Abstract
Pancreatic cancer continues to be a diagnostic and therapeutic challenge. The advent of endoscopic ultrasound-guided interventions have brought about a paradigm shift in the endoscopic approach to diagnosis, treatment and palliation of this common malignancy. The last decade has witnessed significant advances in techniques of endoscopic biliary drainage, endoluminal stenting, celiac plexus neurolysis and image-guided radiation therapy, which have transformed the scope of palliation in pancreatic cancer. Moreover, endoscopic ultrasound-aided intratumoral delivery of fiducials, radioisotopes and chemotherapeutic agents have shown promising results and warrant further investigation. This review summarizes the recent advances in endoscopic applications for the management of pancreatic neoplasms.
Medscape: Continuing Medical Education Online
This activity has been planned and implemented in accordance with the Essential Areas and policies of the Accreditation Council for Continuing Medical Education through the joint sponsorship of Medscape, LLC and Expert Reviews Ltd. Medscape, LLC is accredited by the ACCME to provide continuing medical education for physicians.
Medscape, LLC designates this Journal-based CME activity for a maximum of 1 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
All other clinicians completing this activity will be issued a certificate of participation. To participate in this journal CME activity: (1) review the learning objectives and author disclosures; (2) study the education content; (3) take the post-test with a 70% minimum passing score and complete the evaluation at www.medscape.org/journals/expertgastrohep; (4) view/print certificate.
Release date: December 9, 2011; Expiration date: December 9, 2012
Learning objectives
• Compare different imaging modalities in the diagnosis and staging of pancreatic cancer
• Evaluate the use of EUS and endoscopic retrograde cholangiopancreatography in obtaining the tissue diagnosis of pancreatic cancer
• Analyze the role of EUS in the treatment of pancreatic cancer
• Assess how EUS may be used in palliative procedures for pancreatic cancer
Financial & competing interests disclosure
EDITOR
Elisa Manzotti,Editorial Director, Future Science Group, London, UK
Disclosure:Elisa Manzotti has disclosed no relevant financial relationships.
CME AUTHOR
Charles P Vega, MD,Health Sciences Clinical Professor; Residency Director, Department of Family Medicine, University of California, Irvine, CA, USA
Disclosure:Charles P Vega has disclosed no relevant financial relationships.
AUTHORS
Shounak Majumder, MD,Resident, Internal Medicine, University of Connecticut Health Center, 263 Farmington Avenue, Farmington, CT 06030-3229, USA
Disclosure:Shounak Majumder has disclosed no relevant financial relationships.
Saman Chubineh, MD,Fellow, Gastroenterology, University of Connecticut Health Center, 263 Farmington Avenue, Farmington, CT 06030-3229, USA
Disclosure:Saman Chubineh has disclosed no relevant financial relationships.
John Birk, MD,Associate Professor of Medicine; Chief of Gastroenterology, University of Connecticut Health Center, 263 Farmington Avenue, Farmington, CT 06030-3229, USA
Disclosure:John Birk has disclosed no relevant financial relationships.
Worldwide, pancreatic cancer is the fourth leading cause of cancer-related death in men and the fifth leading cause in women, with an approximate incidence of ten per 100,000 population per year Citation[1]. There has been no appreciable change in the epidemiology of this disease in the past few decades. With the USA recording more than 30,000 deaths in 2008, a number that is almost equal to reported incidence, pancreatic cancer continues to be a diagnostic and therapeutic challenge. The prognosis of pancreatic cancer is dismal, with postoperative 5-year survival rates varying from 3 to 25% Citation[2,3]. Nearly two-thirds of patients with resectable tumors develop local recurrence within 2 years of surgery Citation[4]. The disease is often advanced at presentation and nearly 90% of patients have inoperable disease at the time of diagnosis, with a median survival of approximately 4 months without treatment Citation[3]. In patients with advanced unresectable disease, chemotherapy, radiation or a combination of both may positively influence overall survival and quality of life Citation[5]. Endoscopic intervention is often an integral component of palliation in these patients. Now, with the emerging therapeutic spectrum of endoscopic ultrasound (EUS), endoscopy has even more important in the management of patients with inoperable disease. This article focuses on the role of endoscopy in the diagnosis, staging and treatment of pancreatic malignancy.
Diagnosis & staging of pancreatic cancer
Multiple-imaging modalities are often used in combination in the diagnosis and staging of pancreatic cancer. Commonly used imaging techniques include transabdominal ultrasound, computed tomography (CT), MRI, endoscopic retrograde cholangiopancreatography (ERCP) and EUS. Transabdominal ultrasound with and without contrast-enhancement provides a sensitivity of 86–89% and diagnostic accuracy of approximately 82–86% for diagnosing malignant pancreatic head tumors Citation[6]. Visualization of other regions of the pancreas is often obscured by intestinal gas and is not always reliable. Currently, dynamic contrast-enhanced CT with thin (1 mm) sections is the preferred modality for preoperative staging and assessing resectability in patients with pancreatic cancer. With reported sensitivities ranging from 63 to 92%, CT is an invaluable imaging tool in malignant diseases of the pancreas. Pancreatic MRI is comparable to CT with a sensitivity of detecting pancreatic cancer ranging from 88 to 96% Citation[7]. A recent study demonstrated that multislice CT and MRI had comparable diagnostic accuracy, with no statistically significant differences between the two with regards to either tumor identification or resectability Citation[7]. Moreover, combining the two modalities does not improve diagnostic yield in equivocal cases. CT and MRI have also been shown to be similarly accurate in the detection of small solid pancreatic tumors that are less than 2 cm Citation[8].
EUS for diagnosis & staging
EUS imaging of the pancreas has the inherent advantage of a high-frequency transducer placed in close proximity to the tumor resulting in high-resolution images. In a recent systematic review highlighting the accuracy of EUS compared with CT in the preoperative assessment of pancreatic cancer, Dewitt et al. evaluated 11 studies involving 678 patients Citation[9]. Nine out of 11 studies analyzed tumor detection, and uniformly concluded that the sensitivity of EUS was higher than CT. In this report, EUS appeared to be superior to CT for detecting tumors smaller than 3 cm in diameter Citation[10]. A study evaluating the accuracy of EUS, CT and MRI in the detection of pancreatic tumors less than 2 cm in diameter reported sensitivities of 90, 40 and 33%, respectively Citation[11]. However, most studies comparing EUS and CT are based on older generation scanners and hence underestimate the diagnostic accuracy of CT. The introduction of higher resolution multidetector CT coupled with the development of 3D imaging techniques is expected to improve the CT accuracy for detecting pancreatic tumors, and studies comparing EUS to multidetector CT for small pancreatic tumors are awaited.
