ABSTRACT
It is not yet understood whether, and to what extent, craniosynostosis impacts the development of Attention Deficit/Hyperactivity Disorder (ADHD). This PRISMA compliant and PROSPERO pre-registered (ID: CRD42023458640) systematic review and meta-analysis examines the association of single-suture, non-syndromic craniosynostosis with ADHD and inattention/hyperactivity symptoms. Data from 17 independent studies (Nparticipants = 2,389; Mage = 7.3 years) were analyzed, taking into consideration suture location, surgical status, age, and measures administered, where feasible. Few differences were found between cases and controls, but some studies reported high symptom levels. Additional research is required utilizing larger sample sizes and more comprehensive assessment of ADHD.
Introduction
Single-suture craniosynostosis is characterized by the early fusion of a single cranial suture (sagittal, metopic, unicoronal, or lambdoid) with the resultant skull shape corresponding to the location of the fused suture (Speltz et al., Citation2004). Cranial sutures are dense fibrous joints found between two cranial bones that allow the skull to expand, accommodating for periods of rapid brain growth (Kajdic et al., Citation2018). These sutures typically fuse during early adulthood with the exception of the metopic suture, which generally fuses in early infancy (Betances et al., Citation2020). The prevalence of single suture craniosynostosis is increasing globally, with rates varying between 3 and 8 in every 10,000 live births and a male to female ratio of ~2:1 (Cornelissen et al., Citation2016; DiRocco et al., Citation2009; Lee et al., Citation2012; Tarnow et al., Citation2022). Up to 85% of craniosynostosis cases are classified as single-suture and non-syndromic, with the remaining cases syndromic and characterized by premature fusion of one or more cranial sutures, combined with specific, clinically recognized syndromes such as Pfeiffer or Apert syndrome (Derderian & Seaward, Citation2012; Speltz et al., Citation2004).
A range of mechanisms have been suggested to cause craniosynostosis including various genetic (e.g., single-gene mutations and chromosomal structural aberrations) and environmental risk factors (e.g., fetal head restraint and maternal thyroid dysfunction) (Brooks et al., Citation2018; Tahiri et al., Citation2017). However, the etiology of craniosynostosis is still poorly understood and likely to involve a complex interplay of multiple factors (Gaillard et al., Citation2024).
Common craniosynostosis neurodevelopmental outcomes include increased behavioral issues (e.g., conduct problems) and decreased cognitive functioning (e.g. executive functioning). Nonetheless, only small negative effects are often found, with test scores still within the “normal” range, and results not differing significantly to peers (Osborn et al., Citation2021, Citation2023). Recent research however, has highlighted a pathophysiological difference in individuals with craniosynostosis compared with controls, with smaller volumes of white matter – which directly affect learning and brain function – found in individuals with metopic synostosis, thereby possibly influencing their cognitive functioning and behavior (Gaillard et al., Citation2024).
ADHD is a neurodevelopmental disorder which is characterized by ongoing changes in attention, hyperactivity, and impulsivity (Krieger et al., Citation2020). A formal diagnosis of ADHD requires a multi-factorial assessment process, encompassing multiple areas of an individual’s life and a broad range of feedback from parents, teachers, and caregivers. Clinical judgment is required in order to ensure that the child’s presentation cannot be accounted for by another condition, such as Post-Traumatic Stress Disorder which can also present with attention and hyperactivity difficulties (Martínez et al., Citation2016), and that the developmental stage of the child is considered. Often however, these comprehensive assessments are difficult, and expensive, for families to access. In contrast, screening measures that determine the possibility of a child’s difficulties being associated with ADHD are generally more accessible. This may involve assessments such as cognitive testing or parent-rated questionnaires that assess a child’s levels of attentional functioning and/or hyperactivity symptoms.
A formal diagnosis of ADHD, using the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), requires that the child be present with, for at least six months, persistent patterns of six or more symptoms in two categories: inattention, and hyperactivity/impulsivity (American Psychiatric Association, Citation2013). When diagnosing ADHD using the International Statistical Classification of Diseases and Related Health Problems (ICD-11) (World Health Organization WHO, Citation2019/2021), the same time frames are present as seen in the DSM-5, however, only persistent patterns of either inattention or hyperactivity/impulsivity must be present. While there is some variation between the diagnostic criteria for ADHD in the DSM-5 and ICD-11, the same assessment categories of inattention and hyperactivity/impulsivity are maintained, with similar descriptions of symptomology. Symptoms characterizing inattention include difficulty with sustained attention, frequent daydreaming, and consistent forgetfulness (American Psychiatric Association, Citation2013; World Health Organization (World Health Organization WHO, Citation2019/2021). Whereas hyperactive symptoms involve difficulties controlling vocal volume, excessive speech, and frequent fidgeting and movement (American Psychiatric Association, Citation2013; World Health Organization (WHO), Citation2019/2021).
A recent umbrella meta-analysis reported global prevalence rates of ADHD in children and adolescents from the general community at 8.0% - encompassing 588 included studies (across 13 meta-analyses) with a male-to-female ratio of 2:1 and higher prevalence seen in children (Ayano et al., Citation2023). Moreover, the prevalence of ADHD is increasing and while the reason for the increase is not entirely clear there are some factors understood to be instrumental (Ayano et al., Citation2023). For example, as revisions are made to ADHD diagnostic criteria, the validity and reliability of ADHD diagnostic tools increases (Leffa et al., Citation2022). This change in criterion improves the accuracy of a diagnostic tool to better represent a wider range of individuals, increasing the number of individuals meeting the diagnostic criteria (Kessi et al., Citation2022). As the prevalence of ADHD diagnoses increase so do the number of clinics offering assessment, enhancing accessibility to assessment and therefore number of diagnoses (Thomas et al., Citation2015). Further, genetic factors are recognized to be instrumental to the increasing prevalence of ADHD. Heritability of ADHD is estimated to be as high as 80%, with some researchers suggesting that ADHD may become more prominent as generations progress (Kessi et al., Citation2022).
