Abstract
Objective:
Luseogliflozin is a novel sodium glucose cotransporter 2 inhibitor for type 2 diabetes mellitus (T2DM) treatment. An exploratory Phase II study was conducted to assess the efficacy and safety of several doses of luseogliflozin in Japanese T2DM patients.
Patients and methods:
Japanese T2DM patients aged 20–74 years with hemoglobin A1c (HbA1c) of 6.9–10.5%, fasting plasma glucose (FPG) ≥126 mg/dL and on diet therapy were randomized in a double-blind manner to receive luseogliflozin (0.5, 2.5, or 5 mg) or placebo once daily for 12 weeks (n = 61, 61, 61, and 56, respectively). The primary endpoint was the change in HbA1c from baseline to end of treatment. Other endpoints included FPG, 2 h postprandial plasma glucose (PPG) in a meal tolerance test (MTT), and body weight. Drug safety was also assessed.
Trial registration:
Japan Pharmaceutical Information Center (identifier: JapicCTI-090908).
Results:
Changes in HbA1c from baseline to end of treatment were −0.36, −0.62, and −0.75% in the 0.5, 2.5, and 5 mg luseogliflozin groups, respectively, versus +0.06% in the placebo group (all P < 0.001). The reductions in FPG and 2 h-PPG in the MTT were also significantly greater in the luseogliflozin groups (all P < 0.01) without increases in insulin levels from baseline. Luseogliflozin reduced body weight at all doses. There were no significant differences in the incidences of adverse events among groups. Most adverse events were mild in severity. There were no serious adverse events.
Conclusions:
Although this was a small-scale study with a short duration, all tested doses of luseogliflozin significantly improved glycemic control, reduced body weight, and were well tolerated in Japanese T2DM patients over the 12-week treatment period.
Introduction
Diabetes is thought to affect more than 371 million people worldwide, of whom about 90% have type 2 diabetes mellitus (T2DM)Citation1. Although several oral antidiabetic drugs are used to treat type 2 diabetes, the risk of hypoglycemia, weight gain and insufficient efficacy may limit their use in some patientsCitation2. Dipeptidyl peptidase-4 DPP4 inhibitors are widely used in Japan, and it is possible to achieve good glycemic control without hypoglycemia using this class of drugsCitation3–5. However, although patient weight does not usually change when using DPP4 inhibitors, deteriorations in glycemic control may occur with weight gainCitation6. Therefore, it is essential that novel drugs that overcome these problems are investigated as potential therapies for T2DM.
The renal proximal tubules reabsorb most of the glucose present in the renal filtrate, and less than 1% of glucose in the renal filtrate is ultimately excreted in urine. Sodium glucose cotransporter 2 (SGLT2), which is primarily expressed in the proximal tubuleCitation7, is responsible for about 90% of glucose reabsorption in the kidneyCitation8,Citation9. Animal studies have also shown that inhibition or deletion of SGLT2 promotes urinary glucose excretion and reduces hyperglycemiaCitation10–12, confirming the role of the kidney and SGLT2 in maintaining glucose homeostasis.
These properties of SGLT2 have therefore prompted the development of SGLT2 inhibitors as novel treatments for T2DMCitation13–15. Because SGLT2 activity is independent of insulin and this transporter is not expressed in either pancreatic β cells or insulin-sensitive tissues, SGLT2 inhibitors improve glycemic control in an insulin-independent mannerCitation16.
Luseogliflozin [TS-071; (1S)-1,5-anhydro-1-[5-(4-ethoxybenzyl)-2-methoxy-4-methylphenyl]-1-thio-D-glucitol hydrate] is a novel SGLT2 inhibitor currently under development for the treatment of T2DM. Preclinical studies have shown that luseogliflozin is a specific and selective SGLT2 inhibitor, and that it enhanced urinary glucose excretion in a dose-dependent manner in animal studiesCitation17,Citation18. Luseogliflozin improved glucose tolerance without enhancing insulin secretion in Zucker fatty rats, and reduced hyperglycemia in streptozotocin-induced diabetic rats and db/db miceCitation18. Thus, luseogliflozin ameliorated hyperglycemia without increasing insulin secretion in animal models of diabetes characterized by moderate defects in insulin secretion. However, the effects of luseogliflozin on hyperglycemia and insulin secretion in clinical settings have not been investigated in detail. In one clinical study, single and multiple doses of luseogliflozin dose dependently increased urinary glucose excretion without causing hypoglycemia in healthy Japanese malesCitation19. Additionally, the administration of luseogliflozin for 7 days significantly increased urinary glucose excretion and decreased plasma glucose levels in Japanese patients with T2DMCitation20. However, these studies were too short to examine the effects on hemoglobin A1c (HbA1c) or adequately assess safety.