Irrespective of the imaging modality used, the staging of pancreatic cancer follows the Tumor, Node, Metastasis (TNM) system proposed by the American Joint Committee on Cancer (AJCC). Although surgical and histopathological TNM staging continues to be the ‘gold standard’ for staging pancreatic tumors, imaging provides important information regarding regional lymph node involvement and vascular invasion, which are key factors in deciding preoperative resectability in the absence of distant metastatic disease.
Results of staging accuracy with EUS have been variable. Earlier studies reported a T-staging accuracy range of 74–95% Citation[10]. More recent data reflect a lower accuracy of 62–79% Citation[10]. However, the studies are not comparable as the T-staging for pancreatic cancer has changed twice in recent years: once in 1997, which added a T4 stage, and also in 2002, when portal venous invasion was reclassified as T3, bringing it within the realms of potential resectability. Even with the most recent TNM system, EUS has been found to be superior to multidetector CT for T-staging Citation[12]. In a recent study, although EUS had slightly lower overall staging accuracy compared with helical CT (40 vs 46%), it was associated with a lower risk of overstaging compared with both CT and MRI (5 vs 8 and 7%) Citation[13]. This is of paramount clinical relevance in patients with pancreatic cancer as overstaging may rule out a potentially beneficial resection. Although the same study also stated that EUS had a significantly higher positive and negative predictive value for nodal involvement compared with helical CT or MRI, this finding has not been corroborated in other studies, which have found helical or multidetector CT to be equivalent to EUS for N-staging Citation[12,14]. Moreover, two recent studies found no difference between CT and EUS in predicting resectability Citation[12,14].
With the widespread availability of multidetector CT, which provides a more complete assessment of vascular invasion, distant metastasis and resectability, it is more often the initial imaging test for staging purposes. EUS may be used for nodal assessment in patients with equivocal CT scans and for further characterization of small solid tumors detected on CT.
Role of ERCP in the diagnosis of pancreatic cancer
With the widespread use and growing experience with EUS and helical CT, there is currently no clinical role of ERCP in the diagnosis and staging of pancreatic cancer. Certain signs however, deserve special mention due to their significant association with a detection of pancreatic cancer. The presence of combined dilatation of the bile duct and the pancreatic duct due to a focal obstruction in close continuity (double-duct sign) is considered pathognomonic of a pancreatic head mass. Other features that raise suspicion for malignant disease on ERCP include an abrupt cutoff of the main pancreatic duct or a solitary, long stricture (>1 cm) in the pancreatic duct. However, none of these findings are specific because they may also be observed in chronic pancreatitis.
Tissue sampling for cytological diagnosis of pancreatic tumors
Of the various techniques currently available for cytological diagnosis of pancreatic malignancy, fine-needle aspiration (FNA) and brush cytology are the two most commonly used in clinical practice. The endoscopic approaches for both are considered to have the best yield.
EUS-FNA
FNA is usually either CT-guided or EUS-guided (EUS-FNA). In the early EUS era, imaging was performed using a radial-arrayed EUS, which was unsuitable for EUS-FNA. However, the widespread availability of linear EUS has, in recent years, enabled endoscopists to obtain detailed images and perform EUS-FNA as a one stage procedure Citation[15]. The reported specificity and sensitivity of EUS-FNA is 98 and 85%, respectively, resulting in a positive predictive value close to 100%, but a low negative predictive value Citation[16,17]. Hence, a positive result is reliable but a negative result does not rule out pancreatic cancer. Patients with nondiagnostic results on percutaneous CT-guided biopsy may benefit from EUS-FNA, which has a higher sensitivity Citation[18]. In a recent randomized prospective trial comparing sensitivity of CT-guided FNA and EUS-FNA, EUS-FNA had higher sensitivity (84 vs 62%) but the difference was not statistically significant Citation[19]. EUS-FNA is especially useful for tumors less than 3 cm, which are difficult to identify and target on ultrasound or CT. EUS-FNA is a safe procedure with complication rates as low as 1.1%, even in newer centers with less-experienced operators Citation[20]. Commonly reported complications include bleeding (1–4%), pancreatitis (1–2%) and perforation (0.03%) with a cumulative incidence of less than 3% Citation[21]. In a prospective study of EUS-FNA in 355 patients with solid pancreatic mass, three patients developed pancreatitis and three patients developed post-procedure abdominal pain of unclear etiology that required short inpatient stay and responded to analgesics. Although 2.54% of patients developed complications only 1.9% required hospitalization Citation[22]. None of the patients had perforation or clinically significant bleeding and no specific risk factors could be delineated.
ERCP brush cytology
Biliary brush cytology is a commonly performed technique for sampling tissue during ERCP. Although several other techniques carried out during ERCP, such as cytology of aspirated bile, retrieved stents and endobiliary forceps biopsy have been described, none of these techniques yields a higher detection rate compared with brush cytology alone and are usually more time consuming and technically challenging Citation[23]. Brush cytology has a low sensitivity in the range of 30–60%; however, a positive test has a high positive predictive value Citation[24]. The technique of obtaining multiple brush specimens before and after stricture dilatation improves sensitivity Citation[25]. Some even advocate sending the entire brush for cytological analysis to improve diagnostic yield. Biliary brush specimens should always be obtained during stricture dilatation in patients with suspected pancreatic malignancy. Of note, recent studies suggest that cholangioscopy with guided biopsies had a high diagnostic accuracy (82%) of differentiating malignant from benign lesions in patients with biliary stricture and inconclusive results on brush cytology Citation[26].
