodic headache two weeks ago, occurring mainly in the morning and deteriorating by supine position. History of contact with pet dogs was also noted. On examination, Glasgow Coma Scale was 15, and vital signs were within normal limits, but the patient exhibited a positive Romberg’s test when the head was turned towards the left and a positive pronator drift of the left arm. Fundoscopy indicated raised intracranial pressure as bilateral frank papilloedema was present. Urgent Computed Tomography (CT) scan of the brain was performed, depicting a giant, spherical and well-defined unilocular cyst, CSF iso-dense, involving the right temporoparietal lobe and causing midline shift with dilatation of the contralateral ventricle. Diagnosis of IHC was presumed, but additional considerations in differential diagnosis included brain abscess, cystic astrocytoma or arachnoid cyst. Further evaluation with brain Magnetic Resonance Imaging did not show perilesional oedema or ring-enhancement, and total surgical cyst excision was decided. Histopathology of the excised mass confirmed the diagnosis of Echinococcus granulosus, and the postoperative course was uneventful. Interestingly, anti-Echinococcus ELISA was negative, and the rest of the laboratory tests were unremarkable, including eosinophilic count and liver enzymes. Chest radiography and abdominal sonography were normal; nevertheless, further CT investigation is needed to exclude primary localisation of echinococcosis in other organs.
Learning Points Discussion: IHC should be considered in children with cystic brain lesions, especially in endemic countries. Our patient was initially managed for gastrointestinal symptoms, but suspicion of IHC was raised soon after arrival in ED based on thorough physical examination and neuroimaging. In children, IHC can grow to enormous size without showing significant symptoms due to the elasticity of skull bones and compressibility of the neural tissue, and serum laboratory exams may have minimal diagnostic significance, as brain tissue evokes minimal response.
Session
09-OP-V-d2D: Oral Presentations Session 9 - Day 2 - Zone D
Presentations
ID: 180/09-OP-V-d2D: 1
Oral Presentation (Virtual)
Topics: GENERAL PEDIATRICS
Keywords: ALTE, BRUE
ALTE versus BRUE: what has changed?
Queirós, Joana Carvalho1; Martins, Ines Aires1; Lima, Joana Baptista1; Silva, Gisela1,2; Ramos, Ana1,3; Lima, Rosa1,2
1Pediatrics Department, Centro Materno infantil do Norte, Centro Hospitalar Universitário do Porto; 2Gastroenterology Unit, Pediatrics Department, Centro Materno infantil do Norte, Centro Hospitalar Universitário do Porto; 3Pneumology Unit, Pediatrics Department, Centro Materno infantil do Norte, Centro Hospitalar Universitário do Porto.
Background: In 2016, the American Academy of Pediatrics (AAP) replaced the term Apparent Life-Threatening Event (ALTE) with a new term Brief Resolved Unexplained Events (BRUE), to describe brief, self-limited paroxysmal events without apparent cause and proposed a new diagnostic approach. Nevertheless, the implementation of this new term and its correct approach has proven difficult. (1) we aimed to assess the applicability of the new classification and (2) compare whether there are differences in the approach of these patients.
Methods: A retrospective cohort study was performed. We compared clinical studies and readmissions of infants hospitalized in a tertiary hospital, with the diagnosis of ALTE or BRUE, during the periods before (January/2012–May/2016—group 1) and after (June/2016-December/2021—group 2) the introduction of the new nomenclature. Descriptive analysis followed by univariate analysis was performed.
Results: A total of 153 patients were included, 72 in group 1 and 81 in group 2. 58.2% were female, and the median age at diagnosis was 33.5 days (interquartile range (IQR): 18.7–53.5), with 66 (43.1%) of the patients being under 30 days old. The average length of hospital stay was 4 (IQR: 2.0–6.0) days, and 4 (2.6%) patients were readmitted, with no differences between the two groups. There were no differences in demographic and clinical characteristics between the two groups. (1) The median age at diagnosis was statistically significative higher in group 1–48.63 vs 36.47 (IQR: 18.7–53.5) days, p = 0.044. Patients in the group 2 had lower rates of chest radiography (55.6% vs 39,5%, p = 0.047). However, considering the use of electroencephalogram (EEG) and virological analysis of nasopharyngeal secretions, rates were higher in group 2 than in group 1 (0 vs 7.4%; p = 0.020 and 26.4% vs 46.9%; p = 0.009, respectively). Regarding the laboratory study, no significant differences were found (91.7% vs 92.6%, p = 0.533). The same was true for treatment and final diagnosis, where no significant differences were found between both groups. Gastroesophageal reflux was the most frequent final diagnosis (33.1%).
Conclusions: Comparing the clinical approach after the implementation of the new nomenclature introduction, there were lower rates of chest radiograph use and higher rates of EEG and virological analysis use were found. The availability of these complementary diagnostic tests could partly explain these results. These findings suggest that the clinical application of this classification has raised significant challenges for clinicians in evaluating and caring for these infants.
ID: 181/09-OP-V-d2D: 2
Oral Presentation (Virtual)
Topics: GENERAL PEDIATRICS, EMERGENCY PEDIATRICS
Keywords: Altered mental status, emergency room, emergency pediatrics
Altered mental status admitted in Pediatric Emergency Room in a leve II Portuguese hospital
Queirós, Joana Carvalho1; Martins, Ines Aires1; Leite, Ana Margarida2; Pimenta, Sofia2; Ribeiro, Maria do Céu2; Lira, Sónia2
1Pediatrics Department, Centro Materno infantil do Norte, Centro Hospitalar Universitário do Porto; 2Pediatrics Department, Centro Hospitalar de Tâmega e Sousa.
Background: Altered mental status (AMS) is one of the main neurological emergencies, representing a significant number of pediatric emergency room (ER) admissions. There are many different possible etiologies, and systematic assessment is essential. An emergent clinical evaluation may prevent further deterioration of the impaired consciousness and life-threatening scenarios.
Aim: We aim to describe and characterize patients admitted to the pediatric ER with Altered mental status and their etiological investigation, treatment and orientation.
Methods: Observational and retrospective analysis of the patient’s clinical records admitted to the ER of a level II hospital (without Pediatric Intensive Care Unit (ICU)), with the admission diagnosis of altered mental status, between January/2017 and June/2022. Epidemiological characteristics, etiological investigation, interventions, final diagnosis and orientation were analyzed.
Results: A total of 242 patients were admitted to the ER over 4.5 years. Altered mental status was the cause of admission in 158 (65.3%) cases. In this group, 97 (61.4%) were male, and 73 (46.2%) had a history of relevant diseases. The median age at the ER episode was 36 months (interquartile range (IQR): 16.5–85.0), with a minimum age of 4 days and a maximum of 17 years. The majority of patients (81; 51.3%) were initially managed by pre-hospital care. Seizures were the main cause of admission (64.6%), and 3 (1.9%) were admitted in the ER in cardiorespiratory arrest. Cranioencephalic CT scan was performed in 32.3% and lumbar puncture in 15.8% of the patients. Invasive ventilation was necessary in 19 (12.0%) patients. As a discharge/transfer diagnosis, 49 (31%) patients had febrile or afebrile seizures (1st episode). Infectious causes were identified in 10.1%, intoxication in 7%, and epilepsy in 6.3% of the patients. After stabilization in the ER, 40 (25.3%) patients stayed in the short-stay inpatient unit, and 21 (13.3%) required transfer to the ICU.
Conclusions: Altered mental status represents more than half of all the patients (61.4%) admitted to the ER, although this percentage might be undervalued due to registration errors. Considering the scarcity of available literature, our goal was to clarify our reality and emphasize the need for education and training in emergency situations in order to enable a systematic, quick, and efficient approach.
ID: 194/09-OP-V-d2D: 3
Oral Presentation (Virtual)
Topics: GENERAL PEDIATRICS, NEONATOLOGY
Keywords: breath analysis; ion mobility spectrometry; neonatal incubator; preterm infant; volatile organic compound
Bedside measurement of volatile organic compounds in the atmosphere of neonatal incubators using ion mobility spectrometry
Bous, Michelle1; Steinbach, Julia2; Tutdibi, Erol1; Stutz, Regine1; Kaiser, Elisabeth1; Meyer, Sascha1; Baumbach, Jörg Ingo3; Zemlin, Michael1; Goedicke-Fritz, Sybelle1
1Department of General Paediatrics and Neonatology, Saarland University Medical School, Homburg, Germany; 2Process Analysis & Technology, Reutlingen Research Institute, Reutlingen University, Reutlingen, Germany; 3Technical University Dortmund, Department Bio- and Chemical Engineering, Dortmund, Germany.
Objectives: Early diagnosis of life-threatening diseases such as neonatal sepsis is crucial in the outcome of preterm infants. We hypothesize that volatile organic compounds (VOCs) can be successfully measured in the incubator atmosphere.
Aim: We aim to establish an analysis of VOCs as a rapid, reliable and, most importantly, non-invasive diagnostics in neonatology.
Methods: This feasibility study investigates whether discriminating between occupied and empty incubators is possible by bedside measurement of volatile organic compounds (VOCs) in the neonatal intensive care unit (NICU). VOCs profiles were measured in incubator air using multi capillary column-coupled ion mobility spectrometry (MCC/IMS; BreathDiscovery, B&S Analytik GmbH/ B.Braun Melsungen AG, Dortmund, Germany).
Results: Seventeen incubators occupied by preterm infants (50 measurements) and nine unoccupied incubators were measured, with 37 room air measurements serving as controls. Three VOC signals were identified that allowed discrimination between occupied and unoccupied incubators. The best discrimination was achieved by peak P20 showing a sensitivity, specificity, positive predictive value, and negative predictive value of 94.0%, 88.9%, 97.3%, and 72.3%, respectively. The use of a decision tree improved these values to 100.0%, 88.9%, 98.0%, and 100.0%, respectively.
Conclusion: We developed a bedside method for characterizing VOCs profiles in the atmosphere of neonatal incubators using ion mobility spectrometry. Characterization of the VOCs profiles allowed the differentiation between occupied and empty incubators. Our method provides results within minutes. In further studies, VOCs analysis will be used to identify potential biomarkers to establish non- invasive diagnostics in preterm infants in the future.
ID: 245/09-OP-V-d2D: 4
Oral Presentation (Virtual)
Topics: GENERAL PEDIATRICS, RARE DISEASES
Keywords: Down Syndrome, Chromosomal Disorder, Prenatal diagnosis, Development consultation
Down Syndrome: characterization of the children followed in the Development consultation of our hospital
Pinto, Diana Henriques; Rebelo, Ana Torres; Rodrigues, Sara Sofia S.; Azevedo, Margarida; Monteiro, Virgínia
Centro Hospitalar Entre Douro e Vouga, Portugal.
Introduction: Down syndrome (DS) is one of the most common chromosomal disorders and is the major cause of developmental delay. It is also associated with congenital malformations and specific medical conditions.
Aim: The aim of this study was to characterize the cases of DS in our hospital, aiming to alert to the most common problems.
Methods: The authors characterized the cohort of children attending Development consultation in Centro Hospitalar entre Douro e Vouga between 1999 and 2022.
Results: We have already seen 71 children with DS in our consultation, but only 22 maintain follow-ups at this time. 52% of them were female, and in 10 cases, was made a prenatal diagnosis. (1) In the last decade, the average number of births was 0.7/year, with no births in the majority of the years. The growth of prenatal screening has significantly reduced the number of babies born per year with DS. The average maternal age was 32.4 years. Cardiac (59%), ophthalmologic (46,5%) and otorhinolaryngological (40,8%) pathologies were the most frequent comorbidities. Recurrent lower airway infections (28,5%), endocrinological (28%) and orthopaedic (28%) pathology were also prevalent. (2) Global developmental delay/intellectual developmental disorder was present in all of them, although with a variable spectrum of severity. (3) Most of them were followed up in Early Intervention and Physical Medicine Rehabilitation hospital consultation.
Conclusion: The follow-up of these children involves multidisciplinary assessment and intervention. It is important that the care is standardized so that complications are not missed, enhancing their maximum development and improving their quality of life.
ID: 209/09-OP-V-d2D: 5
Oral Presentation (Virtual)
Topics: GENERAL PEDIATRICS, RARE DISEASES
Keywords: Hereditary Hemorrhagic Telangiectasia, Rendu-Osler-Weber disease, pediatrics
Hereditary Hemorrhagic Telangiectasia – case series report
Queirós, Joana Carvalho1; Ashworth, Joanna1; Barbosa, Telma2
1Pediatrics Departement, Centro Materno infantil do Norte, Centro Hospitalar Universitário do Porto; 2Pneumology Unit, Pediatrics Departement, Centro Materno infantil do Norte, Centro Hospitalar Universitário do Porto.
Background: Hereditary Hemorrhagic Telangiectasia, also known as Rendu-Osler-Weber disease (ROW), is a rare fibrovascular dysplasia that makes vascular walls vulnerable to damage and rupture, which results in bleeding. It has been linked to arteriovenous malformations in several organs, and potential pulmonary complications exist. Treatment is supportive and helps prevent complications.
Case Presentation: We describe two clinical cases followed in a tertiary hospital:
Female, 14 years old, no relevant pathological past history. Evaluated at a Cardiology appointment with syncope and pre-syncope episodes associated with physical efforts. Signs of pulmonary hypertension at echocardiography, confirmed by cardiac catheterization and under sildenafil. She was referred to a Pediatric Pulmonology appointment when she was 5 years old. Frequent epistaxis during airway infection and complaints of fatigue with moderate efforts. Pro-BNP of 636.0 pg/ml. Pulmonary CT with dilatation of the pulmonary artery trunk and its branches; small arteriovenous fistulas. No thoracic deformities or digital hypocratism. No telangiectasias. Angio-CT: “Ectasia of the pulmonary trunk, probably secondary to pulmonary hypertension and arteriovenous malformations.” Respiratory function tests were normal.
Male, 12 years old, referred to a pediatric Pulmonology appointment due to a positive genetic study for ROW (gene ACVRL; c.874C>T p. (Gln292*) variant). Frequent epistaxis, nocturnal dyspnea, wheezing and cough during exercise. Three pneumonias in the previous 3 years. No abnormal findings on physical examination. Cerebral MRI without arteriovenous malformations or aneurysms. The patient started complaining of retrosternal pain and cyanosis after moderate effort. Wheezing, coughing, and frequent self-limited epistaxis persisted. Pulmonary Angio-CT: “Some nodular formations are observed bilaterally, with dimensions not exceeding 4 mm in the LID, as well as 3 and 3.5 mm in the LIE, with a still unspecific aspect”. Due to worsening of respiratory complaints, he started treatment with inhaled bronchodilator and corticoid. Respiratory function tests with: FEV1 2.40 (2.66 after BD, corresponding to 10.7%) | CVF 3.01 | FEV1/CVF 79.73|CPT 3.91. Symptoms at rest improved, with maintenance of dyspnea and wheezing with physical exercise. Epistaxis almost daily.
