Abstract
Objectives
To describe the structure of informal networks for individuals with spinal cord injury (SCI) living in the community, to understand the quality of relationship of informal networks, and to understand the role of informal networks in the prevention and management of secondary health conditions (SHCs).
Design
Mixed-method descriptive study.
Setting
Ontario, Canada
Participants
Community-dwelling adults with an SCI living in Ontario
Interventions/methods
The Arizona Social Support Interview Survey was used to measure social networks. Participants were asked the following open-ended questions: (1) What have been your experiences with your health care in the community? (2) What have been your experiences with care related to prevention and/or management of SHCs?, (3)What has been the role of your informal social networks (friends/family) related to SHCs?
Results
Fourteen key informant interviews were conducted (6 men, 8 women). The overall median for available informal networks was 11.0 persons (range 3–19). The informal network engaged in the following roles: (1) advice/validating concerns; (2) knowledge brokers; (3) advocacy; (4) preventing SHCs; (5) assisting with finances; and (6) managing SHCs. Participants described their informal networks as a “secondary team”; a critical and essential force in dealing with SHCs.
Conclusions
While networks are smaller for persons with SCI compared with the general population, these ties seems to be strong, which is essential when the roles involve a level of trust, certainty, tacit knowledge, and flexibility. These informal networks serve as essential key players in filling the gaps that exist within the formal health care system.
Introduction
Spinal cord injury (SCI) involves significant change(s) with motor, sensory, and/or autonomic functioning, and is associated with high levels of disability.Citation1 In Canada, approximately 44 000 individuals currently live with traumatic SCICitation1,Citation2 and approximately 1100 new cases occur each year,Citation3,Citation4 whereas higher incidence and prevalence rates are reported in the United States of America (USA) with 12 400 new cases per year and an estimated 259 000 prevalent cases.Citation5 Advances in roadside management, early acute medical therapy and surgical decompression, and advances in rehabilitation care have contributed to increased life-expectancy and frequency of community dischargeCitation6 with the mean survival time reported to be more than 30 years.Citation7
While more individuals are surviving initial injury, they are predisposed to multi-system impairments that can lead to the development of serious secondary health complications (SHCs). These include respiratory impairments and related infections, urinary tract infections (UTIs), respiratory infections, heart disease, osteoporosis, upper extremity overuse injuries, sleep disorders, sexual disorders such as erectile dysfunction and ejaculation among men, pressure ulcers, chronic pain, fatigue, depression, and suicide.Citation8,Citation9 While many of these SHCs are preventable and/or responsive to appropriate primary care management,Citation9 they are purported to be key contributors for re-hospitalization and/or death in the post-acute phase.Citation10–Citation13
These high utilization rates of health care servicesCitation11,Citation14–Citation17 suggest that care needs in the community are not being met for this population. Given the reduced lengths of inpatient rehabilitation stay, persons with SCI often require outpatient community services to manage SHCs that have not stabilized at the time of index discharge.Citation18
The shift from centralized to regionalized care has increased responsibility to individuals and their informal care networks, especially for those who are most vulnerable to navigating the health care system.Citation19,Citation20 Formal care providers are usually provided by paid medically trained professionals such as physicians, physical therapists, occupational therapists, nurses, speech language pathologists, social workers, psychologists, and personal attendants. Informal care providers are typically unpaid individuals with minimal previous formal training in health care.Citation21 In contrast to formal providers, informal care providers typically have a pre-existing relationship with the individual for whom the care is being provided. Informal care can involve tasks such as management (organization and referrals), advocacy of care, assistance with cooking, shopping, cleaning, household maintenance, mobility, community participation, basic daily grooming, advice, and emotional support.Citation21
Despite this shift in health service delivery to the community, to date there is a gap in the SCI literature with respect to understanding the formal and informal care-giving networks as they relate to the prevention of SHCs. Understanding the extent to which social systems influence health is just as critical as examining the more bio-medical risk factors of illness.Citation22 Social capital, defined as “features of social organization, such as trust, norms, and networks that can improve efficiency of society by facilitating coordination and cooperation for mutual benefit”(p. 66),Citation23 is an important construct in understanding social context. Broadly, social capital is a multi-faceted construct that relates to social relationships and the resources obtained through these relationships.Citation24
Social networks are a key building block to social capital.Citation25,Citation26 Studying social networks, both formal and informal networks of care, as well as the pattern of their interactions, has been useful in understanding fragmentation of care in other populations with chronic conditions, such as mental health, who have high health care utilization.Citation27–Citation33 For example, integration of mental health services in the community has been challenging, as reflected by the “revolving door” phenomenon.Citation34 This revolving-door concept is an indicator of fragmented care and refers specifically to bounce-back situations whereby patients have four or more admissions to inpatient services within a short time period (i.e. often a year or two).Citation35
There is evidence to suggest that mental health care-giving networks can influence mental health care utilization and negative mental health outcomes.Citation27–Citation32 In particular, social capital measures such as network size and function have been suggested to influence mental health care use.Citation28,Citation29,Citation32 For example, Pescosolido et al.Citation28,Citation29 investigated formal and informal networks and patterns of mental health care use for low income Puerto Ricans with mental health problems. Individuals with larger and more supportive informal networks of care had decreased visits to formal mental health providers.
Similarly, Bonin et al.,Citation32 using the social network theory, examined mental health utilization among homeless individuals living in Quebec. These researchers were interested in examining factors that influenced health care use among those who were impoverished with a mental health disorder in a universal health care system. With the exception of illness history, Bonin et al.Citation32 identified that social networks, environmental characteristics, and patient demographics all significantly predicted utilization of mental health services.
Bonin et al.'sCitation32 findings suggest that the application of the social network theory to identify factors associated with high health care use may be beneficial for studying other vulnerable populations with chronic care needs, such as those with SCI. Understanding these dynamic interconnected factors such as the structure of care networks, the linkages within and between networks, and their overall function, especially for complex populations that interact frequently with the health care environment are important as a means to improve integration of care.Citation28,Citation29,Citation33,Citation36 This methodology has been useful in understanding fragmentation of care such that recommendations to improve the integration of care for the SCI population at the individual, provider, and policy level can then be made.
