Abstract
Objectives:
To assess the incidence and economic impact of postoperative ileus (POI) following laparotomy (open) and laparoscopic procedures for colectomies and cholecystectomies in patients receiving postoperative pain management with opioids.
Methods:
Using the Premier research database, we retrospectively identified adult inpatients discharged between 2008 and 2010 receiving postsurgical opioids following laparotomy and laparoscopic colectomy and cholecystectomy. POI was identified through ICD-9 diagnosis codes and postsurgical morphine equivalent dose (MED) determined.
Results:
A total of 138,068 patients met criteria, and 10.3% had an ileus. Ileus occurred more frequently in colectomy than cholecystectomy and more often when performed by laparotomy. Ileus patients receiving opioids had an increased length of stay (LOS) ranging from 4.8 to 5.7 days, total cost from $9945 to $13,055 and 30 day all-cause readmission rate of 2.3 to 5.3% higher compared to patients without ileus. Patients with ileus received significantly greater MED than those without (median: 285 vs. 95 mg, p < 0.0001) and were twice as likely to have POI. MED above the median in ileus patients was associated with an increase in LOS (3.8 to 7.1 days), total cost ($8458 to $19,562), and readmission in laparoscopic surgeries (4.8 to 5.2%). Readmission rates were similar in ileus patients undergoing open procedures regardless of MED.
Conclusions:
Use of opioids in patients who develop ileus following abdominal surgeries is associated with prolonged hospitalization, greater costs, and increased readmissions. Furthermore, higher doses of opioids are associated with higher incidence of POI. Limitations are related to the retrospective design and the use of administrative data (including reliance on ICD-9 coding). Yet POI may not be coded and therefore underestimated in our study. Assessment of pre-existing disease and preoperative pain management was not assessed. Despite these limitations, strategies to reduce opioid consumption may improve healthcare outcomes and reduce the associated economic impact.
Introduction
Postoperative ileus (POI) is a well known consequence and complication of gastrointestinal (GI), pelvic, and some non-abdominal surgeries, resulting in significant morbidity and patient discomfort and dissatisfactionCitation1,Citation2. Clinically, it is characterized by inability to tolerate solid food, delayed passage of flatus and formed stool, abdominal pain and distension, nausea, vomiting, anorexia, and accumulation of gas or fluids in the bowelCitation3,Citation4. More serious complications can include GI perforation, nosocomial infections, malnourishment and muscular atrophyCitation5. These sequelae make POI one of the most important factors of prolonged hospitalization following abdominal surgeryCitation3. Moreover, prolonged hospitalization can increase the risk of hospital-acquired infectionsCitation6 with the potential to further increase healthcare costs.
The development and consequences of POI following abdominal surgery is further complicated by the need for opioids to manage moderate to severe painCitation4,Citation7. Opioids are associated with bowel dysfunction, POI in non-abdominal procedures, and can exacerbate and prolong recovery from ileus following abdominal surgeriesCitation8,Citation9,Citation10. A systematic review by Wheeler et al. from MEDLINE literature published between 1990 and 2000 reported that 30% of patients receiving opioids for pain treatment experienced GI adverse events including nausea, vomiting and ileus of prolonged durationCitation11. A recent review of the Premier database from 2008 to 2010 revealed that, in selected surgeries, 6.1% of patients treated with opioids had a GI event including ileusCitation12. A 2012 survey of pharmacists identified GI complications as the most commonly reported complication of opioid pain managementCitation13.
Opioids are associated with POICitation1,Citation3,Citation4,Citation10,Citation14 and the dose of morphine required for effective analgesia is in excess of that which causes POICitation1,Citation15. Activation of receptors in the GI tract is responsible for inhibition of gut motility whereas the receptors in the central nervous system mediate analgesiaCitation3,Citation16. Return of GI function appears to be related to opioid dosage, duration, and route of administration and extent of small intestine, stomach and colon involvementCitation4,Citation6,Citation10,Citation14.