Global prevalence rates of attention problems and hyperactivity symptoms are not as widely available, however prevalence data in smaller samples are available. In primary care settings 16% of individuals aged 6–10 years exhibited clinically significant levels of attention difficulties (Spencer et al., Citation2018). In normative data, clinically significant symptoms of hyperactivity were observed in up to 9% of individuals aged 12–17 years (Vugteveen et al., Citation2022). These data show that inattention and hyperactivity are common in general and primary care populations, and as both outcomes are considered potential indicators of ADHD, they should be also be considered when assessing the relationship between ADHD and craniosynostosis (Spencer et al., Citation2018). Understanding differences across study findings is complicated by the fact that attention and hyperactivity assessments may involve objective (e.g., cognitive tests) or subjective (e.g., parent- or self-report questionnaires) measures, with results often differing according to the type of method used (Silk, Citation2012).
It is still unclear as to what the pathogenesis and etiology of ADHD are, however, gene environment interactions are thought to contribute to its development (Li et al., Citation2019). Genetic factors include alterations in dopaminergic pathways, and polymorphisms in genes responsible for encoding dopamine receptors (Kian et al., Citation2022). Environmental factors include prenatal stress and anxiety, exposure to certain environmental toxins (e.g., manganese) and food additives/sugars (Palladino et al., Citation2019).
A recent study using the Behavior Rating Inventory of Executive Function to screen for ADHD, found high levels (18%) of “likely” ADHD in individuals with sagittal synostosis (Osborn et al., Citation2023); however, it is unclear whether this rate is unusual given the paucity of information about ADHD levels (diagnosed or screened) in children with craniosynostosis. Furthermore, while inattention is a requirement of an ADHD diagnosis, findings in regard to attention levels in children with craniosynostosis are mixed. Significant differences between cases and controls on cognitive measures have been found (Osborn et al., Citation2021), whereas other studies have reported no differences (Collett et al., Citation2017). Parental reports of the prevalence of attention problems have nonetheless been high (33%; Almeida et al., Citation2021). Hyperactivity is another symptom that may indicate a child has ADHD. An example of the potential relationship between hyperactivity and craniosynostosis can be seen in two studies assessing developmental outcomes in 5-year-old children (Nparticipants = 80) with sagittal or metopic synostosis (Care, Horton, et al., Citation2019; Edwards-Bailey et al., Citation2023). These children were found to exhibit high levels of hyperactivity when compared to standardized test norms. Similarly, high levels of hyperactivity were observed in 54 7-year-old children with metopic synostosis (Qi et al., Citation2023).
While increased levels of inattention and hyperactivity are found in individuals with craniosynostosis, it is not yet clear if, and to what extent, craniosynostosis impacts the development of ADHD or ADHD symptomology (inattention, hyperactivity). Therefore, the current paper aims to systematically review and meta-analyze ADHD (screened, diagnosed) and ADHD symptomology (inattention, hyperactivity) in individuals with single-suture, non-syndromic craniosynostosis. Further, this review explores, where feasible, whether craniosynostosis type (sagittal, metopic, lambdoid, unicoronal), age (infant 0 - ≤1 yrs, preschool ≥ 2–4 yrs, primary ≥ 5–11 yrs, secondary school ≥ 12–17 yrs, adult ≥18 yrs) and subjective (e.g., parent reported questionnaires) or objective measures (e.g., cognitive testing) impacts this relationship. Narrowing in on a specific craniosynostosis type provides information about which suture locations may be more impacted, and broadening outcomes from just ADHD diagnoses, to screened ADHD and symptomology, provides information on populations who may be affected by ADHD symptomology but have not yet undergone ADHD assessment.
Methodology
Literature search
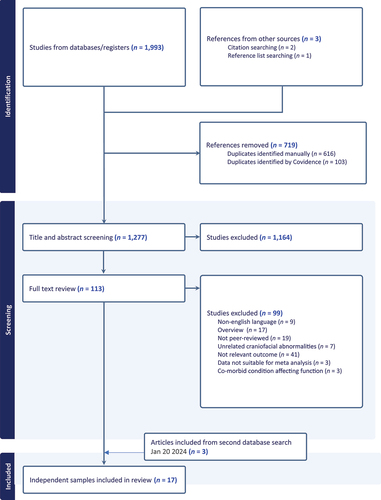
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Page et al., Citation2020) were used in the design and reporting of this systematic review and meta-analysis. The review protocol was preregistered with PROSPERO (CRD42023458640).
A comprehensive online search of PubMed, Scopus, EMBASE, and PsycINFO was conducted under the guidance of an expert research librarian with the purpose of identifying eligible articles which examined the prevalence of ADHD (diagnosed and/or screened), and/or ADHD symptomology (inattention, hyperactivity) in individuals diagnosed with single-suture, non-syndromic craniosynostosis; no additional filters or limitations were applied. The initial search was conducted on April 3, 2023 (see Supplementary Table S1 for detailed logic grids tailored to each database). A date-limited update, utilizing the same parameters and iterative process as the initial search, was undertaken on January 20, 2024. Reference lists of included studies were manually searched, and Scopus citation searches performed in order to identify additional relevant articles.
Study selection
The initial database search identified 1,993 articles, decreasing to 1,274 when duplicates were removed. Covidence systematic review software (Veritas Health Innovation, Melbourne, Australia, www.covidence.org) was used in order to independently co-screen (O.L., research assistant), each paper’s eligibility according to the study’s inclusion and exclusion criteria, which reduced the number of articles to 113. Full-text versions of the articles were obtained, and the eligibility criteria were once again applied by two researchers (O.L., research assistant), resulting in 17 independent samples that could be analyzed. A second search on January 20, 2024 identified 3 additional articles (refer to for a summary of the search process).
For a study to be included in the current meta-analysis, it had to meet the following criteria (a) it examined diagnoses of ADHD, screened for ADHD, or assessed attention or hyperactivity following a diagnosis of single-suture non-syndromic craniosynostosis (sagittal, metopic, unicoronal, lambdoid); (b) data were provided for a craniosynostosis sample (single group) or both a craniosynostosis and control group (two groups); (c) the article was reported in a journal in English, (d) the sample size was >1 (excludes case studies), and (e) data were reported in a way that enabled calculation of an effect size (e.g., M, SD, prevalence).
Studies were excluded if they (a) were reviews or secondary analyses; (b) had not undergone peer review (e.g., dissertations); (c) involved samples that included other conditions known to affect functioning (>10% of the sample); and (d) had identified participants for inclusion due to having cognitive or behavioral problems.
