Abstract
Community musculoskeletal services in Ealing are organized with an integrated care approach, with most patients being managed in primary care and community settings, while, at the same time, providing clear and fast routes to secondary care. This is both clinically effective and cost-effective, reserving hospital referral for patients most likely to need surgery. Ealing Clinical Commissioning Group (CCG) implemented a ‘See and Treat’ interface clinic model to improve surgical conversion rates, reduce unnecessary hospital referrals, and provide community treatment more efficiently than a triage model. A high-profile general practitioner (GP) education programme enabled GPs to triage in their practices and manage patients without referral. The integrated care approach was implemented incrementally in three phases between 2005 and 2013, with a fourth phase planned for 2015. In Phase 3, only patients triaged by GPs to hospital outpatients are triaged by a referral management service, serviced by senior clinicians from the community musculoskeletal service. This secondary triage accounts for 15% of total GP referrals. The remainder being booked directly with no further triage beyond the initial GP triage unless marked ‘urgent’.
Background
Demographics
Ealing is an urban borough situated in West London. It is the third largest London boroughCitation1 with a population of 347 000.Citation2 The population's black and minority ethnic (BME) communities constitute 38% of Ealing's total population.Citation3 This compares with approximately 30% of London's population.Citation2 The age–sex distribution of the population in Ealing is slightly younger than the national average.Citation2 Ealing is a relatively prosperous borough. Nevertheless, the level of deprivation in the east and west of the borough means that overall, Ealing is in the top quintile in England.Citation2 The population of Ealing is served by nine surrounding hospitals within a 7 mile radius in West London,Citation4 with the largest provider having a share of 46% of outpatient activity.Citation5
Healthcare and societal burden
Providing musculoskeletal care is set in the context that 20% of the general practitioner (GP) registered population present each year with a musculoskeletal disorderCitation6,Citation7 and about 50% of these patients are managed by GPs without referral.Citation8 Musculoskeletal disorders are the third highest cause of disability life adjusted years in the UK (after cancer and cardiovascular disease).Citation9 Musculoskeletal disorders account for 30% of all causes of years lived with a disabilityCitation9 and one-third of the population over 65 suffer with a chronic musculoskeletal disorder.Citation10 About 8.5% of the adult population have severe chronic musculoskeletal or neurological pain.Citation11 There is major co-morbidity with cardiovascular disease, diabetes, hypertension, and depression.Citation12 About 11.2 million working days per year are lost through musculoskeletal problems.Citation13
Care closer to home and integrated care
Providing care closer to home has been national policy in successive white papers since the National Health Service (NHS) Plan 2000.Citation14 It is an implied and embedded method of achieving the outcome indicators in ‘Everyone Counts – planning’ published by the new NHS Commissioning Board in 2012.Citation15 The Department of Health piloted a number of models for delivering care closer to home, including practitioners with special interest (GPs, extended scope physiotherapists, and nurses), specialist outreach clinics, interface clinics, and admission avoidance schemes.Citation16
However, a recent systematic review of outcomes of care closer to home schemes showed that although patients appreciate the schemes, care was not shown to be consistently better or worse than in the hospital.Citation16 The schemes reviewed were not conclusively shown to be cost-effective and the report cautioned those wishing to replicate or roll out similar services that one model ‘doesn't fit all’.Citation16
The King's Fund and the Nuffield Trust reviewed models of providing integrated care.Citation17 They concluded that integrated care services could fill the gaps in traditional care models or could be used where there is poor coordination of care, which might lead to an adverse impact on care experiences and outcomes.Citation17 The review concluded that integrated care models should be centred around the needs of patients and are best suited to those people with chronic long-term conditions or medically complex needs.Citation17 The report cautioned that disease-based approaches rather than patient-centred service delivery could lead to new silos of care.Citation17
Musculoskeletal services in Ealing
Community and secondary care
In addition to the 50% of patients presenting with musculoskeletal disorders managed by GPs without referrals, care is provided in community and hospital settings. Phase 2 of the musculoskeletal service redesign brought in a community based ‘See and Treat’ interface service and a GP direct access physiotherapy service in 2007. The descriptionCitation18 and performanceCitation19 of this service have been reported elsewhere.
Local healthcare expenditure and activity
Historically, health expenditure on musculoskeletal disorders in Ealing has been low, more than two standard deviations below the mean. In 2009, programme budgeting data for musculoskeletal problems showed funding at 49% of the national averageCitation20 and yet the service was providing activity at 86% of the national average.Citation21,Citation22 However, Ealing has a slightly higher average programme budget on ‘miscellaneous’ items, which might include some musculoskeletal expenditure.Citation23 Nevertheless, out of a total £1413 expenditure per head of population in Ealing, only £45 per head is spent on musculoskeletal disorders.Citation24
In April 2011, Ealing Primary Care Trust (PCT) divested itself of its provider services, including community physiotherapy. Previously, since the demise of fundholding in 1988, the PCT had been providing both community physiotherapy services and the Ealing hospital outpatient physiotherapy service. From April 2011, the community services of Ealing, Brent, and Harrow were hosted by Ealing Hospital NHS Trust, which formed an ‘integrated care organisation’. This merger was instrumental in achieving service redesign because it overcame a significant obstacle to moving away from the status quo caused by the Department of Health's ‘payment by results’ policy.
