Abstract
Objective:
Diversion and abuse of prescription opioids are important public health concerns in the US. This study examined possible sources of prescription opioids among patients diagnosed with opioid abuse.
Methods:
Commercially insured patients aged 12–64 diagnosed with opioid abuse/dependence (‘abuse’) were identified in OptumHealth Reporting and Insights medical and pharmacy claims data, 2006–2012, and required to have continuous eligibility over an 18 month study period surrounding the first abuse diagnosis. We examined whether abusers had access to prescription opioids through their own prescriptions and/or to diverted prescription opioids through family members’ prescriptions obtained prior to the abuser’s first abuse diagnosis. For comparison, we examined access to prescription opioids of a reference population of non-abusers. Sensitivity analyses focused on patients initially diagnosed with opioid dependence and, separately, abusers not previously treated with buprenorphine.
Results:
Of the 9291 abusers meeting the selection criteria, 79.9% had an opioid prescription prior to their first abuse diagnosis; 20.1% of abusers did not have an opioid prescription prior to their first abuse diagnosis, of whom approximately half (50.8%) had a family member who had an opioid prescription prior to the abuser’s first abuse diagnosis (compared to 42.2% of non-abusers). Similar results were found among patients initially diagnosed with opioid dependence and among abusers not previously treated with buprenorphine.
Limitations:
The study relied on the accuracy of claims data to identify abusers, but opioid abuse is often undiagnosed. In addition, only prescription claims that were reimbursed by a health plan were included in the analysis.
Conclusions:
While most abusers had access to prescription opioids through their own prescriptions, many abusers without their own opioid prescriptions had access to prescription opioids through family members and may have obtained prescription opioids that way. Given the study design and data source, this is likely a conservative estimate of prescription opioid diversion.
Keywords: :
Introduction
In 2012, an estimated 4.9 million (1.9%) Americans aged 12 or older used prescription-type pain relievers non-medically (defined as use without a prescription of the individual’s own or simply for the feeling the drugs caused), and an estimated 2.1 million (0.8%) had pain reliever dependence or abuseCitation1. Diversion of prescription opioids is a widespread problem in the US. Diversion can occur at any point in the drug delivery process from the manufacturing site to the physician’s office, the retail pharmacy, or the patient, and common sources include doctor shopping, pill brokering, and siphoning from the family medicine chestCitation2,Citation3. The primary sources of prescription opioids on the street include the elderly, patients with pain, doctor shoppers, and pill brokers and dealersCitation4. According to the National Survey on Drug Use and Health (NSDUH), the most common sources of pain relievers among non-medical users were friends or relatives. Among persons aged 12 or older in 2011–2012 who used pain relievers non-medically in the past year, 54% obtained the pain relievers they most recently used from a friend or relativeCitation1. Many patients retain opioids after they cease taking the medications, sometimes accumulating large amounts of medications which may be diverted to othersCitation5. Diversion of prescription opioids may occur intentionally (e.g., sharing or selling of prescription medications) or without a patient’s knowledge (e.g., theft of prescription medications).
The objective of this study was to examine possible sources of prescription opioids among diagnosed opioid abusers. To date, studies examining diversion of prescription opioids have relied on self-reported data obtained through surveys of non-medical users of prescription opioids (some of whom may not necessarily be abusing opioids but rather may be self-medicating for pain without a doctor’s prescription) or drug-using street- and club-based populationsCitation1,Citation4. To our knowledge, this is the first broad, population-based research study examining possible sources of prescription opioids among diagnosed abusers using administrative claims data for a commercially insured population. While this analysis does not consider non-commercially-insured populations or undiagnosed opioid abusers, the advantage of using administrative claims data for this type of study is that the data do not rely on self-reporting. Rather, actual opioid abuse or dependence diagnoses as a result of interactions with medical service providers, as well as prescription claims for dispensed prescription opioids, can be observed.