Implications of research
We currently know that individuals with SCI have significant secondary complications and high health care utilization. SHCs continue to be problematic in approximately 20% of this populationCitation37 and with more than 50% self-reporting spasticity, pain, bladder infections in the past year, and for several SHCs including pressure ulcers and autonomic dysreflexia, the odds of developing these SHCs increased per year post injury.Citation9 Despite the relatively low prevalence of SCI, the burdens imposed on the individual and health care system are significant, as demonstrated by high health care utilization, decreased quality of life, and considerable financial costs.Citation2,Citation38
Recently, a systematic review was conducted examining the role of social support and social skills for persons with SCI.Citation39 The authors concluded that, in general, social support led to overall better health and functioning for persons with SCI.Citation39 Thus, as this review highlights, understanding care provision and social networks in the community is important. While we know that SHCs are likely influencing health care use, we do not know what community factors are associated with these SHCs.
This study aimed to provide comprehensive descriptive analyses of community networks for community-dwelling individuals with SCI. This approach will highlight informal network characteristics and how networks influence the journey of care, defined as a complex series of interactions that comprise the processes of health care, as it relates to SHC management.Citation40,Citation41
Objectives
Specifically, this study will:
| 1. | describe the structure of informal networks (e.g., size and type of care providers) for individuals with SCI living in the community; and | ||||
| 2. | understand the quality of relationships of informal networks | ||||
| 3. | understand the role of informal networks in the prevention and management of SHCs. | ||||
Methods
We used a mixed method descriptive approach.Citation42 In-depth semi-structured interviews with community-dwelling individuals with an SCI were conducted. Owing to geographical and accessibility limitations, the interviews were conducted over the telephone and audio-recorded. The consumer interviews ranged from 60 to 90 minutes in length.
Conceptual framework: Network Episode Model
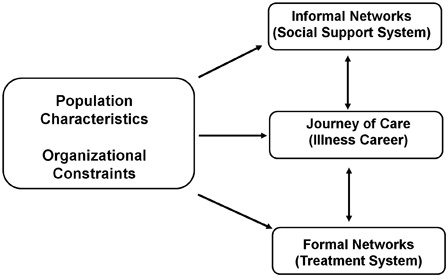
We used Pescosolido's (1991) Network Episode Model (NEM) as a conceptual guide for this study (see ),Citation40 as this model acknowledges the interdependency and social context that exists between individuals, networks, and their journeys of health care. The NEM has four domains, social context (environment), social support system (informal networks), the treatment system (formal networks) and the illness career (journey of care). Based on the social network theory, the NEM highlights the importance of community network structures, processes, and related functional outcomes as dynamic components that influence health behaviors and health outcomes.Citation40 There are four underlying assumptions to this model, (1) communities contain care providers; (2) process of care is dynamic, occurs over time, and develops into patterns and pathways; (3) underlying the processes of health care use are social networks; and (4) social networks may influence the interaction with the care providers.Citation40
While the NEM does not negate the role of the individual as an active agent, it recognizes that social influences can be as equally, if not more important.Citation40 For the purpose of the present exploratory study, we focused specifically on the “population characteristics” and “informal networks” domains of the NEM. We focused in depth on these two domains given the time intensive nature of measuring social networks and efforts to reduce responder burden.
Theoretical position
The theoretical approach underlying this study was that of relativist ontology, that is, previous a priori knowledge helped inform assumptions but allowed for emerging themes to arise.Citation43 The paradigm guiding this research question was a naturalistic interpretive one. This multi-lens approach was concerned with understanding the subjective, complex and contextual experiences of participants.Citation44 The contextual and constructed realities of each participant helped inform and reshape knowledge gained from the research inquiry.Citation45 Furthermore, principles from Thorne's interpretive description methodology facilitated the scientific inquiry, as this approach allowed for a priori assumptions (e.g. network episode theory) to be synthesized with knowledge gained from data, as well as other theoretical and contextual health services clinical knowledge.Citation45
Key informant recruitment
The recruitment strategy included purposeful snowball sampling for maximum variation in key informant experiences.Citation46 We specifically aimed to have fair representation across gender, level of injury (cervical, thoracic, and lumbar), and mechanism of injury (traumatic and non-traumatic), as well as socioeconomic status/funding source for health care services (private payments from motor vehicle accident compensation and public payment for services). We recruited from the community by advertising the study via the Canadian Paraplegic Association (CPA)-Ontario division's website and email distribution. Semi-structured key informant interviews with community-dwelling individuals with an SCI provided the primary source of data. Key informants were at least 18 years of age as we focused specifically on adult experiences.
Informed consent
Approval for this study was obtained from the University Health Network Research Ethics Board, as well as the University of Toronto. All participants provided informed consent prior to the interview.
Data collection
Key informant interviews with participants were conducted using a semi-structured interview guide composed of a number of valid and reliable scales, open-ended questions and potential probes (see for open-ended questions). Based on the NEM, a number of quantitative scales were used to describe socio-demographics and clinical characteristics of participants (items based on the Canadian Community Health Survey (CCHS, version 3.1)Citation47 and the Ontario Spinal Cord Injury Registry (OSCIR),Citation48 social networks (based on CCHS and the Arizona Social Support Interview Schedule (ASSIS)),Citation49 and history of SHCs within the past year (Spinal Cord Injury Secondary Complications Scale (SCI-SCS)).Citation50 The SCI-SCS was instrumental as a probe for detailed discussion related to how each of the identified SHCs was managed and the role informal networks played in these SHCs.
Table 1. Interview guide for open-ended questions with key informants*
Quantitative measures
Population characteristics: demographics and clinical characteristics
Demographic items included the following: age, sex, education, income, ethnicity, language, occupation, employment status, marital status, area of residence (urban/rural), and insurance source for medical care. Clinical characteristics included items such as level of injury, mechanism of injury, and date of injury.
Social networks: formal and informal care networks
Formal care networks (e.g. physicians, rehabilitation professionals, and alternative medicine providers) were assessed using items from the CCHS.Citation47 For example, “Not counting when you were an overnight patient, how many times have you seen or talked on the telephone, about your physical, emotional or mental health with… a family doctor…a specialist… a nurse…a physical therapist…a psychologist…” Participants were asked to provide the initials of the care provider.
The ASSIS is a semi-structured tool that consists of a series of questions that asks about a person's perception of network size and the adequacy of the support received (i.e. satisfaction and need). In particular, the ASSIS measures six functional areas of social networks: (1) material aid; (2) physical assistance; (3) intimate/private interaction; (4) guidance; (5) feedback, and (6) negative social interaction. This tool allows for the following network properties to be measured: (1) network size (including available and utilized social networks), (2) network composition, (3) support satisfaction, (4) support need, and (5) any sources of network conflict.Citation49 The ASSIS has shown good test–retest reliability for size of the available network with correlations ranging from 0.70 (over 1-month period) to 0.88 (over 2 or more days).Citation49,Citation51
The survey starts with the following text: “In the next few minutes I would like to get an idea of the people who are important to you in a number of different ways. I will be reading descriptions of ways that people are often important to us. After I read each description, I will be asking you to give me the first names, the initials, or nicknames of the people who fit the description. These people might be friends, family members, teachers, priests, ministers, doctors, or other people who you might know. If you have any questions about the descriptions I have read, please ask me to try to make it clearer.”
