Abstract
Vitiligo is a common condition characterized by hypopigmented and/or depigmented spots on the skin, affecting approximately 1–2% of the world population. Until approximately 30 years ago, it was exclusively treated by medical therapies. The most commonly used medical therapies include topical steroids, calcineurin inhibitors and phototherapy. Lesions on the face and neck respond the best to medical therapies, followed by lesions on the proximal extremities and trunk, while those distributed over acral parts of extremities and nonhairy areas, such as the wrist, feet and male genitals, respond poorly. Surgical methods complement medical therapies by providing melanocytes to these refractory lesions, and are indicated for unilateral segmental and clinically stable bilateral vitiligo, refractory to medical treatment. Tissue-grafting methods include minigrafting or punch grafting, epidermal grafting and split thickness grafting. These methods use full-thickness punch grafts, roof of epidermal blisters and shave biopsy samples, respectively, as the source of melanocytes. Cellular grafting includes noncultured and cultured melanocytes/keratinocytes suspensions obtained from trypsinizing the shaved skin biopsy sample as a source of melanocytes. Recent advances over the years have enabled dermatologists to treat extensive areas located on any anatomic site in a single operative session by surgical intervention. The purpose of this review is to describe the selection criteria for the surgical treatment, their utility and limitations in the various types of vitiligo.
Medscape: Continuing Medical Education Online
This activity has been planned and implemented in accordance with the Essential Areas and policies of the Accreditation Council for Continuing Medical Education through the joint sponsorship of Medscape, LLC and Expert Reviews Ltd. Medscape, LLC is accredited by the ACCME to provide continuing medical education for physicians. Medscape, LLC designates this educational activity for a maximum of 1.0 AMA PRA Category 1 Credits™. Physicians should only claim credit commensurate with the extent of their participation in the activity. All other clinicians completing this activity will be issued a certificate of participation. To participate in this journal CME activity: (1) review the learning objectives and author disclosures; (2) study the education content; (3) take the post-test and/or complete the evaluation at http://www.medscapecme.com/journal/expertderm; (4) view/print certificate.
Learning objectives
Upon completion of this activity, participants should be able to:
• List factors associated with improved outcomes of surgical treatment for vitiligo
• Describe epidermal grafting procedures for vitiligo
• Identify characteristics of epidermal and split-skin grafting for vitiligo
• Describe the use of cellular grafting techniques for vitiligo
Financial & competing interests disclosure
CME AUTHOR: Charles P Vega, MD,Associate Professor; Residency Director, Department of Family Medicine, University of California, Irvine, CA, USA.Disclosure:Charles P Vega has disclosed no relevant financial relationships.
EDITOR: Elisa Manzotti,Editorial Director, Future Science Group.Disclosure:Elisa Manzotti has disclosed no relevant financial relationships.
AUTHORS
Sanjeev V Mulekar, MD,National Center for Vitiligo and Psoriasis, Riyadh, Saudi Arabia.Disclosure:Sanjeev V Mulekar has disclosed no relevant financial relationships. No writing assistance was utilized in the production of this manuscript.
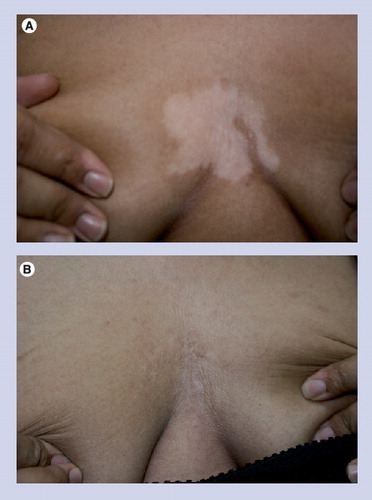
(A) 25-year-old female before treatment. (B) Patient 10 months after treatment with good repigmentation.
Vitiligo is a common condition characterized by hypopigmented and/or depigmented spots on the skin. Clinically, two distinct variants can be recognized. Generalized or bilateral, symmetrical vitiligo is a disease that begins during postnatal life, and with time progressively destroys the melanocytes in the skin, mucus membrane and, in some individuals, in the eyes and ears Citation[1]. Segmental vitiligo is unilateral and asymmetrical, which is often distributed in a dermatomal or quasi-dermatomal fashion. The depigmentation spreads quickly in the affected segments and then stops. In approximately half of the patients with segmental vitiligo, hair follicle melanocytes are affected, resulting in leukotrichia Citation[2].
It is not surprising to find references to the white spots in the ancient literature, due to these obvious skin findings. However, these references were probably not only restricted to vitiligo, but might have included other diseases such as leprosy, which also leaves white spots on the skin, and have been associated with other deformities. Only since the last century has vitiligo vulgaris in the present form been recognized as a progressive disease characterized by melanocyte destruction Citation[3].
Pathogenesis
Various theories have been put forward to explain the pathogenic events leading to melanocyte death and the development of hypopigmented patches. The most commonly accepted hypotheses are autoimmune, autocytotoxic, neural and genetic:
• Autoimmune hypothesis: this is supported by an association with other autoimmune diseases, and the detection of serum autoantibodies to melanocytes in patients with active disease, especially to melanosomal proteins Citation[4]. In addition, histological and immunohistochemical studies in perilesional skin and T-cell analyses in peripheral blood support the involvement of cellular immunity in vitiligo Citation[5];
• Autocytotoxic hypothesis: melanin precursors such as tyrosine have a potential to be cytotoxic to melanocytes. Phenolic and catecholic derivatives, which are structurally similar to tyrosine, are implicated in the development of contact vitiligo Citation[6];
• The neural hypothesis was first suggested by Lerner Citation[7]. In a study conducted to search for a link between vitiligo and the activity of monoaminergic systems, the levels of catecholamines and metabolites were significantly higher in vitiligo patients compared with controls. This may reflect the increased activity of monoaminergic systems in the early phase of the disease Citation[8];
• Genetic factors: several candidate genes and genetically linked loci have been identified that appear to mediate susceptibility to generalized vitiligo Citation[9].