Methods
This study built upon a recently published paper on the costs of opioid abuse from an employer perspectiveCitation6. Specifically, we used the same sample of patients, aged 12–64, diagnosed with opioid abuse or dependence (‘abusers’) as well as a sample of those not diagnosed with opioid abuse or dependence (‘non-abusers’) from the de-identified OptumHealth Reporting and Insights (OptumHealth) medical and pharmacy claims database, Q1 1999–Q1 2012. Patients were required to have continuous eligibility over an 18 month study period surrounding the first abuse diagnosis. Details of the study period and inclusion criteria are described in Rice et al.Citation6. To estimate the potential extent of diversion, we examined what share of abusers had access to prescription opioids through prescriptions they obtained prior to their index date, defined as the date of their first abuse diagnosis. Opioid prescriptions could have been filled at any point prior to the index date, potentially going back several years to as far back as Q1 1999 depending on the availability of prescription drug claims in the OptumHealth database for a given patient. Abusers without such access likely obtained opioids from other sources such as family members, friends, or illicit sources, although cash transactions that did not result in an insurance claim are also possible. It is possible that abusers with their own opioid prescriptions abused opioids obtained from other sources. Because we cannot observe which opioids were actually abused and the sources of those opioids, however, we assume that abusers would first abuse the prescription opioids readily available to them from their own prescriptions before turning to other sources. Among these abusers, we examined what share had a family member with an opioid prescription claim prior to the abuser’s index date. Family member linkage was identified using a unique employee identifier (a random, de-identified family key, or ‘family ID’) for each patient. Family members were defined as any individuals with the same family ID as the abuser. For comparison, we also examined what share of a reference population of non-abusers had access to prescription opioids (either through their own prescriptions or through family members’ prescriptions) prior to their index date, which was defined as the date of a random medical claim for any service since non-abusers did not have any abuse diagnoses by definition . Index dates were selected in the original Rice et al. study, which compared the health care costs of abusers and matched non-abusers during a 12 month observation period centered on the index date. Neither abusers nor non-abusers were required to have an opioid prescription claim to be included in the study. For abusers and family members who had an opioid prescription claim prior to the abuser’s index date, we further examined whether the prescription(s) were for an immediate-release/short-acting (IR/SA) opioid, an extended-release/long-acting (ER/LA) opioid, or both.
We also conducted two sensitivity analyses. First, we examined whether possible sources of prescription opioids differed for patients initially diagnosed with opioid dependence only (‘opioid-dependent patients’), defined as patients with a diagnosis for opioid dependence (International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis codes 304.0x and 304.7x) on their index date. Some of these patients may have had concurrent or subsequent diagnoses for opioid abuse. Second, we excluded patients with a buprenorphine claim prior to their index date, as it is possible that some of these patients were already being treated for opioid addiction or dependence. Buprenorphine is used most commonly in the treatment of opioid addiction and dependence, though it is also used in the treatment of chronic pain.
Results
Our analytic sample included 9291 abusers and 395,901 non-abusers. Of the abusers, 7422 (79.9%) had an opioid prescription claim prior to their index date, and the remaining 1869 (20.1%) did not (; , Column A). Approximately half (50.8%) of the abusers who did not have their own opioid prescription claim prior to their index date (950 out of 1869) had a family member who had an opioid prescription claim prior to that date, and the remainder (919 out of 1869) had neither their own opioid prescription claim prior to their index date nor a family member with an opioid prescription claim prior to that date.
Figure 1. Possible sources of prescription opioids among abusers. N = 9291. Abusers were defined as patients with a diagnosis for opioid abuse or dependence. Family members were identified as any individuals with the same family ID as the abuser. Some of the abusers with ≥1 prior claim for a prescription opioid (79.9%) also had family members with claims for a prescription opioid.
