Abstract
: The World Health Organization’s (WHO) Eastern Mediterranean Region (EMR) continues to face emerging and re-emerging infectious disease outbreaks that result in high morbidity and mortality. Some countries in the region also continue to experience acute or protracted humanitarian emergencies that have resulted in the breakdown of already fragile health systems. We analysed data from epidemiological reports produced by countries and the WHO regional office (WHO EMRO). We describe the disease outbreaks that occurred in 2019 and the mitigation support provided by WHO. Ten countries reported 24 new or ongoing infectious disease outbreaks caused by 13 different pathogens. They include cholera, Crimean-Congo hemorrhagic fever (CCHF), chikungunya, chickenpox (varicella), dengue fever, diphtheria, extensively drug-resistant (XDR) typhoid fever, human immunodeficiency virus (HIV), hepatitis A, measles, Middle East respiratory syndrome (MERS), poliomyelitis, and Rift Valley fever. These resulted in more than one million cases (suspected and laboratory-confirmed) and more than 1500 deaths with an overall case-fatality ratio (CFR) of 0.17%. While WHO continues to support preparedness and response activities in the EMR, more countries continue to face repeated outbreaks coupled with data gaps due to inconsistent reporting. While some countries have reduced cases following enhanced surveillance and response systems, strengthening of country-level health systems is needed.
1. Background
Infectious diseases caused by emerging, re-emerging, and high-threat pathogens continue to cause increased morbidity and mortality, particularly in countries undergoing humanitarian crises. Twelve of the 22 Member States and territories of WHO EMR are directly or indirectly impacted by acute or protracted humanitarian emergencies contributing to fragile health systems and high numbers of internally displaced persons (IDPs) and refugees, often with limited access to basic healthcare services and environmental infrastructure (Ammar et al., Citation2016; Bloom & Cadarette, Citation2019; OCHA, Citation2021; Spernovasilis et al., Citation2017; WHO EMRO, Citation2018).
Other risk factors contributing to the emergence and rapid spread of epidemic diseases in the EMR include rapid or unplanned urbanisation, climate change, weak disease surveillance, limited laboratory diagnostic capacities, increased human-animal interaction and increased population movement (Baig & Shaikh, Citation2012; Buliva et al., Citation2017; Spernovasilis et al., Citation2022).
The frequency and impact of infectious disease outbreaks vary by country, with some experiencing more emerging and ongoing disease outbreaks than others. To monitor this occurrence, the WHO Office for the Eastern Mediterranean Region, in partnership with the US Centers for Disease Control (CDC) and Ministries of Health (MOH), have established a reporting mechanism that uses different electronic disease platforms (Malik et al., Citation2020), such as the Outbreak and Public Health Event Portal (OPHEP) that monitors outbreak trends in the region through a central database that maintains epidemiological data received from country offices and MOHs on disease outbreaks.
To contain the outbreaks and prevent geographic spread, WHO/EMRO works closely with health authorities to provide technical and financial support to the affected countries by applying appropriate public health interventions using science-based control measures (Abubakar et al., Citation2020). We describe the occurrence of the different disease outbreaks, distribution rates, challenges and the support provided by WHO EMRO in 2019. We also provide recommendations that may help prevent and mitigate the spread of the diseases in the region.
2. Materials and methods
We analysed data from the disease outbreak database and other reference materials for 2019 archived at the WHO EMRO, including OPHEP, Weekly Epidemiological Monitor reports, weekly and monthly disease-specific bulletins, outbreak investigation reports and other relevant materials (WHO, Citation2019h; WHO EMRO, Citationn.d.). MOHs and WHO country offices (WCOs) often report the disease outbreak data to the Regional Office. Disease outbreak reports from MoHs and WCOs are generated weekly and monthly, with yearly reviews to provide in-depth descriptive analysis, trends in occurrence and preparedness.
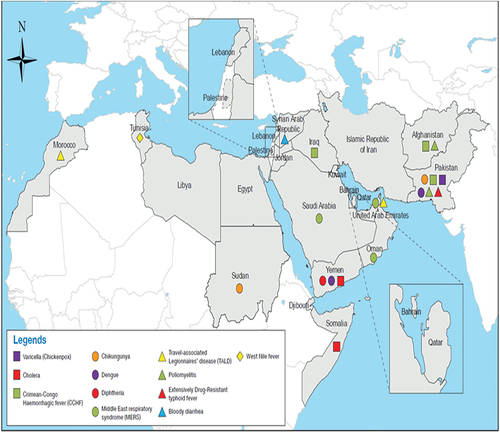
To ensure quality, we checked for accuracy, completeness, consistency, validity and uniqueness of the data. Records were verified (triangulation) for accuracy and consistency across different reports and databases on disease outbreaks, country and time of occurrence. In addition, all generated tables were reviewed for completeness, accuracy and consistency by at least two people. All diseases reported—and included in this analysis met the definitions of being outbreak based on the WHO definition. No additional criteria were applied to the disease definition beyond what specific countries and WHO EMRO had. Data was compiled based on the type of disease outbreak, date and country the outbreak occurred, caseload, deaths, CFR, and WHO support (Tables ). Disease occurrence was calculated using proportions, and case fatality rate was defined as the number of deaths divided by the number of cases in a defined period. These data were mapped or maps (Figures ) generated and/or pulled from existing WHO regional databases and dashboards using Arc GIS, with STATA used for all analysis
Table 1. Infectious Disease Outbreaks reported in EMR countries in 2019
Table 2. Summary of WHO support to EMR outbreaks, 2019
3. Results
3.1. Distribution of outbreaks
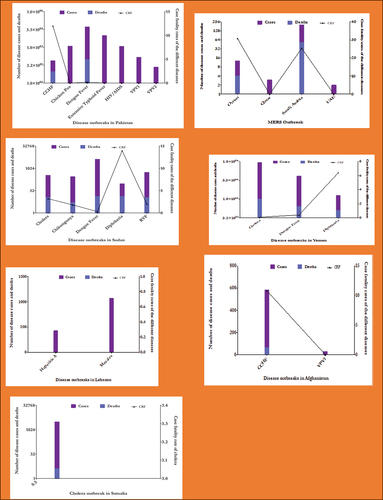
In 2019, ten countries (Figure ) reported 24 disease outbreaks, with more than 1,012,542 suspected cases, including laboratory-confirmed cases and 1692 deaths (CFR = 0.17%). Of all the disease outbreaks, cholera had the largest proportion of caseloads (n = 864,542, 85.3%) with 1040 deaths (CFR 0.12%) (Table , Figures ). On the other hand, Dengue fever had the second-highest caseload (n = 129,972 cases, 12.5%) with 366 deaths (CFR 0.3%).
