Dermoscopy is a noninvasive diagnostic technique for the in vivo observation of pigmented skin lesions. It has been shown that the use of this technique improves the diagnostic accuracy of pigmented skin lesions when compared with clinical examination. One of the most important applications of dermoscopy is for the early diagnosis of melanoma (melanocytic lesion), which can occasionally resemble other nonmelanocytic lesions, such as seborrheic keratosis, basal cell carcinoma and vascular lesions. At present, dermoscopy is performed using a two-step procedure. The first step is to differentiate between melanocytic and nonmelanocytic lesions and the second is to differentiate benign melanocytic lesions from melanoma.
Differentiation between melanocytic & nonmelanocytic skin lesions
Dermoscopy allows the better visualization of anatomic structures of the epidermis, dermoepidermal junction and superficial papillary dermis, eliminating the surface reflection of the stratum corneum and rendering it translucent by different methods (e.g., oil and incident light magnification, polarized light and computerized systems). It is a link between macroscopic clinical dermatology and microscopic dermatopathology. This tool provides us with new morphological criteria for the differentiation of melanoma from other melanocytic and nonmelanocytic pigmented skin lesions Citation[1–6]. It has been shown that the use of this technique improves the diagnostic accuracy of pigmented skin lesions when compared with clinical examination Citation[7,8]. One of the most important applications of dermoscopy is for the early diagnosis of melanoma (melanocytic lesion), which can occasionally look similar to other nonmelanocytic lesions, such as seborrheic keratosis, basal cell carcinoma and vascular lesions.
Following the Consensus Net Meeting on Dermoscopy in July, 2000, dermoscopy is performed using a two-step procedure. The first step is to differentiate between melanocytic and nonmelanocytic lesions and the second is to differentiate benign melanocytic lesions from melanoma Citation[9]. In order to perform this diagnosis, we need to know the different criteria for both melanocytic and nonmelanocytic lesions. Only then can we read the pigmented skin lesions with the dermoscope.