Endoscopy therapeutic strategies
The advent of interventional EUS has brought about another paradigm shift in the endoscopic armamentarium for management of pancreatic cancer. Using a curvilinear echoendoscope placed in the stomach or duodenum, EUS offers access to lesions in different parts of the pancreas, including anatomical regions that are difficult to approach percutaneously. The benefits of EUS in pancreatic cancer, which was initially limited to staging and tissue sampling, has now diversified to include EUS-fine-needle injection (FNI) for celiac plexus neurolysis (CPN), biliary drainage, tumor ablation, injection of chemotherapy agents and deployment of gold fiducials to aid radiation therapy (Box 1). The endoscopic approach using a standard endoscope and during ERCP can also be utilized for endoluminal stenting and biliary drainage.
Celiac plexus block
Pain control is a major therapeutic goal in the palliative care of pancreatic cancer patients. However, pain relief is often an elusive goal and persistent pain may adversely affect the disease course Citation[27]. More than 75% of patients complain of pain at presentation and the prevalence increases to more than 90% as the disease advances Citation[28]. Ablation of the celiac plexus using ethanol and an analgesic (bupivacaine) is a safe pain-control technique with proven efficacy. The use of alcohol as injectate is restricted to patients with pancreatic cancer. Although traditionally performed under radiological guidance using a posterior percutaneous approach, the advent of linear array echoendoscope has allowed for an anterior approach EUS-guided CPN. A recent meta-analysis of five randomized controlled trials documented a fair response to celiac plexus blockade with an overall reduction in the visual analog pain score Citation[28]. In another pooled analysis of eight studies involving 283 patients, 80.12% (95% CI: 74.47–85.22) showed pain relief with EUS-guided CPN Citation[29]. The complication rate of EUS-CPN was reported to be less than 2% in a case series describing two procedures Citation[30]. Adverse events in that series included isolated cases of hypotension and retroperitoneal abscess and two patients with severe self-limiting post-procedure pain. Other rare complications include peripancreatic abscess and the formation of pseudoaneurysm Citation[31]. The use of an anterior endoscopic approach combined with Doppler, reduces the risk of vascular and neurological complications. A study published in early 2011 suggested that celiac ganglion neurolysis – for instance, direct EUS-aided visualization and injection into the celiac ganglion – provided superior pain control compared with injection into the celiac trunk Citation[32]. This difference was independent of tumor size and location, and patients with more severe preprocedure pain demonstrated greater benefit from the procedure. A recent systematic review that aimed to determine the efficacy and safety of CPN overall in reducing pancreatic cancer pain concluded that there is weak statistical evidence that CPN has greater efficacy compared with analgesics for pain relief in this population and is associated with significant reduction in opioid use Citation[33,34].
Biliary drainage
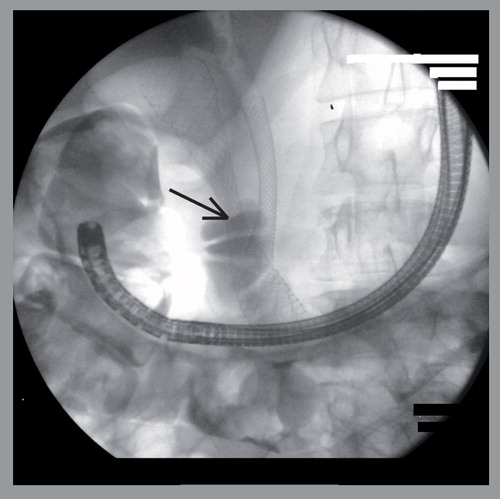
For locally advanced pancreatic cancer, treatment of bile duct obstruction is a key component of effective palliation. Traditionally accomplished by placement of stents by ERCP or percutaneous transhepatic approach, recent investigators have reported techniques of EUS-guided biliary drainage Citation[35–39]. Endobiliary stent choices are plastic or self-expanding metal stents (SEMS) . Metal stents have a longer patency rate but have the inherent disadvantage of nonremoval. They are recommended in patients with expected survival greater than 6 months Citation[40]. In a study comparing plastic and metal stents for palliation of malignant biliary obstruction, the authors concluded that adverse outcomes including cholangitis, stent occlusion and the need for emergency biliary drainage procedures were significantly higher in patients who underwent plastic stent placement (39.3 vs 11.8%; p = 0.017) Citation[41]. Comparing covered to uncovered metal stents, endurance was similar, but covered stents are less prone to obstruction, have longer patency resulting in fewer interventions, lower cumulative costs and are likely to be more effective for distal biliary obstruction Citation[42,43]. However, covered stents have a higher rate of migration, cannot be used for hilar obstruction and there is risk of stent-induced cholecystitis. While uncovered stents have the inherent advantage of being useable anywhere in the biliary tract, tumor ingrowth causing the abovementioned obstruction is a common problem and often results in ineffective long-term palliation. Although argued to the contrary in the past, preoperative biliary drainage and SEMS placement does not affect surgical outcome or overall survival Citation[44–46]. A recent multicenter randomized controlled trial demonstrated that preoperative biliary drainage was, in fact, associated with lower postoperative mortality rate (hazard ratio: 0.90; 95% CI: 0.83–0.97) Citation[45].
ERCP is technically difficult in malignant biliary obstruction and tight stricture or anatomical distortion of the duodenum and the bile duct often impedes successful deep canulation. EUS-guided biliary drainage and stenting is a viable alternative in these patients. The technique usually involves image-guided biliary puncture through the gastric or duodenal wall, followed by guidewire placement along the same tract. This is followed by a ‘rendezvous’ technique, whereby the guidewire is manipulated across the stricture and passed through the ampulla into the duodenum, followed by conventional techniques of SEMS placement. A recent study describing 49 patients with EUS-guided stenting after failed ERCP in patients with biliary stricture reported a success rate of 84% Citation[36]. There was no significant difference of success when comparing intrahepatic and extrahepatic approaches Citation[36]. However, most data on interventional EUS for biliary drainage are based on small case series which are referral center-based and may not be widely applicable.
EUS-guided choledochoduodenostomy is another recently described minimally invasive technique for biliary–enteric anastomosis Citation[46]. Few cases of EUS-guided anterograde SEMS placement have been reported in patients with pancreatic cancer and an endoscopically inaccessible biliary orifice. EUS-guided formation of biliary–enteric communication appears to be a safe and effective strategy in these preliminary reports Citation[47,48]. However, interventional EUS requires a very high degree of skill and is best performed by highly experienced operators. Although none of these novel procedures have been sufficiently standardized to attain widespread use as yet, initial data appear promising.