Other outbreaks included CCHF (n = 658, <1%), varicella (n = 1,285, <1%), chikungunya (n = 281, <1%), diphtheria (n = 2,113, <1%), XDR typhoid fever (n = 9,994, 1%), hepatitis A (n = 426, <1%), HIV (n = 1,228, <1%), measles (n = 5,6090, <1%), MERS (n = 223, <1%), poliomyelitis (n = 176, <1%) and RVF (n = 548, <1%) (Table ).
Yemen recorded the highest caseload in the region (n = 861,096, 99.6%) with 1025 deaths (CFR 0.12%) of all reported cholera and 55.2% of all dengue fever cases (n = 71,688) with 258 deaths (CFR 0.36%). Pakistan recorded the second-highest dengue fever caseload (n = 54,079, 41.6%). Overall, Pakistan had the highest number of disease outbreaks (7) reported in the region, followed by Sudan (5) (Figure ).
MERS had the highest CFR (25.1%) of all the diseases (56 deaths, 233 cases). MERS outbreaks were reported in Oman (13 cases, 4 deaths, CFR 30.8%) and Saudi Arabia (205 cases, 52 deaths, CFR 25.4%). The other diseases with a high fatality ratio were CCHF (658 cases, 72 deaths, CFR 12.8%) and diphtheria (2,113 cases, 142 deaths, CFR 6.7%).
3.2. Epidemiology and presentation of the different disease outbreaks
3.2.1. Chickenpox (Varicella)
Chickenpox occurred in Punjab Province, Pakistan (1,285 cases, 0 deaths) in 2019. The outbreak that started in April 2017 resulted in a total of 18,883 cases (CFR 0.11%) by the end of 2019 (WHO, Citation2019e). Cases peaked during the summer, with sporadic cases reported until the end of the year. This varicella outbreak was possibly made worse by overcrowding, poor hygiene conditions and poor status of the immunity of the affected populations in Pakistan.
The Pakistan Federal MOH and WHO response measures included enhanced surveillance and laboratory capacities for early detection and confirmation of cases, improved data management, proper case management, strengthening risk communication, and community engagement. Rapid Response Teams (RRTs) were trained on outbreak investigation and response and operationalised in order to respond to the outbreaks. In addition, WHO deployed one laboratory expert and two epidemiologists to enhance Punjab’s detection, confirmation, and response capacity (Table ) (WHO, Citation2019o).
3.2.2. Chikungunya
Sudan reported the first-ever chikungunya outbreak (48,763 cases, 5 deaths) in 2018. The outbreak was initially reported in Kassala State and spread to ten other states, presumably due to population movement and poor vector control interventions (WHO, Citation2019e). In 2019, during epidemiological week 38, there was a surge in chikungunya cases, with 287 cases and five deaths (CFR 2%) reported from West Darfur (230 cases, 80.1%). East and South Darfur were also affected, with 24 (8.4%) and 23 (8%) reported cases, respectively (WHO, Citation2019p). Compared to the previous year, fewer cases were reported in 2019 following timely detection and strict implementation of prevention and control measures (WHO, Citation2019e).
WHO provided technical support to the MOH in enhancing disease surveillance, capacity-building for laboratory confirmation of suspected cases, testing kits, health awareness and risk communication materials, and integrated vector control activities such as larvae and adult control, spraying and fogging, and provision of mosquito nets. WHO also deployed one laboratory expert and two epidemiologists in October and November 2019, respectively, to strengthen laboratory capacity at the central and state level for the confirmation of suspected cases as well as to strengthen epidemiologic and data management capabilities for field investigation. Further, experts from the WHO Regional Office were deployed on a rotational basis to build country-level capacity.
3.2.3. Cholera
Cholera contributed the largest proportion of outbreak caseload in the region in 2019 (n = 864,542, 85.3%) with 1040 deaths (CFR 0.12%) (Table , Figures and 2). Cholera outbreaks were reported in Yemen, Somalia, and Sudan (WHO, Citation2019r, Citation2019l, 2019s, Citation2019s, 2019c)
Yemen recorded the highest caseload of cholera in the region (n = 861,096, 99.6%), with 1025 deaths (CFR 0.12%) reported. Cases peaked during epidemiological week 8 to reach the maximum number of about 300,000 suspected cases in week 14, before declining, with the number of cases reported each week remaining relatively high. Yemen’s Ministry of Public Health (MoPH), WHO and other partners instituted a host of preventive and control measures (see Table ) to contain the cholera outbreak, including but not limited to enhanced Early Warning Alert and Response Network (EWARN) for real-time surveillance (WHO, Citation2019t), improved clinical management and infection prevention and control practices in health care settings; provision of medical supplies; risk communication and awareness raising; waste management and water chlorination; and conducting an oral cholera vaccination (OCV) campaign targeting > 1.7 million people in southern and northern governorates (WHO, Citation2019n). In the northern governorates, the campaign’s target population was 1,224,183, with a total of 1,088,081 (89%) receiving the first dose of the vaccine. In the southern governorates, the targeted population was 497,108 with a total of 478,535 (96%) receiving the first dose of the vaccine (WHO, Citation2019n)
In Somalia, a total of 3,100 cholera cases and four deaths (CFR 0.12%) were reported in Banadir region. This outbreak was a continuation of the cholera outbreak that started in 2017 and was attributed to the severe drought that affected many parts of the country, causing limited access to safe water, food insecurity, and disruption of WASH activities. WHO supported the MOH in containing the outbreak through enhanced risk communication and community engagement, strengthening water, sanitation, and hygiene (WASH) activities, and OCV campaigns. For the OCV campaign, out of a target of 642,913, a total of 621,875 (96.7%) people aged one year and above received the first dose of the OCV (WHO, Citation2019). WHO also supported surveillance and reporting through the EWARN system, strengthening laboratory capacities and enhancing case management practices.