The prevalence of diabetes in the Western Pacific region, including Japan, is higher than that in any other regionsCitation1. Japanese patients with T2DM exhibit more severe impairments in insulin secretion than Europeans and Americans, and develop diabetes with only slight worsening of obesityCitation21. Therefore, it is important to investigate whether the SGLT2 inhibitor luseogliflozin, which reduces plasma glucose levels in an insulin-independent manner, is effective in Japanese T2DM patients with impaired insulin secretion. The results are expected to contribute to clinical practice in Japan and will be helpful to clarify the mechanism of action of SGLT2 inhibitors.
Therefore, the purpose of the present study was to examine the efficacy and safety of several doses of luseogliflozin in Japanese patients with T2DM administered for 12 weeks in clinical settings. We also investigated the effect of luseogliflozin on insulin secretion by assessing post-meal insulin secretion in Japanese patients with T2DM.
Patients and methods
Eligibility criteria
Japanese outpatients with T2DM diagnosed according to the guidelines proposed by the Japan Diabetes SocietyCitation22 were eligible if they met the following criteria: HbA1c 6.9–10.5% at Weeks -4 and -1, with a maximum change of 1.0% between these times; fasting plasma glucose (FPG) ≥126 mg/dL; prescribed with stable diet therapy ≥8 weeks before Week -4; and age 20–74 years. The exclusion criteria included the following: insulin-dependent state; diabetes other than type 2 diabetes; the presence of an endocrine disease likely to affect blood glucose; complications of renal disorders (serum creatinine level exceeding the upper limit of the reference range); history of chronic renal disorder or nephrectomy/renal transplantation; complication of or repeated urinary tract infection; clinically evident hepatic disorder (e.g., alanine aminotransferase or aspartate aminotransferase levels ≥2.5 times the upper limit of the reference range); complications of serious gastrointestinal disorder, serious cardiac disorder, or severe diabetic microangiopathy; and complication or history of malignant tumor; serious allergic disposition; use of oral antidiabetic drugs/insulin within 8 weeks before Week -4; use of an investigational drug ≤12 weeks before Week -4; past use of luseogliflozin; heavy alcohol consumption (average consumption of pure alcohol >100 mL/day); pregnant or breast feeding; or were deemed by the investigator to be unsuitable for any other reason. All of the patients provided written informed consent before enrollment.
Study design and treatments
This was a Phase II, randomized, placebo-controlled, double-blind, parallel-group study performed at 40 institutions distributed throughout Japan between April 2009 and November 2009. The study consisted of a 4 week, untreated observation period, in which patient eligibility was assessed and confirmed, followed by a 12-week treatment period. Visits were scheduled at Weeks -4 and -1 (observation period), and at Weeks 0, 2, 4, 8, and 12 in the treatment period.
Patients were randomly allocated to one of four groups (0.5, 2.5, or 5 mg luseogliflozin or placebo) in a 1:1:1:1 ratio. The procedure of allocation and procedures implemented to maintain blinding are summarized in Supplementary appendix 1. The doses of luseogliflozin were chosen based on the safety, pharmacokinetic, and pharmacodynamic data of earlier Phase I studies in healthy Japanese malesCitation19. The study drugs were taken orally, once daily before breakfast. In addition, the patients were to continue their prescribed diet therapy, which was planned for the individual patients at each institution, for the duration of the study. The prescribed number of calories for diet therapy was not to be changed after Week -4. Compliance with these treatments was assessed at each visit (Supplementary appendix 1). If hypoglycemic symptoms appeared, glucose was to be administered orally or intravenously depending on the symptoms.
Oral antidiabetic drugs, insulin, corticosteroids (except for topical use), intravenous fluids containing sugars, and other investigational drugs were prohibited for the entire study duration (observation and treatment periods). However, drugs to treat concomitant disorders (e.g., antidyslipidemic/antihypertensive drugs) could be continued if these drugs were being used from before Week -4, and if their doses and types were not to be changed during the study.