Enteral stenting
Pancreatic cancer is the most common cause of malignant gastroduodenal obstruction Citation[49]. Although bowel obstruction occurs in 11–20% of patients with pancreatic cancer, less than 5% present with these symptoms Citation[50]. Endoscopic placement of SEMS is now the preferred therapy in the palliation of this condition . A recent analysis that pooled results from seven studies demonstrated technical success rates of 92–100% Citation[51]. Clinical outcome parameters, variably defined as improvement in obstructive symptoms or resumption of normal diet after SEMS placement, was measured in six of the seven studies. Five of these studies reported favorable outcome in 81–92% of cases Citation[51]. One of the studies reported a lower clinical success rate of 75%, but was limited by inclusion of patients since 1991, when SEMS were not specifically designed for enteral deployment Citation[52]. The two most recent studies included in this analysis reported technical success of greater than 98% and clinical efficacy of 86–90%, thereby highlighting the technical and device-related advances in endoscopic enteral stent placement Citation[53,54]. Complications range from 11 to 43% and commonly occur in the form of stent migration or reocclusion. The latter is more common in uncovered stents and can be managed by restenting through the occluded stent in most cases. Compared to surgical bypass, endoscopic enteral stenting appears to be cost-effective and associated with less procedure-related morbidity but comparable improvement in quality of life Citation[51,55]. Neither surgery nor enteral stenting has been shown to prolong survival in these patients with malignant gastric outlet obstruction.
EUS-FNI for tumor ablation & intratumoral drug delivery
Over the past few years therapeutic EUS has been utilized for intratumoral delivery of ethanol, chemotherapy drugs and novel antitumor agents. EUS-FNI has the advantages of precise real-time tumor visualization and use of Doppler signals to determine a relatively avascular injection tract.
EUS-guided ethanol, injection alone or in combination with paclitaxel has been tried in small patient groups for ablation of pancreatic cystic neoplasms. After an initial pilot study in 2005 documented safety of ethanol ablation in pancreatic cysts, a randomized controlled trial was performed comparing ethanol to saline injection Citation[56,57]. Patients in the ethanol lavage group had a greater decrease in pancreatic cyst size compared with saline solution lavage, with a comparable safety profile. A recent study involving 52 patients evaluated treatment response with sequential EUS-guided cyst aspiration and ethanol lavage followed by intra-cystic paclitaxel injection and a median post-procedure follow-up of 21 months Citation[58]. Complete resolution defined as cyst volume at final follow-up less than 5% of original volume was noted in 62% of patients and multivariate analysis revealed small cyst size to be the only independent predictor of complete resolution. Procedure-related adverse events were rare (7.6%) and included only one case of pancreatitis. Although results appear promising and technically safe, efficacy needs to be validated in larger patient groups over longer follow-up periods. EUS-guided ethanol ablation has also been used sporadically in patients with insulinoma, who are poor candidates for surgery, with good outcomes, but current guidelines do not support its use in solid pancreatic tumors Citation[59,60].
Novel agents described for use with EUS-FNI in the management of pancreatic cancer include activated lymphocyte culture, oncolytic viruses, viral vectors and immature dendritic cells Citation[61,62]. Chang et al. in 2000 was the first group to report the use of a biological agent in the treatment of pancreatic cancer using the EUS-FNI technique Citation[63]. Although their study demonstrated safety and feasibility of the technique, no follow-up data using the same agent has been reported. Another agent, TNFerade™, is a replication-deficient adenovector expressing the cDNA encoding human TNF-α gene, regulated by a radiation-inducible promoter Egr-1. Its safety was established in a Phase I trial involving 50 patients where it was used in combination with 5-fluorouracil and radiation. Percutaneous and EUS-guided FNI groups demonstrated similar results in terms of partial response and overall progression-free survival (53 vs 47%) Citation[64]. A Phase III trial is currently underway comparing patients receiving standard chemoradiation with or without TNFerade. Oncolytic attenuated adenovirus ONYX-015 and oncolytic herpes simplex virus carrying the GM-CSF gene (OncoVEXGM-CSF™) have also been used in Phase I trials of pancreatic cancer Citation[65,66]. Like most other novel agents they failed to demonstrate any significant survival benefit. The future of pancreatic cancer immunotherapy probably lies in a personalized genomic approach tailored to individual patient and tumor characteristics. EUS-FNI is a relatively safe, minimally invasive approach for direct delivery of antitumor agents, and is likely to have an expanding role in treatment of pancreatic malignancies.
EUS-guided radiation therapy
EUS has also been used for the interstitial implantation of radioactive iodine-125 seeds in a pancreatic tumor. In a recently published study involving 22 patients with a median of ten seeds placed per patient, the authors noted a significant decrease in pain during the week following brachytherapy. However, pain control was not sustained and there was no long-term survival benefit Citation[67]. The development of imaging-guided radiation therapy has been a major advancement in pancreatic cancer palliation. Unlike traditional external beam radiation, which requires target tumor immobilization, imaging-guided radiation therapy utilizes a system of real-time tumor tracking to maintain spatial precision and deliver focused radiation. Radiopaque gold fiducials placed in or near tumor tissue facilitate tumor tracking and subsequent radiation delivery. Traditionally, fiducials were deployed either during surgery or percutaneously under image-guidance. Recent reports have demonstrated the safety of EUS-guided fiducial placement in pancreatic tumors Citation[68,69]. EUS-guided submucosal injection of radioactive liquid tantalum has also been recently used for tumor identification during radiation and surgery Citation[70]. Other EUS-guided coagulative therapies described include radiofrequency ablation and photodynamic therapy Citation[71,72]. However, current data using these techniques in pancreatic cancer are mostly based on animal studies and human trials are awaited.