Approximately 22 million inpatient surgical procedures are performed annually in the United States, and an estimated 2.7 million of these procedures lead to POI lasting multiple daysCitation8,Citation9. A retrospective review from 2002 of ICD-9 codes revealed a 4.3% rate of ileus from more than 800,000 US surgical patientsCitation6,Citation8,Citation9. POI lengthens hospital stay by 2–3 days, is associated with a readmission rate of 10% in abdominal surgery patients, and costs the healthcare system upwards of a billion dollars per yearCitation4,Citation7,Citation17. Nearly 350,000 colorectal and small bowel resections occur annually, at an average stay of almost 11 days, costing the healthcare system $20 billionCitation18. POI affects up to 15–20% of patients undergoing abdominal procedures, 6% to 10% undergoing colon surgery and 10% of patients undergoing cardiac or orthopedic surgeriesCitation15,Citation19.
The purpose of our study was to assess the incidence and economic impact of POI following laparotomy (open) and laparoscopic procedures for colectomies and cholecystectomies. We hypothesized that treatment of postsurgical pain with opioids places patients at increased risk for development and/or prolongation of POI following abdominal procedures, resulting in prolonged hospitalization, increased hospital costs, and need for readmission. Specifically, we sought to (1) determine the incidence of POI following open and laparoscopic colectomy and cholecystectomy; (2) assess the relationship between the amount of postsurgical opioid use and POI for each surgery and its impact on hospital length of stay (LOS), total hospital visit cost and 30 day all-cause readmission; and (3) determine the relationship of morphine equivalent dose to the occurrence of ileus and impact on LOS, total visit cost and 30 day readmission.
Methods
Premier research database
The Premier research database has been described in detail elsewhereCitation12. Briefly, it is a large, service-level, all-payer (including Medicaid, Medicare and commercial) comparative database containing information on approximately five million annual hospital discharges (approximately one-fifth of all acute care hospitalizations in the US) from more than 475 hospitals that primarily represent non-profit, non-governmental, community and teaching hospitals, and health systems. The Premier database includes data on demographic characteristics, discharge diagnoses, and discharge status; provides a daily record of all billed items including procedures, medications, laboratory tests, and diagnostic and therapeutic services at the individual patient level; and includes all International Classification of Diseases–9th Revision–Clinical Modification (ICD-9-CM) diagnosis and procedure codes recorded by the hospital.
Patient population
Patients ≥18 years of age admitted for one of the following abdominal surgical procedures – open colectomy, laparoscopic colectomy, open cholecystectomy, laparoscopic cholecystectomy – and discharged between 1 September 2008 and 31 August 2010 were included in this retrospective analysis including elective and urgent or emergency procedures. Data collected through 30 September 2010 allowed identification of patients with a 30 day readmission at the same hospital. Demographic and clinical characteristics of age, gender, race/ethnicity, admission source, and discharge destination/status were recorded. Use of de-identified information from the database obviated the need for Institutional Review Board (IRB) approval.
All surgical patients in the study received at least one postoperative dose of opioid analgesic. The ileus group was defined as those patients who developed POI as identified by ICD-9 codes 997.4 (Digestive system complications: Complications of intestine [internal anastomosis and bypass not elsewhere classified, except that involving the urinary tract]) and 560.1 (Adynamic ileus; ileus [of intestine] [of bowel] [of colon]; paralysis of intestine or colon) at any positionCitation5. The remainder of the patients receiving opioids was termed the no ileus group.
Opioid analgesics and morphine equivalent dose
Opioid analgesic use included opioid and opioid combination medications and was identified by searching charge master descriptions. String searches were used and included spelling variations to ensure capture of all drugs. Morphine equivalent dose (MED) was calculated and represents the total dose of opioids used during the postoperative time period through discharge. The postoperative dosages of opioids were determined using charge master records and then non-morphine analgesics were converted to an equivalent dose of parenteral morphine with standard conversion tablesCitation20. The MED value for each identified patient was utilized to calculate median MED values for each surgery.
Outcome assessments: length of hospital stay, total hospital cost and 30 day readmission
Hospital LOS and total reported hospital costs were measured during the index visit. LOS in days was reported by the hospital for each discharge. Hospital costs included such categories as medications, operative procedures, diagnostic procedures, laboratory tests, and professional and administrative costs. Readmission was defined as readmission of an individual to the same hospital within 30 days of discharge date for any cause.
