Abstract
Non-adherence to tuberculosis (TB) treatment poses a significant challenge, leading to multidrug-resistant TB and extensively drug-resistant TB. Addressing TB treatment non-adherence is crucial for curing individual patients, controlling TB spread, and reducing TB drug resistance. This study aimed to enhance TB treatment adherence through the application of the Behaviour Change Wheel. The BCW guide was followed to develop the intervention strategy for improving TB treatment adherence among patients. The process involved eight steps across three stages: understanding the behavior, identifying intervention options, and determining content and implementation options. Stage 1 data comprised 16 interviews with TB patients, three with TB district managers, eight with facility operation managers, eight with facility TB focal persons, and three focus group discussions with 18 direct observed treatment supporters. Findings from Stage 1 informed the intervention strategy development. A one-day stakeholder workshop, guided by Stages 2 and 3 of the BCW model, was conducted. The COM-B model analyzed results to identify necessary changes. The BCTv1 taxonomy helped select appropriate behavior change strategies for the intervention. The intervention strategy, named Adherence Improvement Management Strategy (AIMS), was developed through the stakeholder workshop, integrating insights from both approaches and guided by the last two stages of BCW. AIMS involves door-to-door campaigns by community health workers, distributing patient information leaflets to patients, communities, and family members. The BCW framework proved valuable in developing an intervention strategy to enhance TB treatment adherence among patients. Recent research indicates that AIMS is well-structured, patient-centered, coordinated, accessible, safe, and of high quality.
REVIEWING EDITOR:
1. Background
Treatment adherence remains the most underrated and understudied factor affecting the outcome of tuberculosis (TB) therapy. Adherence to treatment is challenging for many patients, given the complexity, modest tolerability, and long duration of TB treatment regimens currently available for both drug-susceptible and -resistant tuberculosis (TB). In turn, low adherence increases the risk of poor outcomes, including treatment failure, relapse, and development or amplification of drug resistance (Alexander et al., Citation2014). According to World Health Organisation (WHO) tuberculosis remains a global public health issue, and it is reportedly to cause illness for around 10 million people every year and has been ranked among the top ten causes of death globally (Alipanah et al., Citation2018). Poor adherence to medication is widely known as the major causative factor for increased risk of morbidity, mortality, and cost burden globally (Bandhu et al., Citation2024). A global meta-analysis conducted in 2018 showed that non-adherence to treatment is a risk factor for multi-drug resistant tuberculosis (MDR-TB) (Barker et al., Citation2016). Multi-drug resistant tuberculosis patients, as compared to drug-susceptible patients, they are found to have more frequently poor treatment outcomes (Barker et al., Citation2016). The factors that affect treatment adherence are divided into five different interacting dimensions, including socio-economic, health care system, condition, therapy, and patient factors. Although studies on adherence in other diseases than TB showed that interventions targeting these factors can significantly improve adherence rates, a better understanding of the effects of possible interventions in TB is required.
To address the issues around TB treatment non-adherence, the Behaviour Change Wheel (BCW) was chosen as the method for intervention development as it combines behaviour analysis with a systematic method to select specific target behaviours to promote effective behaviour change (Bérubé et al., Citation2015). The BCW is a comprehensive guide for developing behaviour change interventions. A model of health behaviour, known as COM-B, is at the fundamental of the BCW. The COM-B model predict that behaviour occurs as an interaction between three conditions: Capability (psychological or physical ability to perform the behaviour); Opportunity (physical and social environment that enables the behaviour); and Motivation (reflective and automatic mechanisms that activate or inhibit behaviour). The BCW also includes numerous intervention options and policy considerations, as outlined by the two outer rings of the wheel. The BCW has a three-stage process to intervention design: 1). Understand the behaviour, 2). Identify intervention options, and 3). Identify components and implementation options (Bérubé et al., Citation2015). Based on this model, the framework for this study was be developed on this three-stage process.
The BCW provides a pathway from the initial analysis of a target behaviour to selecting matching interventions that address identified barriers to performing the desired behaviour. The BCW has been implemented in several studies addressing behaviour change in health professionals (Casey et al., Citation2019; Chimeh et al., Citation2020; Colquhoun et al., Citation2017; Coulson et al., Citation2016). For example, research has explored the barriers and enablers to the delivery of the Healthy Kids Check in Australia (Casey et al., Citation2019), the early management of adults with traumatic spinal cord injury in Canada (Chimeh et al., Citation2020), medication management in multi-morbidity in the UK (Coulson et al., Citation2016), and mental healthcare capacity building in pharmacists in Canada (Colquhoun et al., Citation2017). The BCW has also been proposed as an appropriate model for hearing research (Michie et al., Citation2011). Barker, Atkins, and de Lusignan (Michie et al., Citation2013) were the first to implement the BCW in the field of audiology and designed an intervention to introduce support behaviours for consultations to improve hearing aid use among adults with hearing impairment. The researcher reviewed literature and the effectiveness of various interventions to improve treatment adherence among TB patients and decided to use Behaviour Change Wheel framework as a guide to develop effective intervention to improve TB treatment adherence as it was the aim of the current study.