Data were manually co-extracted from papers by two independent authors (A.O., O.L.). Demographic data encompassed age, sex, and socioeconomic status. Clinical information included craniosynostosis suture location, surgical status, family history of craniosynostosis, and family history of ADHD. Study characteristics included sample size, country of origin, recruitment source, and study design. Outcome data incorporated results from parent-report, self-report, and teacher-report questionnaires in addition to clinician-administered measures of attention, hyperactivity, ADHD screening measures, and diagnoses of ADHD.
Data extracted were statistics necessary for calculating an overall effect size: mean, standard deviation (SD), and event rates. Outcomes were grouped by ADHD diagnosis, ADHD screening, attention, and hyperactivity. Additionally, where data were sufficient, outcomes were grouped and analyzed according to craniosynostosis suture location (sagittal, metopic, unicoronal, lambdoid), surgical status (post-surgery, conservatively managed) mean age (infant 0–≤1 yrs, preschool ≥ 2–4 yrs, primary ≥ 5–11 yrs, secondary school ≥ 12–17 yrs, adult ≥ 18 yrs) and objective or subjective measures. When it was not possible to identify specific categories, findings were reported as “combined.”
Data preparation
In order to maintain consistency, all age statistics were converted from months to years. One study reported diagnoses of Attention Deficit Disorder (ADD) (Kapp-Simon, Citation1998) and was combined with studies reporting diagnoses of ADHD. Overlapping samples were combined and treated as non-independent: (a) two papers from the US-based Infant Learning Project (Collett et al., Citation2017; Kapp-Simon et al., Citation2012); (b) three papers examining metopic synostosis from the Craniofacial Collaboration UK study (Culshaw et al., Citation2022; Edwards-Bailey et al., Citation2023, Citation2024) and c) four papers published by a Swedish research group (Kljajic et al., Citation2021; Kljajić et al., Citation2019, Citation2020, Citation2023). A reference list of included studies is provided in Supplementary Table S2, with overlapping samples marked as (a), (b) and (c) as per above.
Statistical analysis and interpretation
The outcomes analyzed in the current paper were diagnosed ADHD, screened ADHD, or ADHD symptomology (inattention, hyperactivity) with data from included studies analyzed using Comprehensive Meta-Analysis Software version 4 (Borenstein et al., Citation2022). The number of children scoring in the “high” or “very high” categories, as per a given measure’s cutoff threshold, was used to determine the proportion of children experiencing problems with attention or hyperactivity.
In papers with a single group (i.e., craniosynostosis group only) the prevalence of problems was reported. In papers that incorporated controls (i.e., craniosynostosis group + control group), data were analyzed in two ways. First, we calculated odds ratios (OR) in order to determine the likelihood of ADHD diagnoses and/or symptom occurrence in the craniosynostosis group, compared with individuals in the comparison group. ORs > 1 indicate more problems in the craniosynostosis group, while ORs < 1 indicate they have fewer problems, compared to controls. Small, medium and large effects were reported based on OR = 1.68, 3.47 and 6.71, respectively (Chen et al., Citation2010). Second, where mean, standard deviation (SD) and sample size data were provided, Hedges’ g (g) was used to measure the standardized mean difference between craniosynostosis groups and control groups, with g = 0.2, 0.5, and 0.8 equating to small, medium, and large effects, respectively (Cohen, Citation1992). Studies that compared M/SD data of those with craniosynostosis to normative data, and not a recruited control group, were not included in the current study. It is being increasingly recognized that factors such as the Flynn effect (i.e., increasing IQ in general populations) and selection bias (i.e., study participants are not representative of the general population) limits the utility and generalizability of subsequent findings (Long et al., Citation2022).
Random effects models were applied with the assumption that the true effect was similar but not identical across individual studies (Borenstein et al., Citation2010). In all analyses containing two or more studies Q-values were calculated to explain between-study heterogeneity (Borenstein et al., Citation2017). Orwin’s Fail Safe N (Nfs) statistics were calculated for analyses including three or more studies for the purpose of addressing publication bias caused by the tendency for journals to favor statistically significant results, with smaller Nfs indicating potential susceptibility to publication bias (Orwin, Citation1983). Mean effect sizes were calculated with 95% confidence intervals (95% CIs) to determine the precision of each effect. Probability values (p) were used to assess statistical significance. I-squared statistics (I2) were calculated to explain what percentage of the variance in observed effects reflected the variance in true effects rather than sampling error (Borenstein et al., Citation2017). Tau-squared (τ2) was used to explain the variance of true effect size (logit units).
A risk of bias assessment was conducted using two adapted National Heart, Lung, and Blood Institute Quality Assessment Tools (NHLBI; Maryland, United States, www.nhlbi.nih.gov) Observational Cohort and Cross-Sectional Studies (OC-CS), and Case-Control Studies (CCS), in order to assess all included studies for potential methodological bias. Each criterion was assessed (yes, no, not reported, not applicable), and the percentage of papers which met each criterion was calculated.
Results
Study characteristics
Overall, data for 2,389 participants were analyzed. Of the 17 independent studies included, the majority originated from Europe (Nstudies = 9), followed by the United States (Nstudies = 6), then Australia (Nstudies = 2). Included articles were published between 1996 and 2024, and study sample sizes varied considerably (Nrange = 30–1,238). Most studies utilized hospitals/craniofacial units as their primary recruitment source (Nstudies = 15), although a single study each used population data or social media to recruit participants (see Supplementary Table S3 for study characteristics).
Nine studies provided data on ADHD diagnoses (Nparticipants = 1,723), one reported an ADHD screening measure (Nparticipants = 33) and one reported ADHD symptoms (Nparticipants = 219). Seven studies examined attention problems/functioning (Nparticipants = 568) and six studies reported hyperactivity symptoms (Nparticipants = 377) (see Supplementary Table S4 for the outcomes and measures used by each study).
Estimated effect sizes varied considerably across the included studies in each of the outcomes examined, as reflected in the heterogeneity indices (see Supplementary Table S5 for all effect estimates generated and their associated statistics). The results, for the most part, were also susceptible to publication bias (Nfs). Individual findings, grouped by suture location, surgical status, age group, and the type of outcome assessed are discussed in more detail in the following subsections.