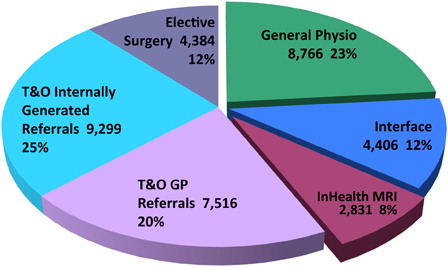
shows how all musculoskeletal activity was divided across community and secondary care prior to Phase 3 of the service redesign. Programme budgeting data show that the 12% of elective surgical activity accounted for 55% of the budget.Citation23 The total secondary care activity accounted for 82% of the budget.Citation23
Performance of local musculoskeletal services
The corollary of both historical underfunding and below average activity was long waiting lists for physiotherapy and elective orthopaedic admissions for Ealing residents. Although the latter was largely addressed by the 18 weeks initiative,Citation25 physiotherapy waits have varied between a median of 22 and 26 weeks since the demise of fundholding in 1998.Citation26 However, with the introduction of Phase 3 of the MSk service redesign in October 2013, median physiotherapy waiting times are down to 8 weeks and interface clinic waiting times are down to 7 weeks.Citation26
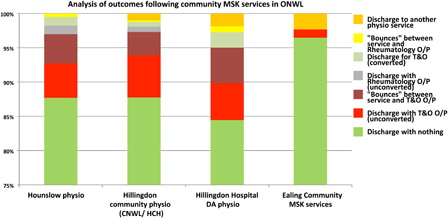
External audit of efficiency
In late 2011, the Delivery Support Unit (DSU) for the eight north west (NW) London PCTs reported on the efficiency of different models of musculoskeletal service provision across the cluster.Citation27,Citation28 The DSU tracked patients by NHS number across community musculoskeletal services, GP access to magnetic resonance imaging (MRI) scanning, hospital rheumatology and orthopaedic outpatients, orthopaedic day case and inpatient activity. They commented that the ‘See and Treat’ service in Ealing had outcomes that ‘appear to be exceptionally strong, with 96% of patients discharged not subsequently receiving treatment in other settings of care. This represents a 10–12% higher performance than other, similar scope services in NW London’Citation27 (see below).
Secondary care activity
Secondary uses statistics data supplied by the NWL Commissioning Support Unit for Ealing Clinical Commissioning Group (CCG) showed a 5% fall in the number of first appointments in orthopaedic outpatients, from all sources, comparing the year to August 2013 with the year to August 2012.Citation29 This was fuelled principally by a drop in GP referrals to outpatients and mirrored by an increase in referrals to the interface service. Over the same period there was a 9.2% drop in elective orthopaedic admissions and a 2.3% drop in day case activity.Citation29 The cause of these drops is multifactorial, including the effectiveness of the Ealing interface service, changes in the acute contracts negotiated by the NW London CCG cluster, and the enforcement of the NW London Planned Procedures with Thresholds (PPwT) policy.Citation30
GP direct access MRI scans
GP access to MRI scanning was purchased from 2007 as part of the 18-week referral to treatment standard by NHS London from a private provider (InHealth, High Wycombe, UK). The Department of Health set milestones for maximum diagnostic waiting times of 6 weeks by 2008.Citation25 The DSU analysis of GP-access to MRI scanning showed that GP-access MRI usage was not associated with treatment in musculoskeletal or orthopaedic clinics or surgery in 60% of patients, and no further NHS treatment in 50% of patients.Citation27 The DSU also demonstrated that where patients had a MRI scan organized by the GP, multiple and complex pathways occurred in 20% of patients and suggested that patients ‘may not be treated in the most appropriate setting’.Citation27
Local guidelines for MRI scanning from primary careCitation31 formed the backbone of high-profile GP education sessions in 2010 and 2012. Monthly returns from the MRI provider (InHealth Ltd) demonstrated a 42% drop in MRI scanning in 2011. Nevertheless, the InHealth data showed that 20% of GP practices continued to request about 80% of the GP-access MRI scans, and MRI rates per 1000 population varied more than 5-fold between practices.Citation32 MRI scanning rates started to rise again and exceeded previous levels by early 2013.Citation33
The GP-access MRI usage data suggested no correlation between MRI scanning, subsequent reduction in healthcare utilization, or scanning as per local clinical guidelines. Therefore, the CCG board accepted a proposal to decommission the GP-access MRI service and re-provision MRI scanning via the interface service as part of the Phase 3 MSk service redesign.Citation34 The quality, innovation, productivity, and prevention (QIPP) improvements and savings resulting from the Phase 3 MSk service redesign have subsequently resulted in quicker access to MRI scanning for those patients where it is clinically necessary, as well as providing earlier access to a clinical opinion, definitive treatment, and increased physiotherapy capacity.
