Abstract
Physical activity (PA) is widely recognised as being integral to physical and mental wellbeing. The World Health Organisation recommends around 150–300 minutes of moderately intense PA per week for adults aged 18–64 years. Physical inactivity costs the UK £7.4 billion per year and is associated with one out of every six deaths that occur in the country. The review aims at exploring the barriers and facilitators to making healthy PA lifestyle choices among UK BAME adults during the COVID-19 pandemic. Database searches were conducted in CINAHL, AMED, Medline, SCOPUS, COCHRANE, EMBASE, and Web of Science. There are 53 records that were identified. After removing three duplicates, the titles and abstracts of 50 papers were screened. Of these, all but 50 studies were excluded after reviewing the title and abstracts, resulting in no studies eligible for inclusion. Data extraction using the JBI-QARI data extraction template was performed, followed by a narrative synthesis of the resulting data; however, no eligible studies were identified. This empty systematic review without meta-analysis, highlighted major research gaps and indicated the state of the evidence between 2019–2021. The review has, through the application of theoretical models (COM-B and TTM), highlighted themes that need to be addressed.
Introduction
Overtime, physical activity (PA) is any body movement produced by skeletal muscles that requires energy intake (Caspersen et al., Citation1985; Dasso, Citation2019; Mbabazi et al., Citation2022b). PA is a lifestyle choice with several advantages for both physical and mental health (Velten et al., Citation2018), however, culture and ill health may impede engagement for many. Recommendations for PA lower the risks of health-related chronic physical inactivity diseases, for example, cardiovascular diseases, diabetes, osteoporosis, reduced fertility, and some cancers (Bull et al., Citation2020; Mbabazi et al., Citation2022a), together with impacts on mental well-being.
Research suggests that exercise may be as simple as a daily 15–30-minute walk (Paluch et al., Citation2022). This has been reported to benefit brain function and boost endorphins, subsequently enhancing mental wellbeing (Stults-Kolehmainen & Sinha, Citation2014; Wojtys, Citation2015). PA has also been proven to enhance an individual’s immune response against respiratory viruses and diseases, such as COVID-19 (Shah et al., Citation2020). In addition, PA participation increases an individual’s psychological, social, and physical well-being. Such findings are recognised globally and evidenced within policy formation (Stults-Kolehmainen & Sinha, Citation2014).
Reflecting on the above, GOV.UK (Citation2019) recommends that adults aged 18–64 should undertake 150–300 minutes of moderate-intensity aerobic PA or 75–150 minutes of vigorous-intensity aerobic PA each week. This should also incorporate muscle-strengthening activities, thereby working all the main muscle groups. Adults aged 65 and older should follow the same PA recommendations as adults, but they should focus on adaptive balance and strength training three or more days a week. The consensus is that any PA is better than none if the above levels cannot be attained. Even though research has found higher rates of physical inactivity among UK adults than in other European countries such as France, Australia, the Netherlands, and Finland, this finding does not demonstrate the diversity of the population within the UK and their respective engagements with PA (GOV.UK, Citation2019).
In the UK, it is broadly understood that many Black, Asian, and minority ethnic (BAME) individuals live a sedentary lifestyle, resulting in worse healthcare (Mbabazi et al., Citation2022a; Stockwell et al., Citation2021; Wickersham et al., Citation2021; Wunsch et al., Citation2022). Recent research studies found that COVID-19 subsequent lockdowns exacerbated the physical and mental health of sedentary and chronically ill UK adult BAME individuals (Ng et al., Citation2021; Stockwell et al., Citation2021). This has led to a drive to create PA solutions for these populations, thereby reducing the number of incidences, prevalence, and mortality rates induced by sedentary lifestyles (Kokkinos, Citation2012; Smith et al., Citation2020). The fact that many individuals in BAME communities are either overweight or obese makes this a particularly pressing concern in context of the well-documented physical and mental health challenges they experience.
In March 2020, World Health Organisation proclaimed the COVID-19 outbreak a worldwide pandemic (Stockwell et al., Citation2021; Wunsch et al., Citation2022). Over 420,000 confirmed cases were confirmed worldwide by October 2020, resulting in nearly 1,150,00 fatalities. Many nations used ‘lockdown’ to prevent COVID-19 transmission, enforcing periods of social isolation with limits placed on distances one could travel from home and the prohibition of ‘unnecessary daily activities’ (Mbabazi et al., Citation2022a; Stockwell et al., Citation2021). These subsequent lockdowns impacted all aspects of life as reflected within the UK (Mbabazi et al., Citation2022b; Wunsch et al., Citation2022).
COVID-19 lockdowns impacted all social, physical, and mental aspects of human existence (Mbabazi et al., Citation2022b) and resulted in many individuals adopting a sedentary lifestyle (Gehlhar et al., Citation2022). This was discovered to have a significant impact on many more vulnerable adults, particularly those with underlying respiratory conditions, for whom outdoor space and exercise are critical to physical well-being (Spruit et al., Citation2016).
Despite the issues outlined above, many individuals found ways to maintain and even enhance their PA participation during these challenging times (Howlett et al., Citation2019). To get them to work with more hesitant groups, like some BAME, it is important to understand what motivates them. To facilitate this, a critical evaluation and analysis using theoretical models like the compatibility, opportunity, motivation, and behaviour (COM-B) model and the transtheoretical model of behaviour change (TTM) can be used (Howlett et al., Citation2019; Jiménez-Zazo et al., Citation2020; Kanavaki et al., Citation2017; Willmott et al., Citation2021).