This study was conducted to address the pervasive issue of tuberculosis (TB) treatment non-adherence, which significantly impacts the effectiveness of TB therapy and contributes to adverse health outcomes, including treatment failure, relapse, and the emergence of drug resistance. Despite the global health significance of TB and the availability of effective treatment regimens, adherence to these regimens remains a challenge for many patients due to various factors such as treatment complexity, long duration, and socioeconomic barriers.
Given the critical importance of adherence to TB treatment for both individual patient outcomes and public health goals, there is a pressing need to develop effective interventions to improve adherence rates.
By applying the BCW framework, the study sought to identify specific behaviors related to TB treatment adherence, understand the underlying determinants of these behaviors, and develop targeted interventions to address barriers and enhance adherence. Ultimately, the goal of this study was to contribute to improving TB treatment outcomes, reducing the burden of TB-related morbidity and mortality, and advancing progress towards global health goals, including those outlined in the Sustainable Development Goals (SDGs). The objective of this study is to develop intervention strategy to improve TB treatment adherence. This study aimed to fill this gap by utilizing the Behaviour Change Wheel (BCW) framework, which offers a systematic approach to understanding behavior and designing interventions to promote behavior change.
2. Methods
2.1. Overview
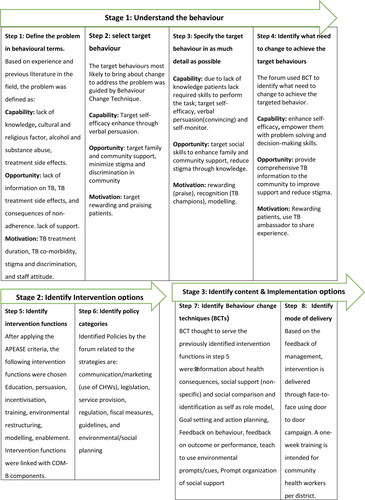
This manuscript describes the developmental process undertaken to enhance TB treatment adherence among TB patients through the application of the Behaviour Change Wheel. The BCW comprises three stages, delineated into eight steps as outlined by Michie et al. (Bérubé et al., Citation2015). The initial stage (Steps 1–4) focuses on ‘understanding the behaviour,’ incorporating the COM-B model in step 4 to delineate the behavioural factors influencing TB patients’ capability, opportunity, and motivation. The subsequent stage (Steps 5 and 6) involves ‘identifying intervention options,’ while the final stage (Steps 7 and 8) pertains to ‘identifying content and implementation options’ (Bérubé et al., Citation2015).
2.2. Study setting
This study took place in selected districts of Limpopo Province, the northernmost in South Africa. The province is predominantly rural, with a diverse population speaking Tshivenda, Xitsonga, and Sepedi. Healthcare facilities vary by district, with CHCs selected based on patient registration numbers. Districts such as Vhembe, Mopani, Sekhukhune, Capricorn, and Waterberg were chosen for their varied treatment success rates, reflecting local healthcare dynamics and community influences on health behaviors.
2.3. Study design
This study employed an exploratory qualitative approach to investigate factors contributing to TB treatment non-adherence. Following Creswell’s (2014) description of qualitative methods as involving rich, narrative-driven exploration with a flexible design, this study aimed to gather insights from stakeholders regarding reasons, opinions, and motivations behind TB treatment non-adherence.
Stakeholders included TB patients, district TB managers, facility operational managers, TB focal persons, and DOTS supporters from selected districts and community health centers (CHCs). A multistage sampling process involved purposive sampling of key informants for in-depth interviews and focus group discussions. TB patients above 18 years, interested in TB issues, and available during data collection were selected using maximum variation sampling. District TB managers, site TB focal persons, facility operational managers, and district DOTS supporters were sampled through non-probability convenience sampling.
