Stroke is the third leading cause of death in the general population after coronary heart disease (CHD) and cancer and it is also the first leading cause of disability in adults Citation[1]. Approximately 550,000 new patients eventually develop stroke every year Citation[1]. From 1950, the stroke mortality rate has shown a clear trend to decrease in the USA (although a slight upturn in the stroke mortality rate has been observed since 1990 Citation[1]).
The reduction in mortality from stroke may be due to the decreased incidence of stroke overall and/or an improved survival after the first stroke occurrence. The declining incidence of stroke supports the hypothesis that aggressive management of cardiovascular (CV) risk factors is effective for its prevention Citation[2,3]. Among modifiable traditional CV risk factors, hypertension is the leading cause of stroke and its treatment reduces morbidity and mortality from stroke by approximately 38% Citation[4,5].
Blood pressure reduction & protection from stroke
A small reduction in blood pressure (BP) results in a substantial reduction in both ischemic and hemorrhagic strokes Citation[4]. In a recent metaregression analysis of 28 major trials in hypertensive or high-risk patients Citation[6], BP-lowering was the major determinant in stroke prevention. A mean BP fall of 10 mmHg was associated with a decrease of approximately 25% in the incidence of stroke.
It is generally believed that any of the commonly used antihypertensive drugs are effective in lowering the incidence of stroke, with larger reductions in BP resulting in larger risk reductions Citation[2,3].
Renin–angiotensin system & stroke
Experimental evidence has linked the renin–angiotensin system (RAS) to the development and progression of cerebrovascular disease, and experimental data suggest that blockade of RAS could exert a specific cerebrovascular protective effect. Angiotensin-converting enzyme inhibitors (ACEIs) and angiotensin receptor blockers (ARBs) may delay the development of atherosclerosis and increase plaque stability. ACEIs may shift the fibrinolytic balance from coagulation to lysis by reducing the angiotensin II-dependent production and secretion of plasminogen activator/inhibitor Citation[7–9]. There is also evidence that the neurological outcome following induction of cerebral ischemia in rats is improved by intracerebral administration of low doses of irbesartan, and that such an effect is prevented by the coadministration of an ARB Citation[10,11]. In rats injured by cerebral artery occlusion and pretreated with candesartan or ramipril at subhypotensive doses, the infarct size was reduced by ARBs, and not by ACEIs Citation[12]. In addition, the neurological damage induced by cerebral ischemia, as well as the reduction in blood flow around the necrotic area, was more severe in angiotensin (AT)2 receptor-deleted mice than in control mice Citation[13]. Thus, experimental studies support the hypothesis that ARBs are more stroke protective than ACEIs.
Angiotensin receptor blockers & stroke
In hypertensive patients with left ventricular hypertrophy included in the Losartan Intervention for End Point Reduction in Hypertension (LIFE) study, a therapeutic strategy based on losartan Citation[14] was more effective than a strategy based on atenolol for prevention of stroke. However, it could be argued that the difference in stroke rate between the two groups was accounted for, at least in part, by the slightly lower (by 2.2 mmHg) BP in the losartan group than in the atenolol group during follow-up.
As far as the secondary prevention of stroke is concerned, the Perindopril Protection Against Recurrent Stroke Study (PROGRESS) trial compared the effect of an active treatment (based on ACEI with or without the combination of a diuretic) versus placebo Citation[15]. Overall, the results confirmed the central role of BP reduction for stroke prevention: systolic BP fell by 5 and 12 mmHg in the perindopril and perindopril plus indapamide strata, respectively, but the reduction in the risk of stroke was significant only in the latter group.
The Morbidity and Mortality after Stroke, Eprosartan Compared with Nitrendipine for Secondary Prevention (MOSES) study conducted in hypertensive patients, who experienced previous stroke, showed a superiority of eprosartan over nitrendipine for prevention of composite end point of cerebrovascular and cardiovascular events plus noncardiovascular death Citation[16]. However, the incidence of first-occurring cerebrovascular events did not differ between the two groups (p = 0.32). Notably, systolic BP was reduced from 150.7 to 137.5 mmHg in the eprosartan arm, and from 152.0 to 136.0 mmHg with the nitrendipine-based regimen (a reduction of approximately 2.9 mmHg in favor of eprosartan).
The Jikei Heart Study (Valsartan in a Japanese population with hypertension and other cardiovascular disease) showed that the addition of an ARB to conventional CV treatment in Asian patients with CV disease was associated with a significant reduction in stroke or transient ischemic attacks despite comparable BP-lowering effects in the two arms Citation[17].