Statistical analyses
All statistical analyses were performed using Version 9.2 of the SAS System for Unix (SAS Institute Inc., Cary, NC, USA). Descriptive statistics for continuous data included mean, standard deviation, median, interquartile range (IQR), and minimum and maximum values. Since length of stay, cost and dose data are not normally distributed, medians and IQR are reported. The Wilcoxon rank-sum test was used to compare medians to determine overall statistical significance of continuous variables between patients exhibiting postoperative ileus and no postoperative ileus. The chi-square test determined significance between ileus and no ileus in categorical comparisons and expressed as percentages. The Wilcoxon rank-sum test was also used to compare medians calculated for morphine equivalent dosing on outcome measurements. A p value ≤0.05 was considered statistically significant. To determine the relationship between the use of above-median total postoperative MED and occurrence of ileus, unadjusted odds ratios (ORs) were calculated. Confidence intervals (95%) that did not include 1 were considered statistically significant.
Results
Study population and demographics
A total of 138,068 patients were identified from the database as having one of the selected surgeries, an ICD-9 coding for ileus, and at least one dose of opioid. The overall incidence of postoperative ileus was 10.3%. The respective occurrence of ileus was 20.6% and 14.6% for patients undergoing open and laparoscopic colectomy and 11.6% and 3.2% undergoing open and laparoscopic cholecystectomy. Regardless of abdominal procedure and surgical technique, patients in the ileus group were significantly older (median [IQR]: 66 [54–77] vs. 57 [42–71], p < 0.0001) and consisted of more white (70% vs. 63.7%, p < 0.0001) males (52% vs. 38.6%, p < 0.0001) when compared to the no ileus group. Patients from both groups represented rural and urban hospitals and teaching and non-teaching centers from all major US geographical locations. Demographics and comparisons for the individual surgical groups are presented in .
Table 1. Demographics in ileus and no ileus patients for open and laparoscopic colectomy and open and laparoscopic cholecystectomy.
Hospital length of stay
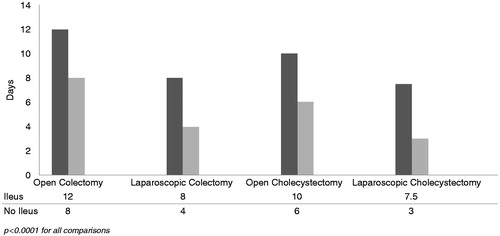
Total number of hospital days for the entire study population was greater in patients with ileus compared to those without (10 [7–16] days vs. 4 [3–7] days; p < 0.0001). The presence of an ileus was associated with a significantly prolonged LOS for each abdominal procedure (). The median difference in LOS associated with having an ileus was 4 days for both open and laparoscopic colectomies and 4 and 4.5 days respectively for open and laparoscopic cholecystectomies.
Total hospital costs
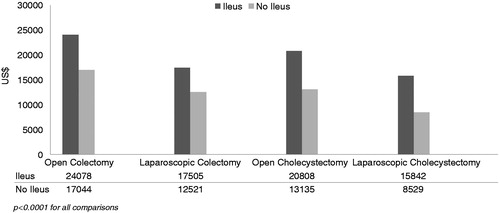
Median total hospital cost for the overall study population was significantly higher in patients with ileus versus no ileus ($21,046 [14,062–35,176] vs. $10,945 [7489–16,682]; p < 0.0001). Total cost per surgical procedure is depicted in . Whether colectomy or cholecystectomy was performed by laparotomy or laparoscopically, the total costs were significantly higher in patients with POI than without. The median difference in costs associated with ileus was $7034 for open colectomy; $4984 for laparoscopic colectomy; $7673 for open cholecystectomy; and $7313 for laparoscopic cholecystectomy.
Thirty-day readmission
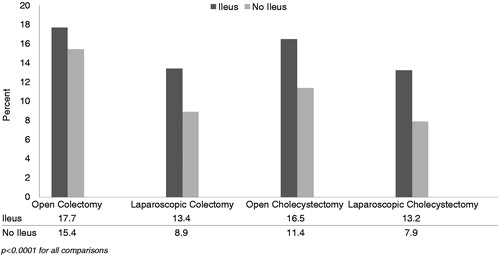
For the entire study population, the overall readmission rate was significantly higher for patients with ileus versus those without (16.1% vs. 10.2%, p < 0.0001). Both open colectomies and open cholecystectomies had higher readmission rates when compared to the same procedures performed laparoscopically (). This difference in readmission rate between ileus and no ileus groups in the open colectomy group (2.3%) was less than that noted for laparoscopic colectomy (4.5%) (p < 0.0001). For open and laparoscopic cholecystectomies the differences in the readmission rate between ileus and no ileus were 5.1% and 5.3%, respectively (p < 0.0001). The reasons for the readmission varied greatly as described by the Medicare Severity Diagnosis Related Group (MS DRG) with up to 6.7% of the discharges for 392 (Esophagitis, GI and miscellaneous Digestive) and 4.5% for 394 (other digestive system). For all the readmissions, there were over 600 different MS-DRGs coded indicating a wide range of reasons for the readmissions.