Delivering service change in Ealing
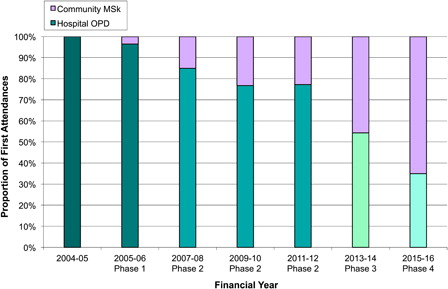
Ealing is in a densely populated area of West London,Citation1 surrounded by nine hospitals providing orthopaedic services.Citation4 Since the inception of CCGs in 2012, each hospital relates to a single CCG that negotiates the acute commissioning contracts on behalf of the other CCGs served by that hospital. However, each CCG has its own Joint Strategic Needs Assessment (JSNA), Commissioning Intentions, and Out of Hospital Strategy and is responsible for commissioning local community services. Ealing PCT considered commissioning a prime vendor model for musculoskeletal service delivery for its residents in 2008 and 2011. However, it was not possible to reach agreement on a prime vendor or other unified model for musculoskeletal service delivery across multiple commissioners and providers in NW London, leaving each CCG (and former PCT) to develop its musculoskeletal service strategy in a piecemeal fashion. Ealing has redesigned musculoskeletal services in a series of three stages to date, and a fourth stage planned for 2015. The effect of this staged approach is shown in below, which shows how the proportion of patients seen in hospital orthopaedic clinics has decreased as patients have transferred to a community interface setting.
Figure 3. Phased MSk service redesign: Ealing – proportion of first attendances: Hospital Orthopaedics and Community Musculoskeletal Interface (% per financial year, all referral sources) (figures are predictions for 2013–2016).
Phase 3 MSk service redesign, 2013
Aims and objectives
The overarching aims of the musculoskeletal service redesign are: to commission high quality and efficient musculoskeletal services that meet the needs of the population, to make best and evidence-based use of scarce healthcare resources, to provide patient choice with services closer to home, to decommission services that are less efficient, and to recycle savings in accordance with the QIPP programme for Ealing CCG.
The specific objectives for the musculoskeletal service redesign are: to commission an enhanced musculoskeletal interface service with consultant input, to expand physiotherapy services, to improve the conversion rates of trauma and orthopaedic outpatient referrals, to reduce unnecessary MRI scanning activity, and to use savings from activity reductions and tariff changes to invest in the expanded community musculoskeletal service.
Costs of service redesign
The full business case for Phase 3 was approved by the CCG Board in March 2013.Citation34 The business caseCitation35 allowed for a 5% annual increase in baseline elective inpatient orthopaedic activity due to population growth, ageing, and obesity; factors which were shown in the Musculoskeletal Framework to be drivers for increasing joint replacement surgery.Citation36 Moving 40% of GP referrals from orthopaedic outpatients to community interface service disinvests £1.17 million per year. Decommissioning GP-access MRI saves £395k per year. Reinvestment in community services costs £1.06 million per year. This includes a small increase in both MRI scanning and onward referrals from the interface service. A one-off waiting physiotherapy waiting list initiative of £200k was granted prior to the start of the new service delivery. The net annual net saving after year 1 is £507k per year.Citation35
Referral pathways
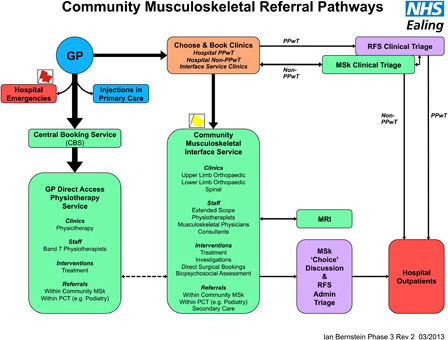
GPs are encouraged to refer patients, whom they would previously have sent for GP-access MRI scanning or orthopaedic outpatients, to the musculoskeletal interface service. This pathway reflects the concept that GP triage patients in their practice. The other triage options for GPs are to refer to physiotherapy or to orthopaedic outpatients. below, shows the referral pathways from a GP perspective, following the Phase 3 MSk service redesign.
Orthopaedic referrals
In accordance with the NW London CCG Cluster PPwT policy, 13 orthopaedic procedures (e.g. hip and knee arthroplasty or revision surgery, arthroscopy, carpal tunnel release) are subject to clinical criteria and thresholds before funding is agreed.Citation30 In NW London, referrals for these procedures have to be made on bespoke ‘Choose and Book’ referral forms and the criteria are checked by each CCG's referral management service. Assuming the GP ticks all the boxes (e.g. to confirm conservative treatment has been tried), the commissioner will pay the provider for the PPwT procedure.
For non-PPwT orthopaedic outpatient referrals from GPs, there is an online triage carried out by senior clinicians from the musculoskeletal service. They can divert patients to the interface or physiotherapy service where it is clinically appropriate to do so (e.g. where conservative options have not been tried, to allow assessment for surgery or where appropriate investigations need to be completed if on a surgical pathway). Alternatively, they can allow the referral to be passed to the hospital. To reduce the administrative burden and delays for the patient, GPs are encouraged to send patients directly to the interface service, in which case no further triage occurs. The business case assumed that at least 55% of GP referrals to orthopaedic outpatients could be seen and treated in the community. This figure is expected to rise to 70% once consultants are in place in the community interface clinics. These figures are predicated upon the low surgical conversion rates (20–30%) for GP referrals direct to hospital compared with 80% from the interface clinic.Citation19,Citation27,Citation37,Citation38 The reason that a diversion figure of only 55% was used for Phase 3 is that following Phases 1 and 2 of the MSk service redesign, GPs are already using the interface service for 37% of their referral activity (see above).
Community staffing, capacity, and outcomes
The interface service is led by a consultant physiotherapist and staffed by 10.7 whole time equivalent (WTE) extended scope physiotherapists and 1.3 WTE musculoskeletal physicians. The interface service has been funded to ‘See and Treat’ 7730 patients per year. The physiotherapy service is staffed by 12 WTE band 7 and 3 WTE band 6 physiotherapists. The physiotherapy service has been funded to treat 10 230 patients per year.