Other possible mechanisms that might be responsible in the pathogenesis are melanocytorrhagy, oxidative stress and a potential interconnection of several factors:
• Melanocytorrhagy. Based on the recent morphologic findings, a new theory is suggested proposing melanocytorrhagy as a primary defect. According to this theory, depigmentation results from chronic detachment of melanocytes and their transepidermal loss due to their increased susceptibility to mechanical and other types of stresses Citation[10];
• Oxidative stress. The accumulation of toxic levels of hydrogen peroxide is documented in the epidermis of vitiligo patients. The crucial deficiencies are of the one or more reducing agents and detoxifying enzymes responsible for maintenance of redox homeostasis Citation[11];
• There may be a potential interconnection of several mechanisms, which may lead to autoimmune destruction of melanocytes. Oxidative stress may play an important role in the pathogenesis of vitiligo by initiating or amplifying the immunologic injury of melanocytes, as well as nitration of tyrosine Citation[12].
To summarize, vitiligo is the result of melanocyte destruction in genetically predisposed individuals due to a combination of pathogenic mechanisms, which include oxidative stress and an increase in catechol/phenol concentration, resulting in melanocytorrhagy and autoimmune activation.
Medical therapies
Despite limited knowledge of the pathogenesis during the early period, the ancient therapies recommended oral or topical administration of herbal medicines with sun exposure. These herbs contain active ingredients similar to psoralens, as discovered by modern pharmacological techniques, and remain the basic principle of present-day treatment, which includes exposure to ultraviolet rays with or without psoralens Citation[3].
With the advances in the knowledge of the pathogenesis, the present medical therapies are directed to prevent the destruction of melanocytes and stimulate the residual melanocytes to induce repigmentation.
Most commonly used medical therapies for localized vitiligo include topical steroids, which suppress the immune system by decreasing immunoglobulin and complement Citation[13], and topical calcineurin inhibitors, for example, tacrolimus, which inhibit T-cell activation by downregulating the transcription of genes encoding proinflammatory cytokines Citation[14]. In addition, there is in vitro evidence demonstrating that direct interaction between tacrolimus and keratinocytes creates a favorable milieu for melanocyte and melanoblast growth and migration Citation[15,16]. For generalized vitiligo, ultraviolet (UV) radiation in the form of UVB and UVA is used as first-line therapy. They act by immunosuppression and stimulate melanocyte multiplication and migration. UVB induces T-regulatory (suppressor) cell activity, which may suppress autoimmune conditions Citation[17]. The sera of patients after UVA therapy contains higher levels of basic fibroblast growth factor (bFGF), stem cell factor and hepatocyte growth factor, which may create a favorable environment for regrowth of melanocytes Citation[18]. Systemic psoralen and UVA increases the number of residual melanocytes, most probably by enhancing melanocyte growth factors, such as bFGF and endothelin 1 Citation[19], and stimulating migration of nondendritic pigment cells along the external root sheath of the hair follicle towards the epidermis Citation[20]. Systemic corticosteroids are used by some only in rapidly progressive disease, and act by reducing antibody-mediated cytotoxicity against pigment cells Citation[21].
However, there is a paucity of a medical therapeutic agent that can prevent melanocyte destruction for a very prolonged period without significant adverse effects, and it is essential to have residual melanocytes in the form of a melanocyte reservoir to achieve their proliferation. Various studies have established the presence of a melanocyte reservoir in the lower third of the hair follicle Citation[20,22]. Recently, melanoctyte stem cells have been demonstrated in the bulge area near the insertion of the hair follicle muscle Citation[23]. The importance of the melanocyte reservoir is clinically evident by the fact that the face and neck have the maximum response rate to the medical therapies, followed by the proximal extremities and trunk. Acral parts of the extremities and non-hairy areas, such as the wrist, feet and male genitals, respond poorly Citation[3]. The presence of leukotrichia is also a poor prognostic sign Citation[24].
Surgical therapies
Until approximately 30 years ago, vitiligo was exclusively treated by medical therapies, and the earliest surgical interventions in the management of vitiligo can be traced to reports by Behl Citation[25,26] and Falabella Citation[27].
Factors to be considered for surgical therapies
Stability
By definition, bilateral vitiligo is an acquired progressive hypopigmentary disease with periods of progression and remission. The commonly accepted guidelines for clinical stability are: no new lesions should appear, existing lesions should remain the same size, absence of koebnerization, spontaneous repigmentation and positive minigraft test, especially when minigrfating is performed. The period of stability varies from 6 months to 3 years Citation[28–31]. In the absence of any rigorous studies and objective tests, these criteria are entirely subjective and sometimes unreliable. This is evident by the fact that in practice we observe repigmentation of existing patches and appearance of new lesions at the same time. We also find patients who show complete repigmentation in some areas, but not in other areas treated surgically at the same time Citation[32]. Partial or complete failure to repigment following different surgical treatments and negative minigraft test has been reported despite clinical stability in the generalized as well as localized type of vitiligo patients Citation[33–36]. Repigmentation of recipient areas in spite of koebnerization of donor site indicates that autoimmune activity may be different at different sites in the same patient Citation[37].
Size of lesions & total area
Tissue-grafting methods, such as minigrafting and blister grafting, are useful to treat small and medium-sized lesions Citation[28,29]. Larger areas can be treated by split thickness graft Citation[38]. Extensive areas can be treated with the development of cultured Citation[39] and non-cultured Citation[36] cellular transplantations.
Anatomical locations
Body folds are not suitable for treatment with minigrafting and blister grafting, due to the difficulty in immobilizing the treated area. Certain areas such as the fingers and toes, palms and soles, lips, eyelids, nipples and areola, elbows and knees, and genitals are considered difficult to treat sites and require special precautions in therapy Citation[29,40,41]. However, noncultured cellular transplantation does not require any special precautions to treat these sites Citation[42].
Type of vitiligo
Segmental vitiligo is the most suitable type for surgical intervention, followed by focal vitiligo. The segmental type is distinct in the sense that it is restricted to only one anatomical part in a dermatomal fashion, progresses quickly and then remains stable for the rest of life Citation[2]. Focal vitiligo may remain localized, but has the potential to transform into generalized type. In the vulgaris type, lesions located on the glabrous skin, and with leukotrichia, are best suited for surgical intervention. The lip-tip type is resistant to surgical therapies, the reason for which is not known.
Age
Surgical therapies are recommended to treat only adults. It has also been recommended to treat highly motivated preadolescents Citation[29]. However, they are not recommended to treat children irrespective of the type and stability. The probable reasons are the invasive nature of the procedures, risk of anesthesia, technical difficulties such as immobilization for prolonged periods and lack of data Citation[29,43,44]. Recently, Mulekar et al. treated 25 children (4–16 years) with localized vitiligo with the noncultured melanocytes–keratinocytes transplant procedure. During a 4.5-year follow-up they reported 77% of the patients had good to excellent repigmentation in the segmental group, and 83% had excellent to good repigmentation in the focal group Citation[45]. No complication of anesthesia was observed in this study.
