Abstract
Background
Bone disease comprising of low bone mineral density (BMD), bone pain, and fractures is a characteristic feature of thalassemia. Vitamin D receptors (VDRs – FokI, TaqI, and Bsml) polymorphisms are closely related to low BMD at the lumbar spine and hips which can be used as a useful genetic marker in predicting bone disease in these patients.
Aim
To find out the status of VDRs gene polymorphisms and its effect on osteoporosis in thalassemia patients of North Indian origin.
Material and methods
BMD was measured in 40 beta-thalassemia major patients by dual-energy X-ray densitometry (DXA). Serum vitamin D levels were estimated by enzyme linked immunosorbant assay. VDR gene polymorphisms (FokI, TaqI, and BsmI) were analyzed by polymerase chain reaction restriction fragment length polymorphism (PCR-RFLP) method.
Results
About 80.6% cases were found to be vitamin D deficient. Z score of BMD of lumbar spine and hips were −2.31 ± 1.18 and −2.09 ± 0.89. Osteoporotic lumbar spine was observed in 42.5% cases of thalassemia. A positive correlation of vitamin D level was found with Z score of BMD of lumbar spine (r = 0.398, P value = 0.027). Polymorphisms of FokI and BsmI were found significantly correlated with BMD of lumbar spine. However, no association of BMD was observed with TaqI polymorphism.
Conclusion
The present study showed a high prevalence of low BMD in thalassemia, suggesting that they should be targeted for DXA screening and osteoporosis prevention before permanent end organ bone damage occurs. The VDR genotyping can be used as additional test in individuals who are susceptible to osteoporosis so that early preventive measurements can be taken.
Introduction
Osteoporosis is characterized by low bone mass and disruption of bone architecture, resulting in reduced bone strength and increased risk of fractures. Osteoporosis has been extensively described to occur in beta-thalassemia,Citation1 especially in adult survivors. Considerable morbidity in older thalassemia patients results from bone disease due to osteopenia and osteoporosis, which is often accompanied by disabling pain and fractures.
The aetiology of bone disease in thalassemia is multifactorial and is still under investigation. Factors such as hormonal deficiency, especially gonadal failure, bone marrow expansion, increased iron stores, desferrioxamine toxicity, and calcium and vitamin D deficiency have been implicated to have a serious impact on the impaired bone metabolism.Citation2
Vitamin D is one of the important factors required for bone development and maintenance of bone mass as well as the principal factor for normal calcium and phosphate homeostasis. Vitamin D status has been linked to bone mineral density (BMD) in both retrospectiveCitation3 and prospective interventionalCitation4 studies.
Several studies have investigated the genetic variants of the gene locus encoding the receptor for the hormonally active form of vitamin D3 (VDR) and BMD.Citation5–Citation9 The human VDR gene consists of six noncoding 5′-untranslated exons and eight coding exons (exons 2–9). Furthermore, the VDR has also a large 3′-untranslated site. Several restriction sites have been used to characterize polymorphisms in the VDR gene. The polymorphic sites, BsmI at intron 8 and TaqI at exon 9, are linked to each other. A FokI site at the translation start site has also been reported as polymorphic and examined in relation to BMD.
The aim of this study was to establish the base line data of VDR gene polymorphism and its association with BMD in thalassemia patients of Indian origin.
Material and methods
Subjects
Forty beta-thalassemia major patients attending IPD at Department of Genetics, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Lucknow for blood transfusion were recruited for the study. Patients who had other medical conditions (heart failure, renal failure, or hypoparathyroidism) and those using medications which affect bone mineral metabolism (as glucocorticoids or anticonvulsant drugs) were excluded from the study. The study protocol was approved by the ethics committee of the SGPGIMS. Written informed consent was obtained from parents or from subjects older than 18 years of age.
Anthropological measurement
Subjects were weighed using a digital scale with light clothing but without shoes (accuracy 0.1 kg). Height was measured in an upright position without shoes by a stadiometer (accuracy 0.1 cm). Body mass index (BMI, kg/m2) was calculated by dividing body weight (kg) by the height squared (mCitation2).