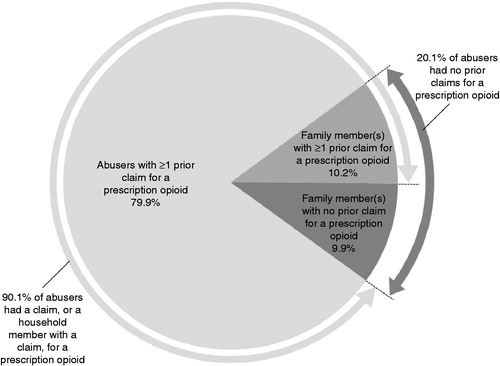
Table 1. Possible sources of prescription opioids among abusers, non-abusers, opioid-dependent patients, and abusers excluding those prescribed buprenorphine.
In contrast, among the reference population of non-abusers, the share of individuals with no claims for opioid prescriptions was larger. In particular, 225,032 (56.8%) non-abusers did not have an opioid prescription claim prior to their index date (, Column B). A relatively smaller share (42.2% vs. 50.8% above) of these patients (94,896 out of 225,032) had a family member with an opioid prescription claim prior to the non-abuser’s index date.
Among the abusers who did not have an opioid prescription claim prior to their index date but had a family member with an opioid prescription claim prior to that date, their family members predominantly had claims for IR/SA opioids only (91.2%), though some abusers’ family members had claims for both IR/SA and ER/LA opioids (8.4%), and a few abusers’ family members had claims for ER/LA opioids only (0.4%) (, Panel A). This distribution of prescription opioids is similar to the distribution of prescription opioids among a broader population. For example, among all opioid prescriptions claims in the OptumHealth database in 2012, 91.4% were for IR/SA opioids, and 8.6% were for ER/LA opioids (results available upon request).
Table 2. Types of prescription opioids obtained by individuals and their family member(s).
Among the 7422 (79.9%) abusers with an opioid prescription claim prior to their index date, most (66.5%) had prescriptions for IR/SA opioids only, though approximately one third (33.1%) had claims for both IR/SA and ER/LA opioids, and a small minority (0.4%) had claims for ER/LA opioids only (, Panel A).
In the first sensitivity analysis, we examined possible sources of prescription opioids among opioid-dependent patients. Of the 9291 abusers who met the initial selection criteria, 7141 (76.9%) had a diagnosis for opioid dependence on their index date. The sources of prescription opioids (, Column C) and types of prescription opioids (, Panel C) among these patients were consistent with the sources and types of prescription opioids among patients diagnosed with opioid abuse or dependence noted above. In the second sensitivity analysis, abusers who had buprenorphine claims prior to their index date were excluded, leaving a sample of 8546 abusers. The sources of prescription opioids (, Column D) and types of prescription opioids (, Panel D) among these patients were also similar to the sources and types of prescription opioids among the full sample of abusers noted above.
Discussion
While most (79.9%) abusers had access to prescription opioids through their own prescriptions, a considerable share (20.1%) of abusers in our sample did not have an opioid prescription claim at any point in their prescription claims history prior to their first abuse diagnosis, suggesting they obtained opioids through other means. Half of the abusers who did not have an opioid prescription claim prior to their index date potentially had access to prescription opioids through immediate family members enrolled in the same health plan. These results were largely unchanged when focusing on opioid-dependent patients or patients not previously treated with buprenorphine. This result is likely a lower-bound estimate of diversion of prescription opioids, as it is possible that some abusers used both prescribed and diverted opioids. The NSDUH reported that 54% of persons aged 12 or older in 2011–2012 who used pain relievers non-medically in the past year obtained the pain relievers they most recently used from a friend or relative for free, which further suggests that our estimate of 20.1% is a conservative estimateCitation1. Compared to the NSDUH, we focused on a narrower population (diagnosed opioid abusers in our analysis vs. non-medical users of prescription pain relievers in the NSDUH), included fewer sources of prescriptions (immediate family members enrolled in the same health plan vs. friends and family), and examined actual prescription claims in administrative data rather than self-reported survey results. In addition, we allowed for opioid prescription claims at any point prior to the index date, potentially going back several years. Had we looked only at prescription opioid claims in the year prior to the index date, there would be a greater share of patients without opioid prescriptions prior to the index date. Therefore, we consider our estimate to be a lower-bound estimate of potential diversion of prescription opioids from other sources. Among individuals who did not have access to prescription opioids themselves, abusers were more likely to have access to prescription opioids from family members than were non-abusers (50.8% vs. 42.2%). The fact that 42.2% of non-abusers without access to prescription opioids themselves potentially had access to prescription opioids from family members is likely attributable to the overall level of utilization of prescription opioids in the US. In addition, the possibility that some of those non-abusers may actually be undiagnosed abusers (as discussed in the limitations section below) could also be a contributing factor.
