Abstract
Objective
To develop a calibrated item bank and computer adaptive test (CAT) to assess the effects of stigma on health-related quality of life in individuals with spinal cord injury (SCI).
Design
Grounded-theory based qualitative item development methods, large-scale item calibration field testing, confirmatory factor analysis, and item response theory (IRT)-based psychometric analyses.
Setting
Five SCI Model System centers and one Department of Veterans Affairs medical center in the United States.
Participants
Adults with traumatic SCI.
Main Outcome Measures
SCI-QOL Stigma Item Bank
Results
A sample of 611 individuals with traumatic SCI completed 30 items assessing SCI-related stigma. After 7 items were iteratively removed, factor analyses confirmed a unidimensional pool of items. Graded Response Model IRT analyses were used to estimate slopes and thresholds for the final 23 items.
Conclusions
The SCI-QOL Stigma item bank is unique not only in the assessment of SCI-related stigma but also in the inclusion of individuals with SCI in all phases of its development. Use of confirmatory factor analytic and IRT methods provide flexibility and precision of measurement. The item bank may be administered as a CAT or as a 10-item fixed-length short form and can be used for research and clinical applications.
Introduction
Spinal cord injury (SCI) involves damage to the spinal cord from external traumaCitation1 such as a motor vehicle crash, fall, or gunshot wound. Most individuals who experience an SCI lose some level of function in their limbs, resulting in dependence on mobility aids – most commonly, manual or power wheelchairs.Citation2 Frequent secondary complications of SCI include bowel, bladder, and sexual dysfunction,Citation2 chronic pain, fatigue, and mood disturbance.Citation3–Citation5 Social participation, or the ability to be involved and engaged in life situationsCitation6 such as those related to family and friends, vocation, and leisure activities – may be quite restricted. Given the visible consequences of SCI, the experience of stigma in social settings can be profound and may have detrimental effects on individuals’ health-related quality of life (HRQOL).Citation4,Citation7–Citation9
Individuals with physical disabilities such as SCI are a minority group and stand out from the population because of their physical limitations.Citation8 SusmanCitation10 describes the relationship between stigma and disability in detail, emphasizing that disabling conditions are stigmatizing to the extent that they elicit negative responses. SCI-related stigma is a result of the visibility of the condition as well as the degree that a person is dependent on help. When communicating in group settings, wheelchair-using individuals often express feelings of being dismissed as if their physical disability is also a mental disability, and report being spoken to as though they cannot comprehend.Citation7,Citation11 These findings were confirmed in unpublished focus group data described by Tulsky et al.,Citation12 wherein participants with SCI described feeling invisible yet conspicuous at the same time and also reported being spoken to slowly, as if their wheelchair was the sign of a cognitive impairment. These examples are the epitome of stigma.
The concept of stigma, signifying a mark of shame or discredit both from one's own internalized attributions, as well as from the perceptions of others, has a long ancestry in the social sciences. Erving Goffman proposed that people are stigmatized when they possess an attribute that is considered undesirable and ‘deeply discrediting.’ Goffman's work identified three aspects of stigma: character blemishes, features of identity (e.g. race, religion, sexual preference) and physical ‘deformities’ such as disability.Citation13 The societal response to such attributes may include labeling, stereotyping, and/or discrimination.Citation14 Though Goffman's seminal work was published over 60 years ago, it is almost universally referenced in modern publications on health- or disability-related stigma.
Several theories surrounding the course of stigma exist in the literature. Goffman suggested that an individual is stigmatized by society when others can see the disabilityCitation13 and all visible disabilities or undesirable physical characteristics are certain to be stigmatized. In contrast, Schneider postulated that the state of being stigmatized was dependent on whether the individual chose to see him/herself in that way.Citation15 These two views compliment a more recent conceptualization in which stigma development involves three distinctions: enacted stigma, perceived (or felt) stigma, and internalized stigma.Citation16–Citation18 Enacted stigma refers to episodes of discrimination and misconduct (e.g. stereotyping, labeling) towards someone who is in a stigmatized group. Perceived stigma describes one's awareness of enacted stigma and can create isolation or exclusion from normal activities, while internalized stigma implies agreement with enacted stigma and a sense of shame from it.Citation19
Health-related stigma is based on negative characteristics of a health condition or state.Citation20 In the last several decades, there has been a great deal of research on the impact of stigma on individuals with conditions such as HIV/AIDS, cancer, mental illness and epilepsy. For example, a recent study examining the effects of stigma on individuals with epilepsy found perceived stigma to negatively impact physical, mental and social health outcomes.Citation14 Unfortunately, though cross-cultural studies suggest that the consequences of stigma are similar across health conditions,Citation20 data on the impact of stigma on individuals with SCI are sorely lacking.
