CHD: Coronary heart disease.
Heart failure (HF) is a common cause of morbidity and mortality with a 20% incidence after age 40 years Citation[1]. As treatments for HF improve, patients will live longer and accumulate more age-related comorbidities such as dementia and diabetes. A common ‘age-related’ comorbidity is osteoporosis, affecting one in four women and one in eight men over the age of 50 years Citation[2]. The only clinical consequences of osteoporosis are fractures (typically the ‘major’ osteoporotic fractures of spine, proximal humerus, distal radius and hip), but fractures can lead to substantial impairments in quality of life, loss of independence and increased morbidity and mortality Citation[2]. Given the increased prevalence of both diseases with age, it is not surprising that HF and osteoporosis commonly coexist. Recent work, however, suggests this coexistence occurs more commonly than age and chance would dictate and there is increasing interest in the associations between HF and osteoporosis. In this article, we describe the studies supporting this association, explore potential epidemiologic and pathophysiologic links between HF and osteoporosis, and consider the clinical implications of this relationship.
Fractures are common in HF
A US cohort study of approximately 6000 community-dwelling subjects followed for 12 years reported a 10% incidence of hip fracture in HF patients Citation[3] and a Canadian cohort study of approximately 45,000 subjects followed for 10 years reported a 10% incidence of major osteoporotic fractures in HF patients Citation[4]. In another Canadian study, restricted to approximately 16,000 older patients with cardiovascular disease, we noted a 1-year incidence of major fracture of 5% Citation[5], and among 600 HF patients followed in a specialty clinic we found at least 12% had a chest radiograph documenting moderate-to-severe vertebral compression fractures Citation[6].
HF is independently associated with fractures
Low bone mineral density (BMD) is the strongest single predictor of osteoporotic fractures and is present in up to 50% of HF patients Citation[7]. Beyond this, HF itself seems to be an independent risk factor for fracture. In a cohort of approximately 30,000 twins followed for 40 years, Sennerby et al. illustrated that the risk of hip fracture was significantly elevated in twins with a diagnosis of HF compared to those without, and this association remained after adjustment for traditional osteoporotic risk factors (adjusted odds ratio [OR]: 4.4; 95% CI: 3.43–5.63) Citation[8]. Indeed, these investigators suggested that genetic endowment explained much of the association between fracture and HF and the risk with HF was greater than for other cardiovascular diseases Citation[8]. In a Canadian population-based administrative cohort study, we compared approximately 16,000 patients with new HF to approximately 14,000 patients with other non-HF cardiovascular diagnoses and demonstrated that HF patients had an adjusted fourfold increased risk for any fracture (4.6 vs 1.0% for controls) and sixfold risk for hip fracture Citation[5]. An observational study from Minnesota (USA) revealed that HF patients were at increased risk of fracture both before (adjusted OR: 1.39; 95% CI: 1.07–1.81) and after (adjusted OR: 1.32; 95% CI: 0.98–1.79) a diagnosis of HF Citation[9]. Unfortunately, none of these studies had BMD data, and to our knowledge there is only one study that has attempted to look at this. In a cohort study of approximately 46,000 patients, all of whom BMD tests were carried out on, we found that BMD was already significantly lower at both the hip and spine in patients with incident HF compared with non-HF controls Citation[4]. In that study, we also showed a 30% increase (adjusted HR 1.28; 95% CI: 1.06–1.53) in the risk of major osteoporotic fracture with HF that was independent of sociodemographic variables, comorbidities, traditional osteoporosis risk factors, medications and BMD Citation[4].
Explaining the associations between HF & osteoporosis
Shared etiologic risk factors
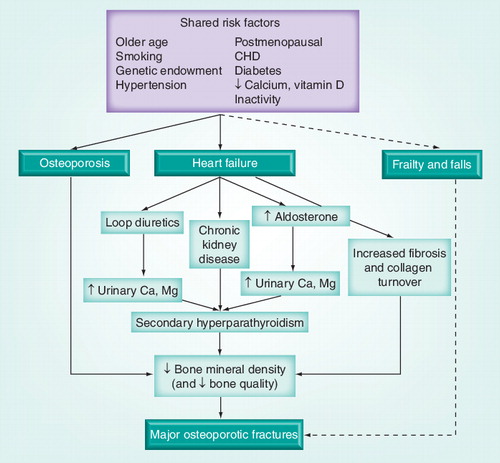
Discovering why HF patients have increased rates of osteoporotic fractures is a key question and several possible explanations exist . Common etiologic risk factors for both HF and osteoporosis include likely culprits such as older age, female sex, postmenopausal status, hypertension, diabetes and smoking. That being said, previous studies have suggested HF is an independent risk factor for fracture despite adjustment for variables representing shared risk Citation[4,5,8,9].