Previous studies suggest that TTM improves adults’ PA behaviours (Jiménez-Zazo et al., Citation2020; Murakami et al., Citation2021). More studies integrating the four behaviour change aspects of TTM are required to analyse the influence of this model on the barriers and facilitators of PA in the BAME group (Jiménez-Zazo et al., Citation2020). This research seeks to explore the barriers and facilitators to making healthy physical activity lifestyle choices among UK BAME adults during the COVID-19 pandemic, through the TTM and COM-B models. This SR is the result of a published protocol in the International Journal of Physical Activity and Health (Mbabazi et al., Citation2022b).
Rationale for the SR
The COVID-19 pandemic’s disproportionate impact on BAME groups highlights the need to investigate them more thoroughly. Despite making up just 13% of the UK population, 35% of COVID-19 critical care patients in England were BAME (Flynn et al., Citation2020). BAME groups were found to be at greater risk of COVID-19 infection, with worse health outcomes and increased mortality rates (Flynn et al., Citation2020). Blacks and South Asians died five times more than Caucasians population (Office for National Statistics, Citation2020). COVID-19, according to researchers, has disrupted health-related behaviours and compromised PA participation across all populations (Nicomedes & Avila, Citation2020). The COVID-19 pandemic and the government’s imposed standard operating procedures of staying home exacerbated adult BAME individuals’ sedentary lifestyles.
No known systematic review (SR) has investigated current primary research exploring the barriers and facilitators to PA among BAME adults in the UK during the COVID-19 pandemic. The study explores this population’s experiences and perceptions of facilitators and barriers to PA participation during the COVID-19 pandemic.
Objectives
To identify current peer-reviewed literature in this specific area.
To explore the influence of the COVID-19 pandemic on the lifestyle choices related to PA participation among UK BAME adults.
To examine the perceptions of UK BAME adults towards PA lifestyle choices.
To determine the enablers, barriers and challenges to improving PA lifestyle choices within the UK adult BAME population.
Methods
This systematic review is registered in PROSPERO 2022 with reference number CRD42022320070. The PRISMA Guidelines for Preferred Reporting Items for Systematic Reviewers and Meta-Analyses were followed in this systematic review. The full protocol for this systematic review has been published in the International Journal of Physical Activity and Health (Mbabazi et al., Citation2022b).
Search strategy
A SR question should be specific, precise, succinct, and comprehensive to direct the literature search. SPIDER (Sample, Phenomenon of Interest, Design, Evaluation and Research Type) was adapted from the PICO (Population, Intervention, Comparison and Outcomes) framework to conduct searches for qualitative studies. In research conducted by Smith et al. (Citation2011), SPIDER demonstrated itself as a tool that makes it simple to create search phrases that align with the main elements of the search question. In this SR of qualitative studies, the SPIDER tool was used as an organising framework to identify the keywords in the search questions ( and ).
Table 1. Demonstrates SPIDER (Sample, Phenomenon of Interest, Design, Evaluation and Research Type) and for the selection of research key terms used in the study.
Table 2. Demonstrates keywords and synonyms using SPIDER tool.
Using the Boolean operators "OR" (for sensitivity) and "AND" (for specificity), link keywords will be applied, further refining the process. The use of operators like ‘AND’, ‘OR’, and ‘NOT’ enhances the precision of the search, making it possible to include or exclude certain terms or to search for articles that contain any one of a set of specified terms (Smith et al., Citation2011). The following comprehensive electronic database searches for example CINAHL, Medline, SCOPUS, COCHRANE, EMBASE, and Web of Science databases were undertaken from 2019 to 2021 (Appendix 1a).
The rationale for conducting a database from 2019 to 2021 was to find contemporary research on primary qualitative studies on barriers and facilitators of physical activity among adult BAME (18 years and older) populations during the COVID-19 pandemic in the UK between 2019–2021 ().
Table 3. Demonstrates keywords and synonyms combined using Boolean operators.
Appendix 1a demonstrates the database-specific search techniques. A bibliographic dataset was developed from the search results, and duplicate entries were eliminated. Two reviewers (JM and FM) independently checked the titles and abstracts of the retrieved papers to see whether they should be included. These two separate writers then examined the entire texts of any relevant publications to determine if they should be included. Discussions were used to settle disagreements. Where there was no consensus, the third reviewer (LAN) would make the decision.
Inclusion/exclusion criteria
Peer-reviewed qualitative studies (for example, using focus groups or semi-structured interviews with a qualitative component) were included with studies about adult BAME populations in the UK. Only studies written in English and published between 2019 to 2021 were included. Any studies that did not meet these criteria were excluded ().
Table 4. Demonstrating inclusion and exclusion criteria.
Study selection
Study selection was done in three steps; the titles and abstracts of relevant papers were independently screened by two authors (JM and FM). The full text of potentially relevant papers was then reviewed for inclusion by these two independents (JM and FM) based upon methodological quality. Sifting was done by two researchers (JM and FM), and in case of a disagreement, a third researcher (LAN) would have been involved. In this review, disagreements were resolved through discussion.
Quality assessment of included literature
Had we found any eligible study, two authors (JM and FM) would have independently assessed the risk of bias in eligible studies. The Critical Appraisal Skills Programme (CASP) checklist would have been used to assess the quality of this (Long et al., Citation2020). Disagreements among reviewers would have been resolved through consultation and discussion with a third independent reviewer (LAN).