Biochemical analysis
Serum calcium, inorganic phosphorus, and alkaline phosphatase levels were determined by an automated analyzer (Randox). Vitamin D was measured by enzyme linked immunosorbant assay (IDS-UK).
Bone mineral density
There is controversy regarding the optimal method for assessing bone mass in the pediatric population. In this study, we assessed BMD using dual X-ray absorptiometry (DXA, HOLOGIC, USA), which still remains the most commonly used method. The advantages of this technique include the relatively low radiation exposure, its worldwide availability, and the short duration of the procedure. Its main disadvantage is the fact that, as DXA is a two-dimensional measurement, results are correlated to body and bone size, a factor that becomes more important in the growing pediatric population.
BMD of the lumbar spine (L1 ± L4) and hips were determined in 40 patients greater than 12 years of age. Pediatric software was used for children with a weight below 30 kg. During measurement of the lumbar spine, the child was supine, and the physiological lumbar lordosis was flattened by elevation of the knees.
Genotype analysis
DNA was extracted from the peripheral blood collected in ethylenediaminetetraacetic acid coated tubes by phenol chloroform method described by Poncz et al.Citation10
The VDR genotyping were done by using polymerase chain reaction restriction fragment length polymorphism (PCR-RFLP) analysis as described below.
BsmI polymorphism
The BsmI polymorphism was analyzed by method described by Morrison et al.Citation11 using forward: 5′-CAACCAAGACTACAAGTACCGCGTCAGTGA-3′ and reverse: 5′-AACCAGCGGGAAGAGGTCAA GGG-3′ primers. The 822 bp amplicon produced was digested at 37°C with BsmI restriction enzyme (New England Biolabs (UK) Ltd, Hitchin, Hertfordshire, UK) as per manufacturer's instructions. The digested products were electrophoresed on ethidium bromide-stained 2% agarose gel.
Homozygous subjects with wild-type alleles showed an intact 822-bp band and were designated as having BB BsmI genotype. Homozygous subjects with alleles containing G at this position showed two bands of 650 and 172 bp and were designated as bb. Subjects with heterozygote status at this position showed all three bands – i.e. 822, 650, and 172 bp and were designated as Bb.
TaqI polymorphism
The TaqI polymorphism was determined according to the method described by Lundin et al.Citation12 A 198-bp DNA fragment was obtained using PCR primers forward: 5′-GTGGGATTGAGCAGTGAG-3′ and reverse: 5′-TGGATCATCTTGGCATA GAG-3′ located within intron 8 and exon 9. PCR products were subjected for digestion with TaqI (New England Biolabs (UK) Ltd) at 37°C for 12 hours and were separated on 2% agarose gel. The presence of a C-T substitution at position 3 on codon 352(ATC-ATT) in exon 9, which codes for isoleucine, is associated with loss of the TaqI restriction site. The TaqI restriction enzyme recognizes and cleaves the ATC allele, which is designated t.
FokI polymorphism
The FokI polymorphism was analyzed as per Harris et al.Citation13 method using forward (5′-AGCTGGCCCTGGCACTGACTCTGCTCT-3′) and reverse primer (5′- ATGGAAACACCT TGCTTCT TCTCCCTC-3′). PCR products were digested with FokI restriction enzyme (New England Biolabs (UK) Ltd) at 37°C for 12 hours and electrophoresed on 3% agarose gel.
The FF genotype lacks FokI site and showed only one band of 265 bp. The ff genotype generated two fragments of 196 and 69 bp. The heterozygote displayed three fragments of 265, 196, and 69 bp, designated as Ff.
Statistical analysis
An analysis of relationships between BMD and clinical parameters, i.e. age, body mass, and height, was performed with the use of the Spearman's rank correlation. Student's t-test was used to compare the means of the two samples. The difference in the mean value of the various biochemical and BMD indicators in subjects with three different genotype groups related to VDR gene polymorphisms was analyzed by using analysis of variance (ANOVA) followed by Bonferoni's test for post-hoc analysis if the ANOVA was significant. A P value <0.05 was considered significant. All the statistical analysis were preformed on SPSS 15.0 (SPSS Inc., New York, USA).