For each functional area, the following related to (1) size, (2) satisfaction, and (3) need were asked of a participant. For example, for the intimate interaction domain: (1) Size –“If you wanted to talk to someone about the things that are very personal and private, who would you talk to? Give me the first names, initials, or nicknames of people who you would talk to about things that are very personal and private”, (2) Satisfaction – “How would you rate your satisfaction or dissatisfaction with the times you talked to people about your personal and private feelings during the past month?” (Response options include very dissatisfied, moderately dissatisfied, slightly dissatisfied, neither satisfied nor dissatisfied, slightly satisfied, moderately satisfied, or very satisfied.), and (3) Need – “During the past month, how much do you think you needed people to talk to about things that were very personal and private? Tell me which statement best describes your need, no need at all, slight need, moderate need, great need, or very great need.”
Secondary health conditions
The SCI-SCS-Modified is a 23-item measure of SHCs that impact health and physical functioning.Citation50 Modified from the longer 40-item Secondary Complication Questionnaire (SCQ), the SCI-SCS was designed to measure complications related to skin, musculoskeletal, pain, and bowel/bladder in the past year. The measure uses a 4-point ordinal scale ranging from 0 (not experienced/insignificant problem never limiting activity) to 3 (significant/chronic problem). Items are summed up and scores can range from 0 to 69, with the higher score reflecting greater problems with SHCs. The SCI-SCS has shown good convergent validity, internal consistency (>0.80), and test–retest reliability (>0.60).Citation50
Data analysis
All key informant interviews were audio-recorded and transcribed verbatim. Data analysis used an iterative constant comparative process involving descriptive and interpretive analyses.Citation43,Citation46,Citation52 Using a template analysis approach,Citation53 a flexible coding structure was developed based on the NEM, which allowed for free nodes when emerging ideas or themes were identified. After each interview, the principal investigator (S.J.T.G.) wrote detailed reflexive notes on major emerging themes, which were later discussed in detail with one of the research investigators (S.B.J.). The principal investigator (S.J.T.G.) coded all transcribed interviews. The other investigators (S.B.J., L.L.-C., B.C.C., T.C., and M.A.M.) independently reviewed a sample (n = 3, 20%) and compared the emergent themes. Data management was facilitated using NVivo9 qualitative analysis computer software, as well as SPSS (SPSS Inc, Chicago, IL) Version 19 for descriptive quantitative analyses.
Results
Fourteen key informant interviews were conducted (6 men and 8 women). Demographics of the sample are shown in . The median age was 47.5 years (31–75). The median number of years post injury was 18 (range of 4–49 years). Approximately half of the participants had an injury at the level of the cervical spine (n = 8). For mobility aids, approximately half of the participants used electrical wheelchairs (n = 8), and the others used manual wheelchairs (n = 6). Approximately a third of the participants had an education level of high school or less (n = 4), associate's degree or bachelor's degree (n = 5), or graduate-level degree (n = 5). Eight individuals lived with a spouse and/or common-law partner, one individual lived with a paid attendant, and five people lived alone.
Table 2. Demographics of participants (n = 14)
The majority of individuals (n = 13) reported significant challenges with SHCs in the past year. In particular, significant or chronic problems were related to pressure sores, muscle spasms, and pain. UTIs were experienced in the last year for eight participants, five of whom reported these infections to be moderate to significant problems. The mean score on the SCI-SCS was 15.3 (SD = 8.2).
Composition of social networks
Overall network size
Using both the CCHS and ASSIS tools, the total network size was calculated. The median network size for participants was 16.5 (range 5–28), which includes family, friends, and health care providers. shows the composition of networks by gender. Similar network compositions were identified for both males and females, with the exception of females having more friends comprising the informal networks (median = 7.0 for females versus 4.5 for males).
Table 3. Identified informal and formal networks by composition, family, friends, and health care providers (n = 14)
Informal networks
Participants are encouraged in the ASSIS to identify any formal and informal members that fit within the six domains. However, with the exception of four participants, individuals only identified family and/or friends rather than formal health care providers within their social networks for the six functional areas within the ASSIS. Specifically, only three individuals identified paid health care professionals as members of their networks within the functional areas of intimate/private as well as advice. All other participants only identified informal care providers. Data analyses were conducted with both formal and informal networks; however, given the small number of formal health care providers identified in the ASSIS, the median values remained unchanged. Therefore, the following results will refer to only informal care providers (family and friends) identified using the ASSIS.
Informal available networks
The overall median for available informal networks was 11.0 (range 3–19). Networks were larger for social support (median = 6.5) and physical assistance (median = 4.0), followed by positive feedback (median = 3.5), advice (median = 3.0), material assistance (median = 2.5), and intimate relations (median = 2.5; see ).
Table 4. Informal network composition, satisfaction, and need, based on the six ASSIS domains
Informal utilized networks
The size of the utilized networks was considerably smaller than the available networks. Utilized network medians were largest for social support (median = 5.5) and physical assistance (median = 2.5). Only one participant reported using material assistance, the remaining sample did not use material support (median = 0.0).
Perceived satisfaction and need
In all six functional areas, participants reported being very satisfied with their networks (medians = 7.0; see ). There was slightly more variation in perceptions of need, as median scores ranged from 1.0 (no need for material assistance) to 5.0 (great need for social support and physical assistance).
Shifting networks following SCI
The majority of individuals felt that their social networks decreased since their SCI, three individuals (21.4%) reported networks were moderately to significantly decreased, and four individuals (28.6%) felt that the networks slightly decreased. Four individuals (28.6%) stated that their networks did not substantially change.
Thematic results: informal social network roles
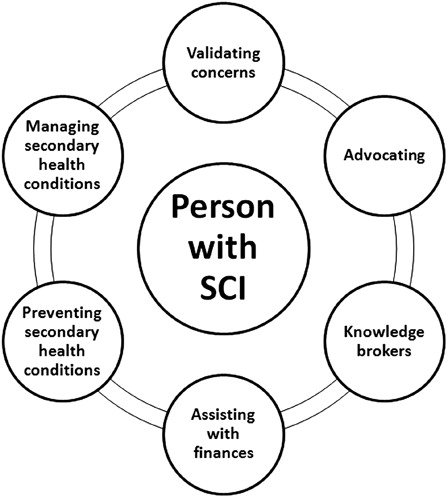
Numerous roles of informal networks were identified related to SHCs (see ).