Data extraction
As this was an empty review, data extraction was not carried out. If we had found eligible studies, two authors (JM and FM) would have independently extracted data from eligible studies using the JBI-QARI (Joanna Briggs Institute) (Munn et al., Citation2014). Data extraction was guided using the SPIDER framework, which was adapted from the PICO (Population, Intervention, Comparison, and Outcomes) framework to conduct searches for qualitative studies. In this SR of qualitative studies, the SPIDER tool was used as an organising framework to identify the keywords in the search questions. This means that the SPIDER framework was used to capture barriers and facilitators of physical activity among the adult BAME population in the UK during the COVID-19 pandemic. Lastly, data outcomes were extracted, and this included data on barriers and facilitators (enablers). The third reviewer (LAN) was available to address any inconsistencies.
Data synthesis
If articles that were suitable for the review had been found, we would have used a narrative approach to synthesise the results.
Summary of findings and assessment of the certainty of the evidence
Not applicable to the current review.
Results
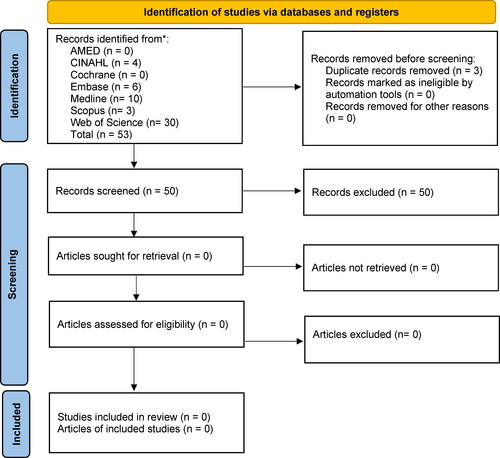
There are 53 records that were identified through AMED, CINAHL, Medline, Scopus, Web of Science, Embase, and Cochrane Library database searches. After removing three duplicates, the titles and abstracts of 50 papers were screened. Of these, all but 50 studies were excluded after reviewing the title and abstract, resulting in no studies eligible for inclusion in this review ().
Discussion
This review was carried out during COVID-19 pandemic, which could explain the barriers as to why there were no qualitative studies on facilitators and barriers to PA participation in the adult BAME population in the period of 2019–2021. No study satisfied all the inclusion criteria; hence, in this review there are no primary qualitative studies obtained about barriers and facilitators to making healthy PA lifestyle choices among UK BAME adults during the COVID-19 pandemic in this SR of qualitative studies, as demonstrated in the PRISMA flow diagram.
PA aspects and theoretical underpinnings
PA has been linked to improved physical health outcomes, including good body image or body satisfaction and the management of long-term illnesses or conditions that may be exacerbated through sedentary lifestyles, such as obesity, diabetes, and hypertension (Kaur et al., Citation2020). The management of such conditions requires regular PA engagement, enabling longer and healthier lives (Williams & Law, Citation2018). However, the COVID-19 pandemic and subsequent lockdowns exacerbated health concerns in individuals with pre-existing conditions (Singh et al., Citation2020). This was particularly concerning upon the contraction of COVID-19, resulting in increased rates of hospitalisation and mortality (Fung & Babik, Citation2021).
Within the UK population, particularly the BAME who gained weight and became morbidly obese through the lockdown restrictions, there was increased dissatisfaction with their body image, leading to low self-esteem and confidence, and depression for many (Vall-Roqué et al., Citation2021). Many individuals who identified with mental health issues during this time identified the COVID-19 lockdowns and restrictions as the primary cause (Pringle et al., Citation2022; Theis et al., Citation2021). This was compounded through compulsory furlough (suspension of jobs), combined with the adoption of a sedentary lifestyle (Dunton et al., Citation2020). Even for those with access to gardens whereby some levels of PA could be maintained, motivation was impacted by the fear of contracting COVID-19 (Kaur et al., Citation2020; Newbold et al., Citation2021). These combined limitations were found to affect BAME populations’ social, physical, psychological, and economic status holistically (Williams et al., Citation2016; Otu et al., Citation2020). Following the previous lockdown, the BAME population are still trying to deal with the long-term effects of living post the COVID-19 pandemic (Mahmood et al., Citation2021).
During the pandemic, there were environmental challenges and lockdowns that affected the general population (Constandt et al., Citation2020). The experiences and perceptions of the importance of living a physically active lifestyle can be examined from individual, structural and community perspectives (McPhee et al., Citation2016). Conversely, many BAME individuals who previously led sedentary lifestyles commenced engagement in vigorous PA during the pandemic, resulting in extreme fatigue and injury for some (Romero-Blanco et al., Citation2020), leading to an association of pain with PA and the giving up of such activities (Thivel et al., Citation2018).
Theoretical underpinnings: role of COM-B model and transtheoretical model (TTM)
COM-B model
The COM-B model suggests that every behaviour (B) has three main components: capability (C), opportunity (O), and motivation (M). To engage in each behaviour, individuals must be mentally and physically capable of doing so (C), have the social and physical opportunity to engage in the behaviour (O), and want or need to engage in the behaviour more than other competing behaviours (M). As each of these factors interacts, interventions must target one or more of them to produce and sustain successful behaviour change (Boyd et al., Citation2020; Michie et al., Citation2011; Michie & West, Citation2021). The COM-B model has been beneficial in identifying personal, societal, and environmental determinants that promote or inhibit PA in adults (Timlin et al., Citation2021).
The COM-B model of behaviour also provides a conceptual framework for constructing programmes aimed at modifying behaviour, such as PA (Michie et al., Citation2011; Michie & West, Citation2021). The relationship between competence, opportunity and motivation suggests that increasing capability and opportunity might enhance motivation to do PA (Rosenkranz et al., Citation2021), thereby forming a cyclical pattern where modifying behaviour may affect capacity, opportunity, and/or motivation (Michie & West, Citation2021). Consequently, behaviour is an integral part of an interacting and developing system. Changes in capacity, opportunity, and motivation must be directly influenced to produce a sustainable change in behaviour.