The interface service has three clinics seeing the following proportions of referrals: spinal (44%), lower limb (38%), and upper limb (18%). Seven per cent of patients are cross-referred for further physiotherapy or classes. The onward referral rate to secondary care is 19%, and is expected to rise a little with the recent service redesign. The MRI rate is 17% and is also expected to rise a little.Citation26,Citation34 The surgical conversion rates are spinal 60%, lower limb 84%, and upper limb 90%.Citation38
As part of the Phase 3 MSk service redesign, recruitment is under way for consultant input: two sessions per week of spinal consultant input, one session per week of upper limb orthopaedic input, one session per week of lower limb orthopaedic input, and one session per week of clinical radiology support. The consultants will be drawn from several secondary care providers to support transparency of patient choice of the surgical provider.
Orthopaedic outpatient activity
The full business case for Phase 3 of the MSk service redesign predicts that activity will shift from outpatients for 3400 patients, who will either be referred directly by GPs to the interface service or diverted by the online triage.Citation35 Consultant-to-consultant and A&E referrals to orthopaedic outpatients are assumed to remain unchanged at 7000 referrals per year. This activity is a potential target for Phase 4 of the MSk service redesign.
Booking and triage services
About 23 000 referrals per year are expected to be handled by the booking and referral management services across physiotherapy, interface, and orthopaedic referrals. About 10–15% of these referrals will be triaged online by the musculoskeletal clinicians supporting the GP Referral Management Service; the remainder will be booked directly by GPs into community clinics. Phase 3 of the MSk service redesign sees a genuine 50% increase in physiotherapy service provision. There is also a 42% increase in interface capacity, but this is dedicated to patients diverted from hospital outpatients.
Waiting times
Phase 3 of the service redesign has brought shorter waiting times for definitive treatment and investigations for the majority of patients. Median physiotherapy waiting times are down to 8 weeks and interface clinic waiting times are down to 7 weeks, both with a target of 4 weeks by April 2014.Citation26 Urgent referrals are currently seen within 2 weeks, and MRI scans can be arranged within 1–4 weeks depending on clinical priority.
Evaluation
Assessing whether integrated service redesign has delivered improvements in care and quality is complex. The King's Fund advises that the appraisal of such schemes should include the impact on outcomes (e.g. NHS Outcomes Framework), patient experience, use of upstream and downstream services, and costs in different parts of the system.Citation17 The King's Fund imply that integrated care redesigns under the current NHS market arrangements reduce patient choice initially through the focus on producing tightly integrated and seamless care with a limited number of providers.Citation39,Citation40 The King's Fund believes that the NHS will need to seek ways of providing choice both within and between integrated care models to drive forward innovations in care.Citation39 In addition, the King's Fund advises that the NHS should support the role of integration in improving patient outcomes.Citation39 However, they warn that focusing on disease-specific models will lead to ‘silos of care’Citation41 rather than holistic care. With these warnings in mind, the Ealing musculoskeletal service will be offering a choice of consultants from different secondary care trusts, and linking up with the education programmes supporting local integrated care pilots for diabetes and frail elderly patients.
Developing primary care
Empowering primary care
A key feature of moving care closer to home is empowering and resourcing primary care.Citation42 Primary care clinicians are well placed to carry out primary triage, signposting, and gatekeeping functions. Primary care clinicians are also pivotal in coordinating care for patients with complex pathways of care.Citation42 GPs are trained to manage patients with multiple morbidities, and are doing so in other settings, e.g. frail elderly and diabetic patients. Primary care nurses deliver core treatments for musculoskeletal disorders including education, advice on losing weight and exercise advice for osteoarthritis, and cardiovascular and osteoporosis screening for patients with inflammatory arthritis. Primary care nurses also share management of disease monitoring for patients on disease modifying drugs for inflammatory arthritides.
However, much of the movement of this work from secondary to primary care has occurred with little support. A high quality and on-going ‘hands-on’ education programme is needed to support GPs, practice nurses, and community nurses to deliver care closer to home for patients with long-term musculoskeletal disorders, particularly in the presence of co-morbidities.
The current model of commissioning in the NHS is clinically led, principally by GPs. GPs are therefore key stakeholders and drivers for change. They need to ensure that as care moves from secondary to primary care, this is achieved with adequate clinical resources, educational support, and with full assessment and mitigation of the clinical risks associated with a new service delivery model.
Primary care workforce training
Ealing PCT took a conscious decision in 2008 that the redesign of the musculoskeletal service provided an opportunity to supplement the meagre undergraduate trainingCitation43 for GPs in musculoskeletal medicine. Ealing PCT abandoned plans for a ‘hub and spoke’ model proposed in 2004. That proposal placed a musculoskeletal triage service at the hub and required GPs to refer all musculoskeletal problems for detailed needs assessment. Instead the PCT funded an ambitious education programme to facilitate GPs triaging patients in their practices into one of four streams: direct access physiotherapy, and spinal, upper, and lower limb interface clinics. The Ealing Action Line was developed for active management in primary care without referral, along with a referral flowchart and local referral advice.Citation44 Key elements of the education programme were to help GPs deliver core musculoskeletal treatments, improve examination skills, and develop confidence with diagnosing and managing musculoskeletal problems. To date, about 50% of Ealing GPs have been through the education programme, and many have refreshed their skills on more than one occasion.
