Dear Editor
The editorial by Maes et al. Citation[1], in which the authors outline an algorithm to diagnose myalgic encephalomyelitis (ME), chronic fatigue syndrome (CFS) and chronic fatigue (CF), is of great relevance. As the authors stipulate, an accurate definition and diagnosis of ME, CFS and CF is crucial. However, two pivotal points of criticism are imperative in this context: the algorithm proposed Citation[1] will leave out all patients fulfilling characteristic criteria for ME, who do not qualify themselves as “fatigued” Citation[2], and, not only as a logical consequence of this, ME is not part of a “chronic fatigue spectrum”.
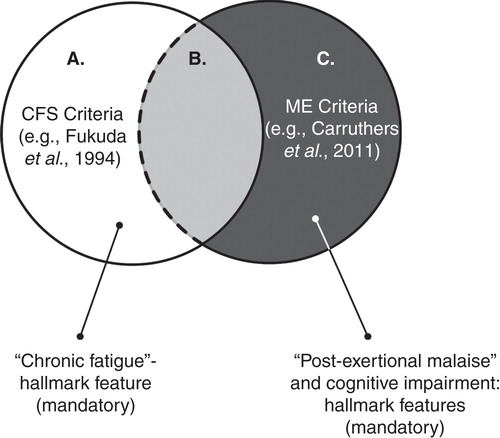
The authors wrongfully state that CFS has been considered a synonym for ME by the World Health Organization since 1969. ME has been described under various terms, e.g., atypical poliomyelitis and epidemic neuromyasthenia, since 1934. Crucial features of ME, as defined by Ramsay and colleagues, were muscle weakness, cognitive deficits, autonomic symptoms and post-exertional malaise: a long-lasting increase in the symptoms after a minor exertion Citation[3]. In 1969, ME was acknowledged by the WHO as a neurological disorder (ICD-8). In 1988 the label CFS and its definition were introduced by Holmes et al. and in 1994 the commonly used Fukuda et al. criteria were published. The feature distinguishing of CFS is “chronic fatigue”. Strangely enough, CFS excludes “chronic fatigue” that is medically explained. Although the WHO considers ME and CFS to be exchangeable since 1994 (ICD-10), the criteria for ME and CFS define two distinctive disorders () Citation[3].
It is estimated 40 – 60% of the patients fulfilling the fatigue-based Fukuda criteria for CFS also meet the diagnostic criteria for ME, primarily defined by flu-like symptoms, post-exertional malaise and cognitive impairment () Citation[3]. However, since the diagnosis of ME does not require “fatigue” Citation[3,4], the CFS criteria leave out an unknown number of patients with ME (). This means that the algorithm proposed by Maes et al. Citation[1], which employs the Fukuda et al.'s CFS criteria as a starting point, is not correct. As the authors of the criteria for ME Citation[4] point out: “fatigue” has been the most confusing and misused criterion. So, pattern recognition methods should be applied to all patients with a potential diagnosis of ME, according to consensus criteria Citation[4], and/or CFS, according to the Fukuda criteria Citation[1], not just to people with “chronic fatigue” Citation[1]. Pattern recognition methods applied to the ME and/or CFS patient populations will not only confirm/reject the validity of the ME criteria Citation[4], but will most likely also unravel clinical and biological subgroups of ME and CFS, which are the key to more effective research and therapies.
The hypothesis that ME is part of a “chronic fatigue spectrum” Citation[1] is invalid. Most importantly, as explained above, “fatigue” is not mandatory for the diagnosis of ME. Moreover, the only data substantiating a “continuum” is the overall severity of the illnesses, not “fatigue” Citation[3], both of which are subjective in nature. As a recent study confirms the CFS criteria, including fatigue, are poorly associated with disability and other symptoms. If there is to be a “spectrum” at all, it would be based on “severity”, not on “fatigue”.
As the authors themselves acknowledge, post-exertional malaise is the symptom which is highly distinctive for ME. Thus, “ME and CFS are qualitatively distinct categories that should be differentiated from each other based on post-exertional malaise and other symptoms” Citation[1]. Research and diagnosis based on ambiguous “chronic fatigue” criterion has shown to be not very effective for ME and CFS. Statistical analyses should be applied to objective measures, e.g., results of exercise tests–retests Citation[5], since subjective measures, e.g., “fatigue” Citation[2] and self-rated post-exertional malaise, are inadequate for an accurate diagnosis.
Lumping distinctive diseases together based on a “chronic fatigue continuum” as proposed will obfuscate research and evidence-based practice. But most importantly, it will leave out many patients with ME Citation[4].
Declaration of interest
The authors state no conflict of interest and have received no payment in preparation of this manuscript.