Many BAME adults post-lockdown found the need to work had to be prioritised over their general wellbeing, inhibiting engagement with PA (Stalsberg & Pedersen, Citation2018; de Boer et al., Citation2021; Withall et al., Citation2011). Others found it difficult to commit to regular PA participation due to childcare issues.
The study findings support the explanation ability of the COM-B model in the context of adult PA (Bethancourt et al., Citation2014; Willmott et al., Citation2021). Adult physical activity barriers and facilitators have been identified as potential policy leads to a better future (Bethancourt et al., Citation2014). More research is required to evaluate the current study’s findings among diverse populations and contexts (Leung, Citation2015; Willmott et al., Citation2021).
When used in combination with the TTM model, COM-B enables the identification of multiple distinct explanatory components that can help explain potential influences on behaviour and capture motivations (Hashemzadeh et al., Citation2019). It has been argued that interventions theoretically underpinned by such behaviour change models help ensure predictable and lasting change (Michie et al., Citation2011).
Transtheoretical model (TTM)
TTM conceptualises behaviour change as a six-stage process, which includes precontemplation, contemplation, preparation, action, maintenance, and termination (Hashemzadeh et al., Citation2019; Murakami et al., Citation2021; Prochaska & Velicer, Citation1997). These phases are transtheoretical and include changing ideas from a range of intervention concepts. Additionally, the behavioural process includes counter conditioning, which leads to the replacement of inactive habits with healthy actions such as helping relationships and the ability to search for social support in sports practice, thereby facilitating further changes (Laird et al., Citation2018; Stonerock & Blumenthal, Citation2017).
Adoption of the TTM is identified as having benefits and drawbacks for PA decision-making (Liu et al., Citation2018). Advantages include the perceived benefits of regular PA (increased fitness), while disadvantages include preconceptions of the problems associated with irregular PA participation due to painful experiences (Booth et al., Citation2012). The TTM seeks to explore the modification of individual behaviour, specifically the PA lifestyle of the adult BAME population in this instance (Hashemzadeh et al., Citation2019; Jiménez-Zazo et al., Citation2020). It may also explain the continuous movement of individuals through six different stages of behavioural change.
As previously noted, this review identified no research findings capturing the BAME experiences or perceptions in the pre-contemplation and contemplation stages about the barriers and facilitators on PA during COVID-19. This is a significant limiting factor, necessitating the need for further research in order that future PA policies may accurately target the fundamental issues.
There were significant fears, stress, stigma and depression aggravated by the COVID-19 pandemic, which were further reinforced by media coverage highlighting the BAME populations’ vulnerability to contraction of the virus, creating a demotivating force and barrier to both physical and social activities (Cabarkapa et al., Citation2020; Rajkumar, Citation2020). The COM-B model is a powerful diagnostic tool that allows researchers to identify the barriers to behaviour and design solutions that are more likely to influence the capability, opportunity, and motivation needed for individuals, groups, or populations (Michie & West, Citation2021). The TTM can be used to assess willingness to change behavioural lifestyles (Hashemzadeh et al., Citation2019), for example, physical activity, because it appeals to the whole population rather than the minority ready to act. Both models are suitable to understand behaviours in adult BAME individuals and thus suitable for the review study. The use of behavioural theoretical underpinnings such as the TTM and COM-B models allows researchers to understand and provide solutions on how policy and public health experts can devise effective and meaningful policies to improve PA and potentially reduce the associated health impacts of inactivity seen in the National Health Service(NHS) (Davis et al., Citation2015; Kwasnicka et al., Citation2016).
Conclusion
The COM-B and TTM models explain human behaviour changes, especially in PA participation. The COM-B model summarises how individual and internal variables interact with social and environmental contexts to attain behavioural objectives. The TTM and COM-B models help capture the experiences of adult BAME individuals regarding barriers and facilitators to PA engagement. Theoretical underpinnings are needed to enhance behaviour modification and lead to sustainable change. This review established the need for increased peer-reviewed primary research into the experiences or perceptions of barriers and facilitators to making healthy choices about PA among BAME adults in the UK during the COVID-19 pandemic, thereby highlighting major research gaps and indicating the state of the evidence between 2019–2021 that needs to be filled.
Recommendations
The lack of current peer-reviewed papers highlights the research gap on barriers and facilitators to making healthy PA lifestyle choices among UK BAME adults during the COVID-19 pandemic. As a result, primary research is required to capture experiences on the barriers and facilitators to making healthy PA lifestyle choices among UK BAME adults during and after the COVID-19 pandemic. This could help in the long-term reduction of physical inactivity-induced health issues and the subsequent burden this may place on NHS resources. Future government policies and health-related initiatives should reflect the findings of previous research, which found PA to be as effective as medicine and, as such, recommend its use by all.
Supplementary material 17 sept 2023.docx
Download MS Word (37.8 KB)Public Interest Statement 17 sept 2023.docx
Download MS Word (13.2 KB)Authors Biography.docx
Download MS Word (13.2 KB)Additional information
Notes on contributors
Johnson Mbabazi
Dr. Johnson Mbabazi, an associate lecturer at Teesside University. He is also the co-founder and chairman of the Teesside University Health Students Research Network. He is a Fellow of the Royal Society of Public Health, a Fellow of the European Public Health Association, and an associate of the Royal College of Physicians. He has published a lot of peer-reviewed articles and books. A multiple international award-winning author and UK Plaque winner. This systematic review is registered in PROSPERO 2022 with reference number CRD42022320070. The findings of this review were disseminated at a poster presentation. The 67th Annual Scientific Meeting at the University of Newcastle Society for Social Medicine and Population Health (SSM) conference poster abstract will help to highlight barriers and facilitators of the physical activities of ethnic minorities and improve policies during COVID-19 and future pandemics.
