Abstract
Aim:
Occlusal therapy is employed to alleviate the symptoms of a temporomandibular disorder (TMD) at times. However, the long-term effect of occlusal therapy in the masticatory system is not well understood. This case study aims to present a 30-year follow-up of a TMD case.
Methodology:
The patient developed TMD with intermittent closed lock of the left temporomandibular joint (TMJ). Chief complaints included trismus, pain, and noise of the left TMJ during function. The patient’s occlusal disharmony was assessed with use of electronic instruments and corrected based on the neuromuscular concept. A minimum-invasive and reversible approach using adhesive occlusal restorations was used.
Results:
The jaw movement and masticatory muscle activity assessed at the 7- and 23-year follow-ups revealed that the established occlusion was well adapted, and re-established the patient’s functional occlusion system. The patient has been free from TMD symptoms with the corrected occlusion for 30 years.
Conclusions:
Occlusal reconstruction based on the neuromuscular concept can be stably integrated into the patient’s functional occlusion system.
Introduction
The physiological masticatory system lies in homeostasis between teeth, periodontium, masticatory muscles, temporomandibular joints, craniofacial skeleton, and the neuromuscular system.Citation1 An occlusal alteration in such homeostasis by dental treatment may lead to disharmony in the masticatory system.Citation2–Citation5
The physiological masticatory function is governed by the neuromuscular control. Therefore, it is not achievable to accurately simulate or evaluate the masticatory system using a dental articulator. Although it is obvious that masticatory muscles are the dominant determinant of jaw movement, the muscles and the mandible position relative to the cranium are not well appreciated in the practice of the conventional mechanical model of occlusion. Mandibular locomotion is powered by masticatory muscles. Temporomandibular joints (TMJs), which connect the cranium and the condyles of the mandible render the mandibular movement flexible. Therefore, factors that negatively impact the function of muscles and TMJs would potentially lead to the development of a temporomandibular disorder (TMD). In this sense, occlusal treatment as a TMD therapy intends to correct the disharmony in the physiological masticatory system. Among the components described above, teeth are the most unstable in the physiological masticatory system. Teeth (location and occlusal morphology) dictate the three-dimensional positioning of the mandible relative to the cranium at the maximum intercuspal position. In other words, one function of the teeth component is to maintain a stable, musculoskeletally harmonized position between the cranium, TMJs, and mandible. When this stable position is altered, the neuromuscular system may adapt a new position and could develop a TMD over time. Most clinicians agree that insertion of an occlusal splint often improves symptoms in TMD patients.Citation6,Citation7 This supports the role of occlusion therapy to maintain the musculoskeletally harmonized positioning between the cranium, TMJs, and mandible. Dental treatment modifies occlusion when necessary, and although rare, this modification may perturb a functional equilibrium of the physiological masticatory system and could lead to the development of TMD. Currently, the etiological role of occlusion in TMD is unclear.Citation8,Citation9 However, it is agreed that occlusion established on an eccentric jaw position will not be tolerated by a host and will cause disharmony in the physiological masticatory system.
Large individual variations exist in physiological occlusion. Physiological occlusion may present with morphologically non-ideal articulation such as skeletal class III occlusion and a crossbite. This variability makes it difficult to identify the etiological relationship between malocclusion and TMD. However, considering that major determinants of jaw movement are muscles, it is not surprising to observe physiological occlusion in individuals with class III occlusion having smooth jaw movement and coordinated balanced muscle activity. Hence, when an occlusal discrepancy is suspected to be involved in TMD, we routinely analyze jaw movement and surface masticatory muscle activity of patients to assess the physiological masticatory system of patients. A non-invasive approach is taken for patients to re-establish acceptable physiological occlusion, typically characterized by smooth jaw movement and symmetric masticatory muscle activity. This case report presents a 30-year follow-up of a TMD case.
Case
A 19-year-old female student visited the prosthodontic clinic at Okayama University, Japan, in 1982 with a chief complaint of trismus, sharp pain, and noise around her left TMJ. No specific medical history was noted. The patient received orthodontic treatment in 1978 when she was 15 years old. The orthodontic treatment corrected her class II malocclusion with strategic extractions of all first premolars. In 1981, the braces were removed and removable retainers were placed; however, she did not wear the retainers. She noticed noise around the left TMJ during jaw opening within half a year of the braces being removed and soon developed limited mouth opening. The patient visited an oral surgery clinic in 1982 and received pharmaceutical therapy consisting of a muscle relaxant. However, no improvement was noted.