Frailty & falls
Frailty can be defined as three or more of the following: unintentional weight loss, self-reported exhaustion, weak grip strength, slow walking speed, and low physical activity Citation[3]. The phenotype of frailty is common in both HF and osteoporosis and may also help explain the link between the two conditions. Frail adults are at increased risk of both falls and fractures Citation[10] and HF patients are at substantially greater risk of frailty than their non-HF counterparts (e.g., adjusted OR: 7.51; 95% CI: 4.66–12.12 in one study) Citation[11]. In the most rigorous study to examine frailty and fractures in HF (a prospective cohort of ∼6000 subjects), Carbone and colleagues showed that adjustment for frailty and osteoporosis risk factors markedly attenuated but did not abolish the association between HF and hip fracture (adjusted OR: 1.59; 95% CI: 0.93–2.72 in men; adjusted OR: 1.41; 95% CI: 0.98–2.32 in women) Citation[3].
Heart failure-related treatments
Medications used to treat HF may also play a role, particularly loop diuretics since they promote calciuresis and lower BMD and also predispose to falls because of orthostasis Citation[12]. Some studies suggest warfarin increases fracture risk, but most other HF treatments (angiotensin-converting enzyme inhibitors, angiotensin-receptor blockers, β-blockers, nitrates, statins, spironolactone, thiazide diuretics) actually decrease fracture risk Citation[13–15]. Regardless, HF patients remain at increased fracture risk even after adjustment for such medications Citation[3–5].
Intersecting biological pathways
Various biological pathways may play a role in the HF–osteoporosis link, although low bone mass (and low bone quality) tend to be the final common pathway leading to fracture . For example, vitamin D is key to bone health and its levels are often low in HF Citation[16]. Elevated markers of fibrosis and collagen formation and degradation are common in HF and these same biomarkers have been linked to increased risk of fracture Citation[17]. A condition unique to HF patients that may lead to fractures is hyperaldosteronism. In animal models, hyperaldosteronism leads to low BMD via magnesium and calcium wasting in the urine with subsequent (secondary) hyperparathyroidism Citation[18]. Furthermore, in one US case–control study among male veterans with HF, those treated with the aldosterone antagonist spironolactone were significantly less likely to fracture compared to those not treated with spironolactone (adjusted OR: 0.58; 95% CI: 0.35–0.96) Citation[15]. If this finding can be replicated, it suggests that spironolactone or other aldosterone antagonists may play a role in the management of osteoporosis and it opens up further avenues of inquiry for scientists.
Future research
Future studies should focus on mechanisms for why HF and osteoporosis frequently coexist. Is it an independent association or just mediated by low BMD? The same could be said for frailty (and falls) and this needs to be studied in HF patients. Future studies should include a range of biomarkers (i.e., vitamin D, markers of fibrosis or collagen turnover and bone turnover, aldosterone, parathyroid hormone, CRP, TNF, and so on) and bone biopsy and bone imaging studies to explore and understand how the various pathways interact. This might even lead to the development of new treatment targets in osteoporosis. Last, medications used to treat HF, such as loop diuretics and spironolactone, need to be understood and examined in the context of bone health and fracture risk.
Managing the osteoporosis care-gap in HF
Regardless of the underlying reasons, fractures are very common in HF and represent avoidable morbidity and mortality. Unfortunately, osteoporosis is an under-recognized and under-treated disease. In our cohort study of approximately 600 patients followed within a specialized HF clinic, only 15% of those with moderate-to-severe vertebral compression fractures were on any prescription osteoporosis treatments Citation[6]. We believe the first step in dealing with this care-gap is to make physicians, particularly cardiologists specializing in HF and primary care physicians, aware of how commonly HF and osteoporosis occur together. Given that treatment with medications such as the bisphosphonates can reduce future fractures by 50% Citation[19], we believe that older patients with HF should be clinically risk stratified (e.g., using FRAX or related instruments) and that most HF patients over the ages of 50–60 years should be considered for BMD testing. Furthermore, because HF patients undergo many chest radiographs, they are essentially ‘screened’ (to some degree) for silent vertebral fractures and we therefore suggest that those reporting and reviewing these films ought to pay attention to more than just the heart and lungs Citation[6].