The recent Phase 3 MSk service redesign built on earlier changes and continues to empower GPs to actively manage about 50% of all musculoskeletal disorders presenting in primary care without referral. Individual GP triage in their practices remains central. Secondary triage is targeted at orthopaedic referrals (PPwT and non-PPwT) and accounts for 15% of total GP referrals; the remainder being booked directly with no further triage beyond the initial GP triage. In addition, any urgent requests directly to the interface or physiotherapy service may be triaged where this challenges short-term capacity. Referral adviceCitation44 has remained consistent over the past 5 years and is distributed regularly to GPs, other community staff, and hospital staff. The musculoskeletal education programme continues to be available to GPs, practice nurses, nurse practitioners, community matrons, and other community staff including podiatry and mental health workers. The programme will be offered to A&E and hospital staff to raise awareness of community options, patient pathways, and ensure patients are given consistent messages, for instance, about the indications for MRI scanning or the role of exercise and physiotherapy. The educational programme therefore remains aligned with service development needs and moving care closer to home.
Drivers and obstacles to change
Drivers for change
The main driver for change in Ealing was the long waiting lists for physiotherapy (median 22 weeks (2012–2013)).Citation26 MRI scans from the interface clinic were available in 3–5 weeks. If a scan was deemed more urgent than this, the only recourse was to request an opinion from the on-call orthopaedic team at one of the local hospitals. Phase 3 of the service redesign has addressed both of these issues.
The JSNA for the London Borough of EalingCitation3 has included a substantial musculoskeletal chapter since 2010, which in turn has informed the Ealing Commissioning Intentions,Citation45 Joint Prevention Strategy,Citation46 Out of Hospital Strategy,Citation47 and the Health and Wellbeing Strategy.Citation48 Having good access to musculoskeletal assessment and treatment, as well as empowering general practice to deliver core treatments is instrumental in delivering these plans locally.
Future JSNAs can be strengthened in the light of recent data from the Global Burden of Disease (GBD) study with UK data analysis,Citation9 supported by Public Health England and pioneering work by Arthritis Research UK.Citation49 The GBD study provided a composite index of normative health (disability-adjusted life years), which means that commissioners and providers will be now able to focus on long-term conditions with high morbidity in addition to those conditions with significant mortality. Musculoskeletal services in Ealing historically incurred relatively low expenditure (£45/head out of a total CCG spend of £1413/head),Citation24 although the number of people requiring assessment, advice, and treatment is high (20% of the population).Citation6,Citation10 As there are public health interventions that can improve musculoskeletal health (exercise, weight loss),Citation9 this can be reflected in the local Health and Well Being strategy, which aims to translate the JSNA into local action points.
The QIPP challenge aims to save the NHS £15–20 billion by 2014 while keeping quality as an organizing principle.Citation50,Citation51 Underlying both the commissioners’ and providers’ plans for the current service redesign is the financial requirement to produce savings while improving the service and maintaining quality.
Overcoming obstacles – the context of change
The main obstacle to Phase 3 of the service redesign has been the frequent reorganization of the NHS. Payment by results provided a significant disincentive for local hospitals to engage in moving services ‘off tariff’ into the community. However, the formation of the Ealing Hospital NHS Trust Integrated Care Organisation in April 2011 was a game-changer in facilitating progress with service redesign. In moving hospital services to the community, one of the hospitals serving the Ealing population could mitigate its financial losses caused by outpatient work moving off tariff by recouping work under a block community contract and also becoming an MRI provider to the interface service.
The move to divest community services from PCTs to provider trusts in 2010–2011 produced additional delay in the MSk service redesign as the merger of the community services with the new host (Ealing Hospital NHS Trust) diverted project management resources away from the MSk service redesign. A number of changes to commissioning arrangements also meant that continuity and consistency of approach was impeded over the period from 2010 to present. In particular, the QIPP challenge meant that commissioning acute services was split away from commissioning community services. The former was dealt with at a cluster level with eight PCTs, the latter at local level for one PCT. Developing an integrated plan across primary community and secondary care was difficult as commissioners at local and cluster level had differing priorities. In fact, the evolution of CCGs following the Health and Social Care Act 2012 has finally driven through the service redesign as priority setting now resided with local clinicians. The new CCG board was focused on addressing a long-standing health inequality, informed by the local JSNA, and were prepared to overcome the obfuscation produced by previous commissioning arrangements.
The challenging economic position meant that CCG finance officers were risk averse and it was difficult to push a case for ‘invest to save’ pump-priming funds. The local provider advised that the service redesign could not proceed until the physiotherapy waiting lists had been cleared. A risk sharing scheme was therefore devised between the commissioner and the provider to achieve the reduction in waiting times before the Phase 3 of the service redesign went live in October 2013.
GPs make up the majority of the CCG executive board, which drives innovation. However, at grass roots, primary care colleagues are weary of change, which may lead to inertia during the implementation phases of a service redesign. There is no doubt that moving care closer to home has pushed work towards general practice, for instance: musculoskeletal assessments, core treatments, and active management without referral. The Royal College of General Practitioners press release highlighted that investment in general practice has fallen by £400 million in real terms in the past 3 years, resulting in a 7% cut in spending per patient.Citation52 In addition, GP spending is 9% of total NHS budget whereas GPs have 90% of contacts with patients.Citation52 It has been an interesting challenge to motivate colleagues through the MSk service redesign's communications stage.