Participant characteristics
The 17 independent studies included in this meta-analysis provided data for 2,389 children (Mage = 7.3 yrs) with single-suture non-syndromic craniosynostosis and 12,742 unaffected controls (Mage = 7.7 yrs). Approximately two-thirds of each group were male (Ncraniosynostosis = 63%, Ncontrols = 69%). Eleven studies examined metopic synostosis (Nparticipants = 527) and nine sagittal synostosis (Nparticipants = 441), but two studies encompassing 1,272 participants (53%) did not report suture location and have been analyzed as “combined” suture locations. Over 80% of participants (Nparticipants = 1999) had received surgery for their condition, with three studies (Nparticipants = 180) reporting data on participants who were conservatively managed and did not receive surgery. No studies provided outcomes that enabled analysis for infants or adults. See for summary characteristics of participants.
Table 1. Summary demographic characteristics of participants (17 independent studies) at baseline.
Study risk of bias assessment
The overall quality of reporting for the included observational cohort (OC-CS; single group) studies was variable (see Supplementary Tables S6 & S7; and ). Most single-group studies failed to report sample size justifications or power descriptions, whether assessors were blind to the participants’ craniosynostosis diagnoses, and whether key confounding variables were considered and adjusted for statistically. In contrast, the quality of the included case-control (CCS; two-group) studies was higher. The majority of case-control studies reported clear research objectives, their inclusion and exclusion criteria, differentiated between cases and controls, and clearly defined the measures and diagnostic tools used.
Figure 2. Prevalence rates, odds ratios and standardized mean differences of ADHD diagnoses or symptoms associated with ADHD, in children with craniosynostosis, partitioned according to suture type, surgical status and age.
Craniosynostosis and ADHD: diagnosis, screened, and symptoms
When studies examining formal diagnoses of ADHD were combined (see ), the frequency of ADHD diagnoses was 7%, a modest rate comparable with the general population (8%) (Ayano et al., Citation2023). Two studies reported rates of ADHD between individuals with craniosynostosis and without, with no difference found between groups (Nparticipants = 1417; OR = 1.01 [95% CI = 0.43–2.37]). Rates of ADHD across the nine studies ranged from 2% to 28% although most studies were small (<66 participants) with the exception of the 2 studies that utilized controls (Collett et al., Citation2017 (Nparticipants = 179); Tillman et al., Citation2020 (Nparticipants = 1238)).
When studies were partitioned according to suture type, individuals with metopic synostosis had the highest rate of diagnosed ADHD (16%; Nstudies = 5), followed by four studies that combined sutures (3%), and one study examining children with sagittal synostosis (2%). The majority of participants had received surgery (Nparticipants = 1478; ADHD = 8%) and the remaining 66 participants, who were a combination of post-surgery + conservatively managed, were also found to have an 8% ADHD prevalence rate. When studies were partitioned by age range, diagnosed ADHD was highest in children of primary school age (12%; Nstudies = 6), with only single studies examining individuals who were younger (preschool; ADHD = 3%) or older (secondary school; ADHD = 2%).
One study used the Behavior Rating Inventory of Executive Function to screen for ADHD, with 18% of both the craniosynostosis and control groups (Nparticipants each group = 33) scoring above the cutoff point for identifying problematic levels of behavior (OR = 1.00 [95% CI = 0.29–3.49]). Lastly, one study used the Child Behavior Checklist to identify attention deficit/hyperactivity problems in pre-school aged children (Ncraniosynostosis = 219; Ncontrols = 217), finding a small effect, but no significant difference, between groups (g = −.18, p = .21).
Craniosynostosis and attention
Only a few studies that have examined attention in craniosynostosis samples were found and therefore results should be interpreted with caution (see ). First, studies that used recommended cutoffs on measures in order to determine the presence of problematic behavior were analyzed. The data from these studies were partitioned according to whether participants were assessed with an “objective,” cognitive measure (Nstudies = 2), or a “subjective” questionnaire that was completed by parents/teachers/caregivers (Nstudies = 2). Attention difficulties were reported in twice as many individuals when questionnaires were completed (31%) compared to when cognitive tests of attention were administered (15%), a result consistent with previous findings. The two studies that assessed children using cognitive tests of attention also used control groups, with the data showing a small negative effect for the craniosynostosis group (OR = 1.74, p = .40), with the small sample size (Ncraniosynostosis = 86; Ncontrols = 39) likely contributing to the non-significance of the result.
Figure 3. Prevalence rates, odds ratios and standardized mean differences of attention problems or attention functioning, in children with craniosynostosis, partitioned according to type of measure administered.
Second, two studies used continuous data to examine differences between groups on either cognitive tests of attention or questionnaires. Small negative group differences (gcognitive/objective = −.29; gquestionnaires/subjective = −.16) were found, but neither result was significant.
Craniosynostosis and hyperactivity
All assessments of hyperactivity were based on parent-reported questionnaires (see ). Two samples provided standardized mean difference data (g = −.06, p = .77), demonstrating that there was no difference between children with craniosynostosis and their peers when parents were asked about their child’s behavior using either the Behavior Assessment System for Children or the Strengths and Difficulties Questionnaire (SDQ). A second meta-analysis used cutoffs on the Connors-3 short, Child Behavior Checklist and SDQ to determine the proportion of children displaying high levels of hyperactivity, with 29% of the overall sample (Nstudies = 4, Nparticipants = 292) exhibiting hyperactivity problems.
Discussion
Data were analyzed from 17 independent studies (Nparticipants = 2,389) in order to determine whether, and to what extent, single-suture, non-syndromic craniosynostosis impacts the development of ADHD or related symptoms (inattention, hyperactivity). Overall, individuals with single-suture, non-syndromic craniosynostosis had similar rates of diagnosed ADHD, attention problems, and hyperactivity symptoms to general population and primary care estimates (Ayano et al., Citation2023; Spencer et al., Citation2018; Vugteveen et al., Citation2022). Where cases with single-suture, non-syndromic craniosynostosis were compared to unaffected control groups, there was no significant difference in scores on diagnoses of ADHD, ADHD screening tests, ADHD symptoms, or measures of attention and hyperactivity (see , and ), although small negative effects were often found. This lack of difference in scores between cases and controls may partially be explained by the limited numbers of studies available for analysis and their generally small sample sizes. For this reason, further testing with larger sample sizes is needed in order to determine more conclusively, whether children with craniosynostosis function more poorly than their peers in these domains.