Advice/validating concerns
Participants described how informal networks served as resources for advice related to SHCs, particularly with respect to validating concerns. Participants often spoke of uncertainty regarding the severity of a SHC and whether or not formal medical assessment/treatment would be warranted. In particular, informal networks often assisted individuals in clinical decision making of and self-management of SHCs.
They're the ones [wife and son] that sort of see me regularly and a lot of times I'll just sort of go is it me or is it really a problem… So if there's ever anything that's sort of a concern or bothering me, I always sort of go to her [wife] first just because I know if I'm at the point where I'm squawking about something, there's something wrong. (Interview Male 011)
Knowledge brokers
Participants described their informal networks as playing an integral role in the acquisition of knowledge related to prevention of and/or management of SHCs. Informal networks assisted individuals with researching and acquiring clinical information, seeking appropriate health services, as well as facilitating knowledge exchange with various health care providers. Furthermore, participants described how their informal networks acted as key players in facilitating linkages to health care professionals with appropriate expertise in managing SHCs.
It was just by luck my wife knew a nurse through a friend of ours who was a bed sore nurse that travelled the world. She said “let me take a look at the wound.” She took a look at the wound. She offered this new product… and it cured me in 6 weeks. The doctor didn't even know about this and he wanted to put me in the hospital for a month after the operation. (Interview Male 013)
In particular, the CPA-Ontario division was mentioned by several participants as being a key lifeline for knowledge brokerage. For example, participants described how the CPA-Ontario provided individuals with a wide range of important information both directly and indirectly related to SHCs, such as self-management, community re-integration (work and volunteer opportunities, and social opportunities), housing and personal support, community health resources, and funding support (assistive devices and equipment, and disability support).
Like I said, CPA, if it hadn't been for the regional coordinator, I would have been left slapping in the wind (Interview Female 008)
Advocacy
Participants discussed how informal networks played a strong advocacy role, especially with respect to SHC management and ensuring that they received timely and appropriate care. Family members and friends often accompanied participants to medical appointments to assist with knowledge exchange and advocate if needed. Participants commonly reported a feeling that the medical community dismissed concerns related to SHCs and appreciated the advocacy role that informal networks played.
I had an encounter with an orthopod who totally dismissed… I had a low energy fracture of the left tibia several years ago. I rolled over in bed and broke it and the first ortho that I saw he says “there's no break there.” Meanwhile my leg is twice the size that it should be and bruised and hot and everything else. My sister actually pointed it out on the x-ray to him. (Interview Female 007)
Assisting with finances
In addition, informal networks also assisted individuals in filling out lengthy documentation for equipment funding, such as financial support for pressure relief cushions, wheel chairs, and home and vehicle modifications. The assistance with these applications was noted to be critically important, as access to assistive devices such as pressure relief cushions was essential in minimizing the occurrence of pressure sores. Participants described that the applications for funding support were time consuming and complicated, and informal networks provided substantial support in negotiating these funding processes.
Another important aspect to financial assistance is the personal financial contribution that informal networks provided. Many individuals described the financial “sacrifice” that their informal networks made, particularly family members, in order to minimize the occurrence of SHCs.
I don't reuse catheters. We [wife and participant] made a conscientious decision when this happened not to reuse catheters. We have the additional cost. Catheters are about $1 a pop… and I go through about 4 or 5 a day. It is a big cost and it's not covered by insurance. But we said we will wear that cost not to go through the risk of urinary tract… But no issues that way but I think it's because we're being very proactive and a lot of people I know aren't in a position where they can afford to sort of buy these things on a one use basis. (Interview Male 011)
Preventing SHCs
Participants were asked about their experiences with prevention and/or management of SHCs. With respect to facilitating prevention, participants described how informal networks assisted with important prevention behavior such as skin checks for pressure sores, swelling, bruises, etc.
I was sitting in a living room one day and I hadn't really noticed any difference in the swelling of my feet. But my boyfriend did. He's like “I don't like the way your feet are looking, they're really swollen for you.” I looked down and it's like oh yeah, I guess they are… So they can sometimes pick up things that you don't and I think that's extremely valuable… You get those that you trust to kind of do the areas that you can't see and they get to a point where they might see something that you're not aware of. (Interview Female 007)
Managing SHCs
Participants indicated that informal networks provided significant assistance with managing SHCs. In addition, informal networks provide assistance in facilitating interaction with health care providers such as setting up medical appointments, transportation to and from medical appointments, as well as physical assistance in physically negotiating often poorly accessible medical offices/examination tables, as part of their role in managing SHCs.
Especially for me because my biggest handicap… I can't even push my hands to click a button or Bluetooth or anything. She [wife] has to do everything on the phone, answer it, deal with all the VHA [home health care] and CCAC [Community Care Access Centre, home care] and everything because it's useless to hand it to me because she's going to do all the follow up. (Interview Male 013)
Informal networks provided substantial personal care with daily secondary complication management such as bladder and bowel care.
… bowel regularity… My body works fine but it doesn't work on a regular enough cycle…I always have to have somebody with me, either it's to pull my pants down or to help maneuver the commode chair because it's a little awkward. So I fundamentally have to work my bowel schedule around when I have somebody in the house to help me. So what I do is I now take basically it's a suppository every two days and I have enough sensation I can tell if my bowels are getting full. So I can tell if there's pressure… and literally I almost run my life around the bowel schedule…the two people that have to handle this with me is either my wife or my son. So I literally have to sort of okay what's your schedule, where are you going, are you going to be in a meeting, just so I can make sure okay… it literally, it's day one or it's day two. If it's day two, you come home. Now my wife fortunately works literally 10 minutes down the road from the house, so if all of a sudden I'm going I've got to go now, I often can just pick up the phone and say please come home now if you can. And she does… (Interview Male 011)
Quality of informal network relationships
Participants discussed the importance of their informal networks and the value that they placed on these relationships. Trust and flexibility were important characteristics of the relationships with informal networks. With respect to trust, individuals described how informal networks provided support, both emotional and physical, in a safe environment.