Our findings also suggest that while diversion of prescription opioids is a substantial problem, the overwhelming majority of diagnosed abusers (90.1%) potentially had access – directly or through family members sharing the same health insurance plan – to prescription opioids prescribed by health care professionals and reimbursed by insurance plans. This is consistent with the low share of non-medical users of pain relievers in the NSDUH who report obtaining pain relievers through illicit means, as noted in the limitations section below.
Our analysis of the types of opioids prescribed to abusers and their family members revealed that abusers and their family members filled different types of prescriptions. A sizeable share (33.1%) of abusers who had an opioid prescription claim prior to their index date had claims for both IR/SA and ER/LA opioids, while only 8.4% of family members who had an opioid prescription claim prior to the abuser’s index date had claims for both IR/SA and ER/LA opioids. Abusers may be more likely to combine both IR/SA and ER/LA opioids. A recent study found that patients prescribed ER/LA and IR/SA opioids concomitantly had a significantly higher risk of opioid overdose than patients prescribed ER/LA or IR/SA opioids aloneCitation7. We also found that 66.5% of abusers who had an opioid prescription claim prior to their index date had claims for IR/SA opioids only, while a much larger share (91.2%) of family members who had a claim prior to the abuser’s index date had claims for IR/SA opioids. This latter result is similar to the market share of IR/SA opioids mentioned above.
This study has several limitations. First, our analysis relies on the accuracy of claims data to identify abusers and opioid prescription claims. Opioid abuse is often undiagnosed. Recent research suggests that the ratio of undiagnosed opioid abuse to diagnosed opioid abuse is approximately 2:1 in a commercially insured populationCitation8. We are unable to identify undiagnosed abusers in this analysis. Our reference population of non-abusers may have captured some undiagnosed abusers. In addition, we are only able to identify prescription claims that were reimbursed by a health plan. Any prescriptions that were paid for by cash only would not be captured in our analysis.
Second, family members were defined as any individuals other than the abuser with the same family ID, but this approach may include family members who do not live in close proximity to the abuser (e.g. college-aged dependents living away from home), and it would exclude family members who are not enrolled in the same health plan, even if they live in close proximity to the abuser (e.g., Medicare-eligible parents). We were also unable to observe in the claims data whether abusers had access to opioids through friends or other sources. However, these other sources are less common. According to the NSDUH, 5.3% of non-medical users of pain relievers aged 12 or older in 2011–2012 obtained pain relievers from a drug dealer or other stranger, stole pain relievers from a physician’s office, clinic, hospital, or pharmacy, or bought pain relievers on the InternetCitation1.
In addition, while we were able to observe whether abusers had an opioid prescription claim prior to their index date, we were unable to definitively identify the specific opioid(s) that were abused. An abuser may have abused an opioid different from the one that was actually prescribed. We were also unable to observe the reason why an opioid was initially prescribed. Presumably, many of the abusers in our study were legitimate pain patients at the time they obtained their first prescription opioids. Finally, this study uses a commercial claims database in the US. Future research should examine the sources of prescription opioids among abusers in the US with other forms of health insurance (e.g., Medicare, Medicaid) or who are uninsured and, separately, the sources of prescription opioids among abusers in other countries.