Skin type
Skin type IV–VI responds quickly to the surgical treatment. Skin type III is slower to repigment, and quite often requires post-operative phototherapy. Type I skin does not tan and hence it is not advisable to treat these patients. Type II skin is likely to yield poor results due to poor ability to tan. There is a common belief among the dermatologists that individuals with lighter skin are not concerned about vitiligo, as it is quite often unnoticed. However, most light-skinned individuals tan significantly during summer, when the hypopigmented lesions stand out and are prone to sunburn. Therefore, they are also keen to seek treatment. On the contrary, hypopigmented lesions are easily noticeable in dark-skinned individuals irrespective of the season. The biggest difference between these two ethnic groups is the social rejection of vitiligo patients in the South Asian and Middle Eastern region. This can be attributed to the different social behavioral pattern of both the societies.
Depigmented versus hypopigmented lesions
The best lesions to treat are depigmented lesions. Hypopigmented lesions are likely to produce cosmetically inferior results Citation[29]. Another risk factor is the koebnerization due to the trauma of dermabrasion. Although the loss of residual pigment in hypopigmented lesions due to the surgical procedure has not been documented, it is possible that a hypopigmented patch will lose pigment and turn depigmented. Thus, it is best to avoid treating hypopigmented lesions surgically.
Donor site
The donor site should be as hidden as possible, but depends upon the method and surgeon’s expertise.
Serial procedures
A single operative procedure does not always result in complete repigmentation, and multiple serial sessions are required to achieve a satisfactory pigmentation. Approximately 50% of patients in the generalized group, and 33% in the segmental group require more than one procedure to achieve near-complete or complete repigmentation at an interval of approximately 4–6 months.
Patient expectations
The expectations of patients may vary from moderate to very high. They may be satisfied with some repigmentation with narrow-band UVB, but expect miracles with the surgical therapies. It may be partly due to the fact that expenses incurred for the surgical treatment are high and are paid at once. On many occasions it is difficult to explain to patients that it is not the preventive treatment, but can only treat the existing achromic patches. The appearance of new lesions and loss of pigment during the follow-up period from previously treated lesions remains a possibility. Another important consideration is that the chances of improvement are conveyed to patients in the form of a percentage. However, this statistical description applies to a group and not to individuals. Hence, it is very disappointing to a patient, especially to segmental vitiligo patients, if they fail to repigment.
Record-keeping
Most studies report repigmentation in terms of a percentage of pigmentation. The vitiligo area scoring index, designed to measure the affected area (Vitiligo Area and Severity Index score) Citation[46], may improve the quality of assessment along with photographic documentation.
Contraindications
The absolute contraindication is keloidal tendencies and hypertrophic scars. Hyperpigmentation in the area of previous injury or burn may be a relative contraindication. However, patients tend to accept hyperpigmentation rather than hypopigmentation. It is not advisable.
Infrastructure & training
Punch grafting is the easiest method, which can be practiced by a physician alone in his/her office and requires simple instruments such as biopsy punches. Epidermal grafting requires special instruments to produce blisters, and a procedure room where a patient can stay for a prolonged period. Split-skin grafting requires surgical skills and a fully equipped operation theatre with its attendant cost. Cultured techniques are complex and need a specialized laboratory with highly trained personnel. Noncultured cellular transplantation is best performed by a physician with an assistant, and requires special instruments and adequate training.
A physician should select the technique depending upon the training, infrastructure and economic affluence of the population.
Surgical methods
Tissue grafting or conventional grafting techniques
Tissue grafting or conventional methods use grafts in the form of blister roof, split thickness skin sample or punch graft. This does not involve cell separation in vitro, and melanocytes are stimulated by UV rays to facilitate their spread in the peri-graft area.
Minigrafting or punch grafting
In this method, grafts are harvested with the help of biopsy punch, preferably from the gluteal region, and fixed into the pits created by a similar instrument to the recipient area. They are secured with micropore tape or steri strips. Dressing is removed after 7–14 days.
The basic procedure has been modified by several practitioners in order to minimize the side effects, to increase the area to be treated and to hasten and improve the pigmentation. The size of the grafts varies from 1 to 3 mm, and are placed 3–10 mm apart, which may be determined by the skin type and graft size Citation[13,28]. The grafts obtained from dark-skinned individuals can be placed 5–10 mm apart due to the properties of melanocytes, which produce larger melanosomes. However, in Caucasian patients, it is advisable to transplant them 3–5 mm apart, as melanocytes obtained from Caucasian skin produce smaller melanosomes Citation[28]. Cobble stoning is the most commonly observed adverse effect of this procedure, which can be prevented by implanting grafts larger than the pits Citation[47], trimming excess adipose tissue from the bottom of grafts Citation[28] and punching the recipient pits 1 mm deeper than the thickness of grafts Citation[35]. Postoperative phototherapy is usually recommended to hasten the perigraft spread of pigment.
In a study to demonstrate the usefulness of minigrafting in the treatment of localized vitiligo, 13 patients achieved 90–100% repigmentation, two had partial improvement and two were not treated as they had a negative minigraft test Citation[33]. In total, 23 patients (36 lesions) were analyzed in a study to evaluate the efficacy of minigrafting in vitiligo vulgaris. In total, 14 of 36 lesions showed 80–99% repigmentation, ten showed 50–80% repigmentation and 12 showed 0–50% repigmentation Citation[35]. Furthermore, in a prospective study by Malakar and Dhar of the 880 patients, 656 patients (74.55%) achieved 90–100% repigmentation. In 10.57%, there was no spread of pigment, while in 2.39%, depigmentation of grafts was noticed. Polka-dot appearance (43.98%) and color mismatch (34.32%) were the most frequent side effects Citation[48].
This is the easiest and most inexpensive method, which can be performed by any dermatologist in his/her office with cosmetically acceptable results. The repigmentation yield ratio varies from 1:10 to 1:20 (Box 1).