A smaller sample size facilitated deep, case-oriented analysis. Key informant interviews included three district managers, eight TB focal persons, eight facility operational managers, and sixteen TB patients. Additionally, three focus group discussions one per district involved six DOTS supporters each, totalling 18 participants. Unstructured in-depth interview and focus group discussion guides collected participants’ socio-demographic information and perceptions on TB treatment adherence. Data, gathered through recorded interviews, discussions, and field notes, were transcribed verbatim and analyzed using Colaizzi’s (1978) seven-step method. Validation of findings was sought through participant feedback.
2.4. Development of intervention strategies
Findings were used as a basis to develop evidence-based intervention strategies to improve TB treatment adherence. A systematic literature review and a stakeholder workshop guided the development process, utilizing the Behaviour Change Wheel (BCW) and APEASE criteria to ensure feasibility and effectiveness. A one-day stakeholder workshop, guided by stages two and three of the BCW model, was conducted. The COM-B model facilitated analysis of the workshop results to identify areas requiring intervention (Michie et al., Citation2013). Additionally, the researcher utilized the taxonomy BCTv1 to pinpoint the most suitable strategies for fostering behaviour change within the intervention (Michie et al., Citation2011).
2.5. Ethical considerations
Ethics approval and consent to participate: The study was conducted according to the guidelines of the Declaration of Helsinki. The proposal was submitted and presented to the School of Health Science and the University Higher Degrees Committee (UHDC), and ethical clearance was granted by the University of Venda, Research Ethics Committee (approval number: SHS/19/PH/28/0411. Permission to conduct the study was obtained from the Limpopo Provincial Department of Health and Vhembe District, Waterberg District, and Capricorn District Department of Health. Furthermore, permission was obtained from the facilities’ operational managers.
Consent forms were given to every participant to complete. The nature of the research was described to the participants, and they were informed of their right to refuse to participate or to withdraw from participating if they felt unable to continue. Participants were also assured that the information they provided would not be used against them or shared with others, but would be reported as findings of the study.
Anonymity was ensured as participants did not write down their names or any personal identification, allowing their participation to remain anonymous. The researcher respected the choices and agreements made with the participants, and the initial agreement was not changed without their knowledge. Participants were not victimized for refusing to participate in the study.
3. Results
After data organization and analysis, five major themes were developed from the findings of this study and sub-themes were also formulated. Participants demographics are shown in annexture 1 below.
3.1. Theme 1: Social and cultural factors
The social and cultural context, including family, community, and household support, has a significant influence on treatment adherence for TB patients. This theme encompasses factors such as stigma, discrimination, and the impact of cultural, religious, and traditional beliefs on patients’ willingness to adhere to TB treatment. The sub-themes identified under this theme are:
Participant 2 said that: patients often believe TB is caused by witchcraft or supernatural forces, leading them to seek help from traditional healers and religious leaders instead of medical facilities.
3.2. Theme 2: Patients related factors
Patient-related factors significantly affect TB treatment adherence, with substance abuse and lack of understanding about the disease and its treatment being major issues. Frequent changes in residential address make it difficult for healthcare workers to track patients, while age, particularly among older individuals, influences adherence due to forgetfulness and negative attitudes. Addressing these factors through targeted education, substance abuse support, and improved communication can enhance treatment adherence and TB control efforts.
Participant 8 noted that; these patients are often drunk and spend most of their time at shebeens, neglecting their treatment. They forget their illness, making it difficult for home-based caregivers to reach them as they leave early and return late without communicating.
3.3. Theme 3: Treatment related factors
Participants expressed challenges with TB treatment adherence due to side effects, extended treatment duration, and comorbidities like HIV. Side effects, including nausea and fatigue, hindered daily activities, while doubts about treatment efficacy arose from prolonged regimens. Co-infected patients found managing multiple treatments overwhelming, leading to potential non-compliance.
Participant 10 added that; Patients report doing hard labor, feeling weak, tired, or in pain, and experiencing fever. They avoid seeking treatment to keep their jobs, as no one else can support their families, and reporting sick means no pay.
3.4. Theme 4: Socio-economic factors
The study identified socio-economic challenges such as unemployment, transport costs, and food insecurity as key barriers to TB treatment adherence. Patients faced difficulties accessing healthcare due to transportation constraints and experienced side effects exacerbated by inadequate nutrition during treatment. Addressing these barriers is crucial to improving TB treatment outcomes.
According to participant 2, a major challenge affecting TB treatment adherence is poverty. Many patients deliberately default on their treatment to continue receiving grants, fearing that getting better will terminate their support.
3.5. Theme 5: Healthcare and health system factors
The study identified healthcare system factors affecting TB treatment adherence, including issues with facility hours, long wait times, and medicine availability. Negative staff attitudes and a lack of DOTS supporters also hindered patient adherence, highlighting the need for patient-centered care and community support interventions to improve TB treatment outcomes. Policymakers and healthcare providers should address these challenges to enhance adherence and reduce TB transmission rates.