The study was conducted according to Good Clinical Practice and the Declaration of Helsinki, and was approved by the institutional review boards at each participating medical institution. This study was registered with the Japan Pharmaceutical Information Center (identifier: JapicCTI-090908).
Study endpoints and measurements
The primary efficacy endpoint was the change in HbA1c from baseline to the end of treatment. Secondary efficacy endpoints included FPG, postprandial plasma glucose (PPG), insulin, intact proinsulin, C-peptide immunoreactivity (CPR), glucagon, glycosylated albumin, body weight, and urinary glucose.
HbA1c was measured in Japan Diabetes Society (JDS) units, which were generally used in Japanese clinical practice at the time of this study. The JDS values were converted to National Glycohemoglobin Standardization Program (NGSP) units using the certified equation for Japanese patientsCitation23: HbA1c (NGSP) (%) = 1.02 × HbA1c (JDS) (%) + 0.25%.
Meal tolerance tests were performed at Weeks 0 (before study drug administration) and 12 using a test meal provided by the sponsor (516 kcal; protein 19.2%, lipids 19.7%, carbohydrates 58.4%). After an overnight fast, the patients attended the medical institution at 8:00–11:00 h, and consumed a test meal for 10 min (±5 min). Blood samples were collected before and at 0.5, 1, and 2 h after the meal to measure plasma glucose, insulin, CPR, and glucagon. Urine was pooled from the start of the meal to 2 h after the meal to measure urinary glucose. The allocated study drug was to be taken within 30 min before the meal.
Efficacy variables were measured at an independent laboratory (Mitsubishi Chemical Medience Corp., Tokyo, Japan). Safety outcomes included adverse events (AEs), clinical laboratory variables, and vital signs, which were assessed at every visit, and 12-lead electrocardiography, which was performed at Weeks -4, 0, 2, and 12. AEs were coded using the Japanese version of the Medical Dictionary for Regulatory Activities, version 12.1, in terms of system organ class and preferred term. AEs were classified in terms of severity (mild, moderate, or severe) and possible association with the study drug (definitely related, probably related, possibly related, not related, or unknown).
Statistical analyses
Based on a study of another SGLT2 inhibitorCitation24, we assumed that the difference between the mean decreases in HbA1c in the 2.5 mg luseogliflozin and placebo groups was 0.42%. With a standard deviation of 0.7%, two-sided significance level of 5%, and statistical power of 80%, at least 45 patients were needed for these two groups. We therefore planned to enroll about 50 patients per treatment group to allow for dropouts and exclusions.
Efficacy analyses were conducted in the full analysis set, which consisted of all patients who took at least one dose of the study drug and in whom efficacy variables were examined at least once. Safety analyses were conducted in the safety analysis set, which consisted of all patients who took at least one dose of the study drug and in whom the safety variables were measured at least once.
Baseline characteristics were compared among the four groups using χ2 tests and analysis of variance. A significance level of 15% (two sided) was used to examine the heterogeneity of patient characteristics.
For primary and secondary efficacy endpoints, the changes from baseline to each point of evaluation and to the end of treatment were calculated. Missing data at the end of treatment were imputed using the last observation carried forward method. The unrestricted least significant difference method was applied to calculate the least squares mean and 95% confidence interval for the changes in efficacy variables in each group, as well as differences between each luseogliflozin group and the placebo group. For these analyses, a significance level of 5% (two-sided) was used. Changes in clinical/laboratory safety variables were determined as described for the efficacy variables. All statistical analyses were performed using SAS version 9.1.3 (SAS Inc., Cary, NC, USA).
Results
Patient characteristics
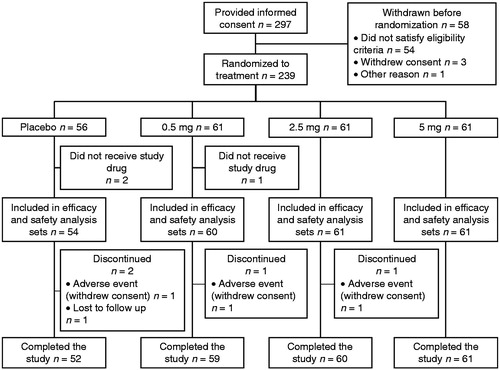
As shown in , of 297 patients who provided informed consent, 239 were randomized into the four groups, with 56–61 patients per group. Overall, 236 patients received the study drug and 232 completed the 12 week study.