Expert commentary
Pancreatic cancer remains a challenging disease from both a diagnostic and therapeutic point of view. The endoscopic approach is fundamental with regards to diagnosis, staging and therapy of the tumor. Diagnosis and staging traditionally involve radiologic approaches, including CT, ultrasound and EUS, often in combination. With the advent of multidetector CT, it is now the imaging and staging modality of choice in patients with a suspected pancreatic mass. MRI confers no additional advantage beyond what is obtained with multidetector CT. EUS has proven to have greater sensitivity for 3 cm or smaller tumors and often compliments cross-sectional imaging for an accurate assessment of staging and resectability. Linear EUS also allows for tissue sampling via FNA, which has proven superior to percutaneous FNA with regards to sensitivity. With its low complication rate, and specificity close to 100%, EUS is an invaluable tool with regards to tissue diagnosis of pancreatic malignancy.
Numerous EUS interventional methods have proven useful. EUS celiac plexus ablation through ethanol or analgesic agents has proven to be a safe, effective and reliable therapy for those with pain secondary to pancreatic malignancy. Therapeutic endoscopic approaches by ERCP for biliary drainage have also proven very useful. EUS-guided biliary access can sometimes be successful after failed standard ERCP approaches. In addition, EUS-guided choledochoduodenostomy is being described as a salvage technique for biliary drainage by formation of biliary–enteric communication.
Treatment of malignant gastroduodenal obstruction through use of endoscopic placement of SEMS has also proven to be highly successful, with a reduction of obstructive symptoms and improved tolerance of diet. Although some complications exist, this method has been shown to have better tolerance in comparison to surgical procedures.
With regards to therapy aimed towards primary pancreatic lesions, EUS-guided injection of ethanol, with and without paclitaxel, initially showed promise for treatment of malignant pancreatic cysts. Decreased pancreatic cystic size and resolution were noted with minimal adverse events. This needs further assessment before being widely adopted. Therapy of solid pancreatic tumors through novel agents including biological response modifiers, TNFerade, and oncolytic attenuated adenovirus, are currently being explored and may prove beneficial. Therapy by local radiation delivered through EUS-FNI has also proven safe and useful in palliation of pancreatic cancer but again needs further evaluation. In conclusion, endoscopy has emerged and is further evolving in the treatment of this important disease.
Five-year view
Many of the EUS-guided interventions for biliary drainage are in the initial phases of clinical use. Given the inherent advantage of highly detailed anatomical visualization, we anticipate increasingly widespread use of EUS-aided intervention for biliary drainage in patients with malignant bile duct obstruction. Overall, this may reduce the need for percutanous transhepatic cholangiograms in the future. However, prospective, randomized clinical trials are required to assess their feasibility and clinical applicability. EUS-guided direct delivery of antitumoral agents including oncolytic viruses and chemotherapeutic agents has the potential for improved treatment efficacy in the future. It is possible that new emerging endoscopic techniques may provide a more accurate and early diagnosis of pancreatic cancer, especially in patients with cystic pancreatic neoplasms, thereby aiding effective treatment with improved clinical outcomes.
Diagnosis/staging
EUS
• Imaging
• Fine-needle aspiration
ERCP
• Imaging
• Brush cytology
• Biopsy
Pain control
EUS
• Celiac plexus neurolysis
• Celiac ganglion neurolysis
Biliary drainage
EUS
• Anterograde
• Rendezvous technique
• Choledochoduodenostomy
ERCP
• SEMS/plastic stent
• Rendezvous technique
Enteral stenting
SEMS deployment
Chemotherapy
EUS-guided fine-needle injection
• Chemotherapy
• Oncolytic virus
• Other agents
Radiation therapy
EUS
• Fiducials
• Photodynamic therapy
• Radiofrequency ablation
Key issues
• Worldwide, pancreatic cancer is the fourth leading cause of cancer-related death in men and the fifth leading cause in women.
• The disease is often advanced at presentation, and almost 90% of patients have inoperable disease at the time of diagnosis.
• Endoscopic ultrasound (EUS) and computer tomography-guided fine-needle aspiration have comparable diagnostic yield for large tumors, with EUS fine-needle aspiration being especially useful for tumors of less than 3 cm, which are difficult to identify and target using ultrasound or computer tomography.
• EUS-guided celiac plexus neurolysis is a safe technique with moderate efficacy for palliation of pain in advanced pancreatic cancer, and can significantly reduce opioid use.
• Preoperative drainage for malignant biliary obstruction is associated with lower postoperative mortality rate.
• Self-expanding metal stent deployment is the preferred intervention for patients with expected survival greater than 6 months and covered stents are recommended for distal bile duct obstruction.
• EUS-guided biliary stenting using the ‘rendezvous technique’ after failed endoscopic retrograde cholangiopancreatography in patients with biliary stricture has a reported success rate of 84%.
• Endoscopic placement of enteral stents has a technical success of greater than 98% and clinical efficacy of 86–90% in patients with gastroduodenal obstruction secondary to pancreatic neoplasm.
• Compared with surgical bypass, endoscopic enteral stenting appears to be cost-effective and associated with less procedure-related morbidity.
• EUS-fine-needle injection is a relatively safe, minimally invasive approach for direct delivery of antitumor agents, but clinical efficacy is yet to be established.
• Recent reports have demonstrated the safety of EUS-guided fiducial placement in pancreatic tumors for subsequent image-guided radiation therapy.
Acknowledgement
We would like to acknowledge the excellent technical support provided by Jessica Kilham.
References
- Krejs GJ. Pancreatic cancer: epidemiology and risk factors. Dig. Dis.28, 355–358 (2010).
- Stephens J, Kuhn J, O’Brien J et al. Surgical morbidity, mortality, and long-term survival in patients with peripancreatic cancer following pancreaticoduodenectomy. Am. J. Surg.174, 600–604 (1997).
- Varadarajulu S, Eloubeidi MA. The role of endoscopic ultrasonography in the evaluation of pancreatico–biliary cancer. Surg. Clin. North Am.90, 251–263 (2010).
- Büchler MW, Werner J, Weitz J. R0 in pancreatic cancer surgery: surgery, pathology, biology, or definition matters? Ann. Surg.251, 1011–1012 (2010).
- Yan BM, Van Dam J. Endoscopic ultrasound-guided intratumoural therapy for pancreatic cancer. Can. J. Gastroenterol.22, 405–410 (2008).