Participant 34 said the health center’s hours are a challenge for farm workers like themselves, as they work weekends and cannot visit the facilities. They cannot keep appointments because the centers close early, and they are unable to request time off without revealing personal health details.
The Overall results were aligned with all eight steps of Behaviour Change Wheel intervention design as shown on below.
3.6. Stage 1: understand the behaviour
3.6.1. Step 1: Define the problem to be addressed in behavioural terms
The challenge of non-adherence to TB treatment among patients is widely recognized, despite various influencing factors identified in existing literature. According to the Behavior Change Wheel (BCW) model, addressing this issue begins with clearly defining the specific behavioral problem (Michie et al., Citation2014). The COM-B (Capability, Opportunity, Motivation-Behavior) model was employed to pinpoint the problem and its components. Despite numerous factors affecting adherence, the study emphasized identifying a specific problem amenable to intervention through these components.
3.6.1.1. Capability
Regarding capability, issues such as insufficient disease knowledge, cultural beliefs, substance use, treatment side effects, and denial were identified in the study (Murphy et al., Citation2014). A notable finding was the knowledge gap in communities, leading patients to seek help from religious or traditional healers before health facilities, which contributes to higher TB transmission rates as seen on the identified themes.
3.6.1.2. Opportunity
Opportunity factors as seen on the themes include social influences like stigma and lack of social support, which hinder patients from disclosing their TB status and seeking appropriate care. Fear of discrimination plays a significant role here.
3.6.1.3. Motivation
Motivation, encompassing psychological processes influencing behavior, highlighted patients’ struggle with the long duration and side effects of treatment (Nezenega et al., Citation2020). From the themes identified, patients’ poor communication with healthcare providers emerged as a critical factor in treatment non-adherence.
3.6.2. Step 2: Select the target behaviours most likely to bring about change to address the problem
After delineating the problem, the next step was to select target behaviours likely to improve TB treatment adherence (Nezenega et al., Citation2020). Recognizing that behaviours exist within a broader system, the study aimed to understand the interplay of relevant behaviours affecting TB non-adherence. The research team used BCW criteria to assess each behaviour’s potential effectiveness and feasibility. This involved evaluating the anticipated impact, likelihood of change based on capability, opportunity, and motivation, potential spill-over effects, and ease of measurement. Behaviours were scored as highly promising, moderately promising, worth considering despite being unpromising, or unsuitable (NICE, Citation2014). The team independently assessed these criteria, resolving disagreements through consensus. The prioritization focused on ensuring TB patients receive comprehensive education and information about TB. The COM-B components were used to articulate the necessary changes to enhance TB treatment adherence in Limpopo province.
3.6.2.1. Capability
Emphasis was placed on improving patients’ self-efficacy and skills through methods like verbal persuasion, enhancing physical and emotional well-being, and promoting self-monitoring.
3.6.2.2. Opportunity
The study highlighted the importance of garnering family and community support and reducing stigma and discrimination within the community as crucial opportunities for behavior change.
3.6.2.3. Motivation
The research identified a lack of motivation among patients to adhere to TB treatment. Proposed strategies included implementing a system of rewards, such as praising adherence, providing reinforcement, and using modeling techniques involving TB ambassadors.
3.6.3. Step 3: Specify the target behaviour in as much detail as possible
The study aimed to specify target behaviours related to TB treatment adherence, detailing the individuals involved, timing, location, frequency, and accompanying persons (Pradipta et al., Citation2018). It employed the COM-B framework to define these behaviours precisely.
3.6.3.1. Capability
Patients often struggle with TB treatment adherence due to a lack of skills and knowledge. Improving self-efficacy through health education and social skills training is essential. Healthcare workers are vital in educating, encouraging, and addressing the physical and emotional well-being of patients.
3.6.3.2. Opportunity
Enhancing family and community support is crucial for TB patients. Many families lack the necessary knowledge about TB, hindering their ability to provide adequate support. Community education to reduce stigma is essential for creating a supportive environment.
3.6.3.3. Motivation
A major challenge is patients’ lack of motivation to adhere to TB treatment. The study recommended incentivizing adherence with rewards like praise and recognition. Sharing success stories and involving community figures as TB ambassadors can also inspire patients to stick to their treatment.