Knowledge on the effects of stigma on individuals with SCI is hindered by the lack of available patient-reported outcomes (PRO) measures of stigma for use in individuals with SCI. The Short Form Health Survey (SF-36),Citation21 Sickness Impact Profile (SIP), Life Satisfaction Questionnaire (LISAT-9/-1), Satisfaction with Life Scale (SWLS),Citation22 and the 26-item version of the World Health Organization Quality of Life Scale (WHOQOL-BREF)Citation23 have demonstrated reliability and validity when used in individuals with SCI, but have been developed with the general population and contain items across a wide range of physical, emotional, and social health. While useful, these instruments do not address the myriad of elements unique to SCI, and, most importantly, none assess stigma specifically.
There also exist a variety of measures intended to assess the objective existence and extent of stigma towards individuals with various types of disabilities including, most notably, the Scale of Attitudes Toward Disabled Persons.Citation24 However, many would argue that it is the subjective experience of stigma that can affect HRQOL. As such, it is important to assess SCI-related stigma from the individual with SCI's own perspective. There are numerous scales measuring the subjective experience of stigma in individuals with a variety of chronic health conditions such as mental illness (e.g. Perceived Devaluation and Discrimination Scale,Citation25 Internalized Stigma of Mental Illness,Citation26 Self-stigma of Mental Illness Scale),Citation27 HIV/AIDS (e.g. HIV Stigma Scale),Citation28 and epilepsy (e.g. Stigma Scale of Epilepsy).Citation29 These scales do focus on many aspects of stigma (e.g. perceived discrimination, enacted discrimination, alienation) that would seem to have face validity for individuals with SCI, however none have been used in SCI research. Therefore, their psychometric properties in individuals with SCI cannot be determined.
A recent National Institutes of Neurological Disorders and Stroke (NINDS) sponsored initiative (Neuro-QOL) developed a calibrated item bank of stigma in individuals with neurological disorders (i.e. stroke, epilepsy, multiple sclerosis, amyotrophic lateral sclerosis, and Parkinson's disease).Citation30,Citation31 However, individuals with SCI were not included in the development, calibration, or validation of this item bank, and most neurological disorders do not share the same level of visibility and cultural image of SCI. A primary goal of the spinal cord injury quality of life (SCI-QOL) initiative has been to adapt the Neuro-QOL for an SCI population. In the first phase of the SCI-QOL study, individuals with SCI cited SCI-related stigma as having a detrimental effect on HRQOL.Citation12 Thus, the research team prioritized the development of an optimized version of the Neuro-QOL Stigma item bank for use in individuals with SCI. This manuscript details the development and calibration of the SCI-QOL Stigma item bank.
Methods
Item development
The first phase of the project included development of new PRO items and evaluation of existing Neuro-QOL items for use in individuals with SCI.Citation32 A variety of qualitative methods were used to identify the most salient aspects of SCI-related stigma.
Individual interviews
A series of individual semi-structured interviews were conducted with 44 individuals with SCI.Citation33 Participants were placed in the role of ‘expert’ and asked to list topics or issues that were important to address when assessing HRQOL in individuals with SCI. Participants discussed issues related to stigma such as being treated differently or unfairly because of their disability, not feeling accepted in social settings, and feeling pitied by others. Twenty-two items were written based on these comments.
Focus groups
The overarching themes that arose from the individual interviews served as a basis for more in-depth examination of physical-medical, emotional, and social components of HRQOL through a series of focus groups with community-dwelling individuals with SCI (12 groups; n = 65) and SCI clinicians (4 groups; n = 42) which were led by an experienced moderator (DV).Citation12 Groups with individuals with SCI focused on one major HRQOL domain, either physical-medical, emotional, or social health, while provider groups covered all domains. Participants in all groups were asked open-ended questions about the definition of HRQOL and the ways in which an SCI could impact HRQOL. Participants were also asked to review and provide feedback on existing HRQOL domains and subdomains. A detailed grounded-theory based qualitative analysis of focus group transcripts was conductedCitation34 and within the broader domain of social health and participation, 10% of consumer comments and 6% of clinician comments were related to stigma. These comments were then reworded as 12 PRO items to form the initial basis of the SCI-QOL Stigma item pool. The project team made a decision to include only those items related to enacted and perceived stigma, or the way an individual believes they are being perceived or treated by others, in the new measure of SCI-related stigma. In contrast, items related to internalized stigma, or one's perception of oneself, were included in the Self-Esteem item bankCitation35 which assesses myriad aspects of an individual's self-appraisal.