Discussion: ROW disease is a rare multisystemic disease whose main initial manifestation is recurrent epistaxis. Due to its rarity, high clinical suspicion is necessary for diagnosis. Nevertheless, the best approach to pulmonary complications is still unknown. An early diagnosis allows for an adequate follow-up and, thus, prevention and treatment of possible complications, with a clear improvement in the quality of life of these patients.
ID: 125/09-OP-V-d2D: 6
Oral Presentation (Virtual)
Topics: GENERAL PEDIATRICS, PSYCHIATRY
Keywords: Pediatric Intensive Care Units, Family Member, Psychology, Long-Term Care
Long-term psychological outcomes in family members of pediatric critical illness survivors: a systematic review
Ko, Michelle Shi Min1; Lee, Wai Kit2; Sultana, Rehena3; Murphy, Beverly4; Heng, Katrina5; Loh, Sin Wee6; Poh, Pei Fen6; Lee, Jan Hau1,6
1Duke-NUS Medical School, Singapore; 2Faculty of Medicine, Nursing, and Health Sciences, Monash University, Melbourne, Australia; 3Duke-NUS Medical School, Centre for Quantitative Medicine, Singapore; 4Duke University, Medical Center Library and Archives, North Carolina, United States of America; 5Doctor Anywhere Private Limited, Singapore; 6KK Women’s and Children’s Hospital, Children’s Intensive Care Unit, Singapore.
Background and Objective: Pediatric critical illness exposes the patients’ family members to stressful experiences that can produce long-term psychological repercussions. While post-intensive care syndrome in pediatrics has been described in survivors, little is known about the psychological sequelae experienced by their family members. We aim to systematically review and critically evaluate the medical literature on long-term psychological outcomes of pediatric intensive care unit (PICU) survivors’ family members.
Methods: We searched the following medical databases from inception up to January 2022: PubMed, Embase, CINAHL and PsycInfo. Studies reporting psychological disorders (defined by the Diagnostic and Statistical Manual of Mental Disorders, 5th edition) in immediate family members and caregivers of PICU patients with a follow-up of at least three months were included. Family members of non-survivors and patients discharged under palliative care were excluded.
Learning Points Discussion: Of 4674 articles identified, 28 articles consisting of 18 independent studies (4 randomized controlled trials, 11 prospective and 3 retrospective cohort studies) were included in our review (total patients = 55,477; total parents = 97,235; total grandparents = 26). 8 studies were conducted in the United States of America, 5 in the Netherlands, 2 in the United Kingdom, 2 in Canada and 1 in Spain. [1] Psychological distress was reported in 35.2–64.3% of family members 3 to 6 months after PICU admission; 40.9–53% continued to be affected 1 year later. Post-traumatic stress disorder was diagnosed in 10–42%, 8–32% and 10.5–48% of parents at 3, 6 and 9 months follow-up, respectively. 20.9–52% of parents experienced moderate to severe anxiety 3 to 6 months later. Depression was reported in 7–42.6% of parents over the same period. At their 1 year follow-up, 17–26% of parents continue to suffer from either anxiety or depression. Despite the reported high prevalence of psychological distress, uptake of mental counselling was disproportionately low, with only 0.7–29% of parents seeking help. Risk factors associated with increased risk of psychiatric morbidity include mothers, parents of younger children and longer duration of the PICU stay. Current gaps in the medical literature include the lack of studies examining long-term psychological outcomes in siblings and from specific geographical regions (e.g., Asia and South America) [2]. There is a high burden of psychological sequelae in family members of PICU survivors. Risk stratification to identify high-risk groups and early interventions for family members during PICU admissions need to be explored to reduce subsequent psychological repercussions.
ID: 220/09-OP-V-d2D: 7
Oral Presentation (Virtual)
Topics: GENERAL PEDIATRICS, GASTROENTEROLOGY
Keywords: Inflammatory bowel disease, immunomodulating therapy
Profiling paediatric patients on immunomodulating therapy for inflammatory bowel disease at a regional centre
Palmer, Zoe Maria; Ahmed, Farooq; Murphy, Anne Marie
University Hospital Limerick, Ireland.
Background: Inflammatory bowel disease (IBD) occurs in roughly 396 per 100,000 patients in Ireland, with 25% of diagnoses made before age 20. A further 25% of these are diagnosed before the age of 10, according to recent studies. (1) This review outlines the caseload and disease burden of IBD in a paediatric population of a regional centre in the Republic of Ireland who receive intravenous (IV) therapy as part of their disease management. It examines distribution across multiple parameters, both intrinsic and extrinsic. We also examine the correlation between these highlighted parameters and the number of clinical contacts for each patient.
Methods: Data analysed in this review encompassed 22 paediatric IBD patients attending a regional-level centre in the Republic of Ireland for IV infusions of disease-modifying therapies. The cohort examined was further subdivided by age, sex, rural versus urban residence, ethnicity and number of clinical contacts. Age was measured in months, and ethnicity separated geographical and cultural ethnic groups. Urban living was defined as residing in a large town or city, and rural as living in a small town, village or more remote setting. The number of clinical contacts included inpatient admissions, attendances for IV therapy or phlebotomy, and outpatient clinics. Emergency department attendances were excluded.
Results: A total of 22 paediatric patients attend the centre for clinical review, phlebotomy, and management of IBD through the use of IV therapies. Of these, 21 patients are administered infliximab, and 1 receives adalimumab IV. The mean age was 13 years and 11 months, with the eldest patient being 17 years and 11 months old, and the youngest 7 years old. There were 2 patients aged under 10 years in the group examined. Regarding sex, there were 16 male patients (72.72%), and 6 female (27.28%). Ethnic background included 18 Irish patients (81.81%), two Polish patients (9.09%), one patient with Western African heritage and one patient from the Irish Travelling Community. The distribution of rural versus urban living showed 13 urban-residing patients (59.09%), with the remaining 9 patients living in rural localities (40.91%). The highest number of clinical contacts was 84, with the lowest being 9. The mean number of clinical contacts was 65.
Conclusions: Through this review, we aim to demonstrate the impact of outlined factors on the disease burden of paediatric IBD patients of one Irish regional centre. We contribute to the literature on the rapidly growing incidence of IBD among Irish children.
ID: 221/09-OP-V-d2D: 8
Oral Presentation (Virtual)
Topics: GENERAL PEDIATRICS, RARE DISEASES
Keywords: Recurrent transient myositis
Recurrent transient myositis in childhood: A case report
Palmer, Zoe Maria; Ahmed, Farooq; Murphy, Anne Marie
University Hospital Limerick, Ireland
Background: Transient myositis, also referred to as benign acute childhood myositis, is a self-limiting condition characterised by bilateral lower limb pain and difficulty mobilising with raised creatine kinase (CK), with an associated viral prodrome. It is most commonly seen in school-age males and typically spontaneously resolves within 7 days of the onset of symptoms. (1) Recurrent transient myositis associated with infection is rare, and some theories propose that it may be secondary to autoimmune activity triggered by viral or bacterial antigens, among other pathologies. (2) We report a rare case of recurrent transient myositis in a school- age child and discuss the management of such cases, as well as potential investigations and diagnoses leading to this repeated presentation.
Case Presentation Summary: A previously well, developmentally normal 12-year-old Irish male presented on 3 separate occasions with 3 discrete episodes of transient myositis following viral illnesses over a 3-year period. The initial presentation to the paediatric emergency department (PED) was due to bilateral lower limb pain with subjective weakness and inability to bear weight roughly 48 hours following resolution of upper respiratory tract infection symptoms secondary to Influenza A. Elevated CK levels of 11,988 IU/L (reference range 0.0–0.6 IU/L) and urine myoglobin of 3,314 micrograms/L (reference range 0.0–10.0 micrograms/L) confirmed diagnosis of transient myositis. The patient was admitted for IV fluid hydration and CK monitoring and was discharged home well with advice regarding oral fluid intake. (1) The second presentation occurred 2 years later, following a confirmed diagnosis of SARS-CoV-2 infection. In a similar clinical picture, the patient presented with extreme fatigue and bilateral lower limb pain and weakness. His symptoms were less severe than the initial presentation, with serum CK of 4,063 IU/L. He was discharged from the PED with advice regarding oral rehydration. (2) The patient’s third presentation occurred roughly 8 weeks following the second episode of transient myositis. He had an unconfirmed viral illness in the preceding days in this instance. The patient did not present to the PED at this time but rather to his general practitioner, who measured CK levels at 1,974 IU/L. He was then referred to paediatric outpatients for further investigations.
Learning Points/Discussion: In this case report, the main learning points and discussion will outline the management of acute presentations of transient myositis in the PED setting, appropriate differential diagnoses and investigations in cases of recurrent transient myositis in school-age children. We add our case to the literature on the phenomenon of recurrent transient myositis in children.
ID: 169/09-OP-V-d2D: 9
Oral Presentation (Virtual)
Topics: GENERAL PEDIATRICS, INFECTIOUS DISEASES
Keywords: Kawasaki Disease, Coronary Aneurysms
Refractory Kawasaki Disease in a young infant – Treatment challenges
Amorim-Figueiredo, Rosa1; Lemos, Ana1; Rito, Tiago2,3; Conde, Marta4; Brito, Maria João1; Pinto, Fátima2,3
1Pediatric Infectious Diseases Unit, Dona Estefânia Hospital, Centro Hospitalar Universitário Lisboa Central, Lisbon, Portugal; 2Department of Pediatric Cardiology and Reference Center for Congenital Heart Diseases, Centro Hospitalar Universitário Lisboa Central, Lisbon, Portugal; 3Member of the European Reference Network for Rare, Low Prevalence Complex Diseases of the Heart (ERN GUARD-Heart); 4Pediatric Rheumatology Unit, Dona Estefânia Hospital, Centro Hospitalar Universitário Lisboa Central, Lisbon, Portugal.
Background: Kawasaki disease (KD) is the leading cause of acquired heart disease in children of developed countries. Refractory KD occurs in 10–38% of the cases. It is associated with an increased risk for coronary artery aneurysms, and treatment remains controversial. Few cases of successful treatment of KD with giant coronary artery aneurysms have been reported.
Case Presentation Summary: A previously healthy 8-month-old male infant with unremarkable medical history presented with a four-days high-grade continuous fever and maculopapular erythematous rash of the face, trunk, palms and soles (Figure ), associated with diarrhoea, cleft lips and strawberry tongue. Laboratory findings showed elevated inflammatory markers (PCR 250 mg/L and ESR 75 mm/h) and four criteria of incomplete KD (normochromic normocytic anemia, hypoalbuminemia, ALT elevation and sterile pyuria). Echocardiogram was normal. KD was assumed, and IVIg (2 g/kg), methylprednisolone (2 mg/kg/day), and lysine acetylsalicylate (30 mg/kg/day) were initiated, but fever resurged and persisted >48 h after 1st IVIg. A 2nd dose of IVIg (2 g/kg) was administered, after cardiac involvement exclusion, ceasing the fever. But there was a new recurrence of fever, and left main coronary (LMCA)/left anterior descending (LAD) and right coronary artery (RCA) dilation were diagnosed. Anticoagulation was initiated, and anakinra was prescribed. Sustained apyrexia and rash involution were achieved at this point, but inflammatory markers remained elevated and coronary changes continued progressing, later developing giant aneurysms. A 3rd dose of IVIg (2g/kg), methylprednisolone pulses (30 mg/kg/day) for 5 days and IV infliximab were administered. Apyrexia and normalization of inflammatory markers were reached, but coronary aneurysms continued to increase, reaching their maximum on the 36th day of illness—LMCA with aneurysmal dilatation of 6.7 mm (z-score+13.4), LDA with proximal aneurysm of 5.5 mm (z-score+18) and distal aneurysm of 7.5 mm (z-score+27), and RCA with proximal aneurysm of 6.8 mm (z-score+17). Treatment with propranolol was started and titrated under continuous cardiac monitoring until beta-blockade was achieved with the aim of reducing the heart rate and the sheer stress of the coronary arteries. This child was discharged 2 months after hospitalization, and at the 8-month-follow-up, the aneurysms were getting smaller.
Discussion: This is a rare case of refractory KD with major late cardiac involvement, albeit early recognition and adequate treatment, showing that serial cardiac evaluations to recognize cardiac involvement are important. This case is interesting because coronary aneurysms continued to increase after controlling clinical and laboratory inflammation, and heart rate reduction was essential to minimize the rupture risk of the coronary arteries.
ID: 102/09-OP-V-d2D: 10
Oral Presentation (Virtual)
Topics: GENERAL PEDIATRICS
Keywords: BMI, height, weight, general anaesthesia
Service Evaluation: Are Community dental operators recording BMI appropriately for children undergoing dental extractions under General Anaesthesia?
Antony, Teena Sara
UK
Introduction: Healthcare providers use body mass index (BMI) to determine height and weight to work out a healthy weight. A retrospective study within the Community service to assess the recording of BMI in paediatric patients undergoing extractions under general anaesthetic. Recording BMI is an important aspect of facilitating treatment plans and their outcomes. This service evaluation aims to assess current practices and advance improvements as needed.
Standards: The standards are based on guidance by the Royal College of Anaesthetists, emphasising the need for recording weights and body mass index before general anaesthetic. The standard GA proforma form across the trust was the local template used. 100% of patients should have their height, weight and BMI recorded.
Aims: 1 To determine if the height and weight are recorded for all patients. 2 To determine if the BMI is recorded appropriately for all patients admitted for a tooth removal under general anaesthesia on the community dental service—paediatric list at the hospital. 3 To understand if children, their families, and healthcare providers (GDP and GMP) are made aware the child is outside the range considered to be a healthy weight and given advice.
Method: Retrospective consecutive record analysis from September 2019-March 2020. Records from our local hospital site were reviewed post-general anaesthetic treatment. Data were input into an excel tables spreadsheet for age, height, weight, and BMI. If BMI was not recorded, it was reviewed for any other reasons.
Results: In the period from September 2019-March 2020, 140 general anaesthetic cases were held at the local hospital site. The records were assessed, 27 records could not be retrieved due to Covid-19 restrictions at the site. Of the remaining 113 records, 102 had both height and weight recorded; however, only 48 had the BMI recorded. Out of 48 records, 26 records scored as unhealthy BMI. None of the records recorded any onward referral for advice on weight management.