3.6.4. Step 4: Identify what needs to change in order to achieve the targeted behaviours?
This step assessed current activity levels among performers to understand factors influencing non-adherence to TB treatment. The target behavior focuses on enhancing self-efficacy, social skills, feelings towards behavior adoption, beliefs about others’ behavior, approval for behavior, clear goals, rewards, a positive behavior-related identity, and environmental changes. The feasibility of these behaviors was assessed, applying findings to the COM-B model (capability, opportunity, motivation), which interact and influence behavior engagement.
3.6.4.1. Capability
Emphasizes boosting self-efficacy, social skills, and changing risk perceptions related to TB treatment.
3.6.4.2. Opportunity
Involves altering environmental contexts and beliefs about the benefits and costs of adherence and addressing stigma through community engagement.
3.6.4.3. Motivation
Targets both automatic (habitual) and reflective (conscious) motivations, using strategies like goal setting, rewards, and role models to enhance adherence.
3.6.5. Step 5: Identify intervention functions
The research team identified relevant COM-B components and addressed barriers through specific intervention functions (Bérubé et al., Citation2015). They refined routine activities to enhance behavior change, focusing on education and skill-building. Intervention priorities were based on previous successes and the needs identified by TB district managers, emphasizing comprehensive health education. Nurses required standardized materials and regular training to manage heavy counselling loads. Patient-centred interventions supported healthcare providers in delivering thorough TB information and counselling. Strategies were aligned with BCW intervention functions and evaluated using APEASE criteria to optimize behavior change capabilities (Nezenega et al., Citation2020; ).
Table 1. Definitions of interventions functions.
3.6.6. Step 6: Identify policy categories
During strategy development process, the research team evaluated policy changes to facilitate behavioral change, aligning with intervention functions such as education, training, environmental restructuring, and incentivization. They used the APEASE criteria to categorize policies into communication/marketing, guidelines, fiscal measures, regulation, legislation, environmental/social planning, and service provision (Michie et al., Citation2014). The team selected relevant policy categories for each intervention function but excluded detailed discussion on policy categories supporting intervention delivery due to scope limitations. As a practical measure within their study’s purview, they intend to create patient information leaflets.
3.6.7. Step 7: Identify behavioural change techniques
The researcher identified several behavioral change techniques to enhance TB treatment adherence (Pradipta et al., Citation2018). These techniques, ranging from health education and peer support to goal setting and social support organization, were carefully chosen and aligned with intervention functions from the BCW framework as shown on below. They form a comprehensive strategy aimed at fostering consistent adherence to TB treatment protocols (Robertson & Jochelson, Citation2006).
Table 2. Identify behavioural change techniques.
3.6.8. 9 Suggested specific strategies to improve TB treatment adherence
The team explored various strategies to improve TB treatment adherence, with participants proposing several approaches. Consolidating these suggestions, key strategies included:
Providing thorough counselling and education about TB to patients and families.
Enhancing visibility of TB programs in communities to correct misconceptions.
Involving families, peers, and social networks in supporting TB patients and spreading health information.
Educating religious leaders and traditional healers to aid in patient referral.
Conducting door-to-door TB campaigns to raise awareness.
Using community TB ambassadors to identify potential cases.
Training healthcare workers to improve service quality and attitudes.
Implementing patient satisfaction surveys to gauge service effectiveness.
Following this, the team prioritized target behaviours using BCW criteria, considering feasibility, impact, and potential for change. In a stakeholder workshop, consensus focused on addressing knowledge gaps among TB patients and the community. The prioritization reaffirmed the importance of comprehensive counselling for TB patients and families, though concerns about nurse workload were noted. Future interventions should aim to ease this burden while maintaining high-quality patient care ().
Table 3. Linking COM-B components, factors influencing TB treatment non-adherence behaviour, intervention functions and specific intervention strategies suggested by participants.
3.6.9. Step 8: Identify mode of delivery
The BCW’s final step involved choosing how to deliver the intervention (Bérubé et al., Citation2015). By specifying techniques for TB treatment adherence, the team identified potential delivery modes (Sinnott et al., Citation2015). They opted for face-to-face interactions via a door-to-door campaign to reach TB patients, families, and communities, addressing widespread knowledge gaps.
This approach encourages patient engagement in health sessions and meets APEASE criteria. Face-to-face interaction supports real-time interpersonal communication, fostering behavior change. Patient information leaflets will accompany these sessions. To ensure effective implementation, community health workers will undergo comprehensive training per district, equipping them to engage patients successfully.