It is critical when examining difficulties with attention and hyperactivity not to conflate a diagnosis of ADHD with a child’s functioning on tests of these symptoms. To be diagnosed with ADHD, a child must undergo a comprehensive and multi-factorial assessment ensuring that their difficulties can not be accounted for by any other condition. Thus, it was deemed more important to ensure that analyses were partitioned into comparable outcomes (e.g., formal ADHD diagnoses vs ADHD screening), than combine related, but not equivalent, measures and domains together. However, given the dearth of research in this area to date, this decision resulted in only a few studies being available per analysis.
Further, one study (Collett et al., Citation2017) had fewer children (Mage = 7 years) with ADHD in their craniosynostosis group (3.9%) than their control group (6.6%). While this difference is small, it may have impacted results on cognitive measures of attention and parental perceptions of behavior, diminishing any potential differences in overall scores between groups. However, cases also reported a similar use of ADHD medication use (5.6% cases, 5.5% controls) highlighting a discrepancy between medication use in children with craniosynostosis versus the number of children with formal diagnoses. Nonetheless, both groups were recruited at 18 months of age and regularly monitored on a range of cognitive and behavioral outcomes. This suggests that this discrepancy in formal diagnosis rates cannot be explained by the fact that one group may have had greater access to the health system and hence, more opportunities for referral and testing.
It remains unclear what impact suture type may have on the development of ADHD or related symptoms as the location of the affected suture was only known for a small proportion of participants. ADHD is associated with atypical brain morphology, especially that of the prefrontal cortex, and individuals often experience difficulties with executive functions such as working memory and sustained attention (Faraone et al., Citation2021). The high rate of diagnosed ADHD found in children with metopic synostosis (16%) is consistent with research advocating that the location of the metopic suture to the frontal lobe may result in greater executive functioning dysregulation (Almeida et al., Citation2024). Similarly, it has also been found that, after adjusting for SES, the only domain with significant differences between conservatively managed children with metopic synostosis and their peers was that of executive functioning (Osborn et al., Citation2021). Further research into these domains is necessary in order to better understand how they are impacted in children with craniosynostosis. The paucity of data examining cognitive and behavioral outcomes in children with other types of craniosynostosis (e.g., lambdoid, unicoronal) demonstrates the need for further research, despite the reduced frequency of their occurrence (Betances et al., Citation2020).
Also highlighted was the disparity between “subjective” measures of attention (e.g., self- or parent-rated questionnaires) and “objective” measures of attention (e.g., cognitive testing). The current study found twice as many parents reported that their child was experiencing problems with behaviors associated with attention, compared with the level of attention problems identified during cognitive testing. This is consistent with research that suggests that each method is measuring a different facet of “attention.” That is, questionnaires measure the behavioral effects of attention problems, while cognitive tests measure “attention” as a specific cognitive construct (Silk, Citation2012). Additionally, it is being increasingly recognized that factors such as the Flynn effect (i.e., increasing IQ in general populations) can limit the utility and generalizability of subsequent findings (Long et al., Citation2022). So, for this reason, when comparisons between groups were being analyzed, we elected to only include studies that recruited a comparison group. We did not include studies that compared M/SD data of individuals with craniosynostosis to normative data only. This decision resulted in a few studies (Nstudies = 3) being excluded because their data was not suitable for the current meta-analysis.
Although data on the age of participants were limited, the majority of research focussed on children of primary school age, with no studies reporting diagnoses of infants or adults. This is not unexpected as few validated measures assess cognitive functions such as attention and executive functioning in pre-schoolers, and there is minimal data available, across any domain, on outcomes in adults with craniosynostosis. Data were also limited on older children’s outcomes, highlighting the need for research on the long-term functioning of children and adults with craniosynostosis. Nonetheless, the data do contribute to the currently limited pool of data regarding ADHD, hyperactivity, and inattention outcomes in those with single-suture, non-syndromic craniosynostosis. Further, the developmental trajectory of ADHD by age was largely consistent with what is typically observed in general populations (Spencer et al., Citation2018). As individuals age they become more adept at regulating attention, and hyperactivity decreasing observed symptomology in both neurotypical and ADHD populations (Leffa et al., Citation2022).
Socioeconomic disparities have been shown to have a large impact on both ADHD and craniosynostosis outcomes. For individuals with craniosynostosis, lower socioeconomic status has been linked to poorer health-care outcomes, longer diagnostic timeframes, and decreased access to relevant clinical treatments (Blum et al., Citation2023). For individuals with ADHD, lower socioeconomic status has been linked to underdiagnosis, decreased access to treatment and medication, and worse ADHD outcomes (Spencer et al., Citation2018). Further, Spencer et al. (Citation2018) suggest that ADHD is more prevalent in lower socioeconomic areas. In the current study, the SES status of only 20% of participants (Nstudies = 7) was described, with even fewer studies controlling for SES in their analyses, suggesting that socioeconomic status should be more centrally considered in analyses of craniosynostosis, especially where ADHD is concerned.
Moreover, in regard to ADHD diagnoses, the purpose of most included studies was for reasons other than specifically examining the prevalence of ADHD, with ADHD diagnosis rates often extracted from demographic information about their participants. Moreover, the two largest studies (Collett et al., Citation2017; Tillman et al., Citation2020) reported low rates of diagnosed ADHD (Nparticipants = 179, 4% & Nparticipants = 1238, 2%, respectively), with smaller studies reporting higher ADHD rates, potentially leading to bias within analyses. It is acknowledged that the diagnosis of ADHD involves considerable resources given the complexity involved. Nevertheless, future research should endeavor to undertake comprehensive assessments of ADHD rather than relying on whether a child has received a diagnosis as part of their usual healthcare.
There are a number of limitations that warrant consideration. First, although factors such as age, sex, and suture location may impact the development of ADHD or problems with attention/hyperactivity, these data were often not reported, or were provided in a form that could not be compared (e.g., results combined for males/females), precluding a comprehensive analysis of these variables. Although the mean age of the sample may have been reported, it was not always clear at what age individuals had been diagnosed with ADHD or, as in some instances, the age range of participants was broad and it is possible that mean age data did not accurately reflect the age categories used in the current analysis. Future research should endeavor to report separate outcome data across age, sex and suture location. Second, as data were limited, data from parent, teacher, and self-report ratings on subjective measures of attention and hyperactivity were combined, precluding an analysis of differences in results across informants. Third, while the included studies were of generally high quality, overall there were few studies that utilized control groups, an inclusion criteria for the current study where differences between groups were reported, highlighting the need to use appropriately matched control groups in order to compare findings.