Conclusion: Nearly half of the records failed to record BMI. In 10% of cases, there was insufficient data to calculate the BMI. There are no specific referral sites for patients with unhealthy BMI.
Recommendations: Staff awareness and training- presentation at a local quality assurance staff meeting and a poster displayed in the department. A re-audit will be done in 12 months. This study developed a need for a pathway for onward referral in patients with high BMI.
ID: 134/09-OP-V-d2D: 11
Oral Presentation (Virtual)
Topics: NEUROLOGY
Keywords: Neuromuscular disorder, Werdnig-Hoffmann disease, Hypotonia
Unexplained hypotonia in an infant
Rebelo, Ana1; Azevedo, Inês1; Pinto, Diana1; Menezes, Catarina2; Garrido, Cristina3; Maio, Inês1
1Centro Hospitalar entre Douro e Vouga, Portugal; 2Centro Materno Infantil do Norte (CMIN), Pediatrics, Porto, Portugal; 3Centro Materno Infantil do Norte (CMIN), Neuropediatrics, Porto, Portugal.
Introduction: Spinal muscular atrophy (SMA) is a rare and severe neuromuscular disorder caused by an autosomal recessive mutation in the survival motor neuron 1 (SMN1) gene. Type 1 SMA, also known as infantile spinal muscular atrophy or Werdnig- Hoffmann disease, is the most severe form.
Case Report: A 5-month-old girl with a history of hypotonia and poor weight gain presented to the emergency department with a 12-hour history of fever, cough and respiratory distress. The mother denied feeding problems, weak sucking or recurrent respiratory infections. She was born at term, appropriate for gestational age and didn’t need resuscitation. On physical examination, she was tachypneic, but oxygen saturation was normal. Subcostal and intercostal retractions were observed with normal pulmonary auscultation. She appeared alert and exhibited a social smile, but her posture was severely hypotonic, and she could not control her head. Deep tendon reflexes were absent, but tongue fasciculations were not observed. Blood tests were normal, and the chest radiograph showed a bell-shaped thorax. She was admitted with suspected spinal muscular atrophy associated with respiratory distress and transferred to a centre with neuropediatrics. Genetic testing revealed mutations in the SMN1 gene with 2 copies of the SMN2 gene. Her disease progressed to severe respiratory insufficiency, requiring mechanical ventilation (Figure ).
Discussion Points: SMA is the most common genetic cause of early infant death. The presence of three or more copies of modifying genes (SMN2) is associated with a milder phenotype. Our patient had only 2 copies; therefore, the overall prognosis is poor. Some cases show early feeding difficulties or a weak cry, but respiratory distress is usually the presenting clinical symptom, as in our case. Weakness of the respiratory muscles leads to progressive respiratory failure, resulting in death at an early age. The treatment used to be mainly supportive and aimed to promote feeding and breathing. In the last decade, drug development for SMA has made tremendous progress. Therapies targeting the underlying disease mechanism include nusinersen for the treatment of all types of SMA and onasemnogene abeparvovec-xioi for the treatment of type 1 SMA. These treatments stop the progression of the disease and allow the acquisition of developmental milestones that these children would never achieve in the natural course of the disease.
Discussion: The diagnosis of SMA should be suspected in any infant with unexplained weakness or hypotonia. Type 1 SMA is a rare entity, but it is important for the pediatrician to be familiar with this condition because of its severe implications.
ID: 185/09-OP-V-d2D: 12
Oral Presentation (Virtual)
Topics: RARE DISEASES, NEUROLOGY
Keywords: Hypotonia, Hyporreflexia, Spinal Muscular Atrophy, Neurodegenerative disorder
Different forms of presentation for the same disease
Pinto, Diana Henriques1; Leuzinger-Dias, Catarina1; Rebelo, Ana1; Souza, Denise1; Garrido, Cristina2; Santos, Manuela2; Tavares, Susana1
1Serviço de Pediatria e Neonatologia, Centro Hospitalar Entre Douro e Vouga, Portugal; 2Serviço de Neuropediatria, Centro Materno Infantil do Norte, Centro Hospitalar do Porto.
Background: Spinal Muscular Atrophy (SMA) is a neurodegenerative disorder of motor neurons usually present in infancy and childhood. It is an autosomal recessive disorder caused by homozygous or compound heterozygous loss of function of the survival motor neuron gene 1 (SMN1). This deficiency causes the degeneration of alpha motor fibres and neuromuscular dysfunction, leading to a phenotypic spectrum classified by the age of onset and clinical course.
Case Presentation Summary: Case 1: A 3-month-old boy, born at 34 weeks and 4 days, with maintained hypotonia and hyporreflexia, was evaluated in a neonatology consultation where he presented tachypneic and tachycardic. There was no history of fever or other associated symptoms. He was admitted to the emergency department, but soon he needed non-invasive ventilation support and was transferred to a centre with pediatric neurology. Molecular genetic analysis confirmed the diagnosis of SMA1. Case 2: An adolescent male, with 13 years old, was referred to pediatric neurology consultation because of muscle weakness in both legs in the last months causing difficulties in performing basic activities during his sports classes. EMG revealed pronounced chronic reinnervation with active denervation in the proximal muscles of the lower limbs. Molecular genetic analysis showed the absence of the SMN1 gene in a homozygous state and the presence of four copies of the SMN2 pseudogene. This finding confirmed SMA3. Case 3: A 25-day newborn baby was referred to pediatric neurology consultation with suspected SMA. He presented with hypotonia and hyperreflexia since he was born. His pregnancy and birth history were unremarkable, and there was no family history of neuromuscular or neurologic disorders or congenital malformations. The neurological assessment revealed absent deep tendon reflexes and poor head and neck control, and SMA1 was confirmed in genetic analysis. Case 4: A 5-month-old girl with global developmental delay and poor weight gain presented to the emergency department with a 12-hour history of fever, cough and respiratory distress. She was tachypneic but with normal pulmonary auscultation and was severely hypotonic. Deep tendon reflexes were absent. She was admitted with suspected SMA associated with respiratory distress and transferred to a centre with pediatric neurology, where the diagnosis was made.
Learning Points Discussion: SMA is sometimes difficult to diagnose, as symptoms can resemble other conditions or medical problems. However, making a diagnosis as soon as possible is extremely important as the prognosis depends on that. With these cases, we aimed to show different types of presentation of this disease.
Session
10-PT-V-d3A: Poster Presentations Session 10 - Day 3 - Zone A
Presentations
9:00am - 9:10am
ID: 159/10-PT-V-d3A: 1
Poster Presentation (Virtual)
Topics: ADOLESCENT MEDICINE
Keywords: Aggressivity, bullying, adolescents, Georgia
Aggressive behavior and bullying among adolescents in Georgia
Pagava, Karaman1; Shengelia, Lela2,3; Phagava, Helen1; Sturua, Lela3; Chiraqadze, Sofio3; Zedgenidze, Julia3; Getia, Nana3; Liluashvili, Levan3
1Tbilisi State Medical University, Georgia; 2University of Georgia; 3Georgian National Center for Disease Control and Public Health.
Background: can be considered as the important health-related behaviour indicator in adolescents. Unfortunately, the corresponding data are scarce, particularly regarding the trends, at least in Georgia. We aimed to define these indicators and their change over the period from 2005 to 2018 in adolescents in Georgia.
Design and Methods: Comparative analysis of the repeated cross-sectional studies conducted throughout Georgia in the years 2005 and 2018. Both studies were done by self-administered questionnaires. The first study was performed in the frame of the Georgian-Swiss Scientific project (sponsored by Swiss National Scientific Foundation SCOPES 7GEPj065646), the second one in the frame of the international Health Behavior in School-Aged Children (HBSC) project supported by the WHO Europe. There were compared data received from the adolescents—first sample (mean age 15.5 ± 1.1)—9490 (61.4% females, 39.6% males); second one (aged 15 years)—respectively 1345 (51.3% and 48.7%).
Results: I sample—during the last year before the investigation, 16.6% of adolescents (females 13.9%, males 18.6%) were the victims of physical abuse; 17.2% (14.4% and 19.3%) adolescents themselves attacked an adult, 26.5% (18.2% and 36.3%) carried weapons, and 33.8% (32.0% and 35.0%) used them in a fight. 22.5% (23.0% and 10.6%) correspondingly were bullied, 23.1 (22.4% and 22.4%) were excluded from the everyday activity by peers. II sample—10.1% (4.4% and 16.2%) of respondents mentioned their aggressive behaviour, 5% of girls and 17% of boys reported that they had been involved in a physical fight. 6.1% (4.3% and 6.2%) were victims of bullying, 10.2% (8.2% and 11.%3) were bullies. Cyberbullying was revealed in 12.1% (8.3% females and 14.7% males), 10.8% (8.7% and 11.7%) were cyberbullies. The unidirectional shifts were not detected.
Conclusions: There are presented descriptive data about aggressive behaviour, bullying and cyberbullying in adolescents in Georgia. We suppose that they can be used as baseline information for planning and assessing the efficacy of special measures in this direction.
ID: 227/10-PT-V-d3A: 2
Poster Presentation (Virtual)
Topics: ENDOCRINOLOGY
Keywords: Congenital hypothyroidism, quality of life, neurodevelopment pathologies
Quality of life in children with congenital hypothyroidism
Curval, Ana Rita; Almeida, Paulo; Castro-Correia, Cíntia
CHUSJ, Portugal.
Background: Congenital hypothyroidism (CH) is a chronic disease characterized by inborn thyroid hormone deficiency that may negatively affect patients’ quality of life (QoL). Pediatric Quality of Life. Inventory 4.0 (PedsQL™) is a validated tool to assess health- related QoL (HRQoL).
Methods: A cross-sectional study including 43 patients with CH was carried out in the pediatric endocrinology department. PedsQL™ was applied to the parents. Patients were divided into four groups according to age: 2–4, 5–7, 8–12, and 13–18 years old. The control group consisted of healthy individuals from the instrument’s validation studies for the Portuguese population and the standard control population used in the PedsQL™ validation study.
Results: Forty-three, 27 (62,8%) girls and 16 (37,2%) boys were included in the study. The median age was 9,2 ± 4,4 years. Sixteen patients had concomitant neurodevelopment pathologies, such as attention deficit hyperactivity disorder (eight patients), intellectual development disorder (six patients) and language delay (two patients). Our results showed that children with congenital hypothyroidism report worse quality of life when compared to healthy children.
Conclusion: This study has shown that children with CH, diagnosed by neonatal screening, are at increased risk for impaired quality of life and self-worth. Thus, it seems important to stimulate children’s social performance and support them with their social skills.
ID: 179/10-PT-V-d3A: 3
Poster Presentation (Virtual)
Topics: GENERAL PEDIATRICS
Keywords: Autism spectrum disorder, Parents, Social support, Family, Friends
Social support in parents of children with autism spectrum disorder
Curval, Ana Rita; Viana, Victor; Guardiano, Micaela
Centro Hospitalar Universitário de São João, Portugal.
Background: The symptoms and concomitant challenging behaviours associated with Autism Spectrum Disorders (ASD) present parents and children with many adverse outcomes, including but not limited to higher parental stress, poor sibling adjustment, family functioning, disruptive behaviour, and social isolation. (1) Social support, especially as provided by close family and friends, has been consistently identified as one of the most powerful predictors of psychological adjustment among parents raising children with ASD.
Methods: Our pediatric development department carried out a cross-sectional study including 51 parents of children with ASD. The study’s objective was to verify the degree of satisfaction of the participants regarding their family, friends, intimacy, and social activities. Data were gathered from participating parents using questionnaires and interviews. (1) According to DSM-5, ASD has been classified into three levels of severity: LEVEL 1—“Requiring support”, LEVEL 2—“requiring substantial support”, and LEVEL 3—“requiring very substantial support”. The instrument used to assess the social support given by parents was the “Social Support Satisfaction Scale”.
Results: The final parent sample consisted of 30 mothers and 21 fathers. Parent age ranged from 28 to 53 years, with a mean of 39,2 (SD = 5,7) years. In terms of child characteristics, 88% were male, and 12% were female, with a mean age of 6,4 years (SD = 3,0). (1) According to DSM-5, 54% of children were classified as level 1, 28% as level 2 and 18% as level 3. 25% of the children were reported by the parent to be primarily nonverbal. Six families had at least one other child who was also diagnosed with ASD. (2) The individualized analysis of the 4 dimensions that the study included showed that the degree of satisfaction of the parents with children with ASD is higher regarding family, followed in descending order by friends, intimacy, and social activities. (3) There was a negative correlation between the children’s age and the degree of parental satisfaction. (4) The relationship between the level of ASD and parental satisfaction wasn’t associated with statistically significant differences.
Conclusion: Based on study findings regarding the importance of help from parents’ informal social network, special attention in this regard should be focused on developing services that assist parents in making more effective use of existing sources of support from family members, friends, and other parents of children with ASD.
ID: 160/10-PT-V-d3A: 4
Poster Presentation (Virtual)
Topics: INFECTIOUS DISEASES, COVID-19
Keywords: Antibiotic stewardship, COVID-19, Georgia
Antibiotic stewardship in Georgian hospitals before and during the COVID-19 pandemic
Pagava, Karaman; Korinteli, Irma G; Phagava, Helen; Korinteli, Irine A
Tbilisi State Medical University, Georgia.
Background: Antibiotic therapy is one of the most important components of the management of infectious diseases. We aimed to study the guideline compliance and usage of quality indicators in antibiotic treatment in hospitals and compare data before and during the COVID-19 pandemic.
Methods and Materials: The Global-PPS was conducted in 25 Georgian hospitals in 2017–2021. The Survey included 1075 inpatients receiving an antibiotic on the day of PPS within 94 adult and pediatric wards. Data were analyzed according to the Global PPS methodology (www.global-pps.com). There were compared data from 2017–2019 (pre-epidemic period) and 2020–2021(period of epidemic).
Results: The average rate of guideline compliance in hospitalized patients at the time of the pandemic was 91.6%, significantly higher than the average guideline compliance rate in the pre-pandemic period (71.9%). The highest rate was achieved in 2021 (92.0%), and the lowest was in 2019 (68.2%). Compared to the pre-pandemic period, the average rate of the usage of quality indicators improved as well: “Reason in note” increased from 54.4% in the pre-pandemic to 72.5% in the pandemic period, and stop/review date increased from 19.3% to 32.6%. Antibacterial treatment average rates based on the infection biomarkers (C-reactive protein, procalcitonin, leukocytosis) increased from 81.3% in the pre-pandemic to 87.5% in the pandemic period. The increase in the use of procalcitonin was most pronounced (1.4% in the pre-pandemic to 13.2% in the pandemic period).