Inclusion of Neuro-QOL items
One of the primary aims of the SCI-QOL project was to optimize the Neuro-QOL measurement system for individuals with SCI. Thus, all Neuro-QOL stigma items were reviewed for content and potential inclusion in the SCI-QOL Stigma bank. The Neuro-QOL items that captured perceived or enacted stigma (e.g. ‘Because of my illness, strangers tended to stare at me’) were adapted and reworded to fit an SCI population. Conversely, Neuro-QOL Stigma items related more to internalized Stigma or self-appraisal (e.g. ‘I was unhappy about how my illness affected my appearance’) were moved to the Self-Esteem bank. Individuals with SCI are not sick and do not have an ‘illness,’ so all Neuro-QOL Stigma items containing the phrase ‘because of my illness’ were modified with permission to ‘because of my injury’ for use in the SCI-QOL. The preliminary pool of SCI-QOL Stigma items was largely based on the Neuro-QOL Stigma bank, with 24 verbatim items included. In every case of a ‘new’ (i.e. derived from focus groups or individual interviews) item with similar content to a Neuro-QOL item, the Neuro-QOL item was retained and the new item discarded. The Neuro-QOL Stigma domain definitionCitation36 was adapted for an SCI population as follows: ‘Others’ perceptions of oneself and publically enacted negativity, prejudice, and discrimination as a result of injury-related manifestations.’
Item refinement
A thorough qualitative item reviewCitation37,Citation38 was conducted on all ‘new’ (i.e. not from Neuro-QOL) items. Initially, project co-investigators with expertise in social and emotional issues related to SCI reviewed all of the ‘new’ items, making suggestions for revisions and deletions as appropriate. Items in the initial pool were revised to optimize wording, eliminate redundancies, and ensure consistency with the domain definition. All retained ‘new’ items were also rephrased for consistency with the Neuro-QOL Stigma item context of ‘Lately’ and the response set of ‘Never /Rarely /Sometimes /Often /Always.’ Next, a series of cognitive debriefing interviewsCitation39 was conducted with individuals with SCI (n = 5 per item).Citation33 Participants were asked to rephrase items in their own words and to describe their decision-making and response retrieval processes. Once the study team incorporated cognitive interview feedback into the item pool, all ‘new’ items underwent a translatability reviewCitation40 to flag wording that would be problematic to translate into Spanish. The last step to prepare the item pool for calibration testing was to conduct a reading level review using the Lexile FrameworkCitation41 to ensure that all items were written at or below a 5th grade reading level. A final pool of 30 items (24 Neuro-QOL items and 6 new items) was utilized for the calibration field testing phase of the project.
Calibration field testing
Sample
Adults with traumatic SCI were recruited from 6 collaborating centers including 5 SCI Model Systems (SCIMS) centers (University of Michigan, Kessler Institute for Rehabilitation/Kessler Foundation, Rehabilitation Institute of Chicago, Craig Hospital, University of Washington) and one Department of Veterans’ Affairs (VA) center (the James J. Peters/Bronx VA). Care was taken to recruit a heterogeneous sample, balanced across diagnosis (paraplegia vs. tetraplegia), severity (complete vs. incomplete injury) and time since injury (<1 year, 1–3 years, >3 years). We did not stratify by gender since the SCI population is predominantly (i.e. approximately 79%) male.Citation42 Inclusion criteria were traumatic etiology of injury, ability to speak and understand English, and age 18 years or older at the time of study participation. Level and etiology of injury and American Spinal Injury Association (ASIA) Impairment Scale (AIS)Citation43 grade were documented through medical record review.
Procedure
The thirty Stigma items were administered with other SCI-QOL items in interview format by trained study personnel using a customized web-based administration platform. Response cards depicting the appropriate response set for each item bank were placed in front of the participant (if in person) or provided to the participant by mail and/or email (if via phone). Interviewers read the items from the computer screen aloud and recorded the participants’ responses which were uploaded in real time. The Institutional Review Board at each participating center reviewed and approved this study.
Analysis
There are two key assumptions underlying the successful application of IRT to any pool of items. First, the pool of items must be essentially unidimensional (i.e. assess a single dominant construct). Items within a unidimensional pool must also be locally independent, that is, the only factor affecting the response to any one item given the response to any other item is the level of the underlying trait in question.Citation44,Citation45 For this study, confirmatory factor analyses with MPlus version 6.0a were conducted to assess fit to a unidimensional model. Several indices of goodness-of-fit were considered. The Tucker-Lewis Index (TLI) is a non-normed fit index which adjusts for the number of degrees of freedom in the model. TLI values above 0.9 are considered good fit and values above 0.95 indicate excellent fit. The comparative fit index (CFI) is a normed fit index which compares the current model to a null or independent model. Possible CFI values range from 0.0 to 1.0, with values above 0.9 indicating good fit and values above 0.95 indicating excellent model fit. The root mean square error of approximation (RMSEA), which divides the F statistic by degrees of freedom to compensate for model complexity, was also used to assess fit to the unidimensional model. When interpreting the RMSEA, perfect fit would be indicated by a value of 0, with commonly accepted cutoff criteria of 0.08 for acceptable fitCitation46 and 0.05 for excellent fit.Citation47 To assess adherence to the IRT assumption of local independence, items were evaluated for local item dependence (LID). Item pairs exhibiting a residual correlation >|0.2| were flagged and at least one of the items was removed from the item pool.
