Abstract
Background and objectives:
Cardiovascular disease is a major concern in HIV-infected patients. Lifetime risk estimations use the risk of developing it over the course of remaining lifetime, and are useful in communicating this risk to young patients. We aim to describe the prevalence of cardiovascular risk factors among a representative sample of HIV-infected subjects under antiretroviral therapy in Spain, and to estimate their lifetime risk of cardiovascular disease.
Methods:
Cross-sectional survey about cardiovascular risk factors in 10 HIV units across Spain. Lifetime risk assessed according to Barry was classified in two major categories: low and high lifetime risk.
Results:
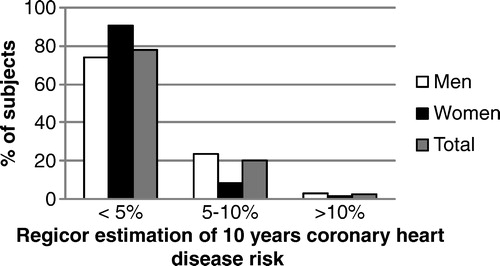
We included 895 subjects, 72% men, median age 45.7 years; median CD4 lymphocyte count 598 cells/μl, median time since HIV diagnosis 11 years, median time on antiretroviral treatment 6.3 years, 87% had undetectable HIV viral load. Tobacco smoking was the most frequent risk factor (54%), followed by dyslipidemia (48.6%) and hypertension (38.6%). Estimated 10-year coronary risk (Framingham/Regicor Risk Score) risk was low ( < 5%) in 78% of the patients, and intermediate (5–10%) in 20%. Lifetime risk estimation showed a high risk profile for 71.4% of the population studied, which was associated with increasing age, prolonged antiretroviral therapy and patient's place of origin.
Conclusions:
Modifiable cardiovascular risk factors in this population are very common. There are significant disparities between the low 10-year risk estimated with the Framingham/Regicor score and the higher lifetime risk in HIV patients on antiretroviral therapy. A more aggressive management of modifiable cardiovascular risk factors in these patients seems advisable.
Introduction
Cardiovascular disease (CVD) is a major concern in persons living with HIV (PLWH).Citation1 Antiretroviral therapy (ART) may lead to profound and durable viral suppression, and this is associated with a significant reduction in HIV-related complications, such as opportunistic infections; however, persistent low-grade inflammation and immune activation is observed in many HIV-infected individuals on suppressive ART, and this may facilitate non-AIDS comorbidities and CVD.Citation2 Nevertheless, traditional cardiovascular risk (CVR) factors such as aging, smoking, diabetes or hypertension are by far the main drivers of incidental cases of ischemic heart disease.Citation3 Information about the prevalence of traditional CVR factors in PLWH, in particular potentially modifiable factors, may be useful to identify treatable health problems and increase the efforts in prevention. Because of the relative low age of PLWH, classical estimates of 10-year CVR usually show a relatively low CVD risk.Citation4 Little information exists about long-term CVR estimates, such as lifetime CVR. This scale estimates the risk of developing CVD over the course of an individual's remaining lifetime, and may be useful in communicating the risk of CVD to young patients.Citation5
Updated information about CVR factors in patients on long-term ART in Spain is scarce; recent reports in HIV infected subjects who are ART-naive or with current ART show tobacco smoking and low HDL-cholesterol as the main CVR factors.Citation6 PLWH on prolonged ART are a group with a probably different CVR profile related to the exposure to ART, in particular to drugs used in the past. The objective of our study is to analyse CVR factors in a sample of patients on ART, to assess its distribution according to some relevant sociodemographic and clinical characteristics, and to estimate the lifetime CVR of this population.
Methods
This is a cross-sectional survey about cardiovascular risk factors in HIV infected subjects under ART in Spain. Subjects invited to participate were patients in care in the HIV units of 10 hospitals in eight cities across Spain, recruited during 2011. To minimize selection bias, all HIV-infected patients were eligible, providing they were receiving antiretroviral treatment by the day of their visit, and they were not pregnant or breastfeeding. Each hospital was asked to include the first 90 eligible subjects seen during a four week period. In all centers, less than 5% of patients refused to participate, mostly because shortage of time. Although a selection bias is not completely excluded, we believe that the population studied is representative of the outpatient population of treated HIV patients.