Conclusions: According to our data, antibiotic therapy guideline compliance and usage of the quality indicators significantly increased during the period of the Covid-19 epidemic in hospitalized patients in Georgia. Our results confirm the effectiveness of the PPS method for the assessment of the quality level of antibiotic therapy. Thus, the method can be successfully used for this purpose.
ID: 161/10-PT-V-d3A: 5
Poster Presentation (Virtual)
Topics: ALLERGY, IMMUNOLOGY & RESPIRATORY
Keywords: Blood rheology, children, allergic diseases
Blood rheology in children with allergic conjunctivitis and rhinosinusitis
Pagava, Karaman1; Mantskava, Maia1,2,3; Momtselidze, Nino2,3; Toklikishvili, Marika2
1Tbilisi State Medical University, Tbilisi, Georgia; 2Laboratory of Rheology and Diagnostic Analytical Services, Ivane Beritashvili Center of Experimental Biomedicine, Tbilisi, Georgia; 3UNIK-Kutaisi University, Kutaisi, Georgia.
Background: Blood is a heterogeneous system consisting of formed elements: erythrocytes, leukocytes, platelets, and plasma. Formed elements are suspended in a colloidal solution of electrolytes, proteins and lipids. The rheological properties of blood largely depend on the structure and function of erythrocytes. Data on the rheological properties of blood in children with allergies are scarce; there is not enough information about RBC membrane properties, such as aggregability and formability in children with allergies. We aimed to study rheological properties in children with allergies.
Methods: We investigated children with allergic conjunctivitis and rhinosinusitis (n = 18, mean age 15 ± 1,3 years), as well as control children with the same average age (n = 10, mean age 15 ± 0,8 years). The disease was diagnosed based on a comprehensive clinical examination, incl. functional and laboratory studies, as well as the results of allergic tests. To determine the rheological properties of blood, we defined the so-called “Red blood rheological coefficient”. This is an original authorized method developed in the Laboratory of Rheology and Diagnostic Analytical services at Ivane Beritashvili Center of Experimental Biomedicine. The data obtained were processed by variational statistics methods with calculating the reliability of numerical differences.
Results: Our studies have shown that pollen allergens played a decisive role in the etiology of allergic conjunctivitis and rhinosinusitis. It turned out that there were disturbances in the rheological properties of blood in the allergic group compared to the control group, and the degree of change in the rheological coefficient directly depended on the severity of the disease.
Conclusions: Children with allergic conjunctivitis and rhinosinusitis have significant changes in the blood’s rheological properties. Their degree and intensity depend on the severity of the clinical course of the disease. Determining indicators characterizing the disturbance of the rheological properties of blood in combination with other clinical and laboratory data might have a prognostic value in allergic diseases in children and contribute to personalized treatment.
ID: 106/10-PT-V-d3A: 6
Poster Presentation (Virtual)
Topics: HAEMATOLOGY/ONCOLOGY, COVID-19
Keywords: COVID-19, Pediatrics, Sickle Cell, Posterior reversible encephalopathy syndrome (PRES), Vaccination
Challenges in the management of multi-system inflammatory syndrome complicated by posterior reversible encephalopathy syndrome in a pediatrics patient with sickle cell disease and COVID-19.
Nguyen, Amy; Ott, Kristen; Assanasen, Chatchawin
University of Texas Health Science Center at San Antonio, United States of America.
Background: In May of 2020, the Center for Disease Control (CDC) sent out an emergency alert for a new phenomenon called multi-system inflammatory syndrome in children (MIS-C) that presents with gastrointestinal symptoms, mucocutaneous rash, myocarditis, coagulopathy, neurological manifestations, and shock in children infected with SARS-CoV-2. Although there are now established guidelines for treatment in the general pediatric population with MIS-C, there are no current recommendations for identifying and treating children with both MIS-C and sickle cell disease (SCD).
Case Description: A fully vaccinated 17-year-old female testing positive for COVID-19 with SCD, asthma, restless leg syndrome (RLS), essential hypertension (HTN), chronic vitamin D deficiency, and chronic opioid use presents to the emergency department with a 2-day history of worsening cough and 1 day of history of worsening chest and abdominal pain. The patient met criteria for acute chest syndrome and was placed on the appropriate treatment regimen, including broad-spectrum antibiotics. Given the patient’s recent SARS-CoV-2 infection, persistent fever, and leukocytosis, MIS-C was suspected, and inflammatory markers were collected, supporting the diagnosis. Anticoagulation with enoxaparin and a 5-day course of methylprednisolone followed by a subsequent 2- week prednisone taper were initiated. IVIG infusion was deferred due to the patient’s increased predisposition to thrombosis secondary to her SCD. Fluctuations in blood pressure due to pain similar to previous episodes of acute chest syndrome were noted, and home antihypertensive continued. Despite therapy, the patient later developed an acute headache followed by a rapid decline in mental status concerning posterior reversible encephalopathy syndrome (PRES), leading to intubation and exchange transfusion. The patient was able to be extubated after two days following strict control of blood pressure and made a full recovery to baseline in subsequent visits.
Learning Points Discussion: This observation allows for the further identification of complications of COVID-19 infection in SCD pediatric patients and calls for a lower threshold of suspicion in physicians for MIS-C regardless of vaccination status in pediatric patients with chronic diseases such as SCD.
ID: 251/10-PT-V-d3A: 7
Poster Presentation (Virtual)
Topics: DERMATOLOGY
Keywords: atopic dermatitis, disease burden, disease management strategies, Europe
Disease burden of pediatric atopic dermatitis in five European countries
Weidinger, Stephan1; Simpson, Eric L.2; Silverberg, Jonathan I.3; Mnif, Tarek4; Thomas, Ryan B.5; Chuang, Chien-Chia6; Rossi, Ana B.6
1University Hospital Schleswig-Holstein, Campus Kiel, Kiel, Germany; 2Oregon Health and Science University, Portland, OR, USA; 3The George Washington University School of Medicine and Health Sciences, Washington, DC, USA; 4Cerner Enviza, Paris, France; 5Regeneron Pharmaceuticals Inc., Tarrytown, NY; 6Sanofi, Cambridge, MA, USA.
Background: Improved knowledge of atopic dermatitis (AD)-related disease burden may be informative for disease management strategies. We describe the impact of AD across severity strata on children and adolescents in Europe.
Methods: EPI-CARE is an international cross-sectional, web-based survey of pediatric patients aged 6 months to 17 years with AD in 18 countries. We present disease burden results from five European countries (Italy, France, the UK, Spain, and Germany). Eligible participants were identified as having “diagnosed AD” based on meeting all items of the International Study of Asthma and Allergies in Childhood criteria and parent/guardian/self-report of ever being told by a physician that their child/they had eczema (parent/guardian- reported for children [6 months to 11 years of age]; self-reported by adolescents [12 to less 17 years]). Infants/preschoolers up to and including 5 years of age were required to meet two additional criteria: (1) itchy rash affecting the face (cheeks, forehead) at any time; and (2) itchy rash affecting elbow to wrist or knee to ankle at any time. AD severity over the last week was assessed using the Patient Global Assessment (parent/guardian-reported for children; self-reported by adolescents) as clear/mild, moderate or severe. We report worst scratch/itch and worst skin pain (past 24 hours/today), sleep quality (previous night), Infant’s Dermatitis Quality of Life (IDQOL; past week; age <4 years), Children’s Dermatology Life Quality Index (CDLQI; past week; age ≥4 years), days missed from school for AD-related reasons (past 4 weeks), and atopic comorbidities.
Results: Among 2700 children/adolescents with “diagnosed AD”, 62.1% had clear/mild AD, 32.8% moderate AD, and 5.0% severe AD. Mean worst scratch/itch and skin pain and sleep quality ranged from approximately 3 (clear/mild) to 7 (severe), while mean IDQOL/CDLQI scores ranged from around 8 (clear/mild) to 20 (severe) (Table ). Many had missed ≥1 school day in the last 4 weeks (57.4–86.7% across severity strata), for means of 4 (mild) to 10 (severe) days; and most had ≥1 atopic comorbidity (78.1–92.3% across severity strata). Disease burden increased significantly with AD severity (Table ).
Table 1. AD burden by disease severitya in the last week
Conclusions: AD is a symptomatic condition that affects sleep, quality of life, and schooling in children/adolescents. Many patients with AD had the added burden of atopic comorbidities (mainly seasonal allergies and asthma).
ID: 252/10-PT-V-d3A: 8
Poster Presentation (Virtual)
Topics: DERMATOLOGY
Keywords: atopic dermatitis, family burden, caregiver burden, disease management strategies, Europe
Impact of atopic dermatitis in a pediatric population on caregivers and families in five European countries
Silverberg, Jonathan I.1; Simpson, Eric L.2; Weidinger, Stephan3; Mnif, Tarek4; Thomas, Ryan B.5; Chuang, Chien-Chia6; Rossi, Ana B.6
1The George Washington University School of Medicine and Health Sciences, Washington, DC, USA; 2Oregon Health and Science University, Portland, OR, USA; 3University Hospital Schleswig-Holstein, Campus Kiel, Kiel, Germany; 4Cerner Enviza, Paris, France; 5Regeneron Pharmaceuticals Inc., Tarrytown, NY, USA; 6Sanofi, Cambridge, MA, USA.
Background: Improved knowledge of the atopic dermatitis (AD)-related family and caregiver burden may be informative for disease management strategies.
Methods: This cross-sectional, web-based, self-report survey of pediatric patients (0.5 to 17 years) was conducted in 18 countries in 5 regions. Parents were invited to participate without knowledge of the survey topic. Quotas were set for age, sex, region (and urban/rural split in some countries), and a weighting adjustment was applied to obtain a representative population for each country. Patients were categorized as having “diagnosed AD” if they: (1) ever had an intermittent itchy rash for ≥6 months AND had this rash in the past 12 months AND it was in the elbow folds, behind the knees, in front of the ankles, under the buttocks, or around the neck/ears/eyes AND (2) self-reported being diagnosed with AD (eczema) by a physician AND (3) for children aged <6 years, had an itchy rash affecting the face AND elbow–wrist or knee–ankle at any time. AD severity in the past week was rated as clear, mild, moderate, or severe by caregivers (of children aged <12 years) or adolescents (aged ≥12 years) using Patient Global Assessment. We report caregiver-reported Dermatitis Family Impact (DFI) scores (range 0–30; past week), hours spent taking care of the child/adolescent due to AD (past week), and days missed from work for AD-related issues (past 4 weeks) from 5 European countries (Italy, France, UK, Spain, Germany).
Results: Among 2,700 children and adolescents with “diagnosed AD”, mean DFI scores increased significantly with AD severity, from 6.9 for patients considered to have clear/mild AD to 17.9 for patients with severe AD (Table ). Overall mean time spent taking care of the child/adolescent due to AD in the past week ranged from 4.2 hours (clear/mild AD) to 14.9 hours (severe AD). Many employed/self-employed caregivers reported missing ≥1 workday for the child’s/adolescent’s AD-related issues in the last 4 weeks (50.1–90.9% across severity strata), for a mean of 6.0 workdays missed for caregivers of children with severe AD (Table ). Results by country are presented in the Table .
Table 1. Caregiver/family burden associated with AD by caregiver-/adolescent-reported disease severity in the last week
Conclusions: Living with and caring for a child or adolescent with AD can have a substantial impact on the lives of caregivers and other family members, as measured by the DFI questionnaire, time performing AD care, and workdays missed for AD-related reasons. Caregiver and family burden increased significantly with the increasing severity of AD in this pediatric population.
ID: 141/10-PT-V-d3A: 9
Poster Presentation (Virtual)
Topics: PSYCHIATRY
Keywords: Oral-facial-digital type 1 syndrome, autism, OFD1 gene variant
Oral-facial-digital type 1 syndrome in a child with autism spectrum disorder
Budisteanu, Magdalena1,2,3; Papuc, Sorina Mihaela2; Erbescu, Alina2; Nedelcu, Cristina1; Arghir, Aurora2
1Prof. Dr. Alex. Obregia Clinical Hospital of Psychiatry, Romania; 2Victor Babes National Institute of Pathology, Bucharest, Romania; 3Titu Maiorescu University, Faculty of Medicine, Bucharest, Romania.
Background: Oral–facial–digital syndromes (OFDS) represent rare genetic conditions with a complex phenotype, including dysmorphic facial features, oral and digital anomalies, brain malformations, and intellectual disability. OFD type 1 is the most common subtype of OFD, caused by X-linked heterozygous mutations of OFD1 gene. In this paper, we present the case of a child with a complex phenotype, including autistic behaviour.
Case Presentation Summary: A 3-year-old girl was referred to the Department of Child Psychiatry for speech delay. She had a history of oral malformation—bifid tongue and oral choristoma operated on at the age of 22 months. The clinical evaluation showed deep-set eyes, anteverted nostrils, high-arched palate, missing lower central incisors, microretrognathia, severe speech delay (she says only one word), autistic behaviour (poor eye contact, stereotypic movements, difficulties in social interaction and adaptation to new situations). The psychological evaluation revealed a QD of 60 and an ADOS score of 20. Brain MRI showed bilateral periventricular heterotopia. She has an older brother with Asperger syndrome associated with a 22q11.21 duplication. [1] DNA extracted from whole blood was used for genetic characterization by array-based comparative genomic hybridization—array-CGH (Agilent Technologies) and of whole exome sequencing—trio WES (child and parents) (Illumina). [2] The genomic profile based on array-CGH was normal, while trio analysis of WES data revealed a de novo variant in the OFD1 gene (NM_003611.2:c.260A>G; NP_003602.1:p.Thy87Cys). This rare variant (rs312262818) was predicted by several computational methods to be deleterious. It was previously reported as pathogenic by Bruel et al. (2017) in a female fetus with hamartoma, bifid tongue, and brain malformation (corpus callosum agenesis and vermian anomalies). Autistic behaviour was rarely reported in patients with OFD1.
Learning Points Discussion: OFD1 is a complex genetic disorder including mainly dysmorphic facial features, oral and digital abnormalities, and different types of brain malformations; intellectual disability was reported in about 50% of cases, usually mild. Autistic behaviour should be considered one of this syndrome’s additional features.