Conclusion
The current study provides an important contribution to the literature by compiling and comprehensively analyzing the research undertaken to date around ADHD, attention functioning and hyperactivity symptoms in children with craniosynostosis. The findings indicate that, overall, there are few differences in these domains between children with and without craniosynostosis. However, relatively limited numbers of studies have explored these domains and thus, further large-scale, longitudinal studies using matched control groups and implementing comprehensive assessments of ADHD for all participants are required. In the meantime, however, children should be monitored for behavioral or cognitive difficulties and appropriate support provided if needed.
Supplemental Material
Download MS Word (56.6 KB)Acknowledgments
The authors would like to thank Lara Ljubicic, who assisted with the searching process.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The authors confirm that the data supporting the findings of this meta-analysis are available within its supplementary materials
Supplementary material
Supplemental data for this article can be accessed online at https://doi.org/10.1080/87565641.2024.2357801
Additional information
Funding
References
- *Almeida, M. N., Alper, D. P., Long, A. S., Barrero, C., Williams, M. C., Boroumand, S. & Alperovich, M. (2021). Risk of ADHD, autism spectrum disorder, and executive function impairment in metopic craniosynostosis. Plastic and Reconstructive Surgery, 10, 1097. Advance Online Publicatiion. https://doi.org/10.1097/PRS.0000000000011249
- Almeida, M. N., Alper, D. P., Parikh, N., De Baun, H., Kammien, A., Persing, J. A., & Alperovich, M. (2024). Comparison of emotional and behavioral regulation between metopic and sagittal synostosis*. Child’s Nervous System. https://doi.org/10.1007/s00381-024-06387-8
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (DSM-5) (5th ed.).
- Ayano, G., Demelash, S., Gizachew, Y., Tsegay, L., & Alat, R. (2023). The global prevalence of attention deficit hyperactivity disorder in children and adolescents: An umbrella review of meta-analyses. Journal of Affective Disorders, 339, 860–866. https://doi.org/10.1016/j.jad.2023.07.071
- Betances, E. M., Mendez, M. D., & Das, J. M. (2020). Craniosynostosis. In Stat Pearls. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK544366/
- Blum, J. D., Ng, J. J., Craig, J., Smith, R., Kota, A., Moura, S. P. & Cho, D. Y. (2023). Sociodemographic disparities in craniosynostosis: A systematic review. Cleft Palate Craniofacial Journal, 10556656231199832. https://doi.org/10.1177/10556656231199832
- *Boltshauser, E., Ludwig, S., Dietrich, F., & Landolt, M. A. (2003). Sagittal craniosynostosis: Cognitive development, behaviour, and quality of life in unoperated children. Neuropediatrics, 34(6), 293–300. https://doi.org/10.1055/s-2003-44667
- Borenstein, M., Hedges, L. V., Higgins, J., & Rothstein, H. (2022). Comprehensive meta-analysis version 4 (Version 4th). Biostat.
- Borenstein, M., Hedges, L. V., Higgins, J. P. T., & Rothstein, H. R. (2010). A basic introduction to fixed-effect and random-effects models for meta-analysis. Research Synthesis Methods, 1(2), 97–111. https://doi.org/10.1002/jrsm.12
- Borenstein, M., Higgins, J. P., Hedges, L. V., & Rothstein, H. R. (2017). Basics of meta-analysis: I2 is not an absolute measure of heterogeneity. Research Synthesis Methods, 8(1), 5–18. https://doi.org/10.1002/jrsm.1230
- Brooks, E. D., Beckett, J. S., Yang, J., Timberlake, A. T., Sun, A. H., Chuang, C., & Persing, J. A. (2018). The etiology of neuronal development in craniosynostosis: A working hypothesis. The Journal of Craniofacial Surgery, 29(1), 49–55. https://doi.org/10.1097/SCS.0000000000004040
- Care, H., Horton, J., Kearney, A., Kennedy-Williams, P., Knapp, M., Rooney, N. & Dalton, L. (2019). Introduction to the craniofacial collaboration UK: A developmental screening protocol at the United Kingdom’s four highly specialized craniofacial centers. Journal of Craniofacial Surgery, 30(1), 83–86. https://doi.org/10.1097/SCS.0000000000004846
- *Care, H., Kennedy-Williams, P., Cunliffe, A., Denly, S., Horton, J., Kearney, A. & Dalton, L. (2019). Preliminary analysis from the craniofacial collaboration United Kingdom developmental outcomes in children with sagittal synostosis. Journal of Craniofacial Surgery, 30(6), 1740–1744. https://doi.org/10.1097/SCS.0000000000005575
- Chen, H., Cohen, P., & Chen, S. (2010). How big is a big odds ratio? Interpreting the magnitudes of odds ratios in epidemiological studies. Communications in Statistics - Simulation and Computation, 39(4), 860–864. https://doi.org/10.1080/03610911003650383
- *Chieffo, D., Tamburrini, G., Massimi, L., DiGiovanni, S., Giansanti, C., Caldarelli, M., & DiRocco, C. (2010). Long-term neuropsychological development in single-suture craniosynostosis treated early: Clinical article. Journal of Neurosurgery: Pediatrics, 5(3), 232–237. https://doi.org/10.3171/2009.10.PEDS09231
- Cohen, J. (1992). A power primer. Psychological Bulletin, 112(1), 155–159. https://doi.org/10.1037/0033-2909.112.1.155
- *Collett, B. R., Kapp-Simon, K. A., Wallace, E., Cradock, M. M., Buono, L., & Speltz, M. L. (2017). Attention and executive function in children with and without single-suture craniosynostosis. Child Neuropsychology, 23(1), 83–98. https://doi.org/10.1080/09297049.2015.1085005