The baseline characteristics of the patients are presented in . The four groups were generally similar in terms of baseline characteristics, although there was some evidence for differences at P < 0.15 among the groups for some factors, including glycosylated albumin, fasting insulin, fasting intact proinsulin, HOMA-R, and HOMA-β. The mean age and HbA1c ranged from 55.2 years to 58.3 years and from 7.88% to 8.16%, respectively.
Table 1. Patient characteristics (full analysis set).
Table 2. Changes in efficacy variables from baseline to the end of treatment (last observation carried forward, full analysis set).
Table 3. Changes in clinical/laboratory variables from baseline to the end of treatment (safety analysis set).
Glycemic control
HbA1c significantly decreased from baseline to the end of treatment in the 0.5, 2.5, and 5 mg groups compared with the placebo group (−0.36%, −0.62%, and −0.75%, respectively, vs. +0.06%; all, P < 0.001; and ). The magnitude of the reduction tended to be greater in the 2.5 and 5 mg groups than in the 0.5 mg group. The mean decrease from baseline in HbA1c was significantly lower at Weeks 4, 8, and 12 in each of the luseogliflozin groups than in the placebo group (all, P < 0.001), and at Week 2 in the 5 mg luseogliflozin group (P = 0.015). The change in HbA1c from baseline to the end of treatment in each luseogliflozin group tended to be greater in patients with higher baseline HbA1c levels, although the numbers of subjects in these subgroups were low (Supplementary table 1). Overall, 8.6% (5/58), 15.0% (9/60), and 20.3% (12/59) of patients achieved HbA1c <7.0% at the end of treatment in the 0.5, 2.5, and 5 mg luseogliflozin groups, respectively, compared with 7.5% (4/53) in the placebo group.
Figure 2. (a) Changes in HbA1c from baseline to each visit or end of treatment (EOT). *P = 0.015 for 5 mg luseogliflozin vs. placebo; †P < 0.001 for all luseogliflozin groups vs. placebo. (b) Placebo-adjusted change in HbA1c from baseline to the EOT. (c) Changes in FPG from baseline to each visit or EOT. *P < 0.05 for 0.5 mg luseogliflozin vs. placebo; †P < 0.001 for 2.5 and 5 mg luseogliflozin vs. placebo. (d) Changes in body weight from baseline to each visit or EOT. *P < 0.05 for 0.5 mg luseogliflozin vs. placebo; †P < 0.001 for 2.5 and 5 mg luseogliflozin vs. placebo. Values are means ± standard error (a, c, and d) or least squares mean ± 95% confidence interval (b). All data are shown for the full analysis set. The last observation carried forward method was applied to data at the EOT. Differences between each luseogliflozin group and placebo were analyzed by the unrestricted least significant difference method. HbA1c, hemoglobin A1c; FPG, fasting plasma glucose.
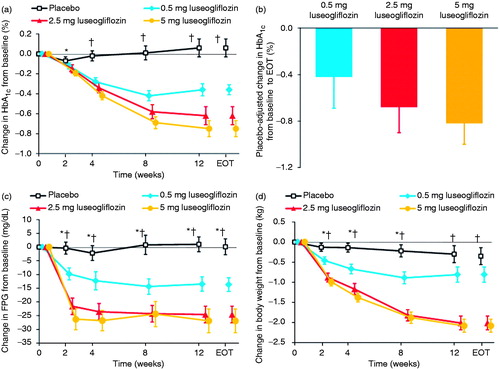
Consistent with the changes in HbA1c, the decreases in FPG from baseline to each visit were significantly greater in all of the luseogliflozin groups than in the placebo group (; all P < 0.05 for 0.5 mg luseogliflozin; all P < 0.001 for 2.5 or 5 mg luseogliflozin), as were the changes from baseline to the end of treatment (). Notably, the reductions in FPG were apparent by Week 2 in all luseogliflozin groups, and the changes tended to be greater in the 2.5 and 5 mg groups than in the 0.5 mg group.