Item slope (discrimination) and threshold (difficulty) parameters were estimated using the graded response IRT model (GRM).Citation48 The S-X2 test using the IRTFITCitation49 macro program was used to further evaluate item fit, with P < 0.05 indicating poor fit and P < 0.01 necessitating item removal. Finally, differential item functioning (DIF) analyses were conducted using lordifCitation50 to examine whether any included items exhibited bias towards any demographic or diagnostic subgroup. DIF analyses identify items that exhibit a difference in item response functions depending on injury subgroup or demography. The most important indicator of DIF is not whether items systematically differentiate relevant subgroups, but whether they do so even after controlling for the level of the underlying trait (e.g. stigma).Citation51 DIF was examined for six categories: age (≤49 vs ≥50), sex (male vs female), education (some college and lower vs college degree and above), diagnosis (tetraplegia vs. paraplegia), severity (incomplete vs. complete), and time post injury (>1 year vs. <1 year). Items were flagged if the probability associated with the χ2 test <0.01 and McFadden's pseudo R2 effect size >0.02 (a small but non-negligible effect).
Transformation to Neuro-QOL metric
Once developed, the initial IRT parameters for the final bank of Stigma items underwent a linear transformation to the Neuro-QOL metric so that SCI-QOL Stigma scores reference the same general neurological population as do the Neuro-QOL Stigma scores. The linking procedure, described by Tulsky et al.,Citation33 consisted of 6 steps. First, the linking configuration was determined through counts of calibration and anchor items Anchor and calibration parameters were then identified for matched items. Linking was conducted using the Stocking and LordCitation52 method. Scatter plots of item parameters and item response plots were created/examined for anchor items, transformation constants were estimated, and the initial item parameters were modified accordingly.
Short form development
For each SCI-QOL item bank, a short, fixed-length form has been developed. These ‘short forms’ provide a paper-and-pencil alternative to CAT administration. Project co-investigators considered both clinical relevance and psychometric item characteristics in the selection of short form items IRT parameters of slope (discrimination) and thresholds (difficulty) were examined. The most informative 1–2 items (i.e. those with the highest slopes) were chosen within each quintile of difficulty. Investigators then considered clinical relevance and similarity to other included items in deciding whether to retain those items selected for their psychometric characteristics, or whether to replace any of them with items with slightly lower slopes.
Reliability study
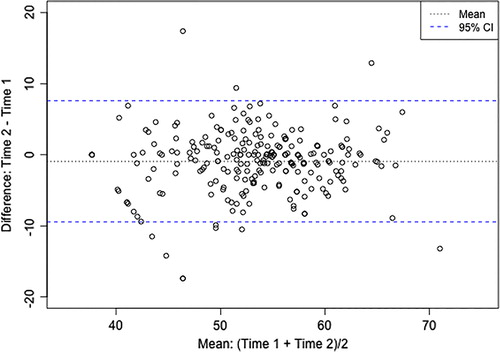
A reliability study has been conducted with individuals with traumatic SCI as a part of an ongoing effort to quantify the psychometric properties of the SCI-QOL item banks. Participants recruited from 4 SCI Model Systems rehabilitation centers completed the SCI-QOL Stigma CAT and short form at baseline and 1–2 weeks. To assess test-retest reliability, Pearson's r and the intraclass correlation coefficient, ICC(2,1),Citation53,Citation54 were calculated and a Bland-Altman plot was developed.
Results
Participant characteristics
Detailed demographic information on focus group participants (n = 65 individuals with SCI and 42 SCI clinicians)Citation12 and on participants in the reliability study (n = 245 individuals with SCI)Citation33 has been published and is not repeated here. A total of 611 participants with traumatic SCI completed the SCI-QOL stigma items as a part of the large-scale SCI-QOL calibration study. Demographic and injury-related information on the calibration sample is summarized in .
Table 1. Demographic and Injury Characteristics of Calibration Sample
Analysis
A total of 3 CFA iterations were run. Five items were removed following the first iteration due to sparse data (i.e. fewer than 4 responses) in one or more categories (3 items) or low item-total correlations (2 items). Two of the removed items exhibited a category inversion whereby the mean raw score for individuals selecting category 5 was lower than for individuals selecting category 4. Following the second iteration of CFA, two additional items were removed for LID.
CFA analyses confirmed fit to a unidimensional model. CFI for the final 23-item bank was 0.941, TLI was 0.935, and RMSEA was 0.088. Item loadings on the single factor were acceptable with R2 for 17 items > 0.4, R2 for 4 items between 0.3 and 0.4, and R2 for 2 items approaching 0.3 (0.269 and 0.0292, respectively). No item pairs exhibited LID. Descriptive statistics on each of the 23 final items are located in .