Initial examination
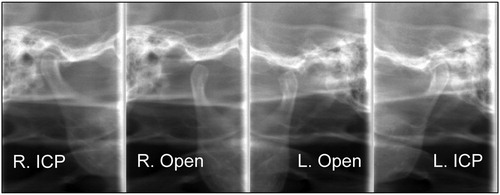
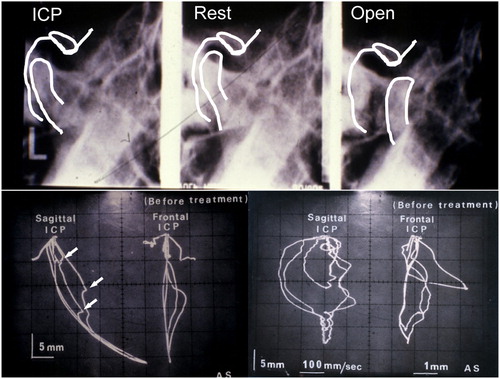
The midline of the mandible deflected to the right (). The maxillary central incisors were extruded with a deep bite. Overbite and overjet were approximately 4 and 2·5 mm, respectively. Advanced wear facets were noted on the incisal edge of the mandibular central incisors. The maxillary second premolars tilted mesially with extrusion. Open space was noted between the left canine and second premolar. Amalgam restorations were noted on the mandibular first molars and left second molar. The maxillary right first molar was restored with a full cast crown. The mandible deviated toward the left during jaw opening, and sharp pain was reported when the clicking noise occurred. Maximum mouth opening was approximately 40 mm. The palpation of TMJ revealed that clicking occurred during a first few jaw openings and no clicking was observed thereafter. Radiographic assessment revealed that the mandibular left condyle positioned posteriorly at the intercuspal position (ICP) and at rest (). During jaw opening, the condyle did not travel far enough anteriorly: the condyle was below the articular tubercle at the maximum opening.
Figure 2. Radiographic images of the mandibular left TMJ at ICP before treatment (top-left), at rest position (top-middle), and at opening position (top-right). The condyle appeared to be displaced posteriorly at ICP and not traveled enough anteriorly at the jaw opening position. No baseline radiographs of the right TMJ are available, due to development failures. Baseline MKG recordings of habitual mandibular movement are shown (bottom). Dyskinesia (arrows) was observed during jaw opening in Scan 1 (bottom-left). The mandible moved anteriorly during closing, arrived at the mid-lingual surface of the maxillary incisor, and slid into ICP. The velocity of jaw movements was recorded and shown in Scan 2 (bottom-right). Bradykinesia was observed when the jaw opened. The velocity of jaw closing movement was normal.
Jaw movement assessment
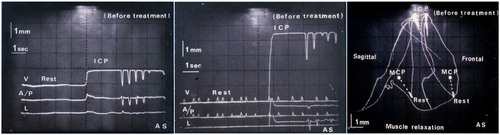
Jaw movements were assessed using a mandibular kinesiograph (MKG K5; Myotronics, Kent, WA, USA). Dyskinesia was observed during jaw opening (arrows in bottom-left). During closing, the mandibular incisors first touched the mid-lingual surface of the maxillary incisors, and from there, the mandible slid posteriorly along the lingual surfaces of the maxillary incisors to ICP. Sagittal trajectories during rapid maximum jaw opening from ICP showed bradykinesia (slow movement) clearly in the opening phase and no deviation in the closing phase ( bottom-right). Dyskinesia was also observed in frontal trajectories. No assessment of the muscle activity of the anterior temporalis and the middle masseters could be performed because a bilateral surface electromyography (EMG) recording device was not available in clinical dentistry in 1982. The patient received transcutaneous electrical nerve stimulation (TENS) using a Myomonitor J2 (Myotronics) to relax muscles.Citation10,Citation11 The Myo-centric position (MCP) was recorded as a reference jaw position.Citation12,Citation13 The intensity of electric stimuli by TENS was increased slightly to move the mandible approximately 1·5 mm above the rest position on a neuromuscular trajectory. This position was considered MCP. The discrepancy between MCP and ICP was approximately 1 mm sagittally, 3·5 mm vertically, and 2 mm laterally (). After 60 minutes of muscle relaxation by TENS, the intensity of TENS was gradually increased until the mandibular incisor lightly touched the lingual surface of the maxillary incisor. This mandibular position was on the TENS-stimulated trajectory of mandibular movement and, therefore, defined as muscular tooth contact position (MTCP). Bite registration at MTCP was taken using low-resistance acrylic impression material (Bosworth Sapphire; H.J. Bosworth Co., Skokie, IL, USA). The diagnostic models were mounted at MTCP using a Terminus Articulator (Myotronics) (). Occlusal discrepancy of 2–3 mm was noted in molar regions.