Fiona MacGregor
Fiona MacGregor is a Principal Lecturer for International, SHLS Allied Health at Teesside University and part of the member of the Teesside University Health Student Research Network (TUHSRN).
Jeff Breckon
Prof. Jeff Breckon is Associate Dean for Research and Innovation in the School of Health and Life Sciences at Teesside University and member of TUHSRN.
Barry Tolchard
Prof. Barry Tolchard is Director of Integrated Care Academy and a member TUHSRN.
David Watson
David Watson, Academic librarian at Teesside University
Julie Hogg
Julie Hogg an academic librarian at Teesside University
Edward Kunonga
Prof. Edward Kunonga is a lecturer and a member of TUHSRN at Teesside University
Dorothy Irene Nalweyiso
Dr. Dorothy Irene Nalweyiso is Doctor of Public Health at Teesside University, part time lecturer at Makerere University and a member TUHSRN.
Jennifer Teke
Dr. Jennifer Teke is Doctor of Public Health at Teesside University, Head of Research & Innovation at Medway Community Hospital and a member of TUHSRN.
Rosemary Dawson
Rosemary Dawson is a consultant midwife and a member of TUHSRN.
George William Kagugube
George William Kagugube is an associate lecturer and a PhD student at University College London as well as a member of TUHSRN.
Mona Salman
Dr. Mona Salman Doctor of Public Health at Teesside University and a member TUHSRN
Andrew S. Richardson
Dr. Andrew S. Richardson is Doctor of Public Health at Teesside University and a member TUHSRN.
Misheck Nkhata
Dr. Misheck Nkhata is a Lecturer in Global Public Health at Teesside University and a m ember of TUHSRN.
Lawrence Achilles Nnyanzi
Dr. Lawrence Achilles Nnyanzi is a Senior Lecturer in Research Methods Programme Leader Doctorate in Public Health and a member of TUHSRN
References
- Bethancourt, H. J., Rosenberg, D. E., Beatty, T., & Arterburn, D. E. (2014). Barriers to and facilitators of physical activity program use among older adults. Clinical Medicine & Research, 12(1–2), 1–11. https://doi.org/10.3121/cmr.2013.1171
- Booth, F. W., Roberts, C. K., & Laye, M. J. (2012). Lack of exercise is a major cause of chronic diseases. Comprehensive Physiology, 2(2), 1143–1211. https://doi.org/10.1002/cphy.c110025
- Boyd, J., McMillan, B., Easton, K., Delaney, B., & Mitchell, C. (2020). Utility of the COM-B model in identifying facilitators and barriers to maintaining a healthy postnatal lifestyle following a diagnosis of gestational diabetes: a qualitative study. BMJ Open, 10(8), e037318. https://doi.org/10.1136/bmjopen-2020-037318
- Bull, F. C., Al-Ansari, S. S., Biddle, S., Borodulin, K., Buman, M. P., Cardon, G., Carty, C., Chaput, J.-P., Chastin, S., Chou, R., Dempsey, P. C., DiPietro, L., Ekelund, U., Firth, J., Friedenreich, C. M., Garcia, L., Gichu, M., Jago, R., Katzmarzyk, P. T., … Willumsen, J. F. (2020). World Health Organization 2020 guidelines on physical activity and sedentary behaviour. British Journal of Sports Medicine, 54(24), 1451–1462. https://doi.org/10.1136/bjsports-2020-102955
- Cabarkapa, S., Nadjidai, S. E., Murgier, J., & Ng, C. H. (2020). The psychological impact of COVID-19 and other viral epidemics on frontline healthcare workers and ways to address it: A rapid systematic review. Brain, Behavior, & Immunity – Health, 8, 100144. https://doi.org/10.1016/j.bbih.2020.100144
- Caspersen, C. J., Powell, K. E., & Christenson, G. M. (1985). Physical activity, exercise, and physical fitness: Definitions and distinctions for health-related research. Public Health Reports (Washington, D.C.: 1974), 100(2), 126–131. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1424733/pdf/pubhealthrep00100-0016.pdf
- Constandt, B., Thibaut, E., De Bosscher, V., Scheerder, J., Ricour, M., & Willem, A. (2020). Exercising in times of lockdown: An analysis of the impact of COVID-19 on levels and patterns of exercise among adults in Belgium. International Journal of Environmental Research and Public Health, 17(11), 4144. https://doi.org/10.3390/ijerph17114144
- Dasso, N. A. (2019). How is exercise different from physical activity? A concept analysis. Nursing Forum, 54(1), 45–52. https://doi.org/10.1111/nuf.12296
- Davis, R., Campbell, R., Hildon, Z., Hobbs, L., & Michie, S. (2015). Theories of behaviour and behaviour change across the social and behavioural sciences: A scoping review. Health Psychology Review, 9(3), 323–344. https://doi.org/10.1080/17437199.2014.941722
- de Boer, W., Mierau, J. O., Schoemaker, J., Viluma, L., & Koning, R. H, Lifelines Corona Research Initiative. (2021). The impact of the Covid-19 crisis on socioeconomic differences in physical activity behavior: Evidence from the Lifelines COVID-19 cohort study. Preventive Medicine, 153, 106823. https://doi.org/10.1016/j.ypmed.2021.106823
- Dunton, G. F., Do, B., & Wang, S. D. (2020). Early effects of the COVID-19 pandemic on physical activity and sedentary behavior in children living in the U.S. BMC Public Health, 20(1), 1351. https://doi.org/10.1186/s12889-020-09429-3
- Flynn, D., Moloney, E., Bhattarai, N., Scott, J., Breckons, M., Avery, L., & Moy, N. (2020). COVID-19 pandemic in the United Kingdom. Health Policy and Technology, 9(4), 673–691. https://doi.org/10.1016/j.hlpt.2020.08.003
- Fung, M., & Babik, J. M. (2021). COVID-19 in immunocompromised hosts: What we know so far. Clinical Infectious Diseases, 72(2), 340–350. https://doi.org/10.1093/cid/ciaa863
- Gehlhar, A., Schmidt, N., Eisenburger, N., Feddern, S., Kossow, A., Nießen, J., Wessely, S., Wiesmüller, G. A., Grüne, B., Joisten, C., & CoCo, F. G. (2022). Impact of physical activity on COVID-19-related symptoms and perception of physical performance, fatigue and exhaustion during stay-at-home orders. BMJ Open Sport & Exercise Medicine, 8(2), e001319. https://doi.org/10.1136/bmjsem-2022-001319
- GOV.UK. (2019). Advancing our health: prevention in the 2020s. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/819766/advancing-our-health-prevention-in-the-2020s-accessible.pdf.