Table 2. SCI-QOL Stigma Bank: Descriptive Item Statistics
The final 23-item bank has a Cronbach's alpha value of 0.936. Item-total correlations range from 0.39 to 0.72. All of the items had more than 25% of the sample selecting category 1 (‘Never’) and less than 12% selecting category 5 (‘Always’).
Graded response model IRT analyses yielded slope values for the 23 items ranging from 1.10 to 2.87, with thresholds ranging from −0.87 to 3.95. Measurement precision in the theta range between –0.5 and 2.4 was roughly equivalent to a classical reliability of 0.95 or better. The S-X2 model fit statistics indicated adequate or better model fit statistics for all but one item at α = 0.05 and all items at α = 0.01. 11 items were flagged for DIF in at least one category based on the chi-square test; however, when the effect size measures were examined, the DIF was negligible. The 18 retained Neuro-QOL items served as ‘anchors’ to conduct the transformation of item parameters to the Neuro-QOL metric. Following transformation, slope values for the 23 items ranged from 1.81 to 4.72 and thresholds ranged from –0.16 to 2.77 (see ). Mean (SD) of the sample shifted from 49.82 (9.66) before transformation to 53.18 (6.69) after transformation.
Table 3. SCI-QOL Stigma Items and Item Bank Parameters
The SCI-QOL Stigma bank demonstrates excellent reliability. Using the calibration data (n = 611), Cronbach's α = 0.936 for full bank administration and α = 0.895 for the 10-item short form. Furthermore, the correlation (Pearson's r) between the baseline and 1–2 week retest assessments was 0.80 for the CAT (n = 245; P < 0.001) and 0.84 for the 10-item short form (n = 168; P < 0.001). ICC (2,1) was 0.79 (95% CI: 0.74 to 0.84) and a Bland-Altman plot is provided as .
Assessment center programming and short form item selection
The IRT parameters for each final SCI-QOL Stigma item were programmed into the Assessment CenterSMCitation55 platform, where the full bank, CAT, and a brief, fixed-length ‘short form’ are available free of charge (see www.assessmentcenter.net). A total of 10 items were selected for the initial SCI-QOL Stigma short form (SF). In keeping with the naming conventions of the Patient Reported Measurement Information System (PROMIS), this form is called the SCI-QOL v1.0 Stigma SF10a. Short form items are indicated by bold text in Tables and .
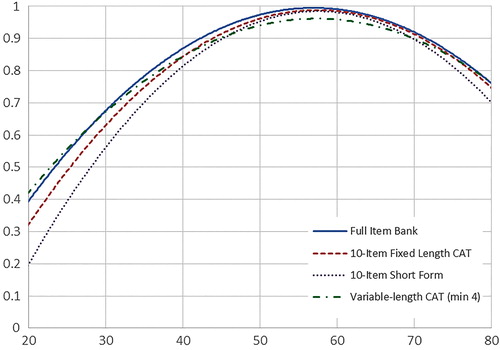
When administered as a CAT, by default Assessment Center will administer a minimum of 4 items and will continue to administer items until the standard error of measurement (SEM) falls below 0.3 or the maximum of 12 items is reached. Users may also modify these CAT parameters to ensure that participants complete a shorter or longer CAT. A comparison of the measurement precision of the full Stigma item bank, the Stigma CAT, and the Stigma SF10a can be found in . Furthermore, reliability curves for full bank, CATs of varying lengths, and SF are located in .
Table 4. Accuracy of Variable and Fixed-Length CAT and 10-item Short Form: Correlations with Full-bank score
Scoring
Higher scores on the Stigma bank indicate a greater degree of perceived stigma. Though SCI-QOL scores were originally developed with a reference population of individuals with traumatic SCI, the transformation to the Neuro-QOL metric yields final standardized scores which now reference the mean of a broader population of individuals with neurological disorders. The Neuro-QOL normative sample for the Stigma item bank included 511 adults with stroke (n = 209), epilepsy (n = 183), Parkinson's disease (n = 50), multiple sclerosis (n = 84), and amyotrophic lateral sclerosis (n = 18) (diagnoses are not mutually exclusive).Citation37 Consequently, SCI-QOL Stigma scores are directly comparable to Neuro-QOL Stigma scores. For CAT administration, Assessment Center automatically transforms IRT-based scaled scores (theta values) into standardized T-scores (mean 50, SD 10). The short form does, however, need to be scored manually. Scores should be produced only for individuals who have completed all 10 items, and are computed by summing the responses to each of the items The lookup table provided as can then be used to transform the raw score to the corresponding IRT-based T-score. A comparison of the range of scores and standard errors for the full bank, CAT, and SF administrations is located in .