Funding
The research leading to these results has received funding from the EEA Grant 2014–2021, under the project contract No 6/2019, and by grants of the Romanian National Authority for Scientific Research Innovation, CCCDI-UEFISCDI, Projects number 87/2019 and 88/2019, COFUND-ERANET E-RARE 3-HETER-OMICS-2, within PNCDI III.
ID: 239/10-PT-V-d3A: 10
Poster Presentation (Virtual)
Topics: NEUROLOGY
Keywords: Epstein - Barr virus, pediatric encephalitis, basal ganglia
Pediatric Epstein - Barr virus associated encephalitis: a case report
Pedrosa, Inês1; Pereira, Ângela2; Figueiroa, Sónia3; Garrido, Cristina3
1Department of Pediatrics, Centro Hospitalar de Leiria, Portugal; 2Department of Pediatrics, Hospital de Braga, Portugal; 3Pediatric Neurology Unit, Centro Materno-Infantil do Norte, Centro Hospitalar Universitário do Porto, Portugal.
Background: Infective encephalitis in the pediatric population is a potentially severe medical condition with high morbidity and long-term sequelae. Establishing a diagnosis of Epstein-Barr virus (EBV) encephalitis can be difficult because most patients don’t show typical symptoms of infectious mononucleosis. Nevertheless, EBV infection can be suspected in the presence of MRI findings of high signal intensities in basal ganglia and documented with serologic tests. The prognosis is usually favourable, with no neurologic sequelae.
Case Presentation Summary: A previously healthy 12-year-old male was admitted to the emergency department for a 2-day history of headache, fever and impaired mental status/bizarre behaviour followed by an episode of generalized seizures (lasting 15 minutes). Upon admission, he appeared lethargic and unresponsive to verbal commands, but no focal neurological deficits were present. The blood panel showed negative inflammatory markers, and the brain CT scan had nonspecific findings. CSF analysis revealed no pleocytosis, normal glucose level and protein 1.02 g/L. Treatment with acyclovir, ceftriaxone and levetiracetam was initiated. At first, the patient’s neurological condition deteriorated, leading to the association of methylprednisolone. During the hospital stay, an EEG showed generalized slow brain electrical activity, and a brain MRI revealed a pattern suggestive of encephalitis with involvement of the basal ganglia (high signal intensities mainly in the left lenticular nucleus), raising the suspicion for an EBV infection as the causative agent. Serologic testing was compatible with acute EBV infection. EBV was also detected in the CSF by PCR. Extensive work-up excluded auto-immune and other infectious causes of encephalitis. Antibiotic treatment was discontinued after negative microbiologic studies. He completed a 10-day course of antiviral therapy plus 3-day of IV corticosteroids administration. At discharge, he still had mild hypokinesia and impaired writing skills. No prodromal symptoms prior to the onset of neurologic symptoms were reported. The patient remains under follow-up in the outpatient setting, with a normal neurological evaluation 2-months after discharge.
Learning Points Discussion: EBV encephalitis isn’t usually associated with an infectious mononucleosis syndrome but should be considered in cases of acute illness of uncertain etiology in the pediatric population and when lesions are localized to the basal ganglia. The laboratory diagnosis is greatly enhanced by the concomitant use of EBV-specific serology and PCR. The role of antiviral therapy and corticosteroids in the management of EBV-associated encephalitis has not been adequately studied to date, but given the potential implications of the disease, it is reasonable to consider such therapies on an individual basis.
ID: 152/10-PT-V-d3A: 11
Poster Presentation (Virtual)
Topics: GASTROENTEROLOGY
Keywords: anti-TNF, Crohn’s Disease, treatment
Real-world Scottish experience of anti-TNF therapy in Crohn’s disease 2016-2020 against ECCO-ESPGHAN recommendations
Scott, Gregor1; Hansen, Richard1; Chalmers, Iain2.
1Department of Paediatric Gastroenterology, Hepatology and Nutrition, Royal Hospital for Children, Glasgow, UK.; 2Department of Paediatric Gastroenterology, Hepatology and Nutrition, Royal Aberdeen’s Children Hospital, Aberdeen, UK.
Background: ECCO-ESPGHAN updated the guideline on the management of paediatric Crohn’s disease (CD) in 2021. This promoted a move to a “top-down” (anti-TNF within 4 weeks of diagnosis) approach for patients who were deemed high-risk. High-risk was defined by extensive panenteric or severe disease, perianal, stricturing and/or penetrating behaviour. We sought to compare the use of anti-TNF therapy in two tertiary care networks in Scotland against the new guidance by conducting a retrospective multi-centre study.
Methods: We analysed electronic health records of all new paediatric CD patients diagnosed in the West and North of Scotland between 01/01/16 and 31/12/20. We collected data on the use of anti-TNF therapy (infliximab or adalimumab) within 18 months of diagnosis. Paris location and behaviour at diagnosis were determined, allowing us to split the patient group into high-risk or low/medium-risk as per the new ECCO-ESPGHAN guidance. Data regarding surgical intervention was collected and defined as: Perianal (Seton suture or drainage of abscess) and/or bowel resection ± stoma formation.
Results: 313 patients were diagnosed with CD. The median age at diagnosis was 12.9 years (minimum 1.1, maximum 16.9). 190 (60.7%) patients were male. 167 (53.4%) were classified as high-risk and 146 (46.6%) were low/medium-risk. 129 (77.2%) high-risk and 59 (40.4%) low/medium-risk patients received anti-TNF within 18 months of diagnosis, with the median start at 5 and 8 months, respectively (Figure demonstrates cumulative anti-TNF new starts by month). 30 (23.3%) high-risk patients and 10 (16.9%) low-risk patients received anti-TNF within 4 weeks of diagnosis. High-risk patients were statistically significantly more likely to receive anti-TNF (76.8% vs 40.4%, p < 0.0001 Fisher’s exact). 26 (8.3%) patients underwent surgical intervention; 21 were high-risk, and 5 low/medium- risk (12.6% vs 3.4%, p = 0.004 Fisher’s exact). 11 underwent surgical intervention at diagnosis (10 high risk, 1 low risk) and therefore received no pre-surgical medical therapy. 35 (21%) of high risk and 85 (58.2%) of low risk patients had neither anti-TNF nor surgery. .
Conclusions: The ECCO-ESPGHAN guidance seeks to shift practice towards “top-down” anti-TNF therapy in high-risk patients. Our real-world data supports this view by showing that high-risk patients are significantly more likely to require biologics within 18 months and significantly more likely to require surgery than low/medium-risk contemporaries. The ECCO-ESPGHAN approach would, however, have led to unnecessary anti-TNF in 21% of our high-risk cohort within 18 months of diagnosis. The financial cost and risk: benefit profile of this group should be considered carefully both in clinical practice and future guidance.
ID: 117/10-PT-V-d3A: 12
Poster Presentation (Virtual)
Topics: HAEMATOLOGY/ONCOLOGY
Keywords: Acute Lymphoblastic Leukemia, Survival Outcome, Philippines
Retrospective study on the survival outcomes of Acute Lymphoblastic Leukemia patients in University of the East, Ramon Magsaysay Memorial Hospital, Philippines from January 2015- December 2020
Yap, Maria Dawn Rosary; Espaldon, Anna Marie De Guzman
University of the East Ramon Magsaysay Memorial Medical Center, Philippines.
Background: Acute lymphoblastic leukaemia (ALL) comprises 75% of all childhood leukaemias. Fifty years ago, ALL had a low survival rate of 10–20%. However, with the introduction of the intensive Berlin–Frankfurt–Münster regimen, the current survival rate of ALL patients is now 90% starting in 2006. This study reviewed the survival outcomes of Acute Lymphoblastic Leukemia patients in a local tertiary hospital from January 2015- December 2020.
Objectives: This study aims to determine the survival outcomes of children 1–18 years old with Acute Lymphoblastic Leukemia (ALL) treated at the University of the East, Ramon Magsaysay (UERM) Memorial Hospital from January 2015- December 2020.
Methodology: Medical charts of newly diagnosed ALL ages 1 to 18 years old from January 2015 to December 2020 were reviewed.
Outcome: The overall outcome of the patients was as follows: 15 patients are still alive (88.23%), one patient abandoned treatment (5.88%) and one patient (5.88%) died due to hyperleukocytosis (ALL-specific mortality). The relapse-free survival was 50% in 6 years, the relapse rate was 43.75%, and the mortality rate was 5.88% (Table ).
Table 1. Association of clinical factors of the patients with Acute Lymphoblastic Leukemia diagnosed at UERM Hospital from January 2015–December 2020 with relapse
Conclusion: The overall survival outcome of ALL is good with the advent of new diagnostic tests and new treatment protocols. The present study summarized the survival rate of childhood ALL in a single tertiary hospital. The relapse-free survival rate was lower, and the relapse rate was higher as compared to international and local studies. This outcome will serve as a basis for future improvement in the UERM Hospital’s treatment for ALL patients.
ID: 171/10-PT-V-d3A: 13
Poster Presentation (Virtual)
Topics: GENERAL PEDIATRICS
Keywords: screen use; infants; toddlers
Screen use by infants and toddlers: an online survey
Queirós Fraga, Catarina Maria; Duarte-Costa, Sílvia; Gonçalves, Claudia; Rodrigues, Nádia
Unidade Local de Saúde de Matosinhos, EPE, Portugal.
Background: For several years, devices with screens have become more common in everyday life. Increasingly small, accessible and intuitive, they are present in practically every home on the globe. Because of the ease and pervasiveness of use, the American Pediatric Association and the World Health Organization have recommended avoiding daily screen use in children up to one year old and limiting it to one to two hours a day in children between two and five years. Little research has been conducted on children under three years old. For this reason, we conducted an online investigation to learn about habits and the impact of screen use on the psychomotor development of children whose parents use social networks.
Methods: An anonymous cross-section survey was administered to parents through social media platforms on behalf of their children under three years old between 9th and 18 February 2022. The survey included closed questions on demography, screen use features, and developmental milestones.
Results: Among the 142 answers regarding children under three years old, authors found that 113 had screens introduced before two years old, 103 were presented to screens by their parents, and 72 were exposed to screens between one to two hours per day. Still, only 4.2% were alone during the exposure. Authors did not find an association between parents’ age, their academic qualification, or work regime to children’s age of initial exposure to screens; as well as didn’t find an association between children’s age of initial exposure and the daily time of exposure or any impact on developmental milestones.
Conclusions: There is no doubt that more studies are needed to clarify the true impact of screen use before three years old. However, it is clear that pediatricians must address this exposure of infants and toddlers with parents early in follow-up to limit impairments in their psychomotor and cognitive development.
ID: 133/10-PT-V-d3A: 14
Poster Presentation (Virtual)
Topics: NEONATOLOGY
Keywords: swaddling, DDH
Swaddling and neonatal hip dislocation
Handelsman, John E.
Hassenfeld Children’s Hospital at NYU Langone, United States of America.
Background and Objective: Hip dislocation in newborns is unlike other musculoskeletal conditions, such as congenital club foot or spina bifida, where obvious bony anomalies are present early in fetal development. Although dislocated, the anatomy of the hip joint is initially normal and only deteriorates if the dislocation is allowed to persist. While in the womb, the legs of the fetus are flexed at the hips and moderately abducted.
Methods: All neonates carry maternal hormones that relax the pelvis to aid delivery. Their hip joints are frequently unstable, and can dislocate if adducted but reduce immediately when the legs are flexed and abducted. Different racial groups have varying traditions in their handling of neonates. Hip dislocation in early infancy occurs most frequently in Northern Italy, Scandinavia and West Germany. Traditionally, babies are wrapped in blankets with their legs extended to keep them warm in these regions. Neonates in other geographic locations are strapped to their mother’s sides or backs, with their hips abducted. Early hip dislocation is infrequent in the indigenous people of Central and Southern Africa, Hong Kong and Northern Canada Salter(1) presented a revealing study of neonatal hip dislocation in two genetically identical North Canadian Indian tribes who handled their infants differently. One strapped their baby with the legs extended to a tikonagan (cradle board). The other left the legs free to abduct and flex. The incidence of hip dislocation was ten times higher in those using the cradleboard.
Learning Points Discussion: The evidence is compelling that maintaining the legs extended in the first weeks of life significantly increases the incidence of permanent hip dislocation. Nevertheless, the tradition of swaddling the legs, thus holding them adducted and extended, is still commonly practised. It is believed that infants are more relaxed when returned to the confined physical position held in the womb. It is not appreciated, however, by those advocating swaddling the legs in extension that the intrauterine position of the hips is flexion and moderate abduction. It is clearly important in the neonate to leave the hips free to flex and abduct. This anatomical position can be encouraged by carrying infants in body devices that hold the legs separated. If swaddling is deemed essential, limit this to the arms.
ID: 284/10-PT-V-d3A: 15
Poster Presentation (Virtual)
Topics: DERMATOLOGY
Keywords: atopic dermatitis, medication use, pediatric population, Europe
Prevalence of atopic dermatitis and medication use in a pediatric population in five European countries
Silverberg, Jonathan I.1; Simpson, Eric L.2; Weidinger, Stephan3; Mnif, Tarek4; Thomas, Ryan B.5; Chuang, Chien-Chia6; Rossi, Ana B.6
1The George Washington University School of Medicine and Health Sciences, Washington, DC, USA; 2Oregon Health and Science University, Portland, OR, USA; 3University Hospital Schleswig-Holstein, Campus Kiel, Kiel, Germany; 4Cerner Enviza, Paris, France; 5Regeneron Pharmaceuticals Inc., Tarrytown, NY, USA; 6Sanofi, Cambridge, MA, USA.
Background: Awareness of prevalence, severity, and medication use for atopic dermatitis (AD) in a pediatric population may inform disease management strategies.
Methods: EPI-CARE—a cross-sectional, web-based, self-reported survey of children aged 6 months to 17 years and their parents—was conducted from 2018 to 2019 in 18 countries in 5 regions. Parents were invited to participate without knowledge of the survey topic. Quotas were set for age, sex, and region (and urban/rural split in some countries), and a weighting adjustment was applied to obtain a representative population for each country. We present prevalence results from five European countries (Italy, France, UK, Spain, and Germany). Outcomes presented here were provided by caregivers (of children aged <12 years) or adolescents (aged ≥12 years). AD prevalence was based on patients who had ever had an intermittent itchy rash for ≥6 months AND had this rash in the past 12 months AND had this rash in the elbow folds, behind the knees, in front of the ankles, under the buttocks, or around the neck/ears/eyes AND self-reported ever being diagnosed with AD (eczema) by a physician. AD severity was rated using patient/caregiver global assessment in the past week as clear, mild, moderate, or severe.