I think that you know a secondary team like the family and friends are just as important if not more so in some aspects of primary health care because the doctors, they see you briefly, they make the diagnosis. But then it's the secondary team if you will that do the day to day things… You're calling them at 3 am going help because you can't get cleaned up or things like that and I think the secondary team is definitely not given enough credit… you've got the system and the team… you know, these are people that you trust that will go to bat for you, that will speak up for you and yet will allow you to be vulnerable. They just take what comes with the disability as it comes… they are a secondary team because they're the ones that are doing the bowel cleanup, the catheters in the middle of the night, the dressing changes, skin checks. You see them every day whereas your healthcare practitioner you're lucky if you see once every 3 months, something like that. (Interview Female 007)
Participants described how the informal networks, in particular family members, always were on-call, available, and adaptable in dealing with issues related to SHCs. These informal networks were described as members of a “secondary team”, critical in the prevention and management of SHCs. Finally, individuals described informal networks changing following their injury, usually becoming smaller but stronger networks.
I found out who my friends were and who weren't my friends or were just acquaintances. I think my network has become a closer network to me, a smaller group of people but closer. (Interview Female 008)
Discussion
Size of caregiving networks
In this descriptive mixed-methods study, we examined the structure, role, and quality of networks of care for persons with an SCI using the NEM. We identified that individuals had an overall median informal and formal network size of 16.5 persons (range 5–28), which included health care professionals, community organizations, friends, and family members. In comparison with the general population, we identified that the size of overall networks for persons with SCI is slightly smaller, as networks in the general population range from 20 to 30 persons.Citation54–Citation56 However, these results are similar to other studies that have used the ASSIS as a measure of networks for other vulnerable populations with disabilities. Previous studies have identified networks to be 11.5 persons for both the mental health populationCitation55 and multiple sclerosis population.Citation57 In the rheumatoid arthritis population, using the Social Network Delineation Questionnaire, Fyrand et al.Citation58 identified a total network size of 15.8 persons. In the general population, size of networks is important, as larger a social network, the more likely information will be passed on and new contacts made.Citation59,Citation60
Using the ASSIS, we identified the median number of available informal networks to be 11 persons (range 3–19). These findings are similar to a previous study that identified the available social support networks for persons with SCI 2 years following injury to be approximately 8.3 persons.Citation61 It is worth noting that the Social Support QuestionnaireCitation62 was used to measure social networks and this instrument has a ceiling of nine persons that can be identified. In our present study we did not have a ceiling limit, as the ASSIS has no restriction on the number of reported networks.
Specifically within intimate relations, participants had a median of 2.5 network members, which is smaller than the general population, as recently, Wellman et al.Citation63 identified in the “Connected Lives Study”, persons living in Toronto felt “very close” to 4.1 network members. Social support and physical assistance networks were larger in size compared with the other four domains, and participants rated these two domains in particular to be of “very great need”. Participants also reported using these social support and physical assistance networks more than the other domains.
Role and quality of relationships
In addition to network size, we examined the role of network members as well as the quality of these relationships. This present study highlighted the importance of understanding the qualitative nature of social networks and the roles which individuals play within the context of SHCs. While the size of the informal networks may be smaller than that of the general population, the close ties with informal networks described by participants in the qualitative interviews was evident. Specifically, bonding cohesive social capital, characterized by intimate relationships in which social and psychological support are provided to help with day to day care needsCitation64 was prominent among participants rather than bridging social capital. Bonding social capital is typically provided by relationships with family members as often these ties involve a significant amount of time with strong intimacy and trust.Citation65 Key players within the social support and physical assistance networks were often family members, particularly spouses and/or significant partners of participants. The latter type of social capital, bridging, is based on weaker ties which are better suited to providing instrumental resources (e.g. access to community services and knowledge diffusion) rather than emotional or physical support.Citation59
Previous research has identified the utility of bridging capital with the “strength of weak ties”Citation59 and “structural holes”,Citation66 that is, by increasing the number of non-redundant connections, individuals in theory have greater opportunity to access resources.Citation24,Citation67 However, in the present research, our qualitative data suggests that participants greatly valued a closer and stronger level of trust with their informal networks given the vulnerability of care provision potentially required. Participants described their informal networks as a “secondary team”, that is, a critical and essential force in dealing directly and indirectly with SHCs. The roles to which the secondary team members engaged in dealing with SHCs were identified as the following: (1) advice/validating concerns; (2) knowledge brokers; (3) advocacy; (4) assisting with finances; (5) preventing SHCs; and (6) managing SHCs. These results support the strength of cohesion,Citation68,Citation69 as strong ties are important when an individual is in a more vulnerable position and there is a need for trust and certainty.Citation68 The roles identified of informal networks for persons with SCI are similar to informal care roles identified for persons with other chronic conditions.Citation70–Citation74 Recently, Essue and colleagues identified key roles in the self-management partnership for persons with complex chronic conditions (i.e. chronic heart failure, chronic obstructive pulmonary disease, and diabetes) to include home-helper, lifestyle coach, advocate, technical care manager, and health information interpreter.
This research suggests informal networks serve as essential key players in filling in the gaps that exist within the formal health care system. In particular, the CPA-Ontario was identified as an essential organization to bridge this gap, serving as a key lifeline for knowledge brokerage and advocacy. The CPA-Ontario is a not-for-profit organization that provides services in the areas of peer support, regional services coordinators, membership, employment services, advocacy, information services, and attendant services.Citation75
Indeed, the gaps and barriers to health service delivery for those with complex chronic disabilities have been previously documented.Citation18 Recently, Meade et al.Citation76 specifically highlighted gaps in formal provider knowledge, provider–patient collaboration, quality of provider–patient communication, and discrimination for persons with SCI. Consistent with these findings, the present study identified that informal networks serve as central advocates, knowledge brokers, and validate secondary complication concerns for persons with SCI.
This research highlighted that these small cohesive networks of close ties are indispensable for persons with a SCI. The reliance on these small care-giving networks highlights the vulnerability and fragility of the informal networks. Persons with SCI might benefit from a more expansive network rich with weak ties to access novel information and diverse resources (e.g. how to prevent SHCs, new technologies, how to apply for equipment funding). Developing and maintaining a larger diverse network with weaker ties may be unattainable for most people with SCI due to the constraints their condition imposes on their social life. Thus, given the complexity of the condition, persons with SCI may only have the time and effort to focus on very close relationships.