Morphine equivalent dosing (MED)
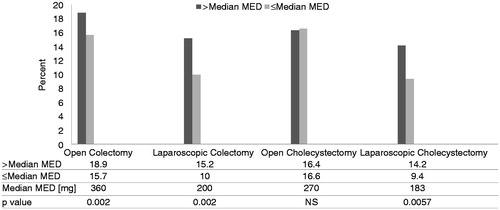
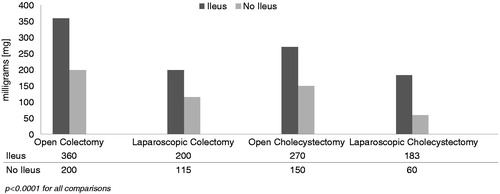
Median (IQR) equivalent milligram (mg) dose of morphine for the entire surgical study population was 105 mg (40–280). For those with ileus the median MED was 285 mg (115–720) and for those without ileus 95 mg (38–243) (p < 0.0001). For all patients having an open procedure (N = 50,476) the median MED was 230 mg (90–600) and for all those with a laparoscopic procedure (N = 87,592) the median MED was 71 mg (30–165). The median MED dose was significantly greater in the ileus vs. no ileus patients (p < 0.0001) for each specific surgery () and was 360 mg (150–903) vs. 235 mg (91–608) for open colectomies; 200 mg (84–503) vs. 115 (48–252) for laparoscopic colectomies; 270 mg (120–696) vs. 150 (65–743) for open cholecystectomies; and 183 mg (73–438) vs. 60 (24–135) for laparoscopic cholecystectomies.
Figure 4. Total morphine equivalent dose in milligrams (mg) for patients with ileus vs no ileus is represented for each surgical procedure.
For the entire surgical study population, patients receiving a total MED greater than the median MED value for their surgery had 1.99 times (OR, 95% CI, 1.92–2.06) higher odds of having an ileus than those receiving MED less than the median. The odds of having an ileus was 1.69 times greater in the open colectomy group (OR, 95% CI, 1.61–1.78) when patients were administered more than the median MED of 360 mg compared to those below the median MED. For laparoscopic colectomy, patients had 2.07 times higher odds of having an ileus (OR, 95% CI, 1.90–2.26) with a MED of more than the median MED of 200 mg. Patients receiving cholecystectomies had 2.19 times higher odds of having an ileus (OR, 95% CI, 1.92–2.48) with a MED of greater than the median value 270 mg when performed by laparotomy and more than 3.86 times higher odds of having an ileus (OR, 95% CI, 3.48–4.27) with a MED of greater than the median of 183 mg when performed laparoscopically.
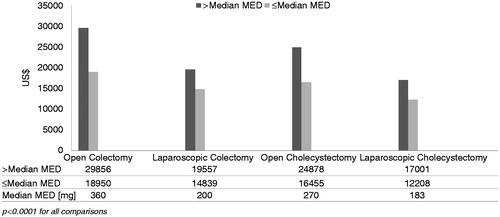
In all ileus surgical groups, doses above the median MED for the specific surgery were associated with a significant increase in median hospital LOS when compared to those equal to or below the median MED (). The median difference in length of stay associated with MED above the median was 5 and 3 days for open and laparoscopic colectomies and 3 days for both open and laparoscopic cholecystectomies. A similar pattern was observed for total hospital costs (). The median difference in costs associated with morphine dosing greater than the median was $10,636 for open colectomy; $4718 for laparoscopic colectomy; $8423 for open cholecystectomy; and $4793 for laparoscopic cholecystectomy. The median costs per day due to prolonged hospital stay associated with MED greater than the median were $2127 for open colectomy; $1573 for laparoscopic colectomy; $2808 for open cholecystectomy; and $1598 for laparoscopic cholecystectomy.