Sample size was maximized by assuming a prevalence of 50% for different subject's features, with a precision of 3.3% and a confidence level of 95%. Ethics' committees of all the participating hospitals approved the study protocol, and a signed informed consent was obtained from each subject. The study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki.
Data collection
Data were obtained from the medical chart and/or during the clinical visit, and included socio-demographic, epidemiologic and clinical information, as well as CVR factors, laboratory parameters and basic anthropometries. Non-modifiable risk factors were defined as follows: age (men older than 55 years, women older than 65 years), male sex, and family history of early CVD (parents or siblings, men younger than 55 years or women younger than 65 years old, with established CVD). Modifiable risk factors were defined as follows: hypertension: prior diagnosis or treatment and/or systolic blood pressure ≥ 140 mm/Hg and/or diastolic blood pressure ≥ 90 mm/Hg (values are de mean of two measurements during the study visit). Tobacco use (self-reported) was categorized as smoking (any amount of cigarettes during the last year or currently) and non-smoking (never smoking or cessation more than one year before). Dyslipidemia: previous diagnosis and treatment, or at least one abnormal value for lipids in fasting conditions (total cholesterol >240 mg/dl, LDL-cholesterol >160 mg/dl, HDL cholesterol < 40 mg/dl, or a total cholesterol/HDL ratio >5). Obesity was defined as a Body Mass Index ≥ 30 kg/m2, and central obesity as a waist circumference >102 cm in men and 88 cm in women. Diabetes mellitus: prior diagnosis or treatment. Physical activity was explored with the question “Do you exercise regularly?” (walk half an hour daily or do some exercise three times/week), and classified as physical inactivity if the answer was negative. Metabolic syndrome was defined by the ATP-III diagnostic criteriaCitation7 as any 3 of the following: abdominal obesity, triglycerides ≥ 150 mg/dl, HDL cholesterol < 40 mg/dl for men or < 50 mg/dl for women, blood pressure ≥ 130/ ≥ 85 mmHg, or fasting glucose ≥ 110 mg/dl.
Regicor score is the adaptation of the Framingham score validated for the Spanish populationCitation8 and was calculated with the Regicor CVR calculator, available at http://www.regicor.org. It calculates the 10 years' risk of coronary heart disease (CHD) (fatal and non-fatal myocardial infarction, silent myocardial infarction, and/or angor pectoris), and its cut-off values are low risk ( < 5%), moderate risk (5–10%), and high risk (>10%).
Lifetime risk of CVD was calculated following the method proposed by Berry et al.,Citation5 based on the estimations of The Cardiovascular Lifetime Risk Pooling Project. This method classifies the lifetime risk in five mutually exclusive categories: (1) all risk factors are optimal; (2) at least one risk factor is not optimal; (3) at least one risk factor (cholesterol level or blood pressure) is high; (4) one major risk factor is present; and (5) two or more major risk factors are present. Definitions of these risk factor strata are shown in . For example, according to these authors, lifetime risk for the total events related to atherosclerotic cardiovascular disease estimated at age 45 is 1.7% for men and 1.6% for women with all risk factors classified as optimal, whereas these figures are 49.5% and 30.7% for men and women with two or more major risk factors. In our analysis, we grouped these five categories into two big ones, i.e. with or without major risk factors: “low risk,” including categories 1, 2, and 3, and “high risk,” including categories 4 and 5, similar to what has been done in other studies.Citation9 Subjects with previous CVD were identified and excluded from the study of CVR factors.
Table 1. Definitions of risk factor strataCitation5
Statistical analysis
Continuous variables are expressed as medians and interquartile range, and categorical variables as numbers and percentages. Comparisons were made by Student's t-test, the Chi-square test, or non-parametric tests when appropriate. Comparisons between subjects with low and high lifetime CVR were made by univariate and multivariate logistic regression models, performed to explore variables that appeared to be independently associated with high CVR, including those variables statistically significant in the univariate analysis or those clinically relevant.
Results
A total of 895 patients were included in the study. shows the clinical characteristics of the study population by gender. Most of the patients studied were male, in the age range between 40 and 50 years, were native Spanish and had an elementary level of education. The main risk practice for HIV acquisition was homosexual practices between men. Our sample has a prolonged history of HIV infection as evidenced by the estimated duration of infection of 11 years and a median of 8 years of antiretroviral therapy. It is noteworthy that 32.5% of patients present hepatitis C co-infection. Regarding ART, most patients were treated with two nucleoside reverse transcriptase inhibitors (NRTIs) and one non-nucleoside reverse transcriptase inhibitor (NNRTI). Treatment at the time of inclusion was fairly stable, as suggests the median time on current therapy over 2 years.