Furthermore, despite the presence of these strong informal networks, the majority of individuals (n = 13) reported significant challenges with SHCs in the past year. This raises concern as to what extent would persons with SCI be able to deal with SHCs if these informal networks were not available and/or be able to engage in the roles described in this research. Based on the present findings, individuals would likely be struggling significantly more to prevent and/or manage SHCs if only relying on the formal health care system. Importantly, there is already significant strain on informal caregivers in assisting with supportive care for persons with SCICitation77–Citation79 and this present research also highlights the extensive roles of informal care providers with SHCs. These extensive roles may create an inequality of exchange,Citation39 as previous research has shown that the more instrumental, information, and emotional support needed from friends, the less satisfaction in social life has been reported by persons with SCI.Citation80 Similarly, Essue et al.Citation72 noted that the informal care-giving relationship can create a conflict between the care recipient and care providers. In Canada, there is a growing recognition of the importance of informal care provision in general, and the need to support the social, health and economic well-being of informal care providers.Citation81 For example, informal care provision affects participation in the workforce and recently there have been policy recommendations for employers to offer flexibility and financial compensation for care provision (e.g. family leave).Citation81 Given the critical roles assigned to informal care providers, it is pertinent that governmental organizations implement structures and policies that minimize the burden of care and ensure care competencies.
Similar to Canada, in Australia, there is a growing acknowledgement of the challenges in access to community-based care and the burden informal care places on care providers.Citation72 For instance, to assess eligibility for community care services, the Commonwealth Government's Nationally Consistent Assessment includes “The Carer Eligibility and Needs Assessment-Revised”(CENA-R) questionnaire as one of the tools to measure carers' needs and the impact of caregiving on the relationship with the care recipient.Citation82 In Canada, the home care assessment process might benefit from such a tool that involves the care provider characteristics, as well as relationship attributes in determining eligibility.
Limitations of the present research
There are some limitations in this study. First, the ASSIS domains may have been too general for persons with SCI, given the complexity of the condition and the wide range of roles in which network members may serve. Given this, the qualitative data were critical to uncover the specific roles informal networks play in dealing with SHCs. For example, most participants did not recall any specific network member in assisting with material aid; however, in the qualitative interviews, findings suggest that informal networks serve a key role in assisting with financial costs. There were several similarities between domains in the ASSIS and those that were identified from the qualitative data such as advice, social support, positive feedback (validation of concerns); however, the qualitative data identified some new items particularly related to process facilitation roles with more specificity to SCI, such as knowledge brokerage, and assisting with funding applications for durable medical equipment and assistive devices.
Currently, there is no gold standard on measuring social support or social capital.Citation39 Thus, the comparison of network size is challenged by the different measures used. Future research in developing metrics on social capital for persons with disabilities may be warranted to explore whether these are common roles for informal care providers assisting those with any complex physical disability. For example, items might address informal caregivers' time off work, costs associated with assistive devices, equipment, medical supplies, technology, transportation, and indirect health care costs not covered under public or private insurance plans. Understanding the role of informal care providers for any complex condition in more detail would be beneficial to policy planning. In addition, future research would be useful in understanding how individuals acquire the networks (e.g. passively assigned or actively sought) and how these network structures change over time.
Finally, another limitation is that these results are based on a small sample of individuals with SCI and need to be considered in other settings. Specifically, persons with high ventilation tetraplegia or individuals requiring 24-hour care are underrepresented. There was an explicit effort for balanced gender distribution for this initial exploratory understanding of social networks; however, this does not reflect the gender distribution of SCI.Citation3
However, this research is useful as a foundation in understanding care networks and SHCs for persons with SCI. In using the NEM, understanding these networks of care and how they may relate to health care utilization and outcomes, recommendations to improve the management of care for the SCI population at the individual, provider, and policy level can be made. Future research is warranted in examining other components of the NEM, specifically the health care environment/system, and how the components of the model interact in the journey of care for persons with SCI. Our research highlighted that while networks are smaller for persons with SCI, these ties are stronger, which is essential when the roles involve a level of trust, certainty, tacit knowledge, and flexibility. Indeed, these networks serve as a critical secondary team for persons with SCI.
Acknowledgements
We acknowledge the support of the Toronto Rehabilitation Institute (TRI), which receives funding under the Provincial Rehabilitation Research Program from the Ministry of Health and Long-Term Care (MOHLTC) in Ontario. The views expressed do not necessarily reflect those of the Ministry. Ms Guilcher's doctoral training has been supported throughout the years by the Canadian Institute for Health Research, Women's College Research Institute, Ontario Neurotrauma Foundation, TRI, Community University Research Alliance, and Ontario Training Collaborative Program in Health Services and Policy Research. Dr Jagtlal is the TRI Chair at the University of Toronto in Health Services Research.
References
- Farry A, Baxter D. The incidence and prevalence of spinal cord injury in Canada: overview and estimates based on current evidence. Rick Hansen Institute Urban Futures Institute; 2010. Available from: http://www.urbanfutures.com/reports/Report%2080.pdf.
- Walker J. Caring for patients with a diagnosis of cancer and spinal metastatic disease. Nurs Stand 2002;16(42):41–4.
- Couris CM, Guilcher SJT, Munce SEP, Fung K, Craven BC, Verrier M, et al. Characteristics of adults with incident traumatic spinal cord injury in Ontario, Canada. Spinal Cord 2010;48(1):39–44.
- Pickett GE, Campos-Benitez M, Keller JL, Duggal N. Epidemiology of traumatic spinal cord injury in Canada. Spine 2006;31(7):799–805.
- McKinley WO, Jackson AB, Cardenas DD, DeVivo MJ. Long-term medical complications after traumatic spinal cord injury: a regional model systems analysis. Arch Physi Medi Rehabil. 1999;80(11):1402–10.
- Strauss DJ, DeVivo MJ, Paculdo DR, Shavelle RM. Trends in life expectancy after spinal cord injury. Arch Phys Med Rehabil 2006;87(8):1079–85.
- National Spinal Cord Injury Statistical Center. Spinal cord injury facts and figures at a glance. J Spinal Cord Med 2012;35(1):68–9.
- Paker N, Soy D, Kesiktas N, Bardak AN, Erbil M, Ersoy S, et al. Reasons for rehospitalization in patients with spinal cord injury: 5 years' experience. Int J Rehabil Res 2006;29(1):71–6.
- Hitzig SL, Tonack M, Campbell KA, McGillivray CF, Boschen KA, Richards K, et al. Secondary health complications in an aging Canadian spinal cord injury sample. Am J Physi Med Rehabil 2008;87(7):545–55.
- Anson CA, Shepherd C. Incidence of secondary complications in spinal cord injury. Int J Rehabil Res 1996;19(1):55–66.
- Dryden DM, Saunders LD, Rowe BH, May LA, Yiannakoulias N, Svenson LW. Utilization of health services following spinal cord injury: a 6-year follow-up study. Spinal Cord 2004;42:513–25.
- Pickelsimer E, Shiroma EJ, Wilson DA. Statewide investigation of medically attended adverse health conditions of persons with spinal cord injury. J Spinal Cord Med 2010;33(3):221–31.