Results
shows mean age, height, weight, and bone mass index of thalassemia patient's recruited for study. About 56.6% boys and 27.7% of girls were of short stature where as weight of 41.6% boys and 33.3% of girls were found below the 5th percentile.
Table 1. Anthropological, biochemical, and BMD characteristics of thalassemia patients
The mean S.Ca level of 40 beta-thalassemia cases was 8.64 ± 1.13 mg/dl which does not differ significantly between boys and girls in the present study (9.10 ± 1.02 and 8.54 ± 1.2 mg/dl, respectively, P value = 0.129). Out of 40 subject calcium deficiency was found in 11 (27.5%) subjects (seven females and four males). The mean serum inorganic phosphorus level was 5.11 ± 1.3 mg/dl and was found elevated in 17 (42.5%) subjects (nine females and eight males).
The mean vitamin D levels were 10.74 ± 8.96 ng/ml. The mean values of vitamin D levels were found significantly higher in boys as compared to girls (13.54 ± 10.34 and 6.32 ± 3.00 ng/ml, respectively; P value = 0.026). Of the subjects studied, 80.6% had vitamin D deficiency (<20 ng/ml) and 12.9% had vitamin D insufficiency (20–32 ng/ml). Only two subjects had sufficient vitamin D status (>32 ng/ml).
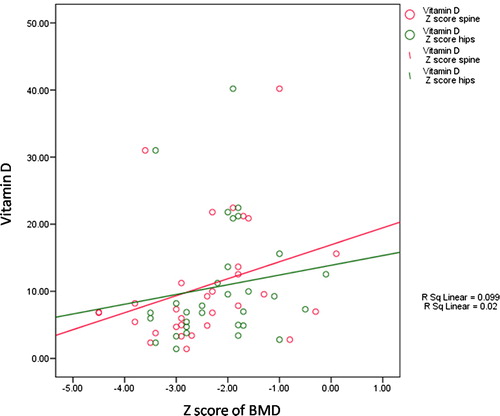
On evaluating Z score of BMD at lumbar spine we found that 20% had normal BMD whereas 37.5% cases had Z score between −1.0 to −2.5 SD suggesting low BMD (osteopenic). Z score was found below −2.5 SD in 42.5% cases indicating osteoporosis at lumbar spine. An analysis of Spearman's rank correlation coefficient indicated a significant influence of serum vitamin D on Z score of BMD at lumbar spine in the studied group of patients (r = 0.398, P value = 0.027) (). Z score of BMD at hips was found as normal, osteopenic, and osteoporotic in 12.5, 55, and 32.5%, respectively.
The genotype distribution of VDR gene polymorphism showed that the study subjects were in Hardy–Weinberg equilibrium FokI, BsmI, and TaqI (P value = 0.889, 0.142, and 0.437, respectively).
Each polymorphism in thalassemia patients was analyzed with respect to its association with BMD at lumbar spine and hips () as well as biochemical parameters ().
Figure 2. Z score of BMD at lumbar spine and hips in different FokI (A), BsmI (B), and TaqI (C) genotypes.
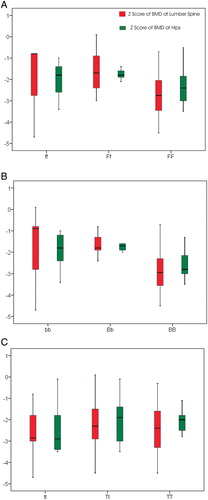
Table 2. Relation between VDR genotypes, BMD, and other studied variables
No association of serum calcium, inorganic phosphorus, alkaline phosphate, and vitamin D was found with any of the VDR gene polymorphism.