3.7. The intervention
The team developed the Adherence Improvement Management Strategy (AIMS) to enhance TB treatment adherence. AIMS incorporates study evidence, data analysis, and expert input to increase TB awareness among patients, families, and communities, aiming to reduce stigma and foster support. It focuses on improving TB understanding, promoting timely health-seeking behavior, encouraging patient status disclosure, and enhancing patient support. Designed with a patient-centered approach, AIMS ensures comprehensive care through coordinated delivery by community health workers distributing patient information leaflets. The strategy includes four key components aligned with the chosen BCT for this study.
3.7.1. Enhance TB knowledge and adherence
The study identifies knowledge gaps among TB patients regarding transmission, prevention, and treatment adherence. To address this, a patient information leaflet has been created for use by community health workers during door-to-door campaigns. These campaigns will educate registered patients and families on TB, covering transmission, prevention, diagnosis, treatment, and adherence, incorporating strategies like providing health information and setting goals.
3.7.2. Encourage timely health-seeking behavior
Early TB diagnosis is crucial for effective treatment and community health. The study promotes messages to encourage prompt health-seeking behavior within affected communities, aiming to reduce transmission and improve health outcomes. Community and family involvement is pivotal, supported by strategies like informing about health consequences.
3.7.3. Facilitate patient status disclosure
Many TB patients hesitate to disclose their status due to stigma. Addressing this involves providing accurate information and support to patients and communities to combat stigma and foster support networks. Strategies include social support and role modeling to create a supportive environment.
3.7.4. Promote patient support
Support throughout the treatment journey is vital for TB patients’ adherence and outcomes. The study emphasizes the role of family and community in providing support, including supervised treatment. Strategies include organizing social support and providing feedback to enhance adherence and outcomes.
4. Discussion
This study uses the BCW model to develop intervention strategy to improve TB treatment adherence among TB patients. The research team has identified the risk of their academic limitations from the beginning, which informed their decision to use the BCW due to its basic and stepwise guidance. Even though the team has also discovered that BCW has a very exciting challenge. Systematically following all steps was difficult and time-consuming, but it ensured consideration of all components of effective behaviour change (Williams & French, Citation2011). The period from the start of the intervention design process to the point of developing and intervention strategy takes a long time since there are stakeholders who must be engaged in each process and also workshop that have to be organized for stakeholders to review the developed strategy. In addition, the framework provides the impression that the development process is a linear, stepwise process. However, the research team found that there were times across the process, particularly in Phase 1, where it was necessary to look back to a previous step and further specify actions within that step before moving forward again. There were also some steps in the BCW that relied completely on decisions of the research team through workshop engagement, and these steps thus seemed more subjective than other steps in the process. This is a challenge that has been noted by other research teams developing healthcare interventions (World Health Organization, Citation2018).
As team progressed through the BCW stages, they found that defining the target was a great benefit as it helped them to stay focused on changing the behaviour of TB patients. A major strength of the BCW model was that it encouraged the research team to specify the target behaviours for change into simpler and more focused behaviours rather than attempting to change too many or too complex behaviours at once. The team also consulted literature for proper guidance as they proceed through stages. The team designed adherence improvement management strategy (AIMS) following the steps of the BCW with the aim to improve TB treatment adherence among TB patients. The adherence improvement management strategy is patient centered and it encourages behaviour of TB patient in order to improve knowledge about TB and TB treatment, promote timely health seeking behaviour, improve patient status discloser and promote patient support. One week training was proposed to be offered to all community health workers including TB staff per district, in order for them to understand the components of the AIMS.
5. Conclusion
Intervention strategies for improving TB treatment adherence were developed using the Behavior Change Wheel framework, which guided the intervention’s design based on the COM-B model (capability, opportunity, motivation, and behavior). This systematic approach ensured that the intervention addressed factors influencing TB treatment non-adherence behavior identified through analysis.
The resulting intervention, known as AIMS, focuses on four core components: enhancing TB and treatment knowledge, promoting timely healthcare seeking, encouraging patient disclosure, and fostering patient support. AIMS aims to deliver comprehensive, patient-centered care through a structured approach facilitated by community health workers. They will engage in door-to-door campaigns using patient information leaflets to educate TB patients, their families, and the community at large.
Community health workers will compile a registry of TB patients, arrange appointments, and provide ongoing support through counseling and monitoring. This proactive approach aims to reduce missed follow-up visits and decrease treatment default rates, ultimately lowering TB-related mortality.
6. Strengths and challenges of the BCW model
The research team found strengths and challenges in using the BCW for the development of the intervention. The major strength of the BCW model is that it encouraged a high level of involvement with stakeholders across the intervention development process, which was highly valuable for successful behaviour change.