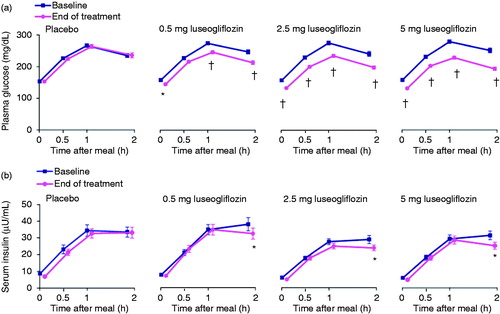
Meal tolerance test
shows the changes in glucose and insulin levels during the meal tolerance test. There were minimal changes in plasma glucose and serum insulin levels at each time-point during the meal tolerance test from baseline to the end of treatment in the placebo group. By contrast, FPG and PPG decreased from baseline to the end of treatment in each of the luseogliflozin groups. The decreases in FPG and PPG were significantly greater in the luseogliflozin groups than in the placebo group (P = 0.004 for before the meal in the 0.5 mg group; P < 0.001 for other groups and times, except at 0.5 h after the meal in the 0.5 mg group; and ). The magnitudes of the decreases in plasma glucose levels in the luseogliflozin groups tended to increase over time after the meal. The plasma glucose AUC0–2h also decreased significantly from baseline to the end of treatment in each of the luseogliflozin groups compared with placebo (all P < 0.001). At baseline, serum insulin levels reached a plateau at 1 h after the meal and reached a peak at 2 h after the meal in all four groups. Meanwhile, 2 h insulin levels were lower at the end of treatment than at baseline in the luseogliflozin groups, consistent with the changes in plasma glucose levels. At the end of treatment, the insulin levels reached a peak at 1 h after the meal, which was earlier than that at baseline. The decreases in 2 h insulin levels were significantly greater in the luseogliflozin groups than in the placebo group (all P < 0.05; and ). However, the changes in serum insulin levels at 0.5 and 1 h after the meal were small or non-existent in each of the luseogliflozin groups, and were not statistically significant compared with the placebo group. In addition, as expected from its mechanism of action, luseogliflozin dose dependently and significantly increased urinary glucose excretion relative to baseline values and the values in the placebo group ().
Figure 3. Plasma glucose (a) and insulin (b) levels during the meal tolerance tests performed at Week 0 and at the end of treatment (EOT). Values are means ± standard error. All data are shown for the full analysis set. The last observation carried forward method was applied to data at EOT. Changes from baseline and differences in the change from baseline to EOT between each luseogliflozin group and placebo were analyzed by the unrestricted least significant difference method. *P < 0.05 vs. placebo; †P < 0.001 vs. placebo.
Body weight
Body weight decreased from baseline in all of the luseogliflozin groups as early as Week 2 and continued to decline for the entire duration of the study (). The reductions at the end of treatment () were significantly greater in the 2.5 and 5 mg luseogliflozin groups than in the placebo group.
Adverse events
The incidence of AEs ranged from 36.1% to 50.0% in each group, while that of adverse drug reactions (ADRs) ranged from 7.4% to 23.0% (). There were no significant differences in the incidences of AEs and ADRs among the four groups. Most AEs were classified as mild and none was classified as severe. There were no deaths during the study and there were no serious AEs.
Table 4. List of adverse events (safety analysis set) defined according to the MedDRA.
In one patient in each of the placebo, 0.5 mg, and 2.5 mg groups, the study drug was suspended and then discontinued because of AEs. The events in the luseogliflozin groups (diarrhea in the 0.5 mg group and penile ulceration in the 2.5 mg group) were classified as mild and the patients recovered.
The most common AEs with an incidence of ≥3% in any luseogliflozin group are listed in . The most common ADRs, with an incidence of ≥3% in any luseogliflozin group, were increased β-N-acetyl-D-glucosaminidase (NAG), pollakiuria, and the presence of ketone bodies in urine.
We also examined the incidence of AEs of special interest (hypoglycemia, urinary tract infections, genital infections, AEs related to pollakiuria, AEs related to renal function, and AEs related to volume depletion) (). Hypoglycemia occurred in one patient treated with 0.5 mg luseogliflozin. This patient reported feeling dizzy and having visual disturbances; these symptoms disappeared after eating. Urinary tract infection occurred in one patient in the 0.5 mg luseogliflozin group who experienced two episodes of cystitis, which resolved after treatment. Both events were considered possibly related to the study drug. Genital infections occurred in one patient in each of the 2.5 mg (vulvitis) and 5 mg groups (vulvovaginal candidiasis), and were mild in severity. Regarding AEs related to volume depletion, thirst occurred in one patient in each of the 0.5 mg and 2.5 mg groups, but these events resolved without treatment. The incidence of AEs related to renal function was similar among the study groups.