Declaration of interest
FNM Twisk was originally involved in the editorial “Diagnosis of Myalgic Encephalomyelitis: where are we now?”, but withdrew as a potential co-author due to differences of opinion relating to the content at the initial stage.
Bibliography
- Maes M, Anderson G, Morris G, Berk M. Diagnosis of myalgic encephalomyelitis: where are we now? Expert Opin Med Diagn 2013; doi:10.1517/17530059.2013.776039
- Jason LA, Evans M, Brown M, et al. Fatigue scales and chronic fatigue syndrome: issues of sensitivity and specificity. Disabil Stud Q 2011;31(1):pii, 1375
- Maes M, Twisk FNM, Johnson C. Myalgic encephalomyelitis (ME), chronic fatigue syndrome (CFS), and chronic fatigue (CF) are distinguished accurately: results of supervised learning techniques applied on clinical and inflammatory data. Psychiatry Res 2012;200(2-3):754-60
- Carruthers BM, van de Sande MI, de Meirleir KL, et al. Myalgic encephalomyelitis: international consensus criteria. J Intern Med 2011;270(4):327-38
- Twisk FNM, Maes M. A review on cognitive behavioral therapy (CBT) and graded exercise therapy (GET) in myalgic encephalomyelitis (ME)/chronic fatigue syndrome (CFS): CBT/GET is not only ineffective and not evidence-based, but also potentially harmful for many patients. Neuro Endocrinol Lett 2009;30(3):284-99
Michael Maes†1 MD PhD & George Anderson2
† Author for correspondence
1Chulalongkorn University, Department of Psychiatry, Bangkok, Thailand [email protected]
2CRC, Rm 30, Glasgow, Scotland
Author's response
Dear Editor
We read the comment by Twisk et al. with interest, and agree that the application of pattern recognition methods are important in defining clinically and biologically based classification. Case definitions should be based on appropriate statistical analyses rather than consensus declarations.
Two major perspectives on myalgic encephalomyelitis (ME)/chronic fatigue syndrome (ME/CFS) diagnosis prevail. The first by the Centers for Disease Control and Prevention (CDC) emphasizes chronic fatigue (CF) Citation[1], creating an umbrella term comprising different CF patient categories Citation[2]. The second view is that there is one homogeneous diagnostic category that does not require the presence of CF, i.e., ME according to the International Consensus Criteria (ICC) Citation[3]. Twisk et al. consider the ICC criteria as the gold standard and CF to be an “ambiguous criterion”.
However, previous diagnostic criteria, including the CDC and ICC, were based on consensus or clinical views and did not pass external statistical validation. Thus, their arguments favouring ICC criteria fail to satisfy the stated criterion of statistical validation. Moreover, the multi-symptom ICC requirements may select for the existing diagnosis of “somatization” (disorder), rather than demarcating a new diagnosis of “ME”. Their view that ME cannot belong to a CF spectrum is driven by their perspective that ME is a homogeneous disorder. First, there is no statistical evidence that ICC criteria-defined ME exists or indeed would differ from somatization. Second, Maes' criteria ME belong to a CF spectrum wherein some symptoms (including post-exertional malaise and inflammatory symptoms) assemble to form a distinct category Citation[2]. Both CFS and ME, as Maes' criteria defined, are complex disorders accompanied by shared neuro-immune disturbances that are more expressed in ME than in CFS. This reflects current evidence showing both qualitative and quantitative clinical and biological differences between CFS and ME, indicative of a categorical CF continuum Citation[2].
Twisk et al. did not consider the complexity of the CF spectrum in relation to comorbid disorders, including depression and somatization Citation[4]. Similar physio-somatic symptoms are key components of these disorders and are associated with neuro-immune disturbances. Therefore, as we already proposed, future research focusing on neuro-immune biomarkers in larger data sets of patients with physio-somatic symptoms (including CF, CFS, ME, depression and somatization) will better delineate new classification rules Citation[4]. Until such time, Maes' criteria give a logical and clear framework with which to define patient presentations.
Bibliography
- Fukuda K, Straus SE, Hickie I, et al. The chronic fatigue syndrome: a comprehensive approach to its definition and study. Ann Intern Med 1994;121(12):953
- Maes M, Twisk FN, Johnson C. Myalgic Encephalomyelitis (ME), Chronic Fatigue Syndrome (CFS), and Chronic Fatigue (CF) are distinguished accurately: results of supervised learning techniques applied on clinical and inflammatory data. Psychiatry Res 2012;200(2-3):754-60
- Carruthers BM, van de Sande MI, De Meirleir KL, et al. Myalgic encephalomyelitis: international Consensus Criteria. J Intern Med 2011;270(4):327-38
- Anderson G, Maes M, Berk M. Biological underpinnings of the commonalities in depression, somatization, and Chronic Fatigue Syndrome. Med Hypotheses 2012;78(6):752-6