Abstract
A 58-year-old woman presented with rheumatoid arthritis-associated Evans syndrome (simultaneous autoimmune hemolytic anemia and autoimmune thrombocytopenic purpura); she was treated unsuccesfully with steroids, romiplostin, rituximab, immunoglobulin G, and splenectomy. The platelet count responded to the combined use of prednisone, eltrombopag, and romiplostin. It may be more reasonable to use combined treatments than sequential monotherapies.
Introduction
Thrombopoietin (TPO) is the key cytokine involved in thrombopoiesis, being the endogenous ligand for the TPO receptor that is expressed on the surface of platelets, megakaryocytes, and megakaryocytic precursors. First-generation thrombopoietic agents were recombinant forms of human TPO, but their development was discontinued after prolonged thrombocytopenia due to the observation of neutralizing auto-antibodies cross-reacting with endogenous TPO. Second-generation thrombopoiesis-stimulating molecules are now available, which have unique pharmacological properties and no sequence homology to endogenous TPO. Two of these new agents, romiplostim and eltrombopag, have already completed phase III trials in primary immune thrombocytopenia and have been granted marketing authorization for use in this disease.Citation1 Phase II and III trials with these novel drugs are ongoing in other conditions characterized by thrombocytopenia, such as chemotherapy, chronic liver disease, and myelodysplastic syndromes. Most of the other second-generation thrombopoietic growth factors are in early-phase clinical development.
Evans syndrome is an uncommon condition defined by the combination, either simultaneously or sequentially, of immune thrombocytopenic purpura and autoimmune hemolytic anemia with a positive direct antiglobulin test in the absence of known underlying etiology.Citation2 First-line therapy is usually corticosteroids and/or intravenous immunoglobulin, to which most patients respond; however, relapse is frequent. Options for second-line therapy include immunosuppressive drugs, especially cyclosporin or mycophenolate mofetil, vincristine, danazol, or a combination of these agents. More recently, patients have been treated with rituximab, which induces remission in the majority, although such responses are short in duration, splenectomy may also be considered although long-term remissions are less frequent than in uncomplicated immune thrombocytopenic purpura (ITP). For very severe and refractory cases stem cell transplantation offers the only chance of long-term cure.Citation3 The use of TPO receptor (TPO-R) agonists has been recently described: one patient responded promptly to the use of romiplostin in a case of Evans syndrome which was refractory to cyclophosphamide and rituximab.Citation4 No cases of simultaneous administration use of two TPO-R agonists have been described to the best of our knowledge in this setting.
Case presentation
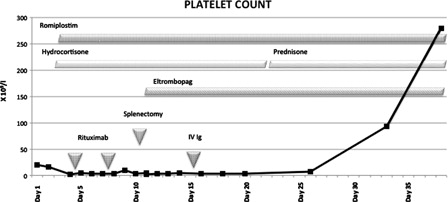
This 58-year-old lady had been treated for rheumatoid arthritis with non-steroidal anti-inflammatory drugs during 20 months. She presented with purpura and symptoms of anemia. The laboratory workup showed anemia (7.7 gr/dl), severe thrombocytopenia (2 × 109/l), increased LDH levels (284 UI/l), reticulocytosis (6%), positive direct antiglobulin test, and anti-platelet antibodies. Rheumatoid factor and antinuclear antibodies were positive but anti-native DNA antibodies were negative. The bone marrow study disclosed multilineage hypercellularity. The patient was admitted to the hospital and intravenous hydrocortisone (300 mg/day) was started, together with romiplostin (250 mg/week), platelets and packed red blood cells were transfused as needed. depicts the use of several treatments. On days 4 and 8, rituximab (100 mg/dose) was delivered. On day 11, laparoscopic splenectomy was performed. On day 12, eltrombopag (50 mg/day) was started. On day 15, intravenous immunoglobulin G (IVIg, 30 g) was delivered; at this point hemolysis diminished. On day 23, she was discharged from the hospital. The patient remained with severe thrombocytopenia until day 26, when a steady increase of platelet count ensued; she was then receiving prednisone (20 mg/day), romiplostin, and eltrombopag (see ). Forty days later the patient remains with a normal platelet count receiving prednisone (10 mg/day), romiplostin (250 mg/week), and eltrombopag (50 mg/day).