Epidermal grafting
Epidermal grafting involves obtaining pure viable epidermis-bearing melanocytes in the form of blisters by applying negative pressure (300–500 mmHg) to the normally pigmented skin. The grafts thus obtained are transferred to the denuded recipient sites. They are held in place for 7 days with nonadherent dressing. This technique was first described by Kistala Citation[49], and was used first to treat leucoderma/vitiligo by Falabella Citation[50,51]. Different custom-made devices, such as an oil rotary vacuum connected to a manometer Citation[52], a manually operated suction unit with transparent plastic cups Citation[53] and disposable syringes attached to a three-way tap with a latex rubber tube and 50 ml syringe Citation[54], are used to produce blisters on the donor and recipient areas. The blisters on both the donor and recipient sites are produced simultaneously. The usual time to harvest blisters is approximately 2–3 h. However, this can be reduced by application of heat, and by selecting the donor skin over bony prominences Citation[54].
In total, 31 patients with segmental vitiligo and 14 nondermatomal type were treated by epidermal grafting, and followed for more than 6 months post-surgically. In the segmental group 25 patients regained normal pigmentation, four had partial improvement and two did not respond to the treatment. In the nondermatomal group, 11 repigmented initially, but three lost the pigment subsequently Citation[52]. Mutalik reported good repigmentation in 48 of 50 patients with localized long-standing stationary patches of vitiligo, treated by epidermal grafting within 3–4 months after transplantation Citation[53]. In a retrospective, uncontrolled case series and literature review, the success rate for generalized and segmental/focal vitiligo was 53% (confidence interval 42–64) and 91% (confidence interval 81–100), respectively, in 117 patients over a post-operative period of 6 months Citation[55].
The significant advantage of this procedure is that this is a scar-less surgery and gives very good cosmetic results. It is easy and inexpensive and can be performed on almost any anatomic site, except body folds. However, it is quite time-consuming and can treat only small areas in a single operative session (Box 2).
Split-skin grafting
Split-skin grafting is the first method used to treat vitiligo surgically. This method uses skin grafts harvested with either a hand-held Humpy’s knife or a motorized Zimmer dermatome and placed directly on the recipient area prepared by laser ablation or motorized dermabrasion. They are secured with surgical dressing, which is removed after 1 week.
Behl reported excellent repigmentation in 70% of 107 treated patients with split-skin grafting Citation[25]. All five patients treated by grafts harvested with a Zimmer dermatome repigmented completely during the follow-up period of 3.5–35.5 months. Although no scarring was observed, all the patients developed milia on the recipient site Citation[56]. In another study by Kahn and Cohen, good to excellent repigmentation was observed in 88% of the 17 procedures performed on 12 patients using meshed grafts without scarring Citation[38]. In another series of 21 patients with 32 stable refractory vitiligo patches, 100% repigmentation was achieved in 22 patches and 90–95% in ten others Citation[57].
The advantage of this method is that large areas can be treated in a single operative session. However, the donor to recipient ratio remains 1:1, and a hospital setting to treat larger areas increases the cost of therapy. Although scarring has been reported at the donor and recipient site, it can be avoided with skilled hands and by the use of instruments such as a Zimmer dermatome. Although it gives excellent results, this is not a popular method with dermatologists, and is mainly practiced and reported by surgeons (Box 3).
Cellular grafting: noncultured & cultured techniques
These techniques use separated cells in the form of suspension. These cellular suspensions are transplanted as noncultured suspension or after culturing them in vitro on to the recipient area.
Initial steps are common to both the techniques. They are as follows: a shave biopsy is taken with the help of a silver’s skin grafting knife (E. Murray Co., UK) or a Goulian skin graft knife (E Weck Co., NJ, USA) from the gluteal area or upper thigh. The specimen is transferred to 0.25% trypsin and incubated for a varying period of 15 min to 3 h Citation[58–61]. After incubation, the skin sample is washed, trypsin is neutralized and epidermis is separated from the dermis mechanically to obtain epidermal cells.
Noncultured melanocyte–keratinocyte transplantation
This technique involves separation of epidermal cells as described earlier (see section entitled ‘Cellular grafting – noncultured & cultured techniques’). The epidermal cells thus obtained are suspended in either normal saline Citation[62], M2 melanocyte medium (Promocell, Heidelberg, Germany) Citation[63], Dulbecco-modified essential medium Citation[64] or sodium lactate Citation[65]. Addition of hyaluronic acid to the cell suspension improves the viscosity and attachment of cells to the recipient site Citation[66]. The epidermis of achromic skin is superficially removed using diamond fraise wheel or Er:YAG laser. Clinically, the level of dermabrasion is determined by the appearance of pinpoint bleeding. The cell suspension seeded on to the recipient area is first covered with collagen dressing, which is held in place with sterile gauze pieces for 1 week. Absolute immobilization is not necessary.
The technique was first reported by Gauthier and Surleve-Bazeille, in which they injected the suspension in the blisters produced on the recipient area Citation[62]. Several modifications have been carried out over the years to make it more effective and simple. Olsson and Juhlin diluted the cell suspension to achieve a donor to recipient ratio of up to 1:10, and prepared the recipient area with motorized dermabrasion using a diamond fraise wheel. This shortened the surgery time significantly, converting it into a day-care procedure. They reported complete repigmentation in most vitiligo patients Citation[63]. Mulekar simplified the procedure further by using Dulbecco’s Modified Eagle’s Medium F12 medium (Invitrogen Corporation, CA, USA) instead of different media at various stages of the procedure. The medium was not supplemented with penicillin, streptomycin and basic fibroblast growth factor, and a CO2 incubator was replaced with an ordinary incubator. The cell separation was performed in the procedure room on a clean bench, thus eliminating the transfer of the shave biopsy sample to a separate laboratory Citation[64].
In a long-term study over a period of 6 years with 142 patients with vitiligo vulgaris, 56% of patients showed excellent, 11% good, 9% fair and 24% poor repigmentation Citation[36]. In another long-term study over a period of 5 years, all the segmental vitiligo patients retained the repigmentation achieved at the end of their respective follow-up period, indicating the possibility of a disease-free period for the rest of their life Citation[64].
There are several advantages of this technique. Extensive areas can be treated from a small skin sample, with cosmetic results comparable with those produced by a cultured technique . This is a day-care procedure, which can be completed in 45 min to 2 h. All the procedure steps can be performed in a clean procedure room. However, it requires specialized instruments such as a dermabrader, incubator and centrifuge. In addition, it requires adequately trained personnel to achieve desired results (Box 4).