In Sudan, the cholera outbreak was reported on 8 September 2019, following heavy rain and flash floods, which affected sanitation, hygienic practices, and WASH activity implementation (WHO EMRO, Citation2019a). A total of 346 cases (11 deaths, CFR 3.2%) were reported, with more than 95% from two states, the Blue Nile State (204) and Sinnar State (130). The Sudan Federal Ministry of Health (FMOH), WHO, and partners effectively contained the outbreak by implementing WASH activities and two rounds of OCV campaigns in October and November 2019, targeting 1.65 million high-risk populations: Blue Nile State (coverage 85%) and Sinnar (coverage 98%). They also established four cholera treatment centres in Blue Nile State and ten cholera treatment hospital wards in Sinnar State. FMOH, with the support of WHO, enhanced the treatment and diagnostic capacities by distributing 25 cholera kits and 5,000 rapid diagnostic test kits (WHO, Citation2019m).
3.2.4. Crimean Congo hemorrhagic fever (CCHF)
In 2019, CCHF outbreaks were reported in Afghanistan and Pakistan, with a total of 658 cases and 72 deaths (CFR 10.9%). Between January and December 2019, a total of 583 suspected cases and 63 deaths (CFR 10.8%) were reported in Afghanistan, mainly in Herat and Kabul provinces, where the main livestock markets in Afghanistan are located. In Afghanistan, CCHF cases peaked during June—July, when farmers take livestock to markets with increased human-animal interaction. There has been an upward trend of cases since 2013 when the official reporting of CCHF cases started in Afghanistan (WHO, Citation2019b). WHO supported Afghanistan MOH in strengthening multisectoral coordination, enhancing early warning surveillance and reporting, improving community engagement and awareness, supporting RRTs and building their capacity in drafting an operational plan to accelerate the response, helping with case management, and blood transfusion service in Herat.
In Pakistan, 75 suspected cases of CCHF (9 deaths, CFR 12.1%) were reported mainly from Balochistan province, while other provinces reported sporadic cases. Increased human-animal interaction, as well as increased movement of animals and animal products, remained the leading causes of the CCHF spread. With the support of WHO, the Ministry/Department of Health worked with relevant stakeholders and neighbouring countries to limit the spread and control the outbreak during peak seasons (WHO, Citation2019b). WHO extended its support in strengthening early detection, laboratory confirmation, clinical management, risk communication and community engagement.
3.2.5. Dengue fever
In 2019, Dengue fever was reported in Yemen, Pakistan, and Sudan, with a cumulative total of 129,972 cases and 366 deaths (CFR 0.3%). Dengue fever had the second-highest caseload at 12.5%, with Yemen and Pakistan accounting for 56.8% and 42.9%, respectively.
In Yemen, a total of 71,688 cases of dengue with 258 deaths (CFR 0.36%) were reported. Of these suspected cases, a total of 794 (IgG) and 590 (IgM) cases were confirmed by ELISA test at the National Center for Public Health Laboratories. The upsurge in dengue cases was linked to the presence of Aedes mosquitoes and heavy rains during October and November, with cases increasing exponentially during the last six weeks of 2019 (WHO, Citation2019f). WHO and MOH enhanced the RRT capacity in the affected governorates while strengthening early warning surveillance, testing, case management, awareness raising and vector control (WHO, Citation2019f).
In Pakistan, dengue fever cases were initially reported in August 2019 from Islamabad and Rawalpindi before spreading countrywide. By the end of 2019, Pakistan reported 54,049 cases and 95 associated deaths (CFR 0.18%) (WHO, Citation2019d). The outbreak peaked in October 2019, but the number of reported cases declined from early November in all parts of the country except Sindh province. WHO supported the health authorities with countrywide dissemination of laboratory protocol and clinical management guidelines. Information, education, and communication (IEC) materials were developed and distributed. WHO also deployed five experts for dengue case management, laboratory investigation, and emergency risk communication, besides supporting the government with medical supplies to manage severe cases (fluids, crystalloids, etc.).
In Sudan, the dengue fever outbreak was confirmed during week 31 of 2019 (July 28‒August 3) in Kassala State before spreading to nine other states with increased human mobility, population dynamics and water storage practices driving the pattern. A total of 4,205 cases with 13 deaths (CFR 0.3%) were reported, with the epidemic peaking during week 46 (761 cases) before tapering off. However, cases continued to be reported until the end of 2019. Integrated vector control activities were implemented. WHO deployed epidemiology, laboratory, clinical, and entomology experts to support the government in laboratory, clinical management, mapping of hotspot areas, as well as vector surveillance and control measures. Funding was also provided for vector control activities and for the procurement of medicines and insecticides.
3.2.6. Diphtheria
In 2019, diphtheria outbreaks occurred in Yemen and Sudan, resulting in 2,113 cases and 142 deaths (CFR 6.7%). In Sudan, the first case was reported on 5 February 2019, with occurrences remaining sporadic until October 2019 (12 cases in total). By December 2019, 93 cases with 13 deaths (CFR 13.98%) were reported from six states, mostly South Darfur State, with 98% of cases from Al-Sunta Locality. Of these, 82% of the reported cases had missed DPT vaccination, with 63% of the cases aged between 5–14 years. Low immunisation coverage, overcrowding, migration, and nutritional status are some of the factors that may influence the occurrence of diphtheria infection (Ramdan et al., Citation2018)
WHO provided support in enhanced case management and strengthened immunisation programmes. The FMOH and State MOH, in partnership with WHO and UNICEF, initiated community awareness campaigns, encouraged timely seeking of health care, conducted training on proper diagnosis/case management/immunisation, and enhanced routine immunisation programs. WHO provided 200 diphtheria antitoxin doses (DAT) and antibiotics. A vaccination campaign targeting 1–15-year-olds using pentavalent and diphtheria vaccines was implemented for 5–15-year-olds in most affected areas and children of nomadic communities (WHO, Citation2019g). An immunisation campaign was launched in Al Sunta area for the first round (November 25 -December 1), targeting 38 881 children aged <15 years old; Penta vaccine for children under 7 years of age and DT for the 7–15-year-old. The second round, targeting the same population, was administered from December 31-January 6, with vaccination coverage estimated at 80% (WHO, Citation2020)
Yemen’s outbreak has been ongoing since October 2017 due to the disruption of routine immunisation services resulting in the accumulation of unvaccinated children. A total of 2,020 cases and 129 deaths (CFR 6.4%) were reported in 2019. The most affected age groups were 6–10-year-olds (26%), followed by 11–15-year-olds (20%), mainly from the Hudaydah Governorate. WHO supported the health authorities in improving early warning surveillance, laboratory case confirmation, routine immunisation, and supplementary immunisation. In 2019, two targeted immunisation campaigns in high-risk governorates were conducted. The tetanus-diphtheria vaccine was administered to over 3.4 million (60%) target children, including 1.2 million children aged 6 weeks to 5 years receiving the Penta vaccine and another 2.2 million aged 5–15 years receiving the Td vaccine (WHO, Citation2019t; WHO EMRO, Citation2019b).