Table 5. T-score lookup table for SCI-QOL Stigma SF10a
Table 6. Breadth of Coverage for Variable Length CAT, Fixed Length CAT, 10-Item Short Form, and Full Item Bank
Discussion
Stigma, or societal negativity, prejudice, or discrimination is a significant HRQOL concern of many individuals with SCI. To date, there have not been not been any measures of Stigma targeted to individuals with SCI, and the SCI-QOL Stigma bank addresses an overlooked need in rehabilitation outcomes assessment for individuals with SCI. Though the Neuro-QOL developed a calibrated bank of Stigma items, these items were not developed or tested with individuals with SCI and furthermore contained the phrase ‘because of my illness’ which individuals with SCI reported as inappropriate and problematic to respond to. Several Neuro-QOL items did not perform well in an SCI population (e.g. ‘I felt embarrassed about my speech’) whereas other important issues (e.g. ‘I was discriminated against’) are not addressed by Neuro-QOL. Additionally, Neuro-QOL included items related to one's perception of oneself alongside items related to the perceptions of the attitudes and behaviors of others; the SCI-QOL has tried to improve upon this conceptualization given the highly visible nature of SCI. Items related to appraisals or perceptions of oneself have been omitted from the SCI-QOL Stigma bank and have instead been included in a new bank of SCI-QOL items specifically related to valuations of one's competence and self-worth, or Self-Esteem.Citation35
Developing and revising the SCI-QOL Stigma items based largely on the input of individuals with SCI and SCI clinicians has helped to ensure that the final SCI-QOL Stigma bank is conceptually grounded to relevant and important aspects of Stigma for the SCI population. It is worth noting, however, that developing items based on feedback from individuals with SCI does not mean that these items are only appropriate for individuals with SCI or that the items themselves could not be equally relevant for other disability populations (e.g. traumatic brain injury, multiple sclerosis). Conducting the calibration testing solely with individuals with SCI, though, has optimized the relevance of CAT-selected items for individuals with SCI. Furthermore, utilizing a linear transformation to place the item calibrations on the Neuro-QOL metric facilitating instantaneous comparison with the larger population of individuals with neurological disorders. The combination of qualitative item development and refinement methods used in conjunction with advanced psychometrics puts the SCI-QOL Stigma item bank at the cutting edge of test development.
Future research should ascertain if this item bank could be used to detect individuals at risk for poor psychosocial adjustment or if the perception of stigma is a state which could be treated. The SCI-QOL Stigma bank is not meant to be used as a diagnostic tool but rather to help researchers and clinicians assess and understand the impact of SCI-related stigma on individuals’ HRQOL. The SCI-QOL Stigma CAT or short form could be included as an outcome variable in clinical trials or intervention research and may also be used clinically to better direct therapy and treatment.
Study limitations and future directions
A potential challenge faced by the SCI-QOL project team was the difficulty of creating a unidimensional assessment tool – a prerequisite for IRT analyses and CAT programming – while accurately representing multiple facets (e.g. perceived, enacted) of a construct such as stigma. There was some precedent to including them in a single item bank as the Neuro-QoL team had found that the items conformed to a unidimensional model. The SCI-QOL project team also wanted to include the most important aspects of stigma and see if the items conformed to a unidimensional model. Another challenge is that Neuro-QOL items were reworded, changing ‘illness’ to ‘injury,’ and an assumption was made that they would be psychometrically equivalent. We also felt that it is important to allow users a way to compare the SCI-QOL Stigma to the Neuro-QoL Stigma score to allow comparison across neurologic conditions. Therefore, we transformed the SCI-QOL Stigma scores to the Neuro-QOL metric as we had done in other groups.Citation33 Further work examining the possible effect of this wording change is important to do in future research to determine if the items are still measuring the same thing. Also, we had redefined our construct of Stigma and had removed some Neuro-QOL items related to how an individual feels about themselves (a construct we call Self Esteem),Citation35 further testing to examine if the underlying construct between the Neuro-QOL Stigma and SCI-QOL Stigma has changed.
Other future directions include examination of responsiveness of the SCI-QOL Stigma item bank to change over time, development of clinically relevant classifications of SCI-QOL Stigma scores, and assessment of convergent and divergent validity with other measures.
Conclusions
The SCI-QOL Stigma item bank is a psychometrically sound measurement tool which can reliably estimate HRQOL effects of SCI-related stigmatization in an SCI population. The Stigma CAT and SF are readily available for use in both research and clinical settings.
Suppliers
Mplus Statistical Analysis with Latent Variables User's Guide [computer program]. Version 6. Los Angeles: Muthen & Muthen; 2007.
Disclaimer statements
Contributors All authors have contributed significantly to the design, analysis and writing of this manuscript. The contents represent original work and have not been published elsewhere. No commercial party having a direct financial interest in the results of the research supporting this article has or will confer a benefit upon the authors or upon any organization with which the authors are associated.
Funding All SCI-QOL items and parameters are © 2015 David Tulsky and Kessler Foundation. All rights reserved. All SCI-QOL items originally from Neuro-QOL are © 2008–2013 David Cella on behalf of the National Institute for Neurological Disorders and Stroke (NINDS). All items are freely available to the public via the Assessment Center platform (www.assessmentcenter.net). There are currently no plans for Dr Tulsky, Kessler Foundation, or the NINDS to profit from the use of the copyrighted material.