In vitro cultured pure melanocytes & coculture of keratinocytes/melanocytes or cultured epidermal sheets
The initial steps to obtain the epidermal cells have been described previously. The cells obtained are transported to the cell culture laboratory for in vitro culture. The culturing process of melanocytes/epidermal sheets bearing melanocytes takes approximately 3 weeks to obtain the adequate yield required for transplantation. Thus, two visits are required to accomplish this treatment. In the first visit, a shave biopsy skin sample is harvested. The second visit is made after about 3 weeks for transplantation of cultured melanocytes/epidermal sheets. The recipient area is denuded with motorized dermabrasion or with Er:YAG laser, and cultured cell suspensions or epidermal sheets are transplanted on to the recipient area and secured by suitable nonadherent dressing.
Olsson and Juhlin reported good cosmetic results in nine of ten patients treated with transplantation of autologous cultured melanocytes. Melanocytes were cultured using PC1 medium (Ventrex, ME, USA) supplemented with 50 U/ml penicillin, 0.05 ng/ml streptomycin, 2 mM L-glutamine and 5 ng/ml bFGF. The melanocytes were seeded at the concentration of 1000–2000/mm2Citation[59]. Melanocytes were isolated from donor skin samples obtained by producing a suction blister, and seeded into flasks containing modified melanocyte medium which consisted of Ham’s F12 nutrient mixture (Gibco®, Invitrogen, CA, USA) supplemented with 50 µg/ml gentamicin, 20 ng/ml recombinant human bFGF (Sigma-Aldrich, MO, USA), 10 ng/ml cholera toxin and 20% fetal calf serum (Biological Industries, Kibbutz, Israel) for the culturing purpose. An adequate number of melanocytes was cultured after an average of 24.1 days. The epidermis of the affected area was removed superficially using a Silktouch Flashscanner® attached to a Sharplan 1030 CO2 laser. The melanocytes suspension was applied to a laser denuded area at the density of 70,000–100,000/cm2. The repigmentation was classified as excellent in 21 and good in four patients with segmental vitiligo in this study Citation[67]. In total, 120 patients were treated with transplantation of autologous pure melanocytes suspension. Cells were cultured in Hu16 medium with Ham F12 nutrient mixture (Gibco) supplemented with 50 µg/ml gentamicin, 20 ng/ml recombinant human bFGF (Sigma-Aldrich), 10 ng/ml cholera toxin and 20% fetal calf serum (Biological Industries). Cells were applied to a laser denuded area in the concentration of 60,000–100,000/cm2. Excellent results were obtained in 84, 54 and 0% of the cases in stable localized group (n = 80), stable generalized group (n = 26) and active generalized group (n = 14), respectively Citation[60]. A total of 2315.8 cm2 of achromic surface in 21 patients was transplanted with autologous cultured epidermis, which was cultured in keratinocyte growth medium: Dulbecco-Vogt Eagle medium and Ham F12 media (2:1 mixture), containing 10% fetal calf serum, 0.1 nM cholera toxin and 10 ng/ml of epidermal growth factor, in 5% carbon dioxide and humidified atmosphere. The recipient area was prepared using pulsed Er:YAG laser (Laser Smart 2940, DEKA Medical Electronics Laser Associated srl, Calenzano, Florence, Italy). The average percentage of repigmentation was 75.9% at 6 months post transplantation. Variation of the melanocyte concentration in cultured epidermis varied from 1:30 to 1:200 Citation[68].
The significant advantage of this technique is the possibility to treat extensive areas with excellent cosmetic results. However, it is very complex procedure requiring specialized instruments such as a carbon dioxide incubator, laminar flow bench and a cell culture laboratory. Due to these limitations, this technique is mainly limited to research facilities (Box 5).
Conclusion
Until approximately 30 years ago, vitiligo was considered as a progressive disease in all patients, and was exclusively treated by medical therapies. Melanocytes destruction is the end result of an incompletely understood pathological process in vitiligo leading to the development of achromic lesions. The aim of the medical therapies is to prevent destruction of melanocytes, and stimulate proliferation and migration of residual melanocytes to achromic areas.
Surgical therapies have an important place in the management of vitiligo in the absence of any credible mechanism, which can prevent destruction of melanocytes for a prolonged period without side effects. The mesenchymal stem cell as a source of melanocytes in vivo is still hypothetical. Recent advances in the surgical methods have enabled the dermatologists to treat any anatomic site with acceptable cosmetic results at least temporarily in the generalized type, and almost permanently in the unilateral segmental type. Due to the high success rate, especially in the localized type, surgical options are being increasingly sought both by patients and physicians.
Expert commentary
Surgical therapies remain a viable option for patients with localized areas that have failed medical intervention. Stable segmental vitiligo with leukotrichia is also considered as an indication for surgical treatment. However, due to its invasive nature, they are not recommended in children; nevertheless, highly motivated preadolescents can be treated under sedation or general anesthesia. In addition, surgical therapies are not used to treat children because of technical difficulties, such as inabilities to immobilize the treated area for a prolonged period. The most commonly used methods, which comprise of tissue grafting, allow covering small- to medium-sized lesions in one operative session. The treatment of joints, fingers, eyelids, areola and genitals requires special precautions to immobilize these parts in order to achieve good results, and hence are considered as difficult-to-treat areas, resulting in physicians being discouraged to treat these sites. Other limiting factors are the prolonged period required to cover a relatively small area, and adverse events associated with the procedure.
With the advancement in the techniques, and horizontal spread of training, surgical therapies are more frequently practiced, especially in Asian countries. The use of cultured or noncultured cellular suspension is a step ahead. This has eliminated many limitations of tissue-grafting methods, and improved cosmetic results. Although the cultured methods appeared more promising and appealing, they are restricted to research centers and universities due to the requirement for a specialized laboratory, inventory of culture media and additives and highly trained personnel, with the associated cost escalations. In order to retain the advantages of cultured techniques, and eliminate the disadvantages of tissue-grafting methods without significant cost escalations, a novel method, which used noncultured cellular suspension, has been tried successfully. However, this is not yet widely practiced due to the lack of training available for physicians.
In recent times, most documentation in the management of vitiligo has focused on surgical therapies. They are highly successful in repigmenting clinically stable lesions on glabrous skin, with leukotrichia and segmental vitiligo. Children with stable localized unilateral vitiligo have been successfully treated with noncultured cellular transplantation, without any morbidity. Therefore, surgical management will be considered more often and as a first choice of treatment in these indications mentioned previously.