Results: Among 20,029 respondents, the estimated AD prevalence was 15.0% overall (10.2% clear/mild, 4.2% moderate, 0.6% severe; Table ). AD prevalence was similar in 3 age groups (14.7% for those aged <6 years, 15.5% for 6 to <12 years, and 14.7% for ≥12 years). Most children and adolescents with AD (89.7%) had received at least one prescription AD treatment in the past 12 months, with 66.1% having used a systemic AD treatment, mainly oral steroids (49.4%). Medication use increased significantly with AD severity.
Table 1. AD prevalence (among all respondents) and treatments used in the past 12 months (among those with AD), overall and by AD severity in the past week
Conclusions: AD affects approximately 15% of children and adolescents in Europe, with nearly a third of these having moderate/severe AD during the past week. Overall, approximately two-thirds of patients with AD received systemic treatment (a large portion among them used systemic steroids), and this increased with disease severity. Systemic steroids are not recommended by guidelines for the treatment of AD in pediatric patients, only as a last resort for severe flares. These data highlight the high medical need for safe systemic treatments that can offer long-term disease control to pediatric patients with AD.
ID: 276/10-PT-V-d3A: 16
Poster Presentation (Virtual)
Topics: ADOLESCENT MEDICINE
Keywords: Adolescence, adoption, fetal alcohol spectrum disorders, neurodevelopment, comorbidity, Eastern Europe
Fetal alcohol spectrum disorders in Easter Europe adopted adolescents: neurodevelopment, comorbid conditions, service use and biopsychosocial profiles
Carrera, Pablo1; Cáceres, Isabel2; Moreno-Maldonado, Concepción3; Palacios, Jesús3; Román, Maite3
1Department of Psychological & Brain Sciences; University of Delaware; 2Department of Education & Communication, Universidad Loyola; 3Department of Developmental and Educational Psychology, Universidad de Sevilla.
Background: Prenatal alcohol exposure and the related fetal alcohol spectrum disorders (FASD) have recently gained attention as factors underlying problematic developmental outcomes among children adopted from Eastern Europe. This study compares adopted adolescents from Eastern Europe with FASD with adopted adolescents not identified as FASD and a group of typically developing, non-adopted children on (1) their degree of impairments in neurodevelopmental domains indicated by diagnostic criteria as characteristic of FASD and (2) the number of co-morbid conditions and service use.
Methods: Data comes from the Longitudinal Adoption & Institutionalization Study at the University of Seville, Spain (LAIS.US) in collaboration with the Health Behaviour in School-Aged Children (HBSC) survey. The sample was composed of 69 intercountry adoptees (mean age = 15.82 years, SD = 1.35) and a group of 30 low-risk, community adolescents (mean age = 16.11 years, SD = 1.12) 12-18-years-old residing in Spain. Validated instruments were used to assess adolescents’ degree of impairment in different neurodevelopmental domains. Data analysis was conducted using descriptive statistics, chi-square test, ANOVA, and Games-Howell post hoc test.
Results: 14 (25.45 %) of the adopted children were identified by their caregivers as having an FASD diagnosis or having suffered prenatal alcohol exposure. Neurodevelopmental impairments were pervasive in the FASD group, especially in language, executive function, and affect regulation; however, they were also prevalent in the non-FASD adoptees to a lesser degree. FASD adoptees presented more comorbid conditions like learning disability, behaviour disorder, or developmental delay and have used counsellors more than non-FASD adoptees (χ2 (1) = 11.15, p = .001), as well as psychotropic medication (χ2 (1) = 4.99, p = .026).
Conclusions: Overall, adopted FASD adolescents showed broader and more widespread impairments than non-FASD-adopted adolescents. Early identification and diagnosis could greatly benefit families and children and prevent the secondary conditions common in individuals affected with FASD. Adopted adolescents with no FASD diagnosis also showed difficulties, although to a lesser degree. Therefore, other factors explaining neurodevelopmental difficulties among adopted children should be examined.
ID: 204/10-PT-V-d3A: 17
Poster Presentation (Virtual)
Topics: NEONATOLOGY
Keywords: neonatology, feed, intolerance, phototherapy
Feed intolerance in preterm babies undergoing phototherapy: A retrospective clinical observational study.
Cherian, Rose; Ponnusamy, Vennila; Lall, Triveni
National Health Service England, UK.
Background: In our NICU, we start and increment feeds for preterm babies based on their risk factors using stratified guidelines categorised as medium, high-risk and extremely high-risk feeding pathways. Feed intolerance is very common in preterm babies and often manifests as large gastric residuals, bilious aspirates or vomiting. We have observed that preterm babies mostly have feed intolerance as bilious aspirates while undergoing phototherapy.
Aim: In this study, we aimed to understand further the characteristics of feed intolerance in babies undergoing phototherapy.
Method: Retrospective observational study on babies born between 23 + 0 and 30 + 0 weeks gestation and receiving phototherapy in the first week of life. Feed intolerance was defined as a) Vomiting—2 or more moderate vomits b) Large gastric residual—Clear but more than previous feed volume c) Bilious aspirates- Dark green colour (avocado/spinach) or Light green but more than ½ volume (wasabi/lime), d) abnormal clinical signs—Abdominal distension/abdominal erythema/blood in stools.
Results: In total, 34 babies were studied over six months. The Table below outlines the characteristics of these babies. Of the total, 65% developed feed intolerance in the first 7 days of life, with the most common type being bilious aspirate (54%). Of these babies (17/22), 77% of them developed feed intolerance after starting phototherapy. 55% of these babies were managed by holding/omitting their feeds and did not develop any other clinical signs. This resulted in a delay in achieving full feeds by a mean of 2.5 days compared to our standard feeding guideline. Feed intolerance was seen proportionately to the babies’ risk status (Ext high risk/high risk/med risk: 13/9/0). While most babies developed feed intolerance after starting phototherapy, the majority of the babies’ feed intolerance resolved by the time phototherapy was discontinued. We also did not find a correlation between the duration/intensity of phototherapy (i.e. increased number of days of phototherapy or multiple sessions) and feed intolerance.
Table 1. Demographics and characteristics of the study population
Conclusions: While most preterm babies receiving phototherapy were often noted to have bilious aspirates, there was no clear correlation seen between the intensity or duration of phototherapy to feed intolerance in our study population. It is likely that the feed intolerance was more related to the risk factors and other co-morbidities—the role of phototherapy in altering the colour of gastric aspirate to bilious needs further exploration. We acknowledge our study’s limitation with smaller numbers and lack of a matched cohort of non-phototherapy babies.
ID: 123/10-PT-V-d3A: 3
Poster Presentation (Onsite)
Topics: GENERAL PEDIATRICS
Keywords: Kawasaki
Erythema and inoculation of Bacillus Calmett-Guerin (BCGitis) as a predictive sign of incomplete Kawasaki disease (KD), atypical and refractory. Presentation of a case.
Castañeda ramirez, Laura Elena
Hospiten Cabo San Lucas, Mexico.
Introduction: The syndrome or Kawasaki disease is a childhood vasculitis, with cardiovascular disease, acute, self-limited, but potentially serious due to the cardiac complications that can occur. Although it is more frequent in Asian countries and currently has a universal distribution. It affects young children, and 85% are under 5 years old; 50% are under 2 years old. It is more frequent in males, with a ratio of 1.5–2.1: 1. In 1951, the Bacillus Calmette-Guerin vaccination was started in Mexico, one of the signs of great value being the presence of erythema and induration at the site of inoculation of the vaccine when it has been applied recently (six months to one year). This sign is present in 36% of cases and has been incorporated into Japan’s diagnostic guidelines for Kawasaki disease. Tomisaku Kawasaki first described this disease in Tokyo, Japan, in 1967 and the vaccine is also applied in Japan. In other countries, the tuberculin skin test (PPD) is performed as a diagnostic tool for Mycobacterium tuberculosis infection. The etiology of KD is still unknown, but most epidemiological data suggest an infectious origin. The possibility that KD vasculitis was caused by an agent that acts as a trigger for an immune response in endothelial cells has also been evaluated rather than by the direct action of the infection on the vessels. We present the clinical case of a 10-month-old infant with a clinical picture of incomplete, atypical and refractory Kawasaki disease, with a 5-day fever, two main criteria and mild pericardial effusion plus BCGitis as a diagnostic sign so as not to delay early treatment ().
Clinical Case: A 10-month-old male infant with no personal pathological perinatal history, fed exclusively at the mother’s breast, with a complete immunization schedule for his age. Started 5 previous days with fever of 39–40°C, diarrhoea and abdominal pain; on physical examination, we found bilateral conjunctival injection, branched tongue, fissured lips and BCGitis of 2 cm in diameter with erythema and induration, a poor general condition, continuous crying, no murmurs, no hepatomegaly, Echocardiogram with mild pericardial.
Discussion: Checking a clinical picture of KD implies ruling out other entities such as Scarlet fever, Stevens-Johnson Syndrome and viral exanthems, among others, and is based on the specific criteria set forth by the research committee of the mucocutaneous nodal syndrome in Japan. The criteria for KD are 5 days of fever and 4 main criteria in the presence of coronary abnormalities on echocardiography. [1] The term atypical or incomplete Kawasaki is reserved for those cases in which the presentation of the disease has an atypical clinic (for example, with renal involvement, acute abdomen, pleural effusion), as in our case, which only presented a fever of 5 days and 2 main criteria as well as mild pericardial effusion and BCGitis.
Results: Importantly, erythema at the BCG and PPD inoculation sites has been described in EK, reinforcing the notion that it is a non-specific inflammatory reaction. Likewise, it has been suggested that the tuberculin skin test (PPD) could provide a diagnostic tool to identify incomplete forms of KD in unvaccinated patients. BCGitis is a predictive sign of diagnostic utility in Incomplete KD in infants under 12 months of age who have the vaccine in our Country, Mexico. (Table )
Table 1. Kawasaki disease criteria
Session
11-OP-V-d3A: Oral Presentations Session 11 - Day 3 - Zone A
Presentations
ID: 219/11-OP-V-d3A: 1
Oral Presentation (Virtual)
Topics: GENERAL PEDIATRICS, PUBLIC HEALTH
Keywords: Obesity, Overweight, Identification, Intervention, Barriers
Supporting clinicians in identifying and offering intervention to children and adolescents with overweight or obesity.
McGirr, Jessica1; O’Malley, Grace2,3; Walsh, Órla1,4
1Department of General Paediatrics & Adolescent Medicine, Children’s Health Ireland at Temple Street, Dublin, Ireland.; 2W82GO Child and Adolescent Weight Management Service, Children’s Health Ireland at Temple Street, Dublin, Ireland.; 3School of Physiotherapy, Division of Population Health Sciences, Royal College of Surgeons in Ireland, Dublin, Ireland.; 4Department of General Paediatrics, Children’s Health Ireland at Connolly, Dublin, Ireland.
Background: In Ireland, 19% of primary school children and 26% of adolescents are either overweight or obese (1,2). An audit of General Paediatric Outpatient Department encounters in an Irish hospital in 2020 revealed that 27% of children and adolescents attending are overweight or obese, but just 16% were offered a growth-related intervention(3).
Methods: An online questionnaire was distributed to healthcare professionals (doctors and nurses) in our General Paediatric Department. All respondents agreed that General Paediatric teams have a shared responsibility in identifying children with overweight/ obesity and offering intervention. Just 12% (n = 1) of respondents reported usually calculating and interpreting BMI at clinic appointments, while 37%(n = 3) rarely or never do. More than one-third of clinicians reported always (12%, n = 1) or usually (25%, n = 2) offering growth interventions to children/ adolescents identified as overweight or obese in the clinic. Barriers to talking to children and their families about growth were noted, including perceived inadequate training (50%, n = 4), fear of consequences (62%, n = 5) and time constraints (62%, n = 5).
Results: A quick reference card was developed and distributed to clinicians (Image 1). This included a QR code to calculate and plot age and sex-specific BMI centiles, as well as examples of people first, non-stigmatising language that can be used when discussing growth. It also included information on factors affecting growth-eating habits, healthy hydration, activity, screen time and sleep. QR codes to websites with further information for parents following growth discussions were placed in all clinic rooms. Multidisciplinary teaching sessions were held, and informal feedback was sought from clinicians (Figure ).
Conclusion: Paediatric obesity prevention and management is a global priority. It is important that healthcare professionals working with children and adolescents identify those with overweight or obese and offer growth-related interventions where appropriate. Possible reasons why this is not routine practice within our department were identified. Resources to support staff in mitigating these barriers were introduced. A larger-scale quality improvement project with data analysis is required to determine the effectiveness of these measures.
ID: 166/11-OP-V-d3A: 2
Oral Presentation (Virtual)
Topics: ADOLESCENT MEDICINE, COVID-19
Keywords: Covid-19 vaccination; adolescents’ attitudes; vaccination side effects
Adolescents’ attitudes toward Covid-19 vaccination
Rebelo, Ana1; Guedes, Raquel2; Tavares, Hugo2
1Centro Hospitalar entre Douro e Vouga, Portugal; 2Centro Hospitalar de Vila Nova de Gaia/Espinho, Portugal.
Background: Coronavirus disease 2019 (Covid-19) was first diagnosed in China in December 2019 and spread worldwide. In August 2021, the Portuguese Health Authorities recommended vaccination against Covid-19 for all adolescents over 12 years of age aligned with other countries. Vaccination hesitancy has been identified, and a study to clarify the adolescents’ attitudes toward Covid- 19 vaccination was conducted.
Methodology: Retrospective study using an anonymous online questionnaire distributed to adolescents of an adolescent outpatient unit between September and November 2021.
Results: Sixty adolescents aged 13–17 years (mean age 15 years) were included in the study. Fifty-eight intended to get vaccinated against Covid-19, but 3 of them were not vaccinated because they had recent Covid-19 infection or were ill. 2 participants did not want to be vaccinated because of potential side effects (2/2), lack of information (1/2) and no confidence in the effectiveness of the vaccine (1/2). In 78% of the cases, the adolescents participated in the decision to be vaccinated, aiming at having a lower risk of getting infected (64%), lower risk of severe symptoms (53%), lower risk of transmissibility (52%), and ability to resume social life (going out, playing sports, attending concerts) (24%). 47% believed in the vaccine’s safety, and 93% did not regret taking the vaccine. 48% had no side effects. Local pain, myalgia, asthenia, headache and fever were the most reported side effects, but none required medical attention.