- Cornelissen, M., den Ottelander, B., Rizopoulos, D., van der Hulst, R., van der Molen, A. M., van der Horst, C. & Mathijssen, I. (2016). Increase of prevalence of craniosynostosis. Journal of Cranio-Maxillofacial Surgery, 44(9), 1273–1279. https://doi.org/10.1016/j.jcms.2016.07.007
- *Culshaw, L., Piggott, K., Care, H., Dalton, L., Denly, S., Horton, J. & Thornhill, H. (2022). The craniofacial collaboration UK: Developmental outcomes in 3-year-old children with metopic synostosis. Journal of Craniofacial Surgery, 33(1), 112–116. https://doi.org/10.1097/SCS.0000000000008045
- Derderian, C., & Seaward, J. (2012). Syndromic craniosynostosis. Seminars in Plastic Surgery, 26(2), 064–075. https://doi.org/10.1055/s-0032-1320064
- DiRocco, F., Arnaud, E., & Renier, D. (2009). Evolution in the frequency of nonsyndromic craniosynostosis. Journal of Neurosurgery: Pediatrics, 4(1), 21–25. https://doi.org/10.3171/2009.3.PEDS08355
- *Doshier, L. J., Muzaffar, A. R., Deidrick, K. K., & Rice, G. B. (2015). Analysis of individualized education programs to quantify long-term educational needs following surgical intervention for single-suture craniosynostosis. Canadian Journal of Plastic Surgery, 23(1), 31–34. https://doi.org/10.1177/229255031502300102
- *Edwards-Bailey, L., Piggott, K., Dalton, L., Horton, J., Parks, C., White, S. & Kearney, A. (2024). The craniofacial collaboration UK: Developmental outcomes in 7- and 10-year-old children with metopic synostosis. Journal of Craniofacial Surgery, 35(1), 96–103. https://doi.org/10.1097/SCS.0000000000009803
- *Edwards-Bailey, L., Piggott, K., Dalton, L., Horton, J., Parks, C., Wright, G., & Kearney, A. (2023). The craniofacial collaboration UK: Developmental outcomes in 5-year-old children with metopic synostosis. Journal of Craniofacial Surgery, 34(3), 855–859. https://doi.org/10.1097/SCS.0000000000009095
- Faraone, S. V., Banaschewski, T., Coghill, D., Zheng, Y., Biederman, J., Bellgrove, M. A. & Wang, Y. (2021). The world federation of ADHD International consensus statement: 208 Evidence-based conclusions about the disorder. Neuroscience & Biobehavioral Reviews, 128, 789–818. https://doi.org/10.1016/j.neubiorev.2021.01.022
- Gaillard, L., Tjaberinga, M., Dremmen, M., Mathijssen, I., & Vrooman, H. (2024). Brain volume in infants with metopic synostosis: Less white matter volume with an accelerated growth pattern in early life. Journal of Anatomy, 00, 1–9. https://doi.org/10.1111/joa.14028
- Kajdic, N., Spazzapan, P., & Velnar, T. (2018). Craniosynostosis-recognition, clinical characteristics, and treatment. Bosnian Journal of Basic Medical Sciences, 18(2), 110–116. https://doi.org/10.17305/bjbms.2017.2083
- *Kapp-Simon, K. A. (1998). Mental development and learning disorders in children with single suture craniosynostosis. Cleft Palate-Craniofacial Journal, 35(3), 197–203. https://doi.org/10.1597/1545-1569_1998_035_0197_mdaldi_2.3.co_2
- *Kapp-Simon, K. A., Collett, B. R., Barr-Schinzel, M. A., Cradock, M. M., Buono, L. A., Pietila, K. E., & Speltz, M. L. (2012). Behavioral adjustment of toddler and preschool-aged children with single-suture craniosynostosis. Plastic and Reconstructive Surgery, 130(3), 635–647. https://doi.org/10.1097/PRS.0b013e31825dc18b
- Kessi, M., Duan, H., Xiong, J., Chen, B., He, F., Yang, L. & Yin, F. (2022). Attention-deficit/hyperactive disorder updates. Frontiers in Molecular Neuroscience, 15, 925049. https://doi.org/10.3389/fnmol.2022.925049
- Kian, N., Samieefar, N., & Rezaei, N. (2022). Prenatal risk factors and genetic causes of ADHD in children. World Journal of Pediatrics, 18(5), 308–319. https://doi.org/10.1007/s12519-022-00524-6
- *Kljajic, M., Maltese, G., Tarnow, P., Sand, P., & Kölby, L. (2021). Children treated for nonsyndromic craniosynostosis exhibit average adaptive behavior skills with only minor shortcomings. Plastic and Reconstructive Surgery, 147(2), 453–464. https://doi.org/10.1097/PRS.0000000000007541
- *Kljajić, M., Maltese, G., Tarnow, P., Sand, P., & Kölby, L. (2019). The cognitive profile of children with nonsyndromic craniosynostosis. Plastic and Reconstructive Surgery, 143(5), 1037e–1052e. https://doi.org/10.1097/PRS.0000000000005515
- *Kljajić, M., Maltese, G., Tarnow, P., Sand, P., & Kölby, L. (2020). Sustained attention and vigilance of children treated for sagittal and metopic craniosynostosis. Child Neuropsychology, 26(4), 475–488. https://doi.org/10.1080/09297049.2019.1682130
- *Kljajić, M., Maltese, G., Tarnow, P., Sand, P., & Kölby, L. (2023). Health-related quality of life of children treated for non-syndromic craniosynostosis. Journal of Plastic Surgery and Hand Surgery, 57(1–6), 408–414. https://doi.org/10.1080/2000656X.2022.2147532
- Krieger, V., Amador-Campos, J. A., Guardia-Olmos, J., & Rodríguez, C. (2020). Executive functions, personality traits and ADHD symptoms in adolescents: A mediation analysis. Public Library of Science ONE, 15(5), e0232470. https://doi.org/10.1371/journal.pone.0232470
- Lee, H. Q., Hutson, J. M., Wray, A. C., Lo, P. A., Chong, D. K., Holmes, A. D., & Greensmith, A. L. (2012). Changing epidemiology of nonsyndromic craniosynostosis and revisiting the risk factors. Journal of Craniofacial Surgery, 23(5), 1245–1251. https://doi.org/10.1097/SCS.0b013e318252d893
- Leffa, D. T., Caye, A., & Rohde, L. A. (2022). ADHD in children and adults: Diagnosis and prognosis. New Discoveries in the Behavioral Neuroscience of Attention-Deficit Hyperactivity Disorder, 57, 1–18. https://doi.org/10.1007/7854_2022_329
- Li, T., Mota, N. R., Galesloot, T. E., Bralten, J., Buitelaar, J. K., IntHout, J. & Franke, B. (2019). ADHD symptoms in the adult general population are associated with factors linked to ADHD in adult patients. European Neuropsychopharmacology, 29(10), 1117–1126. https://doi.org/10.1016/j.euroneuro.2019.07.136