- Grossjohann HS, Rappeport ED, Jensen C et al. Usefulness of contrast-enhanced transabdominal ultrasound for tumor classification and tumor staging in the pancreatic head. Scand. J. Gastroenterol.45, 917–924 (2010).
- Fusari M, Maurea S, Imbriaco M et al. Comparison between multislice CT and MR imaging in the diagnostic evaluation of patients with pancreatic masses. Radiol. Med.115, 453–466 (2010).
- Rao SX, Zeng MS, Cheng WZ, Yao XZ, Jin DY, Ji Y. Small solid tumors (< or = 2 cm) of the pancreas: relative accuracy and differentiation of CT and MR imaging. Hepatogastroenterology58, 996–1001 (2011).
- Dewitt J, Devereaux BM, Lehman GA, Sherman S, Imperiale TF. Comparison of endoscopic ultrasound and computed tomography for the preoperative evaluation of pancreatic cancer: a systematic review. Clin. Gastroenterol. Hepatol.4, 717–725 (2006).
- Owens DJ, Savides TJ. Endoscopic ultrasound staging and novel therapeutics for pancreatic cancer. Surg. Oncol. Clin. N. Am.19, 255–266 (2010).
- Muller MF, Meyenberger C, Bertschinger P et al. Pancreatic tumors: evaluation with endoscopic US, CT, and MR imaging. Radiology190, 745–751 (1994).
- DeWitt J, Devereaux B, Chriswell M et al. Comparison of endoscopic ultrasonography and multidetector computed tomography for detecting and staging pancreatic cancer. Ann. Intern. Med.16, 753–763 (2004).
- Soriano A, Castells A, Ayuso C et al. Preoperative staging and tumor resectability assessment of pancreatic cancer: prospective study comparing endoscopic ultrasonography, helical computed tomography, magnetic resonance imaging, and angiography. Am. J. Gastroenterol.99, 492–501 (2004).
- Ramsay D, Marshall M, Song S et al. Identification and staging of pancreatic tumours using computed tomography, endoscopic ultrasound and mangafodipir trisodium-enhanced magnetic resonance imaging. Australas. Radiol.48, 154–161 (2004).
- Irisawa A. Current role of radial and curved-linear arrayed EUS scopes for diagnosis of pancreatic abnormalities in Japan. Dig. Endosc.23(Suppl. 1), 9–11 (2011).
- Hawes RH, Fockens P (Eds). Endosonography. Saunders Elsevier, Philadelphia, PA, USA (2006).
- Buscail L, Faure P, Bournet B et al. Interventional endoscopic ultrasound in pancreatic diseases. Pancreatology6, 7–16 (2006).
- Harewood GC, Wiersema MJ. Endosonography-guided fine needle aspiration biopsy in the evaluation of pancreatic masses. Am. J. Gastroenterol.97, 1386–1391 (2002).
- Horwhat JD, Paulson EK, McGrath K et al. A randomized comparision of EUS-guided FNA versus CT or US-guided FNA for the evaluation of pancreatic mass lesions. Gastrointest. Endosc.63, 966–975 (2006).
- Eloubeidi MA, Tamhane A. Prospective assessment of diagnostic utility and complications of endoscopic ultrasound-guided fine needle aspiration. Results from a newly developed academic endoscopic ultrasound program. Dig. Dis.26, 356–363 (2008).
- Adler DG, Jacobson BC, Davila RE et al. ASGE guideline: complications of EUS. Gastrointest. Endosc.61, 8–12 (2005).
- Eloubeidi MA, Tamhane A, Varadarajulu S, Wilcox CM. Frequency of major complications after EUS-guided FNA of solid pancreatic masses: a prospective evaluation. Gastrointest. Endosc.63, 622–629 (2006).
- Pausawasdi N, Scheiman J. Endoscopic evaluation and palliation of pancreatic adenocarcinoma: current and future options. Curr. Opin. Gastroenterol.23, 515–521 (2007).
- De Bellis M, Sherman S, Fogel EL et al. Tissue sampling at ERCP in suspected malignant biliary strictures (part 2). Gastrointest. Endosc.56, 720–730 (2002).
- Ornellas LC, Santos Gda C, Nakao FS, Ferrari AP. Comparison between endoscopic brush cytology performed before and after biliary stricture dilation for cancer detection. Arq. Gastroentero.43, 20–23 (2006).
- Ramchandani M, Reddy DN, Gupta R et al. Role of single-operator peroral cholangioscopy in the diagnosis of indeterminate biliary lesions: a single-center, prospective study. Gastrointest. Endosc.74, 511–519 (2011).
- Lillemoe KD, Cameron JL, Kaufman HS et al. Chemical splanchnicectomy in patients with unresectable pancreatic cancer, a prospective randomized trial. Ann. Surg.217, 447–457 (1993).
- Yan BM, Myers RP. Neurolytic celiac plexus block for pain control in unresectable pancreatic cancer. Am. J. Gastroenterol.102, 430–438 (2007).
- Puli SR, Reddy JB, Bechtold ML, Antillon MR, Brugge WR. EUS-guided celiac plexus neurolysis for pain due to chronic pancreatitis or pancreatic cancer pain: a meta-analysis and systematic review. Dig. Dis. Sci.54, 2330–2337 (2009).
- O’Toole TM, Schmulewitz N. Complication rates of EUS-guided celiac plexus blockade and neurolysis: results of a large case series. Endoscopy41, 593–597 (2009).
- Levy MJ, Wiersema MJ. EUS-guided celiac plexus neurolysis and celiac plexus block. Gastrointest. Endosc.57, 923–930 (2003).
- Ascunce G, Ribeiro A, Reis I et al. EUS visualization and direct celiac ganglia neurolysis predicts better pain relief in patients with pancreatic malignancy (with video). Gastrointest. Endosc.73, 267–274 (2011).
- Arcidiacono PG, Calori G, Carrara S et al. Celiac plexus block for pancreatic cancer pain in adults. Cochrane Database Syst. Rev.3, CD007519 (2011).