Discussion/Conclusion: Covid-19 vaccination in adolescents has been a subject of debate. Their input on the decision and expected advantages of being vaccinated is considered valuable to understand better and improve adolescent vaccination coverage. In this study group, adolescents had a positive attitude toward Covid-19 vaccination and participated in the decision to be vaccinated. Besides aiming at reducing the risk of disease, willingness for social life normalization was an important factor in the decision to get vaccinated. Although almost half of the adolescents reported side effects, these were mostly minor, as previously described.
ID: 275/11-OP-V-d3A: 3
Oral Presentation (Virtual)
Topics: ADOLESCENT MEDICINE
Keywords: Adolescence, adoption, residential care, physical growth, mental disabilities
Development of boys and girls in residential care: Results of physical growth and mental health
Fuentes-González, Andrea; Moreno-Maldonado, Concepción; Palacios, Jesús; Moreno, Carmen; Román, Maite
Department of Developmental and Educational Psychology, Universidad de Sevilla.
Background: Adolescence is a vital stage with both challenges and difficulties. This stage presents additional challenges for those boys and girls experiencing early adversity, who were separated from their birth families as a result of experiences of abuse or neglect and who were placed in child protection measures. Long-term stays in residential care are especially negative. Given the importance of rearing contexts for the development of children and adolescents, the objectives of this work are 1) to analyze the physical growth of boys and girls who have lived long-term stays in residential units and 2) to explore characteristics related to chronic diseases and mental health in adolescents who have lived long-term stays in residential care.
Methods: The Longitudinal Adoption & Institutionalization Study at the University of Seville, Spain (LAIS.US), conducted in collaboration with the Health Behaviour in School-Aged Children (HBSC) survey, has studied for more than a decade (in wave 1 the age of children was 4-8 years), the trajectories of children within the child protection system. This work focuses on a sample of 50 boys and girls who began their care trajectories in residential units due to neglect and abuse. Unfortunately, some of them remained in residential care in wave 3 (n =21) when they were between 14 and 18 years of age. Anthropometric indicators (weight, height and head circumference) and a review of the participants’ protection files were used to assess physical development and mental health. Data analysis was conducted using descriptive statistics and mean comparisons. Data were compared with a comparison group.
Results: This work found that height was significantly lower in the residential care group than in the comparison group (p = .01). We did not find any significant relationship to weight and head circumference. 33% of them also had a chronic disease, and the diagnoses were very varied (for example, epilepsy). 43% of residential care adolescents had a psychological diagnosis related to externalizing behaviours in most cases, and 62% were under different psychological treatments. To highlight, a teenager was in a mental health unit in wave 3.
Conclusions: The results showed worse physical development in the residential care group than in the comparison group and a high number of problems in adolescents in residential care. In conclusion, it is necessary to pay attention to the specific needs of this group, establishing protocols and providing specific resources that allow the optimization of the development of boys and girls who go through residential care.
ID: 274/11-OP-V-d3A: 4
Oral Presentation (Virtual)
Topics: ADOLESCENT MEDICINE
Keywords: HBSC, adolescence, bullying, victimization, sex
Psychosocial determinants of bullying victimization among adolescents in Poland and in Spain. Do Polish and Spanish victims differ?
Moreno-Maldonado, Concepción1; Malinowska-Cieślik, Marta2; Rivera, Francisco3; Moreno, Carmen1
1HBSC Spain, Department of Developmental and Educational Psychology, Universidad de Sevilla, Spain; 2HBSC Poland, Department of Environmental Health, Faculty of Health Sciences, Jagiellonian University Medical College, Kraków, Poland; 3HBSC Study, Spain; Department of Experimental Psychology, Universidad de Sevilla, Spain.
Background: School bullying victimization is a sever adolescents’ health and wellbeing problem. The interplay between individual and social factors creates specific conditions facilitating and maintaining youth violence. This study, conducted in the framework of the Health Behaviour in School-aged Children (HBSC), uses data from two countries with a large variation in bullying victimization rates. Poland with high rates and Spain among the lowest, to assess differences in psychosocial determinants of bullying victimization among Polish and Spanish adolescents by sex.
Methods: Sample was composed of 6,898 adolescents from Spain and Poland, aged 11, 13, and 15 years-old, who participated in the 2017/18 HBSC survey (51.6% female). The prevalence of bullying victimization, sociodemographic factors (sex, age, family structure, and family socioeconomic status), health-related behaviors (physical activity, smoking and having been drunk), mental health indicators (psychosomatic complaints and life satisfaction), relationships with family (communication with mother and father), and school related factors (school satisfaction and school stress) were assessed. Descriptive statistics and chi-square test were used to examine sex and country differences in the prevalence of bullying victimization and in all the examined variables. Logistic regression analyses were conducted to examine the association between psychosocial determinants and the risk of being bullied by country and sex.
Results: Bullying victimization was more prevalent in Polish than in Spanish adolescents (OR = 2.689, CI = 2.335, 3.097) and was associated with being a boy, having lower age, living with non-traditional families, having smoke in the last 30 days, and with presenting frequent health complaints, lower life satisfaction, not easy communication with father, lower school satisfaction and higher school pressure. Family affluence and health-related behaviors were not significantly associated. Moreover, a significant interaction was found between sex and country explaining bullying victimization. However, when analysis were conducted segregated by sex and country, consistent patterns were found but also some specificities. For example, in both countries age was significant only for boys, whereas family structure and communication within the family were significant only for girls. In addition, school-related factors appeared associated with having been bullied only for Polish adolescents.
Conclusions: Understanding individual and social factors and differences between two very different countries such as Poland and Spain will help to identify psychosocial determinants that increase the likelihood of being victimized, which differs by sex and country. These results highlight the relevance of specific country and sex components in programs aimed to reduce bullying victimization among adolescents.
Acknowledgment
The HSBC study in Spain was supported by the Spanish Ministry of Health and by the VI Plan Propio de Investigación de la Universidad de Sevilla 2018, under the action “II.5B Contrato de acceso al Sistema Español de Ciencia, Tecnología e Innovación para el Desarrollo del Programa Propio de I + D + i de la Universidad de Sevilla” through a grant awarded to Concepción Moreno-Maldonado
ID: 208/11-OP-V-d3A: 5
Oral Presentation (Virtual)
Topics: INFECTIOUS DISEASES, ALLERGY, IMMUNOLOGY & RESPIRATORY
Keywords: CD40LG gene, Hyperimmunoglobulin M syndrome, Pneumocystis jirovecci, Pneumonia, Primary immunodeficiency
A novel hemizygous CD40LG gene mutation in a case of X-linked hyperIgM syndrome presenting with Pneumocystis pneumonia
Pereira-Nunes, Joana1,2; Granjo Morais, Catarina1,2; Silva, Marta2,3; Grilo, Marta2,3; Louro, Pedro4,5; Vasconcelos, Júlia6; Dias, Sónia6; Reis e Melo, Ana7; Ribeiro, Augusto3.
1Department of Pediatrics, Centro Hospitalar Universitário de São João, Porto, Portugal; 2Department of Gynecology-Obstetrics and Pediatrics, Faculty of Medicine of Porto University, Porto, Portugal; 3Department of Pediatric Intensive Care, Centro Hospitalar Universitário de São João, Porto, Portugal; 4Department of Genetics, Centro Hospitalar Universitário de São João, Porto, Portugal; 5Faculty of Health Sciences, Universidade da Beira Interior, Covilhã, Portugal; 6Department of Immunology, Centro Hospitalar Universitário do Porto, Porto, Portugal; 7Pediatric Infectious Diseases and Primary Immunodeficiencies Unit, Centro Hospitalar Universitário de São João, Porto, Portugal.
Background: Pneumocystis pneumonia (PCP) is an opportunistic and potentially life-threatening infection. In children with primary immunodeficiencies, it is a challenging diagnosis due to non-specific symptoms and difficulties in early recognition of such rare immune disorders. Herein we report a case of a previously healthy infant, in whom PCP presented as his first infection leading to inaugural hyperimmunoglobulin M syndrome (HIGM) diagnosis, unveiling a hemizygous CD40LG gene mutation not previously described.
Case Presentation: A previously healthy five-month-old male, born from consanguineous parents, was referred to the emergency department due to respiratory distress in the previous two weeks. There was no history of fever, cough, upper respiratory symptoms or feeding difficulties. He had been presenting adequate physical growth and neurodevelopment progression and no prior hospitalizations. Immunization according to the national schedule was up-to-date, including the Bacillus Calmette–Guérin vaccine, without known adverse reactions. Physical evaluation revealed significant tachypnea, hypoxemia (minimum SpO2 of 87% in room air), subcostal and intercostal retractions with normal pulmonary and cardiac auscultation. Initial blood workouts showed leukocytosis, without neutrophilia, and a C-reactive protein of 0.8 mg/L. The chest radiograph presented bilateral interstitial infiltrates (Figure ), the echocardiogram was normal, and the respiratory viral panel by polymerase chain reaction (PCR) was negative. The infant was admitted to the Pediatrics Department, and after a transitory improvement under bronchodilators and corticosteroids, he presented progressive clinical worsening. On D2 of hospitalization, a chest CT showed diffuse ground-glass opacities. Intravenous ceftriaxone was initiated. Due to the possible need for ventilatory support, he was transferred to the pediatric intensive care unit (PICU) on D11.(1) Owing to clinical evolution with significant hypoxemia, blood results not compatible with bacterial etiology and interstitial imaging lung abnormalities, a respiratory infection by an atypical agent was suspected. Nasopharyngeal secretions were collected for PCR testing, namely for Pneumocystis jirovecci, and empiric therapeutical treatment with trimethoprim/sulfamethoxazole and piperacillin/tazobactam was started. Invasive mechanical ventilation (IMV) was initiated on D2 of PICU, and he required sustained high ventilatory parameters, evolving to complete bilateral hypotransparency on chest radiograph. A positive PCR result for Pneumocystis jirovecci was known on D3, and a comprehensive immunological workup was performed. HIV screening was negative. Serum immunoglobulins showed: IgG <22 mg/dL (N: 241–613), IgA <6 mg/dL (N: 10–46), IgM = 40 mg/dL (N: 26–60)]. Immunophenotyping revealed reduced T and NK cells populations and almost normal number of B cells (total lymphocyte count 2182/ µl; CD4 + 901/µl; CD8 + 273/µl; NK 46/µl; CD19 + 973/µl). Memory T cells (CD45RO+) were not highly activated, unsuggestive of severe combined immunodeficiency. He began IV immunoglobulin replacement (IVIG) with clinical improvement. CD40 ligand (CD40L) expression on stimulated T cells was normal, evaluated by flow cytometry with a monoclonal antibody (clone 89–76). An immunodeficiency multigene panel identified a novel hemizygous likely pathogenic variant in CD40LG gene [NM_000074.3:c.380dup, p.(Ser128Lysfs*2)], confirming an X-linked HIGM (XHIGM; MIM#308230). After 29 days in PICU and 23 days of IMV, he was transferred to the pediatric ward and posteriorly discharged under IVIG replacement and prophylactic trimethoprim/sulfamethoxazole. CD40L expression was repeated and is under evaluation. Parental studies will be performed.
Discussion: XHIGM is an inborn error of immunity involving the CD40L/CD40 signalling pathway. PCP is the clinical presentation in > 40% of those infants. PCP usually manifests as a respiratory illness characterized by dyspnea, tachypnea, significant hypoxemia, nonproductive cough, and fever. In our patient, significative progressive respiratory distress, hypoxemia and interstitial imaging lung abnormalities were the main manifestations, which reinforces our index of suspicion. XHIGM’s diagnosis was established with clinical, genetic and immunological findings, except for an unusual normal expression of CD40L. Our case stands out since we report a novel hemizygous CD40LG gene mutation. Stem cell transplantation is the only XHIGM’s curative treatment which is being considered for this case.
ID: 196/11-OP-V-d3A: 6
Oral Presentation (Virtual)
Topics: INFECTIOUS DISEASES, EMERGENCY PEDIATRICS
Keywords: Pediatric intensive care, Viral respiratory infections
Acute viral respiratory infections in pediatric intensive care - a 66-patients’ cohort study
Pereira-Nunes, Joana1,2; Mota, Bárbara1,2; Teles Silva, Cláudia2,3; Lisboa, Lurdes3; Ribeiro, Augusto3
1Department of Pediatrics, Centro Hospitalar Universitário de São João, Porto, Portugal; 2Department of Gynecology-Obstetrics and Pediatrics, Faculty of Medicine of Porto University, Porto, Portugal; 3Department of Pediatric Intensive Care, Centro Hospitalar Universitário de São João, Porto, Portugal.
Background: In childhood, acute viral respiratory infections represent a frequent cause of disease with important morbidity and mortality. Herein we describe our five-year acute viral respiratory infections admissions experience in a pediatric intensive care unit (PICU).
Methods: Single center retrospective observational cohort study of acute viral respiratory infections admissions in a tertiary university hospital’s PICU between January/2017 and December/2021. Statistical analysis was performed using IBM SPSS Statistics for Mac, version 27.0 software. Results for continuous variables were expressed as median, minimum and maximum values, and categorical variables were expressed as absolute and relative frequencies.
Results: During the five years, 1484 patients were admitted to PICU, of which sixty-six due to acute viral respiratory infections (4.4%). Most were male (62.1%), with a median age of 8.5 [0–208.0] months old and median hospital admission duration of 8.5 [2–59] days. Most admissions took place during the year 2021 (9.1%). June and August did not present any admission during the five-year period. Final diagnoses were acute bronchiolitis (51.5%), pneumonia (43.9%), laryngotracheobronchitis (3.0%) and epiglottitis (1.5%). Syncytial respiratory virus (56.1%), Metapneumovirus (10.6%) and Rhinovirus (10.6%) were the most frequent virus, all identified by polymerase chain reactions (PCR) methods. Viral co-infection was present in 7.6% of the cases. Bacteria were identified in 59.1%, and in 93.9% of total cases, antibiotics were used. Noninvasive mechanical ventilation, invasive mechanical ventilation, vasopressor support and extracorporeal membrane oxygenation (ECMO) were used in 72.7%, 66.7%, 25.8% and 10.6% of cases, respectively. Two patients died (3.0%), both presenting associated comorbidities (neurodegenerative disease and cardiomyopathy).
Conclusions: Our study reflects the syncytial respiratory virus’ importance in pediatric acute viral respiratory infections. Antibiotics were initially used in a significant number of patients comparably to bacteria identification, which may be related to the patient’s clinical severity. Although variable and multiple factor-dependent (individual patient characteristics, time of the year, disease severity and diagnostic method), monitoring virus detection is important since it may improve diagnostic approaching, patient management and antibiotics use optimization.