Conflicts of interest This study was supported by grant #5R01HD054659 from the National Institutes of Health – Eunice Kennedy Shriver National Institute of Child Health and Human Development/National Center on Medical Rehabilitation Research and the National Institute on Neurological Disorders and Stroke.
Ethics approval None
References
- Taber CW, Venes D. Taber's cyclopedic medial dictionary. F.A Davis.
- O'Connor DL, Young JM, Saul MJ. Living with paraplegia: tensions and contradictions. Health Soc Work 2004;29(3):207–18.
- Pearce JM. Psychosocial factors in chronic disability. Med Sci Monit 2002;8(12):RA275–81.
- Migliorini C, Tonge B, Taleporos G. Spinal cord injury and mental health. Aust N Z J Psychiatry 2008;42(4):309–14.
- Fann JR, Bombardier CH, Richards JS, Tate DG, Wilson CS, Temkin N, Depression after spinal cord injury: comorbidities, mental health service use, and adequacy of treatment. Arch Phys Med Rehabil 2011;92(3):352–60.
- World Health Organization. International Classification of Functioning, Disability, and Health (ICF). Geneva: World Health Organization; 2008.
- Manns PJ, Chad KE. Components of quality of life for persons with a quadriplegic and paraplegic spinal cord injury. Qual Health Res 2001;11(6):795–811.
- Tyrrell AC, Hetz SP, Barg CJ, Latimer AE. Exercise as stigma management for individuals with onset-controllable and onset-uncontrollable spinal cord injury. Rehabil Psychol 2010;55(4):383–90.
- Wang C. Culture, meaning and disability: injury prevention campaigns and the production of stigma. Soc Sci Med 1992;35(9):1093–102.
- Susman J. Disability, stigma and deviance. Soc Sci Med 1994;38(1):15–22.
- Joachim G, Acorn S. Stigma of visible and invisible chronic conditions. J Adv Nurs 2000;32(1):243–8.
- Tulsky DS, Kisala PA, Victorson D, Tate D, Heinemann AW, Amtmann D, Developing a contemporary patient-reported outcomes measure for spinal cord injury. Arch Phys Med Rehabil 2011;92(10):S44–S51.
- Goffman E. Stigma. Notes on the Management of Spoiled Identity. Englewood Cliffs, New Jersey: Prentice-Hall; 1963.
- Viteva E. Impact of stigma on the quality of life of patients with refractory epilepsy. Seizure 2013;22(1):64–9.
- Schneider JW, Conrad P. In the closet with illness: epilepsy, stigma potential and information control. Soc Prob 1980;28(1):32–44.
- Jacoby A. Epilepsy and stigma: an update and critical review. Curr Neurol Neurosci Rep 2008;8(4):339–44.
- Fife BL, Wright ER. The dimensionality of stigma: a comparison of its impact on the self of persons with HIV/AIDS and cancer. J Health Social Behav 2000;41(1):50–67.
- Swendeman D, Rotheram-Borus MJ, Comulada S, Weiss R, Ramos ME. Predictors of HIV-related stigma among young people living with HIV. Health Psychol 2006;25(4):501–9.
- Alonso J, Buron A, Bruffaerts R, He Y, Posada-Villa J, Lepine JP, Association of perceived stigma and mood and anxiety disorders: results from the World Mental Health Surveys. Acta Psychiatr Scand 2008;118(4):305–14.
- Van Brakel WH. Measuring health-related stigma – a literature review. Psychol Health Med 2006;11(3):307–34.
- Ware JEJr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 1992;30(6):473–83.
- Diener E, Emmons RA, Larsen RJ, Griffin S. The Satisfaction With Life Scale. J Pers Assess 1985;49(1):71–5.
- Wilson JR, Hashimoto RE, Dettori JR, Fehlings MG. Spinal cord injury and quality of life: a systematic review of outcome measures. Evid Based Spine Care J 2011;2(1):37–44.
- Antonak RF. Development and psychometric analysis of the Scale of Attitudes Toward Disabled Persons. Journal of Applied Rehabilitation Counseling 1982;13(2):22–9.
- Link BG. Understanding Labeling Effects in the area of mental disorders: an assessment of the effect of expectations of rejection. Am J Community Psychol 1987;11:261–73.
- Ritsher JB, Otilingam PG, Grajales M. Internalized stigma of mental illness: psychometric properties of a new measure. Psychiatry Res 2003;121(1):31–49.
- Corrigan PW, Michaels PJ, Vega E, Gause M, Watson AC, Rusch N. Self-stigma of mental illness scale--short form: reliability and validity. Psychiatry Res 2012;199(1):65–9.
- Berger BE, Ferrans CE, Lashley FR. Measuring stigma in people with HIV: psychometric assessment of the HIV stigma scale. Res Nurs Health 2001;24(6):518–29.
