Introduction
An erythrocytosis is a condition in which there are too many red cells in the body. Red cells are disc-shaped cells which are made in the bone marrow. They are full of a protein, haemoglobin, the protein which carries oxygen round the body and thus oxygen is transported from the lungs to the tissues where it is needed. The oxygen supply to tissues is controlled by the oxygen carrying capacity of haemoglobin which in turn is reflected by the number of red cells.
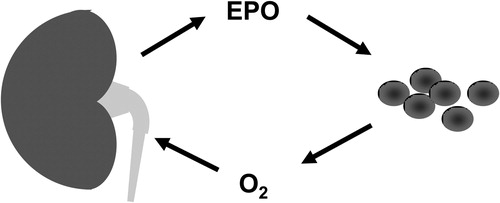
This system is carefully balanced to detect oxygen requirements and produce more red cells in response to increasing oxygen needs. A hormone erythropoietin (EPO) is produced by the kidney in response to changes in oxygen levels and this hormone drives red cell production ().
Figure 1. Oxygen (O2) levels are detected by the kidney which in response to lack of O2 secrets erythropoietin (EPO) into the circulation. This hormone drives red cell production.
The normal red cell count is mirrored by a normal haemoglobin and haematocrit or packed cell volume. A haemoglobin above 185 g/l or a haematocrit above 0.52 in a male or a haemoglobin above 165 g/l or a haematocrit above 0.48 in a female may be indicative of an increase in the number of red cells or the red cell mass known as an erythrocytosis. This is also sometimes referred to as polycythaemia.
Causes
An erythrocytosis can be congenital where it is something which the individual is born with or acquired where some change occurs later in life. The erythrocytosis is described as primary where the cause of the increased red cell production arises because of a defect in the bone marrow and secondary when a secondary cause or something else outside the bone marrow, usually mediated in some way by EPO production, is driving the red cell production.
There are many causes of secondary erythrocytosis from simple reasons for a shortage of oxygen such as living at high altitude or heavy smoking, to rare tumours producing EPO, rare genetic defects in the protein pathways which detect oxygen levels leading to increased EPO production, to deliberate administration of EPO by unscrupulous sportsmen who wish to increase their natural oxygen carrying capacity. A full list of causes of erythrocytosis is detailed in .
Table 1. Causes of an erythrocytosis
Symptoms and signs
Many patients have no symptoms or signs of erythrocytosis. The potential abnormality is discovered when a blood count is carried out for other reasons. Patients may complain of various problems such as itch although this is most usually associated with the primary acquired disorder polycythaemia vera. They may be noticed to have a high colour.
An erythrocytosis may cause thickening of the blood or hyperviscosity. This hyperviscosity can be associated with a diverse range of symptoms such as myalgia and weakness, fatigue, headache, blurred vision, and slowing of mental activity.
Patients with hyperviscosity may be at increased risk of thromboembolic or clotting events.
Tests
The first test undertaking is repetition of the full blood count to confirm the likely presence of an erythrocytosis over time. Testing may then proceed to document further if the red cell mass is truly increased. Investigation will then examine to see is the erythrocytosis is primary or secondary by measuring the EPO levels and investigating for a secondary cause. A careful history and examination should always be conducted and any leads from this as to a possible cause are then investigated further by the appropriate test. There are a large number of investigations which can be undertaken but the order and sequence depends on the clinical presentation. A bone marrow examination may be considered.
Treatment options
Any secondary cause for an erythrocytosis should itself be treated if this is possible.
Further treatment should consider reducing any other risk factors for thromboembolic events such as smoking cessation, control of hypertension, hypercholesterolaemia, or any other risk factors.
The blood viscosity can be reduced by venesection (removal of blood). The amount and frequency of venesection depends on the clinical situation and the patient's symptoms.
Low dose aspirin can also be considered as a method of reducing the thromboembolic risk.
Outlook
The outlook for many patients is dictated by the outlook for the secondary erythrocytosis for instance in a patient with erythrocytosis due to respiratory disease the outlook will depend on the prognosis for the respiratory disease. There is little information available on outlook for congenital secondary erythrocytosis as these cases are very rare; however, perhaps it is worth stating that there is no increased risk of any malignant transformation.
Additional resources
Resources are available for the myriad secondary causes of erythrocytosis. For the myeloproliferative disorders patient websites such as MPD-voice (http://www.mpdvoice.org.uk) is certainly worth a visit but this is focussed on these primary haematological disorders. The website of the MPN&MPNr-EuroNet COST Action BM0902 which is an EU sponsored Network of Experts on the Molecular Diagnosis of Myeloproliferative Neoplasm (MPN)and MPN-related congenital diseases (MPNr) (http://www.mpneuronet.eu/) provides a lot of useful information on diagnostic testing and training for professionals in myeloproliferative disorders including rare congenital erythrocytosis.