FokI polymorphism was found significantly associated with Z score of BMD at lumbar spine (P value = 0.001). Although the Z score of BMD at hips did not differ significantly in different FokI genotype (P value = 0.154), however, a significant correlation with a trend toward higher values for hip bone density of the ff genotype and toward lower value with the homozygous FF genotype was observed (r = −0.386, P value = 0.015).
In case of BsmI polymorphism Z score of BMD was found to be significantly decreased in the presence of B allele in both lumbar spine (r = −0.617, P value = 0.000) and hips (r = −0.598, P value = 0.000).
No significant association was observed in Z score of BMD at lumbar spine (P value = 0.934) and hips (P value = 0.853) with TaqI polymorphism. We also did not find any correlation between Z score of BMD at both lumbar spine(r = −0.041, P value = 0.802) and hips (r = 0.019, P value = 0.909) with TaqI polymorphism.
Discussion
In the present study, BMD was reduced in 32 out of 40 (80%) cases, of which 37.5% had osteopenia and 42.5% had osteoporosis. Osteoporosis is a complex multi-factorial disease with environment, diet, as well as genetics contributing variably to the condition. It represents an important cause of morbidity in patients with beta-thalassemia major.Citation14 Low bone mass in thalassemia is attributed to bone marrow expansion and consequent reduction of trabecular bone tissue and cortical thinning due to increased but ineffective hematopoiesis. In recent years, advances in transfusion management and chelation therapy have achieved an improvement in skeletal development and cosmetic bone appearance. However, despite optimal conventional treatment and decline in endocrine complications, low bone density is still reported in thalassemic patients.Citation15 Our results are similar to those of previous studies which have reported reduced BMD of spine and hips in over two-third patients of β thalassemia major and sickle cell diseaseCitation16–Citation19 from Israel, Italy, and Egypt.
We also found significant positive correlation between serum 25-(OH) vitamin D levels and Z score of BMD at lumbar spine. Vitamin D is known to be an important factor required for bone development, maintenance of bone mass, as well as principal factor required for control of normal calcium and phosphate homeostasis. The study was in agreement with the previous studies reported by Nakamura et al.Citation20 Vupputuri et al.Citation21 Pirinççioğlu et al.Citation22 and Frisk et al.Citation23
Low serum calcium and low serum vitamin D levels with elevated levels of serum inorganic phosphorus and alkaline phosphatase were found in our thalassemia patients. Previously, De Sanctis et al.Citation24 have reported hypocalcemia as a late complication of iron overload in cases of beta-thalassemia. Chatterton et al.Citation25 demonstrated vitamin D deficiency, osteomalacia, and rickets in thalassemia patients as a result of defective 25 hydroxylation of vitamin D due to iron overload and subsequent liver dysfunction. Other mechanisms leading to disturbed calcium, phosphorus, and vitamin D homeostasis include decreased intake, impaired absorption, and reduced synthesis of vitamin D.Citation16
Our results show lower BMD of lumbar spine with FF and BB genotypes in 40 thalassemia patients. BB genotype was also found to be significantly associated with lower BMD of hips as compared to Bb or bb genotypes. However, we have not observed any association between FokI polymorphisms and BMD at hips. The results are in concordance with those of Ferrara et al.Citation17 who have reported combined effects of FokI and BsmI VDR polymorphism on femoral neck and lumbar spine BMD in 108 thalassemia cases from Italy with significantly lower BMD at both sites in all patients with FF VDR genotype and lower BMD of lumbar spine in patients with BB VDR genotype. However, Wu et al.Citation26 showed no association of VDR genotype with BMD. No significant association of TaqI polymorphism with BMD either of lumbar spine or hips was observed. These findings are in contrast to the findings of Spector et al.,Citation27 Nguyen et al.Citation28 and Vupputuri et al.Citation21 who showed a significant association of TaqI with BMD. Hence, VDR gene polymorphisms are considered to be a factor determining bone turnover rate and BMD but remain debatable till date.Citation29
Vitamin D deficiency is common in thalassemia major patients. This deficiency coupled with low calcium levels leads to low BMD. In addition, genetic factors may also influence the BMD as reflected by low BMD in subjects with BB and FF genotypes.