Are angiotensin receptor blockers better than ACEIs?
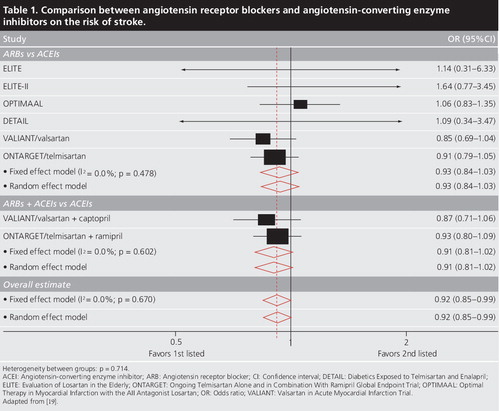
The recent publication of the results of the Ongoing Telmisartan Alone and in Combination with Ramipril Global Endpoint Trial (ONTARGET), a large trial consisting of patients with high CV risk with or without hypertension randomized to an ARB (telmisartan) or an ACEI (ramipril) Citation[18], prompted us to plan a systematic overview of all the outcome trials of both classes of drugs Citation[19].
According to preplanned selection criteria, we selected six trials with a total of 31,632 patients randomized to ARBs and 18,292 patients randomized to ACEIs. Patients enrolled in these trials showed a generally high prevalence of congestive heart failure (CHF), previous myocardial infarction (MI) and/or other conditions defining an increased CV risk.
The odds ratios and 95% confidence intervals for stroke, MI, CV mortality and total mortality were computed for each trial according to fixed- and random-effect models. Preplanned subgroup analyses were also performed, including the comparison of ARBs versus ACEIs as well as ARBs plus ACEIs versus ACEIs.
In the ARB group, there were 2857 MI events, 1273 strokes, 3534 CV deaths and 4776 all-cause deaths. The corresponding number of events for the ACEI group were 1628, 768, 2622 and 2707, respectively. In the overall pooled estimate, the risk of stroke was 8% lower with ARBs than with ACEIs (odds ratio: 0.92; 95% confidence interval: 0.85–0.99, both in a fixed-effect and a random-effect model; p = 0.036) . In a preplanned separate subgroup analysis of ARBs versus ACEIs and ARBs plus ACEIs versus ACEIs, the lesser stroke risk with ARBs did not achieve statistical significance, although the subgroup estimates were consistent and without significance between group heterogeneity (p = 0.714) . No statistical differences in the prevention of MI, CV mortality and all-cause mortality were observed between patients randomized to ARBs, ACEIs or ARBs plus ACEIs.
It is interesting to remark that the overall estimate for the risk of MI between ARBs and ACE–Is was not dissimilar from unity, the odds ratio being 1.01, with the 95% confidence interval being 0.95–1.07 for both the fixed- and random-effect models (p = 0.747). These results put at rest the hypothesis that ARBs could be associated with an excess risk of MI Citation[20].
Overall, these findings indicate that ARBs and ACEIs provide a comparable protective effect on MI, fatal CV events and all-cause mortality. However, the blockade of AT1 receptors resulted in a slightly superior protection from stroke when compared with ACE inhibition Citation[19].
Conclusion
Treatment of hypertension effectively reduces the risk of fatal and nonfatal stroke. Available data support the concept that BP reduction is the leading mechanism for protection from stroke, and that all available antihypertensive drugs are suitable to reach this goal. New evidence suggests that, where the blockade of RAS may be recommended, such as in patients with established CHF or who have experienced prior CV events, a treatment based on ARBs, alone or combined with ACEIs, is slightly more effective than a treatment based on ACEIs alone. This favors the use of ARBs over ACEIs when the risk of stroke is expected to be predominant, such as in patients with a history of cerebrovascular events Citation[21] or in patients of Asian ethnicity Citation[22].
Financial & competing interests disclosure
We gratefully thank the Fondazione Umbra Cuore e Ipertensione (AUCI–ONLUS Foundation) for financial support. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
No writing assistance was utilized in the production of this manuscript.
References
- Carandang R, Seshadri S, Beiser A et al. Trends in incidence, lifetime risk, severity, and 30-day mortality of stroke over the past 50 years. JAMA296, 2939–2946 (2006).
- MacMahon S, Peto R, Cutler J et al. Blood pressure, stroke and coronary heart disease: part 1, prolonged differences in blood pressure: prospective observational studies corrected for the regression dilution bias. Lancet335, 765–774 (1990).
- Collins R, Peto R, MacMahon S et al. Blood pressure, stroke, and coronary heart disease: part 2, short-term reductions in blood pressure: overview of randomised drug trials in their epidemiological context. Lancet335, 827–838 (1990).
- Moser M, Hebert PR. Prevention of disease progression, left ventricular hypertrophy and congestive heart failure in hypertension treatment trials. J. Am. Coll. Cardiol.27, 1214–1218 (1996).
- Moser M. Update on the management of hypertension: recent clinical trials and the JNC 7. J. Clin. Hypertens. (Greenwich)6(Suppl. 2), 4–13 (2004).
- Verdecchia P, Reboldi G, Angeli F et al. Angiotensin-converting enzyme inhibitors and calcium channel blockers for coronary heart disease and stroke prevention. Hypertension46, 386–392 (2005).
- Jilma B, Li-Saw-Hee FL, Wagner OF, Beevers DG, Lip GY. Effects of enalapril and losartan on circulating adhesion molecules and monocyte chemotactic protein-1. Clin. Sci. (Lond).103, 131–136 (2002).
- Gasic S, Wagner OF, Fasching P et al. Fosinopril decreases levels of soluble vascular cell adhesion molecule-1 in borderline hypertensive Type II diabetic patients with microalbuminuria. Am. J. Hypertens.12, 217–222 (1999).
- Hlubocka Z, Umnerova V, Heller S et al. Circulating intercellular cell adhesion molecule-1, endothelin-1 and von Willebrand factor – markers of endothelial dysfunction in uncomplicated essential hypertension: the effect of treatment with ACE inhibitors. J. Hum. Hypertens.16, 557–562 (2002).
- Li J, Culman J, Hortnagl H et al. Angiotensin AT2 receptor protects against cerebral ischemia-induced neuronal injury. FASEB J.19, 617–619 (2005).
- Iwai M, Liu HW, Chen R et al. Possible inhibition of focal cerebral ischemia by angiotensin II Type 2 receptor stimulation. Circulation110, 843–848 (2004).
- Krikov M, Thone-Reineke C, Muller S, Villringer A, Unger T. Candesartan but not ramipril pretreatment improves outcome after stroke and stimulates neurotrophin BNDF/TrkB system in rats. J. Hypertens.26, 544–552 (2008).
- Dai W, Funk A, Herdegen T, Unger T, Culman J. Blockade of central angiotensin AT1 receptors improves neurological outcome and reduces expression of AP-1 transcription factors after focal brain ischemia in rats. Stroke30, 2391–2399 (1999).
- Dahlof B, Devereux RB, Kjeldsen SE et al.; LIFE Study Group. Cardiovascular morbidity and mortality in the Losartan Intervention for Endpoint Reduction in Hypertension study (LIFE): a randomised trial against atenolol. Lancet359, 995–1003 (2002).
- PROGRESS Collaborative Group. Randomised trial of a perindopril based blood pressure lowering regimen among 6105 individuals with prior stroke or transient ischaemic attack. Lancet358, 1033–1041 (2001).
- Schrader J, Luders S, Kulschewski A et al.; MOSES Study Group. Morbidity and Mortality after Stroke, Eprosartan Compared with Nitrendipine for Secondary Prevention. Principal results of a prospective randomized controlled study (MOSES). Stroke36, 1218–1226 (2005).
- Mochizuki S, Dahlöf B, Shimizu M et al.; Jikei Heart Study group. Valsartan in a Japanese population with hypertension and other cardiovascular disease (Jikei Heart Study): a randomised, open-label, blinded endpoint morbidity-mortality study. Lancet369, 1431–1439 (2007).
- The ONTARGET Investigators. Telmisartan, ramipril, or both in patients at high risk for vascular events. N. Engl. J. Med.358, 1547–1559 (2008).
- Reboldi G, Angeli F, Cavallini C, Gentile G, Mancia G, Verdecchia P. Comparison between angiotensin-converting enzyme inhibitors and angiotensin receptor blockers on the risk of myocardial infarction, stroke and death: a meta-analysis. J. Hypertens.26, 1282–1289 (2008).
- Verma S, Strauss M. Angiotensin receptor blocker and myocardial infarction. BMJ329, 1248–1249 (2004).
- Vickrey BG, Rector TS, Wickstrom SL et al. Occurrence of secondary ischemic events among persons with atherosclerotic vascular disease. Stroke33, 901–906 (2002).
- Zhou M, Offer A, Yang G et al. Body mass index, blood pressure, and mortality from stroke: a nationally representative prospective study of 212,000 Chinese men. Stroke39, 753–759 (2008).