Figure 3. The three-dimensional jaw movement from rest position before treatment (left) and post muscle relaxation by TENS (middle). The mandible positioned approximately 0·6 mm anteriorly, 0·4 mm laterally, and 4·5 mm vertically from rest position after muscle relaxation. The position relationship between rest, MCP, and ICP after muscle relaxation by TENS is shown (right). ICP was located approximately 1 mm posterior to, 3·5 mm above, and 2 mm lateral to MCP.
TMD diagnosis
Intermittent closed lock of the left TMJ.
Patient agreement
Consent for publication was obtained from the patient.
Treatment
Since smooth jaw opening and closing were observed without pain when the patient took anterior position, MTCP was used as a therapeutic jaw position to alleviate TMD symptoms. A cranio-mandibular orthopedics (CMO) appliance was fabricated on the lower arch to stabilize the disc and condylar position at MTCP ( top-left). Anatomical occlusal morphology was given to the appliance so that the CMO appliance could maintain the mandibular position relative to the cranium at the maximal intercuspal position, and so the patient could eat with the appliance in place. Occlusal adjustment was performed at MTCP using TENS-stimulated jaw closing. Small pieces of a thin (20 μm) articulating paper were prepared and placed on the occlusal surfaces of the mandibular teeth. TENS-stimulated jaw closing was performed to obtain occlusal contact for adjustment. After use of the CMO appliance for 1 month, smooth jaw movement was observed ( bottom-left). However, ICP was not stable, as shown in the frontal view ( bottom-right). The vertical and anteroposterior movements were approximately 1·5 and 1·0 mm, respectively, which fell in a normal range ( top-right). However, the lateral shift was 0·25 mm, suggesting the requirement of further occlusal adjustment. Periodical occlusal adjustment continued until stable ICP was obtained. After use of the CMO appliance for 2 months, the patient reported neither TMJ pain nor clicking sound, indicating that the given occlusion was accepted by her physiological masticatory system. Hence, this occlusion was transferred to fixed restorations. Posterior onlays were fabricated using hard composite resin material (Isosit; Ivoclar Vivadent, Schaan, Liechtenstein) and seated with dental adhesive cement (Panavia EX; Kuraray, Osaka, Japan) ( top). Occlusal adjustment was performed at MTCP using TENS-stimulated jaw closing as described above ( top-right). Jaw movement was assessed 1 month later. The patient’s jaw movement was smooth, and trajectory was reproducible with the newly established occlusion ( bottom). The patient was placed on the maintenance program.
Figure 5. Fabricated CMO appliance on the mandible cast model had anatomical occlusal morphology (top-left). Jaw movements were recorded using MKG K5 after use of the CMO appliance for 1 month. Jaw open–close movements were smooth (bottom-left), and velocity of the movements was significantly improved (bottom-right). However, ICP appeared not yet stable (bottom-right). The recording of three-dimensional jaw movement from rest position shows that the mandible travels approximately 1·5 mm vertically, 1 mm anteriorly, and 0·2 mm laterally at the incisal position.
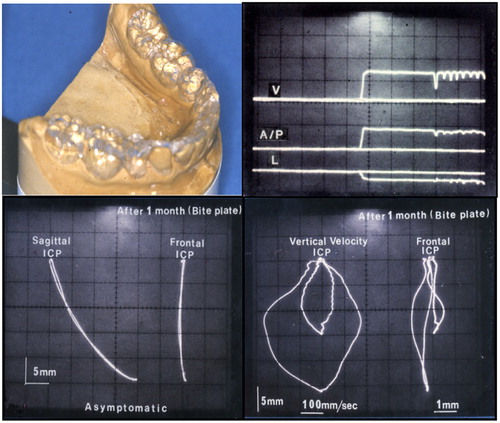
Figure 6. Posterior onlays were fabricated and seated using Panavia EX (top). Jaw movements were recorded using MKG K5 (bottom). Smooth movement to ICP with undisrupted velocity was observed.