The present study showed a high prevalence of low BMD in thalassemia patients, suggesting that they should be targeted for DXA screening and osteoporosis prevention before permanent end organ bone damage occurs. The BMD analysis should be coupled with the VDR genotyping as an additional test in these individuals who are susceptible to osteoporosis so that early preventive measurements can be taken.
Acknowledgements
Authors are thankful to Sanjay Gandhi Post graduate Institute of Medical Sciences, Lucknow for providing infrastructure facility and Council of Science and Technology-UP for providing funding to SA for research work. R.K. is thankful to CSIR-New Delhi for his fellowship.
References
- Domrongkitchaiporn S, Sirikulchayanonta V, Angchaisuksiri P, Stitchantrakul W, Kanokkantapong C, Rajatanavin R. Abnormalities in bone mineral density and bone histology in thalassemia. J Bone Miner Res. 2003;18:1682–8.
- Voskaridou E, Terpos E. New insights into the pathophysiology and management of osteoporosis in patients with beta thalassaemia. Br J Haematol. 2004;127:127–39.
- Bischoff-Ferrari HA, Dietrich T, Orav EJ, Dawson-Hughes B. Positive association between 25-hydroxy vitamin D levels and bone mineral density: a population-based study of younger and older adults. Am J Med. 2004;116:634–9.
- Meier C, Woitge HW, Witte K, Lemmer B, Seibel MJ. Supplementation with oral vitamin D3 and calcium during winter prevents seasonal bone loss: a randomized controlled open-label prospective trial. J Bone Miner Res. 2004;19:1221–30.
- Kanan RM, Varanasi SS, Francis RM, Parker L, Datta HK. Vitamin D receptor gene start codon polymorphism (FokI) and bone mineral density in healthy male subjects. Clin Endocrinol. 2000;53:93–8.
- Tajima O, Ashizawa N, Ishii T, Amagai H, Mashimo T, Liu LJ, et al. Interaction of the effects between vitamin D receptor polymorphism and exercise training on bone metabolism. J Appl Physiol. 2000;88:1271–6.
- Bell NH, Morrison NA, Nguyen TV, Eisman J, Hollis BW. ApaI polymorphisms of the vitamin D receptor predict bone density of the lumbar spine and not racial difference in bone density in young men. J Lab Clin Med. 2001;137:133–40.
- Braga V, Sangalli A, Malerba G, Mottes M, Mirandola S, Gatti D, et al. Relationship among VDR (BsmI and FokI), COLIA1, and CTR polymorphisms with bone mass, bone turnover markers, and sex hormones in men. Calcif Tissue Int. 2002;70:457–62.
- Morrison NA, George PM, Vaughan T, Tilyard MW, Frampton CM, Gilchrist NL. Vitamin D receptor genotypes influence the success of calcitriol therapy for recurrent vertebral fracture in osteoporosis. Ann Intern Med. 2006;145:302–4.
- Poncz M, Solowiejczyk D, Harpel B, Mory Y, Schwartz E, Surrey S. Construction of human gene libraries from small amounts of peripheral blood: analysis of beta-like globin genes. Hemoglobin. 1982;6:27–36.
- Morrison NA, Qi JC, Tokita A, Kelly PJ, Crofts L, Nguyen TV, et al. Prediction of bone density from vitamin D receptor alleles. Nature. 1994;367:284–7.
- Lundin AC, Söderkvist P, Eriksson B, Bergman-Jungeström M, Wingren S. Association of breast cancer progression with a vitamin D receptor gene polymorphism. South-East Sweden Breast Cancer Group. Cancer Res. 1999;59:2332–4.
- Harris SS, Eccleshall TR, Gross C, Dawson-Hughes B, Feldman D. The vitamin D receptor start codon polymorphism (FokI) and bone mineral density in premenopausal American black and white women. J Bone Miner Res. 1997;12:1043–8.