- Hashemzadeh, M., Rahimi, A., Zare-Farashbandi, F., Alavi-Naeini, A. M., & Daei, A. (2019). Transtheoretical model of health behavioral change: A systematic review. Iranian Journal of Nursing and Midwifery Research, 24(2), 83–90. https://doi.org/10.4103/ijnmr.IJNMR_94_17
- Howlett, N., Schulz, J., Trivedi, D., Troop, N., & Chater, A. (2019). A prospective study exploring the construct and predictive validity of the COM-B model for physical activity. Journal of Health Psychology, 24(10), 1378–1391. https://doi.org/10.1177/1359105317739098
- Jiménez-Zazo, F., Romero-Blanco, C., Castro-Lemus, N., Dorado-Suárez, A., & Aznar, S. (2020). Transtheoretical model for physical activity in older adults: Systematic review. International Journal of Environmental Research and Public Health, 17(24), 9262. https://doi.org/10.3390/ijerph17249262
- Kanavaki, A. M., Rushton, A., Efstathiou, N., Alrushud, A., Klocke, R., Abhishek, A., & Duda, J. L. (2017). Barriers and facilitators of physical activity in knee and hip osteoarthritis: A systematic review of qualitative evidence. BMJ Open, 7(12), e017042. https://doi.org/10.1136/bmjopen-2017-017042
- Kaur, H., Singh, T., Arya, Y. K., & Mittal, S. (2020). Physical fitness and exercise during the COVID-19 pandemic: A qualitative enquiry. Frontiers in Psychology, 11, 590172. https://doi.org/10.3389/fpsyg.2020.590172
- Kokkinos, P. (2012). Physical activity, health benefits, and mortality risk. ISRN Cardiology, 2012, 1–14. https://doi.org/10.5402/2012/718789
- Kwasnicka, D., Dombrowski, S. U., White, M., & Sniehotta, F. (2016). Theoretical explanations for maintenance of behaviour change: A systematic review of behaviour theories. Health Psychology Review, 10(3), 277–296. https://doi.org/10.1080/17437199.2016.1151372
- Laird, Y., Fawkner, S., & Niven, A. (2018). A grounded theory of how social support influences physical activity in adolescent girls. International Journal of Qualitative Studies on Health and Well-Being, 13(1), 1435099. https://doi.org/10.1080/17482631.2018.1435099
- Leung, L. (2015). Validity, reliability, and generalizability in qualitative research. Journal of Family Medicine and Primary Care, 4(3), 324–327. https://doi.org/10.4103/2249-4863.161306
- Liu, K. T., Kueh, Y. C., Arifin, W. N., Kim, Y., & Kuan, G. (2018). Application of transtheoretical model on behavioral changes, and amount of physical activity among university’s students. Frontiers in Psychology, 9, 2402. https://doi.org/10.3389/fpsyg.2018.02402
- Long, H. A., French, D. P., & Brooks, J. M. (2020). Optimising the value of the critical appraisal skills programme (CASP) tool for quality appraisal in qualitative evidence synthesis. Research Methods in Medicine & Health Sciences, 1(1), 31–42. https://doi.org/10.1177/2632084320947559
- Mahmood, F., Acharya, D., Kumar, K., & Paudyal, V. (2021). Impact of COVID-19 pandemic on ethnic minority communities: A qualitative study on the perspectives of ethnic minority community leaders. BMJ Open, 11(10), e050584. https://doi.org/10.1136/bmjopen-2021-050584
- Mbabazi, J., Kanmodi, K. K., Kunonga, E., Tolchard, B., & Nnyanzi, L. A. (2022a). Barriers and facilitators of physical activity. Journal of Health and Allied Sciences NU, 13(01), 019–027. https://doi.org/10.1055/s-0042-1753561
- Mbabazi, J., MacGregor, F., Salman, M., Breckon, J., Kunonga, E., Tolchard, B., & Nnyanzi, L. (2022b). Exploring the barriers and facilitators to making healthy physical activity lifestyle choices among UK BAME adults during covid-19 pandemic: A study protocol. International Journal of Physical Activity and Health, 1(3), 1–44. https://scholarworks.boisestate.edu/cgi/viewcontent.cgi?article=1025&context=ijpah https://doi.org/10.18122/ijpah.010303.boisestate
- McPhee, J. S., French, D. P., Jackson, D., Nazroo, J., Pendleton, N., & Degens, H. (2016). Physical activity in older age: Perspectives for healthy ageing and frailty. Biogerontology, 17(3), 567–580. https://doi.org/10.1007/s10522-016-9641-0
- Michie, S., van Stralen, M. M., & West, R. (2011). The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implementation Science, 6(1), 42. https://doi.org/10.1186/1748-5908-6-42
- Michie, S., & West, R. (2021). Sustained behavior change is key to preventing and tackling future pandemics. Nature Medicine, 27(5), 749–752. https://doi.org/10.1038/s41591-021-01345-2
- Munn, Z., Tufanaru, C., & Aromataris, E. (2014). JBI’s systematic reviews: Data extraction and synthesis. AJN, American Journal of Nursing, 114(7), 49–54. https://doi.org/10.1097/01.NAJ.0000451683.66447.89