ID: 146/11-OP-V-d3A: 7
Oral Presentation (Virtual)
Topics: INFECTIOUS DISEASES, COVID-19
Keywords: COVID-19, Pediatric Intensive Care Unit, PIMS-TS
COVID-19 in a Pediatric Intensive Care Unit
Rebelo, Ana1; Silva, Claúdia2; Mota, Teresa2; Silva, Marta João2; Baptista, Maria João2; Ribeiro, Augusto2
1Centro Hospitalar entre Douro e Vouga, Portugal; 2Centro Hospitalar Universitário de São João, Portugal.
Aims and Objectives: The clinical spectrum of COVID-19 ranges from asymptomatic to severe pneumonia with acute respiratory distress syndrome and multiorgan dysfunction. Our objective is to describe the clinical features and management of pediatric patients with acute or recent SARS-CoV-2 infection in a pediatric intensive care unit (PICU).
Methods: Retrospective study of patients admitted to the PICU with confirmed SARS-CoV-2 acute or recent infection (until 60 days before admission) from March 2020 to May 2022. A descriptive analysis of the most relevant variables was performed with SPSS ® Statistics 28.
Results: 19 patients were included, median age of 10 years (0 to 16 years), 5 with comorbidities. Three patients had acute Covid-19 infection, 10 patients had pediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2 (PIMS-TS), and incidental detection of SARS-CoV-2 was observed in 6 patients. The diagnosis was confirmed in 18 patients, by PCR technique or serology (positive IgG), except for one case included in the study due to clinical similarity. The mean hospital stay was 7 days (with no significant difference between groups). In the subgroup of patients with PIMS-TS, the main reason for hospitalization was hemodynamic instability (10/10), followed by the need for respiratory support (8/10), 7 required invasive mechanical ventilation. Fever (10/10) and diarrhea (8/10) were the most frequent symptoms. Cardiac involvement occurred in all patients, 3/10 with coronary artery abnormalities, 7/10 with ventricular dysfunction and all patients required inotropic and/or vasopressor support. 6/10 had nonspecific bowel inflammation (ileitis and colitis). Intravenous immunoglobulin, acetylsalicylic acid, large-spectrum antibiotics and corticosteroids were used in all patients. Ventricular function was normalized in all patients at discharge. In the acute covid-19 infection subgroup, one patient had arrhythmic storm with cardiogenic shock, another had severe necrohemorrhagic pancreatitis, and another had pneumonia with respiratory insufficiency. The first patient required life support with extracorporeal membrane oxygenation for 6 days. Incidental detection of SARS-CoV-2 occurred in patients submitted to elective surgery, trauma, acute myeloid leukemia and Group B streptococcal septicemia. [1] 1/19 patient died with complications of acute myeloid leukemia, he had incidental detection of SARS- CoV-2.
Discussion: All PIMS-TS cases had a severe presentation requiring hemodynamic and respiratory support, however, with favourable and rapid recovery. [1] Different from the adult population, we had a small number of acute COVID-19 infection cases, and only one patient had primary respiratory insufficiency. [2] Covid 19 infection doesn’t seem to have an impact on the prognosis of a pediatric patient with an incidental diagnosis.
ID: 187/11-OP-V-d3A: 8
Oral Presentation (Virtual)
Topics: PUBLIC HEALTH, COVID-19
Keywords: dental, caries, COVID19, antibiotic stewardship
Paediatric attendances at urgent dental care centres throughout NHS Tayside, Scotland during the COVID-19 pandemic: a retrospective analysis
Linden, John1; Curnow, Morag2
1NHS Lothian, Scotland; 2NHS Tayside, Scotland.
Introduction: In March 2020, the COVID-19 lockdown suspended all routine dental care in Scotland. “Advice, Analgesia and Antibiotics” (AAA) was introduced for the initial management of emergencies and Health Boards set up Urgent Dental Care Centres (UDCCs). (1) A retrospective analysis was performed to identify reasons for attendance and treatment provided for all paediatric patients within NHS Tayside.
Methods: A protocol was created, and Caldicott approval was obtained. 1227 patients were identified, of which 407 met the inclusion criteria.
Findings: 56% of patients were female, with an average age of nine. 49% had a Scottish Index of Multiple Deprivation (SIMD) of 5 or less. The commonest reasons for attendance were pulpal and periapical pathology (65%), followed by soft tissue lesions (9%), traumatic dental injuries (TDIs) (8%) and orthodontic problems (7%). Teeth with irreversible pulpitis and acute apical abscesses were mostly extracted (94% with local and 6% general anaesthetic). Most TDIs were due to falls: there were few sporting injuries as team activity was limited. Upper central incisors were the most commonly traumatised teeth, with a 12:13 split between primary and permanent teeth.
Discussion: This project highlighted that even within a UDCC, antimicrobials were occasionally prescribed inappropriately. However, most children had definitive and appropriate treatment. In a climate where treatment options are restricted, the dental team needs to be adaptive in their approach to care. Compliance with trauma guidelines was complicated by lockdown restrictions limiting the number of visits. Caries management proved challenging; however, minimally invasive techniques may be useful in reducing AGPs.
ID: 287/11-OP-V-d3A: 9
Oral Presentation (Virtual)
Topics: ADOLESCENT MEDICINE
Keywords: diet habits, food related behaviours, nutritional status, adolescents, Serbia
Diet habits, food related behaviours and nutritional status of Serbian adolescents
Gudelj Rakic, Jelena; Kilibarda, Biljana; Jovanovic, Verica
Institute of Public Health of Serbia “Dr Milan Jovanovic Batut”, Serbia.
Introduction: Hormonal and metabolic changes leading to changes in body composition but also to changes in diet behaviour may represent a risk for weight gain in adolescence. Studies proved the increasing impact of food-related behaviours on adolescents’ diet habits and nutritional status.
Aim: Primary goal was to examine associations between diet habits, food-related behaviours and nutritional status of Serbian adolescents.
Method: Data were obtained from the Health-Behaviour in School-aged Children survey (HBSC) performed in the spring of 2018. Data on 11, 13 and 15-year-old adolescents, i.e. students of 5th and 7th grade in primary schools and students of the 1st grade of secondary schools in Serbia, were analyzed in line with the international study protocol. Participation in the study was voluntary and anonymous, and a self-administered questionnaire was used according to the international HBSC study protocol. Weight status was defined according to BMI categories for children and youth based on the International standard BMI values according to the International Obesity Task Force.
Results: According to BMI, 18,2% of students were overweight, and every sixth student was obese (5,7%). Boys were more often overweight and obese compared to girls. Almost 8% of adolescents never eat breakfast during the working week, with no significant differences between boys and girls except in 15-year-olds, where girls more often skip breakfast. One-fifth of adolescents snack while watching TV and/or working or playing on the computer, and almost 20% of them eat at least one meal in front of the screens.
Conclusions: Considering the health risks associated with overweight and obesity and their long-term consequences, there is an increasing need for further preventive interventions targeting adolescents aiming at improving diet habits, food-related behaviour and nutritional status.
ID: 257/11-OP-V-d3A: 10
Oral Presentation (Virtual)
Topics: ADOLESCENT MEDICINE, PUBLIC HEALTH
Keywords: Adolescents, ecological model, Life satisfaction, wellbeing, cross-cultural
Adolescent LifeWorlds: An Ecological approach related to adolescent’s Life Satisfaction
Gaspar, Tania1; Moreno-Maldonado, Concepción2; Marques, Adilson3; Salado, Vanesa4; Gaspar Matos, Margarida5; Ercan, Oya6; Richardson, Clive7; Sravrou, Myrto8; Charrier, Lorena9; Tesler, Riki10; Morgan, Antony11; Currie, Candace12
1Lusofona University/HEI-LAB; ISAMB – FM/Lisbon University, PortugalPortugal; 2Department of Evolutionary and Educational Psychology University of Seville, Spain; 3FMH/Universidade de Lisboa, Portugal; 4Department of Experimental Psychology, Universidad de Sevilla, Spain; 5ISAMB – FM/LisbonUniversity, Portugal; 6Department of Pediatrics, Istanbul University-Cerrahpaşa- Turkiye; 7Panteion University of Social and Political Sciences, Athens, Greece; 8University Mental Health, Neurosciences and Precision Medicine Research Institute “Costas Stefanis” (UMHRI), Athens, Greece; 9Department of Public Health Sciences and Pediatrics University of Torino; 10The Department of Health Systems ManagementAriel University, Israel; 11Glasgow Caledonian University London; 12Glasgow Caledonian University London.
Introduction: Multi-level influences that impact adolescents’ health have been conceptualized within the framework of ecological models.
Method: Here, we apply this ecological model to data from a large cross-national study to demonstrate the influence of social health determinants at different system levels. The study is Health Behaviour in School-aged Children (HBSC)—a World Health Organization collaborative cross-national study conducted in 52 countries and regions across Europe and North America (http://www.hbsc.org). We examine HBSC data on a selection of health and well-being indicators (self-reported health, psychosomatic symptoms, and life satisfaction), health-related measures (namely physical activity, healthy eating habits, and alcohol consumption), and developmental context (family support, teacher and classmate support and victimization), as well as gender, age, and socioeconomic status, collected in the survey year 2018/2019 using the international research protocol and questionnaire. The sample included 39,247 students from the Mediterranean countries of Greece, Israel, Italy, Malta, Portugal, and Spain. The mean age of the sampled students is 13.6 years (standard deviation of 1.6), and 52.9% are girls.
Results: Statistically significant differences were observed between boys and girls in different age groups. Using an ecological framework, the determinant of adolescent well-being is examined from the individual level to the country level. A 31% of life satisfaction was explained by the following determinants: being a boy, younger, with higher family affluence, less psychological symptoms, frequent physical activity, daily fruit and vegetables consumption, not drinking alcoholic beverages, having high family support, positive relations with teachers and school friends and not been bullied. When the analysis was stratified by countries, results were mixed, but more similarities than differences were found. Seven factors were related to life satisfaction in all countries: age, family affluence, psychological symptoms, self-perceived health, family support, and relationship with teachers and classmates. Higher life satisfaction is related to healthy eating behaviour in all countries except for Malta by physical activity except in Italy. Low life satisfaction is associated to been bullied in all countries except for Spain and with higher alcohol consumption only in Portugal. Moreover, being a boy was associated with higher life satisfaction in Greece and Spain.
Conclusion: From public health and a public policy perspective, relevant messages must address changeable behaviours and allow more friendly social and physical life contexts. However, more fundamentally, to improve the adolescent population’s health, there is a general need to decrease inequalities by means of more sustainable and multisectoral public policies, to provide better organized educational, health and local services to cope with developmental life challenges, aiming at reducing inequities, now and in the long run.
ID: 226/11-OP-V-d3A: 11
Oral Presentation (Virtual)
Topics: GENERAL PEDIATRICS
Keywords: Vesicoureteral reflux, urinary tract infection, kidney injury
Vesicoureteral reflux - a retrospective study
Curval, Ana Rita1; da Silva Cardoso, Juliana2; Vieira, Beatriz3; Castro, Ribeiro2; Reis, Armando2; Madalena, Célia3
1CHUSJ, Portugal; 2CHP, Portugal; 3CHPVVC, Portugal.
Introduction: Vesicoureteral reflux (VUR) is a common urological abnormality in pediatric age, becoming a serious risk factor for urinary tract infection (UTI), kidney injury, high blood pressure and chronic kidney disease.
Objective: Describing the symptoms of children with VUR and assessing their prognosis.
Methodology: Retrospective analysis of the clinical processes of children diagnosed with VUR followed in the Pediatric Nephrology consultation of a group 1 hospital between 2004 and 2019. The statistical analysis was performed using SPSS statistics, version 25, with p < 0.05 considered statistically significant.
Results: The sample included 164 children, 60.4% (99) female, with a diagnosis median age of 9 months. The diagnosis was made after UTI in 79.9% (131) of the cases. VUR was classified as mild to moderate (grades I to III) in 78.7% (129) of the patients and severe (grades IV and V) in the remainder, being bilateral in 41.5% (68) of the cases. All children underwent conservative treatment, with 36% (59) of the cases requiring surgical treatment. Approximately 36.6% (n = 60) of the children had kidney damage and/or hypofunction. There was a statistically significant association between the degree of VUR and the presence of renal injury and/or hypofunction and the need for surgical treatment and between the occurrence of recurrent UTIs and the presence of renal injury and/or hypofunction (p < 0.01).
Conclusion: Most children with VUR had a favourable evolution. However, the presence of severe VUR and repeated UTIs often led to the existence of renal damage, which makes diagnosis and early treatment imperative.
ID: 285/11-OP-V-d3A: 12
Oral Presentation (Virtual)
Topics: GENERAL PEDIATRICS, PSYCHIATRY
Keywords: Behavioral problem, Preschool children, Risk factors
Prevalence of children at risk of behavioral problems among preschool children between the ages of 3 and 6 years
Chaturvedi, Soumya1; Shrivastava, Neha2; Agrawal, Amit3; Shrivastava, Jyotsna4
1Physician, India; 2Department of Pediatrics, Gandhi Medical College, Bhopal, India; 3Department of Pediatrics, Gandhi Medical College, Bhopal, India; 4Department of Pediatrics, Gandhi Medical College, Bhopal, India.
Background: Behavioral problems often go unnoticed in children; however, it is important to identify and treat the problem in childhood to prevent long-term disability.
Objective: The objective of the study was to find the prevalence of children “at risk” of behavioural problems in preschool children and to identify the social, environmental, and family factors associated with the risk of behavioural problems in preschool children. Materials and Methods: A cross-sectional observational study was conducted on 370 children from 3 to 6 years of age studying in preschools of Bhopal, using the Preschool Pediatric Symptom Checklist. Bivariant analysis was performed using the Chi-square test on STATA 11.2.
Results: Overall prevalence of children at risk of behavioural problems was found to be 46.7% in the studied population. Children belonging to low-income families were at a higher risk of developing behavioural problems (p < 0.001). Working mothers and time spent by fathers had a positive impact on a child’s behaviour (p = 0.008). Other factors that were studied but did not have significant association were gender, age, time spent by the mother with the child, presence of a sibling, and family size.
Conclusion: The main factors contributing to the increase in risk in children for developing behavioural problems were found to be less time spent by the father with the child and lower family income. However, the working status of mothers did not increase the risk of developing behavioural problems.
Disclosure statement
No potential conflict of interest was reported by the author(s).