Seven-year follow-up
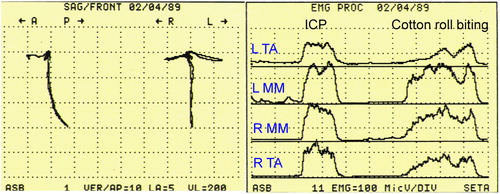
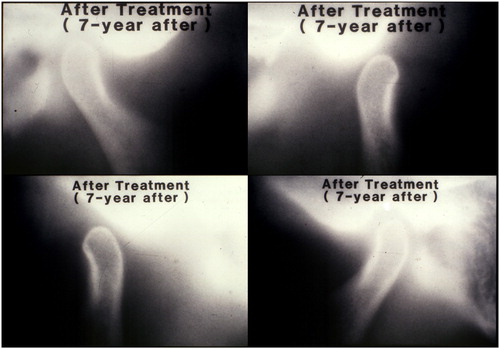
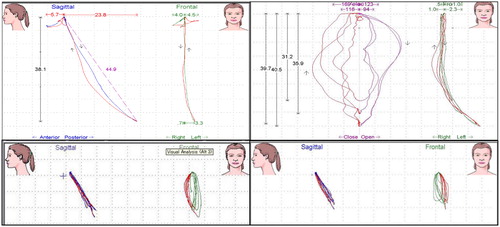
No TMD symptoms were reported. Occlusal wear of the onlay restorations was minimal (), suggesting that the established occlusion was well adapted. Hence, No occlusal adjustment was performed. Jaw movements were evaluated using the K6 diagnostic system (Myotronics). Open–close, protrusive, and lateral movements recorded in the sagittal and frontal planes were smooth ( left). Bilateral surface EMG recordings of the anterior temporalis and the middle masseters were performed using the EM-2 (Myotronics). The patient was instructed to conduct maximal clenching at ICP. Cotton rolls were placed on the occlusal surfaces of the posterior teeth bilaterally, and the patient was instructed to bite the cotton rolls hard. The action potential of EMG of anterior temporal (TA) and middle masseter (MM) muscles were also shown ( right). The first activity in EMG indicates electric discharge from masseter muscles during biting at ICP. The second activity shows muscle activity during cotton roll biting. The EMG result shows relatively symmetric burst in the masseter during clenching, minimum burst at non-clenching, and slight masseter dominance over temporalis.Citation14 These results indicated normal muscle activity of the masseter and temporalis. The radiographic assessment of TMJs affirmed that the condyle was not posteriorly positioned, rather “concentric”Citation15,Citation16 and that the condyle traveled sufficiently anteriorly at jaw opening ().
Figure 7. Intraoral photos taken at the 7-year follow-up. No substantial wear was noted on the resin-only restorations.

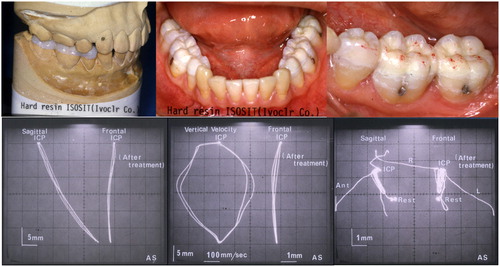
Twenty-three-year follow-up
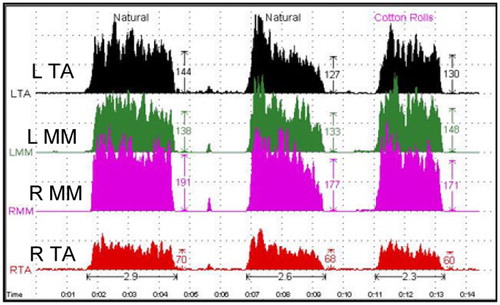
No TMD symptoms, including limited mouth opening, pain, and clicking sound, were reported. Intraorally, wear of the onlay restorations was noted. New restorations were fabricated using a hybrid composite resin material (Estenia, Kuraray) and replaced (). The replacement was completed on one side at one chair time so the established occlusion was maintained. Jaw movements were traced using the K7 computerized mandibular scanner (Myotronics). Jaw movements in sagittal and frontal planes were smooth, and no signs of disc transposition were observed, indicating that closed-lock of the left TMJ was healed ( top). Next, the patient was given chewing gum and instructed to chew. Jaw movements were recorded for the left side chewing ( bottom-left) and the right side chewing ( bottom-right). As shown in , jaw movements during gum chewing were smooth, stable, and reproducible. Bilateral EMG recordings of the anterior temporalis and the middle masseters were performed using K7 eight channel electromyography (Myotronics). The patient was instructed to perform maximal clenching at ICP followed by cotton roll bite as described above. The levels and ratios of the action potentials of EMG for the anterior belly of the temporalis and the middle masseter were normal during biting at ICP and cotton roll biting (the last activity) (), indicating that masticatory muscles functioned in harmony. Radiographic assessment of TMJs showed that the condyles were in the neutral position at ICP and traveled sufficiently anterior at maximum opening ().