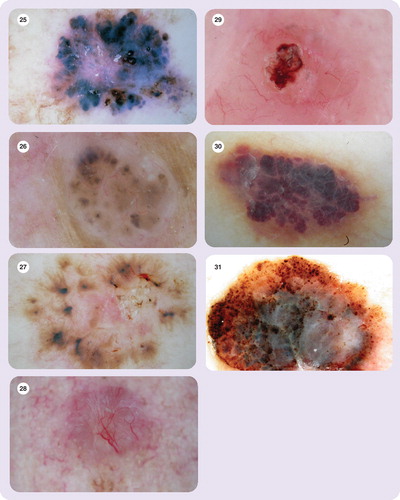
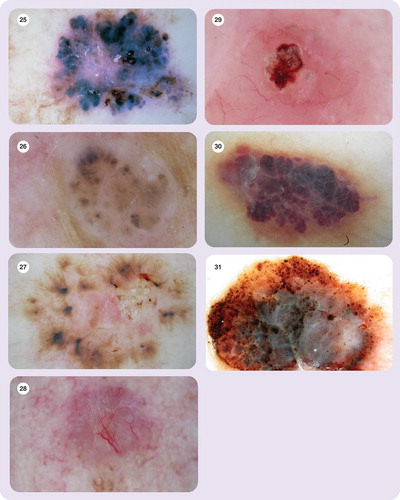
Main criteria for melanocytic lesions
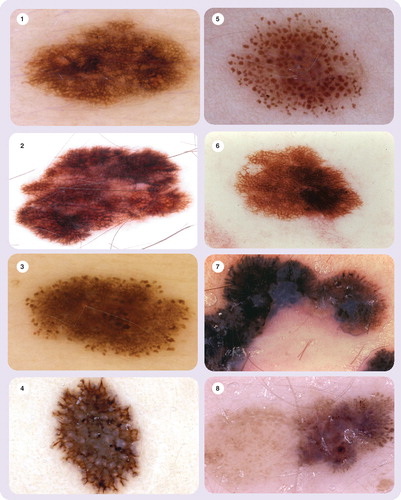
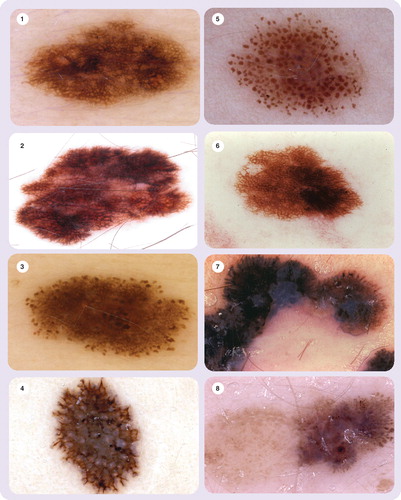
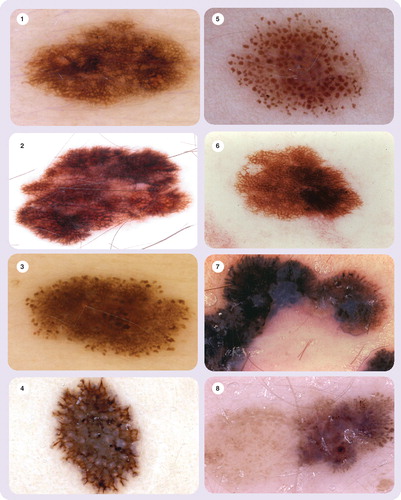
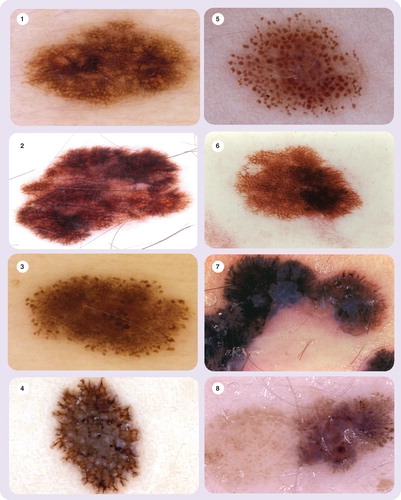
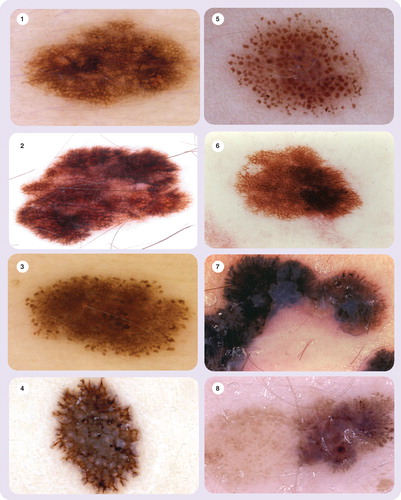
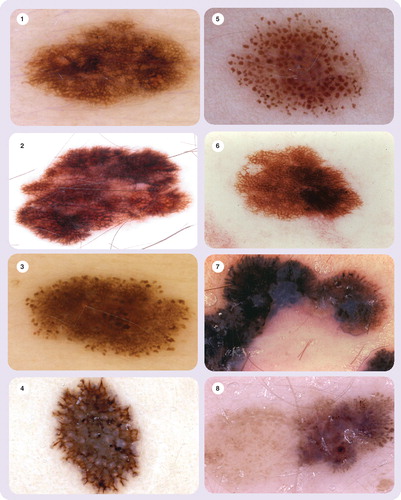
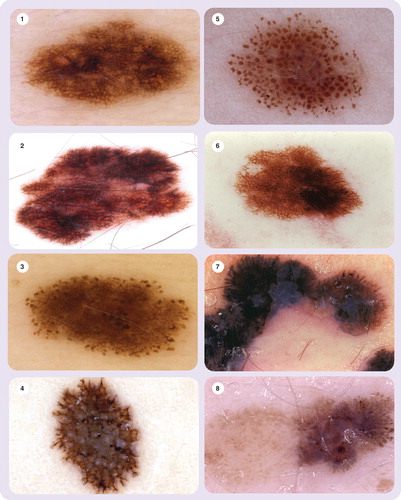
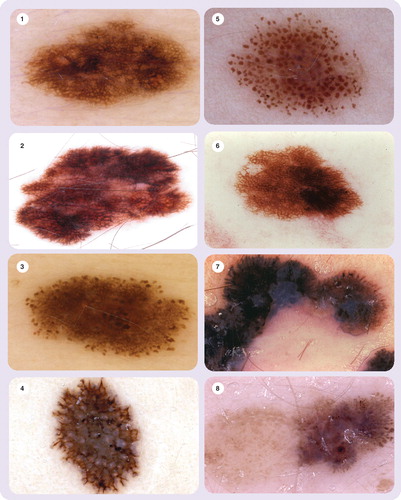
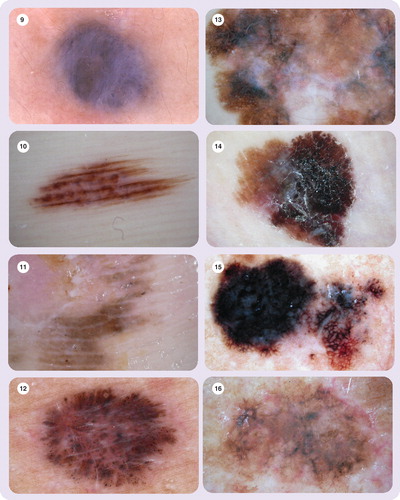
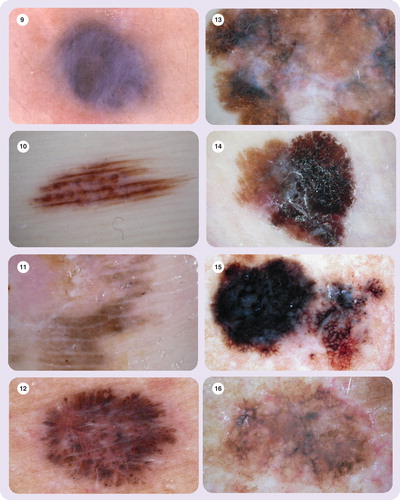
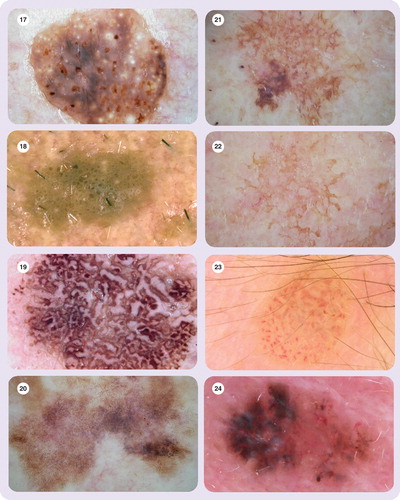
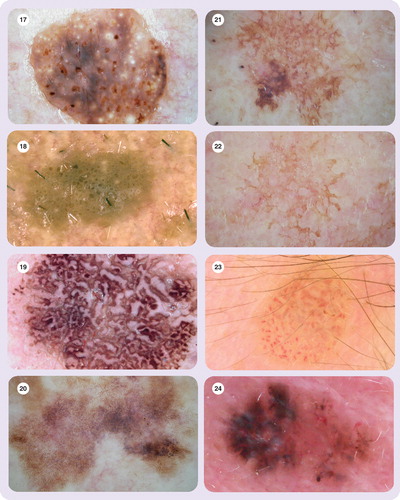
The pigment network presents a grid-like appearance and consists of pigmented lines and hypopigmented holes. It represents the rete ridge pattern of the epidermis .
Aggregated globules are symmetrical, round and well-demarcated structures. They can be brown, black or red in color, and are usually larger than 0.1 mm .