Figure 5. Hospital length of stay based on median morphine equivalent dose. Hospital length of stay in days for patients with ileus vs. no ileus is represented by the median for each surgical procedure. The median morphine dose for each surgical procedure appears in the data table.
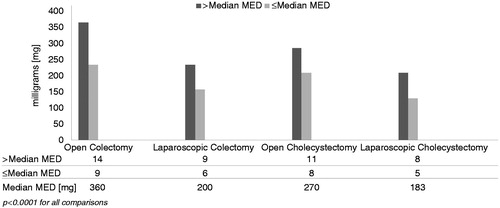
Figure 6. Total hospital costs based on median morphine equivalent dose. Total hospital cost in US dollars for patients with ileus vs. no ileus is represented by the median for each surgical procedure. The median morphine dose for each surgical procedure appears in the data table.
When 30 day readmission rates were assessed for each ileus surgery group using MED above or equal to and below the median (), a slightly different pattern emerged from that noted for LOS and total costs. The rate of readmission for open colectomy was 18.9% for above the median dose and 15.7% for below or equal to the median dose with a difference of 3.2% (p = 0.0002). For laparoscopic colectomy the rate of readmission was 15.2% for above the median dose and 10.0% for below or equal to the median dose with a difference of 5.2% (p = 0.0002). No difference in the readmission rate was discernable in the open cholecystectomies (16.4% vs. 16.6%, p = NS), and rate of readmission for laparoscopic cholecystectomy was 14.2% for above the median dose and 9.4% for below or equal to the median dose with a difference of 4.8% (p = 0.0057).
Discussion
Postoperative ileus occurred more frequently in colectomy than cholecystectomy and more often when these procedures were performed by laparotomy. The observed increase in hospital LOS, total cost for hospitalization, and 30 day all-cause readmission rate in ileus patients appears to be related to type and magnitude of surgery and associated MED. Patients with ileus were associated with higher consumption of opioids than those without ileus, and total morphine dose associated with ileus was specific to surgical technique and abdominal procedure.
Postoperative or primary ileus is an impairment of GI motility usually lasting 2–3 days and varies within the segments of the GI tractCitation5. In contrast to primary ileus, prolonged or paralytic ileus is a pseudo-obstruction of the intestines due to paralysis of the muscles that exceeds 3 days and is associated with narcotic useCitation5,Citation6. Surgical technique, physiologic stress from surgery, inhalation anesthetic agents, pre-existing GI disease, and opioid analgesia are key risk factors associated with POICitation8,Citation9,Citation14,Citation21.
Opioids contribute significantly to the severity and prolongation of POI. The harmful effects of opioids on the GI tract extend to sites from the small intestine to the anorectumCitation1,Citation17. The pharmacologic effects of opioids on GI function include decreased gastric motility and emptying with resultant increased gastroesophageal refluxCitation1,Citation17. Inhibition of propulsion to the small and large intestines results in delayed absorption of medicationsCitation1,Citation22.
Total annual national hospital cost of managing coded POI in abdominal surgeries has been projected to be $1.46 billion for both the index hospitalization and any readmission within 30 daysCitation23,Citation24. The economic consequences include labor costs for nursing staff; costs of equipment and supplies for intravenous hydration, parenteral nutrition, and nasogastric tubes; and laboratory and radiology costs. Pain and discomfort of POI and time to resumption of full activities result in significant patient dissatisfactionCitation1,Citation2. Opioid-related adverse events occurring from treatment of pain in abdominal and non-abdominal surgeries are independently and similarly associated with significant resource utilization, increased economic impact, and patient dissatisfactionCitation12. The present study formally addressed healthcare and economic outcomes in patients who developed POI following colectomy and cholecystectomy and the dosages of opioids received for pain control.
As might be expected from direct manipulation of the colon, our study showed that colectomy performed by open or laparoscopic techniques was associated with an incidence of POI ranging from 14.6 to 20.6%, LOS from 10.9 to 15.4 days, costs of $25,238 to $35,686, and 30 day all-cause readmission rates from 13.4 to 17.7%. Another large database study from 2004 assessing more than 17,000 colectomies from 500 hospitals demonstrated a similar ileus incidence of 17.4%, mean hospital stay of 13.8 days, and total cost of $25,089. Although 30 day readmission rates were not determined in this study, others have reported 3.6% in patients undergoing abdominal procedures and 10% in patients undergoing colorectal surgeryCitation24.