Conclusion
The success of the MSk service redesign is founded on keeping the patient's perspective at the centre of all decision-making. The MSk Core Strategy Group has demonstrated strong leadership and persistence over a number of years to design and steer the service redesign. They have been strongly supported by the new CCG executive. Engaging and maintaining good communications with the main stakeholders facilitated the provider to move away from a hospital-based ‘payment by results’ tariff model and secured support from GPs for a model ‘closer to home’. The education programme has improved confidence in musculoskeletal diagnosis, empowered primary care to deliver core treatments, and improved the quality and appropriateness of referrals. Until we have better outcome data, we cannot be sure that patients who might previously have had hospital inpatient and day case surgery will enjoy similar outcomes with conservative treatment closer to home. However, we believe that this is making the best use of scarce resources and is of overall benefit to the vast majority of patients. Reassuringly, GPs, commissioners, and providers are sharing accountability for delivering clinical, organization, and financial outcomes.
Declaration of interests
Funding none.
Ethical approval not required.
I.B. is a clinical advisor to NHS Ealing CCG and the Arthritis and Musculoskeletal Alliance. He is also a musculoskeletal physician with Ealing Hospital NHS Trust Community Musculoskeletal Service.
Note on references
A supplementary file is available online, in which the URLs below are repeated in a more easily to copy format.
Acknowledgements
I wish to acknowledge the help of the MSk Core Strategy Group in preparing this paper and for permission to use audit data: Rochelle Bloch, Justine Currie, Stephanie Griffiths, Kate Laverty, Robert McLaren, and Neha Unadkat.
References
- Ealing Council. About us. London [accessed 2013 Nov 19]. Available from: http://www.ealing.gov.uk/aboutus.
- London.gov.uk [Internet]. GLA Population Projections 2012 Round, SHLAA, Borough SYA. Excel URL. London [accessed 2013 Nov 19]. Available from: http://data.london.gov.uk/datastore/package/gla-population-projections-2012-round-shlaa-borough-sya.
- Ealing Council. Ealing joint strategic needs assessment. London [accessed 2013 Nov 19]. Available from: http://www.ealing.gov.uk/downloads/download/1018/ealing_joint_strategic_needs_assessment.
- NHS NW London. Shaping a healthier future. London [accessed 2013 Nov 19]. Available from: http://www.healthiernorthwestlondon.nhs.uk/.
- Health and Social Care Information Centre. NHS comparators. Leeds [accessed 2013 Nov 19]. Available from: https://nww.nhscomparators.nhs.uk/.
- Arthritis Research Council. Arthritis: The Big Picture. 2002 [accessed 2013 Nov 19]. Available from: http://www.ipsos-mori.com/Assets/Docs/Archive/Polls/arthritis.pdf.
- Arthritis Research UK National Primary Care Centre. Musculoskeletal Matters: What do general practitioners see? Keele University, 2009 [accessed 2013 Nov 19]. Available from: http://www.keele.ac.uk/media/keeleuniversity/ri/primarycare/bulletins/MusculoskeletalMatters1.pdf.
- Savigny P, Kuntze S, Watson P, Underwood M, Ritchie G, Cotterell M, et al. Low back pain: early management of persistent non-specific low back pain. London: National Collaborating Centre for Primary Care and Royal College of General Practitioners; [accessed 2013 Dec 16]. Available from http://www.nice.org.uk/nicemedia/live/11887/44334/44334.pdf.
- Murray CJL, Richards MA, Newton JN, Fenton KA, Anderson HR, Atkinson C, et al. UK health performance: findings of the Global Burden of Disease Study 2010. Lancet 2013;381(9871):997–1020 [accessed 2013 Nov 19]. Available from: http://dx.doi.org/10.1016/S0140-6736(13)60355-4 and http://viz.healthmetricsandevaluation.org/gbd-compare/.
- Clarke A, Symmons D. The burden of rheumatic disease. Medicine 2006;34(9):333–5 [accessed 2013 Nov 19]. Available from: http://dx.doi.org/10.1053/j.mpmed.2006.06.007.
- Price C. National Pain Audit Final Report. London: Health Quality Improvement Partnership; 2012 [accessed 2013 Nov 19]. Available from: http://www.nationalpainaudit.org.
- Guthrie B, Payne K, Alderson P, McMurdo MET, Mercer SW. Adapting clinical guidelines to take account of multimorbidity. BMJ 2012;345:e6341 [accessed 2013 Nov 19]. Available from: http://dx.doi.org/10.1136/bmj.e6341.
- Arthritis and Musculoskeletal Alliance. Joint working? An audit of the implementation of the Department of Health's musculoskeletal services framework. London: ARMA; 2009 [accessed 2013 Nov 19]. Available from: http://www.arma.uk.net/wp-content/uploads/pdfs/JointWorking.pdf.
- Department of Health. The NHS Plan. London: DH; 2000 [accessed 2013 Nov 19]. Available from: http://webarchive.nationalarchives.gov.uk/20130107105354/http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/@ps/documents/digitalasset/dh_118522.pdf.
- NHS Commissioning Board. Everyone Counts: Planning for Patients 2013/14. Leeds: NHS England; 2012 [accessed 2013 Nov 19]. Available from: http://www.england.nhs.uk/wp-content/uploads/2012/12/everyonecounts-planning.pdf.