- Wyse JM, Carone M, Paquin SC et al. Randomized, double-blind, controlled trial of early endoscopic ultrasound-guided celiac plexus neurolysis to prevent pain progression in patients with newly diagnosed, painful, inoperable pancreatic cancer. J. Clin. Oncol.29, 3541–3546 (2011).
- Shami VM, Kahaleh M. Endoscopic ultrasonography (EUS)-guided access and therapy of pancreatico-biliary disorders: EUS-guided cholangio and pancreatic drainage. Gastrointest. Endosc. Clin. N. Am.17, 581–593 (2007).
- Maranki J, Hernandez AJ, Arslan B et al. Interventional endoscopic ultrasound-guided cholangiography: long-term experience of an emerging alternative to percutaneous transhepatic cholangiography. Endoscopy41, 532–538 (2009).
- Püspök A. Biliary therapy: are we ready for EUS-guidance? Minerva Med.98, 379–384 (2007).
- Mallery S, Matlock J, Freeman ML. EUS-guided rendezvous drainage of obstructed biliary and pancreatic ducts: report of 6 cases. Gastrointest. Endosc.59, 100–107 (2004).
- Prat F, Chapat O, Ducot B et al. Predictive factors for survival of patients with inoperable malignant distal biliary strictures: a practical management guideline. Gut42, 76–80 (1998).
- Perdue DG, Freeman ML, DiSario JA et al. Plastic versus self-expanding metallic stents for malignant hilar biliary obstruction: a prospective multicenter observational cohort study. J. Clin. Gastroenterol.42, 1040–1046 (2008).
- Isayama H, Komatsu Y, Tsujino T et al. A prospective randomized study of ‘covered’ versus ‘uncovered’ diamond stents for the management of distal malignant biliary obstruction. Gut53, 729–734 (2004).
- Yoon WJ, Lee JK, Lee KH et al. A comparison of covered and uncovered wallstents for the management of distal malignant biliary obstruction. Gastrointest. Endosc.63, 996–1000 (2006).
- Lawrence C, Howell DA, Conklin DE et al. Delayed pancreaticoduodenectomy for cancer patients with prior ERCP-placed, nonforeshortening, self-expanding metal stents: a positive outcome. Gastrointest. Endosc.63, 804–807 (2006).
- Eshuis WJ, van der Gaag NA, Rauws EA et al. Therapeutic delay and survival after surgery for cancer of the pancreatic head with or without preoperative biliary drainage. Ann. Surg.252, 840–849 (2010).
- Povoski SP, Karpeh MS Jr, Conlon KC, Blumgart LH, Brennan MF. Association of preoperative biliary drainage with postoperative outcome following pancreaticoduodenectomy. Ann. Surg.230, 131–142 (1999).
- Giovannini M, Moutardier V, Pesenti C et al. Endoscopic ultrasound-guided bilioduodenal anastomosis: a new technique for biliary drainage. Endoscopy33, 898–900 (2001).
- Nguyen-Tang T, Binmoeller KF, Sanchez-Yague A et al. Endoscopic ultrasound (EUS)-guided transhepatic anterograde self-expandable metal stent (SEMS) placement across malignant biliary obstruction. Endoscopy42, 232–236 (2010).
- Belletrutti PJ, Gerdes H, Schattner MA. Successful endoscopic ultrasound-guided transduodenal biliary drainage through a pre-existing duodenal stent. JOP11, 234–236 (2010).
- van Heek NT, van Geenen RC, Busch OR, Gouma DJ. Palliative treatment in ‘peri’-pancreatic carcinoma: stenting or surgical therapy? Acta Gastroenterol. (Belg.)65, 171–175 (2002).
- Kruse EJ. Palliation in pancreatic cancer. Surg. Clin. North Am.90, 355–364 (2010).
- Gaidos JK, Draganov PV. Treatment of malignant gastric outlet obstruction with endoscopically placed self-expandable metal stents. World J. Gastroenterol.15, 4365–4371 (2009).
- Mosler P, Mergener KD, Brandabur JJ et al. Palliation of gastric outlet obstruction and proximal small bowel obstruction with self-expandable metal stents: a single center series. J. Clin. Gastroenterol.39, 124–128 (2005).
- Cho YK, Kim SW, Hur WH et al. Clinical outcomes of self-expandable metal stent and prognostic factors for stent patency in gastric outlet obstruction caused by gastric cancer. Dig. Dis. Sci.55, 668–674 (2010).
- Maetani I, Ukita T, Tada T et al. Metallic stents for gastric outlet obstruction: reintervention rate is lower with uncovered versus covered stents, despite similar outcomes. Gastrointest. Endosc.69, 806–812 (2009).
- Yim HB, Jacobson BC, Saltzman JR et al. Clinical outcome of the use of enteral stents for palliation of patients with malignant upper GI obstruction. Gastrointest. Endosc.53, 329–332 (2001).
- Gan SI, Thompson CC, Lauwers GY et al. Ethanol lavage of pancreatic cystic lesions: initial pilot study. Gastrointest. Endosc.61, 746–752 (2005).
- DeWitt J, McGreevy K, Schmidt CM et al. EUS-guided ethanol versus saline solution lavage for pancreatic cysts: a randomized, double-blind study. Gastrointest. Endosc.70, 710–723 (2009).
- Oh HC, Seo DW, Song TJ et al. Endoscopic ultrasonography-guided ethanol lavage with paclitaxel injection treats patients with pancreatic cysts. Gastroenterology140, 172–179 (2011).
- Jürgensen C, Schuppan D, Neser F et al. EUS-guided alcohol ablation of an insulinoma. Gastrointest. Endosc.63, 1059–1062 (2006).
- Deprez PH, Claessens A, Borbath I et al. Successful endoscopic ultrasound-guided ethanol ablation of a sporadic insulinoma. Acta Gastroenterol. (Belg.)71, 333–337 (2008).
- Irisawa A, Takagi T, Kanazawa M et al. Endoscopic ultrasound-guided fine-needle injection of immature dendritic cells into advanced pancreatic cancer refractory to gemcitabine: a pilot study. Pancreas35, 189–190 (2007).
- Verna EC, Dhar V. Endoscopic ultrasound-guided fine needle injection for cancer therapy: the evolving role of therapeutic endoscopic ultrasound. Ther. Adv. Gastroenterol.1, 103–109 (2008).