Five-year view
The surgical therapies are being increasingly accepted in the management of vitiligo both by patients and physicians. Despite the advances in the technique, we experience partial or complete failures in some of the treated patients regardless of clinical stability. This is due to the absence of any parameter to determine the degree of immunological activity. Research in the understanding of the pathogenesis of vitiligo could help us to determine the stability and prognosis of the surgical treatment.
Histological and immunological evidence suggest that melanocytes from clinically normal skin may also be defective, and this may be one of the reasons for the failure to repigment following the transplantation. The potential of mesenchymal stem cells as a source of melanocytes is still hypothetical, but may provide a solution for the immunologically compromised melanocytes.
Biologics play an important role in the management of autoimmune disorders, and have the potential to transform the medical management of these disorders.
Box 1. Minigrafting or punch grafting.
• Minigrafting or punch grafting is the easiest and cheapest surgical method to treat vitiligo.
• This procedure produces acceptable cosmetic results.
• Cobble stoning and color mismatch are the most commonly reported side effects.
Box 2. Epidermal grafting.
• Epidermal grafting is an easy, safe, inexpensive and effective method for treating vitiligo.
• The technique offers the advantages of good color matching and scar-less surgery.
• Disadvantages include the fact it is time-consuming and unsuitable for body folds.
Box 3. Split-skin grafting.
• Split-skin grafting yields the highest success rate in the treatment of vitiligo, and relatively large areas can be treated.
• The development of milia is the most common side effect.
• Scarring can be avoided by skilled hands and by using suitable instruments.
Box 4. Noncultured melanocyte–keratinocyte transplantation.
• Very large areas can be treated in one operative session of noncultured melanocyte–keratinocyte transplantation.
• Good cosmetic results can be achieved.
• Scarless surgery is achievable at skilled hands.
• Requires specialized instruments and trained personnel.
Box 5. In vitro cultured pure melanocytes and co-culture of keratinocytes/melanocytes or cultured epidermal sheets.
• Treament of vitiligo with in vitro cultured pure melanocytes and co-culture of keratinocytes/melanocytes or cultured epidermal sheets produces excellent cosmetic results.
• Extensive areas can be treated.
• However, the process is complex and requires highly trained personnel and specialized equipment.
• This therapy is mainly restricted to research laboratories.
Key issues
• Most commonly accepted pathogenic mechanisms of vitiligo are autoimmune, autocytotoxic, neural and genetic.
• Other possible mechanisms are melanocytorrhagy, oxidative stress and a potential combination of several factors.
• Most commonly used medical therapies for localized therapies are topical steroids and calcineurin inhibitors.
• Narrow-band ultraviolet B or psoralen and ultraviolet A is the first-line therapy for generalized vitiligo.
• Clinical stability is the most important criteria for surgical treatment.
• Other factors to be considered before selecting surgical treatment are the size of lesions, anatomical location, type of vitiligo, age, skin type, serial procedures, patients’ expectations and infrastructure and training.
• Tissue-grafting methods are commonly practiced and are blister grafting, minigrafting and skin grafting. This does not involve cell separation in vitro.
• Cellular grafting uses separated cells in the form of suspension. These cells are transplanted as noncultured or subsequent to in vitro culture.
• Recent advances in the surgical methods have enabled dermatologists to treat any anatomic site with acceptable cosmetic results at least temporarily in the generalized type, and almost permanently in the unilateral segmental type.
Financial & competing interests disclosure
The author has no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
References
- Lerner AB, Nordlund JJ. Vitiligo: the loss of pigment in the skin, hair and eyes. J. Dermatol.1, 1–8 (1978).
- Hann SK, Lee JH. Segmental vitiligo: clinical findings in 208 patients. J. Am. Acad. Dermatol.35, 671–674 (1996).
- Nordlund JJ, Ortonne JP, Le Poole C. Genetic hypomelanoses: acquired depigmentation. Chapter 30. In: The Pigmentary System. Second Edition. Nordlund JJ, Boissy RE, Hearing VJ, King RA, Oetting WS, Ortonne JP (Eds). Blackwell Publishing, Oxford, UK, 551–598 (2006).
- Kemp EH, Gavalas NG, Gawkrodger DJ, Weetman AP. Autoantibody responses to melanocytes in the depigmenting skin disease vitiligo. Autoimmun. Rev.6, 138–142 (2007).
- Ongenae K, Van Geel N, Naeyaert JM. Evidence for an autoimmune hypothesis of vitiligo. Pigment Cell Res.16, 90–100 (2003).
- Boissy RE, Manga P. On the etiology of contact/occupational vitiligo. Pigment Cell Res.17, 208–214 (2004).
- Lerner AB. Vitiligo. J. Invest. Dermatol.32, 285–310 (1959).
- Cucchi ML, Frattini P, Santagostino G, Orecchia G. Higher plasma catecholamine and metabolite levels in the early phase of nonsegmental vitiligo. Pigment Cell Res.13, 28–32 (2000).
- Spritz RA. The genetics of generalized vitiligo and associated autoimmune diseases. Pigment Cell Res.20, 271–278 (2007).
- Gauthier Y, Cario Andre M, Teib A. A critical appraisal of vitiligo etiologic theories: is melanocytic loss a melanocytorrhagy? Pigment Cell Res.16, 322–332 (2003).
- Westerhof W, d’lschia M. Vitiligo puzzle: the pieces fall in place. Pigment Cell Res.20, 345–359 (2007).
- Namazi MR. Neurogenisc dysregulation, oxidative stress, autoimmunity, and melanocytorrhagy in vitiligo: can they be interconnected? Pigment Cell Res.20, 360–363 (2007).
- Falabella R, Barona MI. Update on skin repigmentation therapies in vitiligo. Pigment Cell Melanoma Res.22, 42–65 (2008).
- Lawrence ID. Tacrolimus (FK506) experience in dermatology. Dermatol. Ther.5, 74–84 (1998).
- Lan CC, Chen GS, Chiou MH, Wu CS, Chang CH, Yu HS. FK506 promoted melanocytes and melanoblast growth and creates of favorable milieu for cell migration via keratinocytes: possible mechanisms of how tacrolimus ointment induces repigmentation in patients with vitiligo. Br. J. Dermatol.153, 498–505 (2005).