- Murakami, M., Aoki, T., Sugiyama, Y., Takeuchi, M., Yui, T., Koyama, M., Ichikawa, Y., Yanagisawa, K., Furuhata, S., Ikezoe, M., Ota, T., & Matsushima, M. (2021). Association between the transtheoretical model approach and sustained intradialytic pedaling exercise: A retrospective cohort study. Medicine, 100(42), e27406. https://doi.org/10.1097/MD.0000000000027406
- Newbold, J. W., Rudnicka, A., & Cox, A. (2021). Staying active while staying home: The use of physical activity technologies during life disruptions. Frontiers in Digital Health, 3, 753115. https://doi.org/10.3389/fdgth.2021.753115
- Ng, S. W. K., Rouhani, F. J., Brunner, S. F., Brzozowska, N., Aitken, S. J., Yang, M., Abascal, F., Moore, L., Nikitopoulou, E., Chappell, L., Leongamornlert, D., Ivovic, A., Robinson, P., Butler, T., Sanders, M. A., Williams, N., Coorens, T. H. H., Teague, J., Raine, K., … Campbell, P. J. (2021). Convergent somatic mutations in metabolism genes in chronic liver disease. Nature, 598(7881), 473–478. https://doi.org/10.1038/s41586-021-03974-6
- Nicomedes, C., & Avila, R. (2020). An analysis on the panic during COVID-19 pandemic through an online form. Journal of Affective Disorders, 276, 14–22. https://doi.org/10.1016/j.jad.2020.06.046
- Office for National Statistics. (2020). Why have Black and South Asian people been hit hardest by COVID-19? Office for National Statistics. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/articl
- Otu, A., Ahinkorah, B. O., Ameyaw, E. K., Seidu, A. A., & Yaya, S. (2020). One country, two crises: What Covid-19 reveals about health inequalities among BAME communities in the United Kingdom and the sustainability of its health system? International Journal for Equity in Health, 19(1), 189. https://doi.org/10.1186/s12939-020-01307-z
- Paluch, A. E., Bajpai, S., Bassett, D. R., Carnethon, M. R., Ekelund, U., Evenson, K. R., Galuska, D. A., Jefferis, B. J., Kraus, W. E., Lee, I.-M., Matthews, C. E., Omura, J. D., Patel, A. V., Pieper, C. F., Rees-Punia, E., Dallmeier, D., Klenk, J., Whincup, P. H., Dooley, E. E., … Fulton, J. E, Steps for Health Collaborative. (2022). Daily steps and all-cause mortality: A meta-analysis of 15 international cohorts. Lancet Public Health, 7(3), e219–e228. https://doi.org/10.1016/S2468-2667(21)00302-9
- Pringle, A., Kime, N., Zwolinsky, S., Rutherford, Z., & Roscoe, C. (2022). An investigation into the physical activity experiences of people living with and beyond cancer during the COVID-19 pandemic. International Journal of Environmental Research and Public Health, 19(5), 2945. https://doi.org/10.3390/ijerph19052945
- Prochaska, J. O., & Velicer, W. F. (1997). The transtheoretical model of health behavior change. American Journal of Health Promotion, 12(1), 38–48. https://doi.org/10.4278/0890-1171-12.1.38
- Rajkumar, R. P. (2020). COVID-19 and mental health: A review of the existing literature. Asian Journal of Psychiatry, 52, 102066. https://doi.org/10.1016/j.ajp.2020.102066
- Romero-Blanco, C., Rodríguez-Almagro, J., Onieva-Zafra, M. D., Parra-Fernández, M. L., Prado-Laguna, M., & Hernández-Martínez, A. (2020). Physical activity and sedentary lifestyle in university students: Changes during confinement due to the COVID-19 pandemic. International Journal of Environmental Research and Public Health, 17(18), 6567. https://doi.org/10.3390/ijerph17186567
- Rosenkranz, R. R., Ridley, K., Guagliano, J. M., & Rosenkranz, S. K. (2021). Physical activity capability, opportunity, motivation and behavior in youth settings: Theoretical framework to guide physical activity leader interventions. International Review of Sport and Exercise Psychology, 16(1), 529–553. https://doi.org/10.1080/1750984X.2021.1904434
- Shah, V. K., Firmal, P., Alam, A., Ganguly, D., & Chattopadhyay, S. (2020). Overview of immune response during SARS-CoV-2 infection: Lessons from the past. Frontiers in Immunology, 11, 1949. https://doi.org/10.3389/fimmu.2020.01949
- Singh, S., Roy, D., Sinha, K., Parveen, S., Sharma, G., & Joshi, G. (2020). Impact of COVID-19 and lockdown on mental health of children and adolescents: A narrative review with recommendations. Psychiatry Research, 293, 113429. https://doi.org/10.1016/j.psychres.2020.113429
- Smith, V., Devane, D., Begley, C. M., & Clarke, M. (2011). Methodology in conducting a systematic review of systematic reviews of healthcare interventions. BMC Medical Research Methodology, 11(1), 15. https://doi.org/10.1186/1471-2288-11-15
- Smith, J. D., Fu, E., & Kobayashi, M. A. (2020). Prevention and management of childhood obesity and its psychological and health comorbidities. Annual Review of Clinical Psychology, 16(1), 351–378. https://doi.org/10.1146/annurev-clinpsy-100219-060201