- DeVivo MJ. Causes and costs of unplanned hospitalizations among persons with spinal cord injury. Top Spinal Cord Inj Rehabil. 2011;16(4):53–61.
- Guilcher SJ, Munce SE, Couris CM, Fung K, Craven BC, Verrier M, et al. Health care utilization in non-traumatic and traumatic spinal cord injury: a population-based study. Spinal Cord 2010;48(1):45–50.
- Jaglal SB, Munce SE, Guilcher SJ, Couris CM, Fung K, Craven BC, et al. Health system factors associated with rehospitalizations after traumatic spinal cord injury: a population-based study. Spinal Cord 2009;47(8):604–9.
- Munce SEP, Guilcher SJT, Couris CM, Fung K, Craven BC, Verrier M, et al. Physician utilization among adults with traumatic spinal cord injury in Ontario: a population-based study. Spinal Cord 2009;47(6):470–6.
- McColl MA, Aiken A, McColl A, Smith K. Primary care for people with SCI. In: , Eng JJ, Teasell RW, Miller WC, Wolfe DL, Townson AF, Hsieh JTC, Connelly SJ, Mehta S, Sakakibara BM, (eds.) Spinal cord injury rehabilitation evidence. Vancouver; 2010. p. 1–24.
- DeJong G, Hoffman J, Meade M, Bombardier C, Deutsch A, Nemunaitis G, et al. Postrehabilitative health care for individuals with SCI: extending health care into the community. Top Spinal Cord Inj Rehabil. 2011;17(2):46–58.
- Tsasis P, Bains J. Management of complex chronic disease: facing the challenges in the Canadian health-care system. Health Serv Manage Res 2008;21(4):228–35.
- Huerta TR, Casebeer A, Vanderplatt M. Using networks to enhance health services delivery: perspectives, paradoxes and propositions. Healthc Papers New Models New Healthc 2006;7(2):10–26.
- Grant K, Amaratunga C, Armstrong P, Boscoe M, Pederson A, Willson K. Caring for/caring about women, home care, and unpaid caregiving. Aurora, Ontario: Garamond Press, Ltd.; 2004.
- Lomas J. Social capital and health: implications for public health and epidemiology. Soc Sci Med 1998;47(9):1181–8.
- Putnam RD. Bowling alone. America's declining social capital. J Democracy 1995;6:65–78.
- Pitkin Derose K, Varda DM. Social capital and health care access: a systematic review. Med Care Res Rev 2009;66(3):272–306.
- Lauder W, Reel S, Farmer J, Griggs H. Social capital, rural nursing and rural nursing theory. Nurs Inq 2006;13(1):73–9.
- Reimer B, Lyons T, Ferguson N, Polanco G. Social capital as social relations: the contribution of normative structures. Sociol Rev 2008;56(2):256–74.
- Bussing R, Zima BT, Gary FA, Mason DM, Leon CE, Sinha K, et al. Social networks, caregiver strain, and utilization of mental health services among elementary school students at high risk for ADHD. J Am Acad Child Adolesc Psychiatry 2003;42(7):842–50.
- Pescosolido BA, Gardner CB, Lubell KM. How people get into mental health services: stories of choice, coercion and ‘muddling through’ from ‘first-timers’. Soc Sci Med 1998;46(2):275–86.
- Pescosolido BA, Wright ER, Alegría M, Vera M. Social networks and patterns of use among the poor with mental health problems in Puerto Rico. Med Care 1998;36(7):1057–72.
- Pescosolido BA, Wright ER. The view from two worlds: the convergence of social network reports between mental health clients and their ties. Soc Sci Med 2004;58(9):1795–806.
- Pescosolido BA. Of pride and prejudice: the role of sociology and social networks in integrating the health sciences. J Health Soc Behav. 2006;47(3):189–208.
- Bonin JP, Fournier L, Blais R. Predictors of mental health service utilization by people using resources for homeless people in Canada. Psychiatr Serv 2007;58(7):936–41.
- Carpentier N, Pomey MP, Contreras R. Social care interface in early-stage dementia practitioners' perspectives on the links between formal and informal networks. J Aging Health 2008;20(6):720–38.
- Munizza C, Furlan PM, D'Elia A, D'Onofrio MR, Leggero P, Punzo F, et al. Emergency psychiatry: a review of the literature. Acta Psychiatr Scand Suppl 1993;88(374):1–51.
- Wuerker AK. The changing careers of patients with chronic mental illness: a study of sequential patterns in mental health service utilization. J Mental Health Administr 1996;23(4):458–70.
- Lemieux-Charles L, Chambers LW, Cockerill R, Jaglal S, Brazil K, Cohen C, et al. Evaluating the effectiveness of community-based dementia care networks: the Dementia Care Networks' Study. Gerontologist 2005;45(4):456–64.
- Chiodo AE, Scelza WM, Kirshblum SC, Wuermser LA, Ho CH, Priebe MM. Spinal cord injury medicine. 5. Long-term medical issues and health maintenance. Arch Phys Med Rehabil 2007;88 (3 Suppl. 1):S76–83.
- Dorsett P, Geraghty T. Health-related outcomes of people with spinal cord injury[mdash]a 10 year longitudinal study. Spinal Cord 2008;46(5):386–91.
- Muller R, Peter C, Cieza A, Geyh S. The role of social support and social skills in people with spinal cord injury[mdash]a systematic review of the literature. Spinal Cord 2012;50(2):94–106.
- Pescosolido BA. Illness careers and network ties: a conceptual model of utilization and compliance. In: Albrecht G, Levy J, (eds) Advances in medical sociology. Greenwich, CT: JAI Press; 1991. p. 161–84.
- Layton A, Mass F, Morgan G. Mapping out the patient's journey: experiences of developing pathways of care. Qual Health Care 1998;7 (Suppl):S30–S6.
- Sandelowski M. Whatever happened to qualitative description? Res Nurs Health 2000;23(4):334–40.
- Patton MQ. Qualitative evaluation and research methods. 3 ed. Thousand Oaks, CA: Sage Publications Inc.; 2001.
- Lincoln YS, Guba EG. Naturalistic inquiry. Beverly Hills, CA: Sage Publications Inc.; 1985.
- Thorne S, Reimer Kirkham S, O'Flynn-Magee K. The analytic challenge in interpretive description. Int J Qual Meth 2004;3(1):1–11.
- Yin R. Case study research: design and methods. 4 ed. Thousand Oaks, CA: Sage Publications Inc.; 2009.