One challenge of using the model was that the BCW process was time-consuming and labor intensive in completing the specified worksheets for each step. While the use of the APEASE criteria were helpful in reducing some subjectivity, the process involved forecasting by the research team and stakeholders and this forecasting may not always be accurate.
Author contributions
HM contributed to the concept, data collection, data analysis, data interpretation and drafting the manuscript. HM contributed to the concept and manuscript review. HM contributed to the concept and manuscript review. HM and TGT contributed to data analysis, data interpretation and manuscript review. HM contributed to the concept, data analysis, data interpretation and manuscript review. All authors reviewed and approved the final version of the manuscript.
Consent for publication
Not applicable.
COVER LETTER.docx
Download MS Word (12.5 KB)Acknowledgments
The authors wish to thank his PhD mentors Prof T.G Tshitangano, Prof T.X Maluleke, the University of Venda Higher Degrees’ Committee, the University of Venda Research and Ethics Committee, the Department of Health, Limpopo Province, and the Managers of the selected CHCs for granting the permission to conduct the study. The participants are also thanked for their consent to be part of the study. The supervisors are thanked for their tireless efforts and guidance.
Availability of data and materials
The datasets during and/or analysed during the current study are not publicly available due as the researcher strictly agreed with Provincial Department of Health and participants that data will not be for public use as the study involved district managers and facility managers. However, only analysed data are only available from the corresponding author on reasonable request.
Disclosure statement
The authors declare no conflict of interest.
Additional information
Funding
Notes on contributors
Hulisani Matakanye
Dr. Hulisani Matakanye is a distinguished scholar in the field of public health, holding a Ph.D. in Public Health. As a Senior Lecturer at the University of South Africa, Dr. Matakanye brings a wealth of knowledge, expertise, and passion for advancing public health research and education. With a focus on improving healthcare outcomes and addressing pressing public health challenges, Dr. Matakanye has dedicated their academic career to conducting impactful research and imparting knowledge to the next generation of health professionals. Their research interests encompass areas such as health behavior change, intervention development, and strategies to enhance healthcare adherence. Dr. Matakanye’s academic contributions extend beyond research, as they actively engage in teaching and mentoring students. Through their role as a Senior Lecturer, they play a pivotal role in shaping the academic and professional development of students pursuing studies in public health. Known for their commitment to excellence and innovation in public health, Dr. Matakanye continues to contribute significantly to the academic community and the broader field of public health through research, publications, and academic leadership.
Takalani Grace Tshitangano
Prof. Takalani Grace Tshitangano is an academic mid-level researcher, who holds a Ph.D degree, MBA, and MPH from South African universities. She is a professor of Public health (health promotion). She has graduated with more than thirty-four MPH and 8 PhD students. She has published more than seventy articles in peer-reviewed journals.
References
- Alexander, K. E., Brijnath, B., & Mazza, D. (2014). Barriers and enablers to delivery of the Healthy Kids Check: An analysis informed by the Theoretical Domains Framework and COM-B model. Implementation Science: IS, 9(1), 60. https://doi.org/10.1186/1748-5908-9-60
- Alipanah, N., Jarlsberg, L., Miller, C., Linh, N. N., Falzon, D., Jaramillo, E., & Nahid, P. (2018). Adherence interventions and outcomes of tuberculosis treatment: A systematic review and meta-analysis of trials and observational studies. PLoS Medicine, 15(7), e1002595. https://doi.org/10.1371/journal.pmed.1002595
- Bandhu, D., Murali Mohan, M., Nittala, N. A. P., Jadhav, P., Bhadauria, A., & Saxena, K. K. (2024). Theories of motivation: A comprehensive analysis of human behavior drivers. Acta Psychologica, 244, 104177. https://doi.org/10.1016/j.actpsy.2024.104177
- Barker, F., Atkins, L., & de Lusignan, S. (2016). Applying the COM-B behaviour model and behaviour change wheel to develop an intervention to improve hearing-aid use in adult auditory rehabilitation. International Journal of Audiology, 55 (sup3), S90–S98. https://doi.org/10.3109/14992027.2015.1120894