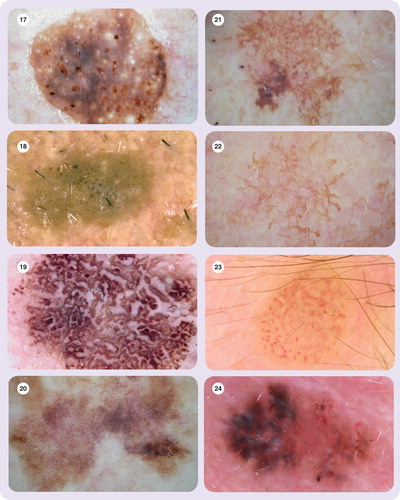
Streaks are the expression of an altered network that becomes broken up. They are characterized by radial streaming and pseudopods.
Radial streaming refers to linear radial extensions of pigment than can appear at the periphery of a lesion.
Pseudopods are finger-like projections than can sometimes be seen at the periphery of the lesion into the normal skin .
Homogeneous blue pigmentation is present in some melanocytic lesions. They present blue-gray areas without structural components and there are pigmented cells in the dermis .
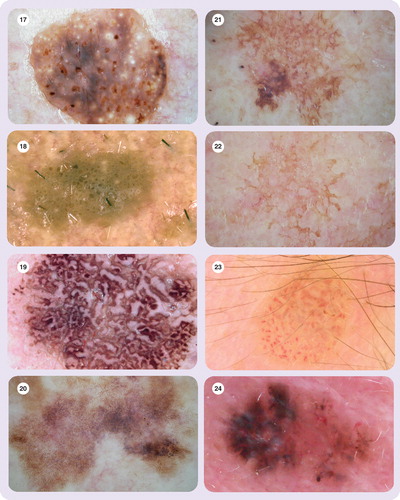
The parallel pattern criterion corresponds to acral melanocytic lesions. In this case, the pigmentation can follow the furrow or the ridge .
In benign melanocytic lesions, the pigmented cells cluster around the crista limitans pigmenting the furrow of the skin; while in melanoma, the pigmented cells cluster around the crista intermedia pigmenting the ridge. At present, the reason why this occurs remains unknown.
Further minor criteria that can be seen in melanocytic lesions
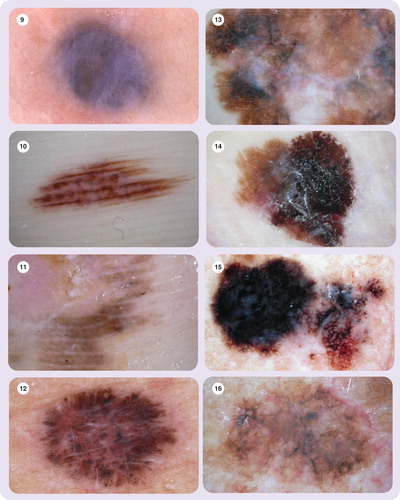
Dots are small, round structures (<0.1 mm). Their color can be black, brown, red or blue-gray, depending on the location of pigment accumulation .
Regression structures are white scar-like or blue-gray areas. Clinically, they correspond to a flat part of the lesion. The histopathological correlation of white areas is fibrosis, while for blue areas it is melanosis .
The blue-whitish veil is an irregular, structureless area of a confluent blue pigmentation with an overlying white ground-glass film. Clinically, it corresponds to an elevated part of the lesion .
Blotches are pigmented areas that can be localized or diffuse, and whose color can range from black to brown or gray .
Hypopigmentation can be areas with decreased pigmentation, which may be either diffuse or localized, focal or multifocal .