- Chang KJ, Nguyen PT, Thompson JA et al. Phase I clinical trial of allogeneic mixed lymphocyte culture (cytoimplant) delivered by endoscopic ultrasound-guided fine-needle injection in patients with advanced pancreatic carcinoma. Cancer15, 1325–1335 (2000).
- Farrell JJ, Senzer N, Hecht JR et al. Long-term data for endoscopic ultrasound (EUS) and percutaneous (PTA) guided intratumoral TNFerade gene delivery combined with chemoradiation in the treatment of locally advanced pancreatic cancer (LAPC). Gastrointest. Endosc.63, AB93 (2006) (Abstract).
- Kasuya H, Takeda S, Nomoto S et al. The potential of oncolytic virus therapy for pancreatic cancer. Cancer Gene Ther.12, 725–736 (2005).
- Hecht JR, Bedford R, Abbruzzese JL et al. A phase I/II trial of intratumoral endoscopic ultrasound injection of ONYX-015 with intravenous gemcitabine in unresectable pancreatic carcinoma. Clin. Cancer Res.9, 555–561 (2003).
- Jin Z, Du Y, Li Z et al. Endoscopic ultrasonography-guided interstitial implantation of iodine 125-seeds combined with chemotherapy in the treatment of unresectable pancreatic carcinoma: a prospective pilot study. Endoscopy40, 314–320 (2008).
- Sanders MK, Moser AJ, Khalid A et al. EUS-guided fiducial placement for stereotactic body radiotherapy in locally advanced and recurrent pancreatic cancer. Gastrointest. Endosc.71, 1178–1184 (2010).
- Dimaio CJ, Nagula S, Goodman KA et al. EUS-guided fiducial placement for image-guided radiation therapy in GI malignancies by using a 22-gauge needle (with videos). Gastrointest. Endosc.71, 1204–1210 (2010).
- Magno P, Giday SA, Gabrielson KL et al. EUS-guided submucosal implantation of a radiopaque marker: a simple and effective procedure to facilitate subsequent surgical and radiation therapy. Gastrointest. Endosc.67, 1147–1152 (2008).
- Goldberg SN, Mallery S, Gazelle GS et al. EUS-guided radiofrequency ablation in the pancreas: results in a porcine model. Gastrointest. Endosc.50, 392–401 (1999).
- Chan HH, Nishioka NS, Mino M et al. EUS-guided photodynamic therapy of the pancreas: a pilot study. Gastrointest. Endosc.59, 95–99 (2004).
Pancreatic cancer: an endoscopic perspective
To obtain credit, you should first read the journal article. After reading the article, you should be able to answer the following, related, multiple-choice questions. To complete the questions (with a minimum 70% passing score) and earn continuing medical education (CME) credit, please go to www.medscape.org/journal/expertgastrohep. Credit cannot be obtained for tests completed on paper, although you may use the worksheet below to keep a record of your answers. You must be a registered user on Medscape.org. If you are not registered on Medscape.org, please click on the New Users: Free Registration link on the left hand side of the website to register. Only one answer is correct for each question. Once you successfully answer all post-test questions you will be able to view and/or print your certificate. For questions regarding the content of this activity, contact the accredited provider, [email protected]. For technical assistance, contact [email protected]. American Medical Association’s Physician’s Recognition Award (AMA PRA) credits are accepted in the US as evidence of participation in CME activities. For further information on this award, please refer to http://www.ama-assn.org/ama/pub/category/2922.html. The AMA has determined that physicians not licensed in the US who participate in this CME activity are eligible for AMA PRA Category 1 Credits™. Through agreements that the AMA has made with agencies in some countries, AMA PRA credit may be acceptable as evidence of participation in CME activities. If you are not licensed in the US, please complete the questions online, print the AMA PRA CME credit certificate and present it to your national medical association for review.
Activity Evaluation: Where 1 is strongly disagree and 5 is strongly agree
1. A 60 year-old woman presents with a 3-month history of abdominal pain with distension and weight loss. You are concerned that this patient may have pancreatic cancer. Which of the following statements regarding the diagnosis of pancreatic cancer is most accurate?
□ A Transabdominal ultrasound has a sensitivity of less than 50% in detecting pancreatic tumors
□ B Pancreatic MRI is superior to multidetector CT (MDCT) in detecting pancreatic tumors
□ C Endoscopic ultrasound (EUS) is superior to older CT technology in diagnosing pancreatic tumors less than 3 cm
□ D EUS has now been proven to be superior to MDCT for pancreatic cancer staging
2. The patient is found to have a pancreatic tumor, which requires a tissue diagnosis. What should you consider regarding the use of EUS and endoscopic retrograde cholangiopancreatography (ERCP) for diagnosing pancreatic cancer?
□ A The principal benefit of EUS-guided fine needle aspiration (FNA) is a high negative predictive value
□ B EUS-guided FNA has a complication rate that exceeds 10% and should only be performed by experienced operators
□ C Endobiliary forceps biopsy is superior to brush cytology alone for diagnosis during ERCP
□ D Brush cytology during ERCP is limited by a sensitivity of less than 60%
3. The patient is diagnosed with pancreatic cancer. Which of the following statements regarding the role of EUS during the treatment of pancreatic cancer is most accurate?
□ A Limited research suggests that EUS-guided injection can effectively treat pancreatic cystic neoplasms
□ B EUS-guided injection appears to be most effective for solid pancreatic tumors
□ C EUS-guided radiation therapy is associated with significant survival benefits
□ D EUS-guided placement of fiducials has proven to be unsafe
4. The patient has a poor response to cancer treatment. What should you consider regarding the use of EUS in palliative treatment for this patient?
□ A Alcohol is now considered the standard injectate for all patients requiring celiac plexus block
□ B The complication rate of EUS-guided celiac plexus block may be less than 2%
□ C Self-expanding metal stents (SEMS) should be used for biliary drainage only when the expected survival is less than 6 months
□ D Uncovered metal biliary stents have longer durations of patency compared with covered stents
Notes
ERCP: Endoscopic retrograde cholangiopancreatography; EUS: Endoscopic ultrasound; SEMS: Self-expanding metal stent.