3.2.7. Extensively drug-resistant (XDR) typhoid fever
Widespread and careless antibiotic usage over the years has driven the evolution of multidrug-resistant strains (MDR) with marked resistance to ampicillin, trimethoprim-sulfamethoxazole, and chloramphenicol and, more recently, extensively drug-resistant (XDR) strains of Salmonella enterica serotype typhi exhibiting resistance to chloramphenicol, ampicillin, co-trimoxazole, and fluoroquinolones, as well as third-generation cephalosporins (Akram et al., Citation2020; Basak et al., Citation2016).
The first XDR typhoid outbreak was confirmed in Pakistan in 2016 and continued till 2019. In 2019, a total of 9,994 cases and zero deaths were recorded in Pakistan. Most of the reported cases (72%) were from the Karachi district of Sindh province. More cases were reported in the year 2019 as compared to the previous years, attributable to poor sanitation and hygiene (WASH) practices, low vaccination coverage, limited surveillance for typhoid fever and the indiscriminate, overuse and misuse of antibiotics (Tharwani et al., Citation2022) The established national XDR task force ensured the standardisation of the response in the affected provinces or districts and maintained a high-level coordination mechanism. The Federal MOH developed a comprehensive national typhoid response plan for 2018–19 to guide the response interventions. WHO supported the health authorities in strengthening laboratory capacity and developing case management guidelines. In November 2019, Pakistan became the first country to introduce the WHO-approved typhoid conjugate vaccine (TCV) in its Expanded Programme on Immunisation, with more than 9.5 million children aged nine months to 15 years old getting vaccinated (coverage 90%) (Aslam et al., Citation2021). The implementation of a multisectoral national action plan covering surveillance, data collection and reporting, laboratory diagnosis, case management, community engagement, and robust WASH interventions was key to controlling this continuous and devastating outbreak. There remain knowledge gaps concerning the XDR typhoid outbreak in Pakistan, which require more research (WHO, Citation2019j).
3.2.8. Hepatitis A
A total of 426 cases and zero deaths were reported in Lebanon, starting in the Rashidiya refugee camp before spreading to Burj Shamali and El Buss refugee camps and later to residential areas of Lebanon. The main drivers behind the spread were poor sanitation, lack of safe water, and improper hygienic practices in the camp environment. The outbreak started with one case during week 35(25‒31 August) and spread to other locations. Later, it peaked in week 36 (27 cases) and week 37 (24 cases) and started to decline in week 38 (12 cases). The most affected age groups were 5–9 and 10–19 years old. WHO supported the health authorities in enhancing early warning surveillance, laboratory confirmation of suspected cases, clinical management practices, and water testing for virus contamination. Campaigns were conducted to improve water surveillance and quality (including water chlorination) and to promote prevention messages.
3.2.9. HIV/AIDS
An HIV outbreak was declared in Ratodero, Larkana District, Pakistan, on 25 April 2019, after several young children were reported to be HIV positive (Ahmed et al., Citation2019) following unsafe blood transfusion and lapses in basic health facilities. Of 38,000 people screened for HIV in Ratodero, 1,228 tested positive (3.23%). Of these positive cases, over 80% were children < 11.WHO and other partners deployed 25 experts to support the investigation and response to the HIV outbreak in Larkana District, Sindh Province. The experts provided technical support for HIV care, laboratory diagnosis, infection prevention and control, blood safety, and for outbreak investigation. Partners and donors collaborated to arrange laboratory testing equipment and establish HIV treatment centres. In addition, WHO provided hands-on clinical management training and set up prevention of mother-to-child transmission clinics. IEC materials were distributed to create awareness and urge people to avoid risky behaviours. A total of 1306 HIV-positive patients were registered at ART centres, and 1,258 received antiretroviral drugs, including 17 children born to HIV-positive mothers on prophylaxis to prevent mother-to-child transmission. Response measures are still ongoing (WHO, Citation2019i).
3.2.10. Measles
In 2019, a total of 56,090 suspected measles cases were reported from 22 countries in the region, among which 8716 were lab-confirmed (WHO, Citation2019a). The highest number of reported cases were in Yemen (9816), Pakistan (Citation9031), and Tunisia (6728) (WHO, Citation2019). In Lebanon, a total of 1,067 cases (zero deaths), 58% of which were laboratory-confirmed and 42% clinically confirmed, were reported by December 2019. The high transmission risk in Lebanon is driven by nationwide case distribution and low vaccination coverage at the national level, coupled with immunity gaps (WHO, Citation2019t). The country host around one million displaced Syrians with limited access to healthcare, limited funding for supplementary immunisation activities to improve measles vaccination coverage and for the epidemiological surveillance unit to support surveillance activities and capacity building(WHO, Citation2019t). WHO and other partners supported measles investigation and response in Lebanon; Lebanon MOH categorised the disease in inter-epidemic stage, the most affected age groups being < 5 and 5–9 years old. Measles vaccination coverage is varied and ranges from 17%−75% in different areas, and 29% of children in Lebanon aged 1–9 years old had received at least one dose of the vaccine. WHO supported MOH with enhanced epidemiologic surveillance, investigation, and social mobilisation. Supplementary immunisation campaigns were conducted in high-risk areas targeting unvaccinated children.
3.2.11. MERS
MERS cases were confirmed in Oman, Qatar, Saudi Arabia, and the United Arab Emirates in 2019, with most cases being reported in Saudi Arabia (WHO, Citation2019; WHO, Citation2019l). A total of 223 laboratory-confirmed cases and 56 associated deaths were reported in 2019 across the region, with 205 (92%) of these cases and 52 (93%) deaths reported from Saudi Arabia. Other countries that reported laboratory-confirmed cases of MERS in 2019 included Oman (13 cases, four deaths, CFR 30.77%) (WHO, Citation2019k), Qatar (three cases, no death), and United Arab Emirates (two cases, no death). Globally, none of the countries outside EMR reported any new cases of MERS in 2019.