Table 2. Sociodemographic and clinical characteristics by gender
Main CVR factors and cardiovascular risk estimations in subjects without prior CVD are shown in . Tobacco smoking was the most frequent risk factor, observed in 55% of the patients. Forty eight percent of the population studied presented dyslipidemia, being the most frequent abnormalities hypertriglyceridemia and low HDL-cholesterol. It is remarkable that only 13% of patients were treated with lipid-lowering agents (mostly statins). There was a previous diagnosis of hypertension in 15% of patients, but almost a quarter of the total population had elevated blood pressure determinations (>140 or >90 mmHg) on current clinical exam. Obesity was diagnosed in 9% of the cases. Global frequency of abdominal obesity was 16%, being more frequent in women, affecting one out of four of them.
Table 3. Cardiovascular risk factors, in subjects without previous cardiovascular disease, by gender
Lifetime risk estimation shows that most of the patient population studied (71%) present a high-risk profile (1 major risk factor or ≥ 2 major risk factors), as shown in and . As opposed to lifetime estimations, estimated 10-year CHD (Regicor score) was low ( < 5%) in 78% of the patients, and intermediate (5–10%) in 20% ( and ). It is remarkable that most female patients (90%) had a low estimate CHD risk. shows the distribution of subjects according to lifetime risk versus Regicor score classification, both in the overall population and in subjects with high risk due to their age (men older than 55 years and women older than 65); it depicts the discrepancy between these two risk estimations, since 367 (68.9%) of the subjects classified as having low short term risk by Regicor, exhibit a high risk profile according to lifetime estimations (similar figures for older subjects)
Figure 1. Cardiovascular risk estimations according to lifetime risk model, by gender. Risk groups: (1) all risk factors are optimal; (2) at least one risk factor is not optimal; (3) at least one risk factor (cholesterol lever or blood pressure) is elevated; (4) one major risk factor is present; (5) two or more major risk factors are present. All risk factors are considered to be optimal if total cholesterol is < 180 mg/dl, untreated blood pressure is < 120/80 mmHg, and the subject is non-smoker, non diabetic. At least one risk factor is non optimal in non-diabetics, non-smokers with total cholesterol between 180 and 199 mg/dl, or untreated blood pressure within 120–139/80–89 mmHg. Risk factors are high in non-smokers, non-diabetics with total cholesterol between 200 and 239 mg/dl or untreated blood pressure within 140–159/90–99 mm Hg. Major risk factors include being a smoker or a diabetic, having treated hypercholesterolemia, having an untreated total cholesterol ≥ 240 mg/dl, having a treated hypertension, or an untreated blood pressure ≥ 160/ ≥ 100 mm/Hg.
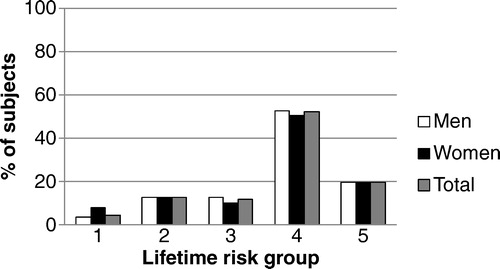
Table 4. Distribution of subjects according to lifetime risk estimation versus Regicor score
shows the characteristics of subjects without previous CVD according to their lifetime risk estimation, and the results of univariate and multivariate logistic regression models. It shows that factors independently associated with a high lifetime risk are age, already significant since age 35, patient's birthplace, since subjects from places different to Spain show a significant, relative protection against CVD risk, and time on ART: the longer the duration of treatment, the greater the estimated CVD lifetime risk, with patients on ART longer than 10 years having an independent risk of high lifetime CVR 2.1 times higher than those on ART 5 years or fewer. Among these subjects on longer ART, high risk was determined mainly by tobacco smoking (58.1%), followed by cholesterol elevations (19.1% had total values between 200 and 239 mg/dl and another 31.6% had higher values and/or received statins), hypertension (11.8% had values within 140–159/90–99 mmHg, and 22.2% had higher values and/or received treatment), and diabetes (9.6%). No relationship was found between the lifetime classification and current or nadir CD4 lymphocyte counts, history of aids, hepatitis C co-infection, type of ART (PI versus NNRTI), or being or not in the first ART regimen.