- Ingham J. Care closer to home Narrative Report. London: Royal College of Physicians; 2012 [accessed 2013 Nov 19]. Available from: http://www.rcplondon.ac.uk/sites/default/files/care-closer-to-home-narrative-report_0.pdf.
- Goodwin N, Smith J. Developing a National Strategy for the Promotion of Integrated Care. The Evidence Base for Integrated Care. London: The King's Fund and the Nuffield Trust; 2011 [accessed 2013 Nov 19]. Available from: http://www.nuffieldtrust.org.uk/sites/files/nuffield/evidence-base-for-integrated-care-251011.pdf.
- Bernstein I. Ealing PCT Integrated Musculoskeletal Service. In: MacDonald R. (ed.) Back from the brink: return to function. British Institute of Musculoskeletal Medicine Spring Symposium; 2009. Int Musculoskelet Med 2009;31(2):87–88, 93 [accessed 2013 Nov 19]. Available from: http://dx.doi.org/10.1179/175361409X412638.
- Bernstein I. Integrated musculoskeletal service design by GP consortia. Lond J Prim Care 2011;4:16–26 [accessed 2013 Nov 19]. Available from: http://www.radcliffehealth.com/sites/radcliffehealth.com/files/ljpc_articles/4_1_4.pdf.
- Department of Health. 2009–10 Programme Budgeting reference cost based PCT Benchmarking Workbook v1.00. London: DH; 2011 [accessed 2013 Nov 19]. Available from: http://webarchive.nationalarchives.gov.uk/20130107105354/http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_123502.zip.
- Dr Foster Intelligence. Practice and Provider Monitor (PPM) Tool® [updated and accessed 2012 May 1]. Available from: http://drfosterintelligence.co.uk.
- Bernstein I. Funding for Community Musculoskeletal Services. Paper. In: Ealing PCT Professional Exec Board meeting minutes. February 2010. London: Ealing PCT; 2010 [accessed 2011 May 4]. Available from: http://www.webarchive.org.uk/wayback/archive/20110504145714/http://www.ealingpct.nhs.uk/Library/Pec_papers/PECBoard2010/March2010/AGENDA%2017%20March%202010.doc
- Department of Health. 2011–12 Programme Budgeting PCT Benchmarking Tool version 1.0. London: DH; 2012 [accessed 2013 Nov 19]. Available from: http://www.networks.nhs.uk/nhs-networks/health-investment-network/documents/2011-12%20Programme%20Budgeting%20Benchmarking%20Tool_FINAL.zip.
- NHS Ealing and Ealing Council. Ealing Joint Strategic Needs Assessment (JSNA) 2009–10 update part two: appendices, pages 34–105. London: Ealing Council; 2010 [accessed 2013 Nov 19]. Available from: http://www.ibyd.co.uk/bhf/documents/Ealing_PCT/JSNA/JSNAupdate2009-2010StatementPartTwo.
- Department of Health. Tackling hospital waiting: the 18 week patient pathway. London: DH; 2006 [accessed 2013 Nov 19]. Available from: http://webarchive.nationalarchives.gov.uk/20130107105354/http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_4134669.pdf.
- Data Analysis Department, Ealing Hospital NHS Trust. CSE Servelec RiO® Data Warehouse Reports Manager [updated daily, accessed 2009–2013].
- Ellis J. MSK Pathways in ONWL Ealing. PowerPoint Presentation to Ealing PCT. London: Delivery Support Unit NHS North West London; 2011.
- Unadkat N, Ellis J. Musculoskeletal Services. PowerPoint Presentation to Ealing PCT. London: Ealing PCT; 2011.
- NW London Commissioning Support Unit. Trauma and Orthopaedic Activity Report 2009–2013. London: NWL CSU; 2013 [report supplied 2013 Oct 3]. Available from: http://www.nwlcsu.nhs.uk.
- NHS North West London. PPwT and IFR GP Briefing Document May 2011 April 2011. London: NHS NWL; 2011 [accessed 2013 Nov 19]. Available from: http://www.northwestlondon.nhs.uk/_uploads/~filestore/7DD06962-D84C-4AF1-B23A-9D3E8D61A08E/ppwt-and-ifr-gp-briefing-document-may-2011.pdf.
- Bernstein I, Johnson B. MRI Scanning from Primary Care for Musculoskeletal Conditions. London: Ealing PCT; 2011 [accessed 2013 Nov 19]. Available from: https://extranet.ealingccg.nhs.uk/Education/Documents/MSK/Advice%20and%20Referrals/Archive/EPCT%20MRI%20Scanning%20from%20Primary%20Care%20for%20Musculoskeletal%20Conditions%20IAB%202011-01-15.pdf.
- Illing L. Ealing MRI Referrals Final Report June 2011. London; InHealth: 2011.
- Laverty K. Direct access MRIs per month at InHealth Apr 2007–Sep 2013. London: NHS Ealing CCG; 2013.
- Musculoskeletal Business Case. In: Minutes of the Meeting of the Ealing Clinical Commissioning Group Governing Body Meeting. London: Ealing CCG; 27 March 2013 [accessed 2013 Nov 19]. Available from: http://www.ealingccg.nhs.uk/media/3737/Paper%201%20Draft%20minutes%2027th%20March.pdf.