- Canada S. Canadian Community Health Survey (CCHS 3.1). Canada: Statistics Canada; 2005.
- Verrier M, Ahn H, Craven C, Drew B, Fehlings M, Ford M, et al. Ontario spinal cord injury informatics: informing practice research and innovations. Ontario Neurotrauma Foundation; November 2009 [January 2012]. Available from: http://www.onf.org/documents/OSCIR.pdf.
- Barrera M. A method for the assessment of social support networks in community survey research. Connections 1980;3(3):8–13.
- Kalpakjian CZ, Scelza WM, Forchheimer MB, Toussaint LL. Preliminary reliability and validity of a Spinal Cord Injury Secondary Conditions Scale. J Spinal Cord Med 2007;30(2):131–9. Epub 2007/06/27.
- Barrera M, Ainlay SL. The structure of social support: a conceptual and empirical analysis. J Commun Psychol 1983;11(2):133–43.
- Miles MB, Huberman AM. Qualitative data analysis – an expanded sourcebook. 2 ed. Thousand Oaks, CA: Sage Publications Inc.; 1994.
- King N. Template analysis. In: , Symon G, Cassell C, (eds.) Qualitative methods and analysis in organisational research: a practical guide. London: Sage; 1998. p. 118–34.
- McFarlane AH, Neale KA, Norman GR, Roy RG, Streiner DL. Methodological issues in developing a scale to measure social support. Schizophr Bull 1981;7(1):90–100. Epub 1981/01/01.
- Goering P, Durbin J, Foster R, Boyles S, Babiak T, Lancee B. Social networks of residents in supportive housing. Community Mental Health J 1992;28(3):199–214.
- Pattison EM, Defrancisco D, Wood P, Frazier H, Crowder J. A psychosocial kinship model for family therapy. Am J Psychiatry 1975;132(12):1246–51.
- Mohr DC, Classen C, Barrera M. The relationship between social support, depression and treatment for depression in people with multiple sclerosis. Psychol Med 2004;34(03):533–41.
- Fyrand L, Moum T, Wichstrom L, Finset A, Glennas A. Social network size of female patients with rheumatoid arthritis compared to healthy controls. Scand J Rheumatol 2000;29(1):38–43.
- Granovetter M. The strength of weak ties. Am J Sociol 1973;78(6):1360–80.
- Wellman B, Milena G. A network is more than the sum of its ties. In: , Wellman B, (ed.) Networks in the global village. Boulder, CO: Westview; 1999. p. 83–118.
- Kennedy P, Marsh N, Lowe R, Grey N, Short E, Rogers B. A longitudinal analysis of psychological impact and coping strategies following spinal cord injury. Br J Health Psychol 2000;5(2):157–72.
- Sarason I, Sarason B, Shearing E, Pearce G. A brief measure of social support: practical and theoretical implications. J Soc Pers Relationships 1987;4:497–510.
- Wellman B, Hogan B, Berg K, Boase J, Carrasco J, Cote R, et al. Connected lives: the project. In: , Patrick P, (ed.) Networked neighborhoods. Guildford, UK: Springer; 2006. p. 157–211.
- Putnam R. Bowling aone: civic disengagement in America. New York: Simon and Schuster; 2000.
- Poortinga W. Social relations or social capital? Individual and community health effects of bonding social capital. Soc Sci Med 2006;63(1):255–70.
- Burt RS. Structural holes: the social structure of competition. Cambridge, MA: Harvard University Press; 1992.
- Gargiulo M, Benassi M. Trapped in your own net? Network cohesion, structural holes, and the adaptation of social capital. Organ Sci 2000;11(2):183–96.
- Krackhardt D. The strength of strong ties: the importance of philos in organizations. In: , Nohria NaE RG, (ed.) Networks and organizations: structure, form, and action. USA: Harvard College; 1992. p. 216–39.
- Coleman JS. Social capital in the creation of human capital. Am J Sociol 1988;94 (Supplement: Organizations and Institutions: Sociological and Economic Approaches to the Analysis of Social Structure):S95–120.
- Sales E. Family burden and quality of life. Qual Life Res 2003;12(0):33–41.
- Goldberg A, Rickler KS. The role of family caregivers for people with chronic illness. Med Health R I 2011;94(2):41–2.
- Essue BM, Jowsey T, Jeon Y-H, Mirzaei M, Pearce-Brown CL, Aspin C, et al. Informal care and the self-management partnership: implications for Australian health policy and practice. Aust Health Rev 2010;34(4):414–22.
- Clark AM, Reid ME, Morrison CE, Capewell S, Murdoch DL, McMurray JJ. The complex nature of informal care in home-based heart failure management. J Adv Nurs 2008;61(4):373–83.
- Knoll SM, Johnson JL. Uncertainty and expectations: taking care of a cardiac surgery patient at home. J Cardiovasc Nurs 2000;14(3):64–75.
- Canadian Paraplegic Association Ontario. [cited 2012 July 30]. Available from: http://www.cpaont.org/page/about-cpa-ontario.
- Meade M, Carr L, Ellenbogen P, Barrett K. Perceptions of provider education and attitude by individuals with spinal cord injury: implications for health care disparities. Top Spinal Cord Inj Rehabil 2011;17(2):25–37.
- Post MW, Bloemen J, de Witte LP. Burden of support for partners of persons with spinal cord injuries. Spinal Cord 2005;43(5):311–9.
- Dickson A, O'Brien G, Ward R, Allan D, O'Carroll R. The impact of assuming the primary caregiver role following traumatic spinal cord injury: an interpretative phenomenological analysis of the spouse's experience. Psychol Health 2010;25(9):1101–20.
- Boschen KA, Tonack M, Gargaro J. The impact of being a support provider to a person living in the community with a spinal cord injury. Rehabil Psychol 2005;50(4):397–407.
- Post MWM, Ros WJG, Schrijvers AJP. Impact of social support on health status and life satisfaction in people with a spinal cord injury. Psychol Health 1999;14(4):679–95.
- Ministry of Health and Long-term Care. Caring about caregivers: caregiving for the future of Ontario. [Internet], November 2009. [cited 2012 January]. Available from: http://theconference.ca/pdf/abrown_Caring_About_Caregivers_Final_Report.pdf.
- New A. Strategy for Community Care – The Way Forward. Nationally Consistent Assessment: status update. Canberra: Australian Government, Department of Health and Ageing; 2008 [cited 2012 February 23]. Available from: http://www.health.gov.au/internet/main/publishing.nsf/Content/FAC055FFD1FFC973CA25742600032F46/$File/NCAF.pdf.