Table 5. Factors associated to high lifetime risk of cardiovascular disease in subjects without previous CVD
Discussion
The major findings of our study are three: first, the high prevalence of modifiable CVD risk factors, in particular the high frequency of smoking and hyperlipidemia, present in about half of the patients studied. Second, the suboptimal proportion of patients on lipid lowering treatments, and third, the striking differences in short- and long-term estimates of CVD, summarized as patients studied show a low short-term CVD but a high lifetime risk of CVD.
Regarding classical CVR factors, the rates of tobacco smoking in PLWH in Spain are remarkably higher than in the general population. Fifty-four percent of PLWH studied are current smokers versus 35.3% in Spanish adult subjects.Citation10 However, these figures have been reduced slightly in recent years among PLWH; in 2004, a similar cross-sectional nationwide study showed a prevalence of 64%;Citation11 Jerico et al.Citation12 in 2006 described a prevalence of 66.8% and Garcia Lázaro et al.Citation13 in 2007, 77%. Recently, Masiá et al,Citation6 analysing a series of patients with shorter ART duration described a prevalence of 46%. This elevated prevalence of smoking in PLWH is very relevant from a clinical point of view and should make us reflect on whether we are making sufficient efforts to help patients leave this chronic disease.Citation14 Smoking cessation is a complex task that must be done through a multidisciplinary effort and often with the help of drugs; medical interventions in PLWH may increase smoking cessation and reduce relapses.Citation15
Hyperlipidemia has been found also very prevalent in our study series, in 48% of the population studied. The most frequent lipid abnormality is hypertriglyceridemia, which affects 38% of the patients studied. The role of triglycerides in CVD risk in the general population is controversial.Citation16 The current consensus is that triglycerides are not directly atherogenic, but represent an important biomarker of CVR. In PLWH the D:A:D study found a marginal association of hypertriglyceridemia and coronary heart disease,Citation17 in part modulated by the values of total and HDL-cholesterol.
An important finding of our study is the relatively small proportion of patients with hyperlipidemia receiving lipid-lowering therapies; in our series, only 13% of them were on statins and 2% on fibrates. Given the strength of the evidence as to the increased frequency of CVD in PLWH, we consider that this finding of such a low proportion of patients on lipid-lowering therapy is alarming. This conservative management of risk factors has been described elsewhereCitation18,Citation19 and might be related to concern about drug interactionsCitation20 and perhaps with less concern about the importance of CVD disease compared that of HIV infection. Physical inactivity is very frequent in this sample, and even when we cannot say it is an independent risk factor with our results, the crude and adjusted odds ratios suggest that it plays an important role in the risk profile of these subjects.
In this study, we also found differences between men and women in CVR factors. The 211 female patients in our sample had a lower educational level and a longer history of HIV infection and ART use, and exhibited a lower level of physical activity and a higher prevalence of abdominal obesity. Additionally, in these women the prevalence of hypertension and dyslipidemia was lower than men with the criteria used, with high HDL-cholesterol and low triglyceride levels. We found no differences between genders when calculating the lifetime risk. This can be considered as a limitation of the study, since with similar lifetime risk estimation; female patients have a significantly lower risk of CVD.
We also would like to highlight from our results the discrepancy between the high prevalence of CVR factors and the relatively low short–term risk estimations using traditional scales, issue that is being increasingly recognized also for HIV negative, general populations.Citation21,Citation22 For example, using slightly different cut-off values, Berry et al.Citation21 and Hulten et al.Citation22 have found that about a half of the subjects included in their studies had a low short-term risk but a high lifetime risk. In our study, this figure is even higher, with almost 70% of subjects with a low short-term estimation who have at least one major risk factor and are classified as having a high risk according to lifetime estimation. Even when the Framingham/Regicor scale estimation is low for most of our patients (77% with < 5% at 10 years), there is a surprisingly elevated frequency of some relevant CVR factors. Since the influence of tobacco smoking and dyslipidemia is undisputed in CVD risk, this suggests that the relatively low age of patients partially offset the risk. Because of the dependency on age, these relatively young HIV-infected patients would be considered at low short-term risk, but actually they are on risk in the long-term in the case that these factors are not modified. In the general population, the combination of the low short-term and high lifetime risk had a baseline burden of subclinical CVD and an increased rate of atherosclerosis progression.Citation21
These discrepancies have been identified in other epidemiological studies conducted in the general population in people under age 50.Citation23 Atherosclerosis occurs over decades and is mainly related to long-term and cumulative exposure to causal, modifiable risk factors.Citation24 Thus, long-term perspective of risk assessment and prevention must be considered, especially among younger individuals. A recently published report from the American College of Cardiology/American Heart Association recommends calculating the long-term risk in patients aged 20–59 years with a 10-year risk less than 7.5%.Citation25 Lifetime risk estimation should not replace the classical 10-year risk assessment on clinical decision-making such as initiation of lipid-lowering therapy, and could provide adjunctive information for risk communication that may help to guide therapeutic lifestyle counseling. To our knowledge, no information has been published on lifetime risk in PLWH. More research is needed to verify the potential utility of using longer-term risk prediction scores to identify HIV-infected patients at higher risk for CHD.