Discussion
The development of thrombocytopenia in Evans syndrome might be associated with both increased platelet destruction and insufficient platelet production.Citation2 Corticosteroids and IVIg therapy reduce platelet destruction, whereas TPO-R agonists increase platelet production.Citation1 TPO-R agonists have been shown to be useful in the treatment of several thrombocytopenic states other than primary autoimmune thrombocytopenia. TPO-R agonists have been useful in resolving the thrombocytopenia of dengue hemorraghic fever,Citation5 graft versus host disease,Citation6 myelodisplasia,Citation7 liver diseases,Citation8 chronic lymphocytic leukemia,Citation9 chemotherapy-induced thrombocytopenia,Citation10 Evans syndrome,Citation4 and other conditions.Citation11 Despite the fact that romiplostin and eltrombopag have similar mechanisms of action,Citation1,Citation11 some differences may explain cases in which thrombocytopenia responds to one but not the other of these two TPO-R agonists.Citation4,Citation12 These differences should also support the combined use of these two TPO-R agonist drugs or with other ones shown to be useful in the treatment of thrombocytopenia.Citation13
In this case, the combination of romiplostin, steroids, rituximab, and splenectomy was unable to resolve the thrombocytopenia, which finally reverted during the combined simultaneous use of romiplostin, eltrombopag, and prednisone. It is clear that the resolution of the thrombocytopenia may have also been induced by all the previous treatments delivered to the patient, included IVIg (see ).
Conclusion
The response observed in this patient suggests that the combined use of drugs, which either reduce platelet destruction or induce platelet production, may be a reasonable approach in cases of refractory thrombocytopenia; it may be more reasonable to use combined treatments than sequential monotherapies. Additional studies are needed to support this observation.
References
- Stasi R, Bosworth J, Rhodes E, Shannon MS, Willis F, Gordon-Smith EC. Thrombopoietic agents. Blood Rev. 2010;24(4–5):179–90.
- Ruiz-Argüelles A. Anemias hemolíticas inmunológicas. In: , Ruiz-Argüelles GJ(eds.) Fundamentos de Hematologìa. 4th ed. Editorial Médica Panamericana. Mexico City, México; 2009. p. 107–16.
- Norton A, Roberts I. Management of Evans syndrome. Br J Haematol. 2006;132(2):125–37.
- González-Nieto JA, Martin-Suarez I, Quattrino S, Ortiz-Lopez E, Muñoz-Beamud FR, Colchero-Fernández J, et al. The efficacy of romiplostim in the treatment of severe thrombocytopenia associated to Evans syndrome refractory to rituximab. Lupus. 2011;20(12):1321–3.
- Rodríguez-Mejorada S, Rosel-Gómez C, Rosado-Castro RA, Domingo-Padilla MA, Ruiz-Delgado GJ. Romiplostim reverts the thrombocytopenia in dengue hemorrhagic fever. Hematol Oncol Stem Cell Ther. 2011;4:48–9.
- Ruiz-Delgado GJ, Lutz-Presno J, Ruiz-Argüelles GJ. Romiplostin may revert the thrombocytopenia in graft versus host disease. Hematology. 2011;16:108–9.
- Kantarjian HM, Giles FJ, Greenberg PL, Paquette RL, Wang ES, Gabrilove JL, et al. Phase II study of romiplostim in patients with low- or intermediate-risk myelodysplastic syndrome receiving azacitidine therapy. Blood. 2010;116:3163–70.
- Moussa MM, Mowafy N. Pre-operative use of romiplostim in thrombocytopenic patients with chronic hepatitis C and liver cirrhosis. J Gastroenterol Hepatol. 2012 July 31. doi: 10.1111/j.1440-1746.2012.07246.x. [Epub ahead of print].
- D'Arena G, Cascavilla N. Romiplostim for chronic lymphocytic leukemia-associated immune thrombocytopenia. Leuk Lymphoma. 2011;52:701–4.
- Demeter J, Istenes I, Fodor A, Paksi M, Dombi P, Valasinyószki E, et al. Efficacy of romiplostim in the treatment of chemotherapy induced thrombocytopenia (CIT) in a patient with mantle cell lymphoma. Pathol Oncol Res. 2011;17:141–3.
- Newland A. Thrombopoietin: too much or too little? Hematology. 2012;17( Suppl. 1):S-166–8.
- No authors listed. Eltrombopag. Idiopathic thrombocytopenic purpura after treatment failure: romiplostim is a better option. Prescrire Int. 2010;19(105):15.
- Mitsuhashi K, Ishiyama M, Imai Y, Shiseki M, Mori N, Teramura M, et al. Combined romiplostin and intravenous immunoglobulin therapy increased platelet count, facilitating splenectomy in a patient with refractory immune thrombocytopenic purpura unresponsive to monotherapy. Brit J Haematol. 2012;158:798–800.