Clinical and laboratory variables
shows the clinical and laboratory variables at baseline and the changes from baseline to the end of treatment. The reductions in systolic blood pressure from baseline to the end of treatment were significantly greater in the 2.5 and 5 mg groups than in the placebo group (both P < 0.05).
The red blood cell count, hemoglobin, hematocrit, and blood urea nitrogen increased significantly from baseline to the end of treatment in all of the luseogliflozin groups versus the placebo group. However, the magnitudes of the increases were small and none of the patients had increases in these parameters that were judged as AEs. Urine volume increased in all of the luseogliflozin groups at the end of treatment from baseline, and the increase was significant in the 5 mg luseogliflozin group versus placebo. Liver enzymes, uric acid, and triglycerides tended to decrease in the luseogliflozin groups versus the placebo group, while free fatty acid levels tended to increase. There were no clinically meaningful changes in serum creatinine, electrolytes, or cystatin C (data not shown).
Discussion
This study revealed that luseogliflozin monotherapy for 12 weeks significantly improved glycemic control (HbA1c, FPG, and PPG) and reduced body weight in Japanese patients with T2DM. The reduction in plasma glucose observed in this study was associated with the increase in urinary glucose excretion, and these effects tended to be greater at luseogliflozin doses of 2.5 or 5 mg than at 0.5 mg. The reductions in HbA1c and FPG were apparent within 2–4 weeks of starting treatment, and were maintained throughout the 12-week treatment period. Plasma glucose decreased rapidly, reaching a plateau at Week 2. This effect was consistent with the results of a prior clinical pharmacology study of luseogliflozinCitation20, and seems to be a favorable aspect of its treatment of T2DM.
The effects of SGLT2 inhibitors in Japanese T2DM patients, who often have impaired early phase insulin secretion after a meal, seem to have attracted considerable attention. The results of the meal tolerance tests performed in the present study are particularly intriguing. In the present study, the early phase insulin levels were not altered by luseogliflozin treatment. However, when we consider that the plasma glucose levels were reduced by luseogliflozin, the early phase insulin secretion seems to have improved. We also demonstrated that the plasma insulin levels measured 2 h after meal ingestion were decreased by luseogliflozin, probably because of the lower glucose levels. Taken together, these results suggest that luseogliflozin indirectly improved insulin secretion in Japanese patients with T2DM.
Luseogliflozin monotherapy not only improved glycemic control but also reduced body weight. The reduction in body weight in the luseogliflozin groups was significant within 2 weeks of starting treatment and had not reached a plateau by Week 12. An increase in energy use and an increase in urine output were thought to contribute to its mechanism.
Luseogliflozin also tended to improve blood pressure, uric acid, and liver function. Therefore, it seems likely that luseogliflozin may have some benefits on the metabolic profiles of T2DM patients.
In this, the first 12 week study of luseogliflozin in patients with T2DM, all of the tested doses of luseogliflozin were well tolerated. Most of the AEs were classified as mild, and there were no deaths or serious AEs during the treatment period.
As expected from the characteristics of SGLT2 inhibitors, luseogliflozin was associated with a low incidence of hypoglycemia. Because SGLT2 is not expressed in pancreatic β cells or insulin-sensitive tissues (e.g., liver and muscle), luseogliflozin is expected to work in an insulin-independent manner. In addition, SGLT2 inhibitors inhibit the reabsorption of about 30–50% of the filtered glucose load, avoiding hypoglycemiaCitation25. Only one episode of hypoglycemia occurred in our study, and it was classified as mild.
Because the kidney is the target organ of luseogliflozin, the effects of luseogliflozin on renal function were assessed. In this study, although increases in markers of renal tubular disorders (e.g., increased NAG or increased urinary β2-microgloblin) were observed in the luseogliflozin groups, they were also observed in the placebo group. These increases were all classified as mild in severity. This means that luseogliflozin did not cause renal impairment or failure in this study. However, longer studies will be needed to assess the effects of luseogliflozin on kidney function.
Increased urinary glucose is also associated with increased risk of genital and urinary tract infections during treatment with SGLT2 inhibitorsCitation26,Citation27. Nevertheless, the incidence of these events was low, all events were classified as mild, and all resolved after appropriate treatment in this study.