Conclusion
This study finds that while many abusers had access to prescription opioids through their own prescriptions, approximately one in five diagnosed abusers had no evidence of ever filling an opioid prescription at any point in their prescription claims history prior to their index date, suggesting that they obtained their opioids from family members or through other means. Approximately half of the abusers who had no evidence of ever filling opioid prescriptions may have had access to prescription opioids through a family member enrolled in the same health plan. Abusers may also have had access to prescription opioids through extended family members, friends, or illicit means. Interventions such as patient and provider education, disposal of unused prescription medications, and routine monitoring may help identify potential abuse and diversion of prescription opioids.
Transparency
Declaration of funding
This study was funded by Purdue Pharma LP.
Declaration of financial/other relationships
A.S., J.B.R., N.Y.K., K.B. and H.G.B. have disclosed that they are employees of Analysis Group Inc., a company that received funding from Purdue Pharma LP to conduct this study. P.H. and R.B.-J. have disclosed that they are employees of Purdue Pharma LP.
CMRO peer reviewers on this manuscript have received an honorarium from CMRO for their review work. Peer reviewer 1 has disclosed that she/he has been a consultant to Inspirion, Mallinckrodt, Baxter, Purdue Pharma LLP, Grunenthal GmhB, Iroko, and Johnson and Johnson. Peer reviewer 2 has no relevant financial or other relationships to disclose.
Acknowledgments
The authors wish to acknowledge the assistance of Caroline J. Enloe in the preparation and submission of the manuscript. Ms. Enloe is an employee of Analysis Group Inc.
Notes
*For abusers, we examined what share had access to a prescription opioid (either through prescriptions obtained by themselves or their family members) prior to their index date, which was defined as the date of their first abuse diagnosis. Because non-abusers did not have an abuse diagnosis, by definition, their index date was defined as the date of a random medical claim for any service.
References
- Substance Abuse and Mental Health Services Administration, Results from the 2012 National Survey on Drug Use and Health: Summary of National Findings, NSDUH Series H-46, HHS Publication No. (SMA) 13-4795. Rockville, MD: Substance Abuse and Mental Health Services Administration, 2013. Available at: http://www.samhsa.gov/data/NSDUH/2012SummNatFindDetTables/NationalFindings/NSDUHresults2012.htm [Last accessed 11 March 2013]
- Green TC, Bowman SE, Ray M, et al. Collaboration or coercion? Partnering to divert prescription opioid medications. J Urban Health 2013;90:758-67
- Inciardi JA, Surratt HL, Kurtz SP, Cicero TJ. Mechanisms of prescription drug diversion among drug-involved club- and street-based populations. Pain Med 2007;8:171-83
- Inciardi JA, Surratt HL, Cicero TJ, Beard RA. Prescription opioid abuse and diversion in an urban community: the results of an ultrarapid assessment. Pain Med 2009;10:537-48
- Lewis ET, Cucciare MA, Trafton JA. What do patients do with unused opioid medications? Clin J Pain 2014;30:654-62
- Rice JB, Kirson NY, Shei A, et al. Estimating the costs of opioid abuse and dependence from an employer perspective: a retrospective analysis using administrative claims data. Appl Health Econ Health Policy 2014;12:435-46
- Coplan P, DeVeaugh-Geiss A, Kadakia A. Comparison of the risk of opioid overdose among patients prescribed immediate-release and extended-release opioid analgesics. Poster presentation at the American Pain Society 33rd Annual Scientific Meeting, 30 April–3 May 2014, Tampa, FL, USA
- Shei A, Rice B, Kirson NY, et al. Methods to estimate the prevalence and healthcare costs of undiagnosed opioid abuse among commercially-insured individuals. Poster presentation at the PAINWeek Conference, 2–6 September 2014, Las Vegas, NV, USA