Figure 11. Jaw movements were recorded by the K7 computerized mandibular scanner at the 23-year follow-up. Mandibular movements were smooth (upper-left). Velocity of movements was not consistent, but was acceptable (upper-right). Jaw movements during gum chewing were recorded: left side chewing (bottom-left) and right side chewing (bottom-right).
Thirty-year follow-up
The patient has been TMD symptom-free for the last 30 years. Neither pain nor clicking sound was reported. The patient was satisfied with her occlusion and the appearance of the restorations. The patient expressed no desire to replace her existing restorations with more esthetic restorations, such as full porcelain crowns.
Discussion
A TMD case with intermittent lock of the left TMJ was treated, based on the neuromuscular concept, and followed for 30 years. This case study shows that occlusal reconstruction based on the neuromuscular concept can be integrated into the patient’s functional occlusion system, thereby contributing to quality of life. While the established jaw position might not be the best one for this patient, it was well adapted and re-established harmonized muscle activity, jaw movements, and condyle positioning. Most importantly, the patient has been TMD symptom-free for 30 years. It must be noted, however, that this case study with a 30-year follow-up involves a single TMD patient, and therefore, may not be representative of the general TMD patient population.
In this case, the patient was offered several treatment options, including orthodontic treatment, posterior gold onlay restorations, and full-mouth esthetic restoration to establish a physiological occlusion. The advantages and disadvantages of each option were thoroughly explained. Since the patient had gone through orthodontic treatment before the TMD symptom developed, this option was not taken, and the restorative approach was considered. The patient accepted the onlay restorations using dental adhesives since this option was a minimal intervention (MI) approach. Hard composite resin onlay restorations were selected instead of gold restorations, due to esthetic concern.
The authors do not regard MTCP as an ideal jaw position, but use MTCP as a therapeutic position from which they start to look for an acceptable physiological jaw position by performing occlusal adjustments.Citation12 In neuromuscular dentistry, MCP is recommended for a therapeutic mandibular position. MCP is typically set on the TENS-stimulated mandibular movement trajectory approximately 2 mm above, and anterior to the rest position. Although MCP represents an excellent mandibular position, it often demands extensive dental work, such as full-mouth oral reconstruction. This could be a great financial burden and is a substantial intervention for patients. Therefore, there is a need to develop an effective treatment approach to establish physiological jaw position yet reduce the patients’ burden. The authors use MTCP routinely as a therapeutic mandibular position instead of MCP. MTCP position is obtained with TENS stimulation after muscle relaxation by TENS for 60 minutes. Using the MTCP position, the authors find that no anterior restorations are typically required, and new therapeutic occlusion can be established with posterior restorations only. The shift of the mandibular position from MCP to MTCP on the TENS-stimulated mandibular movement trajectory appeared to have no negative impact on treatment outcome in the authors’ experience. This could be explained by the fact that a slight alteration in occlusal vertical dimension can be adapted by a host. Most clinicians agree that lateral deviation of the mandible, even a slight shift, causes trauma in the physiological masticatory system; however, patients typically accept the new mandibular position and develop new freeway space when a slight alteration in occlusal vertical dimension is made in harmony with the musculoskeletally stable TMJs and muscles.Citation17–Citation19
When an occlusal discrepancy between the ICP and MTCP is small, occlusal therapy using a conventional bite splint would relieve orofacial pain. However, when an occlusal discrepancy is substantial, as shown in this case study, the authors thoroughly review the patient’s dental history and fabricate a CMO appliance to stabilize the patient’s neuromuscular system.Citation20 Once stabilized, fixed restorations (typically onlays) seated with dental adhesives are used for occlusal therapy. During this process, electric devices, including a mandibular kinesiography, TENS, and EMG, are used for diagnosis and assessment of the treatment outcome.Citation21,Citation22 Absolute numbers (velocity and magnitude of muscle activity) are not critical. Jaw movement smoothness, harmonized muscle activity, and reproducible trajectory are factors to carefully assess for the treatment outcome. For this purpose, the above-mentioned electric devices are useful for evaluating outcome objectively. If necessary, definitive restorations can be delivered, following enough observation time, which ascertains the adaptation of new occlusion to the patient’s physiological masticatory system. The authors’ approach is initially conservative, reversible, and therefore, safe. Advances in adhesive dentistry make this approach successful.