The main limitation of our study is its cross-sectional design, since no causality can be inferred from the results of our study. Moreover, lifetime risk estimations are not validated in PLWH. Life expectancy has increased significantly in HIV-infected patients after the introduction of ART, but it is still lower than that observed in the general population,Citation26 so when estimating the long-term survival in PLWH, these factors should be considered, and perhaps the estimates used in the general population are not fully applicable.
Conclusions
The frequency of modifiable cardiovascular risk factors is high in Spanish HIV-infected patients on therapy. The clinical implications of this finding are important and should lead to a more aggressive management of risk factors. We found a striking contrast between the estimated 10-year cardiovascular risk and lifetime risk. The clinical implications of this finding warrant further study.
Disclaimer Statements
Contributors
Study design: VE. Study implementation: All named authors. Analysis and interpretation of data: VE, AO and AFC. Major contribution to writing: VE, JIB and MM. Read and approved final version: all named authors.
Funding Sources
Unrestricted grant form Gilead Sciences, SL.
Conflicts of Interests
Vicente Estrada has received grants from Gilead, BMS, and Abbvie, and personal fees from ViiV, MSD, and Janssen outside the submitted work.
José Ignacio Bernardino reports other from Gilead Sciences, during the conduct of the study; personal fees from ViiV Healthcare, BMS, MSD, and Janssen, outside the submitted work.
Mar Masiá reports personal fees from Gilead, ViiV, BMS, Janssen, and Merck, outside the submitted work.
José Antonio Iribarren has nothing to disclose.
Alejandra Ortega has nothing to disclose.
Fernando Lozano, reports personal fees from Abbvie, Bristol Myers and Squibb, Boehringer Ingelheim, Gilead Sciences, Janssen-Cilag, and MSD, and grants and personal fees from ViiV Healthcare, outside the submitted work.
Celia Miralles has nothing to disclose.
Julián Olalla reports personal fees from Gilead, MSD, Abbvie, Viiv, and Janssen, outside the submitted work.
Jesús Santos has nothing to disclose.
Maria Jesús Pérez Elías reports grants from Gilead, during the conduct of the study; grants, personal fees, and other from Gilead, personal fees from BMS, grants and personal fees from ViiV, personal fees from MSD and Janssen, outside the submitted work.
Pere Domingo has nothing to disclose.
Arturo Fernández-Cruz has nothing to disclose.
Ethics Approval This study adheres to ethics requirements and reporting guidelines.
Acknowledgements
We thank Ana María Caro-Murillo and Paz Sobrino for writing assistance and statistical analysis.
References
- Palella FJ Jr, Phair JP. Cardiovascular disease in HIV infection. Curr Opin HIV AIDS. 2011;6:266–271.
- Duprez DA, Neuhaus J, Kuller LH, et al. Inflammation, coagulation and cardiovascular disease in HIV-infected individuals. PLoS One. 2012;7:e44454.
- Friis-Moller N, Thiebaut R, Reiss P, et al. Predicting the risk of cardiovascular disease in HIV-infected patients: the data collection on adverse effects of anti-HIV drugs study. Eur J Cardiovasc Prev Rehabil. 2010;17:491–501.
- D'Agostino RB Sr. Cardiovascular risk estimation in 2012: lessons learned and applicability to the HIV population. J Infect Dis. 2012;205(Suppl 3):S362–S367.
- Berry JD, Dyer A, Cai X, et al. Lifetime risks of cardiovascular disease. N Engl J Med. 2012;366:321–329.