In 2019, a total of five healthcare-associated clusters of MERS were reported, including two from Oman, two from Saudi Arabia, and one from Qatar. Of the five clusters, two were reported in hospitals, while three were from households. The two main clusters from Saudi Arabia reported 76 cases and 14 deaths (CFR 18.42%). WHO supported the affected countries in enhancing the reporting mechanisms of all cases while maintaining a regional database to document disease transmission mechanisms, risk factors, and probable prevention strategies. In addition, WHO provided technical guidelines to improve surveillance, laboratory diagnosis, clinical management, and contact tracing. WHO also supported an External Quality Assessment to detect MERS coronavirus by PCR as 100% of participating reference laboratories reported correct results for all specimens of MERS-CoV, with over 20 reference labs in EMR demonstrating good proficiency in MERS-CoV case detection (WHO, Citation2019).
3.2.12. Poliomyelitis
A total of 176 wild poliovirus 1 (WPV1) cases and zero deaths were reported in Afghanistan and Pakistan in 2019. Of these cases, 29 WPV1 were reported from nine provinces in Afghanistan. These included nine cases from Uruzgan province, five cases from Helmand province, six from Kandahar province, two from Paktika and Farah provinces, and one from Kunar, Nangarhar Badghis, Baghlan, and Herat provinces. The remaining 147 WPV1 cases were reported in Pakistan.
In addition to the WPVI, a total of 22 cases of circulating vaccine-derived poliovirus type 2 (cVDPV2) were reported from Pakistan as follows: four from Diamir district of Gilgit-Baltistan province; three each from Torghar, Khyber, and Mohmand; two from Kohistan Lower; and one each from Charsadda, Kohistan Upper, Bajour, Lakki Marwat, and Peshawar districts in Khyber Pakhtunkhwa; one each from Islamabad and Gujranwala district, Punjab province. WHO supported the governments in both countries to boost efforts to eradicate the disease through regular surveillance for identifying hotspots through testing the sewage water/environmental samples for WPV subtypes. In addition to EPI polio doses, several supplementary immunisation campaigns were conducted in high-risk areas to vaccinate missed children. Internal displacement and the prevailing security situation in both countries have resulted in the number of reported cases being higher compared to the last few years, and efforts are being made to reduce and eradicate the disease from both countries with commitment from the highest levels and partnering agencies.
3.2.13. Rift Valley fever (RVF)
The Federal MOH of Sudan declared a RVF outbreak in Week 37 (8‒17 September) of 2019. The first case was reported from the Red Sea State (Tohashban Village) and later spread to five other states. This was escalated by increasing human movement from armed conflict that has characterised the region in the recent past (Ahmed et al., Citation2020). A total of 548 cases of RVF and 11 associated deaths (CFR 2%) were reported in Sudan in 2019. Red Sea State (320 cases) and River Nile State (237 cases) were the most affected, accounting for 99% of cases (WHO, Citation2019q). Out of 153 samples that were tested, 53 tested positive.
In response to the outbreak, the Ministry of Livestock and Fisheries and the Federal MoH, collaborating with other partners, coordinated a response to the outbreak with enhanced surveillance to detect new cases in animals and humans, clinic management of human cases, integrated vector control activities and risk communication and community engagement.
4. Discussion
We analysed infectious disease outbreaks and the containment measures employed by the health authorities with the support of WHO to mitigate their spread in 2019. We found 24 infectious disease outbreaks from 13 different pathogens, reported from 10 countries with 1,012,535 suspected and laboratory-confirmed cases, 1,692 deaths, and a CFR of 0.17%.
There was an uneven distribution of the disease burden across the countries, with Yemen accounting for the largest share of the caseload (92%) from cholera and dengue fever, followed by Pakistan (6.6%, dengue fever). Similarly, Pakistan had the highest number of outbreaks (seven), followed by Sudan (five). The highest fatality ratio was due to MERS in Oman (30.8%) and Saudi Arabia at 25.4% (52/205). The current seventh cholera pandemic remains the biggest challenge in the region, with 864,542 cases reported in 2019, followed by dengue fever at 129,972 cases.
The wild poliovirus eradication remains a challenge in the region. Pakistan and Afghanistan still report cases due to constraints in reaching all children in critical areas due to insecurity and political instability (Bigouette et al., Citation2021). Similarly, immunisation coverage for vaccine-preventable diseases is still low in many countries in the region (Wesolowski et al., Citation2018). WHO supported ministries of health to strengthen essential systems to enhance the prevention and control of disease outbreaks, such as multisectoral coordination, surveillance, public health laboratories, guideline development, clinical management, risk communication and community engagement, and access to health services (WHO, Citation2021). WHO has worked closely with the Member States to improve public health preparedness and response capacities while addressing critical knowledge gaps through research studies. In addition, a regional network for experts and technical institutions was established to facilitate support for international outbreak response (Buliva et al., Citation2017; WHO, Citation2019h).
Despite some progress, multiple challenges remain in dealing with emerging and re-emerging infectious diseases, such as incomplete implementation of the National Action Plan for Health Security (NAPHS) and inadequate investment in International Health Regulations (IHR) core capacities. In addition, some of the outbreak-affected countries, e.g., Yemen, Somalia, and Afghanistan faced protracted or acute emergencies; that led to disrupted or underperforming health systems (Weill et al., Citation2019). In others, including Pakistan, Sudan, Djibouti, etc., the health systems were not well-performing or established due to financial and capacity constraints. This prolonged insecurity and inaccessibility in fragile countries like Syria, Yemen, Somalia, and Iraq have resulted in delayed implementation of the planned prevention and control activities and underutilisation of committed funds, leading to the spread of high-threat pathogen diseases to other areas (Alghazali et al., Citation2019). Further, there was always a demand for more technical, logistic, and financial support from the countries to tackle the outbreaks; however, it was sometimes challenging to identify resources, technical staff, and supplies to meet the countries’ needs (Yousaf et al., Citation2018).
Another challenge was the lack of integrated response plans within the affected countries, with all efforts dealing with specific outbreaks remaining piecemeal. In addition, frequent natural disasters in the region, including floods, droughts, heavy rains, etc., aggravated the existing situation resulting in increased cases.
In other instances, environmental triggers were known to cause some outbreaks, in which case control became difficult because of poor infrastructure and weakened health systems (Siddiqi et al., Citation2019; Wahid, Citation2019). Moreover, significant movements of people complicate the surveillance of disease outbreaks and the administration of prevention and control measures such as vaccination interventions (Rabaan, Citation2019).