For open and laparoscopic cholecystectomies, we observed a similar pattern of LOS, hospital costs, and readmission rates in ileus patients although the magnitude was not as great as that noted for colectomies. Comparison of our findings to other studies was limited as a literature review of the topic yielded little information. An early study from 1993 reported that 20 patients undergoing laparoscopic cholecystectomy did not develop POI since they did not experience abdominal discomfort on the first postoperative day and bowel sounds returned within 6 hours after surgery, first flatus after 12 hours, and bowel movement between 24 and 36 hoursCitation25. Although uncommon, gallstone ileus has been reported following gallbladder removal whereby ‘lost’ gallstones can cause small bowel obstructionCitation26,Citation27.
While the use of laparoscopic surgery is associated with lower risk of ileus and less administration of opioids in our study, it has not eliminated it. This may reflect the evolution of laparoscopic surgery for more advanced and complicated proceduresCitation28. Incision length is not associated with ileus or greater need for morphine in patients undergoing colectomiesCitation29. With respect to cholecystectomies, duration of anesthesia, abdominal manipulation, and operative dissection is similar between open and laparoscopic techniques even though the abdominal cavity is not openedCitation25.
A key finding of our study is the relationship of total cumulative MED to ileus for each surgery and the impact on increasing LOS, costs, and readmission rates. The calculated total cumulative MED dose for the postoperative period was greatest in all procedures performed by laparotomy and in all colectomy surgeries regardless of technique employed. Conversion of dispensed opioids to MED permits the quantification of morphine in all compounds. Morphine, unlike other opiates, has a more pronounced impact on POICitation30. It is a natural opium alkaloid with greater affinity and selectivity for mu-opioid receptors, and its metabolites are more potent than morphine itself. Its onset of analgesia is rapid, with peak effect in 1–2 hours and elimination half-life of 3–5 hoursCitation31.
In our study, although we did not address the effect of opioid route of administration on POI, all have an influenceCitation10,Citation15,Citation30. Intravenously administered morphine has a more pronounced effect on the mu-opioid receptors in the gut than epidural administrationCitation30. Barletta et al. in their study of 279 patients undergoing open and laparoscopic colectomies found a correlation of intravenous opioid use with total hydromorphone dose, maximum daily hydromorphone dose, average daily hydromorphone dose and days of intravenous narcotics. The strongest association was with intravenous hydromorphone equivalents greater than 2 mg dailyCitation32. In another study of colectomy patients, the more morphine that was administered solely through patient-controlled analgesia (PCA), the longer to return of bowel sounds, flatus and first bowel movementCitation6,Citation29.
Fast tracking protocols and enhanced clinical pathways have been instituted by hospitals to reduce occurrence and prolongation of POI. Strategies include laparoscopic surgery, early ambulation and nutrition, avoiding nasogastric tubes and discontinuing opioids as soon as possibleCitation7. Pharmacologic agents that minimize or ameliorate the need for opioids have been investigatedCitation18. Alvimopan and methylnaltrexone, selective peripheral mu-opioid receptor antagonists that do not cross the blood–brain barrier to compromise the analgesic effects of concomitant opioids, have demonstrated mild to moderately severe bowel-related adverse effectsCitation10 that can include abdominal cramping and flatulenceCitation33.
Epidural anesthesia and other opioid-sparing analgesia have been shown to reduce duration of POICitation21,Citation22. Bupivacaine, a local anesthetic used in epidural anesthesia, may be useful in the setting of POI following abdominal surgeries. Following major hepatobiliary surgery, epidural analgesia with morphine plus bupivacaine delivered 1 hour prior to end of the operation allowed for a more rapid return of both normal gut activity with bowel sounds returning in 6 hours postoperatively compared to 30 hours in a morphine alone group and early enteral nutrition compared with epidural analgesia with morphine onlyCitation34. In another study, enhanced recovery of GI function after colonic surgery was observed when epidural bupivacaine with and without morphine was compared to epidural morphine or PCA morphineCitation35.