- Spruit, M. A., Burtin, C., De Boever, P., Langer, D., Vogiatzis, I., Wouters, E. F., & Franssen, F. M. (2016). COPD and exercise: Does it make a difference? Breathe, 12(2), e38–e49. https://doi.org/10.1183/20734735.003916
- Stalsberg, R., & Pedersen, A. V. (2018). Are differences in physical activity across socioeconomic groups associated with choice of physical activity variables to report? International Journal of Environmental Research and Public Health, 15(5), 922. https://doi.org/10.3390/ijerph15050922
- Stockwell, S., Trott, M., Tully, M., Shin, J., Barnett, Y., Butler, L., McDermott, D., Schuch, F., & Smith, L. (2021). Changes in physical activity and sedentary behaviours from before to during the COVID-19 pandemic lockdown: A systematic review. BMJ Open Sport & Exercise Medicine, 7(1), e000960. https://doi.org/10.1136/bmjsem-2020-000960
- Stonerock, G. L., & Blumenthal, J. A. (2017). Role of counseling to promote adherence in healthy lifestyle medicine: Strategies to improve exercise adherence and enhance physical activity. Progress in Cardiovascular Diseases, 59(5), 455–462. https://doi.org/10.1016/j.pcad.2016.09.003
- Stults-Kolehmainen, M. A., & Sinha, R. (2014). The effects of stress on physical activity and exercise. Sports Medicine, 44(1), 81–121. https://doi.org/10.1007/s40279-013-0090-5
- Theis, N., Campbell, N., De Leeuw, J., Owen, M., & Schenke, K. C. (2021). The effects of COVID-19 restrictions on physical activity and mental health of children and young adults with physical and/or intellectual disabilities. Disability and Health Journal, 14(3), 101064. https://doi.org/10.1016/j.dhjo.2021.101064
- Thivel, D., Tremblay, A., Genin, P. M., Panahi, S., Rivière, D., & Duclos, M. (2018). Physical activity, inactivity, and sedentary behaviors: Definitions and implications in occupational health. Frontiers in Public Health, 6, 288. https://doi.org/10.3389/fpubh.2018.00288
- Timlin, D., McCormack, J. M., & Simpson, E. E. (2021). Using the COM-B model to identify barriers and facilitators towards adoption of a diet associated with cognitive function (MIND diet). Public Health Nutrition, 24(7), 1657–1670. https://doi.org/10.1017/S1368980020001445
- Vall-Roqué, H., Andrés, A., & Saldaña, C. (2021). The impact of COVID-19 lockdown on social network sites uses, body image disturbances and self-esteem among adolescent and young women. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 110, 110293. https://doi.org/10.1016/j.pnpbp.2021.110293
- Velten, J., Bieda, A., Scholten, S., Wannemüller, A., & Margraf, J. (2018). Lifestyle choices and mental health: A longitudinal survey with German and Chinese students. BMC Public Health, 18(1), 632. https://doi.org/10.1186/s12889-018-5526-2
- Wickersham, A., Sugg, H. V., Epstein, S., Stewart, R., Ford, T., & Downs, J. (2021). Systematic review and meta-analysis: The association between child and adolescent depression and later educational attainment. Journal of the American Academy of Child & Adolescent Psychiatry, 60(1), 105–118. https://www.sciencedirect.com/science/article/pii/S0890856720320499
- Williams, N. H., & Law, R. J. (2018). Putting function first: Redesigning the primary care management of long-term conditions. British Journal of General Practice, 68(673), 388–389. https://doi.org/10.3399/bjgp18X698249
- Williams, D. R., Priest, N., & Anderson, N. B. (2016). Understanding associations among race, socioeconomic status, and health: Patterns and prospects. Health Psychology, 35(4), 407–411. https://doi.org/10.1037/hea0000242
- Willmott, T. J., Pang, B., & Rundle-Thiele, S. (2021). Capability, opportunity, and motivation: An across contexts empirical examination of the COM-B model. BMC Public Health, 21(1), 1014. https://doi.org/10.1186/s12889-021-11019-w
- Withall, J., Jago, R., & Fox, K. R. (2011). Why some do but most don’t barriers and enablers to engaging low-income groups in physical activity programmes: A mixed methods study. BMC Public Health, 11(1), 507. https://doi.org/10.1186/1471-2458-11-507
- Wojtys, E. M. (2015). Keep on walking. Sports Health: A Multidisciplinary Approach, 7(4), 297–298. https://doi.org/10.1177/1941738115590392
- World Health Organisation. (2020). Physical activity. https://www.who.int/news-room/fact-sheets/detail/physical-activity.
- Wunsch, K., Kienberger, K., & Niessner, C. (2022). Changes in physical activity patterns due to the Covid-19 pandemic: A systematic review and meta-analysis. International Journal of Environmental Research and Public Health, 19(4), 2250. https://doi.org/10.3390/ijerph19042250