Conclusion
HF and osteoporosis-related fractures are strongly associated with each other, and the totality of evidence suggests to us that this association is independent of shared etiologic risk factors, genetic endowment, frailty, medications and low BMD. Much work remains to be carried out to understand these relationships, but in the meantime, patients with HF are at very high risk of future fracture – and should be screened and managed as such.
Financial & competing interests disclosure
SR Majumdar is supported by a Health Scholar Salary Award from the Alberta Heritage Foundation for Medical Research and Alberta Innovates-Health Solutions. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
No writing assistance was utilized in the production of this manuscript.
References
- Lloyd-Jones D, Adams R, Carnethon M et al. For the American heart association statistics committee and stroke statistics subcommittee. Heart disease and stroke statistis-2009 update: a report from the American heart association statistics committee and stroke statistics subcommittee. Circulation119(3), e21–e181 (2009).
- Papaioannou A, Morin S, Cheung AM et al. For the Scientific advisory council of osteoporosis Canada. 2010 clinical practice guidelines for the diagnosis and management of osteoporosis in Canada: summary. CMAJ182(17), 1864–1873 (2010).
- Carbone L, Buzkova P, Fink HA et al. Hip fractures and heart failure: findings from the cardiovascular health study. Eur. Heart J.31(1), 77–84 (2010).
- Majumdar SR, Ezekowitz JA, Lix LM, Leslie LM. Heart failure is a clinically and densitometrically independent and novel risk factor for major osteoporotic fractures: population-based cohort of 45509 subjects. J. Bone Miner. Res.26(Suppl. 1), S10 (2011).
- Van Diepen S, Majumdar SR, Bakal JA, McAlister FA, Ezekowitz JA. Heart failure is a risk factor for orthopedic fracture: a population-based analysis of 16294 patients. Circulation118(19), 1946–1952 (2008).
- Lyons K, Majumdar SR, Ezekowitz JA. The unrecognized burden of osteoporosis-related vertebral fractures in patients with heart failure. Circ. Heart Fail.4(1), 419–424 (2011).
- Shane E, Mancini D, Aaronson K et al. Bone mass, vitamin D deficiency, and hyperparathyroidism in congestive heart failure. Am. J. Med.103(3), 197–207 (1997).
- Sennerby U, Melhus H, Gedeborg R et al. Cardiovascular diseases and risk of hip fracture. JAMA302(15), 1666–1673 (2009).
- Gerber Y, Melton LJ, Weston SA, Roger VL. Osteoporotic fractures and heart failure in the community. Am. J. Med.124(5), 418–425 (2011).
- Rolland Y, Abellan Van Kan G, Benetos A et al. Frailty, osteoporosis and hip fracture: causes, consequences and therapeutic perspectives. J. Nutr. Health Aging12(5), 335–346 (2008).
- Newman AB, Gottdiener JS, McBurnie MA et al. Associations of subclinical cardiovascular disease with frailty. J. Gerontol. A. Biol. Med. Sci.56(3), M156–M166 (2001).
- Lim LS, Fink HA, Kuskowski MA et al. Loop diuretic use and increased rates of hip bone loss in older men: the osteoporotic fractures in men study. Arch. Intern. Med.168(7), 735–740 (2008).
- Wiens M, Etminan M, Gill SS, Takkouche B. Effects of antihypertensive drug treatments on fracture outcomes: a meta-analysis of observation studies. J. Intern. Med.260(4), 350–362 (2006).
- Rejnmark L, Vestergaard P, Mosekilde L. Decreased fracture risk in users of organic nitrates: a nationwide case-control study. J. Bone Miner. Res.21(11), 1811–1817 (2006).
- Carbone LD, Cross JD, Raza SH et al. Fracture risk in men with congestive heart failure: Risk reduction with spironolactone. 52(2), 135–138 (2008).
- Pilz S, Tomaschitz A. Vitamin D status: to be considered in heart failure patients! Eur. J. Heart Fail.13(6), 595–596 (2011).
- Barasch E, Gottdiener JS, Aurigemma G et al. Association between elevated fibrosis markers and heart failure in the elderly: the cardiovascular health study. Circ. Heart Fail.2(4), 202–310 (2009).
- Chhokar VS, Sun Y, Bhattacharya SK et al. Hyperparathyroidism and the calcium paradox of aldosteronism. Circulation111(7), 871–878 (2005).
- Maclean C, Newberry S, Maglione M et al. Systematic review: comparative effectiveness of treatments to prevent fractures in men and women with low bone density or osteoporosis. Ann. Intern. Med.148(3), 197–213 (2008).