The limitations of this study are in part related to the known inherent problems associated with the use of large databases. Specific to our study is reliance on accurate and complete ICD-9 coding. In the case of POI, since it is an expected complication of intra-abdominal surgery, physicians do not always code for it or its symptoms unless it exceeds 3 daysCitation7,Citation30. Hence, the incidence observed in this study could be underestimated. Additionally, we did not assess the contribution of pre-existing GI disease and pre- or intra-operative opioid use to POI, and opioid dose was not censored for ileus outcomes. Other factors affecting postoperative bowel function, such as patient physical status prior to surgery, fluid-electrolyte management and use of antiemetics, were not evaluated. Finally, interpretation of results is based on statistical associations not ‘cause and effect’.
Our study is unique in that it assesses the relationship of opioid administration, MED, POI, LOS, hospital costs, and 30 day readmission rates in patients undergoing open and laparoscopic colectomy and open and laparoscopic cholecystectomy. Although most studies address daily MED, our report identifies the incidence of POI and the total cumulative postoperative median MED associated with ileus and the likelihood of its occurrence with that dosing. These findings add to the existing body of information available on colectomies and significantly contribute to the paucity of literature available for cholecystectomy.
Conclusion
In summary, use of opioids in patients who develop ileus following abdominal surgeries is associated with increased hospital stay, total hospital cost, and readmission rate. Open procedures of colectomy and cholecystectomy are associated with increased incidence of ileus, longer hospital stay, and greater requirements for pain management. Surgeries that directly manipulate the colon, regardless of surgical technique employed, require greater doses of opioids than cholecystectomy. The use of multimodal analgesic strategies may reduce opioid consumption and POI and other opioid-related adverse events. These strategies should improve healthcare outcomes and reduce the associated economic impact.
Transparency
Declaration of funding
This study was funded by Pacira. The potential publication of the results was not dependent upon approval or censorship from the sponsor.
Declaration of financial/other relationships
S.B.R. has disclosed that he is an employee of Premier Research Services, which received funding from Pacira Pharmaceuticals Inc. to conduct this analysis. T.J.G. and G.M.O. have disclosed that they received funding from Pacira Pharmaceuticals Inc. to conduct this analysis. J.P. and S.R. have disclosed that they have no significant relationships with or financial interests in any commercial companies related to this study or article. R.S. has disclosed that he is an employee of Pacira Pharmaceuticals Inc.
CMRO peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
References
- Chamberlain RS, Martindale RG. Evidence-based management of postoperative ileus. Issue 1: The role of the surgeons and the surgical care team: proactive strategies for preventing postoperative ileus. Available at: http://www.ce-university.org/surgery [Last accessed 1 October 2012]
- Litkouhi B. Postpoerative ileus. UpToDate. Available at: http://www.uptodate.com/contents/ postoperative-ileus [Last accessed 27 September 2012]
- Augestad KM, Delaney CP. Postoperative ileus: impact of pharmacological treatment, laparoscopic surgery and enhanced recovery pathways. World J Gastroenterol 2010;16:2067-74
- Erowele GI. Treatment options for postoperative ileus. US Pharmacist 2010;35:55-73
- Salvador CG, Sikirica M, Evans A, et al. Clinical and economic outcomes of prolonged postoperative ileus in patients undergoing hysterectomy and hemicolectomy. Pharm Therapeut 2005;30:590-5
- Johnson MD, Walsh RM. Current therapies to shorten postoperative ileus. Cleveland Clinic J Med 2009;76:641-8
- Doyle E. The search for a therapy to prevent and treat postoperative ileus. Available at: http://www.todayshospitalist.com/index.php?b=articles_read&cnt=227 [Last accessed 15 October 2012]