- Kang HY, Choi YM. FK506 increases pigmentation and migration of human melanocytes. Br. J. Dermatol.155, 1037–1040 (2006).
- Ponsonby AL, Lucas RM, van der Mei IA. UVR, vitamin D and three autoimmune diseases – multiple sclerosis, Type 1 diabetes, rheumatoid arthritis. Photochem. Photobiol.81, 1267–1275 (2005).
- Wu CS, Lan CC, Wang LF, Chen GS, Wu CS, Yu HS. Effects of psoralen plus ultraviolet A irradiation on cultured epidermal cells in vitro and patients with vitiligo in vivo. Br. J. Dermatol.156, 122–129 (2007).
- Abdel-Naser MB, El-Khateeb EA, Sallam TH, el-Menshawi BS. Endothelin-1 is significantly elevated in plasma of patients with vitiligo treated with psoralen plus ultraviolet A. Clin. Exp. Dermatol.31, 571–575 (2006).
- Cui J, Shen LY, Wang CG. Role of hair follicles in the repigmentation of vitiligo. J. Invest. Dermatol.97, 410–416 (1991).
- Razaei N, Gavalas NG, Weetman AP, Kemp EH. Autoimmunity as an etiological factor in vitiligo. J. Eur. Acad. Dermatol. Venereol.21, 865–876 (2007).
- Arrunategui A, Arroyo C, Garcia L et al. Melanocytes reservoir in vitiligo. Int. J. Dermatol.33, 484–487 (1994).
- Loomis CA, Koss J, Chu D. Embryology. In: Dermatology Second Edition. Bolognia JL, Jorizzo JL, and Rapini RP (Eds). Elsevier, Spain, 37–47 (2008).
- Dutta AK, Mandal SB. A clinical study of 650 vitiligo cases and their classification. Indian J. Dermatol.14, 103–111 (1969).
- Behl PN. Treatment of vitiligo with homologous thin Thiersch’s skin grafts. Curr. Med. Pract.8, 218–221 (1964).
- Behl PN, Bhatia RK. Treatment of vitiligo with autologous thin Thiersch’s graft. Int. J. Dermatol.12, 329–331 (1973).
- Falabella R. Repigmentation of segmental vitiligo by autologous minigrafting. J. Am. Acad. Dermatol.9, 514–521 (1983).
- Mutalik S, Ginzburg A. Surgical management of stable vitiligo: a review with personal experience. Dermatol. Surg.26, 248–254 (2000).
- Falabella R. Surgical approaches for stable vitiligo. Dermatol. Surg.31, 1277–1284 (2005).
- Hann SK, Im S, Bong HW, Park YK. Treatment of stable vitiligo with autologous epidermal grafting and PUVA. J. Am. Acad. Dermatol.32, 943–948 (1995).
- Mulekar SV. Melanocyte-keratinocyte cell transplantation for stable vitiligo. Int. J. Dermatol.42, 132–136 (2003).
- Juhlin L. How unstable is the concept of stability in surgical management of vitiligo. Dermatology201, 183 (2000).
- Falabella R. Treatment of localized vitiligo by autologous minigrafting. Arch. Dermatol.124, 1649–1655 (1988).
- Falabella R, Escobar C, Borrero I. Treatment of refractory and stable vitiligo by transplantation of in vitro cultured epidermal autografts bearing melanocytes. J. Am. Acad. Dermatol.26, 230–236 (1992).
- Boersma B, Westerhof W, Bos JD. Repigmentation in vitiligo vulgaris by autologous minigrafting: results in nineteen patients. J. Am. Acad. Dermatol.33, 990–995 (1995).
- Mulekar SV. Long-term follow-up study of 142 patients with vitiligo vulgaris treated by autologous, noncultured melanocyte-keratinocyte cell transplantation. Int. J. Dermatol.44, 841–845 (2005).
- Mulekar SV, Asaad M, Ghwish B, Al Issa A, Al Eisa A. Koebner phenomenon in vitiligo: not always an indication of surgical failure. Arch. Dermatol.143, 801–802 (2007).
- Kahn AM, Cohen MJ. Repigmentation in vitiligo patients. Melanocyte transfer via ultra-thin grafts. Dermatol. Surg.24, 365–367 (1998).
- Olsson MJ, Juhlin L. Transplantation of melanocytes in vitiligo. Br. J. Dermatol.91, 587–591 (1995).
- Gupta S, Narang T, Olsson MJ, Ortonne JP. Surgical management of vitiligo and other leucodermas: evidence-based practice guidelines. In: Surgical Management of Vitiligo. Gupta S, Olsson MJ, Kanwar AJ, Ortonne JP (Eds). Blackwell Publishing Ltd, Oxford, UK, 69–79 (2007).
- Nanda S, Relhan V, Grover C, Reddy BS. Suction blister epidermal grafting for management of eyelid vitiligo: special considerations. Dermatol. Surg.32, 387–392 (2006).
- Mulekar SV, Al Issa A, Al Eisa A. Treatment of vitiligo on difficult-to-treat sites using autologous noncultured cellular grafting. Dermatol. Surg.35, 66–71 (2009).
- Gawkrodger DJ, Ormerod AD, Shaw L et al. Guidelines for the diagnosis and management of vitiligo. Br. J. Dermatol.159, 1051–1076 (2008).
- Huggins RH, Schwartz RA, Janniger CK. Childhood vitiligo. Cutis79, 277–280 (2007).
- Mulekar SV, Al Eisa A, Delvi MB, Al Issa A, Al Saeed AH. Childhood vitiligo: a long-term study of localized vitiligo treated by noncultured cellular grafting. Pediatr. Dermatol. (2009) (Epub ahead of print).
- Hamzavi I, Jain H, McLean D, Shapiro J, Zeng H, Lui H. Parametric modeling of narrowband UV-B phototherapy for vitiligo using a novel quantitative tool: the vitiligo area scoring index. Arch. Dermatol.140, 677–683 (2004).
- Savant SS. Autologous miniature punch skin grafting in stable vitiligo. Indian J. Dermatol. Venereol. Leprol.58, 310–314 (1992).
- Malakar S, Dhar S. Treatment of stable and recalcitrant vitiligo by autologous miniature punch grafting: a prospective study of 1000 patients. Dermatology198, 133–139 (1999).