Disclaimer statements
Contributors AY and YK performed TMD therapy on the patient. All authors analyzed treatment outcome and JY drafted the manuscript. All authors revised the manuscript and approved the final version of the manuscript.
Funding This case report received no specific grant from any funding agencies.
Conflicts of interest None.
Ethics approval It was not required.
References
- McNeill C. Occlusion: what it is and what it is not. J Calif Dent Assoc. 2000;28:748–58.
- Agerberg G. Mandibular function and dysfunction in complete denture wearers–a literature review. J Oral Rehabil. 1988;15:237–49.
- Pullinger AG, Seligman DA, Gornbein JA. A multiple logistic regression analysis of the risk and relative odds of temporomandibular disorders as a function of common occlusal features. J Dent Res. 1993;72:968–79.
- Kirveskari P, Alanen P, Jamsa T. Association between craniomandibular disorders and occlusal interferences. J Prosthet Dent. 1989;62:66–9.
- Kloprogge MJ, van Griethuysen AM. Disturbances in the contraction and co-ordination pattern of the masticatory muscles due to dental restorations. An electromyographic study. J Oral Rehabil. 1976;3:207–16.
- Glass EG, Glaros AG, McGlynn FD. Myofascial pain dysfunction: treatments used by ADA members. J Craniomandib Pract. 1993;11:25–9.
- Glass EG, McGlynn FD, Glaros AG. A survey of treatments for myofascial pain dysfunction. J Craniomandib Pract. 1991;9:165–8.
- Turp JC, Schindler H. The dental occlusion as a suspected cause for TMDs: epidemiological and etiological considerations. J Oral Rehabil. 2012;39:502–12.
- Mejersjo C, Carlsson GE. Analysis of factors influencing the long-term effect of treatment of TMJ-pain dysfunction. J Oral Rehabil. 1984;11:289–97.
- Konchak PA, Thomas NR, Lanigan DT, Devon RM. Freeway space measurement using mandibular kinesiograph and EMG before and after TENS. Angle Orthod. 1988;58:343–50.
- Jankelson B, Sparks S, Crane PF, Radke JC. Neural conduction of the Myo-monitor stimulus: a quantitative analysis. J Prosthet Dent. 1975;34:245–53.
- Bracco P, Deregibus A, Piscetta R. Effects of different jaw relations on postural stability in human subjects. Neurosci Lett. 2004;356:228–30.
- Cooper BC, Kleinberg I. Establishment of a temporomandibular physiological state with neuromuscular orthosis treatment affects reduction of TMD symptoms in 313 patients. J Craniomandib Pract. 2008;26:104–17.
- Cooper BC. The role of bioelectronic instrumentation in the documentation and management of temporomandibular disorders. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;83:91–100.
- Lau KU, Green WF 2nd. Orthosis thickness and its effect on temporomandibular joint space. J Craniomandb Pract. 2003;21:209–20.
- Knoernschild KL, Aquilino SA, Ruprecht A. Transcranial radiography and linear tomography: a comparative study. J Prosthet Dent. 1991;66:239–50.
- McNamara JA Jr. Functional adaptations in the temporomandibular joint. Dent Clin North Am. 1975;19:457–71.
- Carlsson GE, Ingervall B, Kocak G. Effect of increasing vertical dimension on the masticatory system in subjects with natural teeth. J Prosthet Dent. 1979;41:284–9.
- Ormianer Z, Gross M. A 2-year follow-up of mandibular posture following an increase in occlusal vertical dimension beyond the clinical rest position with fixed restorations. J Oral Rehabil. 1998;25:877–83.
- Dinham GA: Myocentric. A clinical appraisal. Angle Orthod. 1984;54:211–7.
- Monaco A, Cattaneo R, Marci MC, Marzo G, Gatto R, Giannoni M. Neuromuscular diagnosis in orthodontics: effects of TENS on maxillo-mandibular relationship. Eur J Paediatr Dent. 2007;8:143–8.
- Pinheiro PF Jr, da Cunha DA, Filho MG, Caldas AS, Melo TM, da Silva HJ. The use of electrognathography in jaw movement research: a literature review. J Craniomandib Pract. 2012;30:293–303.