- Senagore, AJ. Pathogenesis and clinical and economic consequences of postoperative ileus. Am J Health Syst Pharm 2007;64(Suppl 13):S3-7
- Senagore, AJ. Pathogenesis and clinical and economic consequences of postoperative ileus. Clin Exp Gastroenterol 2010;3:87-9
- Holzer P. Treatment of opioid-induced gut dysfunction. Expert Opin Investig Drugs 2007;16:181-94
- Wheeler M, Oderda GM, Ashburn MA, Lipman AG. Adverse effects associated with postoperative opioid analgesia: a systematic review. J Pain 2002;3:159-80
- Oderda GM, Gan TJ, Johnson BH, Robinson SB. Effect of opioid-related adverse events on outcomes in selected surgical patients. J Pain Palliative Care Pharmacother 2013;27:62-70
- Mills JR, Robinson SB, Knudson R. Addressing the Need for Safe and Effective Postsurgical Pain Management: Survey Results from Hospital Pharmacy Practitioners. Premier Healthcare Alliance, Internal document, August 2012
- Ay AA, Kutun S, Ulucanlar H, et al. Risk factors for postoperative ileus. J Korean Surg Soc 2011;81:242-9
- Holte K, Kehlet H. Postoperative ileus. Progress towards effective management. Drug 2002;62:2603-15
- Bream-Rouwenhorst H, Cantrell MA. Alvimopan for postoperative ileus. Am J Health Syst Pharm 2009;66:1267-77
- Bashankaev B, Daniel M, Khaikin M, Wexner SD. Postoperative ileus: an algorithm for prevention and management. Pharmacy Practice News Special Edition 2009;30:71-8
- Lubawski J, Saclarides T. Postoperative ileus: strategies for reduction. Therapeut Clin Risk Manag 2008;4:913-17
- Chamberlain RS, Rathmell J. Evidence-based management of postoperative ileus. Issue 2, Preventing postoperative ileus: the use of epidural analgesia and opioid antagonists to ameliorate adverse effects. Available at: http://www.ce-university.org/surgery [Last accessed 1 October 2012]
- U.S. Department of Health and Human Services. Management of Cancer Pain: Adults. AHCPR Pub. No. 94-0593. Rockville, MD: Agency for Health Care Policy and Research, 1994
- Luckey A, Livingston E, Taché Y. Mechanism and treatment of postoperative ileus. Arch Surg 2003;138:206-14
- Viscusi ER, Gan TJ, Leslie JB, et al. Peripherally acting mu-opioid receptor antagonists and postoperative ileus: mechanisms of action and clinical applicability. Anesth Analg 2009;108:1811-22
- Iyer S, Saunders WB, Stemkowski S. Economic burden of postoperative ileus associated with colectomy in the United States. J Manag Care Pharm 2009;15:485-94
- Goldstein JL, Matuszewski KA, Delaney CP, et al. Inpatient economic burden of postoperative ileus associated with abdominal surgery in the United States. P&T 2007;32:82-90
- Garcia-Caballero M, Vara-Thorbeck C. The evolution of postoperative ileus after laparoscopic cholecystectomy. A comparative study with conventional cholecystectomy and sympathetic blockade treatment. Surg Endosc 1993;7:416-19
- Draganic BD, Reece-Smith H. Gallstone ileus without a gallbladder. Ann Roy Coll Surg Engl 1997;79:231-2
- Ivanov I, Beuran M, Venter MD, et al. Gallstone ileus after laparoscopic cholecystectomy. J Med Life 2012;15:335-41
- Pavoor R, Milsom J. Postoperative ileus after laparoscopic colectomy: elusive and expensive. Letter to the Editor. Ann Surg 2011;254:1057
- Cali RL, Meade PG, Swanson MS, Freeman C. Effect of morphine and incision length on bowel function after colectomy. Dis Colon Rectum 2000;43:163-8
- Goettsch WG, Sukel MP, van der Peet DL, et al. In-hospital use of opioids increases rate of coded postoperative paralytic ileus. Pharmacoepidemiol Drug Saf 2007;16:668-74
- Kodali B-S, Oberoi JS. Management of postoperative pain. UpToDate. Available at: http://www.uptodate.com/contents/management-of-postoperative-pain [Last accessed 27 September 2012]
- Barletta JF, Asgeirsson T, Senagore AJ. Influence of intravenous opioid dose on postoperative ileus. Ann Pharmacother 2011;45:916-23
- Kraft MD. Emerging pharmacologic options for treating postoperative ileus. Am J Health Syst Pharm 2007;64:S13-20
- Barzoi G, Carluccio S, Bianchi B, et al. Morphine plus bupivacaine vs morphine peridural analgesia in abdominal surgery: The effects of postoperative course in major hepatobiliary surgery. HPB Surgery 2000;11:393-9
- Kehlet H. Postoperative ileus. Gut 2000;47(Suppl IV):iv85-6