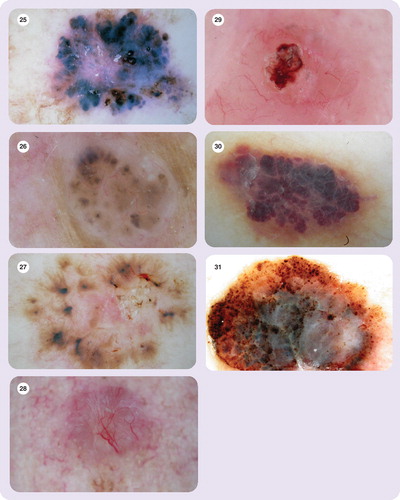
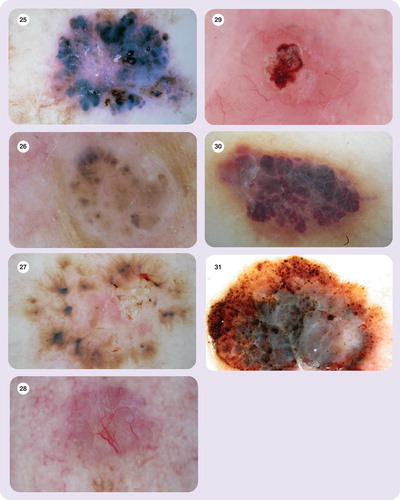
Criteria for seborrheic keratosis
Having discarded a melanocytic lesion, we need to determine whether or not it is a nonmelanocytic lesion, such as seborrheic keratosis, basal cell carcinoma or vascular lesion.
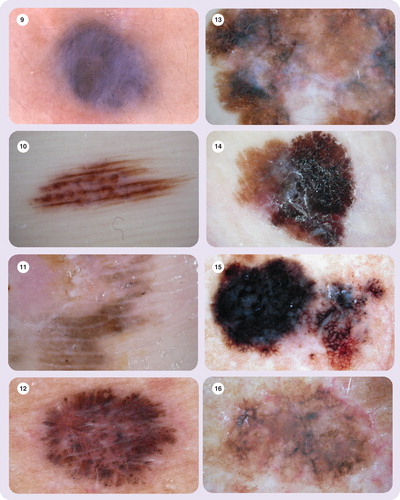
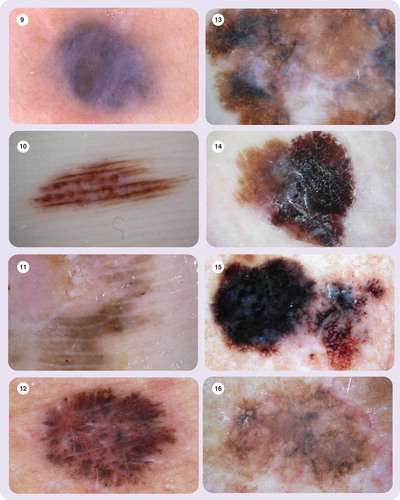
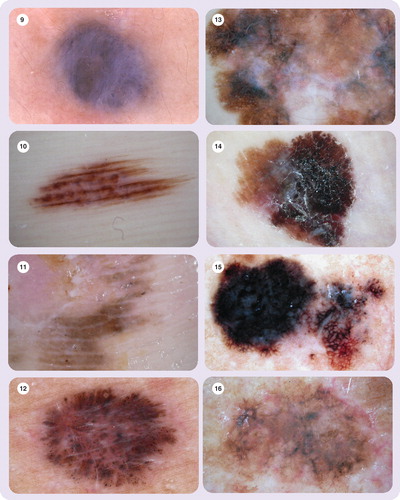
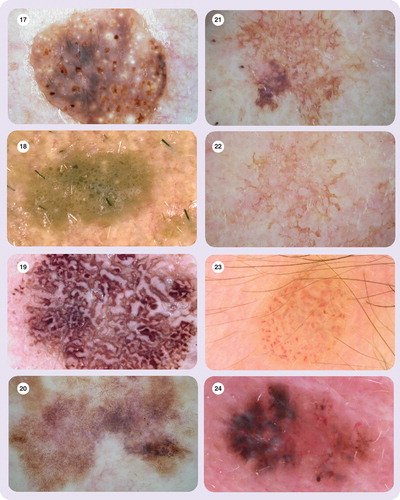
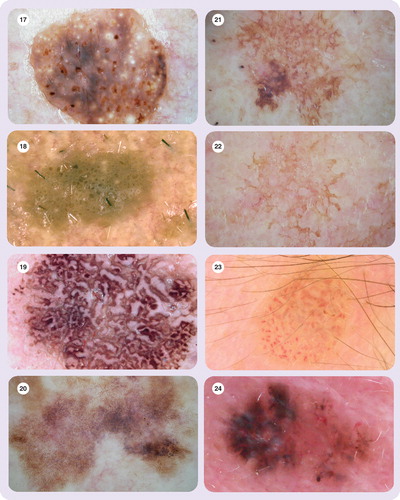
Multiple milia-like cysts are circular whitish-yellow areas. In larger seborrheic keratosisseborrheic keratosis, they show no typical circular shape . They are small in size (0.1–1 mm) and show no communication with the skin surface.