- Masia M, Perez-Cachafeiro S, Leyes M, et al. Riesgo cardiovascular en pacientes con infección por el virus de la inmunodeficiencia humana en España. Cohorte CoRIS, 2011. Enferm Infecc Microbiol Clin. 2012;30:517–527.
- Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III), JAMA. 2001;285:2486–2497.
- Grau M, Marrugat J. Funciones de riesgo en la prevención primaria de las enfermedades cardiovasculares. Rev Esp Cardiol. 2008;61:404–416.
- Petr EJ, Ayers CR, Pandey A, et al. Perceived lifetime risk for cardiovascular disease (from the Dallas Heart Study). Am J Cardiol. 2014;114:53–58.
- Catalina-Romero C, Sainz Gutierrez JC, Quevedo AL, et al. Prevalencia de consumo de tabaco en población trabajadora tras la entrada en vigor de la Ley 42/2010. Rev Esp Salud Publica. 2012;86:177–188.
- Martinez E, Arribas J, López-Aldeguer J. Factors associated with a high cardiovascular risk in HIV infected patients in Spain: a multicenter, nationwide, cross sectional study. Paper presented at: 12th Conference on Retrovirus and Opportunistic Infections; February 22–25, 2005; Boston, MA, USA. Abs # 870.
- Jerico C, Knobel H, Sorli ML, Montero M, Guelar A, Pedro-Botet J. Prevalencia de factores de riesgo cardiovascular en pacientes con infección por el VIH. Rev Clin Esp. 2006;206:556–559.
- Garcia-Lazaro M, Rivero RA, Camacho EA, et al. Variabilidad en la valoración del riesgo coronario en pacientes infectados por el virus de la inmunodeficiencia humana. Med Clin (Barc). 2007;129:521–524.
- Franco M, Cooper R, Bilal U, Fuster V. Control of coronary heart disease risk factors and evidence-based therapies: joint efforts for coronary heart disease prevention in Spain. Rev Esp Cardiol. 2011;64:962–964.
- Huber M, Ledergerber B, Sauter R, et al. Outcome of smoking cessation counselling of HIV-positive persons by HIV care physicians. HIV Med. 2012;13:387–397.
- Miller M, Stone NJ, Ballantyne C, et al. Triglycerides and cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2011;123:2292–2333.
- Worm SW, Kamara DA, Reiss P, et al. Elevated triglycerides and risk of myocardial infarction in HIV-positive persons. AIDS. 2011;25:1497–1504.
- Freiberg MS, Leaf DA, Goulet JL, et al. The association between the receipt of lipid lowering therapy and HIV status among veterans who met NCEP/ATP III criteria for the receipt of lipid lowering medication. J Gen Intern Med. 2009;24:334–340.
- Reinsch N, Neuhaus K, Esser S, et al. Are HIV patients undertreated? Cardiovascular risk factors in HIV: results of the HIV-HEART study. Eur J Prev Cardiol. 2012;19:267–274.
- Ahmed MH, Al-Atta A, Hamad MA. The safety and effectiveness of statins as treatment for HIV-dyslipidemia: the evidence so far and the future challenges. Expert Opin Pharmacother. 2012;13:1901–1909.
- Berry JD, Liu K, Folsom AR, et al. Prevalence and progression of subclinical atherosclerosis in younger adults with low short-term but high lifetime estimated risk for cardiovascular disease: the coronary artery risk development in young adults study and multi-ethnic study of atherosclerosis. Circulation. 2009;119:382–389.
- Hulten E, Villines TC, Cheezum MK, et al. Calcium score, coronary artery disease extent and severity, and clinical outcomes among low Framingham risk patients with low vs high lifetime risk: results from the CONFIRM registry. J Nucl Cardiol. 2014;21:29–37.
- Marma AK, Lloyd-Jones DM. Systematic examination of the updated Framingham heart study general cardiovascular risk profile. Circulation. 2009;120:384–390.
- Ferreira-Gonzalez I. The epidemiology of coronary heart disease. Rev Esp Cardiol. 2014;67:139–144.
- Goff DC Jr, Lloyd-Jones DM, Bennett G, et al. 2013 ACC/AHA Guideline on the Assessment of Cardiovascular Risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25 Supp 2):S49–73.
- Nakagawa F, Lodwick RK, Smith CJ, et al. Projected life expectancy of people with HIV according to timing of diagnosis. AIDS. 2012;26:335–343.