- Bérubé, M., Albert, M., Chauny, J.-M., Contandriopoulos, D., DuSablon, A., Lacroix, S., Gagné, A., Laflamme, É., Boutin, N., Delisle, S., Pauzé, A.-M., & MacThiong, J.-M. (2015). Development of theory-based knowledge translation interventions to facilitate the implementation of evidence-based guidelines on the early management of adults with traumatic spinal cord injury. Journal of Evaluation in Clinical Practice, 21(6), 1157–1168. https://doi.org/10.1111/jep.12342
- Casey, B., Coote, S., & Byrne, M. (2019). Activity matters: A web-based resource to enable people with multiple sclerosis to become more active. Translational Behavioral Medicine, 9(1), 120–128. https://doi.org/10.1093/tbm/iby028
- Chimeh, R. A., Gafar, F., Pradipta, I. S., Akkerman, O. W., Hak, E., Alffenaar, J. C., & van Boven, J. F. M. (2020). Clinical and economic impact of medication non-adherence in drug-susceptible tuberculosis: A systematic review. The International Journal of Tuberculosis and Lung Disease: The Official Journal of the International Union against Tuberculosis and Lung Disease, 24(8), 811–819. https://doi.org/10.5588/ijtld.19.0754
- Colquhoun, H. L., Squires, J. E., Kolehmainen, N., Fraser, C., & Grimshaw, J. M. (2017). Methods for designing interventions to change healthcare professionals’ behaviour: A systematic review. Implementation Science: IS, 12(1), 30. https://doi.org/10.1186/s13012-017-0560-5
- Coulson, N. S., Ferguson, M. A., Henshaw, H., & Heffernan, E. (2016). Applying theories of health behaviour and change to hearing health research: Time for a new approach. International Journal of Audiology, 55 (sup3), S99–S104. https://doi.org/10.3109/14992027.2016.1161851
- Michie, S., Abraham, C., Eccles, M. P., Francis, J. J., Hardeman, W., & Johnston, M. (2011). Strengthening evaluation and implementation by specifying components of behaviour change interventions: A study protocol. Implementation Science, 6(1), 2011. https://doi.org/10.1186/1748-5908-6-10
- Michie, S., Atkins, L., & West, R. (2014). The Behaviour Change Wheel book – A guide to designing interventions (p. 199). Retrieved from http://www.behaviourchangewheel.com/.
- Michie, S., Richardson, M., Johnston, M., Abraham, C., Francis, J., Hardeman, W., Eccles, M. P., Cane, J., & Wood, C. E. (2013). The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Annals of Behavioral Medicine: A Publication of the Society of Behavioral Medicine, 46(1), 81–95. https://doi.org/10.1007/s12160-013-9486-6
- Michie, S., van Stralen, M. M., & West, R. (2011). The Behaviour Change Wheel: a new method for characterising and designing behaviour change interventions. Implementation Science: IS, 6(1), 42. https://doi.org/10.1186/1748-5908-6-42
- Murphy, A. L., Gardner, D. M., Kutcher, S. P., & Martin-Misener, R. (2014). A theory-informed approach to mental health care capacity building for pharmacists. International Journal of Mental Health Systems, 8(1), 46. https://doi.org/10.1186/1752-4458-8-46
- Nezenega, Z. S., Perimal-Lewis, L., & Maeder, A. J. (2020). Factors influencing patient adherence to tuberculosis treatment in Ethiopia: A literature review. International Journal of Environmental Research and Public Health, 17(15), 5626. https://doi.org/10.3390/ijerph17155626
- NICE. (2014). Behaviour change: Individual approaches | guidance and guidelines | NICE. Natl Inst Heal Care Excell. 2014:49. Retrieved from https://www.nice.org.uk/guidance/ph49.
- Pradipta, I. S., Forsman, L. D., Bruchfeld, J., Hak, E., & Alffenaar, J. W. (2018). Risk factors of multidrug-resistant tuberculosis: A global systematic review and meta-analysis. The Journal of Infection, 77(6), 469–478. https://doi.org/10.1016/j.jinf.2018.10.004
- Robertson, R., & Jochelson, K. (2006). Interventions that change clinician behaviour: Mapping the literature. King’s Fund. https://www.nice.org.uk/media/default/about/what-we-do/into-practice/support-for-service-improvement-and-audit/kings-fund-literature-review.pdf
- Sinnott, C., Mercer, S. W., Payne, R. A., Duerden, M., Bradley, C. P., & Byrne, M. (2015). Improving medication management in multimorbidity: Development of the MultimorbiditY Collaborative Medication Review and Decision Making (MY COMRADE) intervention using the Behaviour Change Wheel. Implementation Science: IS, 10(1), 132. https://doi.org/10.1186/s13012-015-0322-1
- Williams, S. L., & French, D. P. (2011). What are the most effective intervention techniques for changing physical activity self-efficacy and physical activity behaviour - and are they the same? Health Education Research, 26(2), 308–322. https://doi.org/10.1093/her/cyr005
- World Health Organization. (2018). Global tuberculosis report WHO 2018. WHO Report 69.