- Kistala U. Suction Blister device for separation of viable epidermis from dermis. J. Invest. Dermatol.50, 129–137 (1968).
- Falabella R. Epidermal grafting. An original technique and its application in achromic and granulating areas. Arch. Dermatol.104, 592–600 (1971).
- Falabella R. Repigmentation of leukoderma by autologous epidermal grafting. J. Dermatol. Surg. Oncol.10, 136–144 (1984).
- Koga M. Epidermal grafting using the tops of suction blisters in the treatment of vitiligo. Arch. Dermatol.124, 1656–1658 (1988).
- Mutalik S. Transplantation of melanocytes by epidermal grafting. An Indian experience. J. Dermatol. Surg. Oncol.19, 231–234 (1993).
- Gupta S, Shroff S. Modified technique of suction blistering for epidermal grafting in vitiligo. Int. J. Dermatol.38, 306–309 (1999).
- Gupta S, Kumar B. Epidermal grafting in vitiligo: influence of age, site of lesion, and type of disease on outcome. J. Am. Acad. Dermatol.104, 99–104 (2003).
- Kahn AM, Cohen MJ. Vitiligo: treatment by dermabrasion and epithelial sheet grafting. J. Am. Acad. Deramatol.33, 646–648 (1995).
- Agrawal K, Agrawal A. Vitiligo: repigmentation with dermabrasion and thin split-thickness skin grafts. Dermatol. Surg.43, 273–274 (1995).
- Falabella R. Transplantation of in vitro-cultured epidermis bearing melanocytes for repigmenting vitiligo. J. Am. Acad. Dermatol.21, 257–264 (1989).
- Olsson MJ, Juhlin L. Repigmentation of vitiligo by transplantation of cultured autologous melanocytes. Acta Derm. Venereol.73, 49–51 (1993).
- Chen YF, Yang PY, Hu DN. Treatment of vitiligo by transplantation of cultured pure melanocyte suspension: analysis of 120 cases. J. Am. Acad. Dermatol.51, 68–74 (2004).
- Pianigiani E, Risulo M, Andreassi A, Taddeucci P, Ierardi F, Andreassi L. Autologous epidermal cultures and narrow-band ultraviolet B in the surgical treatment of vitiligo. Dermatol. Surg.31, 155–159 (2005).
- Gauthier Y, Surleve-Bazeille JE. Autologous grafting with noncultured melanocytes: a simplified method for treatment of depigmented lesions. J. Am. Acad. Dermatol.26, 191–194 (1992).
- Olsson MJ, Juhlin L. Leucoderma treated by transplantation of a basal layer enriched suspension. Br. J. Dermatol.138, 644–648 (1998).
- Mulekar SV. Long-term follow-up study of segmental and focal vitiligo treated by autologous noncultured melanocyte–keratinocyte cell transplantation. Arch. Dermatol.140, 1213–1215 (2004).
- Mulekar SV, Ghwish B, Al Issa A, Al Eisa A. Treatment of vitiligo lesions by ReCell vs conventional melanocyte–keratinocyte transplantation: a pilot study. Br. J. Dermatol.158, 45–49 (2008).
- Van Geel N, Ongenae K, De Mil M, Naeyaert JM. Modified technique of autologous noncultured epidermal cell transplantation for repigmenting vitiligo: a pilot study. Dermatol. Surg.27, 873–876 (2001).
- Chen YF, Chang JS, Yang PY, Hung CM, Huang MH, Hu DN. Transplant of cultured autologous pure melanocytes after laser-abrasion for the treatment of segmental vitiligo. J. Dermatol.27, 434–439 (2000).
- Guerra L, Primavera G, Raskovic D et al. Erbium:Yag laser and cultured epidermis in the surgical therapy of stable vitiligo. Arch. Dermatol.139, 1303–1310 (2003).
Surgical management of vitiligo
To obtain credit, you should first read the journal article. After reading the article, you should be able to answer the following, related, multiple-choice questions. To complete the questions and earn continuing medical education (CME) credit, please go to http://www.medscapecme.com/journal/expertderm. Credit cannot be obtained for tests completed on paper, although you may use the worksheet below to keep a record of your answers. You must be a registered user on Medscape.com. If you are not registered on Medscape.com, please click on the New Users: Free Registration link on the left hand side of the website to register. Only one answer is correct for each question. Once you successfully answer all post-test questions you will be able to view and/or print your certificate. For questions regarding the content of this activity, contact the accredited provider, [email protected]. For technical assistance, contact [email protected]. American Medical Association’s Physician’s Recognition Award (AMA PRA) credits are accepted in the US as evidence of participation in CME activities. For further information on this award, please refer to http://www.ama-assn.org/ama/pub/category/2922.html. The AMA has determined that physicians not licensed in the US who participate in this CME activity are eligible for AMA PRA Category 1 Credits™ Through agreements that the AMA has made with agencies in some countries, AMA PRA credit is acceptable as evidence of participation in CME activities. If you are not licensed in the US and want to obtain an AMA PRA CME credit, please complete the questions online, print the certificate and present it to your national medical association.
Activity Evaluation: Where 1 is strongly disagree and 5 is strongly agree
1. Which of the following variables predicts a better response to surgical treatment for vitiligo?
□ A Location on the palms or fingers versus the trunk
□ B Lip–tip vitiligo versus segmental vitiligo
□ C Type II skin vs type IV–VI skin
□ D Depigmented lesions versus hypopigmented lesions
2. Which of the following statements about minigrafting for vitiligo is most accurate?
□ A Cobblestoning is the most common adverse event associated with minigrafting
□ B Punch grafting generally requires specialized and expensive equipment
□ C Postoperative phototherapy should be avoided in minigrafting
□ D The graft samples are generally placed 1–3 mm apart
3. Which of the following statements about epidermal and split-skin grafting for vitiligo is most accurate?
□ A Blisters can be harvested within 15 minutes during epidermal grafting
□ B Epidermal grafting is associated with prominent scars
□ C Split-skin grafting should only be used to treat small areas of skin
□ D The development of milia is the most common side effect of split-skin grafting
4. Which of the following statements about cellular grafting in the treatment of vitiligo is most accurate?
□ A Pinpoint bleeding of the donor site is a sign that dermabrasion has been too aggressive
□ B Absolute immobilization is required after cellular grafting
□ C Noncultured cellular transplants have been associated with good long-term results
□ DIn vitro cultured cellular transplants are now widely available