- Fernandes PT, Salgado PC, Noronha AL, Sander JW, Li LM. Stigma Scale of Epilepsy: validation process. Arq Neuropsiquiatr 2007;65(Suppl 1):35–42.
- Molina Y, Choi SW, Cella D, Rao D. The Stigma Scale for Chronic Illnesses 8-Item Version (SSCI-8): Development, Validation and Use Across Neurological Conditions. Int J Behav Med 2013;20(3):450–60.
- Rao D, Choi SW, Victorson D, Bode R, Peterman A, Heinemann A, Measuring stigma across neurological conditions: the development of the stigma scale for chronic illness (SSCI). Qual Life Res 2009;18(5):585–95.
- Tulsky D, Kisala PA, Victorson D, Tate DG, Heinemann AW, Charlifue S, Overview of the Spinal Cord Injury – Quality of Life (SCI-QOL) measurement system. J Spinal Cord Med 2015;38(3):257–69.
- Tulsky DS, Kisala PA, Victorson D, Choi SW, Gershon R, Heinemann AW, SCI-QOL: Methodology for the development and calibration of the SCI-QOL item banks. J Spinal Cord Med 2015;38(3):270–87.
- Kisala PA, Tulsky DS. Opportunities for CAT applications in medical rehabilitation: development of targeted item banks. J Appl Meas 2010;11(3):315–30.
- Kalpakjian CZ, Tate DG, Kisala PA, Tulsky DS. Measuring self-esteem after spinal cord injury: Development, validation and psychometric characteristics of the SCI-QOL Self-esteem item bank and short form. J Spinal Cord Med 2015;38(3):377–85.
- Gershon RC, Lai JS, Bode R, Choi S, Moy C, Bleck T, Neuro-QOL: quality of life item banks for adults with neurological disorders: item development and calibrations based upon clinical and general population testing. Qual Life Res 2012;21(3):475–86.
- Cella D, Nowinski C, Peterman A, Victorson D, Miller D, Lai JS, The neurology quality-of-life measurement initiative. Arch Phys Med Rehabil 2011;92(10, Supplement):S28–36.
- DeWalt DA, Rothrock N, Yount S, Stone AA. Evaluation of item candidates: the PROMIS qualitative item review. Med Care 2007;45(5 Suppl 1):S12–21.
- Willis GB. Cognitive Interviewing: a ‘how to’ guide. Research Triangle Park, NC: Research Triangle Institute; 1999.
- Eremenco SL, Cella D, Arnold BJ. A comprehensive method for the translation and cross-cultural validation of health status questionnaires. Eval Health Prof. 2005;28(2):212–32.
- MetaMetrics. The LEXILE framework for reading. Durham, NC: MetaMetrics Inc; 1995.
- National Spinal Cord Injury Statistical Center. SCI Facts and Figures at a Glance. J Spinal Cord Med 2014;37(2):243–4.
- American Spinal Injury Association. International Standards for Neurological and Functional Classification of Spinal Cord Injury. American Spinal Injury Association, International Spinal Cord Society; 2002.
- Steinberg L, Thissen D. Use of item response theory and the testlet concept in the measurement of psychopathology. Psychol Methods 1996;1(1):81–97.
- Lord FM, Novick MR. Statistical Theories of Mental Test Scores. Reading, MA: Addison-Wesley; 1968.
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, (eds.) Testing structural equation models. Newbury Park, CA: Sage; 1993. p. 136–62.
- Steiger J. Structural model evaluation and modification: An interval estimation approach. Multivariate Behavioural Research 1990;25(2):173–80.
- Samejima F, van der Liden W, Hambleton R. The graded response model. Handbook of modern item response theory. New York: Springer; 1996. p. 85–100.
- Terry R, Lee SH, Milburn N. IRT-FIT: Fitting IRT models in SAS®. Technical Manual for Users. 2005.
- Choi SW, Gibbons LE, Crane PK. Lordif: An R package for detecting differential item functioning using iterative hybrid ordinal logistic regression/item response theory and monte carlo simulations. J Stat Softw 2011;39(8):1–30.
- Lai JS. Differential item functioning (DIF). In: Cella D, (ed.) Item Reponse Theory Modeling at CORE. Chicago, IL: Northwestern University; 2002. p. 28–44.
- Stocking ML, FM L. Developing a common metric in item response theory. Appl Psychol Meas 1983;7(2):201–10.
- Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull 1979;86(2):420–8.
- Weir JP. Quantifying test-retest reliability using the intraclass correlation coefficient and the SEM. J Strength Cond Res 2005;19(1):231–40.
- Gershon R, Rothrock NE, Hanrahan RT, Jansky LJ, Harniss M, Riley W. The development of a clinical outcomes survey research application: Assessment Center. Qual Life Res 2010;19(5):677–85.