Another challenge was the lack of awareness among the public about the risk and prevention of common zoonotic and vector-borne diseases like dengue fever resulting in the rapid spread of these outbreaks. Other outbreaks required the involvement of multiple ministries and departments involved in infrastructure, clean water supply, sanitation, disaster preparedness, agriculture and animal health. This added to the delay of constructive response activities due to some countries’ complexities occasioned by armed conflicts. Moreover, data gaps in routine reporting in the region were apparent, with some countries hardly releasing official data, and in cases where it was reported, data proved incomplete or inclusive.
Given the above challenges, we recommend a multisectoral approach to mitigating infectious diseases in EMR. Further efforts should be made to build comprehensive joint strategies in coordination with country governments and external partners for coordinated response and pooling of resources for optimal results. In addition, enhanced data systems and surveillance will go a long way in identifying outbreaks and containing them before they spread. In particular, and given the emerging and re-emerging nature of most outbreaks reported in the region, the investment and use of new disease surveillance methods and technologies, including the use of artificial intelligence (Agrebi & Larbi, Citation2020) could bolster surveillance and response capabilities (Otaigbe, Citation2022), thus turning the tide against the observed infections disease patterns.
In executing this study, some limitations are acknowledged. Poor surveillance or incorrect attribution could have caused some countries to misreport cases and fatalities. In addition, complexities in case definition (suspected, probable, confirmed), which differ from disease to disease or country to country, could have affected case ascertainment for some diseases. Again, the secondary nature of the data analysed means researchers did not have full control over how data was collected and reported. This notwithstanding, the knowledge, experiences and recommendations from this study may be helpful in outbreak prevention and control in similar contexts.
5. Conclusion
The WHO EMR remains an epicentre of emerging infectious disease outbreaks, with Pakistan, Afghanistan, Sudan, Yemen, and Somalia bearing the highest burden. Most outbreaks are preventable, but most of these countries face multiple challenges limiting prevention, early detection, and containment efforts. Weak health systems, limited investment in disease prevention and preparedness, armed conflicts, heavy rainfall, poor surveillance systems, health infrastructure, and gaps in knowledge about some infections exacerbate the situation.
Authors’ contributions
CSC, EM, and CWK wrote the draft manuscript, PO, RB, SE, AA, MT, EB, and AM reviewed, edited, and provided critical inputs and comments.
The researchers work for and support the surveillance and outbreak management workstream of the Infectious Hazard Prevention and Preparedness Unit of the WHO Health Emergencies Department of the WHO Regional Office for the Eastern Mediterranean. The workstream provides technical and operational support to WHO Member States to strengthen their capacities to conduct field investigations to rapidly identify, confirm and respond effectively to outbreaks of emerging infectious diseases (EIDs), many of them in emergency and fragile settings.
Acknowledgments
We are grateful to the WHO Country Offices in the Eastern Mediterranean Region and the Ministries of Health for sharing data and providing information on the response activities conducted for these outbreaks.
Disclosure statement
No potential conflict of interest was reported by the authors.
Data availability statement
The data and materials are available on the WHO EMR website https://www.emro.who.int/pandemic-epidemic-diseases/information-resources/weekly-epidemiological-monitor-2019.html.
Additional information
Funding
References
- Abubakar, A., Elkholy, A., Barakat, A., Shrestha, B., Elhakim, M., Malik, M. R., Bergeri, I., & Samaan, G. (2020). Pandemic influenza preparedness (PIP) framework: Progress challenges in improving influenza preparedness response capacities in the Eastern Mediterranean Region, 2014–2017. Journal of Infection and Public Health, 13(3), 446–17. https://doi.org/10.1016/j.jiph.2019.03.006
- Agrebi, S., & Larbi, A. (2020). Use of artificial intelligence in infectious diseases. Artificial Intelligence in Precision Health, 415–438. https://doi.org/10.1016/B978-0-12-817133-2.00018-5
- Ahmed, A., Ali, Y., Elduma, A., Eldigail, M. H., Mhmoud, R. A., Mohamed, N. S., Ksiazek, T. G., Dietrich, I., & Weaver, S. C. (2020). Unique outbreak of rift valley fever in Sudan, 2019. Emerging Infectious Diseases, 26(12), 3030–3033. https://doi.org/10.3201/eid2612.201599
- Ahmed, A., Hashmi, F. K., & Khan, G. M. (2019). HIV outbreaks in Pakistan. The Lancet HIV, 6(7), e418. https://doi.org/10.1016/S2352-3018(19)30179-1
- Akram, J., Khan, A. S., Khan, H. A., Gilani, S. A., Akram, S. J., Ahmad, F. J., & Mehboob, R. (2020). Extensively Drug-Resistant (XDR) Typhoid: Evolution, prevention, and its management. BioMed Research International, 2020, e6432580. https://doi.org/10.1155/2020/6432580