In this study, the presence of ketone bodies in urine was observed in two patients who were treated with 2.5 mg luseogliflozin. It is possible that the increase in urinary glucose excretion during treatment with luseogliflozin might induce caloric loss and lipolysis. Further studies are needed to examine the changes in serum ketone levels during treatment with luseogliflozin.
The slight increases in red blood cell count, hemoglobin, hematocrit, and blood urea nitrogen in the luseogliflozin groups were possibly due to volume depletion. The increase in urinary glucose excretion might cause osmodiuresis, resulting in increases in these parameters.
The main limitations of this study were the short study duration and the small sample size, which might explain the low incidence of AEs of special interest. Therefore, further studies are necessary to fully evaluate the tolerability of luseogliflozin. Several longer and larger studies including other doses were recently completed, and the results will provide further insight into the safety profile of luseogliflozin.
Conclusions
In conclusion, this was the first randomized controlled trial examining the efficacy and safety of luseogliflozin in Japanese patients with T2DM. Monotherapy with luseogliflozin for 12 weeks was associated with marked improvements in glycemic control and reductions in body weight, and was well tolerated in Japanese patients with T2DM.
Transparency
Declaration of funding
Luseogliflozin is being developed by Taisho Pharmaceutical Co. Ltd. This study was supported by Taisho Pharmaceutical Co. Ltd.
Declaration of financial/other relationships
Y.Se. has disclosed that he has received consultancy fees or lecture fees from Sanofi, Novo Nordisk, Eli Lilly and Company, GlaxoSmithKline, Astellas Pharma, Takeda Pharmaceuticals, Boehringer Ingelheim, Johnson & Johnson, Becton Dickinson and Company, AstraZeneca, and Taisho Pharmaceutical Co. Ltd. T.S. has disclosed that he has received joint research funds from Canon Inc. and consultancy fees from Taisho Pharmaceutical Co. Ltd. A.F. has disclosed that he has received consultancy fees from Taisho Pharmaceutical Co. Ltd. S.S. and Y.Sa. have disclosed that they are employees of Taisho Pharmaceutical Co. Ltd.
CMRO peer reviewers on this manuscript have received an honorarium from CMRO for their review work, but have no relevant financial or other relationships to disclose.
Supplementary Material
Download PDF (34.2 KB)Acknowledgments
The authors thank Nicholas D. Smith PhD for editorial support.
Previous presentation: Parts of this study were reported as an abstract and poster (abstract 998-P) at the 71st Annual Scientific Sessions of the American Diabetes Association, 24–28 June 2011, San Diego, CA, USA; and as an abstract and oral presentation (abstract 148) at the 47th Annual Meeting of the European Association for the Study of Diabetes (EASD), 12–16 September 2011, Lisbon, Portugal.
References
- International Diabetes Federation. IDF Diabetes Atlas 5th Edition 2012 Update: New Estimates for 2012 of Diabetes Prevalence, Mortality, and Healthcare Expenditure. 2012
- Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hyperglycemia in type 2 diabetes: a patient-centered approach: position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 2012;35:1364-79
- Ahren B. DPP-4 inhibition and islet function. J Diabetes Investig 2012;3:3-10
- Seino Y, Yabe D. Glucose-dependent insulinotropic polypeptide and glucagon-like peptide-1: Incretin actions beyond the pancreas. J Diabetes Investig 2013;4:108-30
- Kubota A, Maeda H, Kanamori A, et al. Efficacy and safety of sitagliptin monotherapy and combination therapy in Japanese type 2 diabetes patients. J Diabetes Investig 2012;3:503-9
- Kubota A, Yabe D, Kanamori A, et al. Factors influencing durability of the glucose-lowering effect of sitagliptin combined with a sulfonylurea. J Diabetes Investig 2014: published online 11 February 2014, doi:10.1111/jdi.12182