- Long, A. S., Hauc, S. C., Junn, A. H., Meyer, C., Mayes, L., Persing, J. A., & Alperovich, M. (2022). IQ assessment in craniofacial neurocognitive studies: Interpreting results relative to evidence-based systematic analysis. Plastic and Reconstructive Surgery - Global Open, 10(7), e4405. https://doi.org/10.1097/GOX.0000000000004405
- Martínez, L., Prada, E., Satler, C., Tavares, M. C., & Tomaz, C. (2016). Executive dysfunctions: The role in attention deficit hyperactivity and post-traumatic stress neuropsychiatric disorders. Frontiers in Psychology, 7, 206398. https://doi.org/10.3389/fpsyg.2016.01230
- Orwin, R. G. (1983). A fail-safe N for effect size in meta-analysis. Journal of Educational Statistics, 8(2), 157–159. https://doi.org/10.3102/10769986008002157
- *Osborn, A. J., Roberts, R. M., Dorstyn, D. S., Grave, B. G., & David, D. J. (2023). Behavioural and psychological functioning of children and adults with sagittal synostosis. Journal of Pediatric Neuropsychology, 9(4), 1–17. https://doi.org/10.1007/s40817-023-00149-1
- *Osborn, A. J., Roberts, R. M., Mathias, J. L., Anderson, P. J., & Flapper, W. J. (2021). Cognitive, behavioral and psychological functioning of children and adults with conservatively managed metopic synostosis. Child Neuropsychology, 27(2), 190–208. https://doi.org/10.1080/09297049.2020.1817356
- Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D. & Moher, D. (2020). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. MetaArXiv. https://doi.org/10.31222/osf.io/v7gm2
- Palladino, V. S., McNeill, R., Reif, A., & Kittel-Schneider, S. (2019). Genetic risk factors and gene–environment interactions in adult and childhood attention-deficit/hyperactivity disorder. Psychiatric Genetics, 29(3), 63–78. https://doi.org/10.1097/YPG.0000000000000220
- *Qi, R., Piggott, K., Lloyd-White, S., & Kearney, A. (2023). Developmental outcomes for children with unoperated metopic or sagittal craniosynostosis: Findings at 3 and 7 years from the craniofacial collaboration UK. Journal of Craniofacial Surgery, 34(7), 1953–1958. https://doi.org/10.1097/SCS.0000000000009463
- *Sidoti, E. J., Jr., Marsh, J. L., Marty-Grames, L., & Noetzel, M. J. (1996). Long-term studies of metopic synostosis: Frequency of cognitive impairment and behavioral disturbances. Plastic and Reconstructive Surgery, 97(2), 276–281. https://doi.org/10.1097/00006534-199602000-00002
- Silk, E. (2012). Relationship between subjective and objective measures of attention in a clinical population of children and adolescents. Nova Southeastern University.
- *Snyder, H., & Pope, A. W. (2010). Psychosocial adjustment in children and adolescents with a craniofacial anomaly: Diagnosis-specific patterns. The Cleft Palate-Craniofacial Journal, 47(3), 264–272. https://doi.org/10.1597/08-227.1
- Speltz, M. L., Kapp-Simon, K. A., Cunningham, M., Marsh, J., & Dawson, G. (2004). Single-suture craniosynostosis: A review of neurobehavioral research and theory. Journal of Pediatric Psychology, 29(8), 651–668. https://doi.org/10.1093/jpepsy/jsh068
- Spencer, A. E., Plasencia, N., Sun, Y., Lucke, C., Haile, H., Cronin, R. & Biederman, J. (2018). Screening for attention-deficit/hyperactivity disorder and comorbidities in a diverse, urban primary care setting. Clinical Pediatrics, 57(12), 1442–1452. https://doi.org/10.1177/0009922818787329
- Tahiri, Y., Bartlett, S. P., & Gilardino, M. S. (2017). Evidence-based medicine: Nonsyndromic craniosynostosis. Plastic and Reconstructive Surgery, 140(1), 177e–191e. https://doi.org/10.1097/PRS.0000000000003473
- Tarnow, P., Kölby, L., Maltese, G., Söfteland, M. B., Lewén, A., Nilsson, P. & Nowinski, D. (2022). Incidence of non-syndromic and syndromic craniosynostosis in Sweden. Journal of Craniofacial Surgery, 33(5), 1517–1520. https://doi.org/10.1097/scs.0000000000008457
- Thomas, R., Sanders, S., Doust, J., Beller, E., & Glasziou, P. (2015). Prevalence of attention-deficit/hyperactivity disorder: A systematic review and meta-analysis. Pediatrics, 135(4), e994–e1001. https://doi.org/10.1542/peds.2014-3482
- *Tillman, K. K., Höijer, J., Ramklint, M., Ekselius, L., Nowinski, D., & Papadopoulos, F. C. (2020). Nonsyndromic craniosynostosis is associated with increased risk for psychiatric disorders. Plastic and Reconstructive Surgery, 146(2), 355–365. https://doi.org/10.1097/PRS.0000000000007009
- *van der Vlugt, J. J., van der Meulen, J. J., Creemers, H. E., Verhulst, F. C., Hovius, S. E., & Okkerse, J. M. (2012). Cognitive and behavioral functioning in 82 patients with trigonocephaly. Plastic and Reconstructive Surgery, 130(4), 885–893. https://doi.org/10.1097/PRS.0b013e318262f21f
- Vugteveen, J., de Bildt, A., & Timmerman, M. E. (2022). Normative data for the self-reported and parent-reported strengths and difficulties questionnaire (SDQ) for ages 12–17. Child and Adolescent Psychiatry and Mental Health, 16(1), 1–13. https://doi.org/10.1186/s13034-021-00437-8
- *Wójcicki, P., & Prudel, B. (2019). Trigonocephaly: Long-term results after surgical correction of metopic suture synostosis. Advances in Clinical and Experimental Medicine, 28(5), 625–635. https://doi.org/10.17219/acem/90763
- World Health Organization (WHO). (2019/2021). International classification of diseases, Eleventh Revision (ICD-11). https://icd.who.int/browse11.%20Licensed%20under%20Creative%20Commons%20Attribution-NoDerivatives%203.0%C2%A0IGO%20licence%20(CC%C2%A0BY-ND%C2%A03.0%C2%A0IGO)