Comedo-like openings (irregular crypts) are small, circular, poro-like pseudo-follicular openings that communicate with the surface of the skin. They can be yellow, light brown, dark brown or black . Irregular crypts are large and irregular comedo-like openings that can be seen in large seborrheic keratosis.
Fissures/ridges (brain-like appearence) are size and shape variants of comedo-like openings .
Light brown fingerprint-like structures are tiny ridges running in parallel. They can usually be found at the periphery of the lesions in flat seborrheic keratosis (senile lentigines) .
Moth-eaten border is a concave border in which the pigment ends with a curved structure. This is known as Menzies’ sign and can usually be found in flat seborrheic keratosis . When this jelly-like border (jelly sign) is present, the pigment appears to be on the skin surface, with the appearance of a jelly spread onto the skin. It is usually found in flat seborrheic keratosis .
The typical vascular pattern is hairpin vessels .
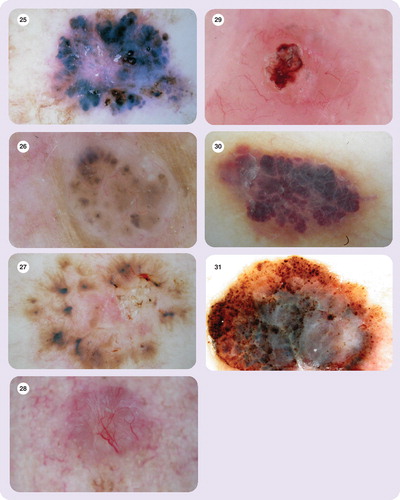
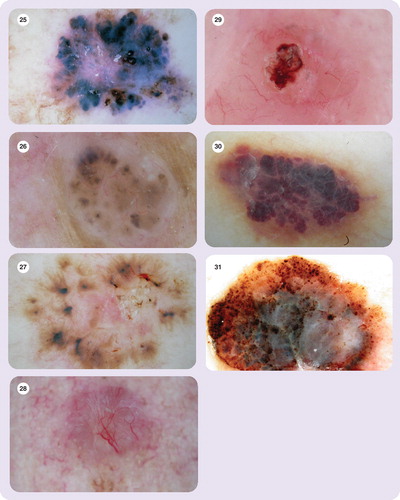
Criteria for basal cell carcinoma
Once all these criteria have been investigated and none are present, a case of seborrheic keratosis can be discarded.
We now need to confirm that we are not in the presence of a basal cell carcinoma. In this case, we need to know and check the criteria for this particular lesion.