- Sabolic I, Vrhovac I, Eror DB, et al. Expression of Na+-D-glucose cotransporter SGLT2 in rodents is kidney-specific and exhibits sex and species differences. Am J Physiol Cell Physiol 2012;302:C1174-88
- Harada N, Inagaki N. Role of sodium-glucose transporters in glucose uptake of the intestine and kidney. J Diabetes Investig 2012;3:352-3
- Bakris GL, Fonseca VA, Sharma K, et al. Renal sodium-glucose transport: role in diabetes mellitus and potential clinical implications. Kidney Int 2009;75:1272-7
- Jurczak MJ, Lee HY, Birkenfeld AL, et al. SGLT2 deletion improves glucose homeostasis and preserves pancreatic beta-cell function. Diabetes 2011;60:890-8
- Vallon V, Platt KA, Cunard R, et al. SGLT2 mediates glucose reabsorption in the early proximal tubule. J Am Soc Nephrol 2011;22:104-12
- Vallon V, Rose M, Gerasimova M, et al. Knockout of Na-glucose transporter SGLT2 attenuates hyperglycemia and glomerular hyperfiltration but not kidney growth or injury in diabetes mellitus. Am J Physiol Renal Physiol 2013;304:F156-67
- Abdul-Ghani MA, DeFronzo RA. Inhibition of renal glucose reabsorption: a novel strategy for achieving glucose control in type 2 diabetes mellitus. Endocr Pract 2008;14:782-90
- DeFronzo RA, Davidson JA, Del Prato S. The role of the kidneys in glucose homeostasis: a new path towards normalizing glycaemia. Diabetes Obes Metab 2012;14:5-14
- Nair S, Wilding JP. Sodium glucose cotransporter 2 inhibitors as a new treatment for diabetes mellitus. J Clin Endocrinol Metab 2010;95:34-42
- Ferrannini E, Solini A. SGLT2 inhibition in diabetes mellitus: rationale and clinical prospects. Nat Rev Endocrinol 2012;8:495-502
- Kakinuma H, Oi T, Hashimoto-Tsuchiya Y, et al. (1S)-1,5-anhydro-1-[5-(4-ethoxybenzyl)-2-methoxy-4-methylphenyl]-1-thio-D-glucitol (TS-071) is a potent, selective sodium-dependent glucose cotransporter 2 (SGLT2) inhibitor for type 2 diabetes treatment. J Med Chem 2010;53:3247-61
- Yamamoto K, Uchida S, Kitano K, et al. TS-071 is a novel, potent and selective renal sodium-glucose cotransporter 2 (SGLT2) inhibitor with anti-hyperglycaemic activity. Br J Pharmacol 2011;164:181-91
- Sasaki T, Seino Y, Fukatsu A, et al. Safety, Pharmacokinetics, and pharmacodynamics of single and multiple luseogliflozin dosing in healthy Japanese males: a randomized, single-blind, placebo-controlled trial. Adv Ther 2014: published online 18 February 2014, doi:10.1007/s12325-014-0102-3
- Sasaki T, Seino Y, Fukatsu A, et al. TS-071, a novel potent and highly selective renal sodium-glucose co-transporter 2 (SGLT2) inhibitor, increases urinary glucose excretion and reduces plasma glucose levels in Japanese patients with type 2 diabetes mellitus. 47th European Association for the Study of Diabetes (EASD) Annual Meeting, 12–16 September 2011. Lisbon, Portugal, 2011
- Fujimoto WY, Boyko EJ, Hayashi T, et al. Risk factors for type 2 diabetes: lessons learned from Japanese Americans in Seattle. J Diabetes Investig 2012;3:212-24
- Kuzuya T, Nakagawa S, Satoh J, et al. Report of the Committee on the Classification and Diagnostic Criteria of Diabetes Mellitus. Diabetes Res Clin Pract 2002;55:65-85
- Kashiwagi A, Kasuga M, Araki E, et al. International clinical harmonization of glycated hemoglobin in Japan: from Japan Diabetes Society to National Glycohemoglobin Standardization Program values. Diabetol Int 2012;3:8-10
- List JF, Woo V, Morales E, et al. Sodium-glucose cotransport inhibition with dapagliflozin in type 2 diabetes. Diabetes Care 2009;32:650-7
- Liu JJ, Lee T, DeFronzo RA. Why Do SGLT2 inhibitors inhibit only 30–50% of renal glucose reabsorption in humans? Diabetes 2012;61:2199-204
- Nicolle LE, Capuano G, Ways K, et al. Effect of canagliflozin, a sodium glucose co-transporter 2 (SGLT2) inhibitor, on bacteriuria and urinary tract infection in subjects with type 2 diabetes enrolled in a 12-week, phase 2 study. Curr Med Res Opin 2012;28:1167-71
- Nyirjesy P, Zhao Y, Ways K, et al. Evaluation of vulvovaginal symptoms and Candida colonization in women with type 2 diabetes mellitus treated with canagliflozin, a sodium glucose co-transporter 2 inhibitor. Curr Med Res Opin 2012;28:1173-8