- Vichinsky EP. The morbidity of bone disease in thalassemia. Ann N Y Acad Sci. 1998;850:344–8.
- Vogiatzi MG, Autio KA, Schneider R, Giardina PJ. Low bone mass in prepubertal children with thalassemia major: insights into the pathogenesis of low bone mass in thalassemia. J Pediatr Endocrinol Metab. 2004;17:1415–21.
- Dresner Pollak R, Rachmilewitz E, Blumenfeld A, Idelson M, Goldfarb AW. Bone mineral metabolism in adults with beta-thalassaemia major and intermedia. Br J Haematol. 2000;111:902–7.
- Ferrara M, Matarese SM, Francese M, Borrelli B, Coppola A, Coppola L, et al. Effect of VDR polymorphisms on growth and bone mineral density in homozygous beta thalassaemia. Br J Haematol. 2002;117:436–40.
- El-Edel RH, Ghonaim MM, Abo-Salem OM, El-Nemr FM. Bone mineral density and vitamin d receptor polymorphism in β-thalassemia major. Pak J Pharm Sci. 2010;23:89–96.
- Hamed HM, Galal A, El Ghamrawy M, AbdEl Azeem K, A El Ghoroury E, Rasheed MA, et al. Vitamin D receptor polymorphisms and indices of bone turnover and bone mass in Egyptian children with sickle cell disease. Res J Med Med Sci. 2010;5:1–7.
- Nakamura K, Ueno K, Nishiwaki T, Okuda Y, Saito T, Tsuchiya Y, et al. Nutrition, mild hyperparathyroidism, and bone mineral density in young Japanese women. Am J Clin Nutr. 2005;82:1127–33.
- Vupputuri MR, Goswami R, Gupta N, Ray D, Tandon N, Kumar N. Prevalence and functional significance of 25-hydroxyvitamin D deficiency and vitamin D receptor gene polymorphisms in Asian Indians. Am J Clin Nutr. 2006;83:1411–9.
- Pirinççioğlu AG, Akpolat V, Köksal O, Haspolat K, Söker M. Bone mineral density in children with beta-thalassemia major in Diyarbakir. Bone. 2011;49(4):819–23.
- Frisk P, Arvidson J, Ljunggren O, Gustafsson J. Decreased bone mineral density in young adults treated with SCT in childhood: the role of 25-hydroxyvitamin D. Bone Marrow Transpl. 2011;47(5):657–62.
- De Sanctis V, Borsari G, Brachi S, Gubellini E, Gamberini MR, Carandina G. A rare cause of heart failure in iron-overload thalassaemic patients-primary hypoparathyroidism. Georgian Med News. 2008;156:111–3.
- Chatterton BE, Thomas CM, Schultz CG. Liver density measured by DEXA correlates with serum ferritin in patients with beta-thalassemia major. J Clin Densitom. 2003;6:283–8.
- Wu W, Zhi XM, Li DF, Lin K, Xu L, Yang YH. Vitamin D receptor gene polymorphism is not associated with bone mineral density of pre-menopausal women in Guangzhou. Nan Fang Yi Ke Da Xue Xue Bao. 2007;27:364–6.
- Spector TD, Keen RW, Arden NK, Morrison NA, Major PJ, Nguyen TV, et al. Influence of vitamin D receptor genotype on bone mineral density in postmenopausal women: a twin study in Britain. BMJ. 1995;310:1357–60.
- Nguyen TV, Esteban LM, White CP, Grant SF, Center JR, Gardiner EM, et al. Contribution of the collagen I alpha 1 and vitamin D receptor genes to the risk of hip fracture in elderly women. J Clin Endocrinol Metab. 2005;90:6575–9.
- Gogas Yavuz D, Keskin L, Kıyıcı S, Sert M, Yazıcı D, Sahin I, et al. Vitamin D receptor gene BsmI, FokI, ApaI, TaqI polymorphisms and bone mineral density in a group of Turkish type 1 diabetic patients. Acta Diabetol. 2011;48(4):329–36.