- Alghazali, K. A., Teoh, B.-T., Loong, S.-K., Sam, S.-S., Che-Mat-Seri, N.-A.-A., Samsudin, N.-I., Yaacob, C.-N., Azizan, N.-S., Oo, A., Baharudin, N.-A., Tan, K.-K., Abd-Jamil, J., Nor’e, S.-S., Khor, C.-S., Johari, J., Mahdy, M. A. K., & AbuBakar, S. (2019). Dengue outbreak during ongoing civil war, Taiz, Yemen. Emerging Infectious Diseases, 25(7), 1397–1400. https://doi.org/10.3201/eid2507.180046
- Ammar, W., Kdouh, O., Hammoud, R., Hamadeh, R., Harb, H., Ammar, Z., Atun, R., Christiani, D., & Zalloua, P. A. (2016). Health system resilience: Lebanon and the Syrian refugee crisis. Journal of Global Health, 6(2), 020704. https://doi.org/10.7189/jogh.06.020704
- Aslam, F., Yue, Y., & Aziz, M. (2021). Introduction of typhoid vaccine in the expanded immunisation program of Pakistan. Human Vaccines & Immunotherapeutics, 17(7), 2132. https://doi.org/10.1080/21645515.2020.1869496
- Baig, M. A., & Shaikh, B. T. (2012). Disease surveillance system: A mandatory conduit for effective control of infectious diseases in Pakistan. Asia Pacific Journal of Public Health, 24(4), 586–594. https://doi.org/10.1177/1010539510395377
- Basak, S., Singh, P., & Rajurkar, M. (2016). Multidrug resistant and extensively drug resistant bacteria: A study. Journal of Pathogens, 2016, 4065603. https://doi.org/10.1155/2016/4065603
- Bigouette, J. P., Wilkinson, A. L., Tallis, G., Burns, C. C., Wassilak, S. G. F., & Vertefeuille, J. F. (2021). Progress toward polio eradication—worldwide, January 2019–June 2021. MMWR Morbidity and Mortality Weekly Report, 70(34), 1129–1135. https://doi.org/10.15585/mmwr.mm7034a1
- Bloom, D. E., & Cadarette, D. (2019). Infectious disease threats in the twenty-first century: Strengthening the global response. Frontiers in Immunology, 10, 549. https://doi.org/10.3389/fimmu.2019.00549
- Buliva, E., Elhakim, M., Tran Minh, N. N., Elkholy, A., Mala, P., Abubakar, A., & Malik, S. M. M. R. (2017). Emerging and Reemerging Diseases in the World Health Organization (WHO) Eastern Mediterranean region—progress, challenges, and WHO initiatives. Frontiers in Public Health, 5, 276. https://doi.org/10.3389/fpubh.2017.00276
- Malik, M., Abubakar, A., Kholy, A. E., Buliva, E., Khan, W., Lamichhane, J., Moen, A., McCarron, M., Zureick, K., & Obtel, M. (2020). Improved capacity for influenza surveillance in the WHO Eastern Mediterranean Region: Progress in a challenging setting. Journal of Infection and Public Health, 13(3), 391–401. https://doi.org/10.1016/j.jiph.2019.07.018
- OCHA. (2021). Global humanitarian overview 2022. United Nations. https://doi.org/10.18356/9789210012423
- Otaigbe, I. (2022). Scaling up artificial intelligence to curb infectious diseases in Africa. Frontiers in Digital Health, 4, 1030427. https://doi.org/10.3389/fdgth.2022.1030427
- Rabaan, A. A. (2019). Cholera: An overview with reference to the Yemen epidemic. Frontiers of Medicine, 13(2), 213–228. https://doi.org/10.1007/s11684-018-0631-2
- Ramdan, M. I., Susanti, R., Ifroh, R. H., & Noviasty, R. (2018). Risk factors for diphtheria outbreak in children aged 1-10 years in East Kalimantan Province, Indonesia. F1000research, 7, 1625. https://doi.org/10.12688/f1000research.16433.1
- Siddiqi, R., Waseem, Y., & Naseeb, M. W. (2019). Drug-resistant typhoid epidemic in Pakistan highlights shortcomings of the public health infrastructure. JPMA The Journal of the Pakistan Medical Association, 69(1), 147–148.
- Spernovasilis, N., Siakallis, G., Tsiodras, S., & Poulakou, G. (2017). Child refugees in Europe and infectious diseases: Threat or Threatened? International Journal of School Health, 4(4), 1–3. https://doi.org/10.5812/intjsh.57923
- Spernovasilis, N., Tsiodras, S., & Poulakou, G. (2022). Emerging and re-emerging infectious diseases: Humankind’s companions and competitors. Microorganisms, 10(1), 98. https://doi.org/10.3390/microorganisms10010098
- Tharwani, Z. H., Kumar, P., Salman, Y., Islam, Z., Ahmad, S., & Essar, M. Y. (2022). Typhoid in Pakistan: Challenges, efforts, and recommendations. Infection and Drug Resistance, 15, 2523–2527. https://doi.org/10.2147/IDR.S365220
- Wahid, B. (2019). Current status of dengue virus, poliovirus, and chikungunya virus in Pakistan. Journal of Medical Virology, 91(10), 1725–1728. https://doi.org/10.1002/jmv.25513
- Weill, F.-X., Domman, D., Njamkepo, E., Almesbahi, A. A., Naji, M., Nasher, S. S., Rakesh, A., Assiri, A. M., Sharma, N. C., Kariuki, S., Pourshafie, M. R., Rauzier, J., Abubakar, A., Carter, J. Y., Wamala, J. F., Seguin, C., Bouchier, C., Malliavin, T., Bakhshi, B., & Quilici, M.-L. (2019). Genomic insights into the 2016–2017 cholera epidemic in Yemen. Nature, 565(7738), 230–233. https://doi.org/10.1038/s41586-018-0818-3
- Wesolowski, A., Winter, A., Tatem, A. J., Qureshi, T., Engø-Monsen, K., Buckee, C. O., Cummings, D. A. T., & Metcalf, C. J. E. (2018). Measles outbreak risk in Pakistan: Exploring the potential of combining vaccination coverage and incidence data with novel data-streams to strengthen control. Epidemiology and Infection, 146(12), 1575–1583. https://doi.org/10.1017/S0950268818001449
- WHO. (2019). Measles outbreak in Lebanon. Weekly Epidemiological Monitor, 12(40), 40–43. https://applications.emro.who.int/docs/epi/2019/Epi_Monitor_2019_12_40.pdf?ua=1&ua=1
- WHO. (2019). OCV Campaign in Somalia 2019. Weekly Epidemiological Monitor, 12(28), 28–33. https://applications.emro.who.int/docs/epi/2019/Epi_Monitor_2019_12_28.pdfhttps://doi.org/10.24945/MVF.03.19.1866-0533.2142 https://applications.emro.who.int/docs/epi/2019/Epi_Monitor_2019_12_28.pdfhttps://doi.org/10.24945/MVF.03.19.1866-0533.2142
- WHO. (2019). Weekly Epidemiological Monitor. Monitor, 12(18), 18–20. https://applications.emro.who.int/docs/epi/2019/Epi_Monitor_2019_12_18.pdf?ua=1&ua=1