- McLaren R, Laverty L. MSK Pathway Redesign – Business Case. In: NHS Ealing Governing Body CCG Meeting 27 March 2013. London: Ealing CCG; 2013 [accessed 2013 Nov 25]. http://www.ealingccg.nhs.uk/media/6122/Paper%209%20MSK_Business_Case_v5%201%2020130319%20-%20JW%20sign%20off.pdf.
- Department of Health. The Musculoskeletal Services Framework. London: Department of Health; 2006 [accessed 2013 Nov 19]. Available from: http://webarchive.nationalarchives.gov.uk/20130107105354/http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_4138412.pdf.
- Griffiths S, Taylor C, Yohannes AM. Conversion Rates and Perceived Barriers to Referral: Views of Extended Scope Physiotherapists in the Primary Care Setting. Musculoskelet Care 2012;10(4):221–31 [accessed 2013 Nov 19]. Available from: http://dx.doi.org/10.1002/msc.1023.
- Griffiths S. Ealing Hospital NHS Trust Community Musculoskeletal Service Lead. Personal communication. 19 Nov 2013.
- Curry N, Ham C. Clinical and service integration. The route to improved outcomes. London: The King's Fund; 2010 [accessed 2013 Nov 19]. Available from: http://www.kingsfund.org.uk/sites/files/kf/Clinical-and-service-integration-Natasha-Curry-Chris-Ham-22-November-2010.pdf.
- Hawkins L. Can competition and integration co-exist in a reformed NHS? London: The King's Fund; 2011 [accessed 2013 Nov 19]. Available from: http://www.kingsfund.org.uk/sites/files/kf/Can-competition-and-integration-co-exist-reformed-NHS-Loraine-Hawkins-July-2011.pdf.
- Ham C. Where next for the NHS reforms? The case for integrated care. London: The King's Fund; 2011 [accessed 2013 Nov 19]. Available from: http://www.kingsfund.org.uk/sites/files/kf/where-next-nhs-reforms-case-for-integrated-care-ham-imison-goodwin-dixon-south-kings-fund-may-2011.pdf.
- Royal College of General Practitioners. Put patients first: Back general practice. London: RCGP; 2013 [accessed 2013 Dec 16]. Available from: http://www.rcgp.org.uk/campaign-home/~/media/Files/Policy/PPF/Put-Patients-First-campaign-brief.ashx.
- Goh L, Samanta A, Cavendish S, Heney D. Rheumatology curriculum: passport to the future successful handling of the musculoskeletal burden? Rheumatology 2004;43(12):1468–72 [accessed 2013 Nov 19]. Available from: http://rheumatology.oxfordjournals.org/content/43/12/1468.full.pdf+html.
- Bernstein I, Griffiths S. GP Referrals for Musculoskeletal Conditions. Ealing – 2013. London: Ealing Hospital NHS Trust; 2013 [accessed 2013 Nov 19]. Available from: http://www.ealinghospital.nhs.uk/EasySiteWeb/GatewayLink.aspx?alId=25693.
- Ealing Clinical Commissioning Group. Ealing CCG – Commissioning Intentions for 2013/14. London: Ealing CCG; 2012 [accessed 2013 Nov 19]. Available from: http://www.ealingccg.nhs.uk/media/2077/Item%2020a%20Ealing%20CCG%20-%20Commissioning%20Intentions%202013-14.pdf.
- Ealing Council. Ealing Joint Prevention Strategy for Adults 2012-16 (Draft). London; 2012 [accessed 2013 Nov 19]. Available from: http://www.ealing.gov.uk/download/meetings/id/846/item_6-ealing_joint_prevention_strategy-draft.
- Ealing Clinical Commissioning Group. Better Care, Closer to Home. Our three-year strategy for coordinated, high quality care out of hospital 2012–2015. London: Ealing CCG; 2012 [accessed 2013 Nov 19]. Available from: http://www.ealingccg.nhs.uk/media/633/NHS%20Ealing%20CCG%20-%20Out%20of%20Hospital%20Strategy.pdf.
- Ealing Council. Ealing Health and Wellbeing Strategy 2012–16. London; 2012 [accessed 2013 Nov 19]. Available from: http://www.ealing.gov.uk/download/meetings/id/1879/item_4-health_and_wellbeing_strategy-final_version-jan_2013.
- Arthritis Research UK. The Musculoskeletal Calculator [accessed 2013 Nov 19]. Available from: http://www.arthritisresearchuk.org/policy-and-public-affairs/policy-priorities-and-projects/musculosketal-health-services/the-musculoskeletal-calculator.aspx.
- Department of Health. NHS Chief Executive's Annual Report 2008-09. London: Department of Health; 2009 [accessed 2013 Nov 19]. Available from: http://webarchive.nationalarchives.gov.uk/20130107105354/http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/documents/digitalasset/dh_099700.pdf.
- Department of Health, McKinsey & Co. Achieving World Class Productivity in the NHS 2009/10 - 2013/14: Detailing the Size of the Opportunity. London: Department of Health; 2009 [accessed 2013 Nov 19]. Available from: http://webarchive.nationalarchives.gov.uk/20130107105354/http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/documents/digitalasset/dh_116521.pdf.
- Royal College of General Practitioners. Patients bear the brunt as GPs reveal a shocking £400 m “black hole.” London: RCGP; 2013 [accessed 2013 Nov 19]. Available from: http://www.rcgp.org.uk/news/2013/october/patients-bear-brunt-as-gps-reveal-shocking-400m-black-hole.aspx.