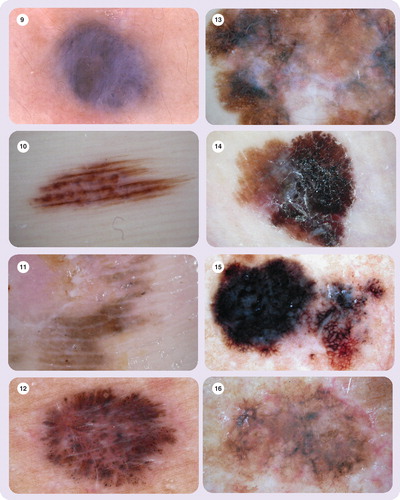
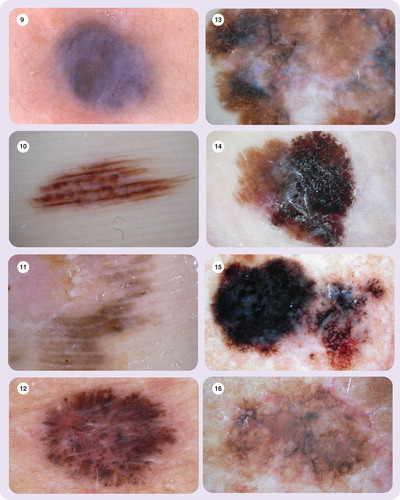
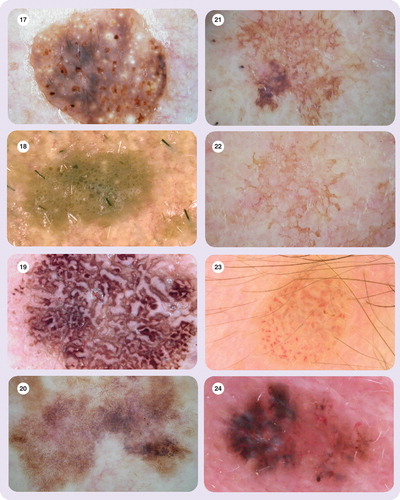
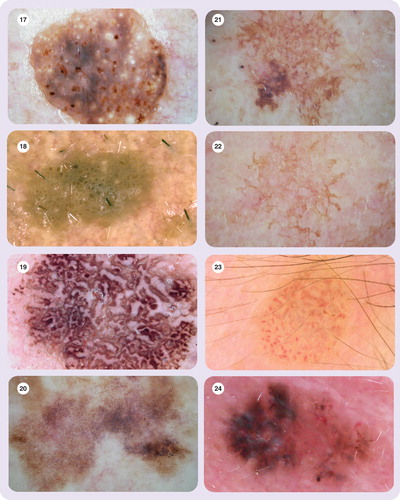
Leaf-like structures is the name given to gray-brown to slate-gray areas situated at the periphery of the lesion. They resemble fingers or maple leaves .
Large blue-gray ovoid nests are well-circumbscribed, confluent pigmented ovoid or elongated areas .
Multiple blue-gray globules are occasionally densely aggregated. It is important to differentiate them from multiple blue-gray dots or melanophages .
Spoke wheel areas are well-circumbscribed radial projections. They are blue, gray or brown in color and meet at an often darker (dark brown, black or blue) central axis .
A vascular pattern has the appearance of arborizing vessels, that is, telangiectases with tree-like branching .
Basal cell carcinoma is also more likely to be ulcerated than melanoma. We need to make sure that the ulceration is not due to recent trauma. It is usually a multiple event .
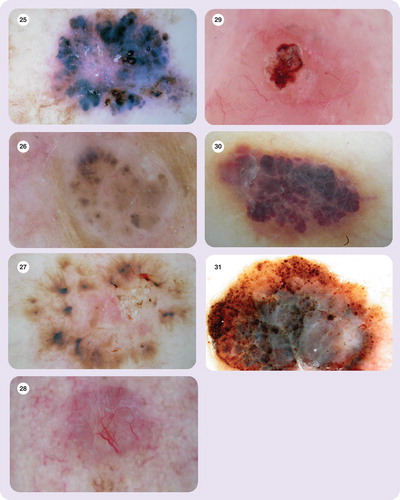
Vascular lesion criteria
Once melanocitic lesions, seborrheic keratosis and basal cell carcinoma are discarded as the cause, we proceed to check the possibility of a vascular lesion.
Lacunar patterns (red lagoons or red lacunas) are sharply demarcated oval areas with a reddish or red-bluish coloration due to increased and dilated vascular spaces within the papillary dermis .
If we have found none of the listed criteria, we are in the presence of a pigmented lesion with no specific criteria or unspecific pattern. We need to consider these lesions as melanocytic without specific pattern. Frequently, these unspecific pigmented lesions are melanomas.