- WHO. (2019). Measles situation in EMR. Weekly Epidemiological Monitor, 12(22), 22. https://applications.emro.who.int/docs/epi/2019/Epi_Monitor_2019_12_22.pdf?ua=1&ua=1
- WHO. (2019). MERS-Cov Laboratory EQA. Weekly Epidemiological Monitor, 12(26), 26–27. https://applications.emro.who.int/docs/epi/2019/Epi_Monitor_2019_12_26.pdf?ua=1&ua=1
- WHO. (2019a). Measles and rubella monthly bulletin [monthly bulletin]. WHO Regional Office for the Eastern Mediterranean. http://www.emro.who.int/images/stories/vpi/documents/measles_rubella_2019_emr.pdf?ua=18
- WHO. (2019b). CCHF cases continuously reported in Afghanistan. Weekly Epidemiological Monitor, 12(33). https://applications.emro.who.int/docs/epi/2019/Epi_Monitor_2019_12_33.pdf?ua=1&ua=1
- WHO. (2019c). Cholera outbreak in Sudan. Weekly Epidemiological Monitor, 12(38). https://applications.emro.who.int/docs/epi/2019/Epi_Monitor_2019_12_38.pdf?ua=1&ua=1
- WHO. (2019d). Dengue cases upsurge, Punjab, Pakistan. Weekly Epidemiological Monitor, 12(35). https://applications.emro.who.int/docs/epi/2019/Epi_Monitor_2019_12_35.pdf?ua=1&ua=1
- WHO. (2019e). Dengue fever in Oman. Weekly Epidemiological Monitor, 12(3). https://applications.emro.who.int/docs/epi/2019/Epi_Monitor_2019_12_3.pdf?ua=1&ua=1
- WHO. (2019f). Dengue in Yemen: Situation update. Weekly Epidemiological Monitor, 12(32). https://applications.emro.who.int/docs/epi/2019/Epi_Monitor_2019_12_32.pdf?ua=1&ua=1
- WHO. (2019g). Diphtheria in Sudan. Weekly Epidemiological Monitor, 12(49). https://applications.emro.who.int/docs/EPI/2019/22244220-2019-12-49.pdf?ua=1&ua=1
- WHO. (2019h). Disease outbreaks in Eastern Mediterranean Region (EMR), January to December 2019. Weekly Epidemiological Monitor, 12(52). https://applications.emro.who.int/docs/EPI/2019/22244220-2019-12-52.pdf?ua=1&ua=1
- WHO. (2019i). HIV Investigation in Pakistan. Weekly Epidemiological Monitor, 12(25). https://applications.emro.who.int/docs/epi/2019/Epi_Monitor_2019_12_25.pdf?ua=1&ua=1
- WHO. (2019j). Knowledge gaps: Multiple drug resistant typhoid fever in Pakistan. Weekly Epidemiological Monitor, 12(6). https://applications.emro.who.int/docs/epi/2019/Epi_Monitor_2019_12_6.pdf?ua=1&ua=1
- WHO. (2019k). MERS cluster in Oman. Weekly Epidemiological Monitor, 12(5). https://applications.emro.who.int/docs/epi/2019/Epi_Monitor_2019_12_5.pdf?ua=1&ua=1
- WHO. (2019l). MERS cluster in Wadi Aldwaser, Saudi Arabia. Weekly Epidemiological Monitor, 12(7). https://applications.emro.who.int/docs/epi/2019/Epi_Monitor_2019_12_7.pdf?ua=1&ua=1
- WHO. (2019m). OCV campaign Sudan. Weekly Epidemiological Monitor, 12(44). https://applications.emro.who.int/docs/epi/2019/22244220-2019-12-44.pdf?ua=1&ua=1
- WHO. (2019n). Oral cholera vaccine (OCV) campaign in Yemen. Weekly Epidemiological Monitor, 12(21). https://applications.emro.who.int/docs/epi/2019/Epi_Monitor_2019_12_21.pdf?ua=1&ua=1
- WHO. (2019o). Rapid Response Teams trainings in Pakistan. Weekly Epidemiological Monitor, 12(15). https://applications.emro.who.int/docs/epi/2019/Epi_Monitor_2019_12_15.pdf
- WHO. (2019p). Resurgence of Chikungunya in Sudan. Weekly Epidemiological Monitor, 12(29). https://applications.emro.who.int/docs/epi/2019/Epi_Monitor_2019_12_29.pdf?ua=1&ua=1
- WHO. (2019q). Rift Valley fever Sudan. Weekly Epidemiological Monitor, 12(43). https://applications.emro.who.int/docs/epi/2019/22244220-2019-12-43.pdf?ua=1&ua=1
- WHO. (2019r). Upsurge of cholera cases in Yemen. Weekly Epidemiological Monitor, 12(12). https://applications.emro.who.int/docs/epi/2019/Epi_Monitor_2019_12_12.pdf?ua=1&ua=1
- WHO. (2019s). Upsurge of Cholera in Somalia. Weekly Epidemiological Monitor, 12(23). https://applications.emro.who.int/docs/epi/2019/Epi_Monitor_2019_12_23.pdf?ua=1&ua=1
- WHO. (2019t). Workshop on evaluation of Yemen’s surveillance system. Weekly Epidemiological Monitor, 12(46). https://applications.emro.who.int/docs/EPI/2019/22244220-2019-12-46.pdf?ua=1&ua=1
- WHO. (2020). Diphtheria situation update: Sudan. Weekly Epidemiological Monitor, 13(2). https://applications.emro.who.int/docs/epi/2020/22244220-2020-13-02.pdf?ua=1
- WHO. (2021). The work of WHO in the Eastern Mediterranean Region: Annual report of the Regional Director 2020. WHO Regional Office for the Eastern Mediterranean. https://apps.who.int/iris/handle/10665/335963
- WHO EMRO. (2018). The work of WHO in the Eastern Mediterranean Region: Annual report of the Regional Director 2018. WHO Regional Office for the Eastern Mediterranean. https://applications.emro.who.int/docs/9789290222781-2019-en.pdf?ua=1
- WHO EMRO. (2019a, November 23). Outbreak update – Cholera in Sudan. Epidemic and Pandemic-Prone Diseases. http://www.emro.who.int/pdf/pandemic-epidemic-diseases/cholera/outbreak-update-cholera-in-sudan-23-november-2019.pdf?ua=1
- WHO EMRO. (2019b). Situation Report September 2019. https://applications.emro.who.int/docs/yem/Yem-Sitrep-Sept-2019.pdf?ua=1&ua=1
- WHO EMRO. (n.d.). Weekly Epidemiological Monitor. World Health Organization - Regional Office for the Eastern Mediterranean. Retrieved July 30, 2022, from http://www.emro.who.int/pandemic-epidemic-diseases/information-resources/weekly-epidemiological-monitor.html
- Yousaf, M. Z., Ashfaq, U. A., Anjum, K. M., & Fatima, S. (2018). Crimean-Congo Hemorrhagic Fever (CCHF) in Pakistan: The “Bell” is ringing silently. Critical Reviews in Eukaryotic Gene Expression, 28(2), 93–100. https://doi.org/10.1615/CritRevEukaryotGeneExpr.2018020593