If we are faced with a melanocytic lesion, we can now begin the second step in order to differentiate a benign melanocytic lesion from a melanoma.
There are different diagnosis methods we can use, such as pattern analysis Citation[11], ABCD rule Citation[14], seven-point checklist Citation[15], 11-point checklist Citation[16] and three-point checklist Citation[17–18] among others.
Conclusion
In my opinion, dermoscopy is the best method for the early clinical diagnosis of melanoma. It is very important to train well in this technique.
Five-year view
Dermoscopy should be included in the resident program as an easy and inexpensive diagnosis method that has been proven to improve the clinical diagnosis of melanoma.
References
- Stolz W. Color Atlas of Dematoscopy. Braun-Falco O, Bilek P, Landthaler M, Cognetta A (Eds). Blackwell Science, Germany (2002).
- Argenziano G, Soyer P, De Giorgio V, Piccolo D. Interactive Atlas of Dermoscopy. EDRA Medical Publishing & New Media, Italy (2000).
- Cabo H. Dermatoscopia. Weber Ferro, Argentina (2000).
- Menzies S, Crotty K, Ingvar C, McCarthy W. An Atlas of Surface Microscopy of Pigmented Skin Lesions, 2nd Edition McGraw-Hill Book Company, Sydney, Australia (2003).
- Malvhey J, Puig S. Principles of Dermoscopy. Creaciones Graficas, Barcelona, Spain (2002).
- de Giorgi V, Massi D, Salvini C, Trez E, Mannone F, Carli P. Dermoscopic feature of combined melanocytic nevi. J. Cutan. Pathol.31, 600–604 (2004).
- PehambergerH, Binder M, Steiner A, Wolff K. In vivo epiluminescencemicroscopy: improvement early diagnosis of melanoma. J. Invest. Dermatol.100, 356 (1993).
- Carli P, De Giorgi V, Soyer HP, Stante M, Mannone F, Giannotti B. Dermoscopy in the diagnosis of pigmented skin lesions: a new semiology for the dermatologist. J. Eur. Acad. Dermatol. Venereol.14, 353–369 (2000).
- Soyer P, Argenziano G, Chimenti S et al. Dermoscopy of Pigmented Skin Lesions. An Atlas Based on the Consensus Net Meeting on Dermoscopy. EDRA Medical Publishing & New Media, Italy (2001).
- Rabinovitz H, Kopf A. Dermoscopy: a practical guide. American Academy of Dermatology (1999).
- Pehamberger H, Steiner A, Wolff K. In vivo epiluminescence microscopy of pigmented skin lesions. I. Pattern analysis of pigmented skin lesions. J. Am. Acad. Dermatol.17, 571–583 (1987).
- Marghoob A, Braun R, Kopf A. Atlas of Dermoscopy. Taylor & Francis, London and New York (2005).
- Menzies S, Westerhoff K, Rabinivitz H et al. Surface microscopy of pigmented basal cell carcinoma. Arch. Dermatol.136, 1012–1016 (2000).
- Stolz W, Riemann A, Cognetta AB et al. ABCD rule of dermatoscopy: a new practical method for early recognition of malignant melanoma. Eur. J. Dermatol.4, 521–527 (1994).
- Argenziano G, Fabbrocini G, Carli P et al. Epiluminescence microscopy for the diagnosis of doubtful melanocytic skin lesions. Arch. Dermatol.134, 1563–1570 (1998).
- Menzies SW, Ingvar C, Crotty KA et al. Frequency and morphologic characteristic of invasive melanomas lacking specific surface microscopic features. Arch. Dermatol.132, 1178–1182 (1996).
- Jorh R, Soyer P, Argenziano G, Hofmann-Wellenhof R, Scalvenzi M. Dermoscopy. The Essentials. Mosby. Elsevier Ltd, New York, USA (2004).
- Zalaudek I, Argenziano G, Soyer HP et al. Three-point checklist of dermoscopy: an open internet study. Br. J